Abstract
Epithelial ovarian cancer (EOC) is the most lethal gynaecological cancer among women worldwide, with the 5-year survival rate ranging between 30 and 40%. Due to the asymptomatic nature of the condition, it is more likely to be diagnosed at an advanced stage, requiring an aggressive therapeutic approach. Cytoreductive surgery (CRS) along with systemic chemotherapy with paclitaxel and carboplatin has been the mainstay of the treatment in the frontline management of EOC. In recent years, neo-adjuvant chemotherapy, followed by interval CRS has become an important strategy for the management of advanced EOC. Due to the high rate of recurrence, the oncology community has begun to shift its focus to molecular-targeted agents and maintenance therapy in the frontline settings. The rationale for maintenance therapy is to delay the progression or relapse of the disease, as long as possible after first-line treatment, irrespective of the amount of residual disease. Tumours with homologous recombination deficiency (HRD) including BReast CAncer gene (BRCA) mutations are found to be sensitive to polyadenosine diphosphate-ribose polymerase (PARP) inhibitors and understanding of HRD status has become important in the frontline setting. PARP inhibitors are reported to provide a significant improvement in progression-free survival and have an acceptable safety profile. PARP inhibitors have also been found to act regardless of BRCA status. Recently, PARP inhibitors as maintenance therapy in the frontline settings showed encouraging results in EOC; however, the results from further trials and survival data from ongoing trials are awaited for understanding the role of this pathway in treatment of EOC. This review discusses an overview of maintenance strategies in newly diagnosed EOC along with considerations for maintenance therapy in EOC with a focus on PARP inhibitors.
Similar content being viewed by others
Introduction
Ovarian cancer (OC) is a lethal gynaecological cancer, with 313,959 new cases and 207,252 deaths, worldwide in 2020 [1]. Among Indian women, OC ranks third after cervical and uterine cancer accounting for approximately 45,701 new cases and 32,077 deaths [1, 2].
Epithelial ovarian cancer (EOC) accounts for over 90% of the OC cases [3]. EOC develops in two different oncogenic pathways. The vast majority follow the type II pathway, present with p53 and BReast CAncer gene (BRCA) mutations, and are high grade serous tumors. Whereas, low-grade serous tumors are characterized by BRAF, KRAS, PTEN, PIK3CA, ARID1A, CTNNB1, and PPP2R1A mutations and progress according to the type I pathway [4]. Due to non-specific symptoms, the disease is usually diagnosed at an advanced stage resulting in a 5-year survival rate ranging between 30 and 40% across the globe, even with optimal care [5].
Cytoreductive surgery (CRS) along with systemic chemotherapy with paclitaxel and carboplatin has been the mainstay of the treatment in the frontline management of EOC for the last 20 years. In recent years, neo-adjuvant chemotherapy, followed by an interval CRS has become an important strategy for the management of advanced OC [6]. In advanced EOC, more than 70% of the patients eventually relapse within 3 years of first-line treatment [7, 8]. With disease progression, other complications such as ascites, bowel obstruction and pleural effusion arise affecting the quality of life. Thus, delaying recurrence or progression of disease and improving survival following first-line treatment is still a significant unmet need in patients with EOC.
At the time of diagnosis, approximately 50% of EOCs exhibit deficiency to repair deoxyribonucleic acid breaks due to alterations (epigenetic and genetic) in homologous recombination repair (HRR) pathway genes [9]. The most prominent one is BRCA mutations in tumour suppressor gene, which accounts for almost 18% of EOC cases [10]. In EOC, germline BRCA (gBRCA) mutations are identified in 13 to 15% of the cases and somatic BRCA mutations are found in 5 to 10% of the cases [11, 12]. The incidence of gBRCA mutation varies widely based on the ethnicity (8 to 17% in Caucasians compared with 15 to 30% in Asians) [13,14,15,16,17,18]. Mutations that interfere with normal function of BRCA are reported to modulate outcomes of treatment with platinum/molecular-targeted drugs [19, 20].
Molecular-targeted drugs─ antiangiogenic agents have demonstrated encouraging results in patients with newly diagnosed advanced OC following first-line treatment [21]. Based on the results of these studies, National Comprehensive Cancer Network®(NCCN®) recommends bevacizumab for targeted therapy with platinum-based chemotherapy and maintenance monotherapy as options in the frontline setting for certain patients with advanced EOC [22]. Post-chemotherapy, maintenance treatment with polyadenosine diphosphate-ribose polymerase (PARP) inhibitors has shown promising results with recurrent disease [23,24,25,26,27]. PARP inhibitors are also recommended as frontline maintenance treatment options for certain patients with EOC [22, 23, 28].
This review explores maintenance therapy as a strategic approach for extended disease control with the intention of prolonging survival in management of newly diagnosed EOC in frontline settings.
Overview of maintenance strategies in epithelial ovarian cancer
Although first-line platinum-based chemotherapy regimen has remained a mainstay in the treatment of EOC, the progression-free survival (PFS) remains poor (< 2 years) necessitating second-line therapies [7, 29,30,31]. The ICON-3 study conducted on patients with histologically confirmed invasive EOC has reported a high relapse rate of above 60% with paclitaxel plus carboplatin regimen [31]. The median PFS period reported in this study was of 17.3 months and median overall survival (OS) of 36.1 months with carboplatin plus paclitaxel regimen [31]. In this context, the maintenance therapy is being studied to delay the progression or relapse of the disease, as long as possible after first-line surgical treatment, irrespective of the amount of residual disease.
Chemotherapeutic agents
Clinical studies (GOG-178 [32], MITO-1 [33], AGO-GINECO [34] and After-6 [35]) examined the efficacy of maintenance treatment with chemotherapeutic agents, 12-cycles of paclitaxel, topotecan, sequential addition of topotecan to carboplatin–paclitaxel, 6-cycles of paclitaxel, respectively after the first-line chemotherapy in improving the prognosis in patients with OC. Studies have revealed a PFS gain of approximately 6 to 8 months when compared with patients who did not receive maintenance therapy, but reported more toxicity and failed to demonstrate survival benefit.
Antiangiogenic drugs
Vascular endothelial growth factor (VEGF) promotes angiogenesis and vascular permeability leading to malignant effusion and disease progression. Patients with high circulating serum levels of VEGF are at an increased risk of disease recurrence and death [36]. The United States (US) Food and Drug Administration (FDA) initially approved bevacizumab, an antiangiogenic drug, in combination with chemotherapy for platinum-resistant recurrent EOC in patients who received no more than two prior chemotherapy regimens based on the results from AURELIA trial [37]. In platinum-sensitive recurrent EOC, bevacizumab was approved in combination with either carboplatin and paclitaxel or carboplatin and gemcitabine, followed by bevacizumab as a single agent, based on the findings from two randomised phase III trials, GOG-0213 [38] and OCEANS [39].
In 2018, the US FDA approved bevacizumab in combination with chemotherapy (carboplatin and paclitaxel), followed by a single agent bevacizumab as maintenance for patients with stage III or IV EOC, after initial surgical resection based on GOG-0218 [40] trial results. GOG-0218 reported an improvement in PFS in patients who received bevacizumab plus chemotherapy followed by bevacizumab maintenance therapy compared with patients who received platinum-based chemotherapy alone (14.1 months vs. 10.3 months, respectively) and no difference was observed in the overall population, in the final protocol-specified analyses [40]. However, in post-hoc subgroup analyses, a significant OS benefit was observed with bevacizumab-concurrent plus maintenance compared with chemotherapy alone in patients with stage IV disease (42.8 months vs. 32.6 months, hazard ratio [HR]: 0.75; 95% confidence interval [CI], 0.59 to 0.95) [41]. ICON-7 study also showed a modest PFS benefit with bevacizumab in patients with less advanced disease (17.3 months vs. 19.8 months, p < 0.004) [21]. However, in high-risk patients (stage III with > 1 cm residual disease or stage IV) a significant improvement in PFS (18.1 months vs. 14.5 months) was observed with corresponding improvement in OS, in an exploratory analyses (39.7 months vs. 30.2 months) [42]. The single-arm ROSiA study reported improved PFS (25.5 months, 95% CI, 23.7 to 27.6 months) with extended use of bevacizumab (continued until progression or for up to 24 months) in combination with paclitaxel after debulking surgery [43].
