Abstract
Background
The impacts of COVID-19 are unprecedented globally. The pandemic is reversing decades of progress in maternal, newborn, child health and nutrition (MNCHN), especially fragile and conflict-affected settings (FCAS) whose populations were already facing challenges in accessing basic health and nutrition services. This study aimed to investigate the collateral impact of COVID-19 on funding, services and MNCHN outcomes in FCAS, as well as adaptations used in the field to continue activities.
Methods
A scoping review of peer-reviewed and grey literature published between 1st March 2020–31st January 2021 was conducted. We analysed 103 publications using a narrative synthesis approach. 39 remote semi-structured key informant interviews with humanitarian actors and donor staff within 12 FCAS were conducted between October 2020 and February 2021. Thematic analysis was undertaken independently by two researchers on interview transcripts and supporting documents provided by key informants, and triangulated with literature review findings.
Results
Funding for MNCHN has been reduced or suspended with increase in cost of continuing the same activities, and diversion of MNCHN funding to COVID-19 activities. Disruption in supply and demand of interventions was reported across different settings which, despite data evidence still being missing, points towards likely increased maternal and child morbidity and mortality. Some positive adaptations including use of technology and decentralisation of services have been reported, however overall adaptation strategies have been insufficient to equitably meet additional challenges posed by the pandemic, and have not been evaluated for their effectiveness.
Conclusions
COVID-19 is further exacerbating negative women’s and children’s health outcomes in FCAS. Increased funding is urgently required to re-establish MNCHN activities which have been deprioritised or halted. Improved planning to sustain routine health services and enable surge planning for emergencies with focus on the community/service users throughout adaptations is vital for improved MNCHN outcomes in FCAS.
Similar content being viewed by others
Introduction
It is estimated that 274 million people will need humanitarian assistance and protection in 2022, of which women and children make up the majority [1]. COVID-19 has had unprecedented health, social and economic impacts globally. It has exacerbated pre-existing inequalities in maternal, newborn, and child health (MNCH) outcomes, with fragile and conflict-affected settings (FCAS) particularly at risk given that these settings reported considerably worse health outcomes compared to other contexts even before the pandemic [2]. This is in large part due to the fragility of the health systems in FCAS, which are operating with restricted resources, decreased numbers of healthcare workers, interrupted supplies and damaged health facilities [3]. The impacts of the pandemic in FCAS are also disproportionately affecting women and children due to existing factors of vulnerability including lack of decision-making power, the gendered role of women as caregivers increasing their risk of virus exposure, and exacerbation of sexual and gender-based violence [4]. Yet, whilst women’s and children’s health and nutrition needs are increasing, essential services for them are now even more difficult to access and utilise, and existing health needs and humanitarian crises have become “secondary” due to the pandemic as COVID-19 measures are prioritised over maintaining essential health services [5].
Evaluations of humanitarian responses to previous crises including the Ebola epidemic in the Democratic Republic of Congo (DRC) and West Africa and the cholera outbreak in Yemen have provided numerous lessons and insights into the impact of outbreaks on health outcomes for vulnerable populations in FCAS [6,7,8]. Evidence from previous outbreaks clearly demonstrates that maintaining essential health care services is critical to reduce additional deaths and that the indirect effects of outbreaks and epidemics exceed the mortality and morbidity caused by it [7, 9]. This is particularly evident in contexts without resilient health systems, such as FCAS. Previous research evaluating indirect crises-related maternal and neonatal deaths in Sierra Leone during the Ebola epidemic found large reductions in antenatal care, family planning, facility delivery and postnatal care with estimates of at least 3600 additional maternal, neonatal and stillbirth deaths in the year 2014–2015 [8].
In previous epidemics in FCAS such as Ebola and Zika, there has been a diversion of funding and other resources (such as staff and supplies) away from MNCH and towards the health emergency presented by the epidemic [10]. This has implications for MNCH service provision and outcomes. In previous epidemics, it resulted in increased stillbirth, maternal and neonatal mortality, as well as compromising quality of care such as with poor infection control practices leading to nosocomial Ebola infection of pregnant women. Additionally, poor quality of care was a deterrent to attendance at MNCH healthcare facilities [10]. There is evidence to suggest funding diversions are occurring in the COVID-19 pandemic away from routine and essential healthcare and towards pandemic response in several humanitarian settings [5]. Whilst this publication is focussed on non-communicable diseases, it raises concerns for funding in MNCHN—particularly in the context of MNCH funding diversions seen in prior epidemics.
There have been a number of studies to date assessing the impact of the COVID-19 pandemic on maternal, newborn, child health and nutrition (MNCHN) outcomes and service utilisation globally demonstrating adverse indirect impacts including increased sexual and gender-based violence, reduced prenatal visits, overwhelmed healthcare infrastructure and implementation of potentially harmful policies despite little evidence [11,12,13,14]. However, no studies to date have focused exclusively on FCAS. To our knowledge, ours is the first study to document the impact of COVID-19 on MNCHN outcomes, funding and programming in FCAS as well as documenting adaptations used in these settings. Our study aims to take an exploratory and explanatory approach to examine this and highlight areas for further research. It intends to provide reflections for donors, humanitarian actors and others working in this sector to improve policy and programming for women and children during and beyond the COVID-19 pandemic.
Methods
This study used mixed methods drawing on two data sources: (1) a scoping literature review and (2) key informant interviews with donor staff and humanitarian actors working in FCAS. The approach was both exploratory and explanatory. Each data source was used to generate new evidence and both sources were triangulated to validate findings.
Literature review
Search strategy
Our review included published peer-reviewed and grey literature both publicly available and shared by the key informants during or after the interviews took place. The search included publications from 1 March 2020 to 31 January 2021 to account for the known start of the pandemic in FCAS. The search strategy (Additional file 1) was based on a published search protocol for a study on a similar topic in low- and middle-income countries (LMICs) [15]. The search terms used referred to categories of population (maternal, newborn, child and adolescent), health services (health care, health systems and provision/use) and settings (FCAS and relevant LMICs).
We searched for publications in Embase, Medline and Global Health databases using the Ovid® search interface. This search was complemented by screening the Repository composed by John Hopkins Centre for Humanitarian Health for relevant results until 2 February 2021. We also screened reference lists of relevant articles including a global scoping review on maternal and perinatal health [13] to identify additional publications.
Grey literature was searched in publicly available records from Interagency Working Group for Reproductive Health in Crises, Save the Children, Médecins Sans Frontières (MSF), the International Rescue Committee (IRC), CARE International, International Committee of the Red Cross, READY Initiative, United Nations Children's Fund (UNICEF), United Nations Population Fund (UNFPA), United Nations High Commissioner for Refugees, Healthy Newborn Network, Women’s Refugee Commission, Marie Stopes international and the Global Financing Facility. We searched for publications related to current UK Government work on the UK Parliament website. We included articles published in academic journals (such as editorials, commentaries, and perspective pieces), reports, relevant news articles, pre-prints of studies and information shared by the interviewees. In addition, we included the available data on the UNICEF’s ‘Tracking the situation of children during COVID-19’ dashboard (‘UNICEF dashboard’ hereafter) [16], using the existing filter for countries with ‘other ongoing humanitarian response’.
Study selection and data extraction
Full inclusion and exclusion criteria for the literature review is presented in Table 1.
The population of interest for the literature review included women, adolescents, newborns and children in fragile and conflict affected states as defined by the World Bank [17] (Additional file 2). Publications from LMICs that were deemed relevant to FCAS were also included. This search focused on interventions including antenatal care (ANC), postnatal care (PNC), deliveries, essential newborn health interventions, child health interventions, vaccinations, and nutrition activities. For the outcome of interest, we excluded the direct effect of the COVID-19 on the interest population as our focus was not on the health outcome of people with COVID-19, but on the health outcomes from the overall disruption of these specialised health care services.
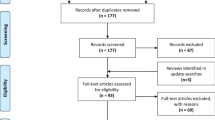
We downloaded all returned citations from databases and grey literature searches into an Endnote library and applied a standard data-screening process (Fig. 1). MR and NSS independently conducted double screening. Titles and abstracts were screened for relevance, and full-text articles screened against inclusion criteria. Grey literature publications were screened first by title and then full-text to consider inclusion. Data from the final selected studies were then extracted into a Microsoft Excel database, with data extraction fields including author and year, country, population, publication type, general topic addressed, types of services provided, and summary of publication where details on reported adaptations, funding and MNCHN outcomes were extracted. We used a narrative synthesis approach due to the heterogeneity of publication outcomes, interventions, and methods.
