Abstract
Inflammatory bowel disease (IBD) is a collective term for inflammatory diseases including Crohn’s disease and ulcerative colitis. Toll-like receptor 4 (TLR4) is thought to play a key role in the pathogenesis of IBD. Inhibition of TLR4 has been recognized as an effective target for the treatment of IBD. Many phytochemicals have been shown to have potential as new drugs for the treatment of IBD. This review surveyed the available literature and reports which focused on the in vivo effects of phytochemicals targeting TLR4 in different models of IBD, and clarified the significance of TLR4 as a current therapeutic target for IBD. Based on our review, we have concluded that phytochemicals targeting TLR4 are potentially effective candidates for developing new therapeutic drugs against IBD.
Similar content being viewed by others
Introduction
For thousands of years, plants have been used as the primary source of medicines [1]. Plants can produce a variety of compounds called phytochemicals [2, 3]. Phytochemicals with multiple therapeutic applications have a variety of biological functions, including anti-inflammatory, antiallergy, anti-cancer, antibiosis, anti-viral, and analgesic functions [4, 5]. Current clinical treatment of inflammatory bowel disease (IBD) is mainly based on drugs and surgery, but adverse side effects and the questionable effectiveness of drug treatment have limited their application [6, 7]. In contrast, the importance of phytochemicals in the therapeutic application of IBD have been highlighted, due to their significant efficacy and fewer side effects [8]. Phytochemicals are a good source of new anti-inflammatory drugs that can modulate various inflammatory responses and fight inflammatory diseases, especially IBD [8, 9].
IBD, including ulcerative colitis (UC) and Crohn’s disease (CD), is a group of chronic recurrent and incurable gastrointestinal diseases with an unknown etiology that can ultimately lead to the destruction of normal intestinal architecture [10]. It is an increasingly important public health issue that is receiving more and more attention. Crohn’s disease occurs primarily in the terminal ileum and adjacent colon, where inflammation can spread to the deeper layers of the intestine [11]. On the other hand, inflammation in ulcerative colitis is limited to the colonic mucosa and begins in the rectum and may involve the entire colon [12]. IBD is known to be caused by an inappropriate response of a dysfunctional mucosal immune system to resident microbiota and other harmful antigens [13]. Additionally, dysfunction of the immune system, particularly Toll-like receptor 4 (TLR4) dysfunction, plays a key role in the pathogenesis of IBD [14]. Although many drugs have been developed to treat IBD, these drugs have adverse side effects on the gastrointestinal tract [15]. Therefore, targeting TLR4 is considered a new therapeutic strategy for patients with IBD [16]. Numerous studies have shown that phytochemicals, including phenolic compounds, terpenoids, alkaloids, and organosulfur compounds, can act as therapeutic agents and exert protective and therapeutic effects on IBD [17]. In particular, some phytochemicals are being studied as antagonists of TLR4 [18]. Considering the advantages of phytochemicals, and their fewer side effects, phytochemicals targeting TLR4 represent a potentially good source of new drugs for the treatment of IBD [14]. The study of the role of phytochemicals targeting TLR4 in IBD contributes to providing a firm theoretical basis for the development of drugs for the treatment of IBD. In the process of researching articles, we found that most studies to date have been based on animal models and cell experiments. Thus, further extensive clinical studies focusing on the efficacy of phytochemicals against IBD via TLR4 should be conducted.
For this review, we searched for relevant articles published between 2011 and December 2021 in PubMed/Medline, using different combinations of key terms including “TLR4”, “inflammatory bowel disease”, “IBD”, “colitis”, “intestinal inflammation”, and “phytochemical”. Articles in our search had to meet the following criteria: (a) the focus was on a natural phytochemical that affects IBD via TLR4, (b) pharmacological studies in vivo animal models, and (c) only English language articles; all papers that did not meet these criteria were excluded. It is important to note that some relevant articles may not have been included in this study because the search strategy we employed was not absolutely perfect.
Toll-like receptor
As the most important pathogen pattern recognition molecules (PPRs), Toll-like receptors (TLRs) are responsible for the activation and association of innate and adaptive immune responses and play a key role in maintaining homeostasis in the gut.
TLRs detect a wide range of pathogen-associated molecular patterns (PAMPs), including Gram-negative and positive bacteria, viruses, nucleic acids, flagellin proteins, lipids, and damage-associated molecular patterns (DAMPs) [19, 20]. TLRs is a family of transmembrane receptors and 13 TLRs have been identified in humans [21]. TLRs contain extracellular leucine-rich repeat (LRR) motifs and cytoplasmic Toll/interleukin-1 receptor (TIR) homology domain. The TIR domain mediates interactions between TLRs and TIR-domain-containing adaptor proteins, leading to the biological specificity of the TLR response [22, 23]. Mammalian TLRs induce a variety of effector molecules, such as iNOS and antimicrobial peptides that can directly destroy microbial pathogens [24]. TLRs are well expressed in different cells or tissues such as dendritic cells, natural killing, epithelium cells, and macrophages [25]. When TLRs are activated, together with the contribution of the secreted proteins myeloid differentiation factor 2 (MD-2) and cluster of differentiation 14 (CD14), they stimulate downstream signal transduction procedures, such as inducing a variety of inflammatory cytokines through transcription by mediating the phosphorylation of IκB to activate NF-κB [13, 26]. This leads to the secretion of pro-inflammatory mediators, which directly affect the immune response [27]. Additionally, the expression of innate immune receptors plays a key role in the abnormal and enhanced inflammatory response. As a result, the mutation and dysregulation of TLRs will lead to the over-generation of IBD [28].