In BOOST trial (phase III trial) involving patients with stage IIB–IV disease, who underwent primary CRS followed by six cycles of chemotherapy (paclitaxel+carboplatin) and bevacizumab, longer treatment with bevacizumab with carboplatin and paclitaxel for up to 30 months have neither showed PFS nor OS benefit [44].
Several other antiangiogenic drugs such as pazopanib, sorafenib, nintedanib and trebananib have been investigated for the management of EOC; however, none of them have been granted approval due to safety concerns (Table 1) [21, 40,41,42,43, 45,46,47,48,49]. Bevacizumab remains an only antiangiogenic drug in market for the treatment of EOC in both frontline as well as in recurrent settings.
PARP inhibitors
The approval of PARP inhibitors in 2014 for the management of recurrent EOC resulted in a paradigm shift in the treatment landscape. PARP inhibitors are one of the new class of medications for EOC, targeting the DNA repair fragility of tumor cells. PARP inhibitors have been shown to trap enzymes PARP1 and PARP2 on DNA, leading to PARP-DNA complexes. This “trapping of PARP” potentiates synergism between PARP inhibition and both platinum-based chemotherapy and alkylating agents. However, there are remarkable differences in the PARP inhibitors ability to trap PARP, based on the size and structure of each molecule [50]. Among PARP inhibitors that have already been evaluated, olaparib, niraparib, and rucaparib trap PARP 100-fold more efficiently compared to veliparib, whereas talazoparib appears to be the most potent PARP trapper investigated so far. Increased PARP trapping is found to be associated with high myelosuppression, which possibly results in variation of the recommended doses across PARP inhibitors [51].
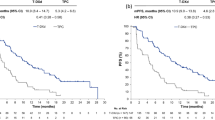
The phase III trials, Study-19 [52, 53], SOLO-2 [24, 25], NOVA [26, 27] and ARIEL-3 [23] have demonstrated PFS benefit with PARP inhibitors maintenance therapy (olaparib, niraparib and rucaparib), in platinum-sensitive recurrent OC. Based on the positive results, the US FDA approved PARP inhibitors for the maintenance treatment of recurrent EOC, fallopian tube or primary peritoneal cancer, in patients who are in complete response (CR) or partial response (PR) to platinum-based chemotherapy. The role of PARP inhibitors as maintenance therapy was evaluated in frontline setting in four phase III trials (SOLO-1 [54], PRIMA [55], PAOLA-1 [56] and VELIA [57]). The details of clinical trials with PARP inhibitors maintenance in OC management are summarised in Table 2.
In SOLO-1 study [54], patients with newly diagnosed stage III-IV, with positive BRCA mutation status showed significant PFS benefit with a 67% risk reduction for disease progression or death in olaparib arm compared with placebo, beyond 5 years (56.0 months vs. 13.8 months, HR: 0.33, 95% CI, 0.25 to 0.43). Olaparib was approved for frontline maintenance therapy in patients with deleterious or suspected deleterious germline or somatic BRCA-mutated EOC, fallopian tube or primary peritoneal cancer based on results of SOLO-1 trial [58].
The PRIMA trial [55] investigated the effectiveness of niraparib first-line maintenance therapy in patients with advanced EOC. A significant improvement in PFS was seen with niraparib over placebo, in the overall population (13.8 months vs. 8.2 months, HR: 0.62, 95% CI, 0.50 to 0.76; p < 0.001) as well as in homologous recombination deficiency (HRD) cohort (21.9 months vs. 10.4 months, HR: 0.43, 95% CI, 0.31 to 0.59, p < 0.001). The homologous recombination-proficient cohort also showed significant improvement in PFS (8.1 months vs. 5.4 months, HR: 0.68, 95% CI, 0.49 to 0.94, p = 0.020); however the magnitude of benefit is much lesser than the other groups. The trial confirmed that the clinical benefit with niraparib frontline maintenance therapy could be extended to all patients with advanced EOC, regardless of HRD status. Niraparib is currently approved for the first-line maintenance treatment of patients with advanced EOC, fallopian tube, or primary peritoneal cancer who are in a complete or partial response to first-line platinum-based chemotherapy [59].
The PAOLA-1 study [56] examined the efficacy of combination therapy of PARP inhibitors with bevacizumab as frontline maintenance therapy in patients with advanced EOC, with complete or partial response to standard platinum-based therapy given with bevacizumab. A significant improvement in PFS was demonstrated in the intention-to-treat population with bevacizumab plus olaparib compared to placebo (22.1 months vs. 16.6 months, HR: 0.59, 95% CI, 0.49 to 0.72, p < 0.0001). An exploratory analyses, in HRD-positive population, an extended PFS benefit has been observed with olaparib plus bevacizumab compared to placebo plus bevacizumab (37.2 months vs. 17.7 months, HR: 0.33; 95% CI, 0.25 to 0.45); no PFS benefit was witnessed in patients with negative HRD status (16.6 months vs. 16.2 months, HR: 1.00, 95% CI, 0.75 to 1.35). In patients with BRCA mutations, an extended PFS has been observed with a 69% risk reduction for disease progression or death in olaparib compared to placebo (37.2 months vs. 21.7 months, HR: 0.31, 95% CI, 0.20 to 0.47) [56]. Olaparib was approved in combination with bevacizumab by the FDA for the first-line maintenance treatment of adult patients with HRD-positive advanced EOC, fallopian tube or primary peritoneal cancer patients who are in CR or PR to first-line platinum-based chemotherapy [58].
The VELIA study [57] assessed the efficacy of veliparib added to first-line therapy with chemotherapy and continued as maintenance monotherapy in patients with newly diagnosed advanced EOC. In the overall population, extended PFS was shown in veliparib cohort (23.5 months vs. 17.3 months, HR: 0.68, 95% CI, 0.56 to 0.83, p < 0.001). In patients with gBRCA mutation, the median PFS was longer with veliparib (34.7 months vs. 22.0 months, HR: 0.44, 95% CI, 0.28 to 0.68, p < 0.001); the benefit was also observed in patients with HRD-positive status (31.9 months vs. 20.5 months, HR: 0.57, 95% CI, 0.43 to 0.76, p < 0.001). No benefit was seen in patients with BRCA wild-type (BRCAwt) disease (HR: 0.80, 95% CI, 0.64 to 1.00) or those with homologous recombination-proficient disease (HR: 0.81, 95% CI, 0.60 to 1.09).
All three studies (PRIMA [55], PAOLA-1 [56], VELIA [57]) were affirmative in the overall population; despite specific genetic aberrations, the HRD-positive patients derived most benefit either due to a BRCA mutation or other HRD.
Novel therapies
In phase III clinical trial (NCT03863860), fuzuloparib (formerly fluzoparib) as maintenance therapy achieved a clinically meaningful and statistically significant improvement in PFS in patients with platinum-sensitive, recurrent OC (12.9 months vs. 5.5 months, 95% CI, 0.17 − 0.36, p < 0.0001) compared with placebo. The risk of disease progression or death was reduced by 75% (HR: 0.25) with manageable safety profile regardless of BRCA mutation status [60].
Immune checkpoint inhibitors
Immune checkpoint inhibitors (ICIs) are drawing attention as drugs that can extend OS. However, the clinical studies on biological maintenance therapies with ICIs have shown neither PFS nor OS benefit [61]. In phase III MIMOSA trial involving stage III-IV OC patients who had complete clinical remission after primary CRS and chemotherapy with platinum and taxane, abagovomab maintenance therapy has showed measurable immune response [62]. However, it did not prolong recurrence-free survival or OS. Several clinical trials for the efficacy of ICIs as first-line maintenance therapy are ongoing (NCT03737643, NCT03038100, NCT03522246) (Table 3). Phase III trials are also currently evaluating combinations of bevacizumab with ICIs in the frontline therapy and maintenance, post to chemotherapy, with data anticipated to emerge over the next 3 years. IMagyn050/GOG 3015/ENGOT OV-39 is one such trial (ICI: atezolizumab, chemotherapy [carboplatin and paclitaxel], which demonstrated no improvement in PFS with ICIs in newly diagnosed OC in the initial results [63].
