Abstract
Background
Chronic myeloid leukemia (CML) is genetically characterized by the occurrence of a reciprocal translocation t(9;22)(q34;q11), resulting in a BCR/ABL gene fusion on the derivative chromosome 22, i.e. the Philadelphia (Ph) chromosome. During CML progression 60–80% of the cases acquire additional genetic changes. Even though hyperdiploidy is not a rare finding in advanced phase-CML, hyperdiploidy together with a T315I kinase domain (KD) mutation in the BCR-ABL gene has not yet been reported.
Results
A complete cytogenetic and molecular cytogenetic analysis; molecular biology methods such as quantitative reverse transcription polymerase chain reaction (RQ-PCR) and allele-specific oligonucleotide (ASO)-PCR; and immunophenotypically confirmed CML in acceleration phase (AP). Our case revealed the presence of hyperdiploidy including multiple copies of the Ph chromosome, presence of b3a2 fusion transcript,T315I mutation in BCR-ABL KD in pre imatinib mesylate (IM) treatment. The ratio of BCR-ABL/ABL expression in post nilotinib treatment was 0.07% on international scale.
Conclusions
The patient demonstrated a good response to nilotinib after imatinib failure; while the hyperdiploid clone disappeared the T315I mutation remained during follow-up. The underlying mechanisms and prognostic implications of these cytogenetic abnormalities are discussed.
Similar content being viewed by others
Background
Chronic myeloid leukemia (CML) is a disorder characterized by the formation of granulocytes in connection with a translocation involving chromosomes 9 and 22. Resulting derivative chromosome 22 is called Philadelphia chromosome (Ph) [1]. A simple reciprocal translocation of t(9;22)(q34;q11) can be observed as single aberration in the early stage chronic phase (CP) whereas in most advanced cases this change is accompanied by other chromosomal aberrations. In fact, a chimeric gene BCR-ABL gene and protein is formed. The fused gene has an oncogenic activity and encodes for an active tyrosine kinase [2]. Hyperdiploidy is not common in CML cases [3] and it is a common finding in advanced phase-CML patients [4],[5] and it was already in one CML-CP patient as a secondary chromosomal aberration after imatinib mesylate (IM) therapy [6].
Imatinib (IM = Glivec, formerly STI571) is a chemically designed drug which blocks BCR/ABL1 tyrosine kinase activity and is successfully used in CML patients [7]. Nilotinib is a second generation tyrosine kinase inhibiter (TKI) with improved target specificity and potency. Nilotinib acts like IM and binds to the kinase domain (KD) of ABL1. This prevents the formation of an active conformation, catalyzing the transduction of the BCR-ABL signal [8]. Nilotinib was approved for CML treatment in CP and AP especially in cases showing IM resistance due to mutations in BCR-ABL tyrosine kinase geneor intolerance to prior successful IM therapy [9],[10]. T315I is one of the most frequent mutations in the BCR-ABL domain and has been associated with TKI resistance of 1st and 2nd generation drugs [11].
Here we presented a new CML case in AP pre IM treatment with hyperdiploidy including more than one copy of the Ph chromosome, presence of b3a2 fusion transcript, a T315I mutation in the BCR-ABL KD, and a ratio of BCR-ABL/ABL1 expression post nilotinib treatment was 0.07% on international scale (IS). This patient demonstrated a good response to nilotinib after imatinib failure.
Case presentation
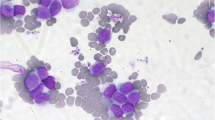
In June 2012 a 53-year-old male was diagnosed as suffering from CML. Physical examination revealed hepatosplenomegaly, several skin nodules (2 cm) in different locations such as neck and armpit (data not shown), anemia, thrombocytopenia, fever, fatigue, and loss of weight were the indicative symptoms. The patient’s hematologic parameters were white blood cells (WBC) of 52.2x109/l (15% of cells were blasts), red blood cell (RBC) count was 2.50x106/mm3, hemoglobin level was 7.1 g/dl and the platelet count was 90x109/l. Serum lactate dehydrogenase value (LDH) was 1,851 U/l (normal level <460 U/l). The patient was diagnosed as CML-AP according to WHO recommendations and in an intermediate Sokal risk of 0.89 (0.8-1.2). No treatment had been administered prior to the test.