The association between dysregulation of the innate immune system and the emergence of several diseases, such as inflammation, autoimmunity, and cancer has made it the focus of the development of many agents countering uncontrolled TLR-mediated signaling, as these receptors are primary regulators of the host’s innate immunity [29]. TLR antagonists have been mainly explored as structural analogs of agonists, which block agonistic action of TLR ligands through binding to the receptor and preventing the propagation of the downstream inflammatory/autoimmune cascades [30, 31]. TLR antagonists are currently in clinical trials for the treatment of septic shock and autoimmune diseases [32]. New evidence suggests that TLR agonists are a promising class of immunomodulatory agents that provide long-term protection against subsequent infectious challenges by enhanced innate immunity [33, 34]. TLR agonists induce augmentation of cell recruitment, antimicrobial effector functions (i.e. respiratory burst, phagocytosis, production of proinflammatory cytokines and chemokines), attenuate inflammation, bacterial clearance, and trigger cross-protection to infection with clinically related pathogens [35]. A number of TLR agonist and antagonist compounds have been designed recently which are able to target specific innate immune receptors (Table 1).
The role of TLR4 in IBD
TLR4, widely expressed in various immune cells and epithelial/endothelial cells, is a key member of TLR family and a classical mediator of inflammation and acts as a signaling molecule between innate and adaptive immunity, as well as between inflammation and infection [45, 46]. TLR4 has been identified as the primary pattern recognition receptor (PRR) as well as the canonical receptor for Gram-negative bacteria’s lipopolysaccharide (LPS), and there is emerging evidence that supports that TLR4 is involved in homeostasis, apoptosis, intestinal inflammation, and inflammatory bowel disease [47,48,49]. TLR4 combined with LPS binding protein (LBP), CD14 and MD-2, acts as PRR for LPS of gram-negative bacteria (Fig. 1) [28]. When LPS is identified, LBP will transfer LPS to cell surface CD14 and then bind to the TLR4/MD-2 receptor complex [50]. Subsequently, TLR4 is activated by the formed LPS–LBP–CD14 complex, signaling through adaptor protein myeloid differentiation 88 (MyD88) and serine kinase IL-1R-associated kinase 4 (IRAK4) and the adaptor protein TNF receptor-associated factor 6 (TRAF6). Then, NF-κB and mitogen-activated protein kinase (MAPK) are activated by this pathway, leading to the transcription of proinflammatory cytokines, such as tumor necrosis factor (TNF)-α and IL-6, -8, and -12, and the initiation of IBD [51,52,53].
Under normal conditions, normal or low expression of TLR4 in intestine controls inflammation, but elevated TLR4 expression in the intestinal mucosa of patients with IBD leads to sustained secretion of inflammatory cytokines and ultimately to the development of intestinal inflammation [54, 55]. Therefore, the occurrence and development of IBD may be related to the abnormal expression of TLR4 in intestinal epithelium. Significantly increased mRNA and protein expression of TLR4 was reported in the colonic mucosa of patients with UC and CD compared to healthy controls [56, 57], similarly suggesting that TLR4 is involved in IBD. Therefore, targeting and inhibiting TLR4 is effective for the treatment of IBD [16].
Phytochemicals targeting the TLR4
Current treatments for IBD can have many side effects, such as fatigue, nausea, abdominal pain, and diarrhoea [15]. Surprisingly, dietary supplements of plant-derived natural compounds are considered to have therapeutic protective and therapeutic effects for IBD [17]. Here, we discuss the present evidence that phytochemicals could induce IBD remission by affecting the TLR4 in animal model systems of IBD (Table 2).
Phenolic compounds
Phenolics is a group of secondary plant metabolites with several classes, including phenolic acids, flavonoids, stilbenes, coumarins, lignins, and tannins [67]. Numerous studies have shown that polyphenols are effective in treating IBD [68, 69].
Curcumin
Curcumin, a plant-derived polyphenolic compound, is naturally present in turmeric (Curcuma longa) and is known to exhibit a variety of pharmacological effects including anti-inflammatory, and anti-tumorigenic [70]. Accumulating evidence has revealed that curcumin has anti-inflammatory effects against IBD. A study reported that curcumin improves 2,4,6-trinitrobenzene sulfonic acid (TNBS)-induced colitis in rats [71]. To investigate the upstream signaling mechanism of curcumin in experimental colitis in rats, Zhaojing Zeng et al. used experimental colitis induced in rats by intra-rectal instillation of TNBS. They found that the levels of TLR4 and NF-κB were significantly upregulated in the inflammatory colon. In contrast with the model group, the curcumin remarkably lowered the levels of TLR4 and NF-κB. In addition, curcumin treatment inhibited Myeloperoxidase (MPO) activity. Curcumin targeting TLR4 may be considered as a putative candidate of treatment in IBD [58].
Baicalin
Baicalin is a kind of flavonoid derived from the roots of traditional Chinese medicine Scutellariae Radix [72], which shows a variety of biological activities such as diminishing inflammation, reducing cellular lipid anabolism, as well as inhibiting bacterial and viral infection [73, 74]. It has been reported that baicalin reduced serum levels of proinflammatory factors IL-1β, IL-6 and CRP [75]. Baicalin ameliorated TNBS-induced colitis injury by suppressing TLR4 signaling in a concentration-dependent manner, inhibiting NF-κB activation and limiting the inflammatory response, such as ICAM-1, MCP-1, Cox-2, TNF-α, IL-1β and IL-6 [59].