Considerations for maintenance therapy
Tumour histology
Although EOC is treated as a single entity, each subtype is associated with a discrete clinical behaviour including pattern of metastases, response to systemic chemotherapy and survival [64]. The histological grading (0-3) created based on response to neo-adjuvant chemotherapy in the basis of degree of disappearance of cancer cells, displacement by necrotic and fibrotic tissue and tumour-induced inflammation showed significant association of histological grades 0-1 (HR: 1.65, p = 0.03) with reduced OS. The analyses also confirmed histological grades 0-1 (odds ratio [OR]: 8.42, p = 0.003) as independent predictors of relapse within 6 months [65]. In serous ovarian tumours, the high-grade tumours are found to be associated with shorter OS than low-grade serous cancers [66]. High-grade serous ovarian carcinoma (HGSOC) is known to be associated with higher incidence of BRCA mutations [67]; they have the best response to PARP inhibitors [56]. Interpretation of cellular morphology defines the EOC subtypes and guides appropriate treatment planning based on tumour and patient characteristics, moreover it may also help in understanding the potential need for maintenance therapy [68].
Molecular status and testing
HRD, a lack of functional components in one or more of the DNA repair pathways like the HRR, is a common feature of OC, especially in HGSOC. BRCA mutations (germline or somatic) are the most prevalent mutations among HRR genes (germline or somatic mutations). Testing for BRCA mutation has proved to be an effective diagnostic and prognostic tool in OC [69], as demonstrated by the efficacy of platinum-based drugs in this disease and the advent of PARP inhibitors for the maintenance treatment of these patients with mutations in HRR genes [19, 20, 70]. In a systematic review of 33 studies in patients with primary or recurrent OC (n = 7745) significantly longer PFS (HR: 0.80; 95% CI, 0.64 to 0.99, p = 0.039) and OS (HR: 0.75, 95% CI, 0.64 to 0.88, p < 0.001) were reported in BRCA1/2 mutation carriers in response to platinum-based chemotherapy [20]. In patients with OC, BRCA-mutated patients had a significant PFS benefit compared with BRCAwt cancer (HR: 0.65; 95% CI, 0.44 to 0.98, p = 0.032) with PARP inhibitors; with no significant difference in somatic and germline mutations carriers [19]. Similar results were reported in another study in patients with HGSOC [70]. This effect has also been observed in patient with HRD [71]. Patients with HRD have a better response possibly because of the synergism of cell-damaging effects. In newly diagnosed advanced OC, higher HRD scores have been associated with improved PFS, indicating a prognostic significance to this marker [72]. It is thus imperative to provide genetic testing for HRD and BRCA for making treatment decisions regarding evaluation of response to chemotherapy or targeted therapy or PARP inhibitor maintenance therapy. Medical societies recommend BRCA testing for all patients diagnosed with OC [22]; however, HRD testing may not lag behind because the clinical validity is assessed in terms of PARP inhibitor benefit rather than in terms of biological HRD status. Hence, HRD status is not routinely tested in many countries. Recently, it was reported that HRR mutation analyses should not be considered as a substitute for HRD determination by BRCA or genomic instability testing, since HRR mutation gene panels failed to demonstrate its utility beyond tumour BRCA mutation for selecting patients who may benefit from maintenance olaparib plus bevacizumab in PAOLA-1 trial [73].
The next generation sequencing (NGS) panel, consisting of multiple genes, can detect different genetic aberrations, point mutations, indels and copy number variations in a single test, in short turnaround times. BRCA tumour testing by NGS simultaneously detect both somatic and germline mutations, allowing the identification of more patients with higher likelihood of benefiting from PARP inhibitors. The NGS gene panels are customisable and provide flexibility to select the therapeutically actionable genes. Companion diagnostics can play an important role in selecting the genes for NGS testing. MyChoice® CDx (Myriad® Genetics Inc) was used in PAOLA- 1[56], PRIMA [55] and VELIA [57] trials to select patients who were most likely to derive therapeutic benefit from these PARP inhibitors. For rucaparib FoundationFocus™ CDxBRCA LOH (Foundation Medicine) was utilised to detect somatic BRCA mutations [23]. Maintenance treatment with targeted agents in advanced OC can be cost-effective, when guided by companion diagnostics.
Safety considerations
Though the clinical benefit of maintenance therapy with anti-angiogenic and PARP inhibitors in the frontline setting is evident, they do carry a risk for toxicity resulting in dose interruptions and reductions. The adverse events (AEs) associated with bevacizumab treatment are hypertension, proteinuria, headache and epistaxis and less commonly taste alteration, rhinitis, dry skin, rectal haemorrhage, exfoliative dermatitis, and lacrimation disorder [74]. The most common > = 3 AEs that occurred at a higher incidence in phase III randomised trials for niraparib, olaparib and veliparib were anaemia followed by thrombocytopenia, neutropenia and fatigue/asthenia (Table 4) [28, 55,56,57]. The incidence of grade > =3 AEs was notably higher in the experimental arm compared with placebo arm in PRIMA [55] and VELIA [57] trials and to a lesser extent in the SOLO-1 trial [28]. In PRIMA [55] and VELIA [57] trials, this elevated incidence was driven by frequent grade > =3 haematological AEs and haematological toxicities, whereas in SOLO-1 [28], the most common grade > =3 AE was anaemia. In the PAOLA-1 [56], incidences of grade > =3 AEs went beyond 50% in both olaparib plus bevacizumab and placebo plus bevacizumab maintenance regimen. However, addition of olaparib to bevacizumab did not increase bevacizumab-associated toxicity. Hypertension was the most frequent grade > =3 AE in PAOLA-1 and olaparib did not seem to increase this classic bevacizumab-associated toxicity; in fact, the olaparib-containing arm was associated with lower incidences of all-grade and grade > =3 hypertension compared with the bevacizumab-alone arm [56]. The patients receiving a combination with chemotherapeutic regimen were found to be at a higher risk of haematologic toxicities [75]. Risk of treatment-induced acute myeloid leukaemia and myelodysplastic syndrome for olaparib and niraparib was reported to be < 1.5 and 0.9% respectively [58, 59]. Fatigue, gastrointestinal problems and haematologic toxicities are the common low-grade AEs reported for PARP inhibitors treatment in patients with EOC. The proportion of patients with AEs leading to treatment discontinuation was high with olaparib plus bevacizumab maintenance (20%) compared with niraparib (12%), olaparib (12%) and veliparib maintenance (19%), whereas dose reduction was high (70%) with niraparib [28, 55,56,57]. In health-related quality of life, no clinically significant change has been observed between the PARP inhibitors maintenance and placebo in PRIMA [55], SOLO-1 [28], PAOLA-1 [56] and VELIA [57] trials. Initiation of prophylactic supportive treatments and dose interruptions may allow resumption of the drugs at the same suggested dose level. The AE profile and the clinical status of the patient should be considered while selecting and initiating therapy with PARP inhibitors [76].
According to real-world evidence from the US healthcare claims data focusing on comparative tolerability and dose modifications in patients with OC receiving PARP inhibitor therapy, the risk of experiencing any clinical events of interest (CEI) was significantly higher with niraparib compared with olaparib (OR: 3.23, 95% CI, 1.89 to 5.50, p < 0.001) and rucaparib (OR: 2.07, 95% CI, 1.08 to 3.97, p < 0.05), with no significant difference between rucaparib and olaparib (OR: 1.56, 95% CI, 0.89 to 2.74, p = 0.1). A similar pattern was reported with haematologic CEIs. PARP inhibitor dose decreases were observed in 21.1, 30.2 and 35.1% of olaparib-, rucaparib- and niraparib- treated patients, respectively [77]. In a comparative study evaluating efficacy and tolerability of olaparib, niraparib and rucaparib in BRCA-mutated platinum-sensitive relapsed OC, olaparib demonstrated superior tolerability with reduced odds for grade 3-4 AEs compared with niraparib and rucaparib and a superior tolerability than niraparib for dose reduction [78].