The patient was referred for a second time in November 2013 and was treated with IM (400 mg/day) for 5 months. Thus therapeutic scheme was changed to nilotinib (600 mg/day) for 6 months with disappeared the previous reported relevant symptoms. The more recent hematological parameters were: WBC 5.3x109/l (50.2% neutrophils, 48.1% lymphocytes, 0.9% monocytes and 0.8% eosinophiles). The platelet count was 118x109/l and the hemoglobin level was 12.4 g/dl.
Results
Pre IM treatment banding cytogenetics revealed a karyotype of 46,XY,t(9;22)[7]/56,XY,+3,+6,+7,+8,+8,+9,t(9;22),+10,+12,+19,+der(22)t(9;22)[5]/57,XY,+3,+6,+7,+8,+8,+9,t(9;22),+10,+12,+15,-18,+19,+der(22)t(9;22)x 2[8]. Post nilotinib treatment banding cytogenetics revealed a karyotype of 46,XY,t(9;22)[1]/46,XY[39] (Figure 1). Further studies were done based on molecular cytogenetics (Figure 2) and molecular genetics (Figure 3). Dual-color-FISH pre IM treatment; using a specific probe for BCR and ABL1 revealed onefusion signal on the derivative chromosomes 9 [der(9)] and another three fusion signals on the up to three Ph chromosomes (Figure 2); and chromosomes 3, 6, 7, 8, 9, 10, 12, 15, 19 and 22, were studied with WCP and/or CEP probes and did not provide any hint on cryptic translocations (data not shown). RT-PCR pre IM treatment and post nilotinib treatment confirmed the presence of the BCR-ABL1 fusion (b3a2 transcript) revealing a major M-BCR transcript (data not shown). RQ-PCR post nilotinib treatment demonstrated a ratio of BCR-ABL/ABL1 expression of 0.07% on IS (data not shown). ASO-PCR pre IM treatment and post nilotinib treatment results showed the presence of the T315I mutation (Figure 3, (Figure 4). The final karyotype pre IM treatment and post nilotinib treatment was determined:
ASO-PCR monitoring and corresponding sensitivity test for detected T315I mutation pre-IM treatment. ASO-PCR products on genomic DNA obtained from healthy donor and our patient. Line M, 1 kb DNA ladder; lines 1,2 blank; lines 3–10 patients ASO-PCR T315I wild-type primers; P, our patient; lines 11–18 ASO-PCR T315I mutated primers; and P*, our patient with T315I mutation.
Pre IM treatment : 46,XY,t(9;22)(q34;q11.2)[7]/56,XY,+3,+6,+7,+8,+8,t(9;22)(q34;q11.2),+10,+12,+19,+der(22)t(9;22)(q34;q11.2)[5]/57,XY,+3,+6,+7,+8,+8,t(9;22)(q34;q11.2),+10,+12,+15,-18,+19,+der(22)t(9;22)(q34;q11.2)x 2[8], and post nilotinib treatment: 46,XY,t(9;22)(q34;q11.2)[1]/46,XY[39].
The abnormal cell population (~19% blasts in peripheral blood specimen) showed the following immunophenotype, which was consistent with CML-AP (WHO recommendations): CD45+, CD34+, CD10+, CD19−, CD20−, CD22−, CD5− and CD7−, HLADr−, CD33+, CD32+, CD16−, CD117−, CD14−, CD15−, CD64− and expressed CD11c, CD38, CD235a and CD13 heterogeneously.
Conclusions
Presence of multiple copies of the Ph chromosome is one of several types of IM resistance mechanisms [12],[13].
According to the literature, there are a few near triploid karyotypes reported in advanced phase-CML [14],[15]. Stagno et al. [2] found a CML case in blast phase with hyperdiploidy and it includes 10% mutant clones with V256G mutation in BCR-ABL domain and e13a2 BCR-ABL transcript. In this paper, we described a new CML case in AP with hyperdiploidy including multiple copies of Ph chromosome, presence of b3a2 fusion transcript and T315I mutation in the BCR-ABL KD. To the best of our knowledge, these chromosomal abnormalities, particularly hyperdiploidy associated with T315I mutation have not been previously observed in CML [16].
