Abstract
Tenosynovial giant cell tumor is a rare proliferative tumor that arises from the synovium, bursae, or tendon sheaths due to an overproduction of colony-stimulating factor 1. Historically, treatment options for patients with local or diffuse tenosynovial giant cell tumor have been limited to surgical interventions. However, for some patients, surgical resection could worsen functional limitations and/or morbidity. In August 2019, the FDA approved pexidartinib (TURALIO™, Daiichi Sankyo), the first systemic treatment option for adult patients with symptomatic tenosynovial giant cell tumor associated with severe morbidity or functional limitations that were not amenable to improvement with surgery. Pexidartinib is an oral tyrosine kinase inhibitor with selective inhibition of colony-stimulating factor 1 receptor and is the first systemic therapy to show significant improvement in overall response rates when compared with placebo. Clinicians using pexidartinib should monitor for liver-related adverse events, which may require treatment interruption, dose reduction, or treatment discontinuation. Pexidartinib provides a novel non-surgical treatment option for patients with tenosynovial giant cell tumor that may significantly improve patients’ overall response, range of motion, physical function, tumor volume, and stiffness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pexidartinib, a tyrosine kinase inhibitor that inhibits colony-stimulating factor 1 receptor, is the first systemic therapy approved for patients with symptomatic tenosynovial giant cell tumor (TGCT) associated with severe morbidity or functional limitations not amenable to improvement with surgery. |
The efficacy of pexidartinib to improve overall response, range of motion, physical function, tumor volume, and stiffness was demonstrated in the ENLIVEN trial, a phase III, two-part study. |
Pexidartinib provides a novel non-surgical treatment option for patients with TGCT; however, additional research is needed to help establish a standardized approach to measure efficacy, unify clinical response and imaging criteria, and establish parameters for treatment duration. |
1 Introduction
Tenosynovial giant cell tumor (TGCT) is a rare proliferative tumor that arises from the synovium, bursae, or tendon sheaths [1, 2]. Within the tumor, there is a small percentage of cells (2–16%) that contain a translocation of chromosomes 1 and 2 [3]. This translocation leads to an overproduction of colony-stimulating factor 1 (CSF1) [3], which attracts macrophages and monocytes to form a tumor [3, 4]. The growth of these tumors can impair nearby tissues and structures, causing patients to experience pain, swelling, and joint limitation [5]. The classification of TGCT is dependent on the growth pattern of the tumor and is classified as being localized or diffused. Localized TGCT (L-TGCT) refers to a small lobulated lesion that mostly arises from the tendon sheath and less frequently from the synovial lining of digital joints [6, 7]. In contrast, diffuse TGCT (D-TGCT) is a more destructive and locally aggressive form of the disease in which the tumor infiltrates soft tissue mass along the synovial lining [6, 7]. TGCT occurs primarily in young adults between 30 and 40 years of age [8]. The annual incidence of TGCT in the United States is approximately 11 cases per million people; of these, 9.2 cases are L-TGCT type and 1.8 cases are D-TGCT type [8]. Although there is no sex predilection in the diffuse type, there is a higher prevalence of L-TGCT in females (1.6–2.1:1) [8].
TGCT commonly occurs in and around the knee [5]; however, other sites such as the flexor tendon sheaths of the hand, hip joints, ankle, and shoulder can also occur [7]. Persistent disease can result in long-term pain or joint dysfunction due to cartilage destruction and bone erosion [5]. Adequate surgical resection, when feasible, remains the treatment of choice for TGCT [9]. While localized disease is readily curable, diffuse disease has shown high recurrence rates with arthroscopy (40%) and open surgery (14%) [8, 9]. Due to the high recurrence rates, patients will go through multiple surgical resections, which may reduce their quality of life, increase morbidity, and reduce the function of affected joints [5]. Historically, treatment options for patients with TGCT have been limited to surgery. However, in rare cases, the tumor is unresectable and could lead to joint replacement or amputation [7]. Since 2008, systemic treatment options for TGCT have been investigated but have been unsuccessful. Clinical activity was seen with monoclonal antibodies and tyrosine kinase inhibitors targeting the CSF1/CSF1 receptor (CSF1R) axis in patients with locally advanced or relapsed D-TGCT [8, 9]. Intravenous monoclonal antibodies, emactuzumab and cabiralizumab, have been tested in patients with TGCT. Although emactuzumab has been discontinued from further development for TGCT, cabiralizumab is currently undergoing a phase II trial. Additionally, clinical trials investigating tyrosine kinase inhibitors, such as imatinib and nilotinib, demonstrated low response rates in patients with TGCT [10, 11].
In August 2019, the FDA approved pexidartinib (TURALIO™, Daiichi Sankyo), the first systemic treatment option for adult patients with symptomatic TGCT associated with severe morbidity or functional limitations that were not amenable to improvement with surgery. Pexidartinib is an oral tyrosine kinase inhibitor with selective inhibition of CSF1R and is the first systemic therapy to show significant improvement in overall response rates (39%) when compared with placebo [12]. This article reviews the pharmacology, clinical efficacy, safety profile of pexidartinib, and its place in therapy.
2 Clinical Pharmacology
2.1 Mechanism of Action
Pexidartinib is a tyrosine kinase inhibitor. It targets CSF1R, KIT proto-oncogene receptor tyrosine kinase (KIT), and FMS-like tyrosine kinase 3 (FLT3) harboring an internal tandem duplication (ITD) mutation. Inhibiting CSF1R is important due to the tumor’s ability to overproduce CSF1.
2.2 Pharmacodynamics
A higher risk of increased aspartate aminotransferase (AST) and alanine aminotransferase (ALT) was associated with higher exposure of pexidartinib. Additionally, increased serum transaminases occurred more frequently with higher doses of pexidartinib. Moreover, cardiac electrophysiology changes were assessed and there were no prolongation of QTc interval at two times the mean maximum exposure of pexidartinib 400 mg twice daily dose.
2.3 Pharmacokinetics
2.3.1 Absorption
Following the oral administration of pexidartinib, the median time to peak concentration (Tmax) is 2.5 h. However, high-fat meals, defined as meals comprising 800–1000 cal with fat being 50% of total caloric content, have been found to delay the Tmax by an additional 2.5 h. The high-fat meal includes approximately 150 cal from protein, 250 cal from carbohydrates, and 500–600 cal from fat. In addition, high-fat meals increase the maximum concentration (Cmax) and area under the curve (AUC0–INF) by 100%, hence dramatically increasing exposure to the drug.
2.3.2 Distribution
Pexidartinib is highly protein-bound. It binds to human serum albumin and α-1 acid glycoprotein by 99% and 89.9%, respectively. Moreover, the apparent volume of distribution is 187 L (27%).
2.3.3 Metabolism
The primary metabolism pathway of pexidartinib is oxidation by cytochrome P450 3A4 (CYP 3A4) enzymes and glucuronidation by UDP glucuronosyltransferase family 1 member A4 (UGT1A4). UGT1A4 catalyzes the formation of the major inactive N-glucuronide, which is approximately a 10% higher exposure than pexidartinib after a single dose.
2.3.4 Elimination
The apparent clearance of pexidartinib is 5.1 L/h. The half-life (t½) is 26.6 h. Sixty-five percent of pexidartinib is excreted via the feces, 44% unchanged. Twenty-seven percent of pexidartinib is renally excreted as metabolites, ≥ 10% as N-glucuronide [13].
3 Dosage and Administration
The recommended dosage of pexidartinib is 400 mg taken twice daily on an empty stomach at least 1 h before or 2 h after a meal or snack. Pexidartinib should be administered until disease progression or unacceptable toxicity occurs. The capsules should be swallowed whole and should not be opened, broken, or chewed. Any missed doses should be skipped and resumed at the next scheduled dose time. Total daily dosage modifications are recommended for adverse events and drug interactions (Table 1) [13].