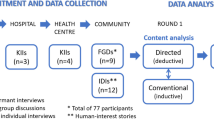
Qualitative interviews
For the qualitative approach we aimed to include a broad range of humanitarian actors to attempt to collect diverse information from a range of FCAS. The inclusion criteria for key informants were humanitarian actors working in FCAS [defined as programme staff, policymakers, practitioners from local and international non-governmental organisations (NGOs) and United Nations (UN) agencies] engaged in MNCHN programming in FCAS during COVID-19 and donor staff funding MNCHN programming in FCAS. Participants were purposively recruited from a list of contacts gathered by the authors that combined information obtained from the authors’ own network, the COVID-19 Humanitarian Platform [18], and contacts provided by the Unicef team who supported this study. This was followed by snowball sampling to identify additional relevant respondents. We sent out invitation emails for recruited potential informants and interviews scheduled with the ones that accepted. All participants gave oral consent to be interviewed and to be recorded.
We conducted 39 remote semi-structured interviews from October 2020 to February 2021. The interviews were carried out via an agreed online platform. We used an adapted version of the interview guide used by the COVID-19 Humanitarian Platform [18] to collect data on programmatic adaptations and innovations in humanitarian settings during the pandemic (Additional file 3). Our guide was adapted for donor staff to include a focus on levels and trends in funding for MNCHN programmes in FCAS before and during COVID-19. All interviews were conducted in English and lasted approximately 1 h. Interviews were transcribed using the software Otter.ai®.
Thematic analysis was undertaken on interview transcripts and supporting documents such as internal non-published reports provided by key informants using Braun and Clarke’s six phases of thematic analysis [19]. Analysis was undertaken independently by two researchers (LS and NSS) using NVivo 12 software. Following familiarisation with the data through reading of transcripts and documents, initial codes were derived which were then collated into themes.
The interview and literature data were triangulated in an iterative process using an exploratory and explanatory approach, with cross-checking of themes across the interview and literature data prior to defining and expanding on themes.
Results
Characteristics of included publications and key informants
A total of 1158 citations were returned from peer-reviewed databases, with 140 additional studies identified in reference lists (Fig. 1). Following full-text screening, 103 publications met the inclusion criteria (Table 2), comprising of 20 peer-reviewed publications (Additional file 4) [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39], 82 grey literature publications (Additional file 4) [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121], and one dataset [16]. The peer-reviewed papers included 8 cross-sectional studies [20, 22, 24, 25, 28, 33, 34, 36], 3 qualitative [29, 37, 39], 4 modelling studies [23, 26, 27, 35] and five reviews [21, 30,31,32, 38]; and the grey literature included 32 non-peer reviewed articles published in an academic journal (e.g., editorials, comment, letters to editor) [40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70, 80], three pre-print studies [71, 95, 120], one blog [111], one non-peer reviewed review [72], 31 reports/briefs from humanitarian actors [75, 77,78,79, 81,82,83,84, 86, 91, 94, 96,97,98,99, 101, 102, 104,105,106, 108, 112, 114,115,116,117,118,119, 121, 122], 10 news articles [73, 74, 87, 88, 100, 107, 109, 110, 113, 123] and four presentations shared by key informants [85, 92, 93, 103]. Overall themes in the publications, 38 mentioned maternal health, 11 on newborn health, 46 in child health and 34 in nutrition. The included dataset was retrieved from the UNICEF dashboard [16] which reported data from 26 countries, of which 23 are part of the World Bank fragile and conflict affected states list [17].
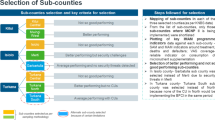
Key informants in the study (n = 39) represented donor staff (n = 3), academics (n = 2) and humanitarian agencies (n = 34). Key informants reported findings from the following 12 fragile and conflict affected states: Afghanistan, Colombia, DRC, Iraq, Nigeria, Somalia, South Sudan, Syria, Venezuela, Yemen, Zimbabwe, and Bangladesh (Cox’s Bazaar) (Fig. 2).
The research findings are presented by the pandemic’s impact on funding for MNCHN, disruptions to these health and nutrition services, impact on MNCHN outcomes, and reported adaptation strategies for these services during the pandemic.
Impacts of funding for MNCH and nutrition
We identified significant impacts on funding for MNCHN in FCAS. There was a clear political priority placed on COVID-19 activities in many countries from the start of the pandemic. Decisions about funding diversions away from MNCHN and towards COVID-19 specific case management activities were driven by governments, donors and stakeholders [53, 70]. Respondents highlighted that in many cases governments explicitly requested MNCHN activities to be deprioritised or prevented them from occurring in favour of COVID-19 activities.
Increase in cost of continuing the same activities
Three interview respondents reporting on Somalia, Iraq and Sudan and two publications [25, 66] highlighted that COVID-19 has led to significantly increased costs of maintaining existing activities for MNCHN. Data from Nigeria that considered the changes in expenditure pre- and during the pandemic found that the cost of giving birth doubled or tripled depending on the route of delivery, with personal protective equipment (PPE) accounting for a large proportion of the cost increase and COVID-19 Polymerase Chain Reaction (PCR) testing that, in many cases, was passed on to women and families [25, 66]. These findings were echoed by interview respondents who also cited increased requirements for consumables such as PPE and service modifications for infection prevention control (IPC). More money was also required for human resources to maintain existing services. This is because a significant number of existing staff with underlying medical risk factors had to be moved away from frontline roles and contexts with difficult medical evacuation, and with staff having to self-isolate or quarantine.
“What we saw in the project, like we make a plan on usually twice a year in terms of like what the project should do and what the focus will be, and which areas need more funding or more budget, so to say, and then it gets approved by headquarters or it will have to be adjusted. So in general the plan of course made before COVID came and then basically when Corona came [NGO] had a big problem all of a sudden because it started being something which was affecting all the projects all across the world, and giving a lot of actually higher needs in terms of budgeting because of all the PPE and like all the problems concerning flights.”—International NGO, South Sudan
Diversion of funding from MNCHN activities to COVID-19 related activities
The diversion of focus towards the pandemic has led to redirection of funds away from MNCHN services according to two publications and 14 interview respondents [62, 117] and 14 interview respondents reporting on Nigeria, Venezuela, Somalia, Afghanistan, Yemen, Bangladesh, Zimbabwe, Iraq, South Sudan, DRC and global FCAS. Reallocations occurred early in the pandemic, with respondents describing a lack of available funds for the initial COVID-19 response from emergency preparedness, which resulted in use of available funds from MNCHN. The primary use for the diverted funds reported was for IPC activities such as procurement of PPE, strengthening of water, sanitation and hygiene (WASH) services and to build additional inpatient capacity for isolation facilities. It was noted that even once additional funding did become available, it was frequently for COVID-19 specific measures only, and less so for maintaining essential services, including MNCHN services. In many cases additional human resources and supplies were also only available for COVID-19 related activities.
“It took a while for the COVID funds to really come. So we had to use the existing funds to support the program during the adaptation and the later phases as well.”—Multilateral organisation, Bangladesh
Planned funding and MNCHN activities which did not materialise
Six interviewees reporting on Yemen, Syria, South Sudan, Bangladesh, DRC, and global FCAS highlighted how the focus on COVID-19 meant that some other MNCH activities that were planned for 2020/2021 did not take place. These included trainings, quality improvement initiatives and entire MNCH programs in some cases. Examples cited included trainings, vaccination activities, HIV and TB, prevention of mother to child transmission (PMTCT), ANC and family planning (FP).
“In many cases funds which had been expected before the pandemic for certain activities did not materialise and planned programs didn’t open. In Yemen we scaled back antenatal and delivery care in an area in the knowledge that another actor had received funding and would start delivering these services; however in the end this actor was not able to open the expected services, citing funding issues… Women were then not receiving these services and we were unable to meet the demand, frequently turning women away in labour. Home deliveries likely increased, and we saw increasing number[s] of neonatal tetanus, probably as a result”—NGO, Yemen
Disruptions to MNCH and nutrition services
Both the demand (service uptake) and supply (service provision) sides of essential MNCHN services in FCAS have been overwhelmingly affected by the pandemic. Factors affecting the demand side identified in literature and interviews included stigma, the fear of infection, interruption of service provision, real or perceived linkage of COVID-19 measures to punitive restrictions on movement and liberty (in particular for migrants and refugees), distance from health facility, difficulties with transportation, increased financial burden and fear of being quarantined following a positive test result [16, 24, 29, 94, 111, 115, 116, 118]. Factors affecting supply side according to literature and interviews included reduced staffing due to MNCHN staff being diverted to COVID-19, staff infected with or scared of contracting the virus at work leading to absences; stock outs and supply issues including PPE and routine medications; and overall deprioritisation of MNCHN [20, 56, 94, 116].