Approximately 10% of CML patients present in advanced phases called CML-AP or blast crisis (CML-BC), without a clinically evident CP [17]. Even with the advent of TKI therapy, the phase of disease remains an important prognostic factor in CML [18],[19].
Disease progression is uncommon currently in CML patients treated in CP with TKI. When it occurs, progression usually occurs early during treatment. 3.3% of CML-CP patients progressed to CML-AP/CML-BC within the first 18 months of therapy, while <1% progressed after 4 years of therapy [20]. The criteria for CML-AP in patients progressing on TKI therapy are still poorly defined and disease progression in CML is currently defined more practically in terms of responsiveness to TKI therapy [16].
The progression to advanced phases of disease is caused by the development of genetic lesions in addition to BCR-ABL; secondary cytogenetic changes are identified in 50-80% of CML- BC cases [21]. Also this phenomenon was described in 5-10% of patients presenting with CML-CP and in 30% of patients developing AP features, and has overall been associated with poor prognosis [22],[23]. Cytogenetic clonal evolution was subsequently considered as one of the factors defining CML-AP [24].
The most common mechanism of secondary resistance to TKI is mutation in the KD of BCR-ABL. These KD mutations develop as a result of selection pressure and correlate with progression to advanced phases and shortened survival. Thus, early identification of IM resistance is critical to allow the use of other, potentially effective therapies, such as second generation TKI and/or stem cell transplantation [25].
The mutation at amino acid 315 in the imatinib-binding site (T315I mutation) confers resistance to imatinib, dasatnib, and nilotinib by preventing access of these drugs to the ATP-binding pocket [26]-[28]. Hughes et al. [29] found six cases (5 IM resistant and one IM intolerant, i.e. six in total) with T315I mutation and two of the six cases did not showed responses to Nilotinib but couldn’t sustain. In addition, Jabbour et al. [30] found one case of CML-AP with T315I mutation and complete cytogenetic response to Nilotinib. Also, Jabbour et al. [31] found of CML-AP with T315I mutation and Nilotinib resistance. However, T315I mutation also was observed in 10 cases post IM failure (4 CP, 5 AP, and 1 blast phase) and 2 cases post Nilotinib treatment in the study by Cortes et al. [32]. Cea et al. [33] also found T315I mutation post IM, post Nilotinib and during Dasatinib treatment in e19a2 BCR/ABL1 CML. Our patient achieved a major cytogenetic response and major molecular response after 6 months of nilotinib treatment with T315I mutation remaining.
The mechanisms by which these mutations develop are poorly understood. KD mutations can be present at low-levels in CML cases prior to exposure to TKI therapy. However, these small mutant clones do not necessarily confer an adverse prognosis and resistant clones may not expand even under the selection pressure of TKI therapy [34],[35]. The KD mutations usually occur within the first 2 years of TKI therapy and are much more common in CML-AP and CML-BC than CML-CP [7].
In conclusion, we described a new CML case in AP pre IM treatment with hyperdiploidy including multiple copies of Ph chromosome, and presence of T315I mutation in the BCR-ABL KD. The patient demonstrated a good response to nilotinib treatment after imatinib course failure. Interestingly hyperdiploidy clone disappeared while the T315I mutation remained.
Materials and methods
Chromosome analysis
Chromosome analysis applying GTG-banding according to standard procedures [36] was performed pre IM treatment and post nilotinib treatment. 20 metaphase cells derived from unstimulated bone marrow culture were analyzed. Karyotypes were described according to the International System for Human Cytogenetic Nomenclature (ISCN 2009).
Molecular cytogenetics
Fluorescence in situ hybridization (FISH) using the LSI BCR/ABL dual color dual fusion translocation probe (Abbott Molecular/Vysis, Des Plaines, IL, USA) and/or chromosome enumeration probes (CEP) for chromosomes 6, 7, 8 and/or 12 (Abbott Molecular/Vysis, Des Plaines, IL, USA) were applied together with whole chromosome painting (WCP) probes for chromosomes 3, 9, 10, 15, 19 and/or 22 (MetaSystems, Altlussheim, Germany) according to manufacturer’s instructions [36]. A minimum of 10 metaphase spreads was analyzed, using a fluorescence microscope (AxioImager.Z1 mot, Carl Zeiss Ltd., Hertfordshir, UK) equipped with appropriate filter sets to discriminate between a maximum of five fluorochromes plus the counterstain DAPI (4′,6- diamino-2-phenylindole). Image capture and processing were performed using an ISIS imaging system (MetaSystems, Altlussheim, Germany).