4 Pivotal Clinical Study
The efficacy of pexidartinib was investigated in a two-part, multicentered, phase III randomized trial, ENLIVEN (Pexidartinib Versus Placebo for Advanced Tenosynovial Giant Cell Tumor) [12]. Part one was double-blinded and part two was open-label. Eligible patients 18 years or older with histologically confirmed TGCT diagnosis, advanced disease for which surgical resection would be associated with potentially worsening functional limitations or severe morbidity (confirmed by two surgeons or multidisciplinary tumor board), a score of at least 4 for pain or stiffness on a scale ranging from 0 to 10, a minimum tumor size of 2 cm, and on stable prescription of an analgesic regimen 2 weeks prior to randomization were included. Patients were excluded if they had previous treatment with pexidartinib or any biologic agent targeting CSF1 or CSF1R. All patients were included in the intention-to-treat analysis. Patients’ demographics were similar across both groups, in which the median age was 44 years; 53% had prior surgery; 88% were diagnosed with diffuse TGCT; and 9% had previously been treated with systemic therapy.
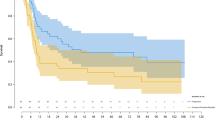
The first part of the study included 120 patients who were randomly assigned in a 1:1 ratio to receive pexidartinib (n = 61) or matching placebo (n = 59) for 24 weeks followed by an assessment at week 25. Patients received a 1000-mg loading dose of pexidartinib divided into two doses daily (400 mg morning, 600 mg evening) for 2 weeks. Following the loading dose period, patients received pexidartinib 400 mg twice a day for 22 weeks. Treatment continued until disease progression, unacceptable toxicity, consent withdrawal, or investigator’s decision to discontinue. At week 25, for part one of the study, the primary endpoint was overall response (complete or partial) based on masked, centrally read magnetic resonance imaging (MRI) and the Response Evaluation Criteria in Solid Tumors (RECIST), version 1.1. Secondary endpoints were assessed at week 25 for part 1 and part 2 of the study. Secondary endpoints included the mean change from baseline in range of motion of the affected joint; mean change from baseline in the Patient-Reported Outcomes Measurement Information System—Physical Function Scale (PROMIS); mean change from baseline in worst stiffness numeric rating scale (NRS); proportion of responders based on Brief Pain Inventory worst pain NRS and analgesic use by Brief Pain Inventory-30; centrally evaluated proportion of patients with overall response based on tumor volume score; and duration of response based on RECIST and tumor volume score (a TGCT-specific method that calculates tumor volume as a percentage of the estimated maximally distended synovial cavity) [14].
Fifty-two patients from the pexidartinib group and 48 patients from the placebo group completed part one of the study. The proportion of patients who achieved overall response by RECIST at week 25 was 39% (24 of 61) in the pexidartinib group versus 0% (0 of 59) in the placebo group. The difference was statistically significant with an absolute difference of 39% [95% CI 27–53] (p < 0.0001). Significant differences were seen between pexidartinib and placebo group in range of motion 8.9% (p = 0.0043); a mean difference score of 5.0 for physical function; (p = 0.0019); and a stiffness score difference of − 2.2 (p < 0.0001). Pain-30 responders were higher with pexidartinib (19 [95% CI 21–44]) compared with placebo (9 [95% CI 8–27]); with an absolute difference of 15.9% [95% CI 1–30]; however, the result was not statistically significant (p = 0.052). The proportion of patients who achieved overall response by tumor volume score at week 25 was 56% (34 of 61) with pexidartinib versus 0% (0 of 59) with placebo; (p < 0.0001). Median duration of response by RECIST (range 0–25 months) or tumor volume score (0–28 months) in the pexidartinib group was not reached.
