Abstract
Introduction
Uganda has high maternal, neonatal, and under-five mortality rates. This study documents stakeholder perspectives on best practices in a maternal and newborn health (MNH) quality-improvement programme implemented in the West Nile region of Uganda to improve delivery and utilisation of MNH services.
Methods
This exploratory cross-sectional qualitative study, conducted at the end of 2021, captured the perspectives of stakeholders representing the different levels of the healthcare system. Data were collected in four districts through: interviews with key informants working at all levels of the health system; focus group discussions with parents and caretakers and with community health workers; and interviews with individual community members whose lives had been impacted by the MNH programme. The initial content analysis was followed by a deductive synthesis pitched according to the different levels of the health system and the health-systems building blocks.
Results
The findings are summarised according to the health-systems building blocks and an account is given of three of the interventions most valued by participants: (1) data use for evidence-based decision making (with regard to human resources, essential reproductive health commodities, and financing); (2) establishment of special newborn care units and high-dependency maternity units at district hospitals and training of the health workforce (also with reference to other infrastructural improvements such as the provision of water, sanitation and hygiene facilities at health facilities); and (3) community referral of pregnant women through a commercial motorcycle voucher referral system.
Conclusion
The MNH programme in the West Nile region adopted a holistic and system-wide approach to addressing the key bottlenecks in the planning, delivery, and monitoring of quality MNH services. There was general stakeholder appreciation across the board that the interventions had the potential to improve quality of care and newborn and maternal health outcomes. However, as the funding was largely donor-driven, questions about government ownership and sustainability in the context of limited resources remain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The reduction of maternal, newborn and under-five mortality remains a challenge in sub-Saharan Africa and the coronavirus pandemic may have stalled or reversed recent progress [1]. Despite support for the three overarching objectives of ‘survive, thrive and transform’ of the 2016–2030 Global Strategy for Women’s, Children’s and Adolescents’ Health [2], many countries are not on track to reach the 2030 targets for Sustainable Development Goal 3, namely reducing the global maternal mortality ratio (MMR) to less than 70 per 100,000 live births, the neonatal mortality rate to 12 per 1,000 live births and the under-5 mortality rate to 25 per 1,000 live births [3]. The government of Uganda’s Sharpened Plan for Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCAH) 2016/2017–2019/2020 focused on addressing underlying constraints and accelerating progress in maternal and child health within the context of the Sustainable Development Goals and the global strategy [4]. This plan outlined the priority interventions for reducing maternal, newborn, and child mortality and described high-impact interventions for addressing the continuum of care that extends through adolescence, pregnancy, childbirth, infancy and childhood. The revised RMNCAH Sharpened Plan 2020/21–2025/6 sets ambitious targets for 2025 with regard to reducing the institutional MMR from 311 to 211 per 100,000 live births and reducing the NMR, which has stagnated at 27 per 1,000 live births for over 20 years, to 12 per 1,000 live births [5].
Maternal and newborn health in the West Nile region, Uganda
The West Nile region in the northwest corner of Uganda shares borders with the Democratic Republic of the Congo and South Sudan. It also hosts more than half of the 1.5 million refugees in the country [6]. The region is classified among the lagging regions of Uganda, hardest hit by food insecurity, with poverty significantly above the national average [7], and conditions that strongly affect maternal and newborn health (MNH) outcomes, in terms of both general health status and capacity to access services. Historically, dismal MNH indicators have been common in the region [8,9,10].
In 2018, the West Nile region embarked on the delivery of an integrated MNH quality-improvement package with substantial investments in high-impact supply-side and demand-side interventions to address key barriers to the availability and utilisation of quality MNH services in all 12 districts. The programme targeted the three delays leading to maternal and newborn deaths, namely delays in the decision to seek care, in arrival at an appropriate health facility, and in the provision of immediate and adequate care [11]. The focus was both on strengthening all levels of the health system and its building blocks to enable rapid response to the needs of mothers and newborns and on increasing community awareness, demand, acceptance, and utilisation of available MNH and nutrition services. Several development partners, donors, and agencies collaborated with the Ministry of Health and district health teams to support different components of the programme. A substantial number of the initiatives were supported by the United Nations Children’s Fund (UNICEF) through implementing partners such as the Association of Volunteers in International Service (AVSI) Foundation. Other partners included the Johns Hopkins Program for International Education in Gynecology and Obstetrics (Jhpiego), the United Nations Population Fund (UNFPA), the International Rescue Committee (IRC) and Marie Stopes Uganda (MSU).
Because of multiple-partner involvement and the comprehensive health-systems strengthening (HSS) approach, it is not possible to measure the impact of individual interventions or activities on the improvement of the MNH programme and maternal and newborn outcomes in the West Nile region. The aim of this study was therefore to answer the following question: What are the perspectives of stakeholders at the various levels of the healthcare system regarding what they consider to be the most valued MNH interventions and practices supported by UNICEF and other partners in the West Nile region of Uganda?
Methodology
Study design
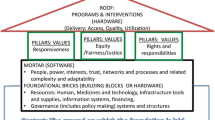
The choice of study design was guided by available budget and UNICEF’s desire to get more in-depth feedback from stakeholders at all levels of the health care system on what they perceived to be the most valuable MNH interventions in terms of improving MNH outcomes. An exploratory cross-sectional design using qualitative methods of data collection was adopted. The data collection techniques were key informant interviews, focus group discussions and in-depth interviews. For data analysis, two widely implemented frameworks – the WHO’s health-systems building blocks [12] and the different levels of the health system [13] – were selected as the lenses for categorising the interventions perceived to be of value and the effect the MNH programme had on people’s lives. The analysis also considered the supply- and demand-side shortcomings, challenges and barriers associated with these interventions.
Study setting
To attain maximum diversity, four of the 12 districts in the West Nile Region were purposively sampled for inclusion in the study. Two high-performing (D2 and D3) and two poorly performing (D1 and D4) districts were selected, based on their ranking in the national district league table of 2017/8 [14]. The two poorly performing districts were classified as high-burden districts with regard to neonatal and under-five mortality and unmet family planning needs and the better performing districts were rated as middle-burden districts [4]. The four districts constitute 50% of the total population of the West Nile region [15], host 60% of the refugees in the region [6] and are characterised by poor access to and low quality of health care services. In 2017/18, the four districts registered some of the poorest MNH indicators in the region, including low antenatal care attendance of 19.4% in the first trimester of pregnancy and high in-facility stillbirths at 87 per 1,000 births [14].