Within MNCHN services, interviews and literature also highlighted a reduction in the quality of care. For example, one online survey across 60 LMICs which includes some FCAS reports that due to understaffing, the rapid change of guidelines or unclear communication and challenges with the supply chain, the quality of maternal and newborn health services is perceived to be deteriorating [56]. Inadequate staffing levels and diversions of resources to COVID-19 were reported by interviewees as further factors contributing to reduced quality of care.
Sexual, reproductive, maternal and newborn health
Eight publications [39, 55, 62, 92, 94, 103, 115, 120], data from UNICEF’s dashboard, [16] and 21 interviews focused on Syria, Venezuela, Somalia, Afghanistan, Bangladesh, Zimbabwe, Iraq, Yemen, DRC, South Sudan, and global FCAS highlighted reduced and even complete suspension of the provision of sexual, reproductive, maternal and newborn services due to COVID-19. A key informant in an NGO reported that outpatient services were significantly reduced in many countries, often to half the normal activity. Interviewees highlighted that ANC services were reduced in many settings to reduce crowding and COVID-19 transmission and, in many cases, women were permitted only one ANC visit. PNC provision was reduced in Zimbabwe, Afghanistan, Venezuela, Bangladesh and South Sudan, with key informants in Bangladesh and Somalia reporting a complete suspension of newborn care [92]. Suspensions of outreach activities were common [39]. Interviewees described reduction in services that would normally have relied on outreach/mobile strategies as entry-points, including for reproductive health and sexual and gender-based violence (SGBV) interventions.
“… In the camp, you have a really big component that's outreach activities. And this was seriously impacted by COVID-19. Outreach activities [were] almost zero for SRH, it almost disappeared completely… I didn't realize at first that it was the most important activity for SRH and SGBV.”—International NGO, Bangladesh
Reduction in service uptake, including in ANC and facility delivery, was also reported across 13 publications [29, 56, 71, 86, 92,93,94, 106, 111, 113, 115, 118, 120], the data set [16] and 23 interviews focused on South Sudan, Nigeria, Bangladesh, Venezuela, Columbia, Afghanistan, Somalia, Zimbabwe, Iraq, Syria, Yemen, DRC and global FCAS. In Cox’s Bazar, ANC consultations for adolescents fell by 65% between January and May 2020 [106]. In Afghanistan, facility-based deliveries decreased by half [94]. Increased home deliveries with traditional birth attendants (TBAs) were reported in six publications, in several countries including Nigeria and Bangladesh [20, 29, 55, 92, 111, 116].
“All other services including antenatal care were disrupted…in theory, the services were not stopped. But people stopped coming to the consultations. People stopped themselves obtaining services. And it was mainly because of the fear…They had the fear that maybe they go to COVID-19 from the hospital, from the healthcare providers…”—Multilateral organisation, Afghanistan
“The bigger concern was we had a huge reduction in the number of patients. So we went from… 2000 deliveries on average to, in July [2020], we had… 900 deliveries… I still don't know where all these people started to go.”—International NGO, Afghanistan
According to key informants, unclear communication and lack of adaptation of COVID-19 messaging for pregnant women also led to confusion about going to health facilities to deliver or not as COVID-19 messaging was advising people to avoid attending them.
“We did see a drop in service utilization. And I think that was probably for a number of reasons. One was….the lack of clarity in in terms of messaging, so should people stay at home or should people still come to the clinic.”—International NGO, South Sudan
Child health
Downscaling and closure of consultations, reduced preventive and curative care, vaccination related to child health was seen in 13 publications [21, 22, 31, 32, 40, 44, 64, 69, 72, 73, 76, 80, 103], the Unicef dashboard [16] and 11 interviews focused on Venezuela, Syria, Afghanistan, Yemen, Bangladesh, Somalia, and multiple/global FCAS. Interviews and literature findings noted a decline in utilisation of outpatient and inpatient child health services [16, 24, 36, 73, 94]. Save the Children examined the impact of COVID-19 on child health in 37 countries and found that more than one third of respondents faced barriers to accessing healthcare including the closure of health facilities, long queues, and shortage of medications [105].
Routine immunisation was disrupted across many settings due to early recommendations from scientific advisory groups for emergencies to suspend all preventative mass vaccination campaigns, which placed children, especially those suffering from malnutrition, at increased risk [16, 32, 69, 73, 80, 103]. Additional reasons cited in the literature for vaccine disruption include delivery systems affected by the pandemic, healthcare services being stretched, social distancing measures, and caregivers becoming fearful of visiting health centres [28, 59, 94, 119]. Several interview respondents attributed the reduction or suspension in vaccination coverage to factors including supply chain issues, suspension of outreach activities to prevent COVID-19 spread and consequences of stopping other services (e.g., ANC) which normally would be used as an opportunity for comprehensive care provision, including vaccination.
The impact of suspensions in vaccination was highlighted in the literature [33, 51]. Despite the declaration of wild polio eradication in Africa in 2020, vaccine-derived polio transmission has increased and is now reported in a number of countries including Niger [32]. In Afghanistan, polio vaccination was stopped and there was a rise in polio cases, particularly in polio free areas [64, 72, 76]. Interview respondents also highlighted concerns of surges of new epidemics of childhood vaccine preventable diseases.
“We are already seeing increases in vaccine-preventable diseases, for example Diphtheria, tetanus pertussis, and measles outbreaks. Polio campaigns were also suspended and Vaccine derived Polio cases are also occurring due to low vaccination coverage.”—NGO, setting anonymised on request
Concerns have been raised over the effects of neglecting malaria control programmes including net distribution, seasonal malaria chemoprevention, and treatment, especially for children, since this age group has the highest burden of malaria, accounting for 70% of global malaria deaths [27, 48, 96, 121].
Nutrition
Nutrition services were suspended in several FCAS, including nutrition centres, food distributions and treatment for child wasting according to four publications [45, 78, 81, 94], the data set [16] and eight interviews focused on global FCAS, Bangladesh, Venezuela, Afghanistan, Syria and Somalia. Reasons for reduced nutrition activities cited in interviews and the literature included a link to reduction or suspension of community outreach activities, measures to prevent gatherings and prevent transmission of COVID-19, and diversion of nutrition staff to COVID-19 [73, 94].
“We were told that you cannot go into the community because you can potentially take COVID in and out to the community… So we had to stop that…And because some of the programs, the nutritional programs such as dinners for kids were shut down… that is a problem because a lot of kids didn't have anything to eat except for what was given in those diners.”—NGO, Venezuela
“When the COVID-19 started… I would say nutrition really suffered, because… they are reassigning… all the nutrition staff to work on COVID-19 related activities. So, we noted that… all the upstream work that we do to do with policy guidelines… things were not moving, everything had to come to a standstill for like five months.”—Multilateral organisation, Somalia
Reports from several countries refer to the difficulties that populations have been facing in accessing and ensuring food supplies. Reduced income, limited resources for quality diets, food insecurity, higher prices in food, limitation of health care services and interruption of humanitarian responses are leading to undernutrition [38, 45, 50, 83, 91, 105, 107, 109, 110, 114]. Interview respondents noted a reduction in uptake of nutrition services during the pandemic despite needs increasing in some contexts, especially for child nutrition interventions.
“There was definitely a reduction in the number of children that were enrolled in supplementary feeding and therapeutic feeding programs. And this was… for a number of reasons. One of them being that you know, people were reluctant to come to the clinics.”—Multilateral organisation, Global
Data collection activities
There was disruption or suspension in routine data collection, monitoring and evaluation and measurement activities in MNCHN according to 18 interview respondents reporting on Bangladesh, South Sudan, Somalia, Venezuela, Columbia, Afghanistan, Yemen, Syria and global FCAS. This was due to deprioritisation of MNCHN measurement activities, inadequate staffing, and difficulty in carrying out activities based in the community due to lack of PPE, movement restrictions and other COVID-19 prevention measures which leads to reduced quantity and quality of data. Multiple community measurement activities were suspended, including mortality surveys, [e.g., Standardised Monitoring and Assessment of Relief and Transitions (SMART) surveys] and nutrition surveys, as well as community surveillance, have also been impacted. As a result, there has been a significant reduction in the visibility of community level deaths of women and children during the pandemic.
“I think everyone, even governments, are facing data collection gaps. Data collection and data quality was in a bad state before COVID-19 in many countries. And now with COVID-19, it's just worsening…we don't know how many people are affected. […] You know, in some countries, community health workers are very strong data collectors. But with COVID-19, they might not even go to the villages where they would normally go.”—Multilateral organisation, global
MNCH and nutrition outcomes
Findings from interviews and published literature point to increased morbidity and mortality associated with MNCHN across several settings related to the disruptions to funding and services, threatening years of advocacy and improvements [6, 43, 56].
