Abstract
Honokiol is a neolignan biphenol found in aerial parts of the Magnolia plant species. The Magnolia plant species traditionally belong to China and have been used for centuries to treat many pathological conditions. Honokiol mitigates the severity of several pathological conditions and has the potential to work as an anti-inflammatory, anti-angiogenic, anticancer, antioxidant, and neurotherapeutic agent. It has a long history of being employed in the healthcare practices of Southeast Asia, but in recent years, a greater scope of research has been conducted on it. Plenty of experimental evidence suggests it could be beneficial as a neuroprotective bioactive molecule. Honokiol has several pharmacological effects, leading to its exploration as a potential therapy for neurological diseases (NDs), including Alzheimer's disease (AD), Parkinson’s disease (PD), cerebral ischemia, anxiety, depression, spinal cord injury, and so on. So, based on the previous experimentation reports, our goal is to discuss the neuroprotective properties of honokiol. Besides, honokiol derivatives have been highlighted recently as possible therapeutic options for NDs. So, this review focuses on honokiol's neurotherapeutic actions and toxicological profile to determine their safety and potential use in neurotherapeutics.
Similar content being viewed by others
Introduction
Neurological diseases (NDs) affects the nervous system, causing symptoms due to body composition or metabolism issues. These symptoms can result from various health issues [1, 2]. Common symptoms of non-infectious brain diseases include muscle paralysis, slurred speech, seizures, and hand numbness. These disorders can lead to NDs such as epilepsy, Alzheimer’s disease (AD), and Parkinson’s disease (PD), causing high mortality rates and cognitive impairment [3]. Aging populations are expected to increase the number of people with disabilities. Mainly, these diseases are more common in the elderly. Age-related conditions are gradually more prevalent, placing massive economic and social pressure on families and communities [4]. Patients with PD and Huntington’s disease (HD) have dopaminergic and spiny striatal neurons that control their movements. AD is characterized by a drop in the brain’s total volume. A condition that affects the nervous system can damage the brain's neuron count. However, to this point, there is still a lack of effective therapeutics for devastating brain disorders. In this regard, the attempt to discover novel, effective molecules should be a crucial research goal [5, 6].
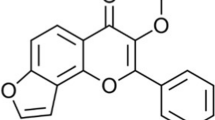
Honokiol (3',5-di-(2-propenyl)-1,1'-biphenyl-2,4'-diol) is a phenylpropanoid molecule that belongs to the category of neolignans. Neolignans belong to a group of plant-based phytochemicals similar to lignans. The shikimic acid pathway can be followed to proceed with the biosynthetic procedures. It contains a para-allyl-phenol and an ortho-, ortho-allyl-phenol linked through a para-C–C coupling [7, 8]. In Asian regions, honokiol is a commonly used ingredient in homeopathic medicine. The potential source of honokiol may be Magnolia Officinalis, which is generally grown in China. Raw materials from Magnolia tree bark, seed cones, and leaves are necessary to extract the lignan honokiol in various plant parts successfully. Honokiol is often used as an effective therapeutics for several medical conditions [9]. The anxiolytic, analgesic, depressive, antithrombotic, antibacterial, antispasmodic, anti-tumorigenic, and neuroprotective effects of honokiol are well-known [10, 11].
Honokiol is a polyphenolic compound with a small molecular size. Its high lipophilicity enables it to cross the blood brain barrier (BBB) and blood-cerebrospinal fluid (CSF) barrier easily. Currently, many research reports indicate that it exhibits significant neuroprotective properties in several animal models of central nervous system (CNS) disorders, such as spinal cord injury, epilepsy, cerebrovascular injury, anxiety, and cognitive disorders. This is attributable to its ability to prevent oxidative damage and neural excitotoxicity, mitigate neuroinflammation, and regulate the functioning of mitochondria [3, 10, 12, 13]. As per a study, honokiol effectively treats PD neuronal and motor impairments by reducing oxidative damage and inflammation, improving overall health [14].
Furthermore, honokiol has been demonstrated to benefit cognitive functioning in APP/PS1 by mitigating mitochondrial damage [13, 15]. The administration of honokiol was found to mitigate cerebral edema and neurobehavioral impairments following subarachnoid hemorrhage by enhancing mitochondrial fusion. This mechanism helped to maintain the structure of mitochondria, safeguard their functionality, and support the survival of neural cells. Honokiol has also been submitted for patent (200310121303.0) as a therapeutic option for ischemic stroke, and clinical trials are expected to commence in China soon [13].
It is already established that honokiol can cross the BBB, and many researchers have argued that honokiol could be a successful therapeutics for various NDs [16, 17]. The neuroprotective effects of honokiol and its derivatives have recently been under increased scrutiny. Honokiol's derivatives were focused on their neurotherapeutic effects and toxicological profile to determine if they could be less hazardous for use.
Honokiol derivatives
Several neuroprotective honokiol derivatives include acetate, glycerol, succinic acid, glucose, glycine, and mannose derivatives. These derivatives are used to develop new compounds with enhanced solubility properties. According to a study, 2- and 4'-OH groups acetylation of honokiol was accomplished by incubating the molecule in acetic anhydride in pyridine for 18 h at 25 °C. This causes the honokiol molecule to become acetylated [18, 19]. As a result, a chemical by-product, honokiol-acetate, is produced. Honokiol-succinic acid was formed by the reaction between honokiol and maleic anhydride (3,4-dihydrofuran-2,5-dion) in pyridine over honokiol-acetate at room temperature (50 °C) [20]. The honokiol-glycine derivative was synthesized by reacting honokiol with glycerol in pyridine for eight hours at 25 °C. Following the reaction of glycine with di-tertbutyl dicarbonate (di-BOC), a synthetic Boc-Gly honokiol called 1,3-diaza-1,3-dicyclohexylpropa-1,2-diene (DCC) is then reacted with triethylamine. Boc-Gly honokiol and 4-dimethyl aminopyridine (DMAP) at 40 °C for six hours. This peptide goes by no specific name. In the next step, a di-Boc on di-Boc-Gly-honokiol was removed by bubbling the EtOAc solution with dry HCl gas at room temperature for four hours. This step constituted the second part of the process. This phase is completed after the second phase [19, 21]. Besides, the processes of glycosylation and deacetylation lead to the formation of honokiol-glycine and honokiol mannose molecules. In the first step of the process, diethyl ether was used to incorporate boron trifluoride into honokiol-glucose, honokiol mannose glucose pentaacetate, and mannose pentaacetate (BF3-Et2O). This results in synthetic honokiol-β-D-tetra acetyl glucopyranoside and honokiol-β-D-tetra acetyl mannopyranoside. In the second step, sodium methoxide cleaves synthetic honokiol-β-D-tetra acetyl glucopyranoside and honokiol-β-D-tetra acetyl. Following this step, the molecule was deprotonated by passage through an Amberlite IR120 (H+) ion exchange column, yielding honokiol. Once this part of the process was complete, the structures of the newly synthesized honokiol-derivatives were determined based on 1H-and 13C-NMR spectrum data collected from those compounds [8, 19, 22, 23].
Besides, many experimental studies reported enormous honokiol derivatives with better therapeutic efficacy [24,25,26,27,28]. For example, experimental investigations were performed on the bark portion of M. officinalis and a total of four novel derivatives of honokiol were successfully isolated, namely (1) 8′,9′-dihydroxymagnaldehyde E, (2) 8′, 9′-dihydroxy Honokiol, (3) erythro-7-O-methylhonokitriol, and (4) threo-7-O-methylhonokitriol. Detailed 1D and 2D NMR investigations and HR-MS analysis served as a base for developing their molecular structures [29].
In another experiment, 4-o-methyl honokiol has gone through synthetic modifications. The experimental findings have been attributed to synthesizing of 31 neolignan honokiol analogs. Xenopus oocytes were used as a model system to investigate how the synthetic analogs work on the GABAA receptors. Honokiol increased chloride currents across receptors expressing GABAA, with EC50 concentrations that ranged from 23.4 μM to 59.6 μM in 7 distinct subunit compositions. The researchers have developed GABAA receptor modulators that exhibit remarkable subtype-selectivity by selectively modifying crucial functions of honokiol, such as its phenolic group, side chains, polarity, and ring positions for substitutions. Compounds composed of amino groups are a newly identified class of GABAA receptor modifiers that exhibit high potency and efficacy. Within this class, several potential lead candidates show promising benefits. The majority of synthetic analogs have yet to be documented. The efficacy of compounds 26 and 31 was approximately 10 times greater than honokiol’s effect [30].
Structural-activity relationship (SAR)
Honokiol, a naturally occurring bioactive substance in magnolia tree bark, has potential therapeutic benefits such as anti-inflammatory, antioxidant, neuroprotective, and anticancer actions. Researchers have investigated its derivatives to improve their pharmacological characteristics and maximize their action. The structural-activity relationship (SAR) of honokiol and its derivatives consists of numerous hydroxyl (-OH) groups that support its antioxidant and free radical scavenging properties [31, 32]. The absorption and distribution of a molecule within a cell can be influenced by its lipophilicity, which is the degree to which it can dissolve in lipid-based environments. Changes to honokiol derivatives’ alkyl or aryl groups can affect their lipophilicity and bioavailability [33]. The biological effects of honokiols can alter when functional groups such as methyl, ethyl, halogen, or amino groups are added to the compound’s structure. For example, adding electron-donating groups may improve its antioxidant properties [31]. The biphenolic structure of honokiol is essential for its biological function, and interactions with biological targets and receptors can be altered by changing the rings or adding fused ring systems [34]. These results allow for innovative novel honokiol compounds with enhanced biological activity. For example, honokiol can improve its solubility and bioavailability by changing its propyl group to a more hydrophobic one [31]. Research on honokiol and its derivatives has shown its versatility in targeting various targets. They can modulate GABAA receptors, which control anxiety, pain, and seizures, and block NMDA receptors, which control pain, neurodegeneration, learning, and memory [11]. There are several potential therapeutic uses for honokiol and its derivatives, but further study is needed to fully understand their mode of action and develop secure and efficient treatments (Figs. 1, 2).
