Abstract
Cardiovascular disease (CVD) remains the predominant cause of mortality and disability worldwide. Against this backdrop, finding effective drugs for the pharmacological treatment of CVD has become one of the most urgent and challenging issues in medical research. Garlic (Allium sativum L.) is one of the oldest plants and is world-renowned for its dietary and medicinal values. Allicin (diallyl thiosulfinate) is one of the primary natural active ingredients in garlic, which has been proven to have powerful cardioprotective effects and mediate various pathological processes related to CVD, such as inflammatory factor secretion, myocardial cell apoptosis, oxidative stress, and more. Therefore, allicin holds a promising application prospect in the treatment of CVD. This review summarized the biological functions of allicin and its potential mechanisms in CVD, including antioxidation, anti-inflammation, and anti-apoptosis effects. Reckoning with these, we delved into recent studies on allicin’s cardioprotective effects concerning various CVDs, such as atherosclerosis, hypertension, myocardial infarction, arrhythmia, cardiac hypertrophy, heart failure, and cardiotoxicity. Further, considering the tremendous advancement in nanomedicine, nanotechnology-based drug delivery systems show promise in addressing limitations of allicin’s clinical applications, including improving its solubility, stability, and bioavailability. Through this review, we hope to provide a reference for further research on allicin in cardioprotection and drug development.
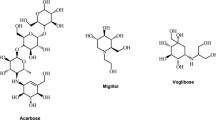
Graphical Abstract

Similar content being viewed by others
Introduction
The term cardiovascular disease (CVD) encompasses a spectrum of conditions that inflict damage upon the heart and vascular system, encompassing hypertension, atherosclerosis, cardiomyopathy, myocardial infarction (MI), and heart failure (HF). These ailments stand as the primary cause of elevated morbidity and mortality on a global scale [1]. Despite the widespread utilization of cardioprotective pharmacotherapy, such as β-blockers, angiotensin-converting enzyme inhibitors (ACEIs), calcium channel blockers (CCBs), and statins, the prevalence of CVD continues to increase annually. Furthermore, chronic administration of these medications frequently results in a spectrum of adverse effects [2]. Therefore, the exploration and development of novel therapeutic agents for cardiovascular disease (CVD) is of paramount clinical significance. In this context, natural medicines are increasingly esteemed for their multiple targets, low cost, and low toxicity in the advancement of CVD treatments.
Garlic (Allium sativum L.) is widely utilized in cooking to enhance the flavor of dishes and has been globally employed since ancient times. Additionally, it possesses therapeutic properties and serves as a traditional medicinal plant used in various indigenous remedies worldwide [3]. The pharmacological benefits of garlic are extensive and well-documented, encompassing antioxidant, anti-inflammatory, antimicrobial, and anticancer properties. Recent epidemiological studies have revealed a negative correlation between garlic intake and the risk of cardiovascular events [4, 5], indicating the potential of garlic as a promising therapeutic agent for treating CVD. Modern pharmacological research has demonstrated that sulfur-containing compounds such as allicin, diallyl disulfide (DDS), diallyl trisulfide (DTS), and S-allyl-l-cysteine (SAC) constitute the main components of garlic [6].
Allicin, the most biologically active sulfur-containing compound of garlic, possesses various cardioprotective properties, including reducing blood pressure, regulating blood lipids, preventing atherosclerosis, and protecting against myocardial injury [7]. Therefore, allicin holds promising application prospects as a bioactive compound for treating CVD. This review presents a comprehensive overview of recent research on the cardioprotective mechanisms and potential clinical applications of allicin in CVD. Additionally, considering the rapid advancements in nanotechnology, novel delivery systems for allicin with improved stability, encapsulation efficiency, and bioavailability are also assessed, such as nanoparticles, liposomes, hydrogels, and nano‐emulsions. We hope to provide guidance and new ideas for drug development and clinical application of allicin in treating CVD.
Allicin in the treatment of CVD
The biological function of allicin
Chemistry properties of allicin
Allicin is present in white garlic and other Allium species such as field garlic (A. vineale L.), wild garlic (A. ursinum L.), elephant garlic (A. ampeloprasum L.), and alpine leek (A. victorialis L.), serves as the predominant biologically active sulfur-containing compound in garlic [6]. Allicin is the source of garlic’s distinctive strong, pungent odor and its spicy flavor profile. In its fresh state, garlic contains alliin (S-allyl-l-cysteine sulfoxide) but lacks free allicin. However, the mechanical crushing of garlic triggers alliinase to rapidly convert alliin into cytotoxic and odoriferous allicin [8].
Allicin, a colorless and oily liquid, exhibits limited solubility in water but is soluble in organic solvents, including ethanol, benzene, and ether. Allicin demonstrates low chemical stability and significant volatility, leading to its decomposition into smaller sulfur-containing compounds like 2-propene sulfenic acid, thioacrolein, and allyl alcohol at room temperature [9]. Furthermore, while allicin is unstable under heat and alkaline conditions, it demonstrates relative stability in acidic environments, particularly within a pH range of 5–7 [10]. In nature, garlic plants produce allicin upon tissue damage; however, it can also be synthesized chemically. For instance, a previous study successfully employed a binary system consisting of the plant enzyme alliinase and its substrate alliin to generate allicin [11]. Additionally, alliin serves as the precursor for allicin and can be obtained from garlic or synthesized through bromopropylation of cysteine followed by hydrogen peroxide oxidation [12].
Anti-inflammatory effects
After the occurrence of cardiovascular diseases, the body’s immune system can be activated, triggering an abnormal autoimmune response that mediates the onset of local inflammation and contributes to the progression of cardiovascular disease. Therefore, inflammation plays a significant role in the development and progression of CVD, including atherosclerosis, thrombosis, MI, and myocardial ischemia–reperfusion (MIR) injury [13]. Targeting anti-inflammatory therapies has emerged as a promising strategy. Accumulating evidence indicates that increased secretion and circulation of inflammatory markers such as Interleukin-6 (IL-6), tumour necrosis factor-alpha (TNF-α), and Interleukin-1β (IL-1β) are associated with the development and exacerbation of CVD [14]. Jessica et al. [15] discovered that allicin can attenuate both transcript and protein expression of pro-inflammatory cytokines IL-1β, IL-6, and IL-12β, while simultaneously enhancing the expression of the anti-inflammatory cytokine IL-10 in lipopolysaccharide (LPS)-induced macrophage model. The administration of allicin exhibited a significant reduction in serum levels of pro-inflammatory cytokines IL-1β, IL-6, and TNF-α across multiple animal models [16, 17].
Recent research indicated that Toll-like receptor 4 (TLR4) and the nuclear factor kappa B (NF-κB) signalling pathway play a role in promoting the activation of cytokines such as TNF-α, IL-6, and IL-1β to exacerbate inflammation, leading to subsequent myocardial tissue damage [18]. Inhibition or absence of TLR4 or NF-κB, which are critical regulators in pro-inflammatory cascades, had been shown to reduce left ventricular remodelling extent and improve cardiac function [19]. Ca2+/calmodulin-dependent protein kinase II (CaMKII) is an essential protein involved in regulating intracellular calcium transport processes and cardiomyocyte contractile function. It mainly phosphorylates calcium transport-related proteins, which increases calcium influx and strengthens cardiomyocyte contractility, thereby affecting cardiac function [20]. Recent findings suggested that CaMKII can trigger NF-κB-mediated pro-inflammatory gene expression and the inflammasome activation via TLR4 to promote the release of downstream pro-inflammatory factors in response to pressure overload [21]. In addition, the NOD-like receptor pyrin domain-containing protein 3 (NLRP3) inflammasome, a multiprotein signalling complex, is also assembled and activated in response to damage-associated molecular patterns (DAMPs), which then catalyzes active forms of pro-inflammatory cytokines, such as IL-1β and IL-18. Therefore, the activation of the NLRP3 inflammasome is considered to be a key link in aggravating vascular and cardiac inflammation [22]. Takeshiet et al. [23] found that allicin significantly reduced serum IL-1β, IL-6, and TNF-α levels, improved calcium homeostasis in cardiomyocytes, downregulated calcium transportation-related CaMKII and inflammation-related NF-κB and NLRP3 expression, which was observed in smooth muscle cells and cardiomyocytes. Additional experiments demonstrated that allicin abrogated inflammation and myocardial fibrosis by blocking the activation of NF-κB and Smad 2/3 signalling, respectively [24]. Moreover, allicin attenuated the LPS-induced increase in NLRP3, pro-IL-1β, and IL-1β proteins. Silencing of Nrf2 by siRNA (siNrf2) significantly attenuated the allicin-induced increase in cell viability and HO-1 and decrease in NLRP3 protein in LPS-stimulated H9C2 cells [25].
