Abstract
Purpose
Infection due to the six ESKAPE pathogens has recently been identified as a serious emerging problem. However, there is still a lack of information on bacteremia caused by these organisms in cancer patients. We aimed to assess the epidemiology, antibiotic therapy and outcomes of bacteremia due to drug-resistant ESKAPE pathogens (rESKAPE) in patients with cancer.
Methods
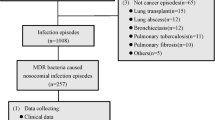
All episodes of bacteremia prospectively documented in hospitalized adults with cancer from 2006 to 2011 were analyzed.
Results
Of 1,148 episodes of bacteremia, 392 (34 %) were caused by ESKAPE pathogens. Fifty-four episodes (4.7 %) were due to rESKAPE strains (vancomycin-resistant Enterococcus faecium 0, methicillin-resistant Staphylococcus aureus (MRSA) 13, extended-spectrum beta-lactamase (ESLB)-producing Klebsiella pneumoniae 7, carbapenem-resistant Acinetobacter baumannii 4, carbapenem- and quinolone-resistant Pseudomonas aeruginosa 18 and derepression chromosomic ß-lactam and ESBL-producing Enterobacter species 12. Risk factors independently associated with rESKAPE bacteremia were comorbidities, prior antibiotic therapy, urinary catheter and urinary tract source. Inappropriate empirical antibiotic therapy was more frequent in patients with rESKAPE bacteremia than in the other cases (55.6 % vs. 21.5 %, p < 0.001). Persistence of bacteremia (25 % vs. 9.7 %), septic metastasis (8 % vs. 4 %) and early case-fatality rate (23 % vs. 11 %) were more frequent in patients with rESKAPE bacteremia than in patients with other etiologies (p < 0.05).
Conclusions
Bacteremia due to rESKAPE pathogens in cancer patients occurs mainly among those with comorbidities who have received prior antibiotic therapy and have a urinary tract source. These patients often receive inappropriate empirical antibiotic therapy and have a poor outcome.

Similar content being viewed by others
References
Kang CI, Kim SH, Park WB, Lee KD, Kim HB, Kim EC, Oh MD, Choe KW (2005) Bloodstream infections caused by antibiotic-resistant gram-negative bacilli: risk factors for mortality and impact of inappropriate initial antimicrobial therapy on outcome. Antimicrob Agents Chemother 49(2):760–766
Schwaber MJ, Carmeli Y (2007) Mortality and delay in effective therapy associated with extended-spectrum beta-lactamase production in Enterobacteriaceae bacteraemia: a systematic review and meta-analysis. J Antimicrob Chemother 60(5):913–920
Giske CG, Monnet DL, Cars O, Carmeli Y (2008) Clinical and economic impact of common multidrug-resistant Gram-negative bacilli. Antimicrob Agents Chemother 52(3):813–821
Paterson DL (2008) Impact of antibiotic resistance in gram-negative bacilli on empirical and definitive antibiotic therapy. Clin Infect Dis 47(Suppl 1):S14–S20
Spanik S, Krupova I, Trupl J, Kunova A, Novotny J, Mateicka F, Pichnova E, Sulcova M, Sabo A, Jurga L, Krcmery JVV (1999) Bacteremia due to multiresistant Gram-negative bacilli in neutropenic cancer patients: a case-controlled study. J Infect Chemother 5(3):180–184
Ramphal R (2004) Changes in the etiology of bacteremia in febrile neutropenic patients and the susceptibilities of the currently isolated pathogens. Clin Infect Dis 39(Suppl 1):S25–S31
Feld R (2008) Bloodstream infections in cancer patients with febrile neutropenia. Int J Antimicrob Agents 32(Suppl 1):S30–S33