Four novel derivatives of honokiol by Zhang et al. [29]
A study on the effects of honokiol and its derivatives on GABAA receptors revealed that these compounds enhanced chloride currents [30]. The potency of these compounds varied depending on the receptor subtype, with honokiol being most potent on α3β2 receptors and 3'-acetylamino-4′-O-methylhonokiol being most potent on α2β2 receptors. Functional groups like methoxy and amino groups could improve the solubility and bioavailability of honokiol derivatives, but these modifications could also reduce their biological activity. The study focused on the SAR in terms of potency (EC50), which indicates receptor affinity. The initial study focused on aliphatic side chain modifications deriving from 4'-O-methyl honokiol (1), producing derivatives 2-8b. The study found that tetrahydro methyl-honokiol 2 was twice as active as 1, and isomerization of the double bond in ring B's side chain slightly reduced the EC50. Hydrobromination in one of the side chains significantly increased the potency of IGABA when the double bond of ring A's side chain was modified. Incorporating a nitro group as a solid electron-drawing entity into ring A resulted in marginally increased biological activity compared to honokiol. Compounds 24a and 24b displayed improved potency due to an unexpected acetylamino group introduction to 1’s side chain (Fig. 3). However, efficacy lagged behind honokiol. A reduction of 23 resulted in 3-amino-4'-o-methylhonokiol, which exhibited a twofold IGABA potentiation (2179%) within the dataset. The acetylated amine 3-n-acetylamino-4'-o-methylhonokiol emerged as a stable, long-lasting derivative with high potency and efficiency (2601%) [30]. This study provides valuable insights into the structure–activity relationship of honokiol and derivatives. The findings of this study could be used to design new compounds with improved biological activity.
Neurotherapeutic properties of honokiol
Alzheimer’s disease (AD)
AD is a progressive neurological disorder and one of the common causes of dementia in people worldwide [3]. AD can be diagnosed based on beta-amyloid (Aβ) aggregates and senile plaques in the cerebral cortex and hippocampus. Abnormal production and accumulation lead to irreversible neuronal cell death [35]. A primary goal of AD research in the modern era is to improve the cellular breakdown system to eliminate Aβ and inflammation as promptly and efficiently as possible. PPAR-γ, known as peroxisome proliferator-activated receptor-β, is the most prominent transcription factor in the ligand-activated nuclear receptor superfamily [36, 37]. There is mounting evidence that PPAR-γ modulates microglia in healthy and diseased states. In addition, PPAR-γ is identified as a therapeutic target for AD. First, PPAR-γ activation increases the expression of its target genes, LXR, CD36, and SRA, and this increase is dose-dependent [38]. By increasing CD36 expression, microglia acquire a more remarkable ability to phagocytose Aβ. Activation of genes such as ABCA1 and ApoE by the transcription factor LXR is a means by which Aβ can be efficiently removed from microglia. An additional effect of PPAR-γ activation is that it interacts with other transcription factors, reducing the amount of DNA binding activity that nuclear factor kappa-B (NF-kB) can [39]. The action of E3 ligase, which PPAR-β regulates, ultimately leads to the degradation of NF-kB/p65. Aβ ubiquitous transcription factor known as NF-kB is responsible for the transcription of various cytokines that promote inflammation. Oxidative stress (OS) is caused by the inappropriate folding of antibodies, which are essential for mitochondrial membrane potential. Sirtuin-3 (SIRT3) degradation activity helps ensure this anomaly does not occur [39, 40]. It has been demonstrated that an essential function of SIRT3 is to protect neurons against excitotoxicity. In the past, the only way to increase SIRT3 levels was to adhere to a strict calorie restriction plan and engage in endurance activity [40, 41]. Plenty of experiments reported that honokiol could be a good choice.
Honokiol has been identified as a potent activator of SIRT3, demonstrating antioxidant properties and enhancing the functioning of mitochondria across multiple experimental designs. Recent evidence indicates that SIRT3 is crucial in advancing various metabolic processes and neurodegenerative ailments. People with AD have an accumulation of Aβ, which is the prelude of extracellular senile plaques, in their brains. This accumulation is associated with a progression of cognitive dysfunction and the loss of neural cells. Aβ is produced via a series of proteolytic cleavages of Aβ precursor protein (APP), initially by β-secretase followed by γ-secretase. Pharmaceutical agents that regulate this particular pathway are widely considered to be among the most promising approaches to the medical management of AD. Ramesh et al. [42] found that honokiol, a compound with the APP and Presenilin PS1 mutation, affected Chinese Hamster Ovary (CHO) cells. They found that honokiol stimulated the expression of SIRT3, reduced reactive oxygen species (ROS) generation, improved antioxidant properties, and increased mitochondrial functionality. This led to a reduction in Aβ and sAPPβ levels.
The study found that honokiol did not affect APP protein concentrations or α-secretase function. Instead, it enhanced AMPK, CREB, and PGC-1α expression, inhibiting β-secretase activity and decreasing Aβ levels. This suggests that honokiol has SIRT3 activator properties, enhancing antioxidant function and controlling mitochondrial energy. This makes it a promising candidate for AD drug development [42]. According to the findings of Wang and colleagues, giving honokiol intraperitoneally to APPswe/PS1dE9 transgenic mice at a dose of 20 mg/kg/day for six weeks significantly restored their spatial memory deficiencies. The study found that honokiol significantly reduced the production of Aβ and the deposition of senile plaques. This was achieved through the downregulation of β-site precursor protein for amyloid cleavage enzyme 1 and the enhancement of Aβ phagocytosis by microglia. The administration of honokiol decreased the activation of glial cells and reduced the synthesis of pro-inflammatory cytokines, including tumor necrosis factor alpha (TNF-α), IL-1β, and IL-6 (Fig. 4). The transcriptional functions and protein concentrations of PPARγ were enhanced by honokiol. The advantageous effects associated with honokiol on pathological alterations, encompassing biochemistry and cognitive function, were found to be impeded by GW9662, a particular PPARγ inhibitor. The results of this study indicate that honokiol has the potential to act as a natural agonist for PPARγ, thereby reducing both neuroinflammation and Aβ generation. Thus, honokiol exhibits promise as a prospective therapeutic strategy for treating AD [43].
According to Lee et al. [44]’s findings, administering a 10 mg/kg dose of an ethanol extract of M. officinalis reduced memory loss in an LPS-induced model of AD in mice using the water maze test [44]. A further investigation was conducted to assess the impact of honokiol on the impairment of memory and learning induced by AβO in mice. The AO intrahippocampal injection was used for developing a mouse model of AD. A Morris water maze (MWM) test measured the subject's cognitive ability. The administration of honokiol resulted in a significant rise in the duration of time spent by the mice with AD in the designated zone during the MWM test.
Furthermore, it was observed that honokiol exhibited a dose-dependent reduction in hippocampal neural apoptosis, ROS generation, and a decline in the membrane potential of mitochondria caused by AβO. In addition, the stimulation of NF-κB caused by AβO was suppressed by honokiol, along with the increased expression of APP and β-secretase [45]. A study investigated the potential benefits of honokiol against mitochondrial abnormalities caused by AβOs in neuronal cells and its impact on cognitive abilities in transgenic AD mice. The findings showed that honokiol increased mitochondrial SIRT3 expression, increasing ATP generation and reducing ROS production. This suggests that honokiol may be therapeutically helpful in postponing the onset of AD symptoms by reducing mitochondrial dysfunction and enhancing SIRT3 hyperactivation [46]. Subsequent investigations have suggested that the neurotherapeutic properties of the molecule, as mentioned above, may be attributed to the mitigation of ROS generation, as well as the curtailment of intracellular calcium upregulation and the hindrance of caspase-3 enzymatic activity. This study's findings offer a scientific justification for the therapeutic application of honokiol in managing AD [1].
According to Matsui et al., [47] honokiol was administered to SAMP8 mice at an oral dose of 0.1 and 1 mg/kg daily for 14 days when the mice were 2 months old. At 2 months of age, the forebrain of SAMP8 mice exhibited reduced activity of Akt, which is a constituent of the prosurvival pathway. The administration of honokiol at a dose of 1 mg/kg for 14 days increased Akt phosphorylation levels in the forebrain region at the age of 2 months. The findings indicate that honokiol may protect against cognitive decline associated with aging by maintaining the integrity of cholinergic neurons in the forebrain. The molecules mentioned above exhibit promising potential as therapeutics for NDs [47].
A study aimed to determine the potential of honokiol in reversing memory and learning deficits caused by scopolamine in mice. The researchers administered 10 and 20 mg/kg of honokiol intraperitoneally for 21 days, substantially enhancing memory and spatial learning function. The administration also reduced the synthesis of prostaglandin E2 (PGE2) and COX-2 mRNA expression in the cerebral cortex of mice administered scopolamine. The mechanistic assessments showed that honokiol significantly reset alterations in phosphorylated Akt and ERK1/2 levels in the cerebral cortex of mice administered scopolamine. The findings support the notion that honokiol has the potential to enhance cognitive function and alleviate memory deficits caused by scopolamine in mice. This protective effect is likely due to suppressing AChE activity and mitigating neuroinflammation in the SCOP-administered mice [48].
Parkinson’s disease (PD)
Neuroinflammation is a complex process that plays a role in various complex conditions affecting the brain, including ischemia injury and neurodegenerative diseases such as multiple sclerosis and PD [49]. Atrophy of projection fibers from the substantia nigra pars compacta to the striatum results from the progressive death of substantia nigra pars compacta dopaminergic (DA) neurons, the most frequent movement state in adults. Activation of glial cells, such as astrocytes and microglia, is a pivotal biological process in neuroinflammation. Astrocytes and microglia undergo substantial structural changes during inflammation, followed by increased production of essential immunomodulatory cytokines [50, 51]. Consequently, astrocytes and microglia, under conditions of inflammatory stress, can produce several cytokines that promote inflammation. These cytokines include IL-6, TNF-α, and IL-1β [52]. Other transcription factors, such as the well-known regulator NF-kB and Krüppel-like factor 4 (KLF4), are involved in similar regulatory pathways that regulate the expression of pro and anti-inflammatory cytokines. Indeed, in addition to its actions in maintaining stem cells, KLF4 was associated with the overexpression of IL-10 and iNOS in macrophages and IL-6 in dendritic cells [53]. Endothelial cells and microglia-like cells belonging to the immune system may benefit from the role that KLF4 plays in regulating pro-inflammatory mediators [54].
Many PPARγ agonists have been shown to provide neuroprotective benefits in both in vitro and in vivo models. Dozens of different animal models of PD have revealed that PPARγ activation reduces levels of OS and inflammation, improves mitochondrial function, reduces glial activation, slows the rate of nigral dopaminergic neuron loss, and increases striatal dopamine levels (Fig. 5) [55, 56]. These outcomes conclude that PPARγ may be a therapeutically productive target for treating PD. So, therapeutic interventions targeting PPARγ in people with PD may effectively reduce the severity of disease symptoms and halt the long process of neurodegeneration [57, 58].