Frontline versus recurrent maintenance – the quintessential paradox
The current treatment landscape for OC has transformed greatly compared with the past decade with the advent and approval of novel therapies. Figure 1 illustrates the evolution of treatment strategies in the management of EOC. The choice of maintenance therapy in frontline or recurrent settings in patients with advanced OC vary based on patient’s clinical features, molecular status, initial therapy and patient’s preferences. Treatment discontinuation is frequently observed with increased lines of therapy in patients with advanced OC [79]. A real-world study reported that approximately half of the treated cohort having a treatment discontinuation or death within the first 4 month or transfer to second-line or later therapies within a few months of initiation of the first-line therapy [80]. A majority (75%) of the patients received standard chemotherapy for advanced disease [80].
Also with multiple relapses, PFS time shortens following each recurrence and subsequent round of therapy (after the first, second, third, fourth and fifth relapse PFS was 10.2, 6.4, 5.6, 4.4 and 4.1 months, respectively) [81]. In advanced cancer, patients may respond well to first-line therapy, but then progress and deteriorate so rapidly that they are unable to receive second-line therapy. Hence, maintenance therapy after induction therapy in frontline setting could be very beneficial in improving survival rates. SOLO-2 trial conducted on patients with platinum-sensitive, relapsed OC and a BRCA mutation has confirmed an OS benefit with olaparib maintenance therapy [24]. Although the improvement in OS with olaparib maintenance therapy was not statistically significant, it was clinically meaningful [24]. The observed PFS benefit in newly diagnosed OC could be possibly due to the introduction of PARP inhibitors at first-line therapy [54]. This could limit the number of patients likely to expire at first tumour progression, along with platinum-resistant relapse within 6 months after the end of chemotherapy and those who would not be benefited from PARP inhibitors during recurrence. With this intent, the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) recommend PARP inhibitors as frontline maintenance therapy options in certain patients with EOC regardless of BRCA status [22]. For patients who did not receive bevacizumab during primary therapy and had CR or PR, the NCCN recommends niraparib therapy as an option in patients with BRCAwt or an unknown status, and olaparib or niraparib as treatment option in patients with BRCA1/2 mutations. In patients with BRCAwt or an unknown status, who had CR or PR and received bevacizumab as a part of primary therapy, bevacizumab alone is recommended as an option for HR proficient or status unknown, and a combination of bevacizumab and olaparib maintenance therapy is recommended as an option for those with HR deficiency. Whereas for patients with BRCA1/2 mutations in CR or PR who received bevacizumab as part of primary therapy, a combination of bevacizumab and olaparib maintenance therapy or olaparib/niraparib alone maintenance therapy are recommended as options [22].
PARP inhibitor combination therapy
In addition to its role as a monotherapy, PARP inhibitor have also proved its use in combination with other DNA-damaging agents, such as chemotherapy and radiation therapy by preventing repair of treatment-induced DNA damage [82]. With the approval of bevacizumab in combination with olaparib, combination therapies with PARP inhibitors are being actively studied. A combination of PARP inhibitors with angiogenesis inhibitors in OC has been studied in several clinical trials [83,84,85,86]. The PARP inhibitor–ICI combination has gained more attention with increased programmed cell death protein-1/programmed death-ligand 1 expression, and lymphocyte infiltration in gBRCA mutated HGSOC compared with BRCAwt disease. The MEDIOLA trial (phase I/II) demonstrated a 70% response rate with olaparib and durvalumab combination therapy in patients with relapsed, platinum-sensitive, BRCA-mutated OC [87].
In the OVARIO study (phase II trial), the addition of niraparib maintenance to first-line platinum-based chemotherapy with bevacizumab demonstrated clinical benefit in patients with advanced OC [88]. In the frontline setting, five ongoing clinical trials (KEYLYNK-001/ENGOT-OV43/MK-7339-001 [Pembrolizumab, Olaparib], FIRST/ENGOT-OV44 [niraparib plus TSR-042], ATHENA [(rucaparib and nivolumab], DUO-O [durvalumab-olaparib], ENGOT-OV39 [atezolizumab, bevacizumab] are investigating a combination of PARP inhibitors and ICIs as first-line maintenance therapy after platinum-based chemotherapy (Table 3).
Apart from the combinations of PARP inhibitors with angiogenesis inhibitors and immune checkpoint inhibitors, other inhibitors that specifically inhibit homologous recombination, such as PI3K-, AKT-, mTOR-, WEE1-, MEK-, and CDK4/6 inhibitors may also be effectively combined with PARP inhibitors [89]. Therapeutically, to sensitize OC with HR proficiency (de novo or acquired) to PARP inhibitors, combinations of PARP inhibitors with drugs that inhibit HR might be an effective approach. In the clinical practice, the target is to reduce overlapping toxicities by optimizing the dose and treatment schedule and use combinations in selected patients who would not benefit from PARP inhibitor monotherapy [89]. Beside, several other novel therapies currently being studied for management of EOC include autologous tumour vaccine (Vigil) [90, 91] and dendritic cell vaccine (SOTIO® DCVAC) [92].
Cost implications
Generally, individuals with cancer need to pay a greater percentage of their treatment costs through coinsurance and deductibles [93]. In most of the cancer patients out-of-pocket cost is a main barrier in starting and adhering to suggested advanced treatments [94]. PARP inhibitors are expensive compared with other available therapies. The out-of-pocket charges may differ depending on the insurance coverage of the patient and the local reimbursement policies. Although most insurance companies arrange for some coverage for PARP inhibitors, the patient’s co-payment may remain unaffordable. The cost of coverage and the size of co-payment may vary geographically. The cost-effective analyses study conducted by Gonzalez et al., reported that universal PARP inhibitor maintenance treatment is cost-effective compared with a biomarker-directed PARP inhibitor strategy [95]. The economic analyses conducted by Tan et al., demonstrated that olaparib has a high potential (87% probability) of being a cost-effective maintenance treatment in Singapore than routine surveillance among patients with advanced OC with BRCA mutations after response to first-line chemotherapy at a willingness-to-pay of Singapore dollar 60,000 per quality-adjusted life-year gained [96].
Conclusion
Antiangiogenic agents and PARP inhibitors have the potential to bridge the unmet need in the management of EOC. Bevacizumab as maintenance treatment has proven its benefit in patients with newly diagnosed advanced EOC at high-risk of disease progression. The use of PARP inhibitors as maintenance with olaparib or niraparib after first-line chemotherapy has shown a significant PFS benefit in the BRCA mutations. The combination maintenance treatment with bevacizumab and PARP inhibitor, olaparib, following first-line chemotherapy has demonstrated encouraging improvement in PFS in the BRCA-mutated and also in the HRD population. Genetic profiling is providing the necessary insights required to determine the sequencing of the available therapies for patients with EOC and help derive maximum benefit. Identification of biomarkers that predict resistance and combination therapies that can help overcome it may prove beneficial. Thus, in the era of personalised cancer medicine, PARP inhibitor maintenance therapy promises to optimise the management and improve outcomes for patients with EOC.
Availability of data and materials
Not applicable.