Patients who completed part one were eligible to enter part two of the study. Additionally, patients with centrally confirmed disease progression before the end of part one were eligible for early entry into part two if found to be on placebo after unmasking. The second part of the study was an open-label extension for an additional 24 weeks and a baseline assessment at week 25. Patients in the treatment group entered part 2 with the same dose they received in part 1 and patients on placebo were given pexidartinib 400 mg twice daily. Forty-eight patients from the pexidartinib and 30 patients from the placebo group entered part two. In the 30-patient placebo group that crossed over to receive pexidartinib, nine patients (30%) had a RECIST response, 17 patients (57%) had a tumor volume score response, and 4 patients (13%) had a mean change in range of motion from the beginning of part two to week 25 of part two. The mean change of the PROMIS was 4.9, stiffness was − 3.0, and pain was − 2.6.
Adverse events of any grade occurred in 60 (98%) of the 61 patients that received pexidartinib and 55 (93%) of the 59 patients that received placebo. Grade 3 or 4 adverse events were higher in patients receiving pexidartinib (44%) compared with placebo (12%). Common grade 3 or 4 adverse events with a higher incidence in the pexidartinib group include elevated AST, ALT, alkaline phosphatase (ALP), and blood pressure. In addition, depigmentation of hair color of any grade was more common with pexidartinib. Adverse events that led to treatment interruption or dose reduction were higher in patients receiving pexidartinib (38%) compared with placebo (10%); these were most commonly due to increases in AST, ALT, or cholestatic hepatotoxicity in the pexidartinib group. Eight (13%) of 61 patients discontinued pexidartinib because of adverse events, of which seven were liver-related. Patients on the crossover pexidartinib treatment had fewer liver enzyme elevations than in part one, and no bilirubin increases or signs of drug-induced cholestatic hepatotoxicity.
5 Safety Considerations
5.1 Drug–Drug Interactions
Pexidartinib can cause serious and potentially fatal liver injury; thus, co-administration of pexidartinib with other products known to cause hepatotoxicity should be avoided. Furthermore, the primary metabolism pathway of pexidartinib is oxidation by CYP3A4 enzymes and glucuronidation by UGT1A4. Therefore, strong inhibitors of CYP3A or UGT should be avoided as they may increase the serum level of pexidartinib and increase occurrence of adverse reactions. Additionally, strong inducers of CYP3A, including grapefruit and grapefruit juice, may decrease the serum level of pexidartinib, which may increase the occurrence of treatment failure, so concomitant use should be avoided. If concomitant use of pexidartinib with a strong CYP3A inhibitor or UGT inhibitor cannot be avoided, the dose of pexidartinib should be reduced (Table 2). When the concomitant use of a strong CYP3A inhibitor or UGT inhibitor is discontinued, the dose of pexidartinib should be increased after three plasma half-lives of the strong CYP3A inhibitor or UGT inhibitor. The dose that the patient received prior to starting the inhibitor should be resumed. Additionally, acid-reducing agents have been found to decrease the Cmax and the AUC of pexidartinib by 55% and 50%, respectively. As a result, the concomitant use of proton pump inhibitors (PPIs) while taking pexidartinib should be avoided. As an alternative to a PPI, pexidartinib can be administered 2 h before or 2 h after taking a locally acting antacid. Moreover, it is recommended that pexidartinib is administered at least 2 h before or 10 h after taking a histamine 2 (H2)-receptor antagonist.
5.2 Contraindications
Currently, there are no known contraindications for pexidartinib.
5.3 Use in Specific Populations
5.3.1 Females and Males of Reproductive Potential
Findings from animal studies indicate that pexidartinib may impair both male and female fertility. Additionally, pexidartinib may cause embryo-fetal harm when administered to a pregnant woman. Thus, before the initiation of pexidartinib in females with reproductive potential, pregnancy status must be verified. Additionally, females of reproductive potential must be counseled to use effective contraception during treatment and for 1 month after the final administration. Likewise, male patients with female partners of reproductive potential must also be counseled to use effective contraception during treatment with pexidartinib and for 1 week after the final dose.