Reverse transcriptase-polymerase chain reaction (RT-PCR) and quantitative reverse transcription polymerase chain reaction (RQ-PCR) for BCR/ABL1 fusion transcripts
Total RNA extracted from peripheral blood sample using the InviTrap RNA kit (Invitek, Berlin, Germany) according to the manufacturer’s recommendations. cDNA was prepared from 5 μg of total RNA with the Genequality BCR-ABL1 kit (AB Analitica, Padova, Italy) and BCR-ABL1 fusion transcript was performed according to the manufacturer’s instructions (AB Analitica, Padova, Italy). RQ-PCR analyses were performed in StepOne Real-Time PCR (Applied Biosystems, Foster City, California, USA) using one-step qRT-PCR BCR-ABL1 kit (MolecularMD, Portland, USA) according to the manufacturer’s recommendations.
Allele-specific oligonucleotide (ASO)-PCR
Mutated or wild-type sequences were amplified in a noncompetitive PCR reaction performed on genomic DNA and PCR conditions using allele-specific and reverse primers for the Thr315Ile mutation as described previously. The length of the PCR product using 1 Kb DNA ladder (Fermentas, Lithuania, Vilnius) was (158 bp). The sensitivity of this assay was determined for each mutation by amplification of 10-fold limited dilutions of 100 ng patient’s DNA at time of resistance in 100 ng healthy control DNA [37].
Flow cytometricimmunophenotype
Flow cytometry of leukemic blasts was performed using a general panel of fluorescent antibodies against the following antigens typical for different cell lineages and cell types: CD1a, CD2, CD3, CD4, CD5, CD8, CD10, CD11b, CD11c, CD13, CD14, CD15, CD16, CD19, CD20, CD22, CD23, CD32, CD33, CD34, CD38, CD41a, CD45, CD56, CD57, CD64, CD103, CD117, CD123, CD209, CD235a and CD243; in addition antibodies against Kappa and Lambda light Chains, sIgD, sIgM, and HLADr were applied (BD Biosciences). Four-color immunophenotyping on peripheral blood specimen was performed. Samples were stained and analyzed on a BD FACSCalibur™ flow cytometer according to BD Biosciences manuals and products insert sheets. Autofluorescence, viability, and isotype controls were included. Flow cytometric data acquisition and analysis were conducted by BD Cellquest™ Pro software.
Consent
Written informed consent was obtained from the patient for publication of this Case Report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Johansson B, Fioretos T, Mitelman F: Cytogenetic and molecular genetic evolution of chronic myeloid leukemia. Acta Haematol 2002, 107: 76–94. 10.1159/000046636
Stagno F, Vigneri P, Consoli ML, Cupri A, Stella S, Tambè L, Massimino M, Manzella L, Di Raimondo F: Hyperdiploidy associated with a high BCR-ABL transcript level may identify patients at risk of progression in chronic myeloid leukemia. Acta Haematol 2012, 127: 7–9. 10.1159/000330607
Belurkar S, Manohar C, Kurien A: Chronic myeloid leukemia with hyperdiploidy: a case report with review of literature. Indian J Med Sci 2013, 67: 188–192. 10.4103/0019-5359.125881
Calabretta B, Perrotti D: The biology of CML blast crisis. Blood 2004, 103: 11. 10.1182/blood-2003-12-4111
Roland B, Blahey Walter B: A case of near triploidy in chronic myelogenousleukemia. Cancer Genet Cytogenet 2000, 121: 96–98. 10.1016/S0165-4608(00)00227-2