Study population and sampling
The study participants were drawn from the national, regional, district, health facility and community levels and comprised MNH programme managers, district health managers, health facility managers and healthcare providers, community health workers and community members. They were purposively selected based on their position, knowledge, experience of and/or involvement with the MNH programme. National and regional participants included UNICEF country and zonal MNH technical officers, respectively. They were health professionals with a background in medicine, nursing and public health.
Participants at the district level were members of the district health team and included district health managers and biostatisticians, who are the custodians of district-health data. Through snowball sampling, the district health managers helped the investigators to recruit eligible health-facility managers and providers. They were drawn from four hospitals (3 public, 1 private-not-for-profit) and three health centres that were beneficiaries of UNICEF partner-driven support.
Health-facility participants adopted the same approach to help identify and recruit community-based informants. Community health workers, commonly known as village health teams (VHTs) were purposively sampled from the communities served by health centres (n = 9) that participated in the MNH programme. Parents and caretakers of children under one year of age and other individuals with unique stories about how the MNH programme impacted their lives were identified by VHTs through snowball sampling.
Recruitment and data collection
Data collection took place in November and December 2021. A total of 99 participants took part in the different interview types, 33 males and 66 females. Table 1 contains a more detailed summary of the participants.
Data collection followed a specific sequence in each district (see Fig. 1). District offices were targeted first to obtain both administrative clearance for the study and permission to conduct interviews with district-level participants. This was followed by interviews held at the hospital, health centres and in the community.
Each data collection method had its own topic guide with open-ended questions, which were informed by information gleaned from an informal review of relevant government and development partner documents pertaining to the MNH programme in the West Nile region. The guides for community participants were developed in English by the investigators and later translated into the local dialects of Lugbara, Alur, and Madi. They were subsequently reviewed by research assistants fluent in the relevant local language.
The first three authors held key informant interviews (KIIs) with managers and healthcare providers from all levels of the health system who were considered to be information rich – zonal and national officials (ZN), district health officials (DO), health-facility (HF) participants (including medical superintendents and those in charge of health centres).
Research assistants fluent in the local language conducted focus group discussions (FGDs) and in-depth individual interviews (IDIs) with community members. The eight assistants (4 males, 4 females) resided in the study districts; all held at least a bachelor’s degree in humanities and some had previous experience in interviewing. They all received thorough orientation and training in the study protocol, the technical interventions and interviewing techniques. In order to elicit more general views of community members on the MNH interventions at community level, separate FGDs with 6-8 participants each were held with each community category (community health workers and parents/caregivers), two discussions per district. The focus of the IDIs was to record ‘human-interest stories’ from individuals who had benefited from specific MNH interventions, such as efforts to promote delivery at health facilities. In each district, a mother, a VHT member and a commercial motorcyclist (a boda-boda rider) (BB) were interviewed to cover perspectives on some of the most important demand-side delays addressed by the interventions.
Interviews lasted between 40 and 60 minutes and all interviews were audio-recorded with permission. KIIs were held in the privacy of regional, district and health-facility offices and other convenient venues like hotel premises. Private places were designated in the communities for FGDs and IDIs. Due to the short timeframe and the fact that interviews took place concurrently in different districts, data saturation could not easily be monitored. The subsequent data analyses revealed recurrent information from the different districts and at the different levels.
Data management and analysis
All the audio-recorded interviews and FGDs were transcribed verbatim and those conducted in the local languages were translated into English. Transcripts were saved electronically with unique ID codes. Audio-recordings and documents were securely kept in the first author’s office.
Data analysis consisted of a combination of inductive and deductive analysis (Fig. 1). The first round of analysis was guided by two different approaches to analysing the content of 38 transcripts. Researchers familiarised themselves with the data, generated initial codes and searched for themes [16]. The first three authors used a directed approach [17] to content analysis and worked together in an iterative process of manual analysis of the data, organising relevant quotes according to specific categories or codes, and developing a coding scheme related to the different health-system levels. The last author performed a conventional content analysis [17] to define codes during data analysis with a view to confirming the feasibility of the interpretation of the first three authors. The supplemental file contains an example of the nodes created from the KIIs using NVivo9 software. The categories and topics that emerged from the two analyses were discussed, compared and combined.
In the second round of analysis, we used the health-systems building blocks [12] and the health-system levels [13] deductively to synthesise the valued interventions emerging from the first round of analysis. This was aimed at aligning our analysis with the conceptualisation of the interventions that were included in the MNH quality-improvement programme documents.
Rigour
Various measures were put in place to enhance the rigour of the study, using Nowell et al.’s pointers for establishing trustworthiness [16]. Credibility is demonstrated by the regular discussions between the researchers from the inception of the study to the report-writing stage and by the audit trail of field notes and coding decisions that was kept. Although the study was funded by UNICEF and its officials contributed to the study design, none of them was involved in the data collection and analysis or the interpretation of findings. Drafts of the study report were circulated among national, zonal and district-level managers in the West Nile region and the study districts for comments. As some of these individuals were key informants in the study, this could be considered a form of member checking. UNICEF also gave feedback to stakeholders at all levels through a PowerPoint presentation and by sharing the final report. With regard to the study itself, researchers from two institutions analysed the data independently, and verbatim quotations from participants are included in this paper. Some of the findings may be transferable to other districts in Uganda with similar populations and contexts. Triangulation, achieved through the inclusion of different categories of informants (district managers, service providers, users of the services and agents in service access) and different data collection methods, demonstrates dependability. Confirmability in study design and data analysis was enhanced by the combination of independent researchers from different institutions and programme staff with diverse disciplinary backgrounds.
Ethical considerations
Ethical clearance was obtained from the Makerere University Higher Degrees Research and Ethics Committee (SPH-2021-162). Permission for the study was obtained from the respective district health offices and managers of health facilities. Written informed consent was obtained from all participants. The data collectors signed confidentiality agreements.
Results
The MNH interventions in the West Nile region should be considered against the macro-level policies and strategic directions of the national development plan. Health-system interventions are endorsed and supervised by the Ministry of Health. Partners saw their role as supporting these policies and strategies, but following a district-needs, HSS approach, to supplement government contributions – ‘they [the partners] keep saying, identify your gap and tell us what you want’ (KII HF D3). Health-system stakeholders perceived all the interventions as equally important in a holistic approach – ‘you cannot really choose because they are all targeting different … [but] not competing priorities’ (KII HF D3).