Naringenin
Naringenin is a citrus flavonoid mainly derived from grapefruit, which has been reported to have antioxidant, anti-inflammatory properties [76, 77]. A recent report showed that the oxidative damage and injury of colon tissues in a mice model of acetic acid-induced colitis was ameliorated by naringenin [78]. It is also reported that naringenin significantly improved colitis in a DSS-induced mice colitis model by inhibiting of TLR4 protein and NF-κB activity, downregulating the expression of inflammatory mediators (iNOS, ICAM-1, MCP-1 Cox-2, TNF-α and IL-6) and the production of inflammatory cytokines (TNF-α and IL-6) [60].
Eriodictyol
Eriodictyol is a natural flavanone mainly isolated from yerba Santa Clause (Eriodictyon californicum), a plant local to North America, which has various physiological functions, including anti-inflammation, anti-oxidation, analgesic effects, neuroprotective effects, improving diabetes and diabetic complications [79]. It has been reported to alleviate cisplatin-induced kidney injury by inhibiting inflammation and oxidative stress [80]. Recently, a study demonstrated that eriodictyol alleviated TNBS-induced intestinal tissue injury in rats through repressing TLR4/NF-κB signaling pathway and reducing pro-inflammatory cytokines levels, such as TNF-α, IL-6, IL-1β, IL-2, and IL-12 [61].
Alkaloids
Alkaloids is a large group of chemicals characterized by the presence of nitrogen in their structure, which could not only downregulate inflammatory cytokines production, reduce oxidative stress, but also inhibit NF-κB levels [81]. An alkaloid was reported to improve the intestinal structure and barrier function in a DSS-induced colitis model [82].
Oxyberberine
Oxyberberine is an oxidized protoberberine alkaloid isolated from the Coptidis chinensis Franch [62]. It has been revealed that oxyberberine has a lot of pharmacological actions including anti-inflammatory, anti-tumor and anti-arrhythmic [83,84,85]. A research reported that oxyberberine alleviated intestinal mucosal inflammation and colonic mucosal injury in DSS-induced colitis mice by suppressing the TLR4–MyD88–NF-κB signaling pathway [62].
Dihydroberberine
Dihydroberberine is a natural occurring isoquinoline alkaloid extracted from the Coptidis chinensis Franch, which is a hydrogenated derivative of berberine [86]. Furthermore, numerous studies have shown that it has stronger anti-inflammatory, anti-atherosclerotic and hypolipidemic activities than berberine does [87]. It was shown that dihydroberberine treatment observably blocked the TLR4/MyD88/NF-κB signaling pathway by inhibiting the protein expression of TLR4, MyD88 and p-IκBα, which in turn suppressed the inflammatory responses and restored gut barrier function. Therefore, dihydroberberine produced a significant protective effect on DSS-induced colitis models [63].
Piperine
Piper species have multiple effects and have been used in traditional medicine to treat a variety of diseases, such as menstrual pain, sleeping problems, tuberculosis, chronic gut-related pain, respiratory tract infections, and arthritic conditions [88].
Piperine was the primary lipophilic component extracted from black pepper (Piper nigrum) and long pepper (Piper longum), which has been reported to be effective against metabolic syndrome and have anti-inflammatory activity [89]. Piperine significantly reduced inflammatory mediators in DSS-induced colitis [90]. According to one research, piperidine not only inhibited the abnormal secretion of pro-inflammatory mediators, including NO, cytokine TNF-α, but also reduced free fatty acid (FFA)-induced TLR4-mediated inflammation [64].
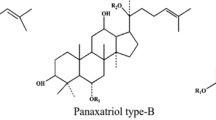
Terpenoids
Terpenoids is a large group of chemicals produced mainly by flowering plants, and to date, about one thousand terpenoids have been isolated [91]. According to the number of their isoprene units, they are divided into several categories, including hemiterpenoids, monoterpenoids, sesquiterpenoids, etc. [92]. It has been shown that terpenoids ameliorated experimental colitis by reducing colonic injury and inflammation and possibly by decreasing permeability [93].
Miltirone
Miltirone is one of the bioactive diterpene quinones extracted from Salvia miltiorrhiza Bunge. It has been reported to have a wide range of activities such as antioxidant, anti-inflammatory effects, etc. [94, 95]. Miltirone could significantly ameliorate the clinical symptoms of TNBS-induced IBD in mice by reducing the levels of inflammatory cytokines, decreasing the protein and mRNA level of IQGAP2, TLR4, MyD88, NF-kB p65. Therefore, the anti-inflammation effect of miltirone in IBD may be related to the TLR4/NF-kB/IQGAP2 signaling pathway [65].
Paeoniflorin
Paeoniflorin is the main bioactive component of Paeonia lactiflora Pall, which is a water-soluble monoterpene glycoside [96]. Paeonia root is one of the famous natural medicines in China, which has been used as medicine in traditional Chinese medicine for thousands of years [97]. Paeoniflorin has been reported to have anti-inflammatory, immunomodulatory, and anti-arthritic effects [98, 99]. A recent investigation (article in Chinese) indicated that the symptoms of oxazolone-induced colitis was effectively improved by paeoniflorin [100]. Paeoniflorin treatment was reported to lead to significant improvement of DSS-induced colitis by significantly reversing the upregulation of TLR4, decreasing the activity of MPO, reducing the production of inflammatory cytokines (TNF-αand IL-6), downregulating inflammatory mediators (MCP-1, Cox-2, IFN-γ, TNF-α, IL-6, and IL-17), and limiting the inflammatory (histological) response [66].