Mechanistic illustration of the therapeutic applications of honokiol in neuroinflammation. Honokiol has the potential to bind and activate peroxisome proliferator-activated receptor gamma (PPAR-γ), subsequently leading to the induction of liver X receptor (LXR), scavenger receptor A (SRA), and cluster of differentiation 36 (CD36) expression. These molecular mechanisms are responsible for facilitating the efficient lysosomal clearance of amyloid-beta (Aβ) in microglial cells. Simultaneously, Honokiol demonstrated inhibitory effects on NF-κB activity and mRNA expression of inflammatory cytokines. Furthermore, it has the capability to stimulate the Nrf2-ARE pathway and mitigate the generation of reactive oxygen species (ROS)
M. Officinalis contains the major bioactive polyphenols honokiol and magnolol, often used in various neurological conditions, including anxiety and nervous tension. In rat models of PD, their two main compounds, magnolol, and honokiol, reduced the extent of nerve damage and behavioral problems. In in vivo and in vitro models of PD, the neuroprotective benefits of honokiol and magnolol can be attributed to the reduction of OS, glial activation, excitotoxicity, and neuronal inflammation (Fig. 5) [31]. Each of these factors plays a role in neurotoxin-induced neurotoxicity and motor impairment. Also, it has been found that honokiol was more effective than magnolol in protecting neurons from damage caused by neurotoxins and oxidants [31, 59]. In addition, honokiol is a retinoid X receptor (RXR) dimer activator and a PPARγ gamma agonist. This study aimed to demonstrate the therapeutic potential of honokiol for neural regeneration activity in PD and hemiparkinsonian rats by suppressing PPARγ activation in rat unilateral striatum using 6-hydroxydopamine injection (6-OHDA) [60].
Honokiol has been shown to have neuroprotective effects, particularly in the context of dopaminergic neuronal degeneration and motor impairments in mice following unilateral striatal injection of 6-OHDA. A recent study found that honokiol reduced the effects of 6-OHDA changes and improved contralateral rotation caused by apomorphine. Additionally, administration of honokiol in the after-treatment phase reduced impaired motor functioning and improved the loss of tyrosine hydroxylase-immunoreactive neurons. The administration of honokiol also reversed the increased expression of inducible nitric oxide synthase (iNOS) in the nigrostriatal region and reduced neuronal nitric oxide synthase (NOS) induced by 6-OHDA. These findings suggest that honokiol has protective and curative functions against motor deficits and dopamine-responsive progressive impairment in mice with 6-OHDA-induced lesions. This may be due to the modulation of NOS signaling. Honokiol can potentially serve as a therapeutic agent for treating neurological symptoms and neuronal degeneration in PD [14]. A subsequent investigation by the same researchers revealed that the inhibitory impact of PPARγ antagonist GW9662 prevented reversing the benefits of honokiol on behavioral problems and striatal PPARγ expression. Notably, the administration of subchronic honokiol resulted in an extension of the life expectancy of mice exhibiting hemiparkinsonian symptoms. The results of this study indicate that honokiol possesses beneficial properties that can improve motor function and prevent dopaminergic injury by modulating PPARγ signaling. Thus, the triggering of PPARγ by Honokiol presents a promising avenue for managing motor manifestations and neurodegeneration in PD, making it an appealing treatment candidate [61]. The neuroprotective potential of Honokiol against PD was investigated by Xu et al. in a model in mice. Sixty male C57BL/6 mice were randomly assigned to five distinct groups: the control group, amantadine group, mitochondrial toxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) model group, and honokiol groups A and B. The study employed a spontaneous movement test to assess the activity frequency of individual mice over 5 min. Additionally, HPLC-electrochemistry was utilized to identify any alterations in dopamine levels in the striatum of the mice. The study's findings indicated that the frequency of spontaneous movement exhibited by mice in the MPTP model group was comparatively lower than that of the control group over 5 min [62].
The compound honokiol has been observed to decrease the inflammatory response to lipopolysaccharide (LPS) in primary cultures of microglia and astrocytes. This effect is achieved by inhibiting pro-inflammatory mediators such as iNOS, IL-6, IL-1β, and TNF-α while simultaneously stimulating the production of anti-inflammatory cytokines such as IL-10. The administration of LPS increased KLF4 expression in both microglia and astrocytes. However, the observed response was attenuated by the application of honokiol. The present study provides further insights into the anti-inflammatory effects of honokiol on central glial cells, thereby substantiating its potential as a therapeutic agent for treating neuroinflammatory conditions [63].
The study conducted by Ye et al. [64] aimed to assess the impact of honokiol on cognitive impairment induced by surgery/anesthesia in mice. The administration of honokiol resulted in the mitigation of surgery-induced cognitive impairment and neuronal cell death, as well as a reduction in neuroinflammation and improvement in OS in the hippocampal region. It was observed that surgery/anesthesia resulted in a significant reduction in the level of expression of SIRT3 in the hippocampus. Conversely, honokiol administration led to a rise in SIRT3 expression, thereby causing a decrease in the acetylation of SOD2. The findings indicate that honokiol-induced activation of SIRT3 may mitigate cognitive decline in mice resulting from surgery and anesthesia. This effect is likely achieved by regulating neuroinflammation and OS in the hippocampus [64].
Magnolol, a structural isomer of honokiol, has been found to protect against MPTP/MPP + -induced toxicity by inhibiting oxidative damage in both in vivo and in vitro models of PD. C57BL/6N mice were administered 30 mg/kg once daily for 4 or 5 days, and both treatments effectively reduced DAT and TH protein levels in the striatum caused by MPTP. However, these interventions did not affect GFAP levels induced by MPTP. Magnolol administration also prevented MPTP-induced lipid peroxidation in the striatum and significantly decreased MPP + -induced cytotoxicity and ROS development in SH-SY5Y cells. These findings suggest that magnolol may confer protection through an antioxidant mechanism in both in vivo and in vitro PD models [65].
A raising body of research has shown that honokiol significantly reduces cognitive deficits brought on by various circumstances [11]. Honokiol is effective in treating newborn discomfort and preventing neurobehavioral problems. Long-term treatment reduces chronic hyperalgesia caused by heat and inhibits acute pain responses 30 min after a formalin assault. Rats with honokiol perform better on learning, memory, and exploratory behavior tests. Treatment normalizes c-Fos expression in the hippocampus and thalamic regions and substance P receptors in the hippocampal alveus. These results suggest honokiol protects newborn rats against acute and long-term pain-induced degradation [66].
Anxiety and depression
Anxiety disorders are common co-morbidities with neuropsychiatric problems and chronic inflammatory ailments including liver damage. Brain-derived neurotrophic factor (BDNF), OS, and peripheral inflammation are significant factors in their pathogenesis. Around one-eighth of the world's population suffers from anxiety-like syndrome [67]. Anti-anxiety medications currently available on the market cause adverse side effects and have low patient compliance rates. Hence, there is a crucial demand to research and develop safer and more potential novel anti-anxiety therapeutics [68]. To find novel therapeutic agents for treating NDs, research on medicinal plant products is continuously progressing in different countries. In various animal models of psychiatric disorders, some plant species have been shown to have pharmacological effects [69].
Honokiol has been extensively researched on whether it possesses antidepressant and anti-anxiety properties. A study conducted by Sulakhiya et al. [71] found that administering honokiol at a higher dosage resulted in a substantial decrease (p < 0.05) of anxiety-like behavior induced by LPS. This was evidenced by an increase in the number of records, the duration spent in the open arm during the EPM test, and an increase in the frequency of entries into the central zone during the OFT. The administration of honokiol prior to lipopolysaccharide exposure reduced peripheral inflammation, as evidenced by decreased levels of plasma IL-1β, IL-6, and TNF-α. Additionally, honokiol treatment led to an improvement in plasma BDNF levels. It prevented liver damage by reducing transaminase levels (ALT and AST), liver OS, and TNF-α activity in mice challenged with LPS.
To summarize, the present study indicates that honokiol positively impacts anxiety-like behavior and liver damage caused by LPS. This effect is likely attributed to the suppression of cytokine production, oxidative stress, and reduction of plasma BDNF level (Table 1). The study's findings indicate that honokiol may have potential as a therapeutic intervention for addressing anxiety and other neurological diseases linked to inflammation and OS [70].
The centrally depressing effects of honokiol may offer not only the anticonvulsant action of the compound but also the anxiolytic efficacy at low dosages. The GABAA receptor is a common target for anxiolytics like benzodiazepines, which may explain its relaxing effect [10]. Kuribara et al. [71] studied the effects of honokiol on animal behavior, finding that a single oral dose increased exploratory behavior and decreased anxiety-related behavior. Multiple doses, even at a minimal dosage of 0.2 mg/kg, led to fewer motor or cognitive adverse effects. The anxiolytic effect of diazepam was disrupted by both flumazenil and bicuculline. However, combined administration of CCK-4 and caffeine with diazepam led to distinct outcomes. The authors concluded that honokiol has anxiolytic effects with a more favorable adverse effect profile than diazepam. Additionally, their findings suggest that honokiol may operate through alternative processes, as evidenced by their observations with caffeine [71].
One of the goals of recent research was to investigate honokiol's influence on sleeping. It was shown that Honokiol, at doses of 10 and 20 mg/kg, dramatically shortened sleep latency and increased the quantity of NREM sleep, but it had no impact on the duration of REM sleep. This same research team discovered that honokiol stimulated sleep-inducing neurons in the ventrolateral preoptic sections of the brain. The fact that honokiol makes it easier to fall asleep and reduces anxiety points to the possibility of further use for this neolignan in anesthesia [72].
In addition, honokiol treatment can prevent cognitive damage and behavior similar to depression caused by prolonged restraint stress by inhibiting stress on the endoplasmic reticulum (ER) in the hippocampus of rats. In an experiment, groups were given Honokiol (3 and 10 mg/kg) and Imipramine (10 and 30 mg/kg) during the previous week. The MWM test was used to evaluate cognitive function. The group with honokiol showed a significant improvement in cognitive function and behavior, similar to depression. However, imipramine could not stop cognitive damage caused by restraint stress despite suppressing depressive-like behavior [73].
Additionally, higher levels of pro-inflammatory cytokines, GRP78, and CHOP were found in the hippocampus of stressed mice than in those without stress. When administered at 10 mg/kg, honokiol significantly suppressed these cytokines, suggesting that honokiol may positively affect restraint stress. This suggests that honokiol may be an exciting treatment option for neuropathophysiological disorders related to ER stress [73].