The findings are divided into four broad topics. Firstly, the MNH interventions and activities valued by stakeholders are described according to health-systems building blocks. This is followed by a more detailed account of three of the most valued MNH interventions: using data to improve the quality of MNH care (district and facility level); upgrading neonatal and maternity units and training the health workforce (facility level); and the boda-boda motorcyclist referral system (community level).
MNH interventions and activities valued by stakeholders
Table 2 summarises the main interventions in the West Nile MNH programme as well as the challenges mentioned by stakeholders, organised according to the WHO’s health-systems building blocks [12]. Some of the interventions were more general, such as the provision of water, sanitation and hygiene (WASH) facilities and the use of data to improve services, whereas others, such as the upgrading of maternity and neonatal units, were specifically focused on improving the quality of MNH care. Interventions considered pivotal were those pertaining to capacity building of managers and healthcare providers and to access to and delivery of safe, quality services.
Coverage of a wide range of interventions was made possible by heavy investment by UNICEF through its development partners. The outstanding challenge is for the district local governments in the region to provide oversight and, in time, take over, scale up and sustain these expensive interventions – ‘at the district [level], local government [should] have [a] certain level of commitment’ (KII ZN). A number of informants identified the two main challenges for healthcare facilities:
‘If finances are there and in the right hands, … the two biggest things for a healthcare facility [are] human resource[s], and then of course, … medicines and supplies. We need … good governance’ [our emphasis] (KII HF D3).
Use of data to improve the quality of maternal and newborn care
At the district, zonal and national levels, participants referred to the partner-supported training activities for district and hospital administrators in planning, management and budgeting to enable them to do evidence-based planning using bottleneck analysis and real-time monitoring and action performance (RTMAP). This is how a district biostatistician explained the way they used data:
‘All the interventions that we implement within the district health sector should be based on evidence-targeted interventions, … and this evidence is actually the data. … So whatever activity we are doing, the [annual] work plan that we generate … is arrived at by analysing data. For example, we are not going to say we are going to do community dialogues if the choice of that activity was not informed by data. So, we always do things according to data. Every activity is backed by evidence. … And it is the direction that even now the Ministry wants. We are not going to say we are going to do this training when we have done our analysis and there's no indication that there was need for training, because … my work is to analyse the data and make the presentation and then we analyse it together. And then we get the root cause of the problem from that data. And that is what informs our work plan, our programming. So, we're not going to tolerate just any activity from any partner, when data has shown that there is no problem there’ (KII DO D2).
Data were also used to identify and analyse the factors contributing to maternal and newborn health outcomes. Reference was made to support for quarterly maternal and perinatal death surveillance and response (MPDSR) meetings that provided crucial data for the district health team’s monitoring of district performance and identification of bottlenecks related to the three delays in care.
One official reflected on HSS based on reliable data as a process that takes time to establish:
‘Many of the interventions happening right now really seem to be new interventions with the results. But it needs time for the district and the local government team to be well versed with data and therefore implement with confidence’ (KII ZN).
Data-based performance included review across the different health-systems building blocks – ‘Through the regular performance review meetings … we jointly generate solutions for improving performance’ (KII DO D3). Three specific building blocks were pertinent in the stakeholder perspectives: human resources; essential reproductive health commodities; and financing.
Human resources
With regard to human resources, reviews highlighted the lack of adequate financial resources to employ sufficient numbers of staff and to conduct MNH capacity building and training activities for which support had been negotiated with development partners. For example, UNICEF supported the districts with ‘the placement, including payment of salary, of the critical staff’ (KII ZN) and complemented the efforts of the district service commissions to recruit and second critical staff cadres in circumstances where there were no funds for recruitment and where the wage bill was not fully utilised by the districts – ‘This staff was initially supported by UNICEF directly, but later on, the district absorbed them’ (KII DO D2).
Essential reproductive health commodities
The performance reviews also considered the availability of essential commodities and proposed solutions for delays in deliveries of commodities from the national medical stores and for challenges in ordering appropriately and on time. Participants at various levels of the health system referred to the support they had received from partners to adequately prioritise reproductive health commodities and thereby avoid supply chain gaps – ‘Much of the things that make [the] community come to the facilities is availability of commodities’ (KII DO D1). One commodity particularly highlighted as an incentive for increasing safe delivery at health facilities was a basic birthing kit (mama kit) for all women – ‘Those small things which we ask from them at times send [put] them off [from giving birth in a health facility]’ (KII DO D1). Unfortunately, these kits were also in short supply.
Health-system stakeholders emphasised the importance of donor support for short- and medium-term ‘buffer stocks’ (KII DO D1) but also the need ‘to build capacity of not only the district, but also the facilities on how to prioritise and manage commodities’ (KII ZN). Although the situation seemed to have improved, the government’s ability to address the procurement challenges in a sustainable manner remained a concern – ‘If for essential commodities, government still relies heavily on partners, then it is a dangerous situation to be in’ (KII ZN). Donor provisions are mostly associated with particular projects and projects are only funded for limited periods.
Financing
Participants expressed concern about the sustainability and maintenance of some of the valued interventions in the MNH programme that required sustained financing. District officials referred to the difference made by support from partners and the implementation of results-based financing (RBF) at health-facility level. Improved performance as demonstrated by the analysis of the collected data meant improved financing through the RBF vehicle, complemented by additional support from partners:
‘RBF funding … has helped us to maintain the hospital. We had a lot of items which are missing … for the management of our cases for maternal-child health. …We tried to buy some … equipment, but where we fell short, UNICEF also came in and it was able to easily procure. …The other factor is just the funding which has improved, which we prioritise’ (KII HF D1).
On the other hand, there were also reports from hospital stakeholders that payment delays through the RBF facility impacted the availability of medicines:
‘We have had babies die, because the mothers cannot afford or they are buying the medicines occasionally. … We have been heavily reliant on … RBF to make sure that we have stock, but the last RBF that came was in quarter two of the last financial year. And even as we talk, we are still demanding money for three quarters, actually four now’ (KII HF D3).
Although health facilities benefited from donor support and RBF, especially where the managers demonstrated good leadership, district-level technical leaders in charge of maternal and child health felt they were underfunded and could not fulfil their leadership and supervisory roles. The absence of a specific budget for MNH at district level also contributed to challenges:
‘There is no budget pointing to maternal and child health. They always say Environmental Health 30% of the PHC [primary health care]. So, which percentage is for maternal health which covers the 80% of the services that are offered? That is a big problem’ (KII DO D3).