Fabarius A, Leitner A, Hochhaus A, Müller MC, Hanfstein B, Haferlach C, Göhring G, Schlegelberger B, Jotterand M, Reiter A, Jung-Munkwitz S, Proetel U, Schwaab J, Hofmann WK, Schubert J, Einsele H, Ho AD, Falge C, Kanz L, Neubauer A, Kneba M, Stegelmann F, Pfreundschuh M, Waller CF, Spiekermann K, Baerlocher GM, Lauseker M, Pfirrmann M, Hasford J, Saussele S, Hehlmann R: SchweizerischeArbeitsgemeinschaftfürKlinischeKrebsforschung (SAKK) and the German CML Study Group: Impact of additional cytogenetic aberrations at diagnosis on prognosis of CML: long-term observation of 1151 patients from the randomized CML Study IV. Blood 2011, 118: 6760–6768. 10.1182/blood-2011-08-373902
Druker BJ, Guilhot F, O’Brien SG, Gathmann I, Kantarjian H, Gattermann N, Deininger MW, Silver RT, Goldman JM, Stone RM, Cervantes F, Hochhaus A, Powell BL, Gabrilove JL, Rousselot P, Reiffers J, Cornelissen JJ, Hughes T, Agis H, Fischer T, Verhoef G, Shepherd J, Saglio G, Gratwohl A, Nielsen JL, Radich JP, Simonsson B, Taylor K, Baccarani M, So C, Letvak L, Larson RA: IRIS Investigators: Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. NEngl J Med 2006, 355: 2408–2417. 10.1056/NEJMoa062867
Weisberg E, Manley P, Mestan J, Cowan-Jacob S, Ray A, Griffin JD: AMN107 (nilotinib): a novel and selective inhibitor of BCR–ABL. Br J Cancer 2006, 94: 765–1769. 10.1038/sj.bjc.6603170
Tojo A, Usuki K, Urabe A, Maeda Y, Kobayashi Y, Jinnai I, Ohyashiki K, Nishimura M, Kawaguchi T, Tanaka H, Miyamura K, Miyazaki Y, Hughes T, Branford S, Okamoto S, Ishikawa J, Okada M, Usui N, Tanii H, Amagasaki T, Natori H, Naoe T: A phase I/II study of nilotinib in Japanese patients with imatinib-resistant or- intolerant Ph + CML or relapsed/refractory Ph + ALL. Int J Hematol 2009, 89: 679–688. 10.1007/s12185-009-0327-0
Cang S, Liu D: P-loop mutations and novel therapeutic approaches for imatinib failures in chronic myeloid leukemia. J Hematol Oncol 2008, 1: 15. 10.1186/1756-8722-1-15
Branford S, Melo JV, Hughes TP: Selecting optimal second-line tyrosine kinase inhibitor therapy for chronic myeloid leukemia patients after imatinib failure: does the BCR-ABL mutation status really matter? Blood 2009, 114: 5426–5435. 10.1182/blood-2009-08-215939
Otero L, Ornellas MH, Dobbin J, de Souza FT: Double Philadelphia-chromosome: a resistance factor on the imatinibmesylate therapy for chronic myeloid leukemia. Int J Lab Hematol 2008, 30: 346–348. 10.1111/j.1751-553X.2007.00957.x
Ossard- Receveur A, Bernheim A, Clausse B, Danglot G, Fauvet D, Leon B, Lozach F: Duplication of the Ph-chromosome as a possible mechanism of resistance to imatinibmesylate in patients with chronic myelogenous leukemia. Cancer Genet Cytogenet 2005, 163: 189–190. 10.1016/j.cancergencyto.2005.05.004
Amiel A, Yukla M, Gaber E, Leopold L, Josef G, Fejgin M, Lishner M: Random aneuploidy in CML patients at diagnosis and under imatinibtreatment. Cancer Genet Cytogenet 2006, 168: 120–123. 10.1016/j.cancergencyto.2006.02.002
Sheth FJ, Sheth JJ, Desai C: Case of near triploidy with i(17)(q10) in blast crisis CML. Cancer Genet Cytogenet 2006, 164: 177–178. 10.1016/j.cancergencyto.2005.07.022
Baccarani M, Saglio G, Goldman J, Hochhaus A, Simonsson B, Appelbaum F, Apperley J, Cervantes F, Cortes J, Deininger M, Gratwohl A, Guilhot F, Horowitz M, Hughes T, Kantarjian H, Larson R, Niederwieser D, Silver R, Hehlmann R: European LeukemiaNet: Evolving concepts in the management of chronic myeloid leukemia: recommendations from an expert panel on behalf of the European Leukemia- Net. Blood 2006, 108: 1809–1820. 10.1182/blood-2006-02-005686
Quintas-Cardama A, Cortes JE: Chronic myeloid leukemia: diagnosis and treatment. Mayo Clin Proc 2006, 81: 973–988. 10.4065/81.7.973