Conclusions and perspective
Today, the incidence of inflammatory bowel disease is increasing in Asian countries, including China, with globalization and lifestyle changes, especially dietary habits. Previous studies have identified that TLR4 signaling pathway plays a key role in the development of IBD. Therefore, targeting the TLR4 signaling pathway for the treatment of IBD is an effective approach. The nucleotide-binding domain and leucine-rich repeat containing (NLR) family is also an important factor to release cytokines and to form the inflammasome, which can form multiprotein complexes termed “inflammasomes” [101]. Among these inflammasomes, the NLRP3 inflammasome, one of NLRs, has been extensively studied of late [102]. Recent studies have suggested that NLRP3 governed the productions of pro-inflammatory cytokines, and is associated with the pathogenesis of more common inflammatory diseases [103]. TLR4 has been reported to regulate the activation of NF-κB p65, which affects the expression of NLRP3/IL-1β [104]. Therefore, targeting TLR4 synergistically with NLRP3 is also an effective way to treat IBD. There are many synthetic drugs being used to treat IBD, but the problem with these drugs is that they have many side effects. However, phytochemicals have been reported to have significant advantages in the treatment of IBD with few negative outcomes. Therefore, it is prudent to consider phytochemicals that modulate TLR4 signaling pathway as potential candidates for IBD treatment, but there are still challenges in bioavailability and delivery. Specifically, this review has focused on phytochemicals that inhibit TLR4 signaling pathway and ameliorate IBD symptoms in vivo in animal model systems. Unfortunately, to date, few clinical trials have been conducted targeting IBD pathobiology by TLR4 modulators. This raises the importance of further experiments and clinical trials focusing on IBD therapy through TLR4-modulating agents. In the future, numerous clinical studies are needed to validate the beneficial effects of phytochemicals targeting TLR4 in the treatment of IBD and to develop new drugs. In the current context of global environmental change, and with biodiversity declining significantly, conserving medicinal plants for treating human illness and maintaining the integrity of the associated local ecological knowledge were recognized as an important component of the Sustainable Development Goal [105]. However, the decline in plant and animal species and the global reduction in the area of nature reserves are challenges affecting biodiversity. Therefore, increasing international cooperation is needed to protect biodiversity.
Availability of data and materials
All data are available in the manuscript and they are showed in figures and tables.
Abbreviations
- BCG:
-
Bacillus Calmette–Guerin
- CD:
-
Crohn’s disease
- CD14:
-
Cluster of differentiation 14
- COVID-19:
-
Corona Virus Disease 2019
- Cox-2:
-
Cyclo-oxygenase-2
- CRP:
-
C-reaction protein
- DAMPs:
-
Damage-associated molecular patterns
- DSS:
-
Dextran sulphate sodium
- FDA:
-
U.S. Food and Drug Administration
- FFA:
-
Free fatty acid
- HPV:
-
Human papillomavirus
- IBD:
-
Inflammatory bowel disease
- ICAM-1:
-
Intercellular adhesion molecule-1
- IFN-γ:
-
Interferon-γ
- IL:
-
Interleukin
- iNOS:
-
Inducible nitric oxide synthase
- IQGAP2:
-
IQ-domain GTPase-activating protein 2
- IRAK4:
-
IL-1R-associated kinase 4
- IROs:
-
Immunoregulatory oligonucleotides
- IκB:
-
IkappaB
- LPS:
-
Lipopolysaccharide
- LRR:
-
Leucine-rich repeat
- MAPK:
-
Mitogen-activated protein kinase
- MCP-1:
-
Monocyte chemoattractant protein-1
- MD-2:
-
Myeloid differentiation factor 2
- MPLA:
-
Monophosphoryl lipid A
- MPO:
-
Myeloperoxidase
- mRNA:
-
Messenger RNA
- MyD88:
-
Myeloid differentiation 88
- NF-κB:
-
Nuclear factor-kappaB
- NLRs:
-
NOD-like receptors
- NO:
-
Nitric oxide
- PAMPs:
-
Pathogen-associated molecular patterns
- PPRs:
-
Pathogen pattern recognition molecules
- PRR:
-
Primary pattern recognition receptor
- TIR:
-
Toll/interleukin-1 receptor
- TLR4:
-
Toll-like receptor 4
- TLRs:
-
Toll-like receptors
- TNBS:
-
2,4,6-Trinitrobenzene sulfonic acid
- TNF-α:
-
Tumor necrosis factor-α
- TRAF6:
-
TNF receptor-associated factor 6
- UC:
-
Ulcerative colitis
References
Veeresham C. Natural products derived from plants as a source of drugs. J Adv Pharm Technol Res. 2012;3(4):200–1.
Xu C. Trends in phytochemical research. J Food Biochem. 2019;43(6):e12913.
Molyneux RJ, Lee ST, Gardner DR, Panter KE, James LF. Phytochemicals: the good, the bad and the ugly? Phytochemistry. 2007;68(22–24):2973–85.
Fridlender M, Kapulnik Y, Koltai H. Plant derived substances with anti-cancer activity: from folklore to practice. Front Plant Sci. 2015;6:799.
Bellik Y, Boukraâ L, Alzahrani HA, Bakhotmah BA, Abdellah F, Hammoudi SM, et al. Molecular mechanism underlying anti-inflammatory and anti-allergic activities of phytochemicals: an update. Molecules. 2012;18(1):322–53.
Rosen MJ, Dhawan A, Saeed SA. Inflammatory bowel disease in children and adolescents. JAMA Pediatr. 2015;169(11):1053–60.
Verstockt B, Ferrante M, Vermeire S, Van Assche G. New treatment options for inflammatory bowel diseases. J Gastroenterol. 2018;53(5):585–90.
Hossen I, Hua W, Ting L, Mehmood A, Jingyi S, Duoxia X, et al. Phytochemicals and inflammatory bowel disease: a review. Crit Rev Food Sci Nutr. 2020;60(8):1321–45.
Zhu F, Du B, Xu B. Anti-inflammatory effects of phytochemicals from fruits, vegetables, and food legumes: a review. Crit Rev Food Sci Nutr. 2018;58(8):1260–70.
Hnatyszyn A, Hryhorowicz S, Kaczmarek-Ryś M, Lis E, Słomski R, Scott RJ, et al. Colorectal carcinoma in the course of inflammatory bowel diseases. Hered Cancer Clin Pract. 2019;17:18.
Kalla R, Ventham NT, Satsangi J, Arnott ID. Crohn’s disease. BMJ. 2014;349:g6670.
Tatiya-Aphiradee N, Chatuphonprasert W, Jarukamjorn K. Immune response and inflammatory pathway of ulcerative colitis. J Basic Clin Physiol Pharmacol. 2018;30(1):1–10.
Lu Y, Li X, Liu S, Zhang Y, Zhang D. Toll-like receptors and inflammatory bowel disease. Front Immunol. 2018;9:72.
Dejban P, Nikravangolsefid N, Chamanara M, Dehpour A, Rashidian A. The role of medicinal products in the treatment of inflammatory bowel diseases (IBD) through inhibition of TLR4/NF-kappaB pathway. Phytother Res. 2021;35(2):835–45.
Rogler G. Gastrointestinal and liver adverse effects of drugs used for treating IBD. Best Pract Res Clin Gastroenterol. 2010;24(2):157–65.
Tam JSY, Coller JK, Hughes PA, Prestidge CA, Bowen JM. Toll-like receptor 4 (TLR4) antagonists as potential therapeutics for intestinal inflammation. Indian J Gastroenterol. 2021;40(1):5–21.
Farzaei MH, Bahramsoltani R, Abdolghaffari AH, Sodagari HR, Esfahani SA, Rezaei N. A mechanistic review on plant-derived natural compounds as dietary supplements for prevention of inflammatory bowel disease. Expert Rev Gastroenterol Hepatol. 2016;10(6):745–58.
Molteni M, Bosi A, Rossetti C. Natural products with toll-like receptor 4 antagonist activity. Int J Inflamm. 2018;2018:2859135.
Mokhtari Y, Pourbagheri-Sigaroodi A, Zafari P, Bagheri N, Ghaffari SH, Bashash D. Toll-like receptors (TLRs): an old family of immune receptors with a new face in cancer pathogenesis. J Cell Mol Med. 2021;25(2):639–51.
Kashani B, Zandi Z, Pourbagheri-Sigaroodi A, Bashash D, Ghaffari SH. The role of toll-like receptor 4 (TLR4) in cancer progression: a possible therapeutic target? J Cell Physiol. 2021;236(6):4121–37.
Ciesielska A, Matyjek M, Kwiatkowska K. TLR4 and CD14 trafficking and its influence on LPS-induced pro-inflammatory signaling. Cell Mol Life Sci. 2021;78(4):1233–61.
Botos I, Segal DM, Davies DR. The structural biology of Toll-like receptors. Structure. 2011;19(4):447–59.
Krishnan J, Selvarajoo K, Tsuchiya M, Lee G, Choi S. Toll-like receptor signal transduction. Exp Mol Med. 2007;39(4):421–38.
Newton K, Dixit VM. Signaling in innate immunity and inflammation. Cold Spring Harb Perspect Biol. 2012;4(3):a006049.
McClure R, Massari P. TLR-dependent human mucosal epithelial cell responses to microbial pathogens. Front Immunol. 2014;5:386.
da Silva Correia J, Soldau K, Christen U, Tobias PS, Ulevitch RJ. Lipopolysaccharide is in close proximity to each of the proteins in its membrane receptor complex transfer from CD14 to TLR4 and MD-2. J Biol Chem. 2001;276(24):21129–35.
Akira S, Takeda K, Kaisho T. Toll-like receptors: critical proteins linking innate and acquired immunity. Nat Immunol. 2001;2(8):675–80.
Kordjazy N, Haj-Mirzaian A, Haj-Mirzaian A, Rohani MM, Gelfand EW, Rezaei N, et al. Role of toll-like receptors in inflammatory bowel disease. Pharmacol Res. 2018;129:204–15.
Patra MC, Choi S. Recent progress in the development of Toll-like receptor (TLR) antagonists. Expert Opin Ther Pat. 2016;26(6):719–30.
Rezaei N. Therapeutic targeting of pattern-recognition receptors. Int Immunopharmacol. 2006;6(6):863–9.
Kanzler H, Barrat FJ, Hessel EM, Coffman RL. Therapeutic targeting of innate immunity with Toll-like receptor agonists and antagonists. Nat Med. 2007;13(5):552–9.
Makkouk A, Abdelnoor AM. The potential use of Toll-like receptor (TLR) agonists and antagonists as prophylactic and/or therapeutic agents. Immunopharmacol Immunotoxicol. 2009;31(3):331–8.
Mifsud EJ, Tan AC, Jackson DC. TLR agonists as modulators of the innate immune response and their potential as agents against infectious disease. Front Immunol. 2014;5:79.
Hernandez A, Patil NK, Stothers CL, Luan L, McBride MA, Owen AM, et al. Immunobiology and application of toll-like receptor 4 agonists to augment host resistance to infection. Pharmacol Res. 2019;150:104502.
Murphey ED, Fang G, Sherwood ER. Endotoxin pretreatment improves bacterial clearance and decreases mortality in mice challenged with Staphylococcus aureus. Shock. 2008;29(4):512–8.
Simons MP, O’Donnell MA, Griffith TS. Role of neutrophils in BCG immunotherapy for bladder cancer. Urol Oncol. 2008;26(4):341–5.
Strayer DR, Carter WA, Stouch BC, Stevens SR, Bateman L, Cimoch PJ, et al. A double-blind, placebo-controlled, randomized, clinical trial of the TLR-3 agonist rintatolimod in severe cases of chronic fatigue syndrome. PLoS ONE. 2012;7(3):e31334.
Kashani B, Zandi Z, Karimzadeh MR, Bashash D, Nasrollahzadeh A, Ghaffari SH. Blockade of TLR4 using TAK-242 (resatorvid) enhances anti-cancer effects of chemotherapeutic agents: a novel synergistic approach for breast and ovarian cancers. Immunol Res. 2019;67(6):505–16.
McKeage K, Romanowski B. AS04-adjuvanted human papillomavirus (HPV) types 16 and 18 vaccine (Cervarix®): a review of its use in the prevention of premalignant cervical lesions and cervical cancer causally related to certain oncogenic HPV types. Drugs. 2011;71(4):465–88.
Bonam SR, Partidos CD, Halmuthur SKM, Muller S. An overview of novel adjuvants designed for improving vaccine efficacy. Trends Pharmacol Sci. 2017;38(9):771–93.
Keshavarz A, Pourbagheri-Sigaroodi A, Zafari P, Bagheri N, Ghaffari SH, Bashash D. Toll-like receptors (TLRs) in cancer; with an extensive focus on TLR agonists and antagonists. IUBMB Life. 2021;73(1):10–25.
Miller RL, Gerster JF, Owens ML, Slade HB, Tomai MA. Imiquimod applied topically: a novel immune response modifier and new class of drug. Int J Immunopharmacol. 1999;21(1):1–14.
Poulas K, Farsalinos K, Zanidis C. Activation of TLR7 and innate immunity as an efficient method against COVID-19 pandemic: imiquimod as a potential therapy. Front Immunol. 2020;11:1373.
Kandimalla ER, Bhagat L, Wang D, Yu D, Sullivan T, La Monica N, et al. Design, synthesis and biological evaluation of novel antagonist compounds of Toll-like receptors 7, 8 and 9. Nucleic Acids Res. 2013;41(6):3947–61.
Akira S. Innate immunity and adjuvants. Philos Trans R Soc Lond B Biol Sci. 2011;366(1579):2748–55.
Li TT, Ogino S, Qian ZR. Toll-like receptor signaling in colorectal cancer: carcinogenesis to cancer therapy. World J Gastroenterol. 2014;20(47):17699–708.
Takahashi K, Sugi Y, Hosono A, Kaminogawa S. Epigenetic regulation of TLR4 gene expression in intestinal epithelial cells for the maintenance of intestinal homeostasis. J Immunol. 2009;183(10):6522–9.
Garcia MM, Goicoechea C, Molina-Álvarez M, Pascual D. Toll-like receptor 4: a promising crossroads in the diagnosis and treatment of several pathologies. Eur J Pharmacol. 2020;874:172975.
Liu L, Li YH, Niu YB, Sun Y, Guo ZJ, Li Q, et al. An apple oligogalactan prevents against inflammation and carcinogenesis by targeting LPS/TLR4/NF-κB pathway in a mouse model of colitis-associated colon cancer. Carcinogenesis. 2010;31(10):1822–32.
Pandey N, Chauhan A, Jain N. TLR4 polymorphisms and expression in solid cancers. Mol Diagn Ther. 2018;22(6):683–702.
Chow JC, Young DW, Golenbock DT, Christ WJ, Gusovsky F. Toll-like receptor-4 mediates lipopolysaccharide-induced signal transduction. J Biol Chem. 1999;274(16):10689–92.
Poltorak A, He X, Smirnova I, Liu MY, Van Huffel C, Du X, et al. Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science. 1998;282(5396):2085–8.
Miggin SM, O’Neill LA. New insights into the regulation of TLR signaling. J Leukoc Biol. 2006;80(2):220–6.
Duchmann R, Kaiser I, Hermann E, Mayet W, Ewe K, Meyer zum Büschenfelde KH. Tolerance exists towards resident intestinal flora but is broken in active inflammatory bowel disease (IBD). Clin Exp Immunol. 1995;102(3):448–55.
Lange S, Delbro DS, Jennische E, Mattsby-Baltzer I. The role of the Lps gene in experimental ulcerative colitis in mice. APMIS. 1996;104(11):823–33.
Brown M, Hughes KR, Moossavi S, Robins A, Mahida YR. Toll-like receptor expression in crypt epithelial cells, putative stem cells and intestinal myofibroblasts isolated from controls and patients with inflammatory bowel disease. Clin Exp Immunol. 2014;178(1):28–39.
Belmonte L, Beutheu Youmba S, Bertiaux-Vandaële N, Antonietti M, Lecleire S, Zalar A, et al. Role of toll like receptors in irritable bowel syndrome: differential mucosal immune activation according to the disease subtype. PLoS ONE. 2012;7(8):e42777.
Zeng Z, Zhan L, Liao H, Chen L, Lv X. Curcumin improves TNBS-induced colitis in rats by inhibiting IL-27 expression via the TLR4/NF-κB signaling pathway. Planta Med. 2013;79(2):102–9.
Cui L, Feng L, Zhang ZH, Jia XB. The anti-inflammation effect of baicalin on experimental colitis through inhibiting TLR4/NF-κB pathway activation. Int Immunopharmacol. 2014;23(1):294–303.
Dou W, Zhang J, Sun A, Zhang E, Ding L, Mukherjee S, et al. Protective effect of naringenin against experimental colitis via suppression of Toll-like receptor 4/NF-κB signalling. Br J Nutr. 2013;110(4):599–608.