A study suggests that honokiol can potentially serve as an antidepressant in rats that have been subjected to chronic unpredictable mild stress (CUMS). This effect is achieved through the regulation of BDNF activity. The administration of honokiol at varying dosages (2, 4, and 8 mg/kg) resulted in the amelioration of behavioral deficits induced by CUMS. The administration of honokiol resulted in normalizing the limbic system hypothalamic–pituitary–adrenal (HPA) axis hyperactivity caused by CUMS, as evidenced by the reduction in serum levels of CRH, ACTH, and CORT. Furthermore, honokiol elicited an upregulation of GRα (both mRNA and protein) and BDNF (both mRNA and protein) within the hippocampal region. The data mentioned above substantiated the antidepressant properties of honokiol, potentially attributed to its capacity to restore the HPA axis function and elevate the BDNF concentration in the hippocampus [74].
The study conducted by Fan et al. [75] demonstrated that the activation of the HIF-1α-VEGF signaling pathway by honokiol resulted in an improvement of depression-like behaviors in rats. Honokiol demonstrated notable antidepressant effects by auguring synaptic plasticity via mechanical means. Honokiol has been observed to trigger the HIF-1α-VEGF signaling pathway both in vitro and in vivo at a molecular level. Additionally, it has been found to enhance the protein expression levels of SYN 1 and PSD 95. The collective findings not only establish an empirical foundation for using honokiol in the clinical management of depression but also propose the possibility of the HIF-1α-VEGF pathway as a viable therapeutic target for depression treatment [75].
The study conducted by Pitta and colleagues revealed that honokiol has the potential to counteract depressive-like behavior and reduce the decline in brain BDNF levels that the administration of corticosterone injections causes over an extended period in mice. The findings indicate that the administration of corticosterone injections for three weeks resulted in a notable increase in the levels of corticosterone in the serum of mice. The administration of corticosterone injections on a repetitive basis resulted in the manifestation of behavior akin to depression in mice. This was evidenced by a marked reduction in sucrose consumption and increased immobility duration during the forced swim test. Additionally, a notable reduction in BDNF levels within the hippocampus was observed in mice treated with corticosterone. The administration of honokiol to mice resulted in a notable reduction in depressive behavior and a concurrent elevation in BDNF levels in mice treated with corticosterone (Table 1) [76].
Honokiol derivatives are expected to be beneficial in anxiety and depressive disorders. Magnolia bark extracts have been used to treat anxiety and psychological problems. The primary components of interest consist of biphenyl-type neolignan honokiol and its isomer magnolol. The compound under investigation is a derivative of honokiol, which contains nitrogen (specifically, 3-acetylamino-4′-O-methylhonokiol, abbreviated AMH). This derivative is a very effective modulator of GABAA receptors. This investigation aims to provide a comprehensive understanding of the correlation between the chemical structure and biological activity of nitrogenated biphenyl-neolignan derivatives. This is achieved by analyzing their allosteric regulation and agonistic actions on α1β2γ2S GABAA receptors. The compound 3-acetamido-4′-ethoxy-3′,5-dipropylbiphenyl-2-ol exhibited the most prominent and most robust attachment to IGABA, but the compound 5′-amino-2-ethoxy-3′,5-dipropylbiphenyl-4′-ol shown a much greater potency [77]. Besides, Thirteen novel glucosides of magnolol and honokiol were synthesized by targeted O-glycosylation reactions using two filamentous fungus, Cunninghamella echinulata AS 3.3400 and Rhizopus japonicus ZW-4. Minor reactions were reported, including hydroxylation and selective 6″-O-acylation. The findings of the bioassay demonstrated that the combination of glucosides with magnolol and honokiol at a concentration of 10 μM effectively reduced the toxic effects generated by glutamate in SK-N-SH cells, reaching a degree of attenuation similar to that seen with MK-801, a positive control. Nevertheless, there was a noticeable rise in the water solubility of the primary glycosylated compounds [78].
Cerebral ischemia
Ischemia of the brain, also known as cerebral ischemia, is a frequent cause of acute brain damage and occurs when the blood supply to the brain is restricted. Ischemia of the brain is considered a medical emergency because, if left untreated, it may lead to cerebral infarctions or global hypoxic-ischemic encephalopathy, both of which have the potential to cause death or lifelong impairment [79]. The study results indicate that honokiol was protective against injury caused by focal cerebral ischemia–reperfusion (FCI/R) in rats. Liou et al. [80] reported that the intravenous delivery of honokiol at varying doses (0.01–1.0 μg/kg) either 15 min before (pre-treatment) or 60 min after (post-treatment) middle cerebral artery occlusion resulted in a dose-dependent decrease in the total infarcted volume by 20–70%. Applying honokiol at concentrations of 0.1 and 1.0 μg/kg, either before or after treatment, resulted in a significant reduction in neutrophil infiltration in the brain affected by infarction. According to the findings, honokiol can potentially protect brain tissue from peroxidation of lipids and infiltration of neutrophils in the context of FCI/R injury.
Additionally, it was observed that cerebral infarction resulting from FCI/R is characterized by significant neutrophil infiltration in the affected area during FCI/R [80]. The administration of honokiol microemulsion resulted in a substantial reduction in neural deficit, infarct volume, and brain water level in rats that underwent cerebral ischemia–reperfusion. Additionally, honokiol at concentrations ranging from 0.1 to 10 μM exhibited a significant reduction in damage caused by oxygen-glucose lack or glutamate in fetal rat cortical neurons. Moreover, the outcomes demonstrated that honokiol exhibited a reversible inhibitory effect of approximately 64% on the NMDA current. To summarize, the therapeutic effects of honokiol have been observed to persist for a minimum of 5 h following the beginning of cerebral ischemia. This may be attributed to the disruption of the PSD95-nNOS interaction, reducing neurotoxic nitric oxide (NO) production [81].
In a separate piece of research, the beneficial properties of honokiol on rat models of ischemia and reperfusion damage were studied. In the group that received honokiol, all histological scores, including hemorrhage, cell infiltration, and cellular degradation, were shown to have decreased significantly. Malondialdehyde levels in ovarian tissue were considerably more remarkable in the torsion and detorsion groups than in the sham and honokiol groups. Therefore, it is possible to conclude that honokiol positively impacts ovarian ischemia/reperfusion damage caused by torsion [82].
A study was undertaken to investigate the neuroprotective properties of 002C-3, its possible mechanisms of action in rats, and its initial toxic effects in mice. The present study employed a rat model to assess its impact and underlying mechanism. Additionally, a dose-restricted experiment was conducted to assess the early toxicity of the model. The administration of a single intravenous bolus of 002C-3 at a dose range of 10–50 μg/kg after reperfusion substantially reduced infarct volumes, neurological scores, and brain water contents. When administered at a high effective level of 1000 times the standard dose, 002C-3 did not exhibit any observable toxicity in mice [83].
Additionally, the mean weight of mice treated with 002C-3 was comparable to that of the control group that received the vehicle. Conversely, magnolol was found to cause significant toxicity and mortality in the mice. To summarize, the compound 002C-3 exhibits a noteworthy safeguarding impact against cerebral ischemia–reperfusion injury, surpassing the potency of magnolol. This beneficial effect may be attributed to its ability to prevent autophagy and apoptosis. Additionally, 002C-3 displays reduced toxicity in comparison to magnolol. The above findings gave valuable information for subsequent investigation and advancement [83].
The neuroprotective potential of honokiol was investigated by Liou et al. [84] in rats that underwent focal cerebral ischemia. The use of honokiol was carried out via IV in two distinct groups: the pre-treatment groups, where the administration took place for 15 min before the obstruction of the right middle cerebral artery, and the treatment groups, where the administration occurred after removing both common carotid artery clips. The study findings indicate that an IV infusion of honokiol at doses of 10–8, 10–7, and 10–6 g/kg did not result in significant hemodynamic alterations in either of the groups. Honokiol exhibited a substantial decrease in the overall infarction volume in both treatment and pre-treatment groups at doses of 10–7 and 10–6 g/kg. The findings of this investigation propose that honokiol exhibits significant potential as a neuroprotective agent in cases of focal cerebral ischemia. The positive impact could be attributed to the antioxidant [84].
Brain ischemia–reperfusion damage may be prevented in rats by administering a synthetic analog of honokiol named W007B. This compound preserves brain tissue by reducing inflammation, autophagy, and apoptosis. Bu et al. [85]’s experimental results indicate that the administration of w007B (at doses of 10 and 50 μg/kg, intravenously immediately after reperfusion) resulted in a substantial reduction in neurological deficit scores, a decrease in infarct size, and a reduction in brain water content. Furthermore, the administration of 50 μg/kg w007B within 3 h after reperfusion (5 h after ischemia) significantly mitigated ischemia-induced brain injury. Furthermore, there was no indication of any toxic effects upon administering a solitary dose of 50 mg/kg w007B (1000 times greater than the maximum effective dose, IP). The study reported a notable decrease in caspase-3 activity and NO production in the injured semi-brain upon administration of w007B.
Additionally, the nuclear level of the p65 subunit of NF-κB was observed to be reduced. Moreover, it elicited a decrease in the expression of Beclin-1 and LC3B-II while inducing an elevation in the level of p62, which are proteins associated with autophagy, in the hemisphere subjected to ischemia/reperfusion injury. In summary, it has been observed that w007B demonstrates a neuroprotective impact on cerebral ischemia–reperfusion injury, with a broader therapeutic time frame and enhanced safety. This effect’s mechanisms may be linked to its anti-inflammatory, anti-apoptotic, and anti-autophagic properties. The findings indicate that w007B exhibits considerable promise as a clinical neuroprotective agent for managing ischemic stroke [85].
Spinal cord injury
Spinal cord injuries (SCIs) are severe medical conditions that have long-lasting effects on patients' lives. Primary and secondary stages of illness develop after SCI. When the spinal cord is compressed, neurons and glia are injured, and axons are lost. Because of the activation of molecular cascades and messenger routes, secondary damage is triggered when axons are severed, or cell membranes are ruptured—secondary damage results from the death of neurons and glial cells from free radicals and OS [96]. Damage to the spinal cord's myelin sheath can also cause its breakdown and demyelination.
The inflammation itself partly causes secondary damage to the spinal cord caused by inflammation. Because of its potent antioxidant and anti-inflammatory characteristics, honokiol is a neuroprotective compound in certain studies. The honokiol compound has an anti-inflammatory effect, and a recently discovered essential target for this activity is Klf4. It has not yet been determined whether or not honokiol can suppress the inflammatory response in a rat model of SCI by regulating the expression of Klf4. According to the findings of Liu and colleagues, honokiol lowers the severity of histopathology, attenuates inflammation, and downregulates the expression of Klf4 in rats with spinal cord injuries. In addition, honokiol enhanced the functional outcome after traumatic SCI and decreased the amount of histopathology that was present. By inhibiting the body's inflammatory response, honokiol not only helps patients recover from spinal cord injuries more quickly and with less pain, but it also minimizes the amount of secondary damage to the tissues that occurs as a result of the injury [97].
