Abstract
Background
Febrile Neutropenia (FN) caused by bacteria in cancer patients is associated with poor prognosis. The aim of this study was to determine the prevalence of FN and associated factors among cancer patients on chemotherapy at Ocean Road Cancer Institute (ORCI), Tanzania.
Methods
A cross-sectional study was conducted from June to September 2019. Study participants were conveniently recruited. A desk review of participants medical records was performed. Standard microbiological procedures used to culture and identify the bacterial isolates from the positive blood cultures of participants that presented with FN. Kirby-Bauer disc diffusion was used to perform the antibiotics susceptibility testing. SPSS version 20.0 and MS Excel were used in data entry and analysis. Chi-Square was used as a measure of association between various factors and neutropenia. P-value less than 0.05 was considered statistically significant.
Results
A total 213 participants were enrolled. Of these 76.1% were female. Most of the participants came from the Coast region. Majority of participants presented with breast Cancer (36.2%) and GIT (20.2%). The prevalence of FN and bacteremia was 5.6% and 35.3% respectively. Staphylococcus Aureus (60%) and Coagulase-Negative Staphylococci (40%) were the main isolates. Of the 6 isolates tested most were resistant to Co-Trimoxazole 4/6 (66.7%) and Doxycycline 3/6 (50%). FN was positively associated with chemotherapy regimen (P = 0.0001), platelets count (P = 0.0001) and use of G-CSF (P = 0.0001).
Conclusion
The prevalence of FN among the cancer patients on chemotherapy in Tanzania is low but associated with drug-resistant bacteria.
Similar content being viewed by others
Background
Many cancer patients that undergo chemotherapy experience reduced immunity and manifests as low number of neutrophils clinically referred as febrile neutropenia (FN). This is due to the type and intensity of chemotherapy treatment received. Reduced immunity and other risk factors make these patients become more exposed to various infections that may present as chemotherapy-induced febrile neutropenia (CIN) [1].
In cancer patients on chemotherapy, FN is considered as a medical emergency as it is the leading cause of various blood stream infections (BSIs) that require a prompt treatment with the right antibiotics at the right time, which is guided by the current laboratory data. The overall mortality risk rates for cancer patients with FN are 15% times higher compared to cancer patients without FN [2].
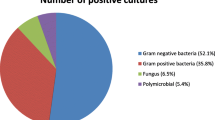
In the past (the 1960s and 1970s), gram-negative bacteria were the main etiology of FN. In the early 1980s, gram-positive organisms had become the most commonly isolated pathogens in most cases of FN patients [3]. Nowadays, there seems to be a change in patterns where the most common pathogens being multiple drug resistant (MDR) gram-negative and gram-positive bacteria. Of recent infections with gram-negative MDR bacterial pathogens, including extended spectrum β-lactamase (ESBL)-producing Enterobacteriaceae, are particularly prevalent among cancer patients worldwide [4, 5].
In Tanzania, BSIs causative agents in FN cancer patients are unknown and they are often treated empirically without support of current laboratory data with regards to the identity(ies) of the causative agent(s), nor their current antimicrobial susceptibility profiles. This practice puts at risks FN cancer patients to suffer adverse effects of inappropriate antibiotic therapies including death. We therefore embarked on a study to determine the prevalence of bacteremia and antibiotic resistance profile of bacteria in FN cancer patients at Ocean Road Cancer Institute (OCRI).
Methodology
The aim of this study was to determine the prevalence of FN and associated factors among cancer patients on chemotherapy at Ocean Road Cancer Institute (ORCI), Tanzania.
A cross-sectional hospital and laboratory-based study, was conducted from June to September 2019. All consenting adult cancer patients receiving chemotherapy at Ocean Road Cancer Institute (ORCI) were conveniently recruited. A desk review of the patient’s medical records was conducted to consider patients for inclusion/exclusion into the study and to obtain clinical data including their current clinical data mainly the type of the cancer diagnosed, the stage of the cancer, co-morbidities, type of the chemotherapy, chemotherapy dose being received per cycle, concurrent chemo-radiotherapy, number of the cycles received and the history of antibiotics received. The participants were then interviewed to gain socio-demographic information.
All study participants presenting with FN were drawn two sets of blood samples to detect any blood stream infections (BSI), particularly bacteria.