Hu LH, Liu JY, Yin JB. Eriodictyol attenuates TNBS-induced ulcerative colitis through repressing TLR4/NF-kB signaling pathway in rats. Kaohsiung J Med Sci. 2021;37(9):812–8.
Li C, Ai G, Wang Y, Lu Q, Luo C, Tan L, et al. Oxyberberine, a novel gut microbiota-mediated metabolite of berberine, possesses superior anti-colitis effect: impact on intestinal epithelial barrier, gut microbiota profile and TLR4-MyD88-NF-κB pathway. Pharmacol Res. 2020;152:104603.
Li C, Dong N, Wu B, Mo Z, Xie J, Lu Q. Dihydroberberine, an isoquinoline alkaloid, exhibits protective effect against dextran sulfate sodium-induced ulcerative colitis in mice. Phytomedicine. 2021;90:153631.
Gupta RA, Motiwala MN, Dumore NG, Danao KR, Ganjare AB. Effect of piperine on inhibition of FFA induced TLR4 mediated inflammation and amelioration of acetic acid induced ulcerative colitis in mice. J Ethnopharmacol. 2015;164:239–46.
Wang H, Gu J, Hou X, Chen J, Yang N, Liu Y, et al. Anti-inflammatory effect of miltirone on inflammatory bowel disease via TLR4/NF-κB/IQGAP2 signaling pathway. Biomed Pharmacother. 2017;85:531–40.
Zhang J, Dou W, Zhang E, Sun A, Ding L, Wei X, et al. Paeoniflorin abrogates DSS-induced colitis via a TLR4-dependent pathway. Am J Physiol Gastrointest Liver Physiol. 2014;306(1):G27-36.
Shahidi F, Yeo J. Bioactivities of phenolics by focusing on suppression of chronic diseases: a review. Int J Mol Sci. 2018;19(6):1573.
Shapiro H, Singer P, Halpern Z, Bruck R. Polyphenols in the treatment of inflammatory bowel disease and acute pancreatitis. Gut. 2007;56(3):426–35.
Romier B, Schneider YJ, Larondelle Y, During A. Dietary polyphenols can modulate the intestinal inflammatory response. Nutr Rev. 2009;67(7):363–78.
Duvoix A, Blasius R, Delhalle S, Schnekenburger M, Morceau F, Henry E, et al. Chemopreventive and therapeutic effects of curcumin. Cancer Lett. 2005;223(2):181–90.
Lubbad A, Oriowo MA, Khan I. Curcumin attenuates inflammation through inhibition of TLR-4 receptor in experimental colitis. Mol Cell Biochem. 2009;322(1–2):127–35.
Wang PQ, Liu Q, Xu WJ, Yu YN, Zhang YY, Li B, et al. Pure mechanistic analysis of additive neuroprotective effects between baicalin and jasminoidin in ischemic stroke mice. Acta Pharmacol Sin. 2018;39(6):961–74.
Wang CZ, He H, Wang X, Yuan CS. Trends in scientific publications of Chinese medicine. Am J Chin Med. 2012;40(6):1099–108.
Hang Y, Qin X, Ren T, Cao J. Baicalin reduces blood lipids and inflammation in patients with coronary artery disease and rheumatoid arthritis: a randomized, double-blind, placebo-controlled trial. Lipids Health Dis. 2018;17(1):146.
Wu T, Weng Z, Xu J, Wen G, Yu Y, Chai Y. Baicalin alleviates osteomyelitis by regulating TLR2 in the murine model. Pathog Dis. 2018;76(2):flx123.
Zaidun NH, Thent ZC, Latiff AA. Combating oxidative stress disorders with citrus flavonoid: Naringenin. Life Sci. 2018;208:111–22.
Wang Q, Ou Y, Hu G, Wen C, Yue S, Chen C, et al. Naringenin attenuates non-alcoholic fatty liver disease by down-regulating the NLRP3/NF-κB pathway in mice. Br J Pharmacol. 2020;177(8):1806–21.
Al-Rejaie SS, Abuohashish HM, Al-Enazi MM, Al-Assaf AH, Parmar MY, Ahmed MM. Protective effect of naringenin on acetic acid-induced ulcerative colitis in rats. World J Gastroenterol. 2013;19(34):5633–44.
Kwon EY, Choi MS. Dietary eriodictyol alleviates adiposity, hepatic steatosis, insulin resistance, and inflammation in diet-induced obese mice. Int J Mol Sci. 2019;20(5):1227.
Hu Q, Zhang DD, Wang L, Lou H, Ren D. Eriodictyol-7-O-glucoside, a novel Nrf2 activator, confers protection against cisplatin-induced toxicity. Food Chem Toxicol. 2012;50(6):1927–32.
Cushnie TP, Cushnie B, Lamb AJ. Alkaloids: an overview of their antibacterial, antibiotic-enhancing and antivirulence activities. Int J Antimicrob Agents. 2014;44(5):377–86.
Zhao WC, Song LJ, Deng HZ. Effect of sophoridine on dextran sulfate sodium-induced colitis in C57BL/6 mice. J Asian Nat Prod Res. 2010;12(11):925–33.
Li CL, Tan LH, Wang YF, Luo CD, Chen HB, Lu Q, et al. Comparison of anti-inflammatory effects of berberine, and its natural oxidative and reduced derivatives from Rhizoma Coptidis in vitro and in vivo. Phytomedicine. 2019;52:272–83.
Chi JF, Chu SH, Lee CS, Chou NK, Su MJ. Mechanical and electrophysiological effects of 8-oxoberberine (JKL1073A) on atrial tissue. Br J Pharmacol. 1996;118(3):503–12.