Abbreviations
- AE:
-
Adverse event
- BRCA :
-
BReast CAncer gene
- BRCAwt:
-
BRCA wild-type
- CEI:
-
Clinical events of interest
- CI:
-
Confidence interval
- CR:
-
Complete response
- CRS:
-
Cytoreductive surgery
- EOC:
-
Epithelial ovarian cancer
- FDA:
-
Food and Drug Administration
- gBRCA :
-
Germline BRCA
- HGSOC:
-
High-grade serous ovarian carcinoma
- HR:
-
Hazard ratio
- HRD:
-
Homologous recombination deficiency
- HRR:
-
Homologous recombination repair
- ICI:
-
Immune checkpoint inhibitor
- NCCN® :
-
National Comprehensive Cancer Network®
- NGS:
-
Next generation sequencing
- OC:
-
Ovarian cancer
- OR:
-
Odds ratio
- OS:
-
Overall survival
- PARP:
-
Polyadenosine diphosphate -ribose polymerase
- PFS:
-
Progression-free survival
- PR:
-
Partial response
- US:
-
United States
- VEGF:
-
Vascular endothelial growth factor
References
Cancer today. n.d. https://gco.iarc.fr/today/online-analysis-table?v=2020&mode=cancer&mode_population=countries&population=900&populations=900&key=asr&sex=2&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=17&group_cancer=1&include_nmsc=1&include_nmsc_other=1. Accessed 25 May 2021.
Cancer tomorrow. n.d. https://gco.iarc.fr/tomorrow/en/dataviz/tables?cancers=25&populations=356&types=1. Accessed 25 May 2021.
Sankaranarayanan R, Ferlay J. Worldwide burden of gynaecological cancer: the size of the problem. Best Pract Res Clin Obstet Gynaecol. 2006;20:207–25. https://doi.org/10.1016/j.bpobgyn.2005.10.007.
Pavlidis N, Rassy E, Vermorken JB, Assi T, Kattan J, Boussios S, et al. The outcome of patients with serous papillary peritoneal cancer, fallopian tube cancer, and epithelial ovarian cancer by treatment eras: 27 years data from the SEER registry. Cancer Epidemiol. 2021;75:102045. https://doi.org/10.1016/j.canep.2021.102045.
Allemani C, Weir HK, Carreira H, Harewood R, Spika D, Wang X-S, et al. Global surveillance of cancer survival 1995-2009: analysis of individual data for 25,676,887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet. 2015;385:977–1010. https://doi.org/10.1016/S0140-6736(14)62038-9.
Kehoe S, Hook J, Nankivell M, Jayson GC, Kitchener H, Lopes T, et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomised, controlled, non-inferiority trial. Lancet. 2015;386:249–57. https://doi.org/10.1016/S0140-6736(14)62223-6.
du Bois A, Reuss A, Pujade-Lauraine E, Harter P, Ray-Coquard I, Pfisterer J. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials. Cancer. 2009;115:1234–44. https://doi.org/10.1002/cncr.24149.
Ledermann JA, Raja FA, Fotopoulou C, Gonzalez-Martin A, Colombo N, Sessa C, et al. Newly diagnosed and relapsed epithelial ovarian carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(Suppl 6):vi24–32. https://doi.org/10.1093/annonc/mdt333.
Colombo N, Sessa C, du Bois A, Ledermann J, McCluggage WG, McNeish I, et al. ESMO-ESGO consensus conference recommendations on ovarian cancer: pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease†. Ann Oncol. 2019;30:672–705. https://doi.org/10.1093/annonc/mdz062.
Manchana T, Phoolcharoen N, Tantbirojn P. BRCA mutation in high grade epithelial ovarian cancers. Gynecol Oncol Rep. 2019;29:102–5. https://doi.org/10.1016/j.gore.2019.07.007.
Konstantinopoulos PA, Norquist B, Lacchetti C, Armstrong D, Grisham RN, Goodfellow PJ, et al. Germline and somatic tumor testing in epithelial ovarian cancer: ASCO guideline. J Clin Oncol. 2020;38:1222–45. https://doi.org/10.1200/JCO.19.02960.
Sugino K, Tamura R, Nakaoka H, Yachida N, Yamaguchi M, Mori Y, et al. Germline and somatic mutations of homologous recombination-associated genes in Japanese ovarian cancer patients. Sci Rep. 2019;9:17808. https://doi.org/10.1038/s41598-019-54116-y.
Zhang S, Royer R, Li S, McLaughlin JR, Rosen B, Risch HA, et al. Frequencies of BRCA1 and BRCA2 mutations among 1,342 unselected patients with invasive ovarian cancer. Gynecol Oncol. 2011;121:353–7. https://doi.org/10.1016/j.ygyno.2011.01.020.
Paradiso AV, Digennaro M, Patruno M, De Summa S, Tommasi S, Berindan-Neagoe I. BRCA germline mutation test for all woman with ovarian cancer? BMC Cancer. 2019;19. https://doi.org/10.1186/s12885-019-5829-4.
Alsop K, Fereday S, Meldrum C, deFazio A, Emmanuel C, George J, et al. BRCA mutation frequency and patterns of treatment response in BRCA mutation–positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group. J Clin Oncol. 2012;30:2654–63. https://doi.org/10.1200/JCO.2011.39.8545.
Gupta S, Rajappa S, Advani SH, Agarwal A, Aggarwal S, Goswami C, et al. 226O - prevalence of germline BRCA1 and BRCA2 mutations and variants among ovarian, primary peritoneal and fallopian tube cancer patients: a multicentre Indian study. Ann Oncol. 2019;30:ix78. https://doi.org/10.1093/annonc/mdz426.002.
Singh J, Thota N, Singh S, Padhi S, Mohan P, Deshwal S, et al. Screening of over 1000 Indian patients with breast and/or ovarian cancer with a multi-gene panel: prevalence of BRCA1/2 and non-BRCA mutations. Breast Cancer Res Treat. 2018;170:189–96. https://doi.org/10.1007/s10549-018-4726-x.
Mehta A, Vasudevan S, Sharma SK, Kumar D, Panigrahi M, Suryavanshi M, et al. Germline BRCA1 and BRCA2 deleterious mutations and variants of unknown clinical significance associated with breast/ovarian cancer: a report from North India. Cancer Manag Res. 2018;10:6505–16. https://doi.org/10.2147/CMAR.S186563.
Hennessy BTJ, Timms KM, Carey MS, Gutin A, Meyer LA, Flake DD, et al. Somatic mutations in BRCA1 and BRCA2 could expand the number of patients that benefit from poly (ADP ribose) polymerase inhibitors in ovarian cancer. J Clin Oncol. 2010;28:3570–6. https://doi.org/10.1200/JCO.2009.27.2997.
Huang Y-W. Association of BRCA1/2 mutations with ovarian cancer prognosis: an updated meta-analysis. Medicine (Baltimore). 2018;97:e9380. https://doi.org/10.1097/MD.0000000000009380.
Perren TJ, Swart AM, Pfisterer J, Ledermann JA, Pujade-Lauraine E, Kristensen G, et al. A phase 3 trial of bevacizumab in ovarian cancer. N Engl J Med. 2011;365:2484–96. https://doi.org/10.1056/NEJMoa1103799.
The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Epithelial Ovarian Cancer/Fallopian Tube Cancer/Primary Peritoneal Cancer V.1.2022. © National Comprehensive Cancer Network, Inc. 2022. All rights reserved. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way. Accessed 25 Jan 2022.
Coleman RL, Oza AM, Lorusso D, Aghajanian C, Oaknin A, Dean A, et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:1949–61. https://doi.org/10.1016/S0140-6736(17)32440-6.
Pujade-Lauraine E, Ledermann JA, Selle F, Gebski V, Penson RT, Oza AM, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1274–84. https://doi.org/10.1016/S1470-2045(17)30469-2.
Poveda A, Floquet A, Ledermann JA, Asher R, Penson RT, Oza AM, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a final analysis of a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2021;22:620–31. https://doi.org/10.1016/S1470-2045(21)00073-5.
Mirza MR, Monk BJ, Herrstedt J, Oza AM, Mahner S, Redondo A, et al. Niraparib maintenance therapy in platinum-sensitive, recurrent ovarian cancer. N Engl J Med. 2016;375:2154–64. https://doi.org/10.1056/NEJMoa1611310.
Matulonis U, Herrstedt J, Oza A, Mahner S, Redondo A, Berton D, et al. Long-term safety and secondary efficacy endpoints in the ENGOT-OV16/NOVA phase III trial of niraparib in recurrent ovarian cancer. Gynecol Oncol. 2021;162:S24–5. https://doi.org/10.1016/S0090-8258(21)00693-4.