A separate study has indicated that honokiol demonstrates protective properties towards neural myelin sheaths in the aftermath of compressed SCI. This is achieved by impeding oligodendrocyte apoptosis through controlling ER-mitochondrial interactions. Following a six-day intervention with honokiol, notable improvements were observed in the locomotor function and pathomorphological alterations of the myelin sheath in rats with chronic spinal cord dorsal column damage (CSCD) compared to the control group. These improvements were accompanied by a significant reduction in the levels of active caspase-3, caspase-12, and cytochrome C. Honokiol has been found to potentially enhance locomotor function and safeguard the neural myelin sheath against demyelination by inhibiting apoptosis of oligodendrocytes (OLs) through the mediation of the ER-mitochondria pathway after cervical SCI [12].
Biochemical and immunohistochemistry research was conducted by Firidin et al. [95] to study the preventive impact of the antioxidant honokiol on neuronal and glial cells in the spinal cord following a lesion to the spinal cord. As a result of the trauma, there was a rise in the production of caspase-3 in multipolar cells and a positive caspase-3 response in solitary glial cells. Canalis ependymalis cells and many glial cells within the honokiol group were found to have low levels of caspase-3 activation. Following a traumatic lesion to the spinal cord, alterations, including degeneration and apoptosis in neuron and glial cells, as well as enhanced inflammation and thrombosis in blood vessels, emerged. The damage was caused by lipid peroxidation as a direct result of an increase in OS. After the honokiol treatment, there was a significant decrease in OS, inflammation, and angiogenetic impact in blood vessels. It is believed that honokiol has a beneficial impact on triggering apoptotic signals in neuronal and glial cells in situations where there has been damage [95].
Pharmacokinetic profile
Pharmacokinetic studies on honokiol medication should be conducted, as well as more precise dose designs for diverse conditions and new drug delivery systems to improve bioavailability in hospital settings. Honokiol primarily undergoes hepatic metabolism and in vivo biotransformation, wherein glucuronidation and sulfation serve as the principal metabolic pathways for the conversion of honokiol into mono-glucuronide honokiol and sulfated mono-hydroxy honokiol before its elimination [98, 99]. Honokiol has a biphasic kinetic profile characterized by an initial rapid distribution phase and a subsequent slower elimination phase. The elimination half-life for honokiol after intravenous administration is 49.2 min for a 5 mg dose and 56.2 min for a 10 mg dose [100, 101]. Plasma concentrations of honokiol in mice treated with liposomal honokiol remained above 30 and 10 μg/mL for 24 and 48 h, respectively.
In contrast, mice treated with free honokiol experienced a rapid decrease in plasma concentration (< 5 μg/mL) within 12 h. These results suggest that liposomal honokiol extends the duration of honokiol circulation in the blood of mice with A549 xenograft tumors, compared to free honokiol [102, 103]. The oral administration of Honokiol to rats resulted in rapid distribution in all organs, with the highest concentration accumulation in the brain, liver, and kidneys [104, 105]. A maximal plasma honokiol concentration of about 1100 µg/mL was achieved in nude mice when honokiol was injected intraperitoneally at a dose of 250 mg/kg. This maximal plasma honokiol concentration was achieved at 27.179 ± 6.252 min after administration. According to the plasma pharmacokinetic curve, the half-life of absorption was 10.121 ± 2.761 min, whereas the elimination half-life was 5.218 ± 0.461 h [106, 107]. The low oral bioavailability of honokiol and magnolol can be due to their substantial first-pass metabolism, low water solubility, and poor absorption [108, 109]. The distribution of magnolol is primarily observed in the kidney, lung, liver, brain, and heart. The liver exhibits the most substantial concentrations of magnolol-glucuronides and magnolol [110, 111].
Clinical status
Implementing clinical trials to establish evidence for improving the management of health-related concerns is necessary. A clinical trial could evaluate strategies to enhance patient compliance with therapeutic regimens [112]. Although several in vivo and in vitro tests on the neuropharmacological activities of honokiol have been conducted, only a few clinical trials have been conducted.
The use of Magnolia bark extract (MBE) as a potential source of beneficial components has been observed in various human research investigations, either in isolation or in combination with other herbal components. In a clinical trial evaluating the efficacy of a dietary supplement containing MBE and phellodendron compared to a placebo, participants were administered a daily dosage of 11.25 mg of honokiol and 0.75 mg of berberine [113]. Forty-two overweight women volunteered for the trial; three dropped out due to side effects (two in the experimental group and one in the placebo arm). Heartburn, shaky hands, prebilabial numbness, sexual dysfunction, thyroid malfunction, weariness, and headaches were some of the symptoms mentioned by the two research participants. No substantial treatment-related adverse events were reported throughout the research, and no statistically significant variations in biochemical markers were seen between the groups [113, 114].
Toxicological profile
The potential risks associated with honokiol cannot be disregarded entirely, as its scientific implementation to people at therapeutic levels has been limited, thereby restricting the assessment of its adverse effect profile. When administered excessively, possible hazards can be anticipated, such as heightened hemorrhaging and probable neurological damage [10]. An investigation was conducted to determine the honokiol microemulsion's acute and subchronic toxicities. During the acute toxicology testing, the mice received graded dosages of honokiol microemulsion through an IV, and they were monitored every day for 14 days for signs of toxic manifestations and death. In the research on sub-chronic toxicity, rats were given honokiol microemulsion injections at 100, 500, and 2500 g/kg body weight (BW) over a month. Following a treatment period of 30 days and a recovery period of 14 days, the rats were slaughtered for hematological, biochemical, and histological analysis. According to the results of acute toxicology tests, the predicted median lethal dose (LD50) in mice was 50.5 mg/kg of body weight. In the subchronic toxicity studies, the amount that produced a non-toxic response was 500 µg/kg b.w. According to the results of this research, the honokiol microemulsion is harmless up to 500 g/kg body weight; nevertheless, it does cause irritation to the vascular tissue at the location of injection, which should be considered when developing therapeutic medications [115]. The present investigation assessed the embryonic and fetal developmental effects of honokiol microemulsion. During the gestational period from day 6 to day 15, pregnant SD rats were subjected to intravenous injection of the drug at varying dose levels of 0, 200, 600, and 2000 g/kg/day. The gravid animals were monitored for variations in body mass and any anomalous modifications and were subsequently undergoing cesarean delivery on gestational day (GD) 20. All offspring procured from the cesarean delivery were evaluated through external inspection and visceral and skeletal examinations. The groups administered with honokiol microemulsion did not exhibit any external modifications or malformations in the visceral and skeletal systems that could be attributed to the treatment. Nonetheless, embryonic-fetal developmental toxicity was detected at a dose level of 2000 g/kg/day, which reduced the body and tail length of fetuses. The established no-observed-adverse-effect level (NOAEL) for honokiol microemulsion is 600 g/kg/day [116].
Honokiol is identified as an effective inhibitor of artery thrombosis. Therefore, it is recommended to use caution when administering honokiol to patients with coagulopathy or those at risk of bleeding or hemorrhage [17]. The categories mentioned above of patients comprise individuals with hemorrhagic stroke, those exhibiting hemorrhagic alterations after ischemic stroke, patients undergoing coumadin or therapeutic Lovenox treatment, and individuals with clotting conditions such as hemophilia or von Willebrand's deficiency. Honokiol exhibits neuroprotective properties at lower doses; however, it is also shown to induce neuronal degeneration in vitro at elevated doses (specifically, 100 µM) [10, 117].
Cosmetics with M. officinalis are currently being promoted as anti-aging products. Like other extracts of Magnolia, MBE has also been associated with cases of allergic contact dermatitis, indicating that this component may be an uncommon allergen [118].
The utilization of Magnolia bark extract (MBE) as a helpful component has been observed in various human research investigations, either in isolation or in combination with other herbal components. In a clinical trial evaluating the efficacy of a dietary supplement containing MBE and phellodendron compared to a placebo, participants were administered a daily dosage of 11.25 mg of honokiol and 0.75 mg of berberine [113]. Forty-two overweight women volunteered for the trial; three dropped out due to side effects (two in the experimental group and one in the placebo arm). Heartburn, shaky hands, prebilabial numbness, sexual dysfunction, thyroid malfunction, weariness, and headaches were some of the symptoms mentioned by the two research participants. No substantial treatment-related adverse events were reported throughout the research, and no statistically significant variations in biochemical markers were seen between the groups [113, 114].
Both magnolol and honokiol were tested for their possible mutagenic and genotoxic effects, although only MBE was used, not the pure chemicals themselves. Human fetal small intestine epithelial noncancerous cells, often employed to examine the biological implications of food or medication, were employed in recent research to assess the genotoxic effects of an aqueous extract of M. officinalis. Thin-layer chromatography was employed to scrutinize the MBE following the European Pharmacopoeia 8.4 monographs. The analysis results revealed that magnolol and honokiol were consistent with the description provided in the European Pharmacopoeia. The decoction contained only negligible amounts of these two neolignans [119].
There may be pharmacokinetic drug interactions between honokiol and drugs that are co-administered and metabolized by CYP2C19, CYP2C8, CYP1A2, CYP2C9, and UGT1A9 [120]. Honokiol is a poor CYP2B6 inducer. Hence, it is unlikely to accelerate the metabolism of other CYP2B6 substrates and create pharmacokinetic drug interactions in human subjects [121]. The prolonging of propofol anesthesia was shown in rats when magnolol inhibited glucuronidation. However, pigs and monkeys, which have metabolic similarities to humans, had a lower sensitivity to glucuronosyltransferase inhibition [114, 122]. A study revealed that pharmacokinetic interactions occur between Magnolol and Piperine in rats. The pharmacokinetic properties of piperine remained unchanged when administered concurrently with magnolol at a 20 mg/kg dose. However, at a high dosage of 40 mg/kg, the maximum concentration of piperine dropped significantly from 4.30 ± 1.47 µg/mL to 2.50 ± 0.78 µg/mL (p < 0.05). No significant differences were observed in the area under the curve (AUC) and half-life (t1/2) of piperine in the plasma when given alone or in combination with magnolol [123].