Microbiological analysis
A volume of 40 mL was drawn aseptically from participants presenting with FN. The BD BACTEC FX40 automated machine was used to culture blood samples. All positive isolates from Blood cultures were isolated using standard microbiological method and subjected to antibiotic susceptibility testing (AST) using the Kerby-Bauer Disk diffusion as par the CLSI 2018 guidelines criteria.
Data analysis and quality plan
Data were analyzed using SPSS version 20.0 Descriptive statistics were used present data. Univariate and multivariate regression analysis were used to establish the significance between dependent and independent variables with P-value less than 0.05 which was considered statistically significant.
Results
Socio-demographic characteristics
This study recruited 213 participants from different regions of Tanzania. The majority of them were females (76.1%) and 88.7% were married. The majority had a petty business (33.3%). For the performance status, the majority were of ECOG-1 & ECOG-2 (81.9%) (Table 1).
Clinical characteristics
Among our participants, the mean BP was 125/75 mmHg, mean HR was 85.7 bpm, mean RR was 20.4 rpm, the mean neutrophil count was 45.9% with the mean ANC of 2.4 × 103/µL, and mean Hb of 12.5 g/dL. The mean albumin was 39.8 g/L, mean ALT was 39.8U/L and mean AST was 30.2 U/L. The mean creatinine was 95.2%. 77.8% were over 40 years old (Table 2).
Prevalence of febrile neutropenia
Out of 213 participants, 14.6% had severe neutropenia, 23.5% had moderate neutropenia, while 9.4% had mild neutropenia. The neutropenia among our study participants was 32.9% with 5.6% presenting with FN (Table 3).
Prevalence of bacteremia
A total of 17 participants presenting with severe neutropenia were each drawn 2 sets of blood samples for culture. The bacteremia rate was 35.3% (6/17) which presented as gas production (5/6) or hemolysis (1/6). Microbiological procedures were performed to identify the isolates from positive culture. All the positive cultures were caused by Gram-Positive bacteria, mainly 66.7% (4/6) were Staphylococcus Aureus and 33.7% (2/6) were Coagulase Negative Staphylococci (CoNS).
Bacterial susceptibility testing
We found that 66.7% (4/6) of the isolated pathogens were resistant to SXT 1.25/23.75 µg, 50% (3/6) were resistant to Doxycycline 30 µg, 33.3% (2/6) were resistant to both Imipenem 10 µg and Vancomycin 30 µg and 16.7% (1/6) were resistant to Clindamycin 2 µg. All the isolates were sensitive to cefoxitin 30 µg, gentamycin 10 µg, ciprofloxacin 5 µg, penicillin 10 µg and meropenem 10 µg.
Association studies
In our study, we have found that various clinical factors were associated with developing neutropenia. By use of univariate and multivariate regression analysis, the following results have been obtained while looking for associations between various factors with neutropenia (Tables 4 and 5). The Performance status, low platelet count, cancer type and the use of G-CSF were found to be statistically significant factors to developing neutropenia.
Discussion
Bacteremia is a common blood stream infection among febrile neutropenic cancer patients on chemotherapy. If not treated urgently and adequately with an appropriate antibiotic, the worst adverse complication happens to the patient: death. In this study, we found that that females (76.1%), as shown in previous studies in Tanzania, have a higher cancer health seeking behavior than males [6]. The finding that Lake Zone have the least number of participants as compared to Dar es Salaam and coastal regions, could be attributed to that most patients from lake zone currently consult at their nearest hospital, Bugando Medical Center (BMC), which has recently started offering cancer services while others may travel miles from their homes to the Coast Region to seek shelters where they can stay while seeking the health care services at ORCI [7] (Fig. 1).
The breast cancer (36.2%) and Gastro-Intestinal tract (GIT) cancers (20.2%) were the most prevalent in our study. This may be due to that breast cancers and gynecological cancers are the most prevalent in Tanzania. Moreover, it could be from the fact that they are more readily detected as the Government has provided facilities and supports regular screening for these type of cancers, adding that women have more seeking behaviors for health care services than men [7] (Fig. 2).