Moore K, Colombo N, Scambia G, Kim B-G, Oaknin A, Friedlander M, et al. Maintenance olaparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med. 2018;379:2495–505. https://doi.org/10.1056/NEJMoa1810858.
Möbus V, Wandt H, Frickhofen N, Bengala C, Champion K, Kimmig R, et al. Phase III trial of high-dose sequential chemotherapy with peripheral blood stem cell support compared with standard dose chemotherapy for first-line treatment of advanced ovarian cancer: intergroup trial of the AGO-Ovar/AIO and EBMT. J Clin Oncol. 2007;25:4187–93. https://doi.org/10.1200/JCO.2006.09.7527.
Bookman MA, Brady MF, McGuire WP, Harper PG, Alberts DS, Friedlander M, et al. Evaluation of new platinum-based treatment regimens in advanced-stage ovarian cancer: a Phase III Trial of the Gynecologic Cancer Intergroup. J Clin Oncol. 2009;27:1419–25. https://doi.org/10.1200/JCO.2008.19.1684.
International Collaborative Ovarian Neoplasm Group. Paclitaxel plus carboplatin versus standard chemotherapy with either single-agent carboplatin or cyclophosphamide, doxorubicin, and cisplatin in women with ovarian cancer: the ICON3 randomised trial. Lancet. 2002;360:505–15. https://doi.org/10.1016/S0140-6736(02)09738-6.
Markman M, Liu PY, Moon J, Monk BJ, Copeland L, Wilczynski S, et al. Impact on survival of 12 versus 3 monthly cycles of paclitaxel (175 mg/m2) administered to patients with advanced ovarian cancer who attained a complete response to primary platinum-paclitaxel: follow-up of a Southwest Oncology Group and Gynecologic Oncology Group phase 3 trial. Gynecol Oncol. 2009;114:195–8. https://doi.org/10.1016/j.ygyno.2009.04.012.
De Placido S, Scambia G, Di Vagno G, Naglieri E, Lombardi AV, Biamonte R, et al. Topotecan compared with no therapy after response to surgery and carboplatin/paclitaxel in patients with ovarian cancer: Multicenter Italian Trials in Ovarian Cancer (MITO-1) randomized study. J Clin Oncol. 2004;22:2635–42. https://doi.org/10.1200/JCO.2004.09.088.
Pfisterer J, Weber B, Reuss A, Kimmig R, du Bois A, Wagner U, et al. Randomized phase III trial of topotecan following carboplatin and paclitaxel in first-line treatment of advanced ovarian cancer: a gynecologic cancer intergroup trial of the AGO-OVAR and GINECO. J Natl Cancer Inst. 2006;98:1036–45. https://doi.org/10.1093/jnci/djj296.
Pecorelli S, Favalli G, Gadducci A, Katsaros D, Panici PB, Carpi A, et al. Phase III trial of observation versus six courses of paclitaxel in patients with advanced epithelial ovarian cancer in complete response after six courses of paclitaxel/platinum-based chemotherapy: final results of the after-6 protocol 1. J Clin Oncol. 2009;27:4642–8. https://doi.org/10.1200/JCO.2009.21.9691.
Bandiera E, Franceschini R, Specchia C, Bignotti E, Trevisiol C, Gion M, et al. Prognostic significance of vascular endothelial growth factor serum determination in women with ovarian cancer. ISRN Obst Gynecol. 2012;2012:1–11. https://doi.org/10.5402/2012/245756.
Pujade-Lauraine E, Hilpert F, Weber B, Reuss A, Poveda A, Kristensen G, et al. Bevacizumab combined with chemotherapy for platinum-resistant recurrent ovarian cancer: the AURELIA open-label randomized phase III trial. J Clin Oncol. 2014;32:1302–8. https://doi.org/10.1200/JCO.2013.51.4489.
Coleman RL, Brady MF, Herzog TJ, Sabbatini P, Armstrong DK, Walker JL, et al. Bevacizumab and paclitaxel-carboplatin chemotherapy and secondary cytoreduction in recurrent, platinum-sensitive ovarian cancer (NRG Oncology/Gynecologic Oncology Group study GOG-0213): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2017;18:779–91. https://doi.org/10.1016/S1470-2045(17)30279-6.
Aghajanian C, Blank SV, Goff BA, Judson PL, Teneriello MG, Husain A, et al. OCEANS: a randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. J Clin Oncol. 2012;30:2039–45. https://doi.org/10.1200/JCO.2012.42.0505.
Burger RA, Brady MF, Bookman MA, Fleming GF, Monk BJ, Huang H, et al. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N Engl J Med. 2011;365:2473–83. https://doi.org/10.1056/NEJMoa1104390.
Burger RA, Enserro D, Tewari KS, Brady MF, Bookman MA, Fleming GF, et al. Final overall survival (OS) analysis of an international randomized trial evaluating bevacizumab (BEV) in the primary treatment of advanced ovarian cancer: a NRG oncology/Gynecologic Oncology Group (GOG) study. JCO. 2018;36:5517. https://doi.org/10.1200/JCO.2018.36.15_suppl.5517.
Oza AM, Cook AD, Pfisterer J, Embleton A, Ledermann JA, Pujade-Lauraine E, et al. Standard chemotherapy with or without bevacizumab for women with newly diagnosed ovarian cancer (ICON7): overall survival results of a phase 3 randomised trial. Lancet Oncol. 2015;16:928–36. https://doi.org/10.1016/S1470-2045(15)00086-8.
Oza AM, Selle F, Davidenko I, Korach J, Mendiola C, Pautier P, et al. Efficacy and safety of bevacizumab-containing therapy in newly diagnosed ovarian cancer: ROSiA single-arm phase 3B study. Int J Gynecol Cancer. 2017;27:50–8. https://doi.org/10.1097/IGC.0000000000000836.
Pfisterer J, Joly F, Kristensen G, Rau J, Mahner S, Pautier P, et al. Optimal treatment duration of bevacizumab (BEV) combined with carboplatin and paclitaxel in patients (pts) with primary epithelial ovarian (EOC), fallopian tube (FTC) or peritoneal cancer (PPC): a multicenter open-label randomized 2-arm phase 3 ENGOT/GCIG trial of the AGO Study Group, GINECO, and NSGO (AGO-OVAR 17/BOOST, GINECO OV118, ENGOT Ov-15, NCT01462890). JCO. 2021;39:5501. https://doi.org/10.1200/JCO.2021.39.15_suppl.5501.
Herzog TJ, Scambia G, Kim B-G, Lhommé C, Markowska J, Ray-Coquard I, et al. A randomized phase II trial of maintenance therapy with Sorafenib in front-line ovarian carcinoma. Gynecol Oncol. 2013;130:25–30. https://doi.org/10.1016/j.ygyno.2013.04.011.
du Bois A, Floquet A, Kim J-W, Rau J, del Campo JM, Friedlander M, et al. Incorporation of pazopanib in maintenance therapy of ovarian cancer. J Clin Oncol. 2014;32:3374–82. https://doi.org/10.1200/JCO.2014.55.7348.
Vergote I, du Bois A, Floquet A, Rau J, Kim J-W, Del Campo JM, et al. Overall survival results of AGO-OVAR16: a phase 3 study of maintenance pazopanib versus placebo in women who have not progressed after first-line chemotherapy for advanced ovarian cancer. Gynecol Oncol. 2019;155:186–91. https://doi.org/10.1016/j.ygyno.2019.08.024.
Ray-Coquard I, Cibula D, Mirza MR, Reuss A, Ricci C, Colombo N, et al. Final results from GCIG/ENGOT/AGO-OVAR 12, a randomised placebo-controlled phase III trial of nintedanib combined with chemotherapy for newly diagnosed advanced ovarian cancer. Int J Cancer. 2020;146:439–48. https://doi.org/10.1002/ijc.32606.
Vergote I, Scambia G, O’Malley DM, Van Calster B, Park S-Y, Del Campo JM, et al. Trebananib or placebo plus carboplatin and paclitaxel as first-line treatment for advanced ovarian cancer (TRINOVA-3/ENGOT-ov2/GOG-3001): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2019;20:862–76. https://doi.org/10.1016/S1470-2045(19)30178-0.