Upgrading neonatal and maternity units and training the health workforce
Quality improvements related to HSS were most visible at health-facility level – ‘Whatever we are doing, we implement at facility level; we pack the knowledge to the facility and it is at that level that we want to see change’ (KII DO D2). Improvements in infrastructure and workforce training were among the interventions particularly valued by healthcare providers.
The establishment, refurbishment and equipping of neonatal care units and high-dependency maternity units for at-risk women at district hospitals were highlights for stakeholders in terms of the reciprocal support between implementing partners and health facilities, with hospitals providing space and partners providing support in the form of equipment, medicines and training.
‘We used to have challenges of monitoring and managing critically ill patients especially those after operation[s]. … And so now we're able to monitor mothers and newborns more effectively’ (KII ZN).
The holistic HSS approach went beyond MNH to include the establishment of WASH facilities, in addition to the provision of neonatal and high-dependency maternity units.
Neonatal care units
All informants appreciated the benefits of the neonatal care units with ‘a lot of equipment that is in there’ (KII HF D3) and how these units influenced survival rates:
‘If I'm on gunpoint and have to choose one [intervention] … I think the neonatal care unit has had the most impact as far as I'm concerned’ (KII HF D3).
‘When a baby is born and has some issues, they are handled in that unit to improve on their survival and also help the community because without that facility, it will lead to a lot of referrals, which some of the clients would not afford’ (KII HF D1).
High-dependency units
UNICEF, through AVSI, established fully functional and well-equipped high-dependency units – ‘an intermediate between the general ward and the ICU [intensive care unit]’ (KII HF D3) – in all district hospitals in the West Nile region. This idea emerged during the coronavirus pandemic:
‘Because mothers were coming later, there was more need for critical care. And so, making sure that facilities had the space and also had the capacity to not only prevent but also manage [critical care needs] in a timely manner … is an intervention that has arisen in response to this whole COVID situation’ (KII ZN).
Participants described the benefits of the improved maternity wards in term of ‘quality of care of critical patients’ (KII HF D2) and maternal survival, because of the capacity to identify complications – ‘especially [during] the critical monitoring period, the 24 hours, so that if anything goes wrong, it can be detected early enough’ (KII HF D1).
‘Then also the high-dependency units with the space especially for the mothers, which were stretched to help us to greatly cut down on maternal deaths when they are in delivery’ (KII HF D1).
Monitoring of equipment provision
Donations of equipment were not channelled through the district office, but were provided in kind directly to facilities, with donor follow-up on the whereabouts and use of the equipment. This promoted accountability and immediate use of equipment.
‘They [the partner] ask you what equipment you want, and they bring, as opposed to say that now let's give you money and you go and buy. … So, I think one of the best practices [is] their way of following up. … If it is the hospital which has requested [equipment] … they come direct to the hospital store, not to district first. … An officer comes following up to see if they are functional. I think that is a very good best practice’ (KII HF D2).
Maintenance of equipment remained a problem and informants reported that some of the equipment provided was not of the right type or was faulty, examples being oxygen concentrators, incubators and warmers.
Other infrastructure improvements
Stakeholders perceived facility-based WASH improvements as very important for improving the quality of MNH care and attracting facility-based deliveries. These improvements included rehabilitating health facilities’ water systems and establishing related infrastructure (e.g. tanks, toilets, taps, sinks, bathrooms). This is ‘because sometimes what pulls away [hinders] people from getting some services in the facility is what the facility will look like’ (KII ZN).
The biggest impact of WASH improvements described by participants was the reduction in infections:
‘It has shifted the problem of sepsis … in [our health centre] … which won an award last year in the whole country. … because there's no sepsis, the place is very clean, water is running everywhere’ (KII DO D3).
Another infrastructural deficit that received much appreciated attention was the issue of unreliable power sources:
‘Having the standby generator is a beautiful [achievement]. This really stands out. … Our emergency deliveries are no longer at stake [risk] because we have a standby power source which was a very big concern [before]’ (KII DO D2).
On the other hand, there were also fuel challenges to running generators during power outages ‘which the hospital budget cannot offset’ (KII HF D1).
Training the health workforce
Establishment of special units was accompanied by thorough training of hospital staff to manage the units and provide comprehensive emergency obstetric and newborn care. Specialists were brought in to train medical officers in order to reduce referrals to regional hospitals. Informants also referred to off-site training and/or on-site mentoring that they felt could have influenced the quality of maternal and newborn care services.
‘When the teams came back [from off-site training], they were able to pass these to other staff. And even when the staff moved on, at least the team they have left behind has picked up from that. And then even the mentorships which have come through, have really improved [the care].’ (KII HF D4)
A catch-22 situation
Despite much appreciation for the contributions of partners and the perceived improvement in health outcomes for mothers and babies, the establishment of the special neonatal units and the high-dependency units has also created a dilemma: what is the point of having brand new units but with no change in staffing norms to make it possible to employ additional specialised staff?
‘You know, there is giving you a new unit that was not planned for and you have to squeeze the little human resource that you have to support the community’ (KII HF D3).
‘We recognise that staffing is really, really a challenge and some of the units may become white elephants because of staffing’ (KII ZN).
Provider participants echoed a similar dilemma: what is the point of training staff, amongst others, on the use of equipment, if there is no reliable power source to keep the equipment running?
‘So, that intervention really worked very much because when that capacity was built, we were able to … create a room as a newborn care unit… [but] we still have that massive challenge of power. So, we could not run our incubator, we could not run the warmers which were donated …. Equipment has been there but since we are not connected to the national grid, running that equipment on solar power was difficult. So, we basically just [make] do. We now ask the mothers to do more of kangaroo temperatures [kangaroo mother care]’ (KII HF D4).
The boda-boda motorcyclist referral system
A key aim of the interventions of the MNH programmes in the West Nile region was to increase utilisation of available services and address two of the delays in MNH care. Village health teams (VHTs) were used to create community awareness of the importance of planning for a health-facility delivery and boda-boda motorcyclists were engaged to transport women to reach the health facility in good time for delivery.