Sexual, reproductive, maternal and newborn health outcomes
Increasingly late presentations which resulted in poorer health and mortality outcomes were reported in two publications [54, 111] and 11 interviews reporting on Venezuela, Bangladesh, Syria, Yemen, South Sudan and global FCAS. Women are reported as arriving late at heath facilities and more frequently presenting with serious complications (such as eclampsia) as ANC services are neglected. [54, 111] Interview respondents also reported women presenting with more severe maternal morbidity and complications linked to reduced pregnancy care and other COVID-19 related impacts, such as iron deficiency anaemia, secondary to increased levels of malnutrition.
“I think one thing that we did see was an increase in late presentations and there was a subtle increase in maternal mortality cases in our clinic over the summer. That speaks to a presentation of patients not coming in for routine, preventative care in their pregnancy, and then having problems later on…”—International NGO, Bangladesh
Estimations looking at the indirect mortality from COVID-19 disruptions in LMICs, indicate that over six months of disruptions would result in an increase of 8.3%-38.6% in maternal deaths per month across 118 countries [26]. Another publication estimated that, over a year in LMICs, a 10% decline in coverage of maternal and newborn health services would mean an additional 1.7 million women who give birth and almost 2.6 million newborns that would experience major complications without receiving the needed obstetric and newborn care. This would result in additional 28,000 maternal deaths and 168,000 newborn deaths [63]. Data from the four most populous LMICs (including Nigeria) could see a 31% increase in maternal and newborn deaths and still births as a result of reduced FP, ANC and facility based deliveries in the next 12 months [100, 111]. Authors caution that these numbers are an underestimation, especially in rural, low resource and FCAS where the most vulnerable pregnant women are [61]. Specific estimates for selected FCAS indicate that the impact of a large service disruption in 2020–2021 would lead to a 1–11% increase in maternal mortality; and that between 10,700 and 725,900 women would be left without access to facility-based deliveries across several FCAS, such as in Yemen, South Sudan and Central African Republic (CAR) [97,98,99, 101, 102, 104, 112].
Nine interview respondents reporting on Bangladesh, Yemen, Syria and global FCAS also highlighted an increase in maternal mortality across a range of humanitarian settings, citing inability to access care, reduced care-seeking behaviour, reduced ANC and potential COVID-19 infection itself as attributing factors.
“…during my first three months of being in Yemen, I had no maternal deaths… then when COVID hit, we had so many more maternal deaths. Sometimes, it's hard for us to say exactly whether it was because of COVID-19 because we didn't actually test everybody. […] It could have been due to COVID. It could have been that people were a lot more afraid of coming to the hospitals, because obviously that was like, I think, a common narrative around the world.”—International NGO, Yemen
Child health
The impact on child health was highlighted by 19 publications [26, 33, 35, 37, 46, 73, 74, 79, 89, 92, 94, 97,98,99, 101, 102, 104, 112, 116] and eight interviews focused on Bangladesh, Venezuela, Yemen, Syria and global FCAS. A report from Save the Children warned that 60 million children will need humanitarian assistance in 2021 to survive, which accounts for half of all children in need globally [74]. A modelling study that considers the excess mortality due to disruptions in essential maternal and child services and access to food reported estimated 253,500 to 1,157,000 additional child deaths in a year in the least and most severe scenarios respectively [26]. This translates to a 9.8–44.7% increase in deaths in under-fives per month across 118 countries LMICs and to a 12–18% increase in selected FCAS [26, 97,98,99, 101, 102, 104, 112].
Interview respondents highlighted increased child morbidity and mortality with children frequently arriving at health facilities late and with severe disease. Key attributing factors included reduction in child health provision facilities, reduced outreach activities, reduced health seeking behaviour and worsening malnutrition.
“…In Yemen, there were a lot of children arriving in a very bad state. In White Nile the team asked because the number in the hospital was very low. And that was because the activities—the screening activities at community level stopped with the pandemic.”—International NGO, Yemen and Sudan
There is a strong argument to continue routine vaccinations, ensuring appropriate use of PPE, hygiene and physical distancing measures are put in place [46]. A modelling study estimated that routine childhood immunisations in selected African countries should be continued as the deaths prevented by this activity outweigh the risk of COVID-19 deaths related with the visits to vaccination clinics [35]. Catch-up programmes in some FCAS were restarted to address the impact of early programme disruptions [79, 92].
Nutrition
Increased risk of malnutrition and worsening nutrition outcomes were reported in 17publications [26, 60, 73, 77, 79, 81, 83, 84, 87, 88, 90, 92, 94, 109, 110, 116, 118] and nine interviews focused on global FCAS, Syria, Venezuela, DRC, Yemen, and Bangladesh. Several settings reported rises in severe acute malnutrition admissions, ranging from increases of 10% up to 70% [73, 77, 87, 94, 109, 118]. Several interviews reported increased malnutrition, with women and children being most at risk, particularly in settings that were already experiencing high levels of food insecurity and malnutrition before COVID-19. Women’s nutrition was also affected with at least a quarter of a million pregnant and lactating women, in Southern Yemen, in need of malnutrition treatment [87, 90]. In a modelling study looking at the indirect mortality from COVID-19 in LMICs including FCAS, the authors estimate that 18–23% of additional deaths in children under-five will be caused by the increased prevalence of wasting [26].
Adaptation strategies for MNCH and nutrition services
The literature search and key informant interviews reported a range of adaptation strategies for MNCHN implemented, most of them with the primary objective of reducing transmission of COVID-19.
Factors enabling successful adaptations of MNCHN services included preparedness, coordination and collaboration between actors, good communication, provision of adequate amount of supplies and support from the local population [75, 81].
Barriers to adaptations include lack of flexible funding, challenges with global supply chains, and capacity to rapidly implement new ways of working [78]. There were concerns from some key informants about whether the priority placed on reducing transmission of COVID-19 compared to other essential services was proportionate to the threat given the seriousness of other factors affecting MNCHN in FCAS. Acceptability of adaptations by the local population was a further challenge faced by several actors. For example, lack of acceptance of one adaptation preventing hospital visitors led to reduced service uptake.
“…The first thing we did was to stop with all the caretakers to enter the hospital, you need to think that in that area, I mean the patient, they are always coming with the mother-in-law… And this was a big, huge thing. And challenge, because also, we need to have a lot of meetings with the elderly, with the community to also make them understand, we need to reduce the flow of the people coming inside and going outside.”—International NGO, Afghanistan
“People started losing trust in our facilities because they came and they didn’t get treated, because there wasn’t anything, which is very unusual… I think that had a very, very huge impact on the perception of the community of what we do.”—International NGO, DRC
Adaptations to funding
There were some accounts of positive adaptations in relation to funding MNCHN services in FCAS. One study highlighted that the pandemic has diversified the funding sources which could be a solution to strengthen reproductive, maternal and child health programmes [117]. 11 interview respondents reporting on South Sudan, Bangladesh, Syria, Afghanistan, Venezuela, Somalia, Yemen and global FCAS reported additional funding being made available from both international internal organisation funding and from donors. Strengthening WASH including IPC was a major reported use for the funding to increase availability and quality of WASH in health facilities and improve communication and education on WASH which had a positive effect beyond the avoidance of COVID-19 infections. Various actors and funders highlighted that funding was not earmarked for the pandemic and could be used for other activities such as MNCHN services.
“On the one hand… IPC improved, hygiene improved, hand washing improved, I mean, it was much more focus put on that, where you could actually even see a reduction in certain diseases…diarrhoeal diseases, and whatever.”—International NGO, DRC
Infection prevention and control measures
Reorganisation of patient flow, social distancing measures (e.g., reduction of hospital visitors, reduction in access to smaller groups of patients at a time, reduced frequency of facility visits), reduced opening hours and reduction or suspension of out-patients department (OPD) consultations were highlighted in six publications and 16 interviews [20, 34, 55, 86, 113, 117] and 16 interviews focused on Syria, South Sudan, Somalia, Afghanistan, Nigeria, Venezuela, Yemen, Bangladesh, Iraq and global FCAS.
“These are services that are usually very crowded. So they tried to adjust the services too. They had longer hours. They gave women specific times to come to reduce some crowding, where they did have to decrease services, they prioritised women that were in the third trimester of pregnancy.”—Multilateral organisation, global
Interview respondents noted that increased WASH activities were implemented in many contexts, with handwashing and environmental IPC prioritised. Emphasis was placed on training staff in IPC and use of PPE in several settings [68].