Concluding remarks and future directions
Even while technological advances have significantly sped up the process of assessing phytochemicals, there is still a lot of work to be done until we have a more definite understanding of the neurotherapeutic advantages of herbal medications. As a consequence of our findings and other studies' findings, we have concluded that honokiol's ability to change several signaling pathways makes it potentially useful as a medicine for treating NDs. Despite the limitations of the ongoing clinical study, honokiol is showing great potential as a potential treatment for a wide range of NDs, including AD, PD, cerebral ischemia, anxiety, depression, spinal cord, and others. Even though a significant amount of preclinical research studies have been carried out to evaluate the neurotherapeutic potential of honokiol, the compound's clinical potential has not yet been used. There is a need for more research to improve the bioavailability of honokiol and for clinical studies to be carried out to evaluate the therapeutic efficacy of these compounds.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Hoi CP, Ho YP, Baum L, Chow AHL. Neuroprotective effect of honokiol and magnolol, compounds from Magnolia officinalis, on beta-amyloid-induced toxicity in PC12 cells. Phyther Res. 2010;24:1538–42.
Lin YR, Chen HH, Ko CH, Chan MH. Neuroprotective activity of honokiol and magnolol in cerebellar granule cell damage. Eur J Pharmacol. 2006;537:64–9.
Talarek S, Listos J, Barreca D, Tellone E, Sureda A, Nabavi SF, et al. Neuroprotective effects of honokiol: from chemistry to medicine. BioFactors. 2017;43:760–9.
Akagi M, Matsui N, Akae H, Hirashima N, Fukuishi N, Fukuyama Y, et al. Nonpeptide neurotrophic agents useful in the treatment of neurodegenerative diseases such as Alzheimer’s disease. J Pharmacol Sci. 2015;127:155–63.
Kubo M. Search of neurotrophin-mimic natural products for prevention and treatment of neurodegenerative disease. Yakugaku Zasshi. 2015;135:1147–52.
Zhu S, Liu F, Zhang R, Xiong Z, Zhang Q, Hao L, et al. Neuroprotective potency of neolignans in Magnolia officinalis cortex against brain disorders. Front Pharmacol. 2022;13:857449.
Esumi T, Makado G, Zhai H, Shimizu Y, Mitsumoto Y, Fukuyama Y. Efficient synthesis and structure-activity relationship of honokiol, a neurotrophic biphenyl-type neolignan. Bioorg Med Chem Lett. 2004;14:2621–5.
Kong Z-L, Tzeng S-C, Liu Y-C. Cytotoxic neolignans: an SAR study. Bioorg Med Chem Lett. 2005;15:163–6.
Aman MM, Mahmoud A, Sinha AC. Chapter 14 - Postoperative Analgesia in Morbid Obesity: An Overview of Multimodal Analgesia and Complimentary Therapies. In: Watson RR, Zibadi SBT-NM of P in the AP, editors. Academic Press; 2017. p. 171–80.
Woodbury A, Yu SP, Wei L, García P. Neuro-modulating effects of Honokiol: a review. Front Neurol. 2013;4:13.
Lin YR, Chen HH, Lin YC, Ko CH, Chan MH. Antinociceptive actions of honokiol and magnolol on glutamatergic and inflammatory pain. J Biomed Sci. 2009. https://doi.org/10.1186/1423-0127-16-94.
Tan Y, Yu H, Sun S, Gan S, Gong R, Jie MK, et al. Honokiol exerts protective effects on neural myelin sheaths after compressed spinal cord injury by inhibiting oligodendrocyte apoptosis through regulation of ER-mitochondrial interactions. J Spinal Cord Med. 2022;45:595–604.
Zhou Y, Tang J, Lan J, Zhang Y, Wang H, Chen Q, et al. Honokiol alleviated neurodegeneration by reducing oxidative stress and improving mitochondrial function in mutant SOD1 cellular and mouse models of amyotrophic lateral sclerosis. Acta Pharm Sin B. 2023;13:577–97.
Chen HH, Chang PC, Chen C, Chan MH. Protective and therapeutic activity of honokiol in reversing motor deficits and neuronal degeneration in the mouse model of Parkinson’s disease. Pharmacol Reports. 2018;70:668–76.
Hou M, Bao W, Gao Y, Chen J, Song G. Honokiol improves cognitive impairment in APP/PS1 mice through activating mitophagy and mitochondrial unfolded protein response. Chem Biol Interact. 2022;351:109741.
Qiang L-Q, Wang C-P, Wang F-M, Pan Y, Yi L-T, Zhang X, et al. Combined administration of the mixture of honokiol and magnolol and ginger oil evokes antidepressant-like synergism in rats. Arch Pharm Res. 2009;32:1281–92.
Hu H, Zhang X, Wang Y, Chen S. Honokiol inhibits arterial thrombosis through endothelial cell protection and stimulation of prostacyclin. Acta Pharmacol Sin. 2005;26:1063–8.
Amblard F, Delinsky D, Arbiser JL, Schinazi RF. Facile purification of honokiol and its antiviral and cytotoxic properties. J Med Chem. 2006;49:3426–7.
Kim Y-S, Lee J-Y, Park J, Hwang W, Lee J, Park D. Synthesis and microbiological evaluation of honokiol derivatives as new antimicrobial agents. Arch Pharm Res. 2010;33:61–5.
Bai X, Cerimele F, Ushio-Fukai M, Waqas M, Campbell PM, Govindarajan B, et al. Honokiol, a small molecular weight natural product, inhibits angiogenesis in vitro and tumor growth in vivo. J Biol Chem. 2003;278:35501–7.
Ho KY, Tsai CC, Chen CP, Huang JS, Lin CC. Antimicrobial activity of honokiol and magnolol isolated from Magnolia officinalis. Phytother Res. 2001;15:139–41.
Kuribara H, Kishi E, Hattori N, Yuzurihara M, Maruyama Y. Application of the elevated plus-maze test in mice for evaluation of the content of honokiol in water extracts of magnolia. Phytother Res. 1999;13:593–6.
Liou K-T, Shen Y-C, Chen C-F, Tsao C-M, Tsai S-K. The anti-inflammatory effect of honokiol on neutrophils: mechanisms in the inhibition of reactive oxygen species production. Eur J Pharmacol. 2003;475:19–27.
Gertsch J, Anavi-Goffer S. Methylhonokiol attenuates neuroinflammation: a role for cannabinoid receptors? J Neuroinflamm. 2012. https://doi.org/10.1186/1742-2094-9-135.
Kuribara H, Kishi E, Kimura M, Weintraub ST, Maruyama Y. Comparative assessment of the anxiolytic-like activities of honokiol and derivatives. Pharmacol Biochem Behav. 2000;67:597–601.
Tripathi S, Chan MH, Chen C. An expedient synthesis of honokiol and its analogues as potential neuropreventive agents. Bioorganic Med Chem Lett. 2012;22:216–21.
Shih HC, Hwang TL, Chen HC, Kuo PC, Lee EJ, Lee KH, et al. Honokiol dimers and magnolol derivatives with new carbon skeletons from the roots of magnolia officinalis and their inhibitory effects on superoxide anion generation and elastase release. PLoS One. 2013;8:e59502.
Rycek L, Puthenkalam R, Schnürch M, Ernst M, Mihovilovic MD. Metal-assisted synthesis of unsymmetrical magnolol and honokiol analogs and their biological assessment as GABAA receptor ligands. Bioorganic Med Chem Lett. 2015;25:400–3.
Zhang B, Yu H, Lu W, Yu B, Liu L, Jia W, et al. Four new honokiol derivatives from the stem bark of Magnolia officinalis and their anticholinesterase activities. Phytochem Lett. 2019;29:195–8.
Taferner B, Schuehly W, Huefner A, Baburin I, Wiesner K, Ecker GF, et al. Modulation of GABAA-receptors by Honokiol and derivatives: subtype selectivity and structure-activity relationship. J Med Chem. 2011;54:5349–61.
Rauf A, Olatunde A, Imran M, Alhumaydhi FA, Aljohani ASM, Khan SA, et al. Honokiol: a review of its pharmacological potential and therapeutic insights. Phytomedicine. 2021;90: 153647. https://doi.org/10.1016/j.phymed.2021.153647.
Gulcin İ. Antioxidants and antioxidant methods: an updated overview. Arch Toxicol. 2020;94:651–715.
Arnott JA, Planey SL. The influence of lipophilicity in drug discovery and design. Expert Opin Drug Discov. 2012;7:863–75.
Esumi T, Makado G, Zhai H, Shimizu Y, Mitsumoto Y, Fukuyama Y. Efficient synthesis and structure—activity relationship of honokiol, a neurotrophic biphenyl-type neolignan. Chem Inform. 2004. https://doi.org/10.1002/chin.200439189.
Schenk D, Hagen M, Seubert P. Current progress in beta-amyloid immunotherapy. Curr Opin Immunol. 2004;16:599–606.
Seo S, Lee K-G, Shin J-S, Chung EK, Lee JY, Kim HJ, et al. 6′-O-Caffeoyldihydrosyringin isolated from Aster glehni suppresses lipopolysaccharide-induced iNOS, COX-2, TNF-α, IL-1β and IL-6 expression via NF-κB and AP-1 inactivation in RAW 264.7 macrophages. Bioorg Med Chem Lett. 2016;26:4592–8.
Bae J-Y, Lee D-S, Cho YK, Lee J-Y, Park J-H, Lee SH. Daphne jejudoensis attenuates LPS-induced inflammation by inhibiting TNF-α, IL-1β, IL-6, iNOS, and COX-2 expression in periodontal ligament cells. Pharmaceuticals. 2022;15:387.
Mandrekar-Colucci S, Landreth GE. Nuclear receptors as therapeutic targets for Alzheimer’s disease. Expert Opin Ther Targets. 2011;15:1085–97.
Zhao X, Gonzales N, Aronowski J. Pleiotropic role of PPAR γ in intracerebral hemorrhage: an intricate system involving Nrf2, RXR, and NF-κB. CNS Neurosci Ther. 2015;21:357–66.
Atallah N, Vasiu R, Bosca AB, Cretu D-I, Georgiu C, Constantin A-M, et al. Microglia—performers of the 21st century. Rom J Morphol Embryol. 2014;55:745–65.
Dar NJ, Glazner GW. Deciphering the neuroprotective and neurogenic potential of soluble amyloid precursor protein alpha (sAPPα). Cell Mol Life Sci. 2020;77:2315–30.
Ramesh S, Govindarajulu M, Lynd T, Briggs G, Adamek D, Jones E, et al. SIRT3 activator Honokiol attenuates β-amyloid by modulating amyloidogenic pathway. PLoS One. 2018;13:e0190350.
Wang D, Dong X, Wang C. Honokiol ameliorates amyloidosis and neuroinflammation and improves cognitive impairment in Alzheimer’s disease transgenic mice. J Pharmacol Exp Ther. 2018;366:470–8.