A boda-boda is a commercial motorcycle taxi used to transport people and commodities. A boda-boda referral system was established to transport high-risk pregnant women and newborns with danger signs to health facilities. Selected boda-boda riders from the communities in the catchment areas of health facilities were trained in basic first aid for pregnant women in labour and on how to transport them to a health facility. Participants explained that the boda-boda motorcyclists operated on a voucher system and the women were not required to pay. When a boda-boda operator brought a woman to the facility, he received a voucher. At the end of the month, the boda-boda operators brought their vouchers to the health facility, where they were verified and reconciled with the health facility’s copies. They were then paid by ASVI through Mobile Money, an electronic wallet service for transferring money anywhere in Uganda with a mobile phone.
The free boda-boda referral system was praised by community participants in all the focus groups and individual interviews as having made a difference – ‘Money which was [formerly] used for transport has been used to support us in other basic needs’ (IDI Mother D1):
‘Pregnant women and their caretakers are provided transport through the boda-boda services, and this helps mothers a lot, especially in our community where the majority of the mothers are poor and cannot afford transport. These boda-bodas don’t ask for money from the mothers because they are paid by AVSI. Very many women and their children from our community have used the boda riders (FGD VHT D1).’
Boda-boda cyclists perceived the timely referral and availability of transport as ‘making it easy for medical management [of emergencies]’ (IDI BB D3) and saving the lives of mothers and babies. Community stakeholders also referred to the boda-boda system as one of the most significant changes with regard to MNH. Free transport through the boda-boda system meant better access to MNH services – ‘The different service available for the mothers and their babies has also made it easy for us to access the services from within our locality’ (FGD Mother D3). Table 3 contains a narrative by one mother who benefited from actions of the VHT and the boda-boda system.
Boda-boda riders elaborated on how the system had changed their own lives for the better and earned them ‘respect from community members’ (IDI BB D4). Informants referred to other benefits like an improved standard of living with better nutrition and improved health and the ability to afford school fees, acquire a phone, buy livestock and repair dwellings. Another major benefit mentioned was learning how to manage money prudently and developing ‘a saving culture in my family’ (IDI BB D2):
‘I don’t touch any other money I get from my business … and the money I get normally accumulates and caters for what I planned to buy or acquire which was not the case at the beginning. … I have opened an account with [X] Town Council SACCO, where I am currently saving money I get from AVSI and other sources. I plan to construct a house’ (IDI BB D1).
However, the boda-boda system was not without challenges. The most important one for the drivers was delays in payment after verification of the vouchers – it ‘took quite a lot of time to effect payments’ (IDI BB D1). Transporting women back from the health facility was not covered by the voucher system. Individual voices referred to unfulfilled requests for ‘reflector gadgets, gumboots and raincoats’ (IDI BB D1) to make transport safer and ‘to enable us to work in even the rainy season’ (IDI BB D2). Other points included a fixed salary, some form of allowance for riders who carried fewer mothers per month and the provision of motorcycles. It also appeared that the boda-boda system was not functional everywhere at the time of the study – ‘the boda-boda referral ceased’ (IDI VHT D3).
This is how the head of a health centre described both the improvement brought about by the boda-boda cyclists with regard to community delays in care seeking and access and the cyclists’ dilemmas associated with the system:
‘One of the good things is we are able to receive a number of referrals from the community to the facilities. … It has really improved the issues of the deliveries at health-facility level. … Then the challenge is the boda-bodas complain about payment. … their money delays for some time and yet they use their fuel. … So, it has really brought the morale of these boda-boda men a bit down. That's why you see there are some who are not so much active in carrying these referrals to the facility’ (KII HF D2).
Discussion
The MNH quality-improvement programme in the West Nile region adopted a holistic, HSS approach based on evidence of effective interventions applied elsewhere [18] and addressed health-system gaps at district, health-facility and community level. The findings illustrate how different health programmes and building blocks do not work separately in silos, but instead work in conjunction to improve service delivery [19, 20]. This may also explain stakeholder perceptions of that interventions were equally important, with the inclusion of broader interventions that impacted on the delivery of the MNH programme (e.g. WASH, use of data and RBF). The interventions that stakeholders valued were also a fulfilment of the policy prescriptions for a high-impact maternal and newborn care package in Uganda [21].
The data-driven approach at district and facility level set the scene for measuring maternal and newborn health outcomes and monitoring the implementation of MNH interventions at the facility and community levels. Facility-based activities that stakeholders at district and facility levels perceived to have improved the quality, uptake and utilisation of MNH services and maternal and newborn health outcomes included the refurbishment of neonatal and maternity units (including upgrades of WASH facilities and the provision of additional power sources) and the upskilling of health managers and frontline healthcare providers through training, on-site mentoring and other capacity-building activities. Community-based interventions perceived to increase maternal and newborn survival included the boda-boda-referral transport system.
The Ugandan government is committed to the use of ‘data for action’. This approach is included not only in the Every Newborn Action Plan (ENAP) [22] and the Ending Preventable Maternal Mortality (EPMM) [23] documents, but also in the survive, thrive and transform agenda ‘to end preventable deaths (survive); ensure health and well-being (thrive); and change how small and sick newborns are cared for (transform)’ (page 91) [24]. The description in our paper focused largely on interventions aimed at transforming the health system to help mothers and their newborns to survive and thrive through quality care. The WHO-UNICEF Survive and Thrive report suggests indicators for the different levels of the health system. National tracking data should include indicators for impact, coverage, service readiness, human resources, equipment and drugs. At the district level data coverage indicators should be complemented with more detailed indicators of service readiness, equipment and drugs. Facility-level management should be responsible for quality improvement process data [24].
The upgrading of facility infrastructure is an intervention that appears in many donor-supported MNH programmes to improve the provision of quality maternal and newborn care. Planning of and investment in hospital infrastructure and capacity building of health providers for small and sick newborn care are currently high on the health agenda in low- and middle-income countries (LMICs) [25] and are also part of the West Nile MNH programme. Two of the meso-level subtype interventions identified by a systematic review of quality improvement initiatives for hospitalised sick and small newborns in LMICs were strengthening facility infrastructure and in-service training (the most featured subtype) [25]. The challenges emanating from infrastructural improvements and human resource challenges mentioned in our study are commonly reported in other studies [26, 27]. One issue that strongly emanated from our study is that there should be a comprehensive strategy for addressing human resources at national level.
