Abstract
Background
Corticosteroid injections are commonly used for the treatment of plantar fasciitis. In recent years, ultrasound-guided multipuncture treatment of the fascia has been described in the literature. Our study aimed to compare the effectiveness of these two techniques in the treatment of plantar fasciitis.
Methods
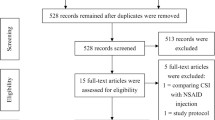
The outcomes achieved over 120 days following the use of these techniques to treat plantar fasciitis were examined. A total of 81 patients were randomly selected for the study; 41 were treated with ultrasound-guided multipuncture and 40 with ultrasound-guided corticosteroid injection. Clinical examinations and ultrasound assessments were performed before treatment and at 30, 60 and 120 days post-treatment. Clinical assessments included the use of a visual analog scale (VAS) to record pain and the Foot Function Index (FFI) to evaluate function. Ultrasound was used to measure the thickness of the plantar fascia.
Results
Both the ultrasound-guided multipuncture and corticosteroid injection techniques were associated with significant functional and echographic improvements at 4 months post-treatment (P < 0.001). Pain did not improve significantly after 120 days with ultrasound-guided corticosteroid injection, whereas significant pain reduction was observed with ultrasound-guided multipuncture.
Conclusion
Corticosteroid injection provides better short-term results in terms of VAS pain and FFI scores. However, ultrasound-guided multipuncture shows superior outcomes in VAS pain and FFI scores at 120 days.
Similar content being viewed by others
Introduction
It is estimated that 10% of the population experiences heel pain at some point in their lives, although there are few high-quality epidemiological studies available [1]. Plantar fasciitis is the most common cause of pain in the lower heel in the United States (US), affecting over 2 million people annually. Its high prevalence in the US (approximately 4–7%) results in an annual expenditure of $284 million on treatments [2]. The incidence of plantar fasciitis is higher among individuals aged 40 to 60 years, with a female-to-male ratio of 2:1 [1, 3]. Plantar fasciitis accounts for 25% of all foot injuries in athletes and is the most common cause of heel pain in this group [4].
The degeneration of the plantar fascia causes plantar fasciitis due to repetitive micro-tears resulting from trauma or overuse rather than a primary inflammatory reaction [5]. Hence, the terms “plantar fasciosis” and, more recently, “plantar fasciopathy” have been coined in the literature. The exact cause of plantar fasciitis is currently unknown, although it is believed to be multifactorial, with abnormal biomechanics and delayed collagen healing in the fascia as possible contributors [6].
Risk factors include excessive foot pronation or flat feet, high-arched feet, shortening of the Achilles tendon or gastrocnemius muscle, limb length discrepancy, obesity, overtraining, prolonged standing or walking, and improper gait [7,8,9,10]. Most patients seek treatment within the first year, and in the vast majority of cases, the pain resolves within this period. Numerous treatments have been proposed in the medical literature, with most specialists opting for conservative treatment, which is effective in 70–80% of cases. The most commonly used approaches are physical therapy, therapies such as shock wave treatment [11,12,13], plantar orthotics, gastrocnemius stretching, and glucocorticosteroid injections (GCI) