Abstract
Background
Tenosynovial giant cell tumor (TGCT) is a rare, locally aggressive neoplasm arising from the synovium of joints, bursae, and tendon sheaths affecting small and large joints. It represents a wide spectrum ranging from minimally symptomatic to massively debilitating. Most findings to date are mainly from small, retrospective case series, and thus the morbidity and actual impact of this rare disease remain to be elucidated. This study prospectively explores the management of TGCT in tertiary sarcoma centers.
Methods
The TGCT Observational Platform Project registry was a multinational, multicenter, prospective observational study involving 12 tertiary sarcoma centers in 7 European countries, and 2 US sites. This study enrolled for 2 years all consecutive ≥ 18 years old patients, with histologically diagnosed primary or recurrent cases of diffuse-type TGCT. Patient demographic and clinical characteristics were collected at baseline and every 6 months for 24 months. Quality of life questionnaires (PROMIS-PF and EQ-5D) were also administered at the same time-points. Here we report baseline patient characteristics.
Results
166 patients were enrolled between November 2016 and March 2019. Baseline characteristics were: mean age 44 years (mean age at disease onset: 39 years), 139/166 (83.7%) had prior treatment, 71/166 patients (42.8%) had ≥ 1 recurrence after treatment of their primary tumor, 76/136 (55.9%) visited a medical specialist ≥ 5 times, 66/116 (56.9%) missed work in the 24 months prior to baseline, and 17/166 (11.6%) changed employment status or retired prematurely due to disease burden. Prior treatment consisted of surgery (i.e., arthroscopic, open synovectomy) (128/166; 77.1%) and systemic treatments (52/166; 31.3%) with imatinib (19/52; 36.5%) or pexidartinib (27/52; 51.9%). Treatment strategies at baseline visits consisted mainly of watchful waiting (81/166; 48.8%), surgery (41/166; 24.7%), or targeted systemic therapy (37/166; 22.3%). Patients indicated for treatment reported more impairment compared to patients indicated for watchful waiting: worst stiffness NRS 5.16/3.44, worst pain NRS 6.13/5.03, PROMIS-PF 39.48/43.85, and EQ-5D VAS 66.54/71.85.
Conclusion
This study confirms that diffuse-type TGCT can highly impact quality of life. A prospective observational registry in rare disease is feasible and can be a tool to collect curated-population reflective data in orphan diseases.
Name of registry: Tenosynovial Giant Cell Tumors (TGCT) Observational Platform Project (TOPP).
Trial registration number: NCT02948088.
Date of registration: 10 October 2016.
URL of Trial registry record: https://clinicaltrials.gov/ct2/show/NCT02948088?term=NCT02948088&draw=2.
Similar content being viewed by others
Introduction
Tenosynovial giant cell tumor (TGCT) is a rare, locally aggressive mesenchymal neoplasm arising from the synovium of joints, bursae, and tendon sheaths and affects both small and large joints [1]. Two main subtypes of TGCT are defined based on clinical and radiological characteristics: localized- and diffuse-type TGCT (L-TGCT and dt-TGCT). The malignant version of TGCT is extremely rare [2]. From the molecular point of view, both subtypes usually share the presence of a fusion involving the colony stimulating factor (CSF) gene, which drives tumor growth [3, 4]. Although both subtypes share a common pathophysiology, they represent a wide spectrum of clinical entities, making TGCT behavior complex and hard to predict [5]. Clinical disease spectrum ranges from mildly symptomatic to extremely debilitating, where patients present with symptoms like pain, stiffness, swelling, and limitation in range of motion [6]. Further characterization of disease severity has been made to identify cases as mild localized, severe localized, moderate diffuse, or severe diffuse [7]. Uniform magnetic resonance (MR) descriptions are of utmost significance for clinical and research purposes. The classification of clear MR criteria is challenging, due to the rarity of the tumor and small number of heterogeneous cases, variety of joints involved, different disease severity as well as several treatment modalities. To date, MR imaging (MRI) has shown to be the best distinguishing method for evaluation of TGCT. The proposed TGCT severity classification informs physicians and patients on disease extent and risk for recurrence after surgical treatment. Definition of the most severe subgroup attributes to a universal identification of eligible patients for systemic therapy or trials for novel agents [7]. Also, ultrasound has been used effectively in the evaluation of soft-tissue masses, particularly involving the knee joint. Soft-tissue sarcomas appear as a complex mass with increased vascularity [8]. Diffusion-weighted echo-planar MRI is potentially helpful in differentiating malignant soft tissue tumors from benign masses as well as in grading malignancy [9]. Muscle sarcomas are indicated to present a broad range of apparent diffusion coefficient (ADC), dependent on diffusion-weighted imaging (DWI) which is crucial regarding tumor composition, and distinguishing between malignant and benign lesions [10].
Although less prevalent, dt-TGCT is an aggressive multi-lobulated lesion located intra- and/or extra-articular, affecting various joints in the body (mainly the knee) and having a detrimental effect on quality of life (QoL) [11,12,13,14]. Incidence rate of dt-TGCT is estimated at 5 per million person-years [11]. Due to non-specific symptoms and the rarity of this disease, a proper diagnosis can sometimes take many years, which in turn may severely delay optimal treatment and care for these patients, resulting in them facing a higher risk of excessive, inadequate, or under treatment [11, 15]. Once diagnosed, treatment options include mostly surgical intervention. However, recently tyrosine kinase inhibitors (TKIs) that target the CSF1 receptor (CSF1R) have been used for treatment in cases where surgery is not an option [3, 16,17,18,19,20,21]
As the predominant epidemiologic understanding of dt-TGCT to date comes mainly from small, retrospective studies that traditionally focused on oncological outcomes, questions to elaborate the true morbidity and actual impact on QoL, both the disease and its various treatment options remains to be elucidated [1, 22]. Given this context, there is a need for a better understanding of the natural history of this tumor to understand the burden of dt-TGCT from a patient perspective and of the treatment landscape beyond a single institution. Additionally, there is the need to explore the current management of TGCT, particularly of the diffuse type (including functional details measured pre- and post-treatment) to describe the spectrum of indications, challenges, and the actual impact on patient QoL and ability to work.
To this end, the first multinational, multicenter, prospective, non-interventional, observational disease registry study, named TGCT Observational Platform Project (TOPP), was launched in November 2016, involving hospitals and tertiary sarcoma centers from Europe (EU) and the United States (US). All patients included in the study were to be followed up with for a minimum of 2 years. Herein, we report on patient demographics and clinical characteristics at the time when patients were entered into the registry (baseline). This includes main disease characteristics, treatment patterns, and outcomes of the dt-TGCT patient population from varying geographical regions to better understand the breadth of the patient journey. In addition, we aimed at identifying and describing factors influencing treatment decision making, in the absence of consensus treatment guidelines.
Methods
Study design and participants
This global multicenter, prospective sponsored study included all consecutive patients from 12 tertiary sarcoma centers in 7 EU countries from 2016 to 2018. Two sites in the US enrolled patients from 2017 to 2019. Patients were enrolled during a 2-year period with prospective follow-up over 24 months. Participating sites were selected based of their expertise in treatment of TGCT.
Eligible patients were 18 years or older, with a primary or recurrent dt-TGCT. TGCT had to be histologically confirmed and assessed as diffuse-type based on MRI or clinical presentation if this was missing. Dt-TGCT is often characterized by a multi-nodular tumor on MRI. The institutional review board or ethics board provided approval in each center, and written informed consent was obtained from each patient who participated in this study.
Primary diagnosis was defined as patients who were awaiting treatment or were treated and showed no evidence of local progression at baseline. Recurrent disease was defined as tumor recurrence after complete resection or progression of residual tumor. Therapy-naïve patients received no therapy prior to baseline and were consequently admitted as primary diagnosed patients. Disease severity was in line with the TGCT severity classification by Mastboom et al., with severe dt-TGCT classified as intra- and extra-articular involvement with involvement of one or more ligaments or muscular/tendinous tissue observed on MRI [7].
Patient demographics, complete TGCT-related history, and current status, including radiologic assessments and health resources used in the past 24 months, were collected at baseline. Baseline visits occurred at the outpatient clinic of either the department of orthopedic surgery or the oncology department. Baseline data on TGCT-related patient-reported outcomes (PRO) for pain, stiffness, swelling, and limitations in range of motion were collected and followed every year thereafter through electronic data capture. The patient-reported outcome measurements (PROMs) were administered at baseline consisting of the mean brief pain inventory (BPI), mean worst pain and stiffness numerical rating scale (NRS), the Patient-Reported Outcome Measurement Information System Physical Functioning® (PROMIS-PF), and the EuroQoL 5D (EQ-5D) (Additonal file 1). Admission status at baseline was categorized into patients with a primary diagnosis or recurrent disease.
Statistical analysis
Continuous data were described using either means and standard deviations (SD) or medians and interquartile ranges (IQR). Categorical variables were summarized as number of observations and percentages (%) of the observations in each category. Percentages do not include the missing category and are calculated over the number of subjects with available (non-missing) data. The whole analysis was descriptive only. Statistical analysis was performed using the Statistical Analysis System (SAS©) Version 9.4 under Microsoft Windows Operating System. Because dt-TGCT is an orphan disease, no formal sample size consideration has been performed, as recruitment of patients within the scheduled 2-year period was expected to be difficult.
Results
Between November 2016 and March 2019, 166 patients from the EU and US were enrolled in the TOPP registry. Description of baseline patient demographics and clinical characteristics are provided in Table 1. The mean age at diagnosis was 39.0 years (range, 14.4–75.6; SD ± 14.42) and median time from diagnosis until TOPP entry point was 29.7 months (IQR, 9.5–80.0). TGCT had a female predilection (n = 102; 61.4%), and the knee joint was predominantly affected (n = 112; 68.5%). Other involved locations were the ankle (n = 19; 11.4%), the hip (n = 12; 7.2%), the shoulder (n = 8; 4.8%), the foot (n = 5, 3.0%), the elbow (n = 3, 1.8%), the hand (n = 3, 1.8%), and the temporomandibular joint (n = 1; 0.6%). Ninety-five patients (57.2%) were primary diagnosed cases, and 71 patients (42.8%) had at least one recurrence prior to baseline, occurring after any treatment of their primary tumor.
Diagnostic pathway
A median of 16.9 months (IQR, 4.0–44.0) elapsed from onset of symptoms until diagnosis of TGCT (Table 2). Most commonly, MRIs requested closest to baseline of TOPP were for postoperative follow-up (n = 56; 40.0%). Of all MRIs, dt-TGCT was generally located both intra- and extra-articular (n = 90/147; 61.2%) with involvement of ligaments (n = 88/134; 65.7%), and tendons and muscles (n = 99/141; 70.2%), classifying half of the patients (n = 83) with severe dt-TGCT at baseline (Table 2). If assessable, severe dt-TGCT was observed in the knee, ankle, hip, and other locations in 51.5% (n = 51/99), 55.6% (n = 5/9), 58.8% (n = 10/17) and 77.2% (n = 17/22) of the cases, respectively.
Sixty-nine patients (41.6%) were classified severe dt-TGCT even after treatment, exemplifying the continued severity of the disease. Histological confirmation was primarily obtained after excisional biopsy (n = 32; 41.6%), however several non-excisional biopsy techniques were also performed in other patients (e.g., core needle biopsy, arthroscopic biopsy, or fine needle aspiration). In 13%, TGCT diagnosis was based on surgical histology from samples obtained during procedure undertaken for suspicion of a malignancy (Table 2).
Treatments received prior to baseline of TOPP
Of 166 patients who entered the TOPP study, 139 (83.7%) had already been exposed to a TGCT-related treatment, whereas only 27/166 patients (16.3%) were treatment-naïve (Table 1). Ninety-five patients (57.2%) were primary diagnosed cases, and 71 patients (42.8%) had at least one recurrence prior to baseline, occurring after any treatment of their primary tumor (Table 3).
Of 57 patients treated with surgery at the time of initial diagnosis, 30 (31.6%) had been treated arthroscopically. At the time of relapse, 71 (100%) patients had a re-operation, and in this case the surgical approach was open synovectomy in 49 (69.0%) and arthroscopic in 33 (46.5%). Five patients (3.9%) had received a (tumor) prosthesis secondary to TGCT in four cases due to a recurrent tumor. Fifty-two patients (31.3%) received systemic treatment; in 39.4% (28/71) this was indicated in recurrent cases and was still ongoing in 34.6% (18/52) at baseline. Thirty-two of 52 cases (62.7%) were indicated for systemic therapies because of locally advanced TGCT, 9.8% (5/52) as neo-adjuvant, 7.8% (4/52) for maintenance, and 7.8% (4/52) for palliative therapy. Eleven patients (21.2%) received systemic therapies as first treatment for TGCT. TKIs imatinib (off label) or pexidartinib (in research setting) were most frequently administered as latest treatment prior to baseline (46/47; 97.9%) (Table 3). Radiation therapy, comprising external beam radiotherapy and radiosynoviorthesis with 90Yttrium, was administered in 15/166 (9%) and mostly performed as adjuvant therapy after surgery in refractory cases (10/15; 66.7%) (Table 3). Eighty-eight (53%) of all cases had received prior and concomitant therapies for TGCT-related symptoms.
Treatment strategies at time of TOPP study entry
Treatment strategies at baseline visits of TOPP consisted of watchful waiting (n = 81/166; 48.8%), surgery only (n = 41/166; 24.7%), or targeted systemic therapy only (n = 37/166; 22.3%). A multimodality approach was administered in 7/166 (4.2%) of cases, comprising different therapy combinations (e.g., surgery, targeted systemic therapies, and/or radiation therapy) (Additonal file 1).
A conservative monitoring approach at baseline was primarily decided on for patients who received only surgery before baseline (n = 47/81; 58.0%) (Table 4). Most MRIs were conducted as regular postoperative follow-up (n = 43/75; 57.3%), and this group comprised the lowest percentage of severe cases (n = 38/81; 46.9%). Non-invasive interventions were common in this group; 26.2% of the patients received rehabilitation (n = 17), and patients in need of physical therapy (n = 23, 28.4%) had a median of 18 (range, 4.0–200.0) sessions.
Patients indicated for surgery in this population were most recently diagnosed with TGCT. A median of 6.7 (IQR, 1.2–59.8) months elapsed from TGCT diagnosis until baseline, and 65.9% (n = 27) had a primary diagnosis, of which 16/41 (39.0%) were therapy-naïve at baseline. Furthermore, MRIs closest to baseline were primarily indicated to diagnose TGCT (n = 23; 57.5%) (Table 4).
Twenty-one (56.8%) of the patients indicated for targeted systemic therapies at TOPP baseline already had received multimodality treatment before baseline. None of these patients were therapy-naïve at baseline, and just 7 (18.9%) patients had only surgery before. MRIs were predominantly obtained due to progressive complaints (n = 13; 37.1%), and in this patient group the highest percentage of recurrent (n = 18; 48.6%) and severe dt-TGCT (n = 21; 56.8%) was observed. These patients visited medical specialists at a median of 12 times (range, 2.0–65.0) in the 24 months prior to baseline. Patients indicated for systemic therapies had a median age of 48.0 years (range 20.0–73.0). In addition, analgesics were most used by these patients (n = 9; 23.3%) and mean worst stiffness and pain NRS scores of 5.3 (SD ± 2.55) and 5.8 (SD ± 1.97), respectively, were reported. Physical functioning was limited with a median PROMIS-PF score of 39.98, and the lowest QoL scores were reported with an EQ-5D index score of 0.74 and visual analog scale (VAS) score of 70.0. At baseline, 33 patients (89.2%) had a current systemic therapy, of which 18 (54.5%) were started before. All current systemic therapies consisted of TKIs imatinib (n = 14; 42.4%) and pexidartinib (n = 19; 57.6%).
Only 11 patients did not report complaints due to TGCT at baseline, resulting in 93.4% of patients with at least one complaint. Patients indicated for treatment reported TGCT-related symptoms (e.g., pain, stiffness, swelling, and limited range of motion) more frequently compared to those with a wait-and-see policy (Table 4), except for swelling, which was least experienced by patients treated with systemic therapies (51.4%), and 68.3% indicated for surgery at baseline suffered from 3 or more TGCT-related symptoms. Both patient groups indicated for surgery and systemic therapies reported higher pain severity (4.25) and interference scores (3.00) compared to patients indicated for watchful waiting (2.25; 1.57). In addition, both treatment groups reported lower PROMIS-PF scores (39.54 and 39.98, respectively), EQ-5D index scores (0.80 and 0.74, respectively) and EQ-5D VAS scores (69.0 and 70.0, respectively).
Health economics related to the TOPP cohort
Thirty-three patients (23.9%) required at least 5 visits from disease onset, before reaching a diagnosis of TGCT. In addition, 76 patients (55.9%) consulted a medical specialist 5 times or more in the 24 months prior to baseline. Thirty-six patients (25.5%) had more than 10 physical therapy sessions in the 24 months prior to baseline. Hospitalization and rehabilitation were required in 91.0% (151/166) and 18.6% (26/140), respectively, with a median of 3.0 (range, 1.0–184.0) and 15.0 (range, 1.0–120.0) days, respectively. Fifteen (9.9%) patients were hospitalized 5 or more times. Sixty-six patients (56.9%) missed work due to their TGCT in the 2 years prior to baseline, with a median of 25.0 days (range, 1.0–75.0). More importantly, of 146 patients who were employed, 17 (11.6%) were forced to change their employment status or even retire prematurely due to disease burden. Domestic help was necessary in 26 cases (16.0%).
Discussion
TOPP represents the largest prospective, international, multicenter disease registry for dt-TGCT, being able to include 166 patients in slightly more than 2 years and shows that conducting collaborative observational studies for a rare tumor is feasible. Current literature is largely focused on the oncological outcomes of this often-chronic disease [16, 18, 20, 23,24,25,26,27]. Baseline data derived from this registry help to describe a preliminary understanding of the dt-TGCT patient journey and treatment decisions around disease onset and diagnosis of dt-TGCT patients. We believe that such study design can guide collection of high-quality data for other orphan diseases.
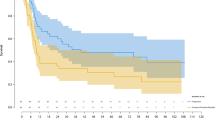
The present study confirmed that TGCT has its onset in a relatively young, educated, and working patient population with a female predilection [11, 12]. Time between onset of symptoms until diagnosis averaged more than a year, and in this time interval several medical specialists were frequently visited. An under- or overestimation could be introduced due to a recall bias. Nonspecific clinical signs and symptoms in TGCT patients often mimicked other mono-articular pathologies, resulting in frequent consultation of various healthcare professionals (e.g., physical therapists, rheumatologists, and sports doctors) and lag time in diagnosis (Figs. 1, 2) [28]. MRI was the non-invasive gold standard to diagnose TGCT type and distinguish between the localized and diffuse subtypes [29, 30]. In addition, this modality was frequently utilized for postoperative surveillance for recurrence, evaluation of worsening complaints (e.g., distinguishing degenerative arthritic symptoms or internal derangement of the joint), or pre-surgical planning (Table 2). Definitive diagnosis was predominantly obtained by histological confirmation through different forms of biopsies [31, 32]. In 10 cases, TGCT was coincidentally diagnosed after surgery for an initial suspicion of cancer. Disease mimicking and unfamiliarity could possibly introduce such misdiagnoses, with potential major consequences for a patient.