Use of technology
Telemedicine was used as an adaptation strategy in a number of FCAS according to four publications [34, 56, 86, 113] and eight interviews focused on Venezuela, Columbia, Afghanistan, Yemen, Bangladesh and global FCAS. Several interview respondents highlighted that MNCHN service provision was shifted to online modalities, for example mobile phone/WhatsApp calls and messaging. In addition to its use for providing services and information to users, interview respondents noted the use of online technology for staff training (including on COVID-19 measures and for maintaining essential health services) and to adapt data collection in several settings to try and continue the delivery of routine monitoring and evaluation on MNCHN data.
“They can do the consultation remotely, using the tablet, community health workers, you know, bring it to the pregnant woman and then they consult with the midwives. And then for the other thing also that we also try to improve in is using the mobile phone platform […]—the community can text a message to the health provider or to the community health workers about their problems.”—Governmental agency, Bangladesh
Nevertheless, the impact of limited use of telemedicine services has not been equitable across settings and socioeconomic groups. Some respondents noted that access and proficiency in technology was a challenge for adaptation strategies involving online tools for staff and target populations; and literature highlighted that it might not be a realistic solution for some settings [30].
Decentralisation of services
Due to the decrease in demand for facility-based health care, it was crucial to provide MNCHN services at the community level according to two publications and 13 interviews [56, 117] and 13 interviews focused on Bangladesh, Venezuela, Yemen, Somalia, South Sudan, Afghanistan, Zimbabwe, Syria, Venezuela and global FCAS. Several interview respondents intended to shift MNCHN services to mobile or outreach services to better reach populations in the community. Examples of how they managed to operationalise this shift included using important community gathering places such as the local mosque to provide health promotion and related services.
“We decided to use a mobile clinic to do outpatient treatment… We just needed to be closer to the population to do this screening and treatment at the community level. We left the hospital and moved to the community to try to treat the malnourished children earlier.”—International NGO, Yemen
Interview respondents described new communication and advocacy activities on maintaining essential services to reassure and continue promotion of usage of MNCHN services, such as institutional deliveries.
“Community messaging has been a key part of what we’ve done. To reassure people that the services are still open and safe to attend. And also information about COVID, how to stay safe, hand washing, guidance, all those kinds of things that we’ve seen in many other contexts globally.”—International NGO, Yemen
Another form of decentralisation of services was using self-care interventions. Several respondents mentioned the shift in global nutrition guidance to using mother/caregiver led mid upper arm circumference (MUAC) measurements to screen for malnutrition at home, with guidance on when to seek health care given to caregivers. This adaptation was also highlighted in the literature [16, 75, 81].
Interview respondents also described how treatment protocols in some settings were altered to continue essential healthcare whilst reducing contact frequency at facilities. Measures included giving longer durations of medication and food rations and encouraging use of long-acting reversible contraceptives (e.g., intrauterine devices, implants).
However, some interview respondents noted that despite the intention to increase community-based services, the extent to which this has actual been possible has been limited in many settings. This was attributed to funding constraints, the repurposing of community health workers to COVID-19 related activities, and limitations to community gatherings. In some countries, outreach activities were suspended during the pandemic.
Discussion
Our findings demonstrate that in many cases funding for MNCH and nutrition in FCAS has been diverted, reduced, or suspended during the COVID-19 pandemic. Supply and use of MNCHN services has also been disrupted due to a combination of factors, with reported increased morbidity and mortality across MNCHN. Humanitarian actors have adapted and implemented strategies to improve access to MNCHN interventions as part of the pandemic response, but in most FCAS included in the study, they have been limited, insufficient to account for overall disruption to services, and subject to inequities in their provision. Across the study, the findings from our literature search and interviews were generally complementary.
This study highlights the impacts of the COVID-19 pandemic on funding of MNCHN, and particularly the deprioritisation of funding by governments in favour of resource allocation to COVID-19 specific measures. Diversion of funding away from MNCH has previously been documented across prior infectious disease outbreaks and epidemics including Ebola and Zika [10]. There is a clear call for governments to firstly ensure that funding for MNCHN is re-established to pre-pandemic levels. Given the reported impacts on reduced service provision and uptake and resulting poor MNCHN outcomes, additional funding should be leveraged to address the collateral impacts on MNCHN. A greater focus should be placed funding for health system strengthening activities. Emergency preparedness plans must include capacity and funding to maintain MNCHN activities.
Supply- and demand-side challenges to MNCHN services have also been seen across previous large-scale infectious disease outbreaks, particularly in contexts with fragile health systems [124]. Our study findings suggest the integration of the COVID-19 response into essential health care as a possible way to develop long term strengthening of fragile health systems [41].
Although limited and incomplete, available evidence shows that preventable deaths are occurring due to COVID-19 disruptions in MNCHN services. Evidence from previous pandemics shows that indirect impacts can be greater than the disease itself [124]. Whilst empirical research reporting on wider health implications of COVID-19 in humanitarian settings remains scarce, a series of case studies on the collateral impact of COVID-19 on non-communicable diseases across six humanitarian settings highlights reduced access to and provision of health services as well as financial and human resource diversion towards COVID-19—similar to the findings of our study [5].
Literature drawing on lessons from previous outbreaks highlights the importance of maintaining essential general health services in humanitarian settings, ensuring access to IPC/WASH for displaced populations and promoting community trust and engagement as part of effective public health measures [7]. In addition to ensuring prioritisation of MNCHN and maintenance of essential services in times of additional crisis, a holistic public health approach should be taken to reduce supply and demand barriers. Surge and emergency preparedness planning is crucial to prevent stock outs and supply issues, and protection of healthcare and other front-facing staff is a priority to continue services. Community engagement, rumour management and clear communication are all important to understand and alleviate concerns. Opportunities to combine community preventive activities together should be explored to increase efficiency and expedite catch-up activities such as nutritional interventions, mass vaccination campaigns, Vitamin A, bed nets, seasonal malaria chemoprophylaxis (SMC), and other activities.
Whilst limited in some settings, our finding of a range of adaptation strategies for MNCHN is echoed across other studies [10, 20]. The importance for documenting and sharing these solutions has been highlighted [125]. Additionally, capacity building and continued training of staff is critical to implementing adaptations. Integration of monitoring and evaluation into adaptations with regular reviews is also vital to measure impacts. Some studies included from the literature review also note that investing in primary health care and in the integration of COVID-19 response into essential health care could be the way to strengthen already fragile health systems [41, 43]. Donors should make available additional funding to enable adaptations to be fully implemented.
To our knowledge, this is the first study to investigate the collateral impact of COVID-19 on MNCHN across multiple FCAS. Our study is reasonably extensive in that it includes data from the literature and interviews from the majority of FCAS (51.28%). Interviews covered a range of actors including funders, staff at the global level in multilateral organisations, humanitarian field staff and clinical staff. We aimed to ensure that this study was comprehensive, utilising snowballing to identify further interview participants and utilised data provided by the key informants. The triangulation of the data allowed for a broader analysis of the current situation, strengthening our findings.
However, this study also has several limitations. Through the range of settings in which data collection was undertaken, this study emphasises breadth in its findings and recommendations. Context matters, and therefore the findings and recommendations will not be generalisable to every FCAS. Future research should be designed to analyse regional or other contextual trends. Although we included English, Portuguese, Spanish, and French articles in the review, we may have missed relevant articles published in other languages. All included peer-reviewed articles were observational studies, and thus causation cannot be attributed. Whilst the use of online modalities for interviews undoubtedly increased the ability for data collection, a documented challenge of research within FCAS is poor internet access [126]. It is therefore possible that information from additional key informants was missed if they were unable to participate due to internet access issues. Crucially, this study does not include the voices of individuals from affected communities. Some humanitarian data sources were also not able to be included due to the design, for example food security data. It was not feasible to collect data from populations directly affected within the bounds of this study, but as a result these findings and recommendations should be taken with some caution as they may not be representative of the views of patients and service users in affected populations. Lastly, it is important to consider the positionality of the researchers and the associated political, social, economic and historical contexts and power hierarchies that occur when doing research in FCAS [127]. This study was led by a team of high-income country researchers, none of whom are from affected communities within FCAS. This will have impacted the study design, data collection and interpretation; and findings should again be considered in light of this.
We do not yet know the full extent of the impact of COVID-19 related disruptions on MNCHN outcomes. Since existing data collection, including mortality surveillance and surveys, and data analysis have been disrupted, limited evidence exists evaluating the impacts of demand and supply disruptions across the settings. Further work should seek to further gather rigorous data and evaluate the impacts of COVID-19 on MNCHN in FCAS so that future programmes can be best adapted to prioritise, meeting the needs of women and children.
Conclusions
Our study findings show that the COVID-19 pandemic is exacerbating negative MNCHN outcomes in FCAS that were already significantly worse compared to other settings before COVID-19 due to lack of resources and the deprioritisation of essential services for women and children. These findings also demonstrate that lessons learned from previous epidemics on reducing their indirect impacts on MNCHN have not been systematically integrated into humanitarian responses in FCAS during COVID-19. While humanitarian actors have made several adaptations to continue providing MNCHN services during the pandemic, these strategies have often been implemented unevenly within and across settings, and not been evaluated.