Boussios S, Karihtala P, Moschetta M, Abson C, Karathanasi A, Zakynthinakis-Kyriakou N, et al. Veliparib in ovarian cancer: a new synthetically lethal therapeutic approach. Investig New Drugs. 2020;38:181–93. https://doi.org/10.1007/s10637-019-00867-4.
Boussios S, Moschetta M, Karihtala P, Samartzis EP, Sheriff M, Pappas-Gogos G, et al. Development of new poly(ADP-ribose) polymerase (PARP) inhibitors in ovarian cancer: Quo Vadis? Ann Transl Med. 2020;8:1706. https://doi.org/10.21037/atm.2020.03.156.
Ledermann J, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian cancer. N Engl J Med. 2012;366:1382–92. https://doi.org/10.1056/NEJMoa1105535.
Ledermann J, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, et al. Olaparib maintenance therapy in patients with platinum-sensitive relapsed serous ovarian cancer: a preplanned retrospective analysis of outcomes by BRCA status in a randomised phase 2 trial. Lancet Oncol. 2014;15:852–61. https://doi.org/10.1016/S1470-2045(14)70228-1.
Banerjee S, Moore KN, Colombo N, Scambia G, Kim B-G, Oaknin A, et al. 811MO Maintenance olaparib for patients (pts) with newly diagnosed, advanced ovarian cancer (OC) and a BRCA mutation (BRCAm): 5-year (y) follow-up (f/u) from SOLO1. Ann Oncol. 2020;31:S613. https://doi.org/10.1016/j.annonc.2020.08.950.
González-Martín A, Pothuri B, Vergote I, DePont Christensen R, Graybill W, Mirza MR, et al. Niraparib in patients with newly diagnosed advanced ovarian cancer. N Engl J Med. 2019;381:2391–402. https://doi.org/10.1056/NEJMoa1910962.
Ray-Coquard I, Pautier P, Pignata S, Pérol D, González-Martín A, Berger R, et al. Olaparib plus Bevacizumab as first-line maintenance in ovarian cancer. N Engl J Med. 2019;381:2416–28. https://doi.org/10.1056/NEJMoa1911361.
Coleman RL, Fleming GF, Brady MF, Swisher EM, Steffensen KD, Friedlander M, et al. Veliparib with first-line chemotherapy and as maintenance therapy in ovarian cancer. N Engl J Med. 2019;381:2403–15. https://doi.org/10.1056/NEJMoa1909707.
AstraZeneca. Lynparza, FDA Label. n.d.
GlaxoSmithKline. ZEJULA (Niraparib). Label. n.d.
Fuzuloparib maintenance therapy improves progression-free survival in patients with recurrent ovarian cancer - The ASCO Post. n.d. https://ascopost.com/issues/may-25-2021/fuzuloparib-maintenance-therapy-improves-progression-free-survival-in-patients-with-recurrent-ovarian-cancer/. Accessed 16 Nov 2021.
Hall GD, Brown JM, Coleman RE, Stead M, Metcalf KS, Peel KR, et al. Maintenance treatment with interferon for advanced ovarian cancer: results of the northern and Yorkshire gynaecology group randomised phase III study. Br J Cancer. 2004;91:621–6. https://doi.org/10.1038/sj.bjc.6602037.
Sabbatini P, Harter P, Scambia G, Sehouli J, Meier W, Wimberger P, et al. Abagovomab as maintenance therapy in patients with epithelial ovarian cancer: a phase III trial of the AGO OVAR, COGI, GINECO, and GEICO—the MIMOSA study. J Clin Oncol. 2013;31:1554–61. https://doi.org/10.1200/JCO.2012.46.4057.
Moore KN, Bookman M, Sehouli J, Miller A, Anderson C, Scambia G, et al. Atezolizumab, bevacizumab, and chemotherapy for newly diagnosed stage III or IV ovarian cancer: placebo-controlled randomized phase III trial (IMagyn050/GOG 3015/ENGOT-OV39). J Clin Oncol. 2021;39:1842–55. https://doi.org/10.1200/JCO.21.00306.
Banerjee S, Kaye SB. New strategies in the treatment of ovarian cancer: current clinical perspectives and future potential. Clin Cancer Res. 2013;19:961–8. https://doi.org/10.1158/1078-0432.CCR-12-2243.
Muraji M, Sudo T, Iwasaki S, Ueno S, Wakahashi S, Yamaguchi S, et al. Histopathology predicts clinical outcome in advanced epithelial ovarian cancer patients treated with neoadjuvant chemotherapy and debulking surgery. Gynecol Oncol. 2013;131:531–4. https://doi.org/10.1016/j.ygyno.2013.09.030.
Kosary CL. FIGO stage, histology, histologic grade, age and race as prognostic factors in determining survival for cancers of the female gynecological system: an analysis of 1973-87 SEER cases of cancers of the endometrium, cervix, ovary, vulva, and vagina. Semin Surg Oncol. 1994;10:31–46. https://doi.org/10.1002/ssu.2980100107.
Lisio M-A, Fu L, Goyeneche A, Gao Z, Telleria C. High-grade serous ovarian cancer: basic sciences, clinical and therapeutic standpoints. Int J Mol Sci. 2019;20:952. https://doi.org/10.3390/ijms20040952.
Jayson GC, Kohn EC, Kitchener HC, Ledermann JA. Ovarian cancer. Lancet. 2014;384:1376–88. https://doi.org/10.1016/S0140-6736(13)62146-7.
Konstantinopoulos PA, Ceccaldi R, Shapiro GI, D’Andrea AD. Homologous recombination deficiency: exploiting the fundamental vulnerability of ovarian cancer. Cancer Discov. 2015;5:1137–54. https://doi.org/10.1158/2159-8290.CD-15-0714.
Hodgson DR, Dougherty BA, Lai Z, Fielding A, Grinsted L, Spencer S, et al. Candidate biomarkers of PARP inhibitor sensitivity in ovarian cancer beyond the BRCA genes. Br J Cancer. 2018;119:1401–9. https://doi.org/10.1038/s41416-018-0274-8.
Huang X, Jia H, Xiao Q, Li R, Wang X, Yin H, et al. Efficacy and prognostic factors for PARP inhibitors in patients with ovarian cancer. Front Oncol. 2020;10:958. https://doi.org/10.3389/fonc.2020.00958.
Ngoi NYL, Tan DSP. The role of homologous recombination deficiency testing in ovarian cancer and its clinical implications: do we need it? ESMO Open. 2021;6:100144. https://doi.org/10.1016/j.esmoop.2021.100144.
Pujade-Lauraine E, Brown J, Barnicle A, Rowe P, Lao-Sirieix P, Criscione S, et al. Homologous recombination repair mutation gene panels (excluding BRCA) are not predictive of maintenance olaparib plus bevacizumab efficacy in the first-line PAOLA-1/ENGOT-ov25 trial. Gynecol Oncol. 2021;162:S26–7. https://doi.org/10.1016/S0090-8258(21)00695-8.
Randall LM, Monk BJ. Bevacizumab toxicities and their management in ovarian cancer. Gynecol Oncol. 2010;117:497–504. https://doi.org/10.1016/j.ygyno.2010.02.021.
Zhou JX, Feng LJ, Zhang X. Risk of severe hematologic toxicities in cancer patients treated with PARP inhibitors: a meta-analysis of randomized controlled trials. Drug Des Devel Ther. 2017;11:3009–17. https://doi.org/10.2147/DDDT.S147726.
Pothuri B, O’Cearbhaill R, Eskander R, Armstrong D. Frontline PARP inhibitor maintenance therapy in ovarian cancer: a Society of Gynecologic Oncology practice statement. Gynecol Oncol. 2020;159:8–12. https://doi.org/10.1016/j.ygyno.2020.07.097.