A typical timeline of dt-TGCT in a single TOPP patient. The disease had its onset in an 18-year-old patient who was forced to stop exercising and in need of physical therapy due to dt-TGCT-related complaints. Several recurrences occurred despite multimodality treatment, leading to secondary gonarthrosis at the age of 25
This figure represents the general patient journey of patients with dt-TGCT. Non-specific symptoms and disease unawareness results in several visits to different healthcare practitioners and unnecessary or excessive treatment in first and second line before referral to an orthopedic or sarcoma oncologist
The primary form of care for TGCT is complete surgical removal of abnormal tissue, performed arthroscopically, open or combined, often requiring multiple incisions to access the disease thoroughly. However, there is a high risk for recurrence, especially in dt-TGCT, due to invasive growth both in and outside the joint [15, 19, 24, 33]. Synovectomies are generally relatively invasive, with a high recurrence rate and repetitive surgery causing significant impairment [24]. Multimodality treatments (e.g., external beam radiotherapy and radiosynoviorthesis) have been performed in an attempt to reduce the recurrence rate in dt-TGCT, leading to varied reported outcomes [25,26,27]. In addition to surgery, several CSF1R inhibitors including TKIs showed promising results in tumor volume decrease and reduction of debilitating symptoms [16, 18, 20, 21, 34]. Of the TKIs, pexidartinib is an FDA-approved systemic therapy, recently added as a category 1 recommendation for the treatment of adult patients with symptomatic TGCT/pigmented villonodular synovitis (PVNS) associated with severe morbidity or functional limitations that is not amenable to improvement with surgery.
Our results confirm that surgery was the mainstay of treatment (75%), which is consistent with other studies [15, 24, 33]. Furthermore, all patients with recurrent dt-TGCT disease had surgery, often combined with other treatment modalities (Fig. 3). Synovectomies were mostly performed open. To date, literature reported conflicting results regarding different surgical techniques, not favoring one over another [23, 35, 36]. However, we hypothesize that open surgery may allow for better overview of tumor, located intra- and extra-articular, with extension to surrounding tissues, possibly resulting in more complete removal of disease burden. Almost a third of the patients received systemic therapies, mainly TKIs such as pexidartinib (in research setting) and imatinib (off label)—a relatively high percentage, possibly due to a selection bias since sarcoma centers participating in TOPP were also involved in clinical studies on TGCT. Use of TKIs was mostly found indicated in locally advanced refractory cases, illustrating this modality being considered a last resort for patients who are not amenable for surgery (Fig. 2). An individual well-thought-out treatment decision made by a multidisciplinary team of medical specialists is therefore needed regarding both surgical and systemic treatment options with such rates of response, local recurrence, complications, and side effects.
This flowchart gives a schematic overview of the treatment types patients received prior to TOPP, according to tumor status: primary diagnosis or recurrent disease. In addition, the cohort is stratified into 2 patient groups according to treatment plan at baseline: watchful waiting and indicated treatment at baseline. Possibly important factors in treatment decision making are shown per subgroup
Given the lack of understanding of this disease, the incidence of TGCT may be underestimated as disease awareness increases and diagnostic tools improve [13]. Diagnostic delay results in multiple visits to different health care practitioners (e.g., general practitioner, physiotherapist, sports medicine doctor, rheumatologist) and unnecessary or excessive treatments (e.g., use of painkillers or diagnostic arthroscopies) in the first and second line before referral to an orthopedic or sarcoma oncologist [15, 37]. If treated inadequately, aggressive dt-TGCT can become a chronic illness affecting an otherwise young, healthy patient population, leading to a significantly decreased QoL and concurrent high social costs (e.g., sick leave, medical costs) (Fig. 1) [13, 38].
Current literature lacks treatment guidelines and does not present relevant clinical findings that support clinical decision making. Creating insight on such important factors can be of great value in optimizing treatment strategies. Different treatment strategies were selected at baseline of TOPP, predominantly watchful waiting, surgery, or systemic therapies. The number and type of follow-up visits were not controlled, as they were influenced by patient and physician concerns. Systemic therapies were predominantly indicated for older patients with recurrent and severe dt-TGCT despite their having received multimodality treatment before. This patient group reported the highest decrease in QoL and experienced a major limitation in physical functioning. The use of systemic therapies in the setting of relapsed dt-TGCT might be justified in an attempt to avoid chronic disability [16, 18, 20]. Local experience and availability of TKIs during TOPP possibly influenced the choice for treatment in the tertiary reference centers, with a preference for surgery followed by TKI. Primary or refractory cases are predominantly treated at doctors’ preference. Improved disease-specific patient education, multidisciplinary discussion, and shared decision making would enable better treatment selection for each patient.
At baseline of TOPP, patients with a wait-and-see policy reported fewer TGCT-related symptoms, less frequent use of painkillers, and higher QoL, advocating that the lack of symptoms may be the driving force for choosing a more conservative approach. We therefore considered PRO to be important influencers in shared treatment decision making, which is consistent with the increasing role of patient-based care in chronic diseases, especially in a benign disease such as TGCT [39].
The aim of TOPP is to provide insight on disease burden including healthcare utilization, treatment landscape, and current management of TGCT in the tertiary sarcoma center setting. In 2 years prior to baseline, medical professionals were often consulted, a fourth of the patients needed multiple physical therapy sessions, and medical specialists were frequently visited by more than half of the patients (Table 5). Hospitalization and, to a lesser degree, rehabilitation were common with varying duration. Like the study by Burton et al., this suggests that TGCT causes a high health economic burden. In a like manner, this suggests that dt-TGCT increases social costs [38]. In the population studied, illness often caused work absence, intermittently more than 5 weeks of work in total in 2 years’ time (Table 5). Additionally, several patients were forced to change their employment status from full-time to part-time, some had to become unemployed, while some even had to enter early retirement, all due to dt-TGCT. The demand for domestic help illustrates the impairment in activities of daily living. Worsening of dt-TGCT over time will potentially increase the interference of the disease with work and the healthcare utilization. However, since this study only reports data captured at baseline, we are not able to analyze such a change over a period of time.