Singh S, Verma M, Malhotra M, Prakash S, Singh TD. Cytotoxicity of alkaloids isolated from Argemone mexicana on SW480 human colon cancer cell line. Pharm Biol. 2016;54(4):740–5.
Jin Y, Khadka DB, Cho WJ. Pharmacological effects of berberine and its derivatives: a patent update. Expert Opin Ther Pat. 2016;26(2):229–43.
Chen J, Cao J, Fang L, Liu B, Zhou Q, Sun Y, et al. Berberine derivatives reduce atherosclerotic plaque size and vulnerability in apoE(-/-) mice. J Transl Med. 2014;12:326.
Kim HG, Han EH, Jang WS, Choi JH, Khanal T, Park BH, et al. Piperine inhibits PMA-induced cyclooxygenase-2 expression through downregulating NF-κB, C/EBP and AP-1 signaling pathways in murine macrophages. Food Chem Toxicol. 2012;50(7):2342–8.
Diwan V, Poudyal H, Brown L. Piperine attenuates cardiovascular, liver and metabolic changes in high carbohydrate, high fat-fed rats. Cell Biochem Biophys. 2013;67(2):297–304.
Hu D, Wang Y, Chen Z, Ma Z, You Q, Zhang X, et al. The protective effect of piperine on dextran sulfate sodium induced inflammatory bowel disease and its relation with pregnane X receptor activation. J Ethnopharmacol. 2015;169:109–23.
Pichersky E, Raguso RA. Why do plants produce so many terpenoid compounds? New Phytol. 2018;220(3):692–702.
El-Baba C, Baassiri A, Kiriako G, Dia B, Fadlallah S, Moodad S, et al. Terpenoids’ anti-cancer effects: focus on autophagy. Apoptosis. 2021;26(9–10):491–511.
Kazi HA, Qian Z. Crocetin reduces TNBS-induced experimental colitis in mice by downregulation of NFkB. Saudi J Gastroenterol. 2009;15(3):181–7.
Wang X, Morris-Natschke SL, Lee KH. New developments in the chemistry and biology of the bioactive constituents of Tanshen. Med Res Rev. 2007;27(1):133–48.
Lee WY, Chiu LC, Yeung JH. Cytotoxicity of major tanshinones isolated from Danshen (Salvia miltiorrhiza) on HepG2 cells in relation to glutathione perturbation. Food Chem Toxicol. 2008;46(1):328–38.
Shi D, Li X, Li D, Zhao Q, Shen Y, Yan H, et al. Oral administration of paeoniflorin attenuates allergic contact dermatitis by inhibiting dendritic cell migration and Th1 and Th17 differentiation in a mouse model. Int Immunopharmacol. 2015;25(2):432–9.
Jin L, Zhang LM, Xie KQ, Ye Y, Feng L. Paeoniflorin suppresses the expression of intercellular adhesion molecule-1 (ICAM-1) in endotoxin-treated human monocytic cells. Br J Pharmacol. 2011;164(2b):694–703.
Tsuboi H, Hossain K, Akhand AA, Takeda K, Du J, Rifa’i M, et al. Paeoniflorin induces apoptosis of lymphocytes through a redox-linked mechanism. J Cell Biochem. 2004;93(1):162–72.
Zhang W, Dai SM. Mechanisms involved in the therapeutic effects of Paeonia lactiflora Pallas in rheumatoid arthritis. Int Immunopharmacol. 2012;14(1):27–31.
Zhou Y, Wang H, Li YS, Tao YW, Zhang JY, Zhang ZQ. Paeoniflorin increases beta-defensin expression and attenuates lesion in the colonic mucosa from mice with oxazolone-induced colitis. Yao Xue Xue Bao. 2010;45(1):37–42.
He Y, Hara H, Núñez G. Mechanism and regulation of NLRP3 inflammasome activation. Trends Biochem Sci. 2016;41(12):1012–21.
He X, Wei Z, Wang J, Kou J, Liu W, Fu Y, et al. Alpinetin attenuates inflammatory responses by suppressing TLR4 and NLRP3 signaling pathways in DSS-induced acute colitis. Sci Rep. 2016;6:28370.
Luo YP, Jiang L, Kang K, Fei DS, Meng XL, Nan CC, et al. Hemin inhibits NLRP3 inflammasome activation in sepsis-induced acute lung injury, involving heme oxygenase-1. Int Immunopharmacol. 2014;20(1):24–32.
Chen Z, Zhang Y, Lin R, Meng X, Zhao W, Shen W, et al. Cronobacter sakazakii induces necrotizing enterocolitis by regulating NLRP3 inflammasome expression via TLR4. J Med Microbiol. 2020;69(5):748–58.
Thorn JPR, Thornton TF, Helfgott A, Willis KJ. Indigenous uses of wild and tended plant biodiversity maintain ecosystem services in agricultural landscapes of the Terai Plains of Nepal. J Ethnobiol Ethnomed. 2020;16(1):33.
Acknowledgements
The authors would like to thank the reviewers and also the authors of all references.
Funding
This study was supported by the Luzhou People’s Government-Southwest Medical University Science and Technology Strategic Cooperation Climbing Plan (No. 2021LZXNYD-D14).
Author information
Authors and Affiliations
Contributions
WD and LH conducted the analytical part, wrote the manuscript. WQ downloaded the reference and processed the graph and the table in the manuscript. SL and HX conceived and coordinated the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dai, W., Long, L., Wang, X. et al. Phytochemicals targeting Toll-like receptors 4 (TLR4) in inflammatory bowel disease. Chin Med 17, 53 (2022). https://doi.org/10.1186/s13020-022-00611-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13020-022-00611-w