Arend R, O’Malley D, Banerjee S, McLaurin K, Davidson R, Long G. Comparative tolerability and dose modifications of poly(ADP-ribose) polymerase inhibitors in ovarian cancer: a retrospective cohort study of US healthcare claims data. Gynecol Oncol. 2021;162:S116. https://doi.org/10.1016/S0090-8258(21)00862-3.
Sackeyfio A, Nussey F, Friedlander M, Pujade-Lauraine E. Comparative efficacy and tolerability of the PARP inhibitors, olaparib 300 mg tablets BID, niraparib 300 mg capsules QD and rucaparib 600 mg tablets BID as maintenance treatment in BRCA -mutated ( BRCA m) platinum-sensitive relapsed ovarian. Gynecol Oncol. 2018;149:43–4. https://doi.org/10.1016/j.ygyno.2018.04.094.
Houben E, van Haalen HGM, Sparreboom W, Overbeek JA, Ezendam NPM, Pijnenborg JMA, et al. Chemotherapy for ovarian cancer in the Netherlands: a population-based study on treatment patterns and outcomes. Med Oncol. 2017;34:50. https://doi.org/10.1007/s12032-017-0901-x.
Beachler DC, Lamy F-X, Russo L, Taylor DH, Dinh J, Yin R, et al. A real-world study on characteristics, treatments and outcomes in US patients with advanced stage ovarian cancer. J Ovarian Res. 2020;13:101. https://doi.org/10.1186/s13048-020-00691-y.
Hanker LC, Loibl S, Burchardi N, Pfisterer J, Meier W, Pujade-Lauraine E, et al. The impact of second to sixth line therapy on survival of relapsed ovarian cancer after primary taxane/platinum-based therapy. Ann Oncol. 2012;23:2605–12. https://doi.org/10.1093/annonc/mds203.
Boussios S, Karathanasi A, Cooke D, Neille C, Sadauskaite A, Moschetta M, et al. PARP inhibitors in ovarian cancer: the route to “Ithaca”. Diagnostics (Basel). 2019;9:55. https://doi.org/10.3390/diagnostics9020055.
Dean E, Middleton MR, Pwint T, Swaisland H, Carmichael J, Goodege-Kunwar P, et al. Phase I study to assess the safety and tolerability of olaparib in combination with bevacizumab in patients with advanced solid tumours. Br J Cancer. 2012;106:468–74. https://doi.org/10.1038/bjc.2011.555.
Mirza MR, Bergmann TK, Mau-Sørensen M, dePont Christensen R, Åvall-Lundqvist E, Birrer MJ, et al. A phase I study of the PARP inhibitor niraparib in combination with bevacizumab in platinum-sensitive epithelial ovarian cancer: NSGO AVANOVA1/ENGOT-OV24. Cancer Chemother Pharmacol. 2019;84:791–8. https://doi.org/10.1007/s00280-019-03917-z.
Mirza MR, Åvall Lundqvist E, Birrer MJ, dePont Christensen R, Nyvang G-B, Malander S, et al. Niraparib plus bevacizumab versus niraparib alone for platinum-sensitive recurrent ovarian cancer (NSGO-AVANOVA2/ENGOT-ov24): a randomised, phase 2, superiority trial. Lancet Oncol. 2019;20:1409–19. https://doi.org/10.1016/S1470-2045(19)30515-7.
Liu JF, Barry WT, Birrer M, Lee J-M, Buckanovich RJ, Fleming GF, et al. Combination cediranib and olaparib versus olaparib alone for women with recurrent platinum-sensitive ovarian cancer: a randomised phase 2 study. Lancet Oncol. 2014;15:1207–14. https://doi.org/10.1016/S1470-2045(14)70391-2.
Drew Y, Kaufman B, Banerjee S, Lortholary A, Hong SH, Park YH, et al. 1190PD - phase II study of olaparib + durvalumab (MEDIOLA): updated results in germline BRCA-mutated platinum-sensitive relapsed (PSR) ovarian cancer (OC). Ann Oncol. 2019;30:v485–6. https://doi.org/10.1093/annonc/mdz253.016.
Hardesty M, Krivak T, Wright G, Hamilton E, Fleming E, Belotte J, et al. Phase II OVARIO study of niraparib + bevacizumab therapy in advanced ovarian cancer following front-line platinum-based chemotherapy with bevacizumab. Gynecol Oncol. 2021;162:S17. https://doi.org/10.1016/S0090-8258(21)00679-X.
Boussios S, Karihtala P, Moschetta M, Karathanasi A, Sadauskaite A, Rassy E, et al. Combined strategies with poly (ADP-ribose) polymerase (PARP) inhibitors for the treatment of ovarian cancer: a literature review. Diagnostics. 2019;9:87. https://doi.org/10.3390/diagnostics9030087.
Rocconi RP, Grosen EA, Ghamande SA, Chan JK, Barve MA, Oh J, et al. Gemogenovatucel-T (Vigil) immunotherapy as maintenance in frontline stage III/IV ovarian cancer (VITAL): a randomised, double-blind, placebo-controlled, phase 2b trial. Lancet Oncol. 2020;21:1661–72. https://doi.org/10.1016/S1470-2045(20)30533-7.
Oh J, Barve M, Matthews CM, Koon EC, Heffernan TP, Fine B, et al. Phase II study of Vigil® DNA engineered immunotherapy as maintenance in advanced stage ovarian cancer. Gynecol Oncol. 2016;143:504–10. https://doi.org/10.1016/j.ygyno.2016.09.018.
Cibula D, Mallmann P, Knapp P, Melichar B, Klat J, Minar L, et al. Dendritic cell vaccine (DCVAC) with chemotherapy (ct) in patients (pts) with recurrent epithelial ovarian carcinoma (EOC) after complete response (CR) to 1st-line platinum (Pt)-based ct: primary analysis of a phase 2, open-label, randomized, multicenter trial. J Clin Oncol. 2018;36:e17515. https://doi.org/10.1200/JCO.2018.36.15_suppl.e17515.
Schnipper LE, Davidson NE, Wollins DS, Tyne C, Blayney DW, Blum D, et al. American Society of Clinical Oncology statement: a conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33:2563–77. https://doi.org/10.1200/JCO.2015.61.6706.
Dusetzina SB, Winn AN, Abel GA, Huskamp HA, Keating NL. Cost sharing and adherence to tyrosine kinase inhibitors for patients with chronic myeloid leukemia. J Clin Oncol. 2014;32:306–11. https://doi.org/10.1200/JCO.2013.52.9123.
Gonzalez R, Havrilesky LJ, Myers ER, Secord AA, Dottino JA, Berchuck A, et al. Cost-effectiveness analysis comparing “PARP inhibitors-for-all” to the biomarker-directed use of PARP inhibitor maintenance therapy for newly diagnosed advanced stage ovarian cancer. Gynecol Oncol. 2020;159:483–90. https://doi.org/10.1016/j.ygyno.2020.08.003.
Tan DS, Chan JJ, Hettle R, Ghosh W, Viswambaram A, Yu CC. Cost-effectiveness of olaparib versus routine surveillance in the maintenance setting for patients with BRCA-mutated advanced ovarian cancer after response to first-line platinum-based chemotherapy in Singapore. J Gynecol Oncol. 2021;32:e27. https://doi.org/10.3802/jgo.2021.32.e27.
Acknowledgements
The authors would like to thank AstraZeneca Pharma India Ltd., Bangalore for the development of this manuscript in collaboration with Dr. Sasikala Somara, Labcorp Scientific Services & Solutions Pvt. Ltd. in accordance with GPP3 guidelines (http://www.ismpp.org/gpp3).
Funding
The preparation of this review article and funding of the journal’s article processing charges was supported by AstraZeneca Pharma India Limited. All authors had full access to all the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analyses.
Author information
Authors and Affiliations
Contributions
All named authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Authors don’t have any competing interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nag, S., Aggarwal, S., Rauthan, A. et al. Maintenance therapy for newly diagnosed epithelial ovarian cancer– a review. J Ovarian Res 15, 88 (2022). https://doi.org/10.1186/s13048-022-01020-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13048-022-01020-1