Globally governments and development partners are continuously considering innovative ways to reduce the delays that can occur between a pregnant woman and her family’s decision to seek facility-based delivery care and her arrival at a health facility. This discussion usually includes available transport options. Boda-boda transport is common in countries like Uganda, Kenya and Tanzania and also elsewhere in the world, where it may be known by other names. One Ugandan study reported on training boda-boda riders for transporting emergency medical cases in general [28]. Two further studies showed an increase in facility-based antenatal and/or delivery care. A non-randomised controlled trial in the Busoga region of Uganda used monetary and non-monetary incentives for mothers, midwives, VHTs and boda-boda riders and showed both an increase in the use of boda-boda transport by expectant women to reach a facility for delivery and a decrease in response time from trained boda-boda riders [29]. A quasi-experimental pilot study in Eastern Uganda using supply- and demand-side incentives – including vouchers for transport – showed a marked increase in facility-based antenatal and delivery care, which again dropped off at the end of the pilot [30]. In addition, economic spill-over effects on the family and dependants – similar to the findings in our study – were also reported [31]. The study also reported concerns with regard to sustainability and cost-effectiveness [30]. None of these studies reported on the impact of this intervention.
The three-delay model has been widely used in LMICs to identify barriers to access to obstetric care with a view to designing evidence-based interventions to improve care and service delivery [32]. Uganda was the first country to expand the application of the three-delay model to explore the identification of causes of newborn mortality [33]. Although there are many references to the three-delay model in Ugandan policy documents and instruments, according to Mukuru et al., the piecemeal additions to policy instruments and the lack of coherence and consistency have resulted in the persistence of the three delays [34]. In our study, stakeholders referred to challenges in the continuity of delivering donor-supported interventions aimed at addressing the three delays and raised questions about sustainability without increased contributions from government. This was mentioned particularly with reference to resources for essential medications and fuel, the staffing of upgraded maternal and newborn units, and the boda-boda transport system.
Stakeholders had positive perceptions of the MNH interventions in the West Nile region, but also referred to challenges, gaps and bottlenecks. This suggests that the design of interventions based on the health-systems building blocks framework and the three-delay model may not be able to capture all the dynamic and complex processes and outcomes of an interlinked system and the broader community determinants of health-seeking behaviour [35, 36]. A case in point that was emphasised in our study was the upgrading of infrastructure and the provision of equipment, but also the non-availability of more healthcare providers, incompatibilities between equipment and the power supply, and the lack of fuel for generators. Cessation or deterioration of certain interventions and delays in payment could well demoralise frontline healthcare workers and community providers in the long run. Furthermore, interventions should transcend mere technology and the provision of a reliable power supply for special care units to include a person-centred enabling environment with privacy, positive healthcare provider communication, and positive facility leadership structures as the basis for sustained improvement in respectful and dignified maternal and newborn care [37].
While policies and strategies in Uganda are well formulated at the national level, stakeholders in our study alluded to having limited resources for the operationalisation of MNH policies at the district, health-facility and community levels. There were indications that at a national level some of the more general priorities had not been addressed sufficiently and general gaps in staffing norms and insufficient funding for district health offices were perceived to impact on the provision of MNH services. It is common for insufficient funding to be underrated at a central level, from which only limited funding is provided, with strings attached. Fiscal decentralisation of sufficient resources and district management has been challenging in several settings [19, 38].
Furthermore, donor support should not be seen as a panacea for all health-system problems. Sociologists have argued that the discourse of sustainability among donors and non-governmental organisations actually contributes to the undermining of HSS projects. This is based on the so-called ‘sustainability doctrine’ which favours short-term funding streams for targeted interventions instead of addressing the long-term needs of local populations [39, 40]. Sustainability was also raised in our study with regard to the maintenance of WASH facilities, the financing of essential commodities and the appointment and retention of special-skills staff for the newly established maternal and newborn units.
It has been argued that HSS should consider establishing resilient systems [41]. Most sources included in a scoping review by Fridel et al. referred to the characteristics of health-system resilience in terms of adaptation, maintenance, absorption, learning, transformation, and withstanding and responding to shocks [42]. These characteristics have not been explored in our study and merit further attention.
Methodological considerations and limitations
The study was conducted in only four districts in one region of Uganda. A purposive sample covered four diverse districts, different levels of the health system and provider and beneficiary stakeholders to allow for maximum variation. Our study did not elicit the perspectives of community leaders, however.
The use of snowballing through the hierarchies of the health system may have introduced bias because potential participants were known to the level above, so power imbalances may have come into play. The fact that study participants included members involved in the implementation of the quality-improvement programme in the West Nile region may also have created social desirability bias in participant descriptions of the interventions. To reduce potential bias, investigators included probes on challenges experienced in the implementation of the MNH programme in the KIIs and compared perspectives across the different districts and health-system levels. Although the findings may not be generalizable because district contexts and leaderships vary and each district has its own configuration of partners, other districts and countries may find many of the findings transferable because of the universality of the interventions included in the programme. Table 4 provides a list of recommendations for consideration in planning the way forward for the MNH programme.
Conclusion
The MNH programme in the West Nile region adopted a holistic and system-wide approach to addressing the key bottlenecks in the planning, delivery, and monitoring of quality MNH services and was largely shaped by a conducive policy environment and outstanding donor support. Stakeholders at the various levels of the health system expressed appreciation for the most important innovations included in the programme to improve quality, to provide the needed facilities for safe delivery and to reduce all three sources of delay. Although there was a general view across the board that the interventions had the potential to improve newborn and maternal health outcomes, the implementation of HSS initiatives needs to be well planned and can be suboptimal if resource constraints do not allow for appropriate alignment between the health-systems building blocks and the different levels of care. Since the funding was donor-driven, questions about government ownership and sustainability in the context of limited resources remain.
Disclaimer
The views are those of the authors and do not reflect the official position of the United Nations Children’s Fund.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available because it was a qualitative study but are available from the corresponding author on reasonable request.
Abbreviations
- HSS:
-
Health-systems strengthening
- FGD:
-
Focus group discussion
- IDI:
-
In-depth individual interview
- KII:
-
Key informant interview
- LMICs:
-
Low- and middle-income countries
- MMR:
-
Maternal mortality ratio
- MNH:
-
Maternal and newborn health
- RBF:
-
Results-based financing
- RMNCAH:
-
Reproductive, Maternal, Newborn, Child and Adolescent Health
- UNICEF:
-
United Nations Children’s Fund
- VHT:
-
Village health team
- WASH:
-
Water, sanitation and hygiene
- WHO:
-
World Health Organization
References
United Nations. The Sustainable Development Goals Report. 2021. https://unstats.un.org/sdgs/report/2021/. Accessed 24 Aug 2022.