Anti-oxidative stress
Oxidative stress plays a pivotal role in the pathophysiological mechanisms of various cardiovascular diseases and is involved in all stages of CVD onset and progression. Its mechanism encompasses complex signalling molecules and regulatory pathways, thereby emphasizing the pivotal role of antioxidant stress in the treatment of CVD. Oxidative stress refers to an imbalance between reactive oxygen species (ROS) generation and antioxidants within the body or cells when exposed to diverse detrimental stimuli, ultimately resulting in tissue damage [26]. ROS are the main compounds involved in oxidative stress reactions, including oxygen free radicals such as superoxide, hydroxyl radicals, singlet oxygen, and peroxyl radicals, as well as non-radicals that can generate free radicals, such as hydrogen peroxide (H2O2) and hypochlorous acid [27]. A study discovered that pre-incubation with allicin (0.3–10 μM) could concentration-dependently mitigate the increase of intracellular ROS induced by H2O2 in H9C2 cells and protect these cells against H2O2-induced damage [28]. Wang et al. [29] demonstrated that allicin exhibited a protective effect against injury induced by high glucose/hypoxia in aortic endothelial cells by significantly reducing ROS production, which may involve inhibiting the PKC pathway and regulating the HIF-1α signalling pathway.
Malondialdehyde (MDA) is the final product of lipid peroxidation reactions caused by oxygen free radicals, displaying significant cytotoxicity and exacerbating cell membrane damage. It is commonly used as an indicator reflecting the degree of oxidative stress and the amount of oxygen-free radical generation [30]. Various endogenous enzymes and non-enzyme antioxidants present in normal myocardium are sufficient to counteract the cytotoxic products of ROS, including antioxidant enzymes such as superoxide dismutase (SOD), glutathione peroxidase (GSH-Px), catalase (CAT), and peroxidase (Prx). Allicin supplementation can significantly reduce serum MDA levels in rabbits fed with a 1% high-cholesterol diet, while simultaneously increasing serum HDL-C, GSH, and SOD levels [31]. Additionally, allicin can enhance the activity of SOD, CAT, and GSH-Px, thereby improving both systolic and diastolic function in the myocardium of rats experiencing MIR injury [16]. This mechanism was partly associated with alleviating the activation of the p38 signalling pathway. Liu et al. [24] indicated that allicin protected cardiac function and prevented the development of cardiac hypertrophy through ROS-dependent mechanisms involving multiple intracellular signalling, such as ERK1/2, JNK1/2, and AKT signalling pathways.
Anti-apoptosis
Apoptosis is a programmed cell death process that is activated by various signalling cascades and regulated by intricate networks. Two extrinsic and intrinsic signalling pathways mainly regulate apoptosis. The extrinsic apoptosis pathway is initiated by death ligands triggering death receptor signalling on the cell surface. The intrinsic apoptosis pathway is activated by oxidative stress, calcium overload, DNA damage, and activation of various transcription factors within the mitochondria, leading to an intracellular apoptosis pathway. Regardless of whether it follows the extrinsic or intrinsic pathway, apoptosis ultimately leads to the activation of effector caspase-3 and induces cell death. In CVD, apoptosis of myocardial cells can exacerbate pathological processes by reducing their numbers. Therefore, it is crucial to reduce and inhibit myocardial cell apoptosis for effective treatment of CVD. A study demonstrated that allicin treatment effectively modulated apoptosis-related proteins, leading to a reduction in the expression levels of Bax and cleaved caspase-3, while simultaneously increasing the expression levels of Bcl-2 and cytosolic cytochrome C [32]. Deng et al. [33] found that allicin treatment enhanced cell viability and reduced apoptosis from 13.5 ± 1.2% to 6.11 ± 0.15% compared with hypoxia/reoxygenation in H9C2 cells.
Guo et al. discovered that allicin inhibited the high glucose-induced activation of caspase-3 and nuclear translocation of NF-κB, which appeared to suppress elevated glucose-induced cardiomyocyte apoptosis by inhibiting NADPH oxidase-related ROS and its downstream JNK/NF-κB signalling pathway [34]. Ma et al. [35] established an MI model by ligating the left coronary artery, demonstrating that the myocardial apoptotic index was also markedly lowered in allicin-treated rats. Furthermore, allicin can effectively reduce cardiomyocyte apoptosis in rat models of MI by significantly regulating the JNK signalling pathway [36]. Mohamed et al. [37] observed that methotrexate (MTX), a chemotherapy drug known for its severe cardiac side effects, induced alterations in the cardiac histopathology and enhanced the caspase-3 expression in the rat cardiac tissues, indicating the exacerbation of cardiomyocyte apoptosis. Allicin administration at a dosage of 20 mg/kg orally for 2 weeks effectively attenuated MTX-induced apoptosis of myocardial cells. Similarly, intraperitoneal injection of doxorubicin (DOX) resulted in significant activation of caspase-3 in myocardial tissue, which was markedly alleviated by pretreatment with allicin and restored cardiac structure [17] (Fig. 1).
Allicin can exert cardioprotective effects on CVD through various pathways, including anti-apoptosis, antioxidant stress reduction, and anti-inflammatory effects. Allicin regulates the expression of caspase-3 by increasing the level of Bcl-2/Bax, thereby inhibiting apoptosis triggered by the death-receptor pathway. Allicin exhibits inhibitory effects on multiple pathways involved in ROS-mediated oxidative stress, such as the Nrf2 pathway, JNK pathway, and NF-ĸB pathway. Furthermore, allicin can inhibit the activation of inflammatory response by blocking both TLR/NF-ĸB pathway and Ca2+-mediated CaMKII signaling pathway. BAX BCL2-associated X protein, Bcl-2 B-cell lymphoma 2, CaMKII Ca2+/calmodulin-dependent kinase II, JNK c-Jun N-terminal kinase, NF-ĸB nuclear factor-kappaB, Nrf2 nuclear factor erythroid-2-related factor 2, ROS reactive oxygen species, TLR Toll-like receptor 4
Atherosclerosis
Atherosclerosis (AS), a chronic arterial disease characterized by arterial inflammation and lipid deposition within the vessel wall intima, is closely associated with the development of CVD [38]. Elevated levels of triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), and total cholesterol (TC) have been identified as significant contributors to AS. In individuals with hypercholesterolemia, a daily intake of 9.6 mg of allicin resulted in a reduction of TC by 4.2% and LDL-C by 6.6% [39]. Similarly, Lu et al. [40] discovered that allicin decreased TC, TG, and LDL-C levels in mice fed a high-cholesterol diet while also mitigating oxidative stress damage, inflammatory responses, vascular dysfunction, and aortic lesions. Lin et al. [41] found that allicin reduced cholesterol levels in foam cells and enhanced cholesterol efflux by activating the peroxisome proliferator-activated receptor γ (PPARγ)/liver X receptor alpha (LXRα) signalling pathway, thereby reducing lipid accumulation. Nantiya et al. [42] demonstrated that allicin possessed hypolipidemic effects by upregulating low-density lipoprotein receptor (LDLR) expression through the activation of sterol regulatory element binding proteins 2 (SREBP2) and downregulating proprotein convertase subtilisin/kexin type 9 (PCSK9) expression via the suppression of hepatocyte nuclear factor 1α (HNF1α), thereby enhancing the uptake of LDL by HepG2 cells. Moreover, as mentioned earlier, the study also revealed that the efficacy of allicin (200 μM) in lowering blood lipids was comparable to atorvastatin’s effect (10 μM).