The majority of participants had the performance status of ECOG-2. The main reasons for this could be that most of the patients consult health care services late while some of them seek first the traditional healer or stay home and come for consultation when the disease has already progressed [6]. The practice of delayed health seeking behavior of healthcare services could be a result of low awareness of cancer especially among women from rural areas of Tanzania [8, 9]. The other reasons could be that patients who come from faraway are afraid of the financial burden to the patients and their families as well as the stigma associated with cancer [10, 11].
The overall neutropenia rate was 38.1%, with 23.5% presenting as moderate neutropenia and 14.6% as severe neutropenia. This neutropenia rate is high, in our settings and factors like age, performance status, G-CSF as part of their treatment regimen, low platelet count and the type of cancer, mainly the hematological cancer are likely to induce neutropenia. The severe neutropenia rate was high in study participants below 20 years of age is in contrast to findings from other studies, which have linked severe neutropenia with older age [3, 4], but this could be linked with the hematological cancers that were the most prevalent in this young age group. These findings need to be further investigated, particularly if the neutropenia is associated with viral and parasitic pathogens for which we were not able to identify. However, our findings are similar to other studies in others countries that have linked development of severe neutropenia with hematological cancer, and older age [3, 4]. The rate of severe neutropenia was also high in people using alkylating agents, anthracyclines, imatinib and antimetabolites as part of their chemotherapy regimen (Fig. 3). These chemotherapeutic classes are known commonly to cause neutropenia [12]. However, participants using plant alkaloids had a low severe neutropenia rate in comparison to other chemotherapy agents. In 2009, Pettengell et al. [13] have found neutropenia rate in cancer patients to be 35% in a study done in Europe and this was similar to what we found in our study despite the difference in settings and facilities. Nonetheless, in the present study, neutropenia rate is much lower than those of studies conducted in Japan where the Chemotherapy-induced neutropenia was found to be 50.5% [14]. The practices, environmental factors and local settings maybe the main key contributors to findings despite the difference in settings. In Tanzania, there a common practice of administering the G-CSF to patients who present with moderate and severe neutropenia to boost their immunity and to keep the track in their treatment courses.
The prevalence of FN was 5.6% in the general population. It was low because many patients getting neutropenia are administered the G-CSF and this may delay the anticipated FN, which is beneficial to the patients attending chemotherapy ward at ORCI. The use of G-CSF may contribute to the prevention of FN among the cancer patients receiving chemotherapy and also enhancing to boost their immunity while achieving the desired therapeutic outcomes. However, our findings have found a likelihood contribution of the use of these G-CSF in developing neutropenia. They contribute to the accelerated myelosuppression which later leads to the lack of immunity to the patients, hence the increased susceptibility to blood stream infections. Comparing to other studies in other settings, there is a close similarity of results with those of Japan and USA [15]. Contrary, the FN rates were low in our settings compared to those in other countries around the world [16,17,18,19,20,21]. This may show the improved practices in Tanzania while managing the FN among this group of patients.
The prevalence of bacteremia was very high and mainly caused by gram-positive bacteria. The most common isolates were S. Aureus and were associated with resistance to commonly prescribed antibiotics. This is something alarming in Tanzania among the cancer patients on chemotherapy, as they may be prone to non-curable infections or expensive to treat as well. The isolates found in our results were similar to what found in other studies conducted around the globe which presented with alarming findings [4, 22, 23]. However, the bacteremia rates are higher than those of other studies conducted in other countries around the world where the prevalence of bacteremia reported in those countries was lower than that we found in our settings [23,24,25,26,27,28,29]. This variability in terms of prevalence may have been a result of our limited sample size for this study, and the study design but also the study settings available.
The bacterial isolates were found to be resistant to some strong antibiotics like vancomycin and meropenem, but also sensitive to Oxacillin (Cefoxitin). The staphylococci, mainly S. Aureus were the most prevalent among the participants and majority of them were MDR. In our study settings, attention is needed as the infections are caused by Gram-Positive bacteria that drug-resistant; and the empirical choice of the antibiotics should be based on the individual patient blood culture and AST data. Otherwise, the AST for any admitted FN is needed to accurately provide the right antibiotics. Studies conducted in Egypt and Iran had similar results to ours in that the majority of infections among the FN cancer patients on chemotherapy were caused by Gram-Positive Bacteria [28]. Staphylococcus Aureus (S.A) = 67% and Coagulase-Negative Staphylococci (CoNS) = 33% members of the ESKAPE group were the main isolates of bacteria of the study. Moghnieh et al. 2015 reported similar isolates in Lebanon and South Africa where studies by Louw et al. 2010 found that 42.7% and 49% of bacteremia in FN cancer patients were caused by gram-positive bacteria (GP), specifically methicillin-resistant CoNS [12, 16]. The finding that only gram-positive bacteria were associated with bacteremia in Tanzanian FN cancer patients is in contrast to findings from other studies that associated bacteremia in FN cancer patients with both gram-positive and gram negative bacteria [4, 30,31,32]. This variability may be due to limited number of repeated samples taken to perform blood cultures in this study. As studies have shown that repeating blood cultures may increase the success rate of detecting positive blood cultures [33,34,35,36].