Political will and mobilising of sufficient resources, with sustained commitment from donors, governments, NGOs and multilateral organisations working in FCAS are urgently needed to prevent further negative impacts on mothers and children. Steps must be taken to strengthen health systems and existing MNCHN services, ensuring that the most vulnerable populations are reached. Timely data collection is also needed to be able to use data to inform MNCHN programming in real-time, and research should be embedded within MNCHN programming in FCAS to assess the effectives of implementation strategies. Continued advocacy efforts are also vital to the prioritisation of MNCHN services, with particular attention needed to mitigate the predicted negative secondary effects of COVID-19 on MNCHN outcomes in FCAS over the coming years.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to the protection of individual privacy.
Abbreviations
- ANC:
-
Antenatal care
- CAR:
-
Central African Republic
- COVID-19:
-
Coronavirus disease 2019
- DRC:
-
Democratic Republic of Congo
- FCAS:
-
Fragile and conflict-affected settings
- FP:
-
Family planning
- IPC:
-
Infection prevention and control
- IRC:
-
The International Rescue Committee
- LMIC:
-
Low- and middle-income country
- MNCH:
-
Maternal, newborn, and child health
- MNCHN:
-
Maternal, newborn, child health and nutrition
- MSF:
-
Médecins Sans Frontières
- MUAC:
-
Mid upper arm circumference
- NGO:
-
Non-governmental Organisation
- PMTCT:
-
Prevention of mother to child transmission
- PNC:
-
Postnatal care
- PPE:
-
Personal protective equipment
- OPD:
-
Out-patients department
- SGBV:
-
Sexual and gender-based violence
- SMART:
-
Standardised monitoring and assessment of relief and transitions
- SMC:
-
Seasonal malaria chemoprophylaxis
- SRH:
-
Sexual and reproductive health
- TBA:
-
Traditional birth attendant
- UN:
-
United Nations
- UNFPA:
-
United Nations Population Fund
- UNICEF:
-
United Nations Children's Fund
- WASH:
-
Water, sanitation and hygiene
References
OCHA. Global Humanitarian Overview 2022 [Internet]. [cited 2021 Dec 3]. https://gho.unocha.org/.
United Nations Population Fund (UNFPA). Maternal mortality in humanitarian crises and in fragile settings. 2015.
Percival V, Richards E, MacLean T, Theobald S. Health systems and gender in post-conflict contexts: building back better? Confl Health. 2014;8(1):1–14.
Meagher K, Singh NS, Patel P. The role of gender inclusive leadership during the COVID-19 pandemic to support vulnerable populations in conflict settings. BMJ Glob Heal. 2020;5(9):e003760.
iMMAP. The effects of COVID-19 on non-communicable disease: a case study of six countries. J Lang Relatsh. 2021. https://reliefweb.int/report/bangladesh/effects-covid-19-non-communicable-diseases-case-study-six-countries.
ODI/ALNAP. From Ebola & Cholera to COVID-19—applying lessons from responses during cholera and Ebola outbreaks to COVID-19 response; 2020. https://www.alnap.org/help-library/from-ebola-cholera-to-covid-19-applying-lessons-from-responses-during-cholera-and-ebola.
Lau LS, Samari G, Moresky RT, Casey SE, Kachur SP, Roberts LF, et al. COVID-19 in humanitarian settings and lessons learned from past epidemics. Nat Med. 2020;26(5):647–8.
Sochas L, Channon AA, Nam S. Counting indirect crisis-related deaths in the context of a low-resilience health system: the case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Policy Plan. 2017;32:iii32–9.
Phillips DE, Bhutta ZA, Binagwaho A, Boerma T, Freeman MC, Hirschhorn LR, et al. Learning from exemplars in global health: a road map for mitigating indirect effects of COVID-19 on maternal and child health On behalf of the Exemplars in Global Health Partnership Commentary Learning from Exemplars in Global Health: a road map for mitig. BMJ Glob Health. 2020;5:3430.
Takemoto MLS, McKay G, Amorim M, Gbomosa CN, Tengbeh AF, Wenham C. How can countries create outbreak response policies that are sensitive to maternal health? BMJ. 2021;373:1–4.
Di Toro F, Gjoka M, Di Lorenzo G, De Santo D, De Seta F, Maso G, et al. Impact of COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin Microbiol Infect. 2021;27(1):36–46.
Wei SQ, Bilodeau-Bertrand M, Liu S, Auger N. The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis. CMAJ. 2021;193(16):E540–8.
Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review, vol. 18, Reproductive Health. BioMed Central Ltd; 2021. p. 10.
Picchioni F, Goulao LF, Roberfroid D. The impact of COVID-19 on diet quality, food security and nutrition in low and middle income countries: a systematic review of the evidence. Clin Nutr. 2021.
Benova L, Huysmans E, Portela A. Rapid scoping review of measures taken to maintain the provision and the use of essential services for MNCAAH (maternal, newborn, child, adolescent and older person’s health).protocols.io; 2020.
UNICEF. Tracking the situation of children during COVID-19. Dashboard. 2020.
The World Bank. FY21 List of Fragile and Conflict-affected Situations. FCS List. 2020.
COVID-19 Humanitarian Team. COVID-19 Humanitarian Platform. 2020.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Semaan A, Audet C, Huysmans E, Afolabi B, Assarag B, Banke-Thomas A, et al. Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Glob Heal. 2020;5(6):e002967.
Coker M, Folayan MO, Michelow IC, Oladokun RE, Torbunde N, Sam-Agudu NA. Things must not fall apart: the ripple effects of the COVID-19 pandemic on children in sub-Saharan Africa. Pediatr Res. 2020;89:1–9.
Ogundele IO, Alakaloko FM, Nwokoro CC, Ameh EA. Early impact of COVID-19 pandemic on paediatric surgical practice in Nigeria: a national survey of paediatric surgeons. BMJ Paediatr Open. 2020;4(1):732.
Minckas N, Medvedev MM, Adejuyigbe EA, Brotherton H, Chellani H, Estifanos AS, et al. Preterm care during the COVID-19 pandemic: a comparative risk analysis of neonatal deaths averted by kangaroo mother care versus mortality due to SARS-CoV-2 infection. EClinicalMedicine. 2021;33:100733.
Enyama D, Chelo D, Noukeu Njinkui D, Mayouego Kouam J, Fokam Djike Puepi Y, Mekone Nkwele I, et al. Impact of the COVID-19 pandemic on pediatricians’ clinical activity in Cameroon. Arch Pediatr. 2020;27:423–7.
Banke-Thomas A, Makwe CC, Balogun M, Afolabi BB, Alex-Nwangwu TA, Ameh CA. Utilization cost of maternity services for childbirth among pregnant women with coronavirus disease 2019 in Nigeria’s epicenter. Int J Gynaecol Obs. 2020;152:242–8.
Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, Tam Y, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Heal. 2020;8(7):e901–8.
Sherrard-Smith E, Hogan AB, Hamlet A, Watson OJ, Whittaker C, Winskill P, et al. The potential public health consequences of COVID-19 on malaria in Africa. Nat Med. 2020;26(9):1411–6.
Bizri AR, Khachfe HH, Fares MY, Musharrafieh U. COVID-19 pandemic: an insult over injury for Lebanon. J Community Health. 2020;46:487–93.
Lusambili AM, Martini M, Abdirahman F, Asante A, Ochieng S, Guni JN, et al. “We have a lot of home deliveries” A qualitative study on the impact of COVID-19 on access to and utilization of reproductive, maternal, newborn and child health care among refugee women in urban Eastleigh, Kenya. J Migr Heal. 2020;1:1–2.
Ijarotimi OA, Ubom AE, Olofinbiyi BA, Kuye-Kuku T, Orji EO, Ikimalo JI. COVID-19 and obstetric practice: a critical review of the Nigerian situation. Vol. 151, International Journal of Gynecology and Obstetrics. Wiley; 2020. p. 17–22.
Zar HJ, Dawa J, Fischer GB, Castro-Rodriguez JA. Challenges of COVID-19 in children in low- and middle-income countries. Paediatr Respir Rev. 2020;35:70–4.
Dinleyici EC, Borrow R, Safadi MAP, van Damme P, Munoz FM. Vaccines and routine immunization strategies during the COVID-19 pandemic. Hum Vaccin Immunother. 2020;17:400–7.
Masresha BG, Luce R Jr, Shibeshi ME, Ntsama B, N’Diaye A, Chakauya J, et al. The performance of routine immunization in selected African countries during the first six months of the COVID-19 pandemic. Pan Afr Med J. 2020;37(Suppl 1):12.