5.3.2 Lactation
Currently, there are no data about the presence of pexidartinib or its metabolites in either human or animal milk, nor are there data about the effects of pexidartinib on a breastfed child or on milk production. However, due to the potential for serious adverse reactions in a breastfed child, lactating women should be advised to not breastfeed during treatment with pexidartinib and for a minimum of 1 week after the final dose.
5.3.3 Renal Impairment
For patients with mild to severe renal impairment (CrCl 15–89 mL/min, estimated by Cockcroft–Gault), the dosage of pexidartinib should be adjusted to 200 mg in the morning and 400 mg in the evening.
5.3.4 Hepatic Impairment
There are no dosage adjustments recommended for patients with mild hepatic impairment. Additionally, no dosage recommendations have been established for patients with moderate to severe hepatic impairment. It is recommended to avoid pexidartinib in patients with pre-existing increased serum transaminases, total bilirubin or direct bilirubin (greater than upper limit of normal), or active liver or biliary tract disease, including increased ALP. Moreover, because of the risk of hepatotoxicity, pexidartinib is only available through a risk evaluation and mitigation strategies (REMS) program. The program includes requirements that must be followed by prescribers, patients, and pharmacies prior to dispensing. The most notable requirements of the REMS program include prescriber certification and education, patients’ enrollment for inclusion in a patient registry, and pharmacy certification with the program.
5.3.5 Geriatric Population
Due to insufficient numbers of geriatric patients aged 65 years and over enrolled in the pexidartinib clinical trial, there is no evidence to determine whether the geriatric population responds differently from younger patients.
5.3.6 Pediatric Population
The safety and effectiveness of pexidartinib in pediatric patients has not been established [13].
6 Formulary Considerations
Although surgery remains the mainstay of treatment for TGCT, for some patients, surgical resection could worsen functional limitations and/or morbidity. Pexidartinib provides a novel non-surgical treatment option for patients with L-TGCT or D-TGCT that may significantly improve patients’ overall response, range of motion, physical function, tumor volume, and stiffness.
Due to a lack of well-defined parameters for the indication of pexidartinib, it may be used in any line of therapy as long as the patient is symptomatic and not fit for surgery. The term ‘symptomatic’ is subjective as it is not well defined in the literature. Symptoms can include but are not limited to pain, range of motion, and quality of life. Additionally, the criteria for not being ‘surgically fit’ is not well defined in the literature and is subject to the judgment of a surgeon. Additionally, there lacks a standardized approach to measuring the efficacy of pexidartinib (by pain assessment tools, functional scales, and quality-of-life assessments). There also lacks a unifying criteria for imaging studies with defined prognostic factors as well as the establishment of parameters for treatment duration. Therefore, the criteria for prescribing pexidartinib is driven by the judgment of the treating physician. This may lead to difficulties in establishing guideline-directed therapy for pexidartinib and provide variation in coverage for commercial, federal, or state plans. The wholesale acquisition cost (WAC) for a 28-day supply of pexidartinib is US$18,480 for the 800-mg daily dose, US$13,860 for the 600-mg daily dose, US$9240 for the 400-mg daily dose, and US$4620 for the 200-mg daily dose [15]. Copay programs and program assistant programs are available for eligible patients. In addition to the REMS requirements, providers prescribing pexidartinib will need to route all prescriptions to Biologics by McKesson; the only specialty pharmacy authorized to manage and dispense pexidartinib.
7 Conclusion
Pexidartinib is the first systemic therapy approved for patients with symptomatic TGCT associated with severe morbidity or functional limitations not amenable to improvement with surgery. The unique mechanism of action of the drug, a tyrosine kinase inhibitor that inhibits CSF-1 receptor, has shown high response rates when compared with other agents studied. Clinicians using pexidartinib should monitor for liver-related adverse events that may require treatment interruption, dose reduction, or treatment discontinuation. Although significant differences in pain were not seen between pexidartinib and the placebo group, pexidartinib showed significant differences in patients’ overall response, range of motion, physical function, tumor volume, and stiffness. Therefore, pexidartinib would be of value in the clinical setting for patients who may benefit from a systemic option. Additional research is needed to help establish a standardized approach to measuring efficacy, unifying clinical response and imaging criteria, and to establish parameters for treatment duration.