In terms of antibiotics susceptibility patterns all isolates were 100% sensitive to cefoxitin, gentamycin, ciprofloxacin, penicillin and meropenem, and which is similar to what was found in studies done in other countries like USA, India, Iran, Ghana and Uganda [23, 37,38,39,40,41,42].
Nevertheless, our study found that the majority of isolates to have a high resistance rate to SXT and Doxycycline, with a moderate resistance to Imipenem, Vancomycin and Clindamycin. And similar findings have reported in Uganda which is a neighbor Country for Tanzania [37]; proving that the AMR problem is real in the Sub-Saharan Africa. The isolation of multi-drug resistance (MDR) Staphylococcus aureus is a warning signal to our clinical settings, as this finding suggests that the antimicrobial resistance (AMR) may be increasingly being evidenced among cancer patients. The emergence of MDR pathogens causing FN in cancer patients in Tanzania indicates treating FN cancer may be a challenge in future due to wide spread AMR as it has been shown in other countries [22, 43, 44]. Moreover, the finding that resistance to Vancomycin was 50% of isolated CoNS and in 25% of isolates S. Aureus may be an indicator that antimicrobial stewardship and rational use of antimicrobials needs to be strengthened in Tanzania [14, 17,18,19,20, 45]. The current practice of clinicians prescribing without support of microbiology laboratory AST data needs to be curbed through continuing professional development and advocating for antimicrobial stewardship in clinical settings. However, enforcing antimicrobial stewardship in LMICs like Tanzania, maybe a challenge due to limited resources for health. To effectively use the available health care resources in Tanzania, Policy-makers have to improve the existing policies, guidelines and practices for antimicrobial stewardship. This will ensure reduced mortality, morbidity and cost associated with treating FN in cancer patients infected with MDR pathogens and continued to use Ciprofloxacin for prophylaxis [21, 46, 47].
Several factors were associated with developing neutropenia. With the univariate and multivariate regression analysis, we found that the type of cancer (Hematological Vs Non-hematological), low platelet count, use of G-CSF and poor performance status of the patient can be the predictive factors for likelihood of developing neutropenia and eventually FN. There was poor performance status [15] and the same finding have been reported in Canada by Younus [48]; however, there was no association of neutropenia with combined therapy in our study as it has been reported in Japan and United Kingdom (UK) [15, 48] as was reported in the UK [49]. Differences in patient populations may have contributed to these differences. However, we were unable to do the correlation analysis between neutropenia and bacteremia as well as between bacteremia and type of tumor because bacteremia status was found in a few patients (6/17). We hope that other studies will address this correlation in the future.
Study limitations
There was a risk of missing the real candidates who presented with FN because some of them were quickly admitted and administered antibiotics as well as the G-CSF. Those candidates would be found at the time when it is not possible to draw the blood for culture because it could lead to false results. We were unable to identify the fungal infections as well.