While designed to report on epidemiologic data on dt-TGCT, the TOPP study is exposed to potential selection bias, (i.e., underreferral of less severe cases to tertiary sarcoma centers). In addition, patients referred to such sarcoma centers are generally more impaired by dt-TGCT, and the lack of patients treated in non-specialized centers could give an overestimation of the disease burden and healthcare utilization. To avoid selection of patients and thus violation of the “real-life” principle, no explicit non-eligibility criteria were defined. In addition, as data about medical history that were not considered essential or were difficult to remember were collected at baseline, an underreporting of data might have occurred.
The present findings from baseline and 2 years prior to study entry provide new insights into patient management before arriving in a tertiary sarcoma center. They strongly suggest that dt-TGCT has its onset in a relatively young and working population but whose dt-TGCT diagnosis is often delayed, most likely due to disease unfamiliarity or misdiagnosis. Evaluation of patient groups stratified by treatment received prior to study entry and at baseline in particular surgery and/or systemic therapy illustrate significant continued burden of disease. This is compounded by health economics and PRO data. Choice of treatment in the study population was mostly based on admission status, clinical experience, and PRO. Synovectomies were the mainstay of treatment, whereas TKIs were mostly restricted to severe and refractory cases, while a wait-and-see policy was applied for patients with less severe symptomatology. Within the context of these findings, developing multidisciplinary guidelines for the treatment of primary and refractory cases is of the utmost importance. Final results from the completed study will build upon these preliminary yet foundational understandings of the typical dt-TGCT patient journey profile in this rare disease.
Availability of data and materials
De-identified individual participant data (IPD) and applicable supporting clinical trial documents may be available upon request at https://vivli.org/ourmember/daiichi-sankyo/.
References
Ottaviani S, Ayral X, Dougados M, Gossec L. Pigmented villonodular synovitis: a retrospective single-center study of 122 cases and review of the literature. Semin Arthritis Rheum. 2011;40(6):539–46.
de St. Aubain Somerhausen N, van de Rijn M. Tenosynovial giant cell tumour. In: Board WCoTE, editor. 5th World Health Organization classification of tumours of soft tissue and bone. 5th ed. Lyon: IARC Press; 2020. p. 133–6.
Brahmi M, Vinceneux A, Cassier PA. Current systemic treatment options for tenosynovial giant cell tumor/pigmented villonodular synovitis: targeting the CSF1/CSF1R axis. Curr Treat Opt Oncol. 2016;17(2):10.
Brahmi M, Alberti L, Tirode F, et al. Complete response to CSF1R inhibitor in a translocation variant of teno-synovial giant cell tumor without genomic alteration of the CSF1 gene. Ann Oncol. 2018;29(6):1488–9.
Mastboom MJL, Hoek DM, Bovee J, van de Sande MAJ, Szuhai K. Does CSF1 overexpression or rearrangement influence biological behaviour in tenosynovial giant cell tumours of the knee? Histopathology. 2019;74(2):332–40.
Gelhorn HL, Tong S, McQuarrie K, et al. Patient-reported symptoms of tenosynovial giant cell tumors. Clin Ther. 2016;38(4):778–93.
Mastboom MJL, Verspoor FGM, Hanff DF, et al. Severity classification of tenosynovial giant cell tumours on MR imaging. Surg Oncol. 2018;27(3):544–50.
Razek AA, Fouda NS, Elmetwaley N, Elbogdady E. Sonography of the knee joint(). J Ultrasound. 2009;12(2):53–60.
Razek A, Nada N, Ghaniem M, Elkhamary S. Assessment of soft tissue tumours of the extremities with diffusion echoplanar MR imaging. Radiol Med. 2012;117(1):96–101.
Surov A, Nagata S, Razek AA, Tirumani SH, Wienke A, Kahn T. Comparison of ADC values in different malignancies of the skeletal musculature: a multicentric analysis. Skelet Radiol. 2015;44(7):995–1000.
Mastboom MJL, Verspoor FGM, Verschoor AJ, et al. Higher incidence rates than previously known in tenosynovial giant cell tumors. Acta Orthop. 2017;88(6):688–94.
Ehrenstein V, Andersen SL, Qazi I, et al. Tenosynovial giant cell tumor: incidence, prevalence, patient characteristics, and recurrence. A registry-based cohort study in Denmark. J Rheumatol. 2017;44(10):1476–83.
van der Heijden L, Mastboom MJ, Dijkstra PD, van de Sande MA. Functional outcome and quality of life after the surgical treatment for diffuse-type giant-cell tumour around the knee: a retrospective analysis of 30 patients. Bone Joint J. 2014;96-b(8):1111–8.
Gelhorn HL, Ye X, Speck RM, et al. The measurement of physical functioning among patients with Tenosynovial Giant Cell Tumor (TGCT) using the Patient-Reported Outcomes Measurement Information System (PROMIS). J Patient Rep Outcomes. 2019;3(1):6.
van der Heijden L, Gibbons CL, Hassan AB, et al. A multidisciplinary approach to giant cell tumors of tendon sheath and synovium—a critical appraisal of literature and treatment proposal. J Surg Oncol. 2013;107(4):433–45.