Every Woman Every Child. The global strategy for women’s, children’s and adolescents’ health (2016-2030). 2015. https://www.everywomaneverychild.org/wp-content/uploads/2017/10/EWEC_GSUpdate_Full_EN_2017_web-1.pdf. Accessed 3 Aug 2022.
World Health Organization (WHO). Health in 2015: from MDGs to SDGs. Geneva: WHO; 2015. https://www.who.int/data/gho/publications/mdgs-sdgs. Accessed 4 Jan 2022.
Government of Uganda, Ministry of Health. Investment Case: Reproductive, Maternal, Newborn, Child and Adolescent Health Sharpened Plan for Uganda 2016/17-2019/2020. Kampala: Ministry of Health; 2016. https://www.health.go.ug/cause/reproductive-maternal-newborn-child-and-adolescent-sharpened-plan-for-uganda-2016-17-2019-20/. Accessed 21 Sept 2021.
Government of Uganda, Ministry of Health. Reproductive, Maternal, Newborn, Child, Adolescent and Healthy Aging Sharpened Plan II 2020/21 – 2025/26. November 2020.
UNHCR. Uganda Comprehensive Refugee Response Portal (data for 31 August, 2021). 2021. https://data2.unhcr.org/en/country/uga. Accessed 21 Sept 2021.
Government of Uganda, National Planning Authority. Third National Development Plan (NDPIII) 2020/21 – 2024/25. Kampala: Ministry of Finance, Planning and Economic Development; 2020. http://www.npa.go.ug/wp-content/uploads/2020/08/NDPIII-Finale_Compressed.pdf. Accessed 30 Jan 2023.
Akello B, Nabiwemba E, Zirabamuzaale C, Orach CG. Risk factors for perinatal mortality in Arua regional referral hospital, West Nile, Uganda. East Afr J Public Health. 2008;5(3):180-185. https://doi.org/10.4314/eajph.v4315i4313.39000.
Komakech H, Lubogo D, Nabiwemba E, Orach CG. Essential newborn care practices and determinants amongst mothers of infants aged 0-6 months in refugee settlements, Adjumani district, west Nile, Uganda. PLoS One. 2020;15(4):e0231970. https://doi.org/10.1371/journal.pone.0231970.
Roberts DA, Ng M, Ikilezi G, et al. Benchmarking health system performance across regions in Uganda: a systematic analysis of levels and trends in key maternal and child health interventions, 1990–2011. BMC Medicine. 2015;13(1):285. https://doi.org/10.1186/s12916-12015-10518-x.
Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38(8):1091–110.
World Health Organization (WHO). Monitoring the building blocks of health systems: a handbook of indicators and their measurements strategies. Geneva: WHO; 2010. https://apps.who.int/iris/bitstream/handle/10665/258734/9789241564052-eng.pdf. Accessed 20 Sept 2021.
Samuels F, Amaya A, Rodríguez Pose R, Balabanova D. Pathways to progress: a multi-level approach to strengthening health systems. Findings on maternal and child health in Nepal, Mozambique and Rwanda, and neglected tropical diseases in Cambodia and Sierra Leone. London: Overseas Develpment Institute;2014. https://odi.org/documents/4697/9370.pdf. Accessed 2 June 2022.
Government of Uganda, Ministry of Health. Annual Health Sector Performance Report. Financial Year 2017/18. Kampala: Ministry of Health; 2018. http://library.health.go.ug/sites/default/files/resources/AHSPR%202017_18%20FY.pdf. Accessed 22 Sept 2022.
Uganda Bureau of Statistics (UBOS). The National Population and Housing Census 2014 – Main Report. Kampala: UBOS; 2016. https://www.ubos.org/wp-content/uploads/publications/03_20182014_National_Census_Main_Report.pdf. Accessed 30 Jan 2023.
Nowell L, Norris J, White D, Moules N. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Meth. 2017;16(1):1–13. https://doi.org/10.1177/1609406917733847.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Lassi ZS, Salam RA, Das JK, Bhutta ZA. Essential interventions for maternal, newborn and child health: background and methodology. Reprod Health. 2014;11(1):S1. https://doi.org/10.1186/1742-4755-1111-S1181-S1181.
Cobos Muñoz D, Merino Amador P, Monzon Llamas L, Martinez Hernandez D, Santos Sancho JM. Decentralization of health systems in low and middle income countries: a systematic review. Int J Public Health. 2017;62(2):219-29. https://doi.org/10.1007/s00038-00016-00872-00032.
Kuruvilla S, Bustreo F, Kuo T, et al. The Global strategy for women's, children's and adolescents' health (2016-2030): a roadmap based on evidence and country experience. Bull World Health Organ. 2016;94(5):398-400. https://doi.org/10.2471/blt.2416.170431.
Otolorin E, Gomez P, Currie S, Thapa K, Dao B. Essential basic and emergency obstetric and newborn care: from education and training to service delivery and quality of care. Int J Gynaecol Obstet. 2015;130(Suppl 2):S46–53. https://doi.org/10.1016/j.ijgo.2015.1003.1007.
World Health Organization (WHO), United Nations Children's Fund (UNICEF). Every Newborn: an action plan to end preventable deaths. Geneva: WHO; 2014. https://cdn.who.int/media/docs/default-source/mca-documents/advisory-groups/quality-of-care/every-new-born-action-plan-(enap).pdf?sfvrsn=4d7b389_2. Accessed 14 April 2023.
World Health Organization (WHO), United Nations Population Fund (UNFPA). Ending preventable maternal mortality (EPMM): a renewed focus for improving maternal and newborn health and well-being Geneva: WHO; 2021. https://apps.who.int/iris/bitstream/handle/10665/350834/9789240040519-eng.pdf. Accessed 14 Apr 2023.
World Health Organization (WHO), United Nations Children's Fund (UNICEF). Survive and thrive: transforming care for every small and sick newborn. Geneva: WHO; 2019. https://apps.who.int/iris/bitstream/handle/10665/276655/WHO-FWC-MCA-18.11-eng.pdf?ua=1. Accessed 14 Apr 2023.
Zaka N, Alexander EC, Manikam L, et al. Quality improvement initiatives for hospitalised small and sick newborns in low- and middle-income countries: a systematic review. Implement Sci. 2018;13(1):20. https://doi.org/10.1186/s13012-018-0712-2.