Additionally, allicin has been shown to effectively mitigate the risk factors associated with atherosclerosis (AS) and delay its onset and progression. Homocysteine (Hcy) is an independent risk factor for AS. Liu et al. [43] found that allicin effectively reduced the carotid intima-media thickness (cIMT), TC, and TG by lowering plasma Hcy levels, thereby preventing the development of AS in patients with hyperhomocysteinemia. In recent years, an increasing body of research indicated that alterations in the composition of gut microbiota and the metabolites derived from it have significant implications for the progression of AS [44]. The gut microbiota-generated metabolite, trimethylamine N-oxide (TMAO), is widely recognized as a significant risk factor in promoting the progression of atherosclerosis [45]. Elevated blood levels of trimethylamine oxide (TMAO) have been demonstrated to be associated with an increased risk of major adverse cardiovascular events and all-cause mortality [46]. TMAO is implicated in inflammation and oxidative stress, cholesterol metabolism, bile acid metabolism, and foam cell formation in AS [47]. A recent study found that the consumption of raw garlic juice for 1 week inhibited TMAO formation and increased the relative abundance of beneficial gut bacteria in individuals with high TMAO levels [48]. Allicin also significantly decreased serum TMAO levels and attenuated aortic lesions in carnitine-induced apolipoprotein E-deficient (ApoE) mice. These findings indicate that allicin may play a vital role in delaying the occurrence and progression of AS through multiple targets and mechanisms (Table 1).
Hypertension
Hypertension is a significant risk factor for CVD. The pathogenesis of hypertension is commonly believed to involve endothelial dysfunction and increased peripheral vascular resistance [49]. Elkayam et al. [50] discovered that the administration of 80 mg/kg/day of allicin for 6 weeks resulted in reduced systolic blood pressure in spontaneously hypertensive rats (SHRs). The impact of allicin on blood pressure and renal function was comparable to that of losartan in rats with chronic kidney disease, and the antihypertensive effect of allicin was associated with the upregulation of angiotensin II receptor type 2 (AT2R) and endothelial nitric oxide synthase (eNOS) as vasodilators [51]. On the other hand, studies found that the anti-hypertensive effect of allicin can be primarily attributed to its easy degradation into organosulfur compounds in the presence of thiols, becoming an effective endogenous hydrogen sulfide (H2S) donor in the body [52]. H2S has been established as a potent gaseous signalling molecule with vasodilatory activity, playing a crucial role in maintaining basal blood pressure and contributing to hypertension development [53]. Cui et al. [54] demonstrated that allicin promotes vasorelaxation through both the NO-soluble guanylate cyclase-cyclic guanosine monophosphate (NO-sGC-cGMP) pathway and prostacyclin-adenylyl cyclase-cyclic adenosine monophosphate (PGI2-AC-cAMP) pathway via H2S production, thus exhibiting robust anti-hypertensive effects in SHRs. Additionally, remodelling caused by hypertension is considered the pathological basis of target organ damage [55]. Liu et al. [23] concluded that allicin effectively ameliorated vascular and cardiac remodelling induced by hypertension through inhibition of the CaMKII/NF-κB signalling pathway, reduction in serum levels of IL-1β, IL-6, and TNF-α, improvement in calcium homeostasis in cardiomyocytes, and downregulation of the NLRP3 inflammasome. In summary, these studies provide evidence for the beneficial antihypertensive effects of allicin (Table 2).
Myocardial infarction and myocardial ischemia–reperfusion injury
Cardiomyocyte apoptosis is a crucial pathological factor associated with MI. The extent of cardiomyocyte apoptosis positively correlates with the severity of MI [56]. Allicin had been reported to reduce infarct size and improve cardiac function by inhibiting the Bcl-2/Bax signaling pathway-dependent cell apoptosis [35]. Furthermore, the administration of Allicin can dose-dependently decrease levels of creatine kinase and lactate dehydrogenase after MI. In a rat model of MI induced by subcutaneous injection of isoproterenol, allicin significantly alleviated cardiomyocyte apoptosis by regulating the c-Jun N-terminal kinase (JNK) signalling pathway. Its inhibitory effect may be attributed to the activation of the endogenous protective eNOS/NO-mediated antioxidant stress signalling pathway [36]. In addition, the H2S synthesizing enzymes cystathionine-β-synthase (CBS) and cystathionine-γ-lyase (CSE) in myocardial tissues of rats decreased after MI, leading to a significant reduction in H2S in myocardial tissues and blood. As an influential donor of H2S within the body, Allicin can elevate CBS and CSE levels in myocardial tissues, maintain Ca2+ homeostasis of cardiomyocytes, regulate coronary artery vasodilation, and thus exert protective effects on ischemic myocardium [57].
Myocardial ischemia–reperfusion (MIR) injury is a complicated pathophysiological process characterized by intense inflammatory reactions, cardiomyocyte apoptosis, oxidative stress, and Ca2+ overload. Allicin significantly attenuated the release of inflammatory factors such as IL-6, TNF-α, and IL-8 in the serum after MIR by inhibiting the activation of the p38/MAPK signalling pathway. Additionally, allicin can enhance the activities of SOD, CAT, and GSH-Px to ameliorate myocardial contractility and relaxation function [16]. Deng et al. [33] simulated MIR injury in vitro using a hypoxia-reoxygenation (HR) model with pig cardiomyocytes and observed that allicin significantly reduced the expressions of IL-6 and TNF-α after HR, as well as mitigating the loss of mitochondrial membrane potential.
This study also revealed that allicin decreased the apoptosis rate of HR-induced cardiomyocytes, reduced the expressions of apoptosis-related proteins Bax, cleaved caspase-3, and cytosolic cytochrome C, and increased the expression of Bcl-2. Gao et al. [58] pointed out that pretreatment with allicin reduced infarct size and improved cardiac function in MIR mice partially by inhibiting the PI3K-mediated GRK2/PLC-γ/IP3R signalling pathway, thereby suppressing Ca2+ overload-induced cardiomyocyte apoptosis. These findings suggest that allicin confers protection to cardiomyocytes against HR damage through attenuation of apoptosis, inflammation, and mitochondrial injury. Additionally, Liu et al. [59] discovered that allicin promoted angiogenesis and safeguards myocardial tissue from HR injury by modulating miR-19a-3p to inhibit the PI3K/AKT signalling pathway (Table 3).
Cardiac hypertrophy
Cardiac hypertrophy (CH) is an adaptive compensatory response of the heart to oxidative stress, hemodynamic load, angiotensin II (Ang II), hormones, and other stimulating factors [60]. Persistent CH can lead to cardiac dilation, heart failure, and even sudden cardiac death. Pressure overload induces CH accompanied by an elevation in ROS, which activates various hypertrophy signals and factors. However, treatment with a free radical scavenger effectively mitigates the hypertrophic response [61]. Li et al. [62] discovered that allicin activates the Nrf2/HO-1 antioxidant signalling pathway to decrease ROS levels, carbonylated proteins, and thiobarbituric acid reactive substances (TBARS), while enhancing GPx activity. This prevented the development of cardiac remodelling and retards the progression of CH in Ang II-induced CH rats. Liu et al. [24] found that allicin markedly inhibited hypertrophy responses induced by Ang II or pressure overload and increased ROS generation and NADPH oxidase activity in an animal model of CH. The underlying mechanism might be the ROS-dependent ERK1/2, JNK1/2, and AKT signalling pathways blockage.
A recent study revealed that allicin significantly improved cardiac function in rats with abdominal aortic constriction (AAC)-induced CH [63]. Specifically, allicin not only reduced CH marker proteins such as brain natriuretic peptide (BNP) and β-myosin heavy chain (β-MHC) but also decreased autophagy marker proteins including Beclin-1 and LC3-II in the hearts of AAC-induced rats and Ang II-treated neonatal rat cardiomyocytes. The beneficial effects of allicin were found to be antagonized by the pharmacological inhibitor of the mammalian target of rapamycin (mTOR). These findings elucidate a potential mechanism through which allicin attenuates CH by inhibiting excessive autophagy via activation of PI3K/Akt/mTOR and MAPK/ERK/mTOR signaling pathways. Interestingly, considering the significant correlation between cardiac microvascular damage and the development of CH, Shi et al. [64] discovered that allicin improved the distribution and expression of platelet endothelial cell adhesion molecule-1 (PECAM-1) while activating the PECAM-1-PI3K-Akt-eNOS signaling pathway. This activation facilitated migration and angiogenesis in cardiac microvascular endothelial cells, thereby advancing the modification ability of their shear adaptation. These findings provide potent support for the potential therapeutic application of allicin in managing CH (Table 4).