Verspoor FGM, Mastboom MJL, Hannink G, et al. Long-term efficacy of imatinib mesylate in patients with advanced Tenosynovial Giant Cell Tumor. Sci Rep. 2019;9(1):14551.
Tap WD, Wainberg ZA, Anthony SP, et al. Structure-guided blockade of CSF1R kinase in tenosynovial giant-cell tumor. N Engl J Med. 2015;373(5):428–37.
Tap WD, Gelderblom H, Palmerini E, et al. Pexidartinib versus placebo for advanced tenosynovial giant cell tumour (ENLIVEN): a randomised phase 3 trial. Lancet. 2019;394(10197):478–87.
Staals EL, Ferrari S, Donati DM, Palmerini E. Diffuse-type tenosynovial giant cell tumour: current treatment concepts and future perspectives. Eur J Cancer. 2016;63:34–40.
Gelderblom H, Cropet C, Chevreau C, et al. Nilotinib in locally advanced pigmented villonodular synovitis: a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2018;19(5):639–48.
Cassier PA, Italiano A, Gomez-Roca CA, et al. CSF1R inhibition with emactuzumab in locally advanced diffuse-type tenosynovial giant cell tumours of the soft tissue: a dose-escalation and dose-expansion phase 1 study. Lancet Oncol. 2015;16(8):949–56.
van der Heijden L, Gibbons CL, Dijkstra PD, et al. The management of diffuse-type giant cell tumour (pigmented villonodular synovitis) and giant cell tumour of tendon sheath (nodular tenosynovitis). J Bone Joint Surg Br. 2012;94(7):882–8.
Noailles T, Brulefert K, Briand S, et al. Giant cell tumor of tendon sheath: Open surgery or arthroscopic synovectomy? A systematic review of the literature. Orthop Traumatol Surg Res. 2017;103(5):809–14.
Mastboom MJL, Palmerini E, Verspoor FGM, et al. Surgical outcomes of patients with diffuse-type tenosynovial giant-cell tumours: an international, retrospective, cohort study. Lancet Oncol. 2019;20(6):877–86.
Mollon B, Lee A, Busse JW, et al. The effect of surgical synovectomy and radiotherapy on the rate of recurrence of pigmented villonodular synovitis of the knee: an individual patient meta-analysis. Bone Joint J. 2015;97-b(4):550–7.
Gortzak Y, Vitenberg M, Frenkel Rutenberg T, et al. Inconclusive benefit of adjuvant (90)Yttrium hydroxyapatite to radiosynovectomy for diffuse-type tenosynovial giant-cell tumour of the knee. Bone Joint J. 2018;100-b(7):984–8.
Durr HR, Capellen CF, Klein A, et al. The effects of radiosynoviorthesis in pigmented villonodular synovitis of the knee. Arch Orthop Trauma Surg. 2019;139(5):623–7.
Byers PD, Cotton RE, Deacon OW, et al. The diagnosis and treatment of pigmented villonodular synovitis. J Bone Joint Surg Br. 1968;50(2):290–305.
Hughes TH, Sartoris DJ, Schweitzer ME, Resnick DL. Pigmented villonodular synovitis: MRI characteristics. Skelet Radiol. 1995;24(1):7–12.
Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis: radiologic–pathologic correlation. Radiographics. 2008;28(5):1493–518.
Somerhausen NS, Fletcher CD. Diffuse-type giant cell tumor: clinicopathologic and immunohistochemical analysis of 50 cases with extraarticular disease. Am J Surg Pathol. 2000;24(4):479–92.
West RB, Rubin BP, Miller MA, et al. A landscape effect in tenosynovial giant-cell tumor from activation of CSF1 expression by a translocation in a minority of tumor cells. Proc Natl Acad Sci U S A. 2006;103(3):690–5.
Palmerini E, Staals EL, Maki RG, et al. Tenosynovial giant cell tumour/pigmented villonodular synovitis: outcome of 294 patients before the era of kinase inhibitors. Eur J Cancer. 2015;51(2):210–7.
Cannarile MA, Weisser M, Jacob W, Jegg AM, Ries CH, Ruttinger D. Colony-stimulating factor 1 receptor (CSF1R) inhibitors in cancer therapy. J Immunother Cancer. 2017;5(1):53.
Stephan SR, Shallop B, Lackman R, Kim TW, Mulcahey MK. Pigmented villonodular synovitis: a comprehensive review and proposed treatment algorithm. JBJS Rev. 2016;4(7):01874474-201607000-00005. https://doi.org/10.2106/JBJS.RVW.15.00086.
Colman MW, Ye J, Weiss KR, Goodman MA, McGough RL 3rd. Does combined open and arthroscopic synovectomy for diffuse PVNS of the knee improve recurrence rates? Clin Orthop Relat Res. 2013;471(3):883–90.
Xie GP, Jiang N, Liang CX, et al. Pigmented villonodular synovitis: a retrospective multicenter study of 237 cases. PLoS ONE. 2015;10(3):e0121451.