Conclusion
The prevalence of FN among the cancer patients on chemotherapy is relatively low at ORCI compared to other countries. The use of G-CSF, low platelet count and poor performance status have been found to contribute to developing neutropenia among this group of patients. However, bacteremia rates are relatively higher and associated with drug resistant pathogens. Clinicians at OCRI should consider the previous regimen of the patient as well as the performance status to predict the likelihood of cancer patients developing neutropenia, that may eventually lead to developing FN. There should be a regular test for blood culture and AST for effective patient management.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AIDS:
-
Acquired Immuno-Deficiency Syndrome
- ALT:
-
Alanine Aminotransferase
- AMR:
-
Antimicrobial resistance
- ANC:
-
Absolute Neutrophil Count
- ASP:
-
Antimicrobial Stewardship Program
- AST:
-
Antibiotics susceptibility testing
- BMC:
-
Bugando Medical Center
- BMI:
-
Body Mass Index
- BSIs:
-
Blood Stream Infections
- CNS:
-
Central Nervous System
- CoNS:
-
Coagulase-negative Staphylococci
- COPD:
-
Chronic Obstructive Pulmonary Disease
- CPL:
-
Central Pathology Laboratory
- CSF:
-
Colony stimulating factor
- DBP:
-
Diastolic Blood Pressure
- ECOG:
-
Eastern Cooperative Oncology Group
- ESKAPE:
-
Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter spp.
- ESBL:
-
Extended Spectrum β-lactamase producing Enterobacteriaceae
- FAO:
-
Food and Agriculture Organization
- FBP:
-
Full blood picture
- FN:
-
Febrile Neutropenia
- GARP:
-
Global Antimicrobial resistance partnership
- G-CSF:
-
Granulocyte-colony stimulating factor
- GIT:
-
Gastro-Intestinal Tact
- GN:
-
Gram Negative
- GP:
-
Gram Positive
- GU:
-
Genito-Urinary
- HIV:
-
Human Immune Virus
- H&N:
-
Head and Neck
- HR:
-
Heart rate
- HTN:
-
Hypertension
- IDSA:
-
Infectious disease society of America
- IV:
-
Intra-Venous
- LMICs:
-
Low- and Middle-Income Countries
- MAb:
-
Monoclonal antibody
- MBC:
-
Metastatic Breast Cancer
- MCRC:
-
Metastatic Colon/Rectal Cancer
- MLC:
-
Metastatic Lung Cancer
- MNH:
-
Muhimbili National Hospital
- MOC:
-
Metastatic Ovarian Cancer
- MPC:
-
Metastatic Prostate Cancer
- MRSA:
-
Methicillin Resistant Staphylococcal Aureus
- MUHAS:
-
Muhimbili University of Health and Allied Sciences
- ORCI:
-
Ocean Road Cancer Institute
- PMN:
-
Poly-Morph Nuclear cells
- RR:
-
Respiratory rate
- SBP:
-
Systolic Blood Pressure
- SD:
-
Standard Deviation
- ST:
-
Soft Tissue
- SXT:
-
Sulfamethoxazole/Trimethoprim
- UICC:
-
Union for International Cancer Control
- WHO:
-
World Health Organization
References
Rasmy A, Amal A FS and SW. Febrile Neutropenia in Cancer Patient: Epidemiology, Microbiology, Pathophysiology and Management. J Cancer Prev Curr Res. 2016;5(3). http://medcraveonline.com/JCPCR/JCPCR-05-00165.php
Lyman GH, Michels SL, Reynolds MW, Barron R, Tomic KS, Yu J. Risk of mortality in patients with cancer who experience febrile neutropenia. Cancer. 2010;116(23):5555–63. https://doi.org/10.1002/cncr.25332.
Mikulska GG. Bloodstream infections in neutropenic cancer patients: a practical update. Virulence. 2016;7(3):280–97.
Tohamy ST, Aboshanab KM, El-Mahallawy HA, El-Ansary MR, Afifi SS. Prevalence of multidrug-resistant Gram-negative pathogens isolated from febrile neutropenic cancer patients with bloodstream infections in Egypt and new synergistic antibiotic combinations. Infect Drug Resist. 2018;11:791–803.
Carmona-Bayonas A, Jiménez-Fonseca P, Echaburu JV, Antonio M, Font C, Biosca M, et al. Prediction of serious complications in patients with seemingly stable febrile neutropenia: Validation of the clinical index of stable febrile neutropenia in a prospective cohort of patients from the FINITE study. J Clin Oncol. 2015;33(5):465–71. https://doi.org/10.1200/JCO.2014.57.2347.
Kazaura MR, Kombe D, Yuma S, Mtiro H, Mlawa G. Health seeking behavior among cancer patients attending Ocean Road Cancer Institute, Tanzania. East Afr J Public Health. 2007;4(1):19–22.
Burson AM, Soliman AS, Ngoma TA, Mwaiselage J, Ogweyo P, Eissa MS, et al. Clinical and epidemiologic profile of breast cancer in Tanzania. Breast Dis. 2010;31(1):33–41.