Myocardial fibrosis
Myocardial fibrosis is the result of excessive fibrillar collagen synthesis and deposition, which determines the clinical course and outcome of HF patients [65]. The transforming growth factor-β (TGF-β)/Smad signalling pathway has been proven to play a crucial role in the progression of myocardial fibrosis [66], thus making it a potential therapeutic target. Li et al. [67] demonstrated that allicin exhibited an anti-myocardial fibrosis effect on MI rats by repressing the deposition of myocardial collagen fibres through downregulating expressions of collagen I, collagen III, TGF-β1, and Smad3 while upregulating expression of Smad7. Liu et al. [68] showed that allicin exerted a protective effect against cardiac dysfunction and cardiomyocyte apoptosis, while also inhibiting the progression of myocardial fibrosis in streptozotocin (STZ)-induced diabetic rats. The mechanism underlying its amelioration of myocardial fibrosis was associated with the inhibition of CTGF and TGF-β protein expression. In addition, the extent of fibrosis is closely related to inflammatory responses. NF-κB serves as a prototypical pro-inflammatory signalling pathway capable of activating the TGF-β pathway to facilitate myocardial fibrosis [69]. Kong et al. [19] found that allicin alleviated cardiac dysfunction and decreased myocardial fibrosis in STZ-induced diabetic rats by inhibiting the NF-κB signalling pathway (Table 5).
Arrhythmias
Arrhythmias often result from alterations in the electrophysiological properties of cardiomyocytes and their underlying ion channels [70]. Numerous studies have indicated that garlic and garlic extract can improve arrhythmias through modulation of ion channels [71]. Deng et al. [72] found that allicin inhibited the transient outward K+ current in a concentration-dependent manner and prolonged the action potential duration of human atrial myocytes, but it did not affect the ultrarapid delayed rectifier K+ current and the L-type Ca2+ current. Building upon this finding, Cao et al. [73] further demonstrated that allicin also exhibited an inhibitory effect on the transient outward potassium current (Ito) in mouse ventricular myocytes. High-dose allicin (≥ 100 µmol/L) accelerated the voltage-dependent inactivation of Ito in mouse ventricular myocytes, which may be the potential mechanism by which allicin exerts its anti-arrhythmic effect. The Cav1.2 channel conducts the L-type calcium current (ICaL), which mediates excitation–contraction coupling and action potential duration, thereby playing a crucial role in cardiac electrophysiological activities [74]. Han et al. [75] indicated that allicin inhibited Cav1.2 channels by reducing the expression of channel proteins, providing a partial explanation for its inhibitory potential. Allicin also effectively inactivated the ΔKPQ-SCN5A mutant channel in congenital long QT syndrome type 3 (LQT3), thereby reducing the late sodium current of the ΔKPQ-SCN5A mutation [76]. Moreover, allicin decreased the ratio of late sodium current to peak current (INa,L/INa,P) by promoting Nav1.5 distribution on the cell membrane, resulting in therapeutic effects on LQT3. These findings indicate that allicin can ameliorate arrhythmias by regulating multiple ion channels (Table 6).
Cardiotoxicity
Cardiotoxicity is a severe side effect secondary to cardiac damage caused by chemotherapy drugs, ultimately leading to MI, myocardial fibrosis, and HF [77]. Therefore, there is an urgent need to explore natural extracts that can alleviate cardiotoxicity. In rat models of TZB-induced cardiotoxicity, allicin treatment not only reduced the levels of pro-inflammatory cytokines and myocardial enzymes, including TNFα, IL-1β, IL-6, cTnI, cTnT, and LDH [78], but also significantly attenuated cell apoptosis and ROS levels. These findings suggest that allicin possesses anti-inflammatory, anti-fibrotic, antioxidant, antihyperlipidemic, and anti-apoptotic properties that can potentially alleviate TZB-induced cardiotoxicity. Thubiani et al. [79] revealed that allicin-attenuated adriamycin (ADR) -induced myocardial injury by inhibiting oxidative stress and inflammation. Allicin pretreatment significantly suppressed the elevation of ADR-induced serum CK-MB and LDH levels, as well as diminished the expression of oxidative parameters such as TNF-α and TGF-β. Furthermore, allicin exhibited a protective role against DOX-induced cardiotoxicity by effectively alleviating cardiac oxidative damage, apoptosis, and inflammation [17]. These findings highlight the potential clinical application of allicin as a promising natural drug for anti-cardiotoxicity (Table 7).
Noval nanotechnology-based drug delivery strategies of allicin
Allicin has substantial potential for CVD therapy. Consequently, the majority of existing research has focused on elucidating allicin’s biological activity and potential health benefits rather than its pharmacokinetics. However, due to its lipophilic nature and poor water solubility, allicin exhibits limited dissolution and bioavailability when administered as a drug. Numerous studies have indicated that its half-life is less than 1 min, highlighting its inherent instability [80]. Moreover, being a stimulating ingredient, allicin may induce adverse reactions such as intolerance, allergy, and gastrointestinal disturbances [81]. These factors undoubtedly pose substantial challenges in effectively translating it into therapeutic modalities. Therefore, it is imperative to explore safer, more stable delivery systems with low toxicity and high loading capacity for allicin to enhance its applicability in CVD treatment.
In recent years, nano-biotechnology has garnered much greater attention as a burgeoning field with immense scope and application in drug delivery platforms. Advances in nanotechnology-based drug delivery systems show promise in addressing these challenges, potentially enhancing the solubility, stability, and bioavailability of allicin. Currently, various nanoformulations such as nanoemulsions [82], liposomes [83], hydrogels [84], gelatin nanoparticles [85], and other miscellaneous formulations [86] not only have the ability to encapsulate and protect allicin from degradation but also improve its solubility, stability, permeability, and retention at the target site [87] (Fig. 2).
Nanoparticles
Nanoparticles (NPs) are solid particles ranging in size from 1 to 100 nm, possessing a substantial surface area that enables the encapsulation or adsorption of drugs and other active ingredients onto their substrate [88]. Consequently, NPs facilitate enhanced drug absorption and bioavailability. Due to their diminutive size, NPs possess not only the capability to traverse cell membranes or the blood–brain barrier for targeted drug delivery but also evade immune surveillance to prolong their retention times within biological tissues. Therefore, NPs have emerged as a promising drug delivery system in medicine, particularly for disease treatment and diagnosis [89]. Moreover, the advantages of nanoparticles as delivery systems lie in their ability to increase drug loading capacity, enhance stability, exert sustained control over release properties, and facilitate the transport of drugs across cell membranes or biological barriers through precise modulation of their morphology, surface chemistry pharmacokinetics, and release characteristics. A recent study discovered that the allicin-loaded polylactic acid–glycolic acid nanoparticles enhanced the encapsulation efficiency and drug-loading capacity of allicin, while also ensuring a consistent controlled-release rate of allicin in an acidic environment [87]. Hashemy et al. [90] developed polyethylene glycol and folic acid-modified chitosan-egg phospholipid nanoparticles loaded with allicin (AC-PLCF-NPs), which demonstrated potent inhibitory activity against Gram-negative bacterial strains and enhanced cytotoxicity against HT-29 cancer cells compared to free allicin. Chen et al. [86] developed a functionalized adipo-8 aptamer loaded with allicin to form a synergistic binary-drug delivery system for treating obesity. This study demonstrated that this nanoparticle-based system efficiently protected allicin from degradation, exhibiting significant potential in encapsulating, transporting, and releasing the molecular cargo into white adipose tissue. Despite the considerable potential of NPs in drug delivery applications loaded with allicin, it is imperative to consider their potential toxic effects. Various factors may influence the toxicity and biocompatibility of nanoparticles, necessitating thorough investigation before their application in biomedicine.
Liposomes
Liposomes are spherical, double-layered vesicles formed by an amphiphilic phospholipid membrane, which contains an aqueous core and a hydrophobic surface. Due to the excellent cell affinity of the lipid-like bilayer membrane, liposomes exhibit remarkable biodegradation, biocompatibility, and sustained release characteristics [91]. Simultaneously, they effectively shield drugs from external environmental factors such as enzymatic degradation, pH changes, chemical hydrolysis, and oxidative degradation thereby enhancing drug stability. Additionally, liposomes can encapsulate, deliver, and release various water-soluble materials and lipid-soluble and amphiphilic substances [92]. These advantages establish liposomes as one of the most commonly utilized nano drug delivery systems. Cristian et al. [83] developed a liposome nanodrug delivery system, demonstrating that liposomes serve as a suitable encapsulation system for stabilizing garlic active compounds and enhancing the stability of allicin. The application of liposomes, however, still encounters several challenges such as limited drug loading capacity, inadequate long-term stability, and high costs associated with large-scale industrial production [93].