References
Shetty SK, Hegde U, Agarwal G, Sreeshyla HS. Chondroid tenosynovial giant cell tumor of temporomandibular joint. Ann Maxillofac Surg. 2018;8(2):327–9.
Gouin F, Noailles T. Localized and diffuse forms of tenosynovial giant cell tumor (formerly giant cell tumor of the tendon sheath and pigmented villonodular synovitis). Orthop Traumatol Surg Res. 2017;103(1, Supplement):S91–S9797.
West RB, Rubin BP, Miller MA, Subramanian S, Kaygusuz G, Montgomery K, et al. A landscape effect in tenosynovial giant-cell tumor from activation of CSF1 expression by a translocation in a minority of tumor cells. Proc Natl Acad Sci USA. 2006;103(3):690–5.
Cupp JS, Miller MA, Montgomery KD, Nielsen TO, O'Connell JX, Huntsman D, et al. Translocation and expression of CSF1 in pigmented villonodular synovitis, tenosynovial giant cell tumor, rheumatoid arthritis and other reactive synovitides. Am J Surg Pathol. 2007;31(6):970–6.
Tenosynovial Giant Cell Tumor. https://rarediseases.org/rare-diseases/tenosynovial-giant-cell-tumor/. 2017.
Ofluoglu O. Pigmented villonodular synovitis. Orthop Clin N Am. 2006;37(1):23–33.
Mastboom MJL, Verspoor FGM, Verschoor AJ, Uittenbogaard D, Nemeth B, Mastboom WJB, et al. Higher incidence rates than previously known in tenosynovial giant cell tumors. Acta Orthop. 2017;88(6):688–94.
Giustini N, Bernthal NM, Bukata SV, Singh AS. Tenosynovial giant cell tumor: case report of a patient effectively treated with pexidartinib (PLX3397) and review of the literature. Clin Sarcoma Res. 2018;8:14.
Brahmi M, Vinceneux A, Cassier PA. Current systemic treatment options for tenosynovial giant cell tumor/pigmented villonodular synovitis: targeting the CSF1/CSF1R axis. Curr Treat Options Oncol. 2016;17(2):10.
Cassier PA, Gelderblom H, Stacchiotti S, Thomas D, Maki RG, Kroep JR, et al. Efficacy of imatinib mesylate for the treatment of locally advanced and/or metastatic tenosynovial giant cell tumor/pigmented villonodular synovitis. Cancer. 2012;118(6):1649–55.
Gelderblom H, Cropet C, Chevreau C, Boyle R, Tattersall M, Stacchiotti S, et al. Nilotinib in locally advanced pigmented villonodular synovitis: a multicentre, open-label, single-arm, phase 2 trial. Lancet Oncol. 2018;19(5):639–48.
Tap WD, Gelderblom H, Palmerini E, Desai J, Bauer S, Blay JY, et al. Pexidartinib versus placebo for advanced tenosynovial giant cell tumour (ENLIVEN): a randomised phase 3 trial. Lancet. 2019;394(10197):478–87.
TURALIO (pexidartinib) [package insert]. Basking Ridge: Daiichi Sankyo, Inc; 2019.
Tap WD, Wainberg ZA, Anthony SP, Ibrahim PN, Zhang C, Healey JH, et al. Structure-guided blockade of CSF1R kinase in tenosynovial giant-cell tumor. N Engl J Med. 2015;373(5):428–37.
TURALIOTM (pexidartinib) Academy of Managed Care Pharmacy (AMCP) v4.0 Formulary Submission Dossier. Daiichi-Sankyo; 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was not funded.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Monestime, S., Lazaridis, D. Pexidartinib (TURALIO™): The First FDA-Indicated Systemic Treatment for Tenosynovial Giant Cell Tumor. Drugs R D 20, 189–195 (2020). https://doi.org/10.1007/s40268-020-00314-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40268-020-00314-3