Klastersky J, Ameye L, Maertens J, Georgala A, Muanza F, Aoun M, Ferrant A, Rapoport B, Rolston K, Paesmans M (2007) Bacteraemia in febrile neutropenic cancer patients. Int J Antimicrob Agents 30(Suppl 1):S51–S59
Gonzalez-Barca E, Fernandez-Sevilla A, Carratala J, Salar A, Peris J, Granena A, Gudiol F (1999) Prognostic factors influencing mortality in cancer patients with neutropenia and bacteremia. Eur J Clin Microbiol Infect Dis 18(8):539–544
Rice LB (2008) Federal funding for the study of antimicrobial resistance in nosocomial pathogens: no ESKAPE. J Infect Dis 197(8):1079–1081
Boucher HW, Talbot GH, Bradley JS, Edwards JE, Gilbert D, Rice LB, Scheld M, Spellberg B, Bartlett J (2009) Bad bugs, no drugs: no ESKAPE! An update from the infectious diseases society of America. Clin Infect Dis 48(1):1–12
Sandiumenge A, Lisboa T, Gomez F, Hernandez P, Canadell L, Rello J (2011) Effect of antibiotic diversity on ventilator-associated pneumonia caused by ESKAPE Organisms. Chest 140(3):643–651
Bow EJ (2013) There should be no ESKAPE for febrile neutropenic cancer patients: the dearth of effective antibacterial drugs threatens anticancer efficacy. J Antimicrob Chemother 68(3):492–495
Harris AD, Karchmer TB, Carmeli Y, Samore MH (2001) Methodological principles of case–control studies that analyzed risk factors for antibiotic resistance: a systematic review. Clin Infect Dis 32(7):1055–1061
Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, Lamm W, Clark C, MacFarquhar J, Walton AL, Reller LB, Sexton DJ (2002) Health care-associated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 137(10):791–797
Klastersky J, Paesmans M, Rubenstein EB, Boyer M, Elting L, Feld R, Gallagher J, Herrstedt J, Rapoport B, Rolston K, Talcott J (2000) The multinational association for supportive care in cancer risk index: a multinational scoring system for identifying low-risk febrile neutropenic cancer patients. J Clin Oncol 18(16):3038–3051
Clinical and Laboratory Sandards Institute (formery NCCLS). Performance standards for antimicrobial susceptibility testing: twenty-second informational supplement. CLSI document M100-S22 (ISBN 1-56238-785-5)
Lee K, Lim YS, Yong D, Yum JH, Chong Y (2003) Evaluation of the Hodge test and the imipenem-EDTA double-disk synergy test for differentiating metallo-beta-lactamase-producing isolates of Pseudomonas spp. and Acinetobacter spp. J Clin Microbiol 41(10):4623–4629
Gudiol C, Tubau F, Calatayud L, Garcia-Vidal C, Cisnal M, Sanchez-Ortega I, Duarte R, Calvo M, Carratala J (2011) Bacteraemia due to multidrug-resistant Gram-negative bacilli in cancer patients: risk factors, antibiotic therapy and outcomes. J Antimicrob Chemother 66(3):657–663
Irfan S, Idrees F, Mehraj V, Habib F, Adil S, Hasan R (2008) Emergence of carbapenem resistant Gram negative and vancomycin resistant Gram positive organisms in bacteremic isolates of febrile neutropenic patients: a descriptive study. BMC Infect Dis 8:80
Ohmagari N, Hanna H, Graviss L, Hackett B, Perego C, Gonzalez V, Dvorak T, Hogan H, Hachem R, Rolston K, Raad I (2005) Risk factors for infections with multidrug-resistant Pseudomonas aeruginosa in patients with cancer. Cancer 104(1):205–212
Garnica M, Maiolino A, Nucci M (2009) Factors associated with bacteremia due to multidrug-resistant Gram-negative bacilli in hematopoietic stem cell transplant recipients. Braz J Med Biol Res 42(3):289–293