Jabbour E, Kantarjian H, Jones D, Talpaz M, Bekele N, O’Brien S, Zhou X, Luthra R, Garcia-Manero G, Giles F, Rios MB, Verstovsek S, Cortes J: Frequency and clinical significance of BCR-ABL mutations in patients with chronic myeloid leukemia treated with imatinibmesylate. Leukemia 2006, 20: 1767–1773. 10.1038/sj.leu.2404318
Mitchell B, Deininger M: Techniques for risk stratification of newly diagnosed patients with chronic myeloid leukemia. Leuk Lymphoma 2011, 52: 4–11. 10.3109/10428194.2010.546916
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F, Cornelissen JJ, Fischer T, Hochhaus A, Hughes T, Lechner K, Nielsen JL, Rousselot P, Reiffers J, Saglio G, Shepherd J, Simonsson B, Gratwohl A, Goldman JM, Kantarjian H, Taylor K, Verhoef G, Bolton AE, Capdeville R, Druker BJ: IRIS Investigators: Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 2003, 348: 994–1004. 10.1056/NEJMoa022457
Feng J, Le Beau MM, Larson RA, Rowley JD, Vardiman JW: The relationship between secondary chromosomal abnormalities and blast transformation in chronic myelogenousleukemia. Leukemia 1995, 9: 628–633.
Swolin B, Weinfeld A, Westin J, Waldenström J, Magnusson B: Karyotypic evolution in Ph-positive chronic myeloid leukemia in relation to management and disease progression. Cancer Genet Cytogenet 1985, 18: 65–79. 10.1016/0165-4608(85)90041-X
Sokal JE, Gomez GA, Baccarani M, Tura S, Clarkson BD, Cervantes F, Rozman C, Carbonell F, Anger B, Heimpel H: Prognostic significance of additional cytogenetic abnormalities at diagnosis of Philadelphia chromosome-positive chronic granulocytic leukemia. Blood 1988, 72: 294–298.
Kantarjian HM, Dixon D, Keating MJ, Talpaz M, Walters RS, McCredie KB, Freireich EJ: Characteristics of accelerated disease in chronic myelogenousleukemia. Cancer 1988, 61: 1441–1446. 10.1002/1097-0142(19880401)61:7<1441::AID-CNCR2820610727>3.0.CO;2-C
Soverini S, Martinelli G, Rosti G, Bassi S, Amabile M, Poerio A, Giannini B, Trabacchi E, Castagnetti F, Testoni N, Luatti S, de Vivo A, Cilloni D, Izzo B, Fava M, Abruzzese E, Alberti D, Pane F, Saglio G, Baccarani M: ABL mutations in late chronic phase chronic myeloid leukemia patients with upfront cytogenetic resistance to imatinib are associated with a greater likelihood of progression to blast crisis and shorter survival: a study by the GIMEMA Working Party on Chronic Myeloid Leukemia. J Clin Oncol 2005, 23: 4100–4109. 10.1200/JCO.2005.05.531
Hasserjian RP: Chronic myelogenous leukemia in the age of imatinib: assessing response, acceleration, and blast phase. J Hematopathol 2011, 4: 81–92. 10.1007/s12308-011-0093-9
Apperley JF, Cortes JE, Kim DW, Roy L, Roboz GJ, Rosti G, Bullorsky EO, Abruzzese E, Hochhaus A, Heim D, de Souza CA, Larson RA, Lipton JH, Khoury HJ, Kim HJ, Sillaber C, Hughes TP, Erben P, Van Tornout J, Stone RM: Dasatinib in the treatment of chronic myeloid leukemia in accelerated phase after imatinib failure: the START A trial. J Clin Oncol 2009, 27: 3472–3479. 10.1200/JCO.2007.14.3339
O’Hare T, Walters DK, Stoffregen EP, Jia T, Manley PW, Mestan J, Cowan-Jacob SW, Lee FY, Heinrich MC, Deininger MW, Druker BJ: In vitro activity of Bcr-Abl inhibitors AMN107 and BMS-354825 against clinically relevant imatinibresistantAbl kinase domain mutants. Cancer Res 2005, 65: 4500–4505. 10.1158/0008-5472.CAN-05-0259