Moyo J, Madziyire G. Use of telemedicine in obstetrics and gynaecology in Zimbabwe during a lockdown period. Pan Afr Med J. 2020;35(Supplement 2):1–4.
Abbas K, Procter SR, van Zandvoort K, Clark A, Funk S, Mengistu T, et al. Routine childhood immunisation during the COVID-19 pandemic in Africa: a benefit–risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob Health. 2020;8(10):e1264–72.
Mahmassani D, Tamim H, Makki M, Hitti E. The impact of COVID-19 lockdown measures on ED visits in Lebanon. Am J Emerg Med. 2020;46:634–9.
Abdulah DM, Abdulla BMO, Liamputtong P. Psychological response of children to home confinement during COVID-19: a qualitative arts-based research. Int J Soc Psychiatry. 2020;67:761–9.
Akseer N, Kandru G, Keats EC, Bhutta ZA. COVID-19 pandemic and mitigation strategies: implications for maternal and child health and nutrition. Am J Clin Nutr. 2020;112(2):251–6.
Ahmed SAKS, Ajisola M, Azeem K, Bakibinga P, Chen Y-F, Choudhury NN, et al. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob Heal. 2020;5(8):e003042.
Govender K, Cowden RG, Nyamaruze P, Armstrong RM, Hatane L. Beyond the disease: contextualized implications of the COVID-19 pandemic for children and young people living in Eastern and Southern Africa. Front Public Heal. 2020;8:504.
Dmello BS, Housseine N. Impact of COVID-19 on maternal and child health. 2020.
Walker D, Chandir S. COVID-19’s lost generation of unvaccinated children. 2021.
Castro A. Maternal and child mortality worsens in Latin America and the Caribbean. Lancet. 2020;396:e85.
Mustafa F, Green RJ. The implications of COVID-19 for the children of Africa. S Afr Med J. 2020;110(6):1–1.
Fore HH, Dongyu Q, Beasley DM, Ghebreyesus TA. Child malnutrition and COVID-19: the time to act is now. The Lancet. 2020;396:517–8.
Mellis C. Sustaining routine childhood immunisations during COVID-19 in Africa. J Paediatr Child Health. 2020;57:457.
Fore HH. A wake-up call: COVID-19 and its impact on children’s health and wellbeing. Lancet Global Health. 2020;8:e861–2.
Nghochuzie NN, Olwal CO, Udoakang AJ, Amenga-Etego LN-K, Amambua-Ngwa A. Pausing the fight against malaria to combat the COVID-19 pandemic in Africa: is the future of malaria bleak? Front Microbiol. 2020;11:1476.
The Lancet Global Health. Food insecurity will be the sting in the tail of COVID-19. Lancet Global Health. 2020;8:e737.
Aborode AT, Ogunsola SO, Adeyemo AO. A crisis within a crisis: Covid-19 and hunger in African children. Am J Trop Med Hyg. 2021;104:30.
Adamu AA, Jalo RI, Habonimana D, Wiysonge CS. COVID-19 and routine childhood immunization in Africa: leveraging systems thinking and implementation science to improve immunization system performance. Int J Infect Dis. 2020;98:161–5.
Busch-Hallen J, Walters D, Rowe S, Chowdhury A, Arabi M. Impact of COVID-19 on maternal and child health. Lancet Global Health. 2020;8:e1257.
Kabir M, Saqib MAN, Zaid M, Ahmed H, Afzal MS. COVID-19, economic impact and child mortality: a global concern. Clin Nutr. 2020;39(7):2322–3.
Murewanhema G, Makurumidze R. Essential health services delivery in Zimbabwe during the COVID-19 pandemic: perspectives and recommendations. Pan Afr Med J. 2020;35(Suppl 2):143.
Khamala Wangamati C, Sundby J. The ramifications of COVID-19 on maternal health in Kenya. Sex Reprod Health Matters. 2020;28(1):1804716.
Graham WJ, Afolabi B, Benova L, Campbell OMR, Filippi V, Nakimuli A, et al. Protecting hard-won gains for mothers and newborns in low-income and middle-income countries in the face of COVID-19: call for a service safety net. BMJ Glob Health. 2020;5(6):2754.
Menendez C, Gonzalez R, Donnay F, Leke RGF. Avoiding indirect effects of COVID-19 on maternal and child health. Lancet Global Health. 2020;8:e863–4.
Hobday K, Prata N, Hulme J, Homer CS. Preventing post-partum haemorrhage at home during COVID-19: what are we waiting for? Lancet Glob Heal. 2021;9(3):e245–6.
Nelson R. COVID-19 disrupts vaccine delivery. Lancet Infect Dis. 2020;20(5):546.
Headey D, Heidkamp R, Osendarp S, Ruel M, Scott N, Black R, et al. Impacts of COVID-19 on childhood malnutrition and nutrition-related mortality. The Lancet. 2020;396:519–21.
McClure EM, Kinney MV, Leisher SH, Nam SL, Quigley P, Storey C, et al. Impact of COVID-19 on maternal and child health. Lancet Global Health. 2020;8:e1258.
Ogunkola IO, Adebisi YA, Imo UF, Odey GO, Esu E, Lucero-Prisno DE. Impact of COVID-19 pandemic on antenatal healthcare services in Sub-Saharan Africa. Public Heal Pract. 2021;2:100076.
Riley T, Sully E, Ahmed Z, Biddlecom A. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low-and middle-income countries. Int Perspect Sex Reprod Health. 2020;46:73–6.
Ahmadi A, Essar MY, Lin X, Adebisi YA, Lucero-Prisno DE. Polio in Afghanistan: the current situation amid COVID-19. Am J Trop Med Hyg. 2020;103(4):1367–9.
Ogundele OA, Omotoso AA, Fagbemi AT. COVID-19 outbreak: a potential threat to routine vaccination programme activities in Nigeria. Hum Vaccines Immunother. 2020;17:661–3.
Adesunkanmi AO, Ubom AE, Olasehinde O, Fasubaa OB, Ijarotimi OA, Adesunkanmi ARK, et al. Impact of COVID-19 on the cost of surgical and obstetric care: experience from a Nigerian teaching hospital and a review of the Nigerian situation. Pan Afr Med J. 2020;37(Suppl 1):15.
Francis NN, Pegg S. Socially distanced school-based nutrition program under COVID 19 in the rural Niger Delta. Extr Ind Soc. 2020;7(2):576–9.
Elhadi M, Msherghi A, Elgzairi M, Alsuyihili A, Elkhafeefi F, Bouhuwaish A, et al. Assessment of the preparedness of obstetrics and gynecology healthcare systems during the COVID-19 pandemic in Libya. Int J Gynaecol Obstet. 2020;150:406–24.
Roberts L. Pandemic brings mass vaccinations to a halt. Science (80-). 2020;368:116–7.
Cardwell R, Ghazalian PL. COVID-19 and international food assistance: policy proposals to keep food flowing. Spec Sect Pandemics Sustain. 2020;135:105059.
Chimhuya S, Neal SR, Chimhini G, Gannon H, Cortina-Borja M, Crehan C, et al. Indirect impacts of the COVID-19 pandemic at two tertiary neonatal units in Zimbabwe and Malawi: an interrupted time series analysis. medRxiv. 2021.
Hrynick T, Ripoll S, Carter S. Review: broader health impacts of vertical responses to COVID-19 in lon- and middle- income countries (LMICs). Brighton; 2020.
ICRC. Somalia: decline in primary health care visits and childhood vaccinations during COVID-19. 2020.
Save the Children. 60 Million Children across eight of the biggest humanitarian crises need help to survive this year, Warns Save the Children. 2021.
Rahimov BB, Singh K, Bazar C. Integrating screening for acute malnutrition into the vitamin A supplementation campaign in the Rohingya camps during the pandemic. Field Exch Emerg Nutr Netw ENN. 2020;63:61–3.
Martinez M, Akbar E, Wadood Z, Shukla H, et al. Progress toward poliomyelitis eradication—Afghanistan, January 2019–July 2020. 2020.
iMMAP/DFS COVID-19. Situational Analysis. Update#4 - Syria. 2020.
IRC. Continuing care during COVID-19: adopting life-saving approaches to treat acute malnutrition. 2020.
UNICEF. UNICEF Bangladesh Country Office. COVID-19 Response Monthly Report 17. 2020.
Roberts L. Why measles deaths are surging—and coronavirus could make it worse. Nature. 2020;580:446–7.
Dube BT, Chelang M, Mustaphi P, Harlass S, Bourdaire J, Singh K, et al. Adaptations to CMAM programming in Cox’a Bazar in the context of the COVID-19 pandemic. Field Exch Emerg Nutr Netw ENN. 2020;63:57–60.