Moshi FV, Vandervort EB, Kibusi SM. Cervical cancer awareness among women in Tanzania: an analysis of data from the 2011–12 Tanzania HIV and Malaria indicators survey. Int J Chronic Dis. 2018;2018:1–7.
Ng’ida FD, Kotoroi GL, Mwangi R, Mabelele MM, Kitau J, Mahande MJ. Knowledge and practices on breast cancer detection and associated challenges among women aged 35 years and above in Tanzania: a case in Morogoro rural district. Breast Cancer Targets Ther. 2019;11:191–7.
Runge AS, Bernstein ME, Lucas AN, Tewari KS. Cervical cancer in Tanzania: A systematic review of current challenges in six domains. Vol. 29, Gynecologic Oncology Reports. Elsevier; 2019. p. 40–7.
Vrinten C, Gallagher A, Waller J, Marlow LAV. Cancer stigma and cancer screening attendance: a population based survey in England. BMC Cancer. 2019;19(1):1–10.
Louw V, van der Westhuizen J, Rautenbach W, van der Berg E, Wamelink M, Joubert G. The antibiotic susceptibility of bacteria isolated from blood cultures during episodes of neutropenic fever in patients with acute myeloid leukaemia. S Afr J Epidemiol Infect. 2010;25(2):9–11.
Pettengell R, Bosly A, Szucs TD, Jackisch C, Leonard R, Paridaens R, et al. Chemotherapy-induced neutropenia and febrile neutropenia in patients with gynecologic malignancy. Anticancer Drugs. 2009;4(4):1054–60. https://doi.org/10.1086/383048.
Maertens J, Georgala A, Rolston K, Paesmans M, Rapoport B, Ferrant A, et al. Bacteraemia in febrile neutropenic cancer patients. Int J Antimicrob Agents. 2007;30:51–9.
Hashiguchi Y, Kasai M, Fukuda T, Ichimura T, Yasui T, Sumi T. Chemotherapy-induced neutropenia and febrile neutropenia in patients with gynecologic malignancy. Anticancer Drugs. 2015;26(10):1054–60.
Moghnieh R, Estaitieh N, Mugharbil A, Jisr T, Abdallah DI, Ziade F, et al. Third generation cephalosporin resistant Enterobacteriaceae and multidrug resistant gram-negative bacteria causing bacteremia in febrile neutropenia adult cancer patients in Lebanon, broad spectrum antibiotics use as a major risk factor, and correlation w. Front Cell Infect Microbiol. 2015;5:11. https://doi.org/10.3389/fcimb.2015.00011.
Lalami Y, Klastersky J. Impact of chemotherapy-induced neutropenia (CIN) and febrile neutropenia (FN) on cancer treatment outcomes: An overview about well-established and recently emerging clinical data. Vol. 120, Critical Reviews in Oncology/Hematology. 2017. p. 163–79. https://linkinghub.elsevier.com/retrieve/pii/S104084281730313X
Lehrnbecher T, Robinson P, Fisher B, Alexander S, Ammann RA, Beauchemin M, et al. Guideline for the management of fever and neutropenia in children with cancer and hematopoietic stem-cell transplantation recipients: 2017 update. J Clin Oncol. 2017;35(18):2082–94. https://doi.org/10.1200/JCO.2016.71.7017.
Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T, et al. Guidelines for the use of antimicrobial agents in neutropenic patients with cancer. IDSA Guidel. 2002;34:203–8.
Dellit TH, Owens RC, Mcgowan JE, Gerding DN, Weinstein RA, Burke JP, et al. Infectious diseases society of American and the society for healthcare epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44:159–77.
Song S, Vuai MS, Zhong M. The role of bacteria in cancer therapy - Enemies in the past, but allies at present. Vol. 13, Infectious Agents and Cancer. BioMed Central; 2018. p. 9. https://doi.org/10.1186/s13027-018-0180-y
Bodro M, Gudiol C, Garcia-Vidal C, Tubau F, Contra A, Boix L, et al. Epidemiology, antibiotic therapy and outcomes of bacteremia caused by drug-resistant ESKAPE pathogens in cancer patients. Support Care Cancer. 2014;22(3):603–10. https://doi.org/10.1007/s00520-013-2012-3.