Hydrogels
Hydrogel is a type of polymer characterized by its three-dimensional network structure formed through the cross-linking of the polymer backbone and hydrophilic functional groups via covalent bonds, ionic bonds, hydrogen bonds, or physical entanglement [94]. The hydrogel-based drug delivery systems have emerged as a promising approach for targeted and sustained drug release due to their exceptional biocompatibility, adjustable physicochemical properties, and ability to encapsulate both hydrophilic and hydrophobic drugs [95]. With further research, hydrogel shows promising potential in myocardial repair due to its similar three-dimensional structure to the extracellular matrix, excellent biocompatibility and mechanical properties, as well as its ability to provide a physiological environment akin to that of native myocardium [96]. A recent study indicated that the application of a smart hydrogel coating loaded with allicin can have the potential to facilitate endothelial cell regeneration, suppress smooth muscle cell proliferation, and mitigate the inflammatory response surrounding blood vessels to promote neovascularization in vivo [84]. This hydrogel system had excellent biocompatibility and could regulate the atherosclerotic microenvironment and prevent in-stent restenosis by continuously releasing allicin. Although significant advancements have been made in the field of hydrogels for cardiac tissue engineering, several critical challenges remain to be addressed before their safe implementation in clinical practice. For instance, further investigation is required regarding the selection of appropriate materials for cardiac repair, optimal dosage and timing of injection, and efficient distribution strategies [97].
Nanoemulsions
Nanoemulsions (NEs) is a stable, transparent, and low-viscosity dispersion system composed of the oil phase, water phase, surfactant, and cosurfactant in appropriate proportions. It has been found that NEs, as a novel nano-drug delivery system, have the characteristics of enhancing the solubility, stability, and bioavailability of poorly soluble drugs due to their small and uniform particle size, and thus have the functions of targeting and sustained release drug delivery [98]. Due to these advantages, NEs are rapidly emerging as a versatile platform for drug delivery and biomedical applications. Ke et al. [82] discovered that the in vitro drug release kinetics of allicin from the NEs drug delivery system exhibited a delayed release under various biological pH conditions. Moreover, allicin demonstrated prolonged and sustained drug release, particularly in an inflammatory environment. However, NEs also present certain limitations, such as the potential risk of surfactant-induced toxicity and inadequate long-term stability, thereby rendering it unsuitable for serving as a carrier for sustained-release drugs over extended periods [99].
In conclusion, drug delivery strategies based on nanotechnology offer the potential to revolutionize the way allicin is administered and targeted within the body. Nevertheless, while allicin-loaded nanoformulations have demonstrated potential in treating various diseases, the cardioprotective mechanisms of allicin-based nanoformulations remain poorly understood and require further research. In the future, preclinical assessment of allicin-loaded nanoformulations in animal models could be a viable research approach to comprehend allicin’s stability and bioavailability fully. Additionally, conducting a comparative analysis of various drug delivery methods and designing targeted delivery systems can offer additional insights to enhance allicin’s therapeutic potential.
Limitations of clinical application
Finding feasible and effective natural pharmaceutical ingredients for the treatment of CVD has always been one of the most challenging issues in medical research. Due to the unsatisfactory efficacy of most existing drugs targeting various CVD, natural ingredients like allicin have emerged as a promising treatment option for CVD patients. However, the clinical application of allicin still has certain limitations. Firstly, due to the unstable chemical properties and unpredictable bioavailability of allicin, further research is needed on purification processes and preparation methods to improve its stability and pharmacological activity. Recent advances in formulation strategies and nanotechnology-based drug delivery systems show promise in addressing these challenges, potentially improving allicin’s solubility, stability, and bioavailability [100, 101]. Meanwhile, the targeting technology of nanoscale materials enabled the delivery of active ingredients to the desired action site in sufficient concentrations, enhancing their ability to get absorbed into cells. These form the rationale and potential approaches to developing innovative delivery strategies to boost the bioavailability and stability of allicin [102].
Secondly, while various researchers have targeted several signalling pathways to investigate the mechanism behind the cardiovascular protective efficacy of allicin, additional research is still required to comprehend these molecular targets of allicin inside diverse CVD fully. Furthermore, despite promising preclinical research on the cardioprotective potential of garlic components, the paucity of well-studied, potent clinical studies and thorough safety assessments increases the desire for additional clinical research [103]. Therefore, to ensure the safety and efficacy of allicin in preventing and treating CVD and to better understand its effects, it is imperative to conduct large-scale randomized clinical trials and further basic research.
Conclusions
CVD severely threatens human health. These diseases may be alleviated with ingredients derived from natural medicines. Allicin is a natural bioactive compound with cardioprotective effects, especially anti-inflammatory, anti-apoptotic, and anti-oxidative stress effects through multi-targets and multi-mechanisms. Although it has shown promising potential in the treatment of numerous CVDs such as atherosclerosis, myocardial infarction, hypertension, heart failure, arrhythmias, cardiac hypertrophy, myocardial fibrosis, and cardiotoxicity, further studies and trials are required to validate the beneficial treatment of allicin in CVD which have not been exhaustively examined. More importantly, the problems of instability, poor bioavailability, and irritating odor are supposed to be resolved in future experimental studies. Several novel delivery systems for allicin have been developed, ensuring high stability, loading capacity, and bioavailability. Future research should prioritize the development of delivery systems with high loading capacities for allicin while maintaining a precisely targeted therapy for CVD. Overall, allicin is a prospective choice for treating CVD and will likely be used to prevent and manage CVD in the future.
Availability of data and materials
Not applicable.
Abbreviations
- ACEIs:
-
Angiotensin-converting enzyme inhibitors
- ApoE:
-
Apolipoprotein E-deficient
- Ang II:
-
Angiotensin II
- AS:
-
Atherosclerosis
- AT2R:
-
Angiotensin II receptor type 2
- BNP:
-
Brain natriuretic peptide
- CAT:
-
Catalase
- CCBs:
-
Calcium channel blockers
- CH:
-
Cardiac hypertrophy
- cIMT:
-
Carotid intima-media thickness
- DAMPs:
-
Damage-associated molecular patterns
- DDS:
-
Diallyl disulfide
- DOX:
-
Doxorubicin
- DTS:
-
Diallyl trisulfide
- eNOS:
-
Endothelial nitric oxide synthase
- GSH-Px:
-
Glutathione peroxidase
- H2O2 :
-
Hydrogen peroxide
- H2S:
-
Hydrogen sulfide
- Hcy:
-
Homocysteine
- HF:
-
Heart failure
- HR:
-
Hypoxia-reoxygenation
- IL-6:
-
Interleukin-6
- JNK:
-
Jun N-terminal kinase
- LDL-C:
-
Low-density lipoprotein cholesterol
- LDLR:
-
Low-density lipoprotein receptor
- LXRα:
-
Liver X receptor alpha
- MDA:
-
Malondialdehyde
- mTOR:
-
Mammalian target of rapamycin
- MI:
-
Myocardial infarction
- MI/R:
-
Myocardial ischemia–reperfusion
- MTX:
-
Methotrexate
- NF-κB:
-
Nuclear factor kappa B
- NLRP3:
-
NOD-like receptor pyrin domain-containing protein 3
- NO-sGC-cGMP:
-
NO-soluble guanylate cyclase-cyclic guanosine monophosphate
- PCSK9:
-
Proprotein convertase subtilisin/kexin type 9
- PGI2-AC-cAMP:
-
Prostacyclin-adenylyl cyclase-cyclic adenosine monophosphate
- PPARγ:
-
Peroxisome proliferator-activated receptor γ
- Prx:
-
Peroxidase
- ROS:
-
Reactive oxygen speciesc
- SAC:
-
S-allyl cysteine
- SOD:
-
Superoxide dismutase
- SREBP2:
-
Sterol regulatory element binding proteins 2
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- TGF-β:
-
Transforming growth factor-β
- TLR4:
-
Toll-like receptor 4
- TMAO:
-
Trimethylamine-N-oxide
- TNF-α:
-
Tumor necrosis factor-alpha
References
Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145(8):e153–639.
Vaduganathan M, Mensah GA, Turco JV, Fuster V, Roth GA. The global burden of cardiovascular diseases and risk: a compass for future health. J Am Coll Cardiol. 2022;80(25):2361–71.