Lee YJ, Choi DY, Yun YP, Han SB, Kim HM, Lee K, et al. Ethanol extract of magnolia officinalis prevents lipopolysaccharide-induced memory deficiency via its antineuroinflammatory and antiamyloidogenic effects. Phyther Res. 2013;27:438–47.
Wang M, Li Y, Ni C, Song G. Honokiol attenuates oligomeric amyloid β 1–42 -induced Alzheimer’s disease in mice through attenuating mitochondrial apoptosis and inhibiting the nuclear factor Kappa-B signaling pathway. Cell Physiol Biochem. 2017;43:69–81.
Li H, Jia J, Wang W, Hou T, Tian Y, Wu Q, et al. Honokiol alleviates cognitive deficits of Alzheimer’s disease (PS1 V97L) transgenic mice by activating mitochondrial SIRT3. J Alzheimer’s Dis. 2018;64:291–302.
Matsui N, Takahashi K, Takeichi M, Kuroshita T, Noguchi K, Yamazaki K, et al. Magnolol and honokiol prevent learning and memory impairment and cholinergic deficit in SAMP8 mice. Brain Res. 2009;1305:108–17.
Xian YF, Ip SP, Mao QQ, Su ZR, Chen JN, Lai XP, et al. Honokiol improves learning and memory impairments induced by scopolamine in mice. Eur J Pharmacol. 2015;760:88–95.
Davie CA. A review of Parkinson’s disease. Br Med Bull. 2008;86:109–27.
De Lau LML, Breteler MMB. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006;5:525–35.
Zhang P, Liu X, Zhu Y, Chen S, Zhou D, Wang Y. Honokiol inhibits the inflammatory reaction during cerebral ischemia reperfusion by suppressing NF- kappaB activation and cytokine production of glial cells. Neurosci Lett. 2013;534:123–7.
Tse AK-W, Wan C-K, Shen X-L, Yang M, Fong W-F. Honokiol inhibits TNF-α-stimulated NF-κB activation and NF-κB-regulated gene expression through suppression of IKK activation. Biochem Pharmacol. 2005;70:1443–57.
Spencer JPE, Vafeiadou K, Williams RJ, Vauzour D. Neuroinflammation: modulation by flavonoids and mechanisms of action. Mol Aspects Med. 2012;33:83–97.
Shen B, Smith RS, Hsu Y-T, Chao L, Chao J. Kruppel-like factor 4 is a novel mediator of kallistatin in inhibiting endothelial inflammation via increased endothelial nitric-oxide synthase expression*. J Biol Chem. 2009;284:35471–8.
Ghaleb AM, Yang VW. Krüppel-like factor 4 (KLF4): what we currently know. Gene. 2017;611:27–37.
Desvergne B, Michalik L, Wahli W. Be fit or be sick: peroxisome proliferator-activated receptors are down the road. Mol Endocrinol. 2004;18:1321–32.
Corona JC, Duchen MR. PPARγ and PGC-1α as therapeutic targets in Parkinson’s. Neurochem Res. 2015;40:308–16.
Abbott BD. Review of the expression of peroxisome proliferator-activated receptors alpha (PPARα), beta (PPARβ), and gamma (PPARγ) in rodent and human development. Reprod Toxicol. 2009;27:246–57.
Chen C, Zhang Q-W, Ye Y, Lin L-G. Honokiol: a naturally occurring lignan with pleiotropic bioactivities. Chin J Nat Med. 2021;19:481–90.
Dreier D, Latkolik S, Rycek L, Schnürch M, Dymáková A, Atanasov AG, et al. Linked magnolol dimer as a selective PPARγ agonist—structure-based rational design, synthesis, and bioactivity evaluation. Sci Rep. 2017;7:13002.
Chen HH, Chang PC, Wey SP, Chen PM, Chen C, Chan MH. Therapeutic effects of honokiol on motor impairment in hemiparkinsonian mice are associated with reversing neurodegeneration and targeting PPARγ regulation. Biomed Pharmacother. 2018;108:254–62.
Xu Y, Tang S, Wang J, Lei Q, Feng C. Neuroprotective effects of honokiol on mouse model with parkinson’s disease. Jiefangjun Yixue Zazhi. 2008;33:981–2.
Uta R, François C, Marvin H, Philipp A, Andrea PP, Henrik W, et al. Anti-inflammatory properties of honokiol in activated primary microglia and astrocytes. J Neuroimmunol. 2018;323:78–86.
Ye JS, Chen L, Lu YY, Lei SQ, Peng M, Xia ZY. SIRT3 activator honokiol ameliorates surgery/anesthesia-induced cognitive decline in mice through anti-oxidative stress and anti-inflammatory in hippocampus. CNS Neurosci Ther. 2019;25:355–66.
Muroyama A, Fujita A, Lv C, Kobayashi S, Fukuyama Y, Mitsumoto Y. Magnolol protects against MPTP/MPP + -induced toxicity via inhibition of oxidative stress in in vivo and in vitro models of Parkinson’s disease. Parkinsons Dis. 2012. https://doi.org/10.1155/2012/985157.
Woodbury A, Yu SP, Chen D, Gu X, Lee JH, Zhang J, et al. Honokiol for the treatment of neonatal pain and prevention of consequent neurobehavioral disorders. J Nat Prod. 2015;78:2531–6.
Soncini R, de Souza DF, Neves AP, Braga DS, Andrade CAF, Giusti-Paiva A. Dipyrone attenuates acute sickness response to lipopolysaccharide in mice. Neurosci Lett. 2012;516:114–8.
Bassi GS, Kanashiro A, Santin FM, de Souza GEP, Nobre MJ, Coimbra NC. Lipopolysaccharide-induced sickness behaviour evaluated in different models of anxiety and innate fear in rats. Basic Clin Pharmacol Toxicol. 2012;110:359–69.
Chan SHH, Wu C-WJ, Chang AYW, Hsu K-S, Chan JYH. Transcriptional upregulation of brain-derived neurotrophic factor in rostral ventrolateral medulla by angiotensin II: significance in superoxide homeostasis and neural regulation of arterial pressure. Circ Res. 2010;107:1127–39.
Sulakhiya K, Kumar P, Gurjar SS, Barua CC, Hazarika NK. Beneficial effect of honokiol on lipopolysaccharide induced anxiety-like behavior and liver damage in mice. Pharmacol Biochem Behav. 2015;132:79–87.
Kuribara H, Stavinoha WB, Maruyama Y. Behavioural pharmacological characteristics of honokiol, an anxiolytic agent present in extracts of Magnolia bark, evaluated by an elevated plus-maze test in mice. J Pharm Pharmacol. 1998;50:819–26.
Qu WM, Yue XF, Sun Y, Fan K, Chen CR, Hou YP, et al. Honokiol promotes non-rapid eye movement sleep via the benzodiazepine site of the GABAA receptor in mice. Br J Pharmacol. 2012;167:587–98.
Jangra A, Dwivedi S, Sriram CS, Gurjar SS, Kwatra M, Sulakhiya K, et al. Honokiol abrogates chronic restraint stress-induced cognitive impairment and depressive-like behaviour by blocking endoplasmic reticulum stress in the hippocampus of mice. Eur J Pharmacol. 2016;770:25–32.
Wang C, Gan D, Wu J, Liao M, Liao X, Ai W. Honokiol exerts antidepressant effects in rats exposed to chronic unpredictable mild stress by regulating brain derived neurotrophic factor level and hypothalamus–pituitary–adrenal axis activity. Neurochem Res. 2018;43:1519–28.
Fan XX, Sun WY, Li Y, Tang Q, Li LN, Yu X, et al. Honokiol improves depression-like behaviors in rats by HIF-1α- VEGF signaling pathway activation. Front Pharmacol. 2022. https://doi.org/10.3389/fphar.2022.968124.
Pitta S, Augustine BB, Kasala ER, Sulakhiya K, Ravindranath V, Lahkar M. Honokiol reverses depressive-like behavior and decrease in brain BDNF levels induced by chronic corticosterone injections in mice. Pharmacogn J. 2013;5:211–5.
Bernaskova M, Schoeffmann A, Schuehly W, Hufner A, Baburin I, Hering S. Nitrogenated honokiol derivatives allosterically modulate GABAA receptors and act as strong partial agonists. Bioorganic Med Chem. 2015;23:6757–62.
Yang L, Wang Z, Lei H, Chen R, Wang X, Peng Y, et al. Neuroprotective glucosides of magnolol and honokiol from microbial-specific glycosylation. Tetrahedron. 2014;70:8244–51.
Uddin MZ, Rana MS, Hossain S, Ferdous S, Dutta E, Dutta M, et al. In vivo neuroprotective, antinociceptive, anti-inflammatory potential in Swiss albino mice and in vitro antioxidant and clot lysis activities of fractionated Holigarna longifolia Roxb. bark extract. J Complement Altern Med. 2019;17:20190102. https://doi.org/10.1515/jcim-2019-0102.
Liou KT, Shen YC, Chen CF, Tsao CM, Tsai SK. Honokiol protects rat brain from focal cerebral ischemia-reperfusion injury by inhibiting neutrophil infiltration and reactive oxygen species production. Brain Res. 2003;992:159–66.
Hu Z, Bian X, Liu X, Zhu Y, Zhang X, Chen S, et al. Honokiol protects brain against ischemia-reperfusion injury in rats through disrupting PSD95-nNOS interaction. Brain Res. 2013;1491:204–12.
Tunc SY, Agacayak E, Goruk NY, Icen MS, Turgut A, Alabalik U, et al. Protective effects of honokiol on ischemia/reperfusion injury of rat ovary: an experimental study. Drug Des Devel Ther. 2016;10:1077–83.
Li H, Liu X, Zhu Y, Liu Y, Wang Y. Magnolol derivative 002C–3 protects brain against ischemia-reperfusion injury via inhibiting apoptosis and autophagy. Neurosci Lett. 2015;588:178–83.
Liou KT, Lin SM, Huang SS, Chih CL, Tsai SK. Honokiol ameliorates cerebral infarction from ischemia-reperfusion injury in rats. Planta Med. 2003;69:130–4.
Bu Q, Liu X, Zhu Y, Liu Y, Wang Y. W007B protects brain against ischemia-reperfusion injury in rats through inhibiting inflammation, apoptosis and autophagy. Brain Res. 2014;1558:100–8.
Hou YC, Lee Chao PD, Chen SY. Honokiol and magnolol increased hippocampal acetylcholine release in freely-moving rats. Am J Chin Med. 2000;28:379–84.
Li W, Wang S, Zhang H, Li B, Xu L, Li Y, et al. Honokiol restores microglial phagocytosis by reversing metabolic reprogramming. J Alzheimer’s Dis. 2021;82:1475–85.