Irfan S, Idrees F, Mehraj V, Habib F, Adil S, Hasan R. Emergence of Carbapenem resistant Gram negative and vancomycin resistant Gram positive organisms in bacteremic isolates of febrile neutropenic patients: a descriptive study. BMC Infect Dis. 2008;8(1):80. https://doi.org/10.1186/1471-2334-8-80.
Kim HS, Lee SY, Kim JW, Choi YJ, Park IH, Lee KS, et al. Incidence and predictors of febrile neutropenia among early-stage breast cancer patients receiving anthracycline-based chemotherapy in Korea. Oncol. 2016;91(5):274–82.
Lakhe NA, Sylla K, Mbaye KD, Ndiaye R, Marie V, Cisse P, et al. Bacteremia: Profile and antibiotic resistance at the infectious and tropical diseases clinic in Fann Hospital, Dakar. Senegal J Infect Dis Ther. 2018;6(1):1–8.
Ibrahim TM, Pang C. Bacteremia pattern in febrile neutropenia among adults cancer patients receiving chemotherapy in an Australia Regional Hospital. Univers J Public Heal. 2017;5(4):172–5.
Moremi N, Claus H, Mshana SE. Antimicrobial resistance pattern: A report of microbiological cultures at a tertiary hospital in Tanzania. Vol. 16, BMC Infectious Diseases. 2016. p. 756. https://doi.org/10.1186/s12879-016-2082-1
Meidani M, Bagheri A, Khorvash F. A population-based study of bacterial spectrum in febrile neutropenic patients. Jundishapur J Microbiol. 2013;6(2):150–6.
Onken A, Said AK, Jørstad M, Jenum PA, Blomberg B. Prevalence and antimicrobial resistance of microbes causing bloodstream infections in unguja, Zanzibar. PLoS ONE. 2015;10(12):e0145632. https://doi.org/10.1371/journal.pone.0145632.
Dias P, Lakshika S, Lenaduwe A. Risk factors for Bacteraemia in Cancer Patients Contributors: 1. Sonali Lenaduwe 1, BSc (Hons) in Medical Laboratory Sciences, Demonstrator, Faculty of Allied Health Sciences, General Sir John Kotelawala Defence University, Sri Lanka. 2. Achini Sandunika. bioRxiv. 2018;386193. https://doi.org/10.1101/386193v3.abstract
Herrera PCMDJPCMLGIPVCJPVPMLARFP and F. Multidrug-resistant Gram-negative Bacteremia in Cancer Patients: Development of a Clinical Score for Risk Assessment. 2017;4(Suppl 1):2017.
Herrera F, Laborde A, Rossi IR, Guerrini G, Jordan R, Valledor A, et al. Prognostic factors for 7-day and 30-day mortality during gram-negative bacteremia episodes in cancer and hematopoietic stem cell transplant patients. Int J Infect Dis. 2018;73:3.
Mushtaq A, Bredell BX, Soubani AO. Repeating blood cultures after initial bacteremia: when and how often? Cleve Clin J Med. 2019;86(2):89–92.
Tabriz MS, Riederer K, Baran J, Khatib R. Repeating blood cultures during hospital stay: practice pattern at a teaching hospital and a proposal for guidelines. Clin Microbiol Infect. 2004;10(7):624–7.
Lambregts MMC, Warreman EB, Bernards AT, Veelken H, von dem Borne PA, Dekkers OM, et al. Distribution and clinical determinants of time-to-positivity of blood cultures in patients with neutropenia. Eur J Haematol. 2018;100(2):206–14. https://doi.org/10.1111/ejh.13001.
Wiggers JB, Xiong W, Daneman N. Sending repeat cultures: Is there a role in the management of bacteremic episodes? (SCRIBE study). BMC Infect Dis. 2016;16(1):1–10.
Lubwama M, Phipps W, Najjuka CF, Kajumbula H, Ddungu H, Kambugu JB, et al. Bacteremia in febrile cancer patients in Uganda. BMC Res Notes. 2019;12(1):464. https://doi.org/10.1186/s13104-019-4520-9.
Ramphal R. Changes in the etiology of bacteremia in febrile neutropenic patients and the susceptibilities of the currently isolated pathogens. Clin Infect Dis. 2004;39(s1):S25-31. https://doi.org/10.1086/383048.