Tudu CK, Dutta T, Ghorai M, Biswas P, Samanta D, Oleksak P, et al. Traditional uses, phytochemistry, pharmacology and toxicology of garlic (Allium sativum), a storehouse of diverse phytochemicals: a review of research from the last decade focusing on health and nutritional implications. Front Nutr. 2022;9: 949554.
Wlosinska M, Nilsson AC, Hlebowicz J, Hauggaard A, Kjellin M, Fakhro M, et al. The effect of aged garlic extract on the atherosclerotic process—a randomized double-blind placebo-controlled trial. BMC Complement Med Ther. 2020;20(1):132.
Schwingshackl L, Missbach B, Hoffmann G. An umbrella review of garlic intake and risk of cardiovascular disease. Phytomed Int J Phytother Phytopharmacol. 2016;23(11):1127–33.
Borlinghaus J, Albrecht F, Gruhlke MC, Nwachukwu ID, Slusarenko AJ. Allicin: chemistry and biological properties. Molecules. 2014;19(8):12591–618.
Sánchez-Gloria JL, Arellano-Buendía AS, Juárez-Rojas JG, García-Arroyo FE, Argüello-García R, Sánchez-Muñoz F, et al. Cellular mechanisms underlying the cardioprotective role of allicin on cardiovascular diseases. Int J Mol Sci. 2022;23(16):9082.
Verma T, Aggarwal A, Dey P, Chauhan AK, Rashid S, Chen KT, et al. Medicinal and therapeutic properties of garlic, garlic essential oil, and garlic-based snack food: an updated review. Front Nutr. 2023;10:1120377.
Fujisawa H, Suma K, Origuchi K, Seki T, Ariga T. Thermostability of allicin determined by chemical and biological assays. Biosci Biotechnol Biochem. 2008;72(11):2877–83.
Wang H, Li X, Liu X, Shen D, Qiu Y, Zhang X, et al. Influence of pH, concentration and light on stability of allicin in garlic (Allium sativum L.) aqueous extract as measured by UPLC. J Sci Food Agric. 2015;95(9):1838–44.
Fry FH, Okarter N, Baynton-Smith C, Kershaw MJ, Talbot NJ, Jacob C. Use of a substrate/alliinase combination to generate antifungal activity in situ. J Agric Food Chem. 2005;53(3):574–80.
Li F, Li Q, Wu S, Tan Z. Salting-out extraction of allicin from garlic (Allium sativum L.) based on ethanol/ammonium sulfate in laboratory and pilot scale. Food Chem. 2017;217:91–7.
Figueiredo CS, Roseira ES, Viana TT, Silveira MAD, de Melo RMV, Fernandez MG, et al. Inflammation in coronary atherosclerosis: insights into pathogenesis and therapeutic potential of anti-inflammatory drugs. Pharmaceuticals. 2023;16(9):1242.
Ong SB, Hernández-Reséndiz S, Crespo-Avilan GE, Mukhametshina RT, Kwek XY, Cabrera-Fuentes HA, et al. Inflammation following acute myocardial infarction: multiple players, dynamic roles, and novel therapeutic opportunities. Pharmacol Ther. 2018;186:73–87.
Hitchcock JK, Mkwanazi N, Barnett C, Graham LM, Katz AA, Hunter R, et al. The garlic compound Z-ajoene, S-thiolates COX2 and STAT3 and dampens the inflammatory response in RAW264.7 macrophages. Mol Nutr Food Res. 2021;65(3): e2000854.
Liu S, He Y, Shi J, Liu L, Ma H, He L, et al. Allicin attenuates myocardial ischemia reperfusion injury in rats by inhibition of inflammation and oxidative stress. Transplant Proc. 2019;51(6):2060–5.
Abdel-Daim MM, Kilany OE, Khalifa HA, Ahmed AAM. Allicin ameliorates doxorubicin-induced cardiotoxicity in rats via suppression of oxidative stress, inflammation and apoptosis. Cancer Chemother Pharmacol. 2017;80(4):745–53.
Zhang Z, Chen F, Wan J, Liu X. Potential traditional Chinese medicines with anti-inflammation in the prevention of heart failure following myocardial infarction. Chin Med. 2023;18(1):28.
Kong L, Ji X, Liu Y, Du Y. Effect of artemisinin combined with allicin on improving cardiac function, fibrosis and NF-κB signaling pathway in rats with diabetic cardiomyopathy. Acta Biochim Pol. 2023;70(2):401–5.
Weinreuter M, Kreusser MM, Beckendorf J, Schreiter FC, Leuschner F, Lehmann LH, et al. CaM Kinase II mediates maladaptive post-infarct remodeling and pro-inflammatory chemoattractant signaling but not acute myocardial ischemia/reperfusion injury. EMBO Mol Med. 2014;6(10):1231–45.
Suetomi T, Willeford A, Brand CS, Cho Y, Ross RS, Miyamoto S, et al. Inflammation and NLRP3 inflammasome activation initiated in response to pressure overload by Ca(2+)/calmodulin-dependent protein kinase II δ signaling in cardiomyocytes are essential for adverse cardiac remodeling. Circulation. 2018;138(22):2530–44.
Toldo S, Abbate A. The role of the NLRP3 inflammasome and pyroptosis in cardiovascular diseases. Nat Rev Cardiol. 2023;21(4):219–37.
Liu W, Xu S, Liang S, Duan C, Xu Z, Zhao L, et al. Hypertensive vascular and cardiac remodeling protection by allicin in spontaneous hypertension rats via CaMKII/NF-κB pathway. Biomed Pharmacother. 2022;155: 113802.
Liu C, Cao F, Tang QZ, Yan L, Dong YG, Zhu LH, et al. Allicin protects against cardiac hypertrophy and fibrosis via attenuating reactive oxygen species-dependent signaling pathways. J Nutr Biochem. 2010;21(12):1238–50.
Sun F, Xu K, Zhou J, Zhang W, Duan G, Lei M. Allicin protects against LPS-induced cardiomyocyte injury by activating Nrf2-HO-1 and inhibiting NLRP3 pathways. BMC Cardiovasc Disord. 2023;23(1):410.
Vekic J, Stromsnes K, Mazzalai S, Zeljkovic A, Rizzo M, Gambini J. Oxidative stress, atherogenic dyslipidemia, and cardiovascular risk. Biomedicines. 2023;11(11):2897.
Yan Q, Liu S, Sun Y, Chen C, Yang S, Lin M, et al. Targeting oxidative stress as a preventive and therapeutic approach for cardiovascular disease. J Transl Med. 2023;21(1):519.
Chan JY, Tsui HT, Chung IY, Chan RY, Kwan YW, Chan SW. Allicin protects rat cardiomyoblasts (H9c2 cells) from hydrogen peroxide-induced oxidative injury through inhibiting the generation of intracellular reactive oxygen species. Int J Food Sci Nutr. 2014;65(7):868–73.
Wang SL, Liu DS, Liang ES, Gao YH, Cui Y, Liu YZ, et al. Protective effect of allicin on high glucose/hypoxia-induced aortic endothelial cells via reduction of oxidative stress. Exp Ther Med. 2015;10(4):1394–400.
Dieterich S, Bieligk U, Beulich K, Hasenfuss G, Prestle J. Gene expression of antioxidative enzymes in the human heart: increased expression of catalase in the end-stage failing heart. Circulation. 2000;101(1):33–9.
El-Sheakh AR, Ghoneim HA, Suddek GM, Ammar ESM. Attenuation of oxidative stress, inflammation, and endothelial dysfunction in hypercholesterolemic rabbits by allicin. Can J Physiol Pharmacol. 2016;94(2):216–24.
Lv R, Du L, Lu C, Wu J, Ding M, Wang C, et al. Allicin protects against H2O2-induced apoptosis of PC12 cells via the mitochondrial pathway. Exp Ther Med. 2017;14(3):2053–9.
Deng X, Yang P, Gao T, Liu M, Li X. Allicin attenuates myocardial apoptosis, inflammation and mitochondrial injury during hypoxia-reoxygenation: an in vitro study. BMC Cardiovasc Disord. 2021;21(1):200.
Kuo WW, Wang WJ, Tsai CY, Way CL, Hsu HH, Chen LM. Diallyl trisufide (DATS) suppresses high glucose-induced cardiomyocyte apoptosis by inhibiting JNK/NFκB signaling via attenuating ROS generation. Int J Cardiol. 2013;168(1):270–80.