Burton TM, Ye X, Parker ED, Bancroft T, Healey J. Burden of illness associated with tenosynovial giant cell tumors. Clin Ther. 2018;40(4):593-602.e1.
Dubertret L. Patient-based medicine and psoriasis. Acta Dermatovenerol Croat. 2010;18(4):311–4.
Acknowledgements
The authors would like to acknowledge Antonio Lopez Pousa, Medical Oncology Department, Hospital Sant Pau, Barcelona, Spain for his contributions to the study. Medical writing support and editorial assistance in the development of the article were provided by Phillip Giannopoulos, Ph.D. of SciStrategy Communications, and funded by Daiichi Sankyo, Inc.
The authors wish to thank the TOPP Study Group, including Bart Schreuder, Department of Orthopaedic Oncology, Radboud University, Nijmegen, Netherlands; Andreas Leithner, Department of Orthopaedics and Trauma, Medical University of Graz, Graz, Austria; Javier Martin-Broto, Seville Institute of Biomedicine, Virgen del Rocio University Hospital, Sevilla, Spain; Francois Gouin, Orthopedic and Trauma Surgery, CHU de Nantes, Nantes, France; and Thomas Cosker, Nuffield Orthopaedic Centre, Oxford, United Kingdom, for their patient inclusion and data collection.
Funding
Sponsored by Daiichi Sankyo, Co., Ltd; ClinicalTrials.gov Number NCT02948088. The Department of Orthopaedics of the Leiden University Medical Center receives research funding from Daiichi Sankyo. All research funding for Memorial Sloan Kettering is supported in part by a grant from the National Institutes of Health/National Cancer Institute (#P30 CA008748). Employees of the funder participated in the study design and conduct and were involved in collection, analysis, and interpretation of the data.
Author information
Authors and Affiliations
Consortia
Contributions
GS, NMB, JHH, PL, EP, ELS, and MAJvdS were responsible for the conception and design of the study. NMB, JHH, EP, ELS, the TOPP Study Group, and MAJvdS collected the data. EMF assembled the data and performed the statistical analysis. GS, NMB, JHH, PL, EMF, EP, ELS, and MAJvdS interpreted the data. GS drafted the manuscript, after which NMB, JHH, EP, SB, HG, ELS, JLB, and MAJvdS revised the manuscript with important intellectual content. GS, NMB, JHH, EP, SB, HG, ELS, JLB, EMF, XY, PL, and MAJvdS all reviewed and approved the final version of the manuscript before submission. The corresponding authors take responsibility for the integrity of work, from inception to published article. The TOPP Study Group consists of contributors taking part in the steering committee and/or responsible for patient inclusion and data collection. The TOPP Study Group members all have reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This non-interventional study was conducted according to the Declaration of Helsinki (October 2013) and Good Clinical Practice guidelines of the International Conference on Harmonisation. This study is registered with ClinicalTrials.gov (Number NCT02948088), and the institutional review board at each participating center approved the study.
Consent for publication
All patients provided written consent.
Competing interests
NMB reports consulting fees from Daiichi Sankyo, Zimmer Biomet, and Onkos Surgical. GS reports research funding to his institution (LUMC) from Daiichi Sankyo. JHH reports consulting fees from Daiichi Sankyo. EP served on an advisory board for Amgen, Daiichi Sankyo, Lilly, Eusa Pharma, Deciphera; research funding from Bristol-Myers Squibb, Pfizer, PharmaMar, and travel support from Lilly, PharmaMar, and Takeda. SB reports advisory board fees for Deciphera, Blueprint Medicines, ADC Therapeutics, Nanobiotix, Bayer, Lilly, Novartis, Exelixis, Daiichi Sankyo, and Roche; CME honoraria from PharmaMar, Lilly, and Novartis; research funding from Incyte, Blueprint Medicines, and Novartis; and travel support from PharmaMar. HG reports research funding to his institution (LUMC) from Daiichi Sankyo. ELS has served on a steering committee for Daiichi Sankyo Europe GmbH and an advisory board for Daiichi Sankyo Inc. JLB declares no competing interests. EMF, XY, and PL are employees for Daiichi Sankyo. MAJvdS reports research funding from Daiichi Sankyo. The TOPP Study Group reports the following conflicts of interests: BS reports limited research administrative compensation from Daiichi Sankyo; AL reports institution education grants from Johnson and Johnson, Alphamed, and Globus; JMB reports research funding from Lilly, PharmaMar, Eisai, Novartis, GSK, LIXTE, Karyopharm, Celgene, Pfizer, BMS, Blueprint, Deciphera, Nektar, Forma, Amgen, and Daiichi Sankyo; FG reports consulting fees from Amgen, stock ownership in Atlanthera, and honoraria from Deciphera; ALP and TC declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. TOPP registry description, breakdown by country, participating centers, and patient-reported outcome measurements.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bernthal, N.M., Spierenburg, G., Healey, J.H. et al. The diffuse-type tenosynovial giant cell tumor (dt-TGCT) patient journey: a prospective multicenter study. Orphanet J Rare Dis 16, 191 (2021). https://doi.org/10.1186/s13023-021-01820-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13023-021-01820-6