Trecarichi EM, Tumbarello M, Spanu T, Caira M, Fianchi L, Chiusolo P, Fadda G, Leone G, Cauda R, Pagano L (2009) Incidence and clinical impact of extended-spectrum-beta-lactamase (ESBL) production and fluoroquinolone resistance in bloodstream infections caused by Escherichia coli in patients with hematological malignancies. J Infect 58(4):299–307
Oliveira AL, de Souza M, Carvalho-Dias VM, Ruiz MA, Silla L, Tanaka PY, Simoes BP, Trabasso P, Seber A, Lotfi CJ, Zanichelli MA, Araujo VR, Godoy C, Maiolino A, Urakawa P, Cunha CA, de Souza CA, Pasquini R, Nucci M (2007) Epidemiology of bacteremia and factors associated with multi-drug-resistant gram-negative bacteremia in hematopoietic stem cell transplant recipients. Bone Marrow Transplant 39(12):775–781
Cordonnier C, Herbrecht R, Buzyn A, Leverger G, Leclercq R, Nitenberg G, Bastuji-Garin S (2005) Risk factors for Gram-negative bacterial infections in febrile neutropenia. Haematologica 90(8):1102–1109
Gudiol C, Bodro M, Simonetti A, Tubau F, Gonzalez-Barca E, Cisnal M, Domingo-Domenech E, Jimenez L, Carratala J (2013) Changing aetiology, clinical features, antimicrobial resistance, and outcomes of bloodstream infection in neutropenic cancer patients. Clin Microbiol Infect 19(5):474–479. doi:10.1111/j.1469-0691.2012.03879.x
Gudiol C, Calatayud L, Garcia-Vidal C, Lora-Tamayo J, Cisnal M, Duarte R, Arnan M, Marin M, Carratala J, Gudiol F (2010) Bacteraemia due to extended-spectrum beta-lactamase-producing Escherichia coli (ESBL-EC) in cancer patients: clinical features, risk factors, molecular epidemiology and outcome. J Antimicrob Chemother 65(2):333–341
Wang SS, Lee NY, Hsueh PR, Huang WH, Tsui KC, Lee HC, Wu CJ, Chang CM, Huang CC, Huang CF, Ko WC (2011) Clinical manifestations and prognostic factors in cancer patients with bacteremia due to extended-spectrum beta-lactamase-producing Escherichia coli or Klebsiella pneumoniae. J Microbiol Immunol Infect 44(4):282–288
Kang CI, Chung DR, Ko KS, Peck KR, Song JH (2012) Risk factors for infection and treatment outcome of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae bacteremia in patients with hematologic malignancy. Ann Hematol 91(1):115–121
Rangaraj G, Granwehr BP, Jiang Y, Hachem R, Raad I (2010) Perils of quinolone exposure in cancer patients: breakthrough bacteremia with multidrug-resistant organisms. Cancer 116(4):967–973
LeBlanc L, Pepin J, Toulouse K, Ouellette MF, Coulombe MA, Corriveau MP, Alary ME (2006) Fluoroquinolones and risk for methicillin-resistant Staphylococcus aureus, Canada. Emerg Infect Dis 12(9):1398–1405
Acknowledgment
This study was supported by Ministerio de Economía y Competitividad, Instituto de Salud Carlos III (ISCIII) co-financed by the European Regional Development Fund (ERDF) “A Way to Achieve Europe,” the Spanish Network for Research in Infectious Diseases (REIPI RD06/0008). Dr. Bodro is the recipient of a research grant from the Bellvitge Biomedical Research Institute (IDIBELL). Dr. Garcia-Vidal is the recipient of a Juan de la Cierva research grant from the ISCIII.
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Bodro, M., Gudiol, C., Garcia-Vidal, C. et al. Epidemiology, antibiotic therapy and outcomes of bacteremia caused by drug-resistant ESKAPE pathogens in cancer patients. Support Care Cancer 22, 603–610 (2014). https://doi.org/10.1007/s00520-013-2012-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-2012-3