Ma LN, Li LD, Li SC, Hao XM, Zhang JY, He P, et al. Allicin improves cardiac function by protecting against apoptosis in rat model of myocardial infarction. Chin J Integr Med. 2017;23(8):589–97.
Xu W, Li XP, Li EZ, Liu YF, Zhao J, Wei LN, et al. Protective effects of allicin on ISO-induced rat model of myocardial infarction via JNK signaling pathway. Pharmacology. 2020;105(9–10):505–13.
Aboubakr M, Farag A, Elfadadny A, Alkafafy M, Soliman A, Elbadawy M. Antioxidant and anti-apoptotic potency of allicin and lycopene against methotrexate-induced cardiac injury in rats. Environ Sci Pollut Res Int. 2023;30(38):88724–33.
Popa-Fotea NM, Ferdoschi CE, Micheu MM. Molecular and cellular mechanisms of inflammation in atherosclerosis. Front Cardiovasc Med. 2023;10:1200341.
Kannar D, Wattanapenpaiboon N, Savige GS, Wahlqvist ML. Hypocholesterolemic effect of an enteric-coated garlic supplement. J Am Coll Nutr. 2001;20(3):225–31.
Lu Y, He Z, Shen X, Xu X, Fan J, Wu S, et al. Cholesterol-lowering effect of allicin on hypercholesterolemic ICR mice. Oxid Med Cell Longev. 2012;2012: 489690.
Lin XL, Hu HJ, Liu YB, Hu XM, Fan XJ, Zou WW, et al. Allicin induces the upregulation of ABCA1 expression via PPARγ/LXRα signaling in THP-1 macrophage-derived foam cells. Int J Mol Med. 2017;39(6):1452–60.
Nawaka N, Wanmasae S, Makarasen A, Dechtrirat D, Techasakul S, Jeenduang N. Allicin and capsaicin ameliorated hypercholesterolemia by upregulating LDLR and downregulating PCSK9 expression in HepG2 cells. Int J Mol Sci. 2022;23(22):14299.
Liu DS, Wang SL, Li JM, Liang ES, Yan MZ, Gao W. Allicin improves carotid artery intima-media thickness in coronary artery disease patients with hyperhomocysteinemia. Exp Ther Med. 2017;14(2):1722–6.
ElHage R, Al-Arawe N, Hinterseher I. The role of the gut microbiome and trimethylamine oxide in atherosclerosis and age-related disease. Int J Mol Sci. 2023;24(3):2399.
Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013;368(17):1575–84.
Schiattarella GG, Sannino A, Toscano E, Giugliano G, Gargiulo G, Franzone A, et al. Gut microbe-generated metabolite trimethylamine-N-oxide as cardiovascular risk biomarker: a systematic review and dose-response meta-analysis. Eur Heart J. 2017;38(39):2948–56.
Cao H, Zhu Y, Hu G, Zhang Q, Zheng L. Gut microbiome and metabolites, the future direction of diagnosis and treatment of atherosclerosis? Pharmacol Res. 2023;187: 106586.
Panyod S, Wu WK, Chen PC, Chong KV, Yang YT, Chuang HL, et al. Atherosclerosis amelioration by allicin in raw garlic through gut microbiota and trimethylamine-N-oxide modulation. NPJ Biofilms Microbiomes. 2022;8(1):4.
Sen L, Zuo SJ, Cao L, Liu DZ, Zhang SQ, Cao YX. Vasodilation and hypotension of a novel 3-benzylquinazolin- 4(3H)-one derivative via the inhibition of calcium flux. Eur J Pharmacol. 2016;791:741–50.
Elkayam A, Peleg E, Grossman E, Shabtay Z, Sharabi Y. Effects of allicin on cardiovascular risk factors in spontaneously hypertensive rats. Israel Med Assoc J. 2013;15(3):170–3.
García Trejo E, Arellano Buendía AS, Sánchez Reyes O, García Arroyo FE, Arguello García R, Loredo Mendoza ML, et al. The beneficial effects of allicin in chronic kidney disease are comparable to losartan. Int J Mol Sci. 2017;18(9):1980.
Bradley JM, Organ CL, Lefer DJ. Garlic-derived organic polysulfides and myocardial protection. J Nutr. 2016;146(2):403s-s409.
Kanagy NL, Szabo C, Papapetropoulos A. Vascular biology of hydrogen sulfide. Am J Physiol Cell Physiol. 2017;312(5):C537–49.
Cui T, Liu W, Chen S, Yu C, Li Y, Zhang JY. Antihypertensive effects of allicin on spontaneously hypertensive rats via vasorelaxation and hydrogen sulfide mechanisms. Biomed Pharmacother = Biomedecine & pharmacotherapie. 2020;128: 110240.
Brown IAM, Diederich L, Good ME, DeLalio LJ, Murphy SA, Cortese-Krott MM, et al. Vascular smooth muscle remodeling in conductive and resistance arteries in hypertension. Arterioscler Thromb Vasc Biol. 2018;38(9):1969–85.
Teringova E, Tousek P. Apoptosis in ischemic heart disease. J Transl Med. 2017;15(1):87.
Cui T, Liu W, Yu C, Ren J, Li Y, Shi X, et al. Protective effects of allicin on acute myocardial infarction in rats via hydrogen sulfide-mediated regulation of coronary arterial vasomotor function and myocardial calcium transport. Front Pharmacol. 2021;12: 752244.
Gao T, Yang P, Fu D, Liu M, Deng X, Shao M, et al. The protective effect of allicin on myocardial ischemia-reperfusion by inhibition of Ca(2+) overload-induced cardiomyocyte apoptosis via the PI3K/GRK2/PLC-γ/IP3R signaling pathway. Aging. 2021;13(15):19643–56.
Liu M, Yang P, Fu D, Gao T, Deng X, Shao M, et al. Allicin protects against myocardial I/R by accelerating angiogenesis via the miR-19a-3p/PI3K/AKT axis. Aging. 2021;13(19):22843–55.
Martin TG, Juarros MA, Leinwand LA. Regression of cardiac hypertrophy in health and disease: mechanisms and therapeutic potential. Nat Rev Cardiol. 2023;20(5):347–63.
Ramachandra CJA, Cong S, Chan X, Yap EP, Yu F, Hausenloy DJ. Oxidative stress in cardiac hypertrophy: from molecular mechanisms to novel therapeutic targets. Free Radic Biol Med. 2021;166:297–312.
Li XH, Li CY, Xiang ZG, Hu JJ, Lu JM, Tian RB, et al. Allicin ameliorates cardiac hypertrophy and fibrosis through enhancing of Nrf2 antioxidant signaling pathways. Cardiovasc Drugs Ther. 2012;26(6):457–65.
Ba L, Gao J, Chen Y, Qi H, Dong C, Pan H, et al. Allicin attenuates pathological cardiac hypertrophy by inhibiting autophagy via activation of PI3K/Akt/mTOR and MAPK/ERK/mTOR signaling pathways. Phytomed Int J Phytother Phytopharmacol. 2019;58: 152765.
Shi P, Cao Y, Gao J, Fu B, Ren J, Ba L, et al. Allicin improves the function of cardiac microvascular endothelial cells by increasing PECAM-1 in rats with cardiac hypertrophy. Phytomed Int J Phytother Phytopharmacol. 2018;51:241–54.
Heymans S, González A, Pizard A, Papageorgiou AP, López-Andrés N, Jaisser F, et al. Searching for new mechanisms of myocardial fibrosis with diagnostic and/or therapeutic potential. Eur J Heart Fail. 2015;17(8):764–71.
Li C, Meng X, Wang L, Dai X. Mechanism of action of non-coding RNAs and traditional Chinese medicine in myocardial fibrosis: focus on the TGF-β/Smad signaling pathway. Front Pharmacol. 2023;14:1092148.
Li SC, Ma LN, Chen J, Li YK. Effect of allicin on myocardial fibrosis after myocardial infarction in rats and its relationship with TGFβ/Smads signal transduction. Zhongguo Zhong yao za zhi = Zhongguo zhongyao zazhi = China J Chin Mater Med. 2016;41(13):2517–21.
Liu Y, Qi H, Wang Y, Wu M, Cao Y, Huang W, et al. Allicin protects against myocardial apoptosis and fibrosis in streptozotocin-induced diabetic rats. Phytomed Int J Phytother Phytopharmacol. 2012;19(8–9):693–8.