Zhang B, Wang PP, Hu KL, Li LN, Yu X, Lu Y, et al. Antidepressant-like effect and mechanism of action of honokiol on the mouse lipopolysaccharide (LPS) depression model. Molecules. 2019;24:2035.
Xu Q, Yi LT, Pan Y, Wang X, Li YC, Li JM, et al. Antidepressant-like effects of the mixture of honokiol and magnolol from the barks of Magnolia officinalis in stressed rodents. Prog Neuro-Psychopharmacol Biol Psychiatry. 2008;32:715–25.
Wang PP, Liu BX, Yang T, Li LN, Wang SY, Chang HS. Antidepressant effect and mechanism of honokiol on acute and chronic stress mouse. Chin Pharm J. 2017;52:2161–5.
Borgonetti V, Governa P, Manetti F, Miraldi E, Biagi M, Galeotti N. A honokiol-enriched Magnolia officinalis Rehder bark extract possesses anxiolytic-like activity with neuroprotective effect through the modulation of CB1 receptor. J Pharm Pharmacol. 2021;73:1161–8.
Wang H, Liao Z, Sun X, Shi Q, Huo G, Xie Y, et al. Intravenous administration of honokiol provides neuroprotection and improves functional recovery after traumatic brain injury through cell cycle inhibition. Neuropharmacology. 2014;86:9–21.
Liao G, Zhao Z, Yang H, Li X. Honokiol ameliorates radiation-induced brain injury via the activation of SIRT3. J Int Med Res. 2020. https://doi.org/10.1177/0300060520963993.
Ermiş IS, Deveci E. Investigation of the biochemical, histopathological, and immunohistochemical effects of honokiol on the changes in the choroid plexus after traumatic brain injury in rats. Anal Quant Cytopathol Histopathol. 2021;43:417–25.
Firidin MN, Akyüz ME. Prophylactic effects of Honokiol on spinal cord injury in rats. Anal Quant Cytopathol Histopathol. 2021;43:477–83.
Zheng Y, Mao Y-R, Yuan T-F, Xu D-S, Cheng L-M. Multimodal treatment for spinal cord injury: a sword of neuroregeneration upon neuromodulation. Neural Regen Res. 2020;15:1437–50.
Liu J, Zhang C, Liu Z, Zhang J, Xiang Z, Sun T. Honokiol downregulates kruppel-like factor 4 expression, attenuates inflammation, and reduces histopathology after spinal cord injury in rats. Spine. 2015;40:363–8.
Böhmdorfer M, Maier-Salamon A, Taferner B, Reznicek G, Thalhammer T, Hering S, et al. In vitro metabolism and disposition of honokiol in rat and human livers. J Pharm Sci. 2011;100:3506–16.
Ong CP, Lee WL, Tang YQ, Yap WH. Honokiol: a review of its anticancer potential and mechanisms. Cancers. 2019;12:48.
Tsai T-H, Chou C-J, Cheng F-C, Chen C-F. Pharmacokinetics of Honokiol after intravenous administration in rats assessed using high performance liquid chromatography. J Chromatogr B Biomed Sci Appl. 1994;655:41–5.
Arora S, Singh S, Piazza GA, Contreras CM, Panyam J, Singh AP. Honokiol: a novel natural agent for cancer prevention and therapy. Curr Mol Med. 2012;12:1244–52.
Jiang Q, Fan L, Yang G, Guo W-H, Hou W, Chen L, et al. Improved therapeutic effectiveness by combining liposomal honokiol with cisplatin in lung cancer model. BMC Cancer. 2008;8:1–8.
Averett C, Arora S, Zubair H, Singh S, Bhardwaj A, Singh AP. Chapter Nine - Molecular Targets of Honokiol: A Promising Phytochemical for Effective Cancer Management. In: Bathaie SZ, Tamanoi FBT-TE, editors. Nat Prod Cancer Signal Isoprenoids, Polyphenols Flavonoids. Academic Press; 2014. p. 175–93.
Jun-Jun W, Xiao-Lei M, Jing-Ya C, Yong C. The pharmacokinetics and tissue distribution of honokiol and its metabolites in rats. Eur J Drug Metab Pharmacokinet. 2016;41:587–94.
Khatoon F, Ali S, Kumar V, Elasbali AM, Alhassan HH, Alharethi SH, et al. Pharmacological features, health benefits and clinical implications of honokiol. J Biomol Struct Dyn. 2022. https://doi.org/10.1080/07391102.2022.2120541.
Chen F, Wang T, Wu Y-F, Gu Y, Xu X-L, Zheng S, et al. Honokiol: a potent chemotherapy candidate for human colorectal carcinoma. World J Gastroenterol WJG. 2004;10:3459.
Shigemura K, Arbiser JL, Sun S, Zayzafoon M, Johnstone PAS, Fujisawa M, et al. Honokiol, a natural plant product, inhibits the bone metastatic growth of human prostate cancer cells. Cancer Interdiscip Int J Am Cancer Soc. 2007;109:1279–89.
Lin H-L, Cheng W-T, Chen L-C, Ho H-O, Lin S-Y, Hsieh C-M. Honokiol/magnolol-loaded self-assembling lecithin-based mixed polymeric micelles (lb MPMs) for improving solubility to enhance oral bioavailability. Int J Nanomed. 2021;16:651–65.
Mottaghi S, Abbaszadeh H. Natural lignans Honokiol and magnolol as potential anticarcinogenic and anticancer agents. A comprehensive mechanistic review. Nutr Cancer. 2022;74:761–78.
Lin S-P, Tsai S-Y, Chao P-DL, Chen Y-C, Hou Y-C. Pharmacokinetics, bioavailability, and tissue distribution of magnolol following single and repeated dosing of magnolol to rats. Planta Med. 2011;77:1800–5.
Zhang J, Chen Z, Huang X, Shi W, Zhang R, Chen M, et al. Insights on the multifunctional activities of magnolol. Biomed Res Int. 2019. https://doi.org/10.1155/2019/1847130.
Lang T, Siribaddana S. Clinical trials have gone global: is this a good thing? PLoS Med. 2012;9: e1001228.
Kalman DS, Feldman S, Feldman R, Schwartz HI, Krieger DR, Garrison R. Effect of a proprietary Magnolia and Phellodendron extract on stress levels in healthy women: A pilot, double-blind, placebo-controlled clinical trial. Nutr J. 2008. https://doi.org/10.1186/1475-2891-7-11.
Sarrica A, Kirika N, Romeo M, Salmona M, Diomede L. Safety and toxicology of magnolol and Honokiol. Planta Med. 2018;84:1151–64.
Zhang Q, Li J, Zhang W, An Q, Wen J, Wang A, et al. Acute and sub-chronic toxicity studies of honokiol microemulsion. Regul Toxicol Pharmacol. 2015;71:428–36.
Zhang Q, Ye X, Wang L, Peng B, Zhang Y, Bao J, et al. Embryo-fetal development toxicity of honokiol microemulsion intravenously administered to pregnant rats. Regul Toxicol Pharmacol. 2016;74:117–22.
Fukuyama Y, Nakade K, Minoshima Y, Yokoyama R, Zhai H, Mitsumoto Y. Neurotrophic activity of honokiol on the cultures of fetal rat cortical neurons. Bioorganic Med Chem Lett. 2002;12:1163–6.
Mitra S, Tareq AM, Das R, Emran TB, Nainu F, Chakraborty AJ et al. Polyphenols: A first evidence in the synergism and bioactivities. Food Rev Int. 2023;39:4419–41. https://doi.org/10.1080/87559129.2022.2026376.
Nachtergael A, Poivre M, Belayew A, Duez P. In vitro genotoxicity tests point to an unexpected and harmful effect of a Magnolia and Aristolochia association. J Ethnopharmacol. 2015;174:178–86.
Jeong H-U, Kong TY, Kwon SS, Hong S-W, Yeon SH, Choi J-H, et al. Effect of Honokiol on cytochrome P450 and UDP-glucuronosyltransferase enzyme activities in human liver microsomes. Molecules. 2013;18:10681–93.
Cho Y-Y, Jeong H-U, Kim J-H, Lee HS. Effect of Honokiol on the induction of drug-metabolizing enzymes in human hepatocytes. Drug Des Devel Ther. 2014. https://doi.org/10.2147/DDDT.S72305.
Yang L, Zhu L, Ge G, Xiao L, Wu Y, Liang S, et al. Species-associated differences in the inhibition of propofol glucuronidation by magnolol. J Am Assoc Lab Anim Sci. 2014;53:408–11.
Chen X-Y, Yang G-H, Li C-L, Yu X-T, Wang X-F, Zheng Y-F, et al. Pharmacokinetic interaction between magnolol and piperine in rats. Trop J Pharm Res. 2016;15:631–8.
Acknowledgements
The authors express their gratitude to the Deanship of Scientific Research at King Khalid University for funding this work through the Large Research Group Project under grant number RGP.02/339/44.
Funding
The authors declare no competing interests.
Author information
Authors and Affiliations
Contributions
MF: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Resources; Software; Visualization; Roles/Writing—original draft; Writing—review and editing. JK: Data curation; Investigation; Methodology; Resources; Software; Roles/Writing—original draft; Writing—review and editing. MZ: Data curation; Investigation; Methodology; Resources; Software; Roles/Writing—original draft; Writing—review and editing; Supervision. NN: Data curation; Investigation; Methodology; Resources; Software; Roles/Writing—original draft; Writing—review and editing. LPS: Data curation; Investigation; Methodology; Resources; Software; Writing—review and editing. SK: Formal analysis; Investigation; Validation; Visualization; Roles/Writing—review & editing. RP: Formal analysis; Investigation; Validation; Visualization; Roles/Writing—review & editing. PAK: Formal analysis; Investigation; Validation; Visualization; Roles/Writing—review and editing. FN: Formal analysis; Investigation; Validation; Visualization; Roles/Writing—review & editing. MA: Formal analysis; Investigation; Validation; Visualization; Roles/Writing—review and editing. SL.K: Formal analysis; Investigation; Validation; Visualization; Roles/Writing—review and editing. RD: Formal analysis; Investigation; Validation; Visualization; Roles/Writing—review & editing TBE: Conceptualization; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Supervision; Validation; Visualization; Writing—review and editing. PW: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Supervision; Validation; Visualization; Roles/Writing—original draft; Writing—review & editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors approved the final manuscript and the submission to this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Faysal, M., Khan, J., Zehravi, M. et al. Neuropharmacological potential of honokiol and its derivatives from Chinese herb Magnolia species: understandings from therapeutic viewpoint. Chin Med 18, 154 (2023). https://doi.org/10.1186/s13020-023-00846-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13020-023-00846-1