International Development Committee. Covid-19 in developing countries: secondary impacts. 2020.
Chatterjee A. The potential impact of health care disruption on child mortality in the Middle East and North Africa due to COVID-19. 2020.
OCHA. Recent Developments in Northwest Syria. Situation Report No. 21. 2020.
Physicians Across Continents. Community surveillance Report May 20—Syria. 2020.
UNFPA. SRH Programme in NWS 2020 during the COVID-19 pandemic. 2021.
Reuters. Child malnutrition at record highs in parts of Yemen: U.N. survey. Reuters. 2020.
International Committee of the Red Cross. Nigeria: surge in malnutrition cases raises fear of looming disaster. International Committee of the Red Cross. 2020.
Save the Children. YEMEN: tens of thousands of severely malnourished children are left without treatment since March. 2020.
UNICEF UK. Malnutrition surges among young children in Yemen as conditions worsen. UNICEF UK. 2020.
Inter-Sector Coordination Group (ISCG) Gender Hub. In the shadows of the pandemic gendered impact of covid19 on rohingya and host communities. 2020.
UNICEF. Analysis of Continuity of Critical Health and Nutrition Services—Zimbabwe. 2020.
UNICEF. Trends and implications of Covid in the health sector—Somalia. 2020.
MSF. Responding to COVID-19. Global Accountability Report 2. June to August 2020. 2020.
Nwafor JI, Okedo-Alex IN, Ikeotuonye AC. Prevalence and predictors of depression, anxiety and stress symptoms among pregnant women during COVID-19-related lockdown in Abakaliki, Nigeria. 2020.
World Health Organization. The potential impact of health service disruptions on the burden of malaria: a modelling analysis for countries in Sub-Saharan Africa. Gene; 2020.
Global Financing Facility. Preserve Essential Health Services during the COVID-19 Pandemic—Yemen. 2020.
Global Financing Facility. Preserve essential health services during the COVID-19 Pandemic - South Sudan. 2020.
Global Financing Facility. Preserver les Services de Sante Essentiels Pendant la Pandemie de COVID-19—Niger. 2020.
Stein D, Ward K, Cantelmo C. Estimating the Potential Impact of COVID-19 on Mothers and Newborns in Low- and Middle-Income Countries. Health Policy Plus. 2020.
Global Financing Facility. Preserve essential health services during the COVID-19 pandemic—Somalia. 2020.
Global Financing Facility. Preserver les Services de Sante Essentiels Pendant la Pandemie de COVID-19—Republique Centrafricane. 2020.
UN Country Office Syria. COVID-19 Socio-Economic Impact Assessment. 2020.
Global Financing Facility. preserve essential health services during the COVID-19 Pandemic—Nigeria. 2020.
Edwards J. Protect a Generation. The impact of COVID-19 on children’s lives. 2020.
CARE. Girl-driven change. Meeting the needs of adolescent girls during COVID-19 and beyond. 2020.
Khorsandi P. World Food Programme warns of worsening famine in Yemen. World Food Program. 2021.
Richards K, Abdi M, Stephenson H, Northcote C, Mathieson K. Nutrition critical: why we must act now to tackle child malnutrition. London; 2020.
McKernan B. Yemen: in a country stalked by disease, Covid barely registers. The Guardian. 2020.
Al Hosse M, Edwards M. Inside the childhood hunger ‘emergency’ in Syria’a Idlib. The New Humanitarian. 2020.
Penn-Kekana L. COVID-19 and MNCH: beyond the models, what are we hearing from countries? 2020.
Global Financing facility. Preserver les Services de Sante Essentiels Pendant la Pandemie de COVID-19 - Republique Democratique du Congo. 2020.
Ramoni R. How COVID-19 is affecting antenatal care. Daily Trust. 2020.
World Vision. A double-edged sword. Protection risks facing Venezuelan children during the COVID-19 Pandemic. 2020.
Laouan FZ. Rapid Gender Analysis COVID-19. West Africa-April 2020. 2020.
Save the Children. Impact of Covid19 Outbreak on women and children: save the Children Somalia Multi Sector Study. 2020.
Janvrin A, McKay G. READY: global readiness for major disease outbreak response. Maternal, Newborn, and reproductive health and COVID-19: adaptations, successes, challenges, and next steps. An expert consultation. 2020.
Social Sciences Analytics Cell (CASS). The impacts of the COVID-19 outbreak response on women and girls in the Democratic Republic of the Congo. 2020.
West K. Collateral impacts of COVID-19 on non-COVID health—an update. 2020.
Ameh CA, Banke-Thomas AA, Balogun M, Makwe CC, Afolabi B. Reproductive maternal and Newborn Health providers assessment of facility preparedness and its Determinants during the COVID-19 pandemic in Lagos, Nigeria. 2020.
The Global Fund. Mitigating the impact of COVID-19 on countries affected by HIV, tuberculosis and malaria. Geneva; 2020.
Martinez M, Akbar IE, Wadood MZ, Shukla H, Jorba J, Ehrhardt D. Progress toward poliomyelitis eradication—Afghanistan, January 2019–July 2020. MMWR Morb Mortal Wkly Rep. 2020;69(40):1464–8.
Casey SE, Gallagher MC, Kakesa J, Kalyanpur A, Muselemu JB, Rafanoharana RV, et al. Contraceptive use among adolescent and young women in North and South Kivu, Democratic Republic of the Congo: a cross-sectional population-based survey. PLoS Med. 2020;17(3):1–16. https://doi.org/10.1371/journal.pmed.1003086.
Jones SA, Gopalakrishnan S, Ameh CA, White S, Van Den Broek NR. ‘Women and babies are dying but not of Ebola’: the effect of the Ebola virus epidemic on the availability, uptake and outcomes of maternal and newborn health services in Sierra Leone. BMJ Glob Health. 2016;1(3):e000065.
Benova L, Sarkar NDP, Fasehun LKO, Semaan A, Affun-Adegbulu C. A call to action: documenting and sharing solutions and adaptations in sexual, reproductive, maternal and newborn health care provision during the COVID-19 pandemic. Sex Reprod Heal Matters. 2020;28(1):9–12. https://doi.org/10.1080/26410397.2020.1838054.
Martineau T, Woodward A, Sheahan K, Sondorp E. Health systems research in fragile and conflict affected states: a qualitative study of associated challenges. Health Res Policy Syst. 2017;15(1):1–12.
Singh NS, Lokot M, Undie C-C, Onyango MA, Morgan R, Harmer A, et al. Research in forced displacement: guidance for a feminist and decolonial approach. Lancet. 2021;397:560–2.
Acknowledgements
We would like to thank all key informants who took part in the study. We are also grateful to the many contributors who have supported the development of this research, including colleagues from the COVID-19 Humanitarian Platform (London School of Hygiene and Tropical Medicine: Ana Teresa Afonso, Emily Bowler, Hayley Conyers, Casey Lynn Crow, Emilie Grant, Isabella Jäntti, Laura Limarzi Klyn, Adebanwo Kuye, Valentina Marino-Melán, Andrew Mok Yuan Min, Pia Mingkwan, Emre Oguzman, María J Blanco Penedo, James Smith; Geneva Centre for Humanitarian Studies: Karl Blanchet, Alex Odlum; Center for Humanitarian Health, Johns Hopkins School of Public Health: Chiara Altare, Paul Spiegel) and Liam Sollis, Delphine Valette, Jenny Vaughan, and the UNICEF UK Advocacy and International Programmes Engagement Teams.
Funding
This work was jointly supported by Unicef and UK Research and Innovation as part of the Global Challenges Research Fund, Grant No. ES/P010873/1.
Author information
Authors and Affiliations
Contributions
NSS conceptualised the study. MR and NR provided input on data collection tools and procedures. MR led the scoping reviewing and qualitative data collection with NSS. MR and LS analysed data and wrote the first draft of the paper with inputs from NSS. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study underwent ethical review from the London School of Hygiene and Tropical Medicine, UK and was deemed exempt due to not being classified as human subject research. All participants gave consent to participate in the study. We anonymised all transcribed interviews.
Consent for publication
All participants whose data is used in this manuscript gave oral consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Search terms for scoping review.
Additional file 2.
List of included countries as per World Bank.
Additional file 3.
Interview Guide.
Additional file 4.
Characteristics and key findings of literature included in the review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rodo, M., Singh, L., Russell, N. et al. A mixed methods study to assess the impact of COVID-19 on maternal, newborn, child health and nutrition in fragile and conflict-affected settings. Confl Health 16, 30 (2022). https://doi.org/10.1186/s13031-022-00465-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13031-022-00465-x