Yin C, Ye Z, Wu J, Huang C, Pan L, Ding H, et al. Elevated Wnt2 and Wnt4 activate NF-κB signaling to promote cardiac fibrosis by cooperation of Fzd4/2 and LRP6 following myocardial infarction. EBioMedicine. 2021;74: 103745.
Yan Z, Zhong L, Zhu W, Chung SK, Hou P. Chinese herbal medicine for the treatment of cardiovascular diseases—targeting cardiac ion channels. Pharmacol Res. 2023;192: 106765.
Banerjee SK, Maulik SK. Effect of garlic on cardiovascular disorders: a review. Nutr J. 2002;1:4.
Deng CY, Rao F, Kuang SJ, Wu SL, Shan ZX, Li XH, et al. Allitridi inhibits transient outward potassium currents in human atrial myocytes. Clin Exp Pharmacol Physiol. 2011;38(5):323–7.
Cao H, Huang C, Wang X. Allicin inhibits transient outward potassium currents in mouse ventricular myocytes. Exp Ther Med. 2016;11(5):1896–900.
Qu Z, Xie LH, Olcese R, Karagueuzian HS, Chen PS, Garfinkel A, et al. Early afterdepolarizations in cardiac myocytes: beyond reduced repolarization reserve. Cardiovasc Res. 2013;99(1):6–15.
Han D, Xu L, Liu P, Liu Y, Sun C, Yin Y. Allicin disrupts cardiac Cav1.2 channels via trafficking. Pharm Biol. 2019;57(1):245–9.
Chen Y, Huang Y, Bai J, Liu C, Ma S, Li J, et al. Effects of allicin on late sodium current caused by ΔKPQ-SCN5A mutation in HEK293 cells. Front Physiol. 2021;12: 636485.
Graffagnino J, Kondapalli L, Arora G, Hawi R, Lenneman CG. Strategies to prevent cardiotoxicity. Curr Treat Options Oncol. 2020;21(4):32.
Mousa AM, Soliman KEA, Alhumaydhi FA, Almatroudi A, Allemailem KS, Alsahli MA, et al. Could allicin alleviate trastuzumab-induced cardiotoxicity in a rat model through antioxidant, anti-inflammatory, and antihyperlipidemic properties? Life Sci. 2022;302: 120656.
Al-Thubiani WS, Abuzinadah OAH, El-Aziz GSA. Betanin and allicin ameliorate adriamycin-induced cardiotoxicity in rats by ameliorating cardiac ischemia and improving antioxidant efficiency. J Pharm Res Int. 2021;33(7):39–56.
Leontiev R, Hohaus N, Jacob C, Gruhlke MCH, Slusarenko AJ. A comparison of the antibacterial and antifungal activities of thiosulfinate analogues of allicin. Sci Rep. 2018;8(1):6763.
El-SaberBatiha G, MagdyBeshbishy A, Wasef LG, Elewa YH, Al-Sagan AA, AbdEl-Hack ME, et al. Chemical constituents and pharmacological activities of garlic (Allium sativum L.): a review. Nutrients. 2020;12(3):872.
Phan KS, Nguyen TM, To XT, Le TTH, Nguyen TT, Pham KD, et al. Allium sativum@AgNPs and Phyllanthus urinaria@AgNPs: a comparative analysis for antibacterial application. RSC Adv. 2022;12(55):35730–43.
Pinilla CM, Noreña CP, Brandelli A. Development and characterization of phosphatidylcholine nanovesicles, containing garlic extract, with antilisterial activity in milk. Food Chem. 2017;220:470–6.
Han X, Lu B, Zou D, Luo X, Liu L, Maitz MF, et al. Allicin-loaded intelligent hydrogel coating improving vascular implant performance. ACS Appl Mater Interfaces. 2023;15(32):38247–63.
Ossama M, Hathout RM, Attia DA, Mortada ND. Augmented cytotoxicity using the physical adsorption of Poloxamer 188 on allicin-loaded gelatin nanoparticles. J Pharm Pharmacol. 2021;73(5):664–72.
Chen X, He X, Gao R, Lan X, Zhu L, Chen K, et al. Aptamer-functionalized binary-drug delivery system for synergetic obesity therapy. ACS Nano. 2022;16(1):1036–50.
Deng Y, Ho CT, Lan Y, Xiao J, Lu M. Bioavailability, health benefits, and delivery systems of allicin: a review. J Agric Food Chem. 2023;71(49):19207–20.
Mohamed NA, Marei I, Crovella S, Abou-Saleh H. Recent developments in nanomaterials-based drug delivery and upgrading treatment of cardiovascular diseases. Int J Mol Sci. 2022;23(3):1404.
Abid J, Khalil FMA, Saeed S, Khan SU, Iqbal I, Khan SU, et al. Nano revolution in cardiovascular health: nanoparticles (NPs) as tiny titans for diagnosis and therapeutics. Curr Probl Cardiol. 2024;49(5): 102466.
Hashemy SI, Amiri H, Hosseini H, Sadeghzadeh F, Jaseem MMM, Tabrizi MH. PEGylated lecithin-chitosan-folic acid nanoparticles as nanocarriers of allicin for in vitro controlled release and anticancer effects. Appl Biochem Biotechnol. 2023;195(7):4036–52.
Liu P, Chen G, Zhang J. A review of liposomes as a drug delivery system: current status of approved products, regulatory environments, and future perspectives. Molecules. 2022;27(4):1372.
Guimarães D, Cavaco-Paulo A, Nogueira E. Design of liposomes as drug delivery system for therapeutic applications. Int J Pharm. 2021;601: 120571.
Al-Jamal WT, Kostarelos K. Liposomes: from a clinically established drug delivery system to a nanoparticle platform for theranostic nanomedicine. Acc Chem Res. 2011;44(10):1094–104.
Kharkar PM, Kiick KL, Kloxin AM. Designing degradable hydrogels for orthogonal control of cell microenvironments. Chem Soc Rev. 2013;42(17):7335–72.
Koetting MC, Peters JT, Steichen SD, Peppas NA. Stimulus-responsive hydrogels: theory, modern advances, and applications. Mater Sci Eng R Rep. 2015;93:1–49.
Xu Q, Xiao Z, Yang Q, Yu T, Deng X, Chen N, et al. Hydrogel-based cardiac repair and regeneration function in the treatment of myocardial infarction. Mater Today Bio. 2024;25: 100978.
Zhang J, Guo Y, Bai Y, Wei Y. Application of biomedical materials in the diagnosis and treatment of myocardial infarction. J Nanobiotechnol. 2023;21(1):298.
Yukuyama MN, Kato ET, Lobenberg R, Bou-Chacra NA. Challenges and future prospects of nanoemulsion as a drug delivery system. Curr Pharm Des. 2017;23(3):495–508.
Liang CX, Qi DL, Zhang LN, Lu P, Liu ZD. Preparation and evaluation of a water-in-oil nanoemulsion drug delivery system loaded with salidroside. Chin J Nat Med. 2021;19(3):231–40.
Lu X, Wang C, Zhao M, Wu J, Niu Z, Zhang X, et al. Improving the bioavailability and bioactivity of garlic bioactive compounds via nanotechnology. Crit Rev Food Sci Nutr. 2022;62(30):8467–96.
Bala R, Madaan R, Chauhan S, Gupta M, Dubey AK, Zahoor I, et al. Revitalizing allicin for cancer therapy: advances in formulation strategies to enhance bioavailability, stability, and clinical efficacy. Naunyn Schmiedebergs Arch Pharmacol. 2023;397(2):703–24.
Pandey P, Khan F, Alshammari N, Saeed A, Aqil F, Saeed M. Updates on the anticancer potential of garlic organosulfur compounds and their nanoformulations: plant therapeutics in cancer management. Front Pharmacol. 2023;14:1154034.
Lawson LD, Hunsaker SM. Allicin bioavailability and bioequivalence from garlic supplements and garlic foods. Nutrients. 2018;10(7):812.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China, Grant Number 82274331.
Author information
Authors and Affiliations
Contributions
Y.G. performed conceptualization and design; investigation, data curation, and writing were performed by B.W., G.Q., S.L., J.Y., H.J., M.L.; validation, review, and editing were performed by X.L. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gao, Y., Wang, B., Qin, G. et al. Therapeutic potentials of allicin in cardiovascular disease: advances and future directions. Chin Med 19, 93 (2024). https://doi.org/10.1186/s13020-024-00936-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13020-024-00936-8