Nishimwe C, McHunu GG. Stakeholders perceptions regarding implementing maternal and newborn health care programs in Rwanda. BMC Health Serv Res. 2021;21(1):796. https://doi.org/10.1186/s12913-021-06824-3.
Masefield SC, Msosa A, Grugel J. Challenges to effective governance in a low income healthcare system: a qualitative study of stakeholder perceptions in Malawi. BMC Health Serv Res. 2020;20(1):1142. https://doi.org/10.1186/s12913-020-06002-x.
Brown HA, Stratton AJ, Gill J, Robinson SF, Tumisiime V, Brady C. Piloting a layperson prehospital care system in rural Uganda. Prehosp Disaster Med. 2023;38(2):179–84. https://doi.org/10.1017/S1049023X23000201.
Muluya KM, Mugisha JF, Kithuka P, et al. Incentives for mothers, health workers and “boda-boda” riders to improve community-based referral process and deliveries in the rural community: a case of Busoga Region in Uganda. Reprod Health. 2022;19(1):24. https://doi.org/10.1186/s12978-022-01334-9.
Ekirapa-Kiracho E, Waiswa P, Rahman MH, et al. Increasing access to institutional deliveries using demand and supply side incentives: early results from a quasi-experimental study. BMC Int Health Hum Rights. 2011;11(1):S11. https://doi.org/10.1186/1472-698X-11-S1-S11.
Pariyo GW, Mayora C, Okui O, et al. Exploring new health markets: experiences from informal providers of transport for maternal health services in Eastern Uganda. BMC Int Health Hum Rights. 2011;11(1):S10. https://doi.org/10.1186/1472-698X-11-S1-S10.
Actis Danna V, Bedwell C, Wakasiaka S, Lavender T. Utility of the three-delays model and its potential for supporting a solution-based approach to accessing intrapartum care in low- and middle-income countries. A qualitative evidence synthesis. Glob Health Action. 2020;13(1):1819052. https://doi.org/10.1080/16549716.16542020.11819052.
Waiswa P, Kallander K, Peterson S, Tomson G, Pariyo GW. Using the three delays model to understand why newborn babies die in eastern Uganda. Trop Med Int Health. 2010;15(8):964-972. https://doi.org/10.1111/j.1365-3156.2010.02557.x.
Mukuru M, Gorry J, Kiwanuka SN, Gibson L, Musoke D, Ssengooba F. Designed to fail? Revisiting Uganda's maternal health policies to understand policy design issues underpinning missed targets for reduction of maternal mortality ratio (MMR): 2000-2015. Int J Health Policy Manag. 2022;11(10):2124-2134. https://doi.org/10.34172/ijhpm.2021.127.
Mounier-Jack S, Griffiths UK, Closser S, Burchett H, Marchal B. Measuring the health systems impact of disease control programmes: a critical reflection on the WHO building blocks framework. BMC Public Health. 2014;14:278. https://doi.org/10.1186/1471-2458-1114-1278.
Sacks E, Morrow M, Story WT, et al. Beyond the building blocks: integrating community roles into health systems frameworks to achieve health for all. BMJ Glob Health. 2019;3(Suppl 3):e001384. https://doi.org/10.1136/bmjgh-002018-001384.
Mdoe P, Mills TA, Chasweka R, et al. Lay and healthcare providers’ experiences to inform future of respectful maternal and newborn care in Tanzania and Malawi: an appreciative inquiry. BMJ Open. 2021;11(9):e046248. https://doi.org/10.1136/bmjopen-042020-046248.
Bulthuis SE, Kok MC, Amon S, et al. How district health decision-making is shaped within decentralised contexts: a qualitative research in Malawi, Uganda and Ghana. Glob Public Health. 2021;16(1):120-135. https://doi.org/10.1080/17441692.17442020.11791213.
Swidler A, Watkins SC. 'Teach a man to fish': the doctrine of sustainability and its effects on three strata of Malawian society. World Dev. 2009;37(7):1182-1196. https://doi.org/10.1016/j.worlddev.2008.11.002.
Marten M. The “Sustainability Doctrine” in donor-driven maternal health programs in Tanzania (chapter 5). In: Wallace L, MacDonald M, Storeng K, eds. Anthropologies of global maternal and reproductive health: from policy spaces to sites of practice. Cham: Springer; 2022. https://www.ncbi.nlm.nih.gov/books/NBK584049/. Accessed 14 Apr 2023.
Ekman B, Pathmanathan I, Liljestrand J. Integrating health interventions for women, newborn babies, and children: a framework for action. Lancet. 2008;372(9642):990-1000. https://doi.org/10.1016/s0140-6736(1008)61408-61407.
Fridell M, Edwin S, von Schreeb J, Saulnier DD. Health system resilience: what are we talking about? A scoping review mapping characteristics and keywords. Int J Health Policy Manag. 2020;9(1):6-16. https://doi.org/10.15171/ijhpm.12019.15171.
Acknowledgements
The authors wish to thank the individuals who participated in the interviews and the research teams who assisted with data collection. We acknowledge the assistance received from the Uganda Ministry of Health, district health offices and the management of health facilities in the West Nile region.
Funding
This study was funded by UNICEF Uganda (Contracts 43329525 and 43341761). AM-B’s work was covered by Contract 43341761 between UNICEF Eastern and Southern African Region and the University of Pretoria, South Africa.
Author information
Authors and Affiliations
Contributions
SM, GL, PP, CM, FM, FG, TDH, AGA and A-MB conceptualised the study and contributed to its design. SM, XN and CNM collected the interview data. SM, XN, CNM and A-MB analysed the data. SM, XN and AM-B drafted the manuscript. XN, FM, FG, TDH, and AGA reviewed the manuscript and made further inputs. All the authors have critically reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Makerere University Higher Degrees Research and Ethics Committee (SPH-2021-162). Permission for the study was obtained from the respective district health offices and managers of health facilities. Written informed consent was obtained from all participants. The data collectors signed confidentiality agreements. All methods were performed in accordance with the relevant ethical and institutional guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Muhumuza, S., Nsabagasani, X., Muhangi, C.N. et al. Perspectives of stakeholders regarding the value of maternal and newborn health interventions and practices supported by UNICEF and other partners in the West Nile region of Uganda: a qualitative study. BMC Health Serv Res 23, 473 (2023). https://doi.org/10.1186/s12913-023-09480-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-09480-x