Hughes T, Saglio G, Branford S, Soverini S, Kim DW, Müller MC, Martinelli G, Cortes J, Beppu L, Gottardi E, Kim D, Erben P, Shou Y, Haque A, Gallagher N, Radich J, Hochhaus A: Impact of baseline BCR-ABL mutations on response to nilotinib in patients with chronic myeloid leukemia in chronic phase. J Clin Oncol 2009, 27: 4204–4210. 10.1200/JCO.2009.21.8230
Jabbour E, Kantarjian H, Jones D, Breeden M, Garcia-Manero G, O’Brien S, Ravandi F, Borthakur G, Cortes J: Characteristics and outcomes of patients with chronic myeloid leukemia and T315I mutation following failure of imatinibmesylatetherapy. Blood 2008, 112: 53–55. 10.1182/blood-2007-11-123950
Jabbour E, Cortés JE, Kantarjian H: Second-line therapy and beyond resistance for the treatment of patients with chronic myeloid leukemia post imatinibfailure. Clin Lymphoma Myeloma 2009, 9: S272-S279. 10.3816/CLM.2009.s.023
Cortes J, Jabbour E, Kantarjian H, Yin CC, Shan J, O’Brien S, Garcia-Manero G, Giles F, Breeden M, Reeves N, Wierda WG, Jones D: Dynamics of BCR-ABL kinase domain mutations in chronic myeloid leukemia after sequential treatment with multiple tyrosine kinase inhibitors. Blood 2007, 110: 4005–4011. 10.1182/blood-2007-03-080838
Cea M, Cirmena G, Garuti A, Rocco I, Palermo C, Cagnetta A, Moran E, Colombo N, Grasso R, Fugazza G, Gobbi M, Nencioni A, Ballestrero A, Patrone F: A T315I mutation in e19a2 BCR/ABL1 chronic myeloid leukemia responding to dasatinib. Leuk Res 2010, 34: e240-e242. 10.1016/j.leukres.2010.03.036
O’Hare T, Eide CA, Deininger MW: Bcr-Abl kinase domain mutations, drug resistance, and the road to a cure for chronic myeloid leukemia. Blood 2007, 110: 2242–2249. 10.1182/blood-2007-03-066936
Willis SG, Lange T, Demehri S, Otto S, Crossman L, Niederwieser D, Stoffregen EP, McWeeney S, Kovacs I, Park B, Druker BJ, Deininger MW: High-sensitivity detection of BCR-ABL kinase domain mutations in imatinib-naive patients: correlation with clonal cytogenetic evolution but not response to therapy. Blood 2005, 106: 2128–2137. 10.1182/blood-2005-03-1036
AL-achkar W, Wafa A, Nweder MS: A complex translocation t(5;9;22) in Philadelphia cells involving the short arm of chromosome 5 in a case of chronic myelogenousleukemia. J Exp Clin Cancer Res 2007, 26: 411–415.
Roche-Lestienne C, Soenen-Cornu V, Grardel-Duflos N, Laï JL, Philippe N, Facon T, Fenaux P, Preudhomme C: Several types of mutations of the Abl gene can be found in chronic myeloid leukemia patients resistant to STI571, and they can pre-exist to the onset of treatment. Blood 2002, 100: 1014–1018. 10.1182/blood.V100.3.1014
Acknowledgements
We thank Prof. I. Othman, the Director General of Atomic Energy Commission of SYRIA (AECS) and Dr. N. Mirali, Head of Molecular Biology and Biotechnology Department for their support. This work was supported by the AECS, in parts by the DAAD.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
AW and FM provided the case and/or did primary cytogenetic and main part of the FISH-tests; AA did the flow cytometry analysis; TL and MAKO did detailed FISH studies. WA supervised the cytogenetic analysis as Director of the MBBD. AW and TL drafted the paper and all authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Al-Achkar, W., Moassass, F., Ikhtiar, A. et al. Hyperdiploidy associated with T315I mutation in BCR-ABL kinase domain in an accelerated phase-chronic myeloid leukemia case. Mol Cytogenet 7, 89 (2014). https://doi.org/10.1186/s13039-014-0089-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13039-014-0089-0