Rolston KVI. Bacterial infection in neutropenic cancer patients: an overview. Iran J Clin Infect Dis. 2009;4(2):115–22.
Prabahar K, Dinesh S, Barla S. Antibiotics utilization pattern in pediatrics. Asian J Pharm. 2017;2017(1):230–4.
Rather IA, Kim BC, Bajpai VK, Park YH. Self-medication and antibiotic resistance: Crisis, current challenges, and prevention. Vol. 24, Saudi Journal of Biological Sciences. 2017. p. 808–12.
Obeng-Nkrumah N, Labi A-K, Acquah ME, Donkor ES. Bloodstream infections in patients with malignancies: implications for antibiotic treatment in a Ghanaian tertiary setting. BMC Res Notes. 2015;8(1):742.
El-mahallawy HA, Shawky S, El-wakil M. Bacteremia due to ESKAPE pathogens: an emerging problem in cancer patients. J Egypt Natl Canc Inst. 2016;28(3):157–62. https://doi.org/10.1016/j.jnci.2016.05.002.
Santajit S, Indrawattana N. Mechanisms of Antimicrobial Resistance in ESKAPE Pathogens. Vol. 2016, BioMed Research International. 2016.
Klastersky J. Management of fever in neutropenic patients with different risks of complications. Clin Infect Dis. 2004;39(s1):S32–7. https://doi.org/10.1086/383050.
Rattinger GB, Mullins CD, Zuckerman IH, Onukwugha E, Walker LD, Gundlapalli A, et al. A Sustainable Strategy to Prevent Misuse of Antibiotics for Acute Respiratory Infections. PLoS ONE. 2012;7(12):e51147.
Escrihuela-Vidal F, Laporte J, Albasanz-Puig A, Gudiol C. Update on the management of febrile neutropenia in hematologic patients. Vol. 32, Revista espanola de quimioterapia : publicacion oficial de la Sociedad Espanola de Quimioterapia. NLM (Medline); 2019. p. 55–8.
Younus J, Vandenberg T, Jawaid M, Jawaid MA. Febrile neutropenia rates with adjuvant docetaxel and cyclophosphamide chemotherapy in early breast cancer: discrepancy between published reports and community practice-an updated analysis. Curr Oncol. 2012;19(6):332–4.
Netelenbos T, Massey E, de Wreede LC, Harding K, Hamblin A, Sekhar M, et al. The burden of invasive infections in neutropenic patients: incidence, outcomes, and use of granulocyte transfusions. Transfusion. 2019;59(1):160–8. https://doi.org/10.1111/trf.14994.
Acknowledgements
I am thankful to Muhimbili University of Health and Allied Sciences, Ocean Road Cancer Institute and Muhimbili National Hospital for the administrative assistance given during this study. Grateful to all technical personnel who gave their assistance during data collection.
Funding
No funds have been received for this study. It was part of the academic completion.
Author information
Authors and Affiliations
Contributions
LCS: Drafted and wrote the manuscript, collected data, analyzed data and presented the results with discussion and conclusion. He wrote the approved final manuscript as well. DM: Supervised the whole study process, reviewed, edited and approved the final manuscript. OM: Co-supervised the study and reviewed the final manuscript. NJD: Co-supervised the study and reviewed the final manuscript. RR: Statistically analyzed the collected data and presented the findings.
Corresponding author
Ethics declarations
Ethical considerations
Ethical approval was obtained from the Institutional Review Board (IRB) of Muhimbili University of Health and Allied Sciences in Dar Es Salaam, Tanzania; and the permission to start collecting data was obtained from Ocean Road Cancer Institute’s leadership. Informed consent was obtained from study participants and participation was voluntary. Confidentiality was insured by identifying the data collection form by serial coded serial numbers, and no name or other participant’s personal identifiers were recorded.
Competing interests
The authors declare that they have no competing interests in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Safari, L.C., Mloka, D., Minzi, O. et al. Prevalence of blood stream infections and associated factors among febrile neutropenic cancer patients on chemotherapy at Ocean Road Cancer Institute, Tanzania. Infect Agents Cancer 18, 52 (2023). https://doi.org/10.1186/s13027-023-00533-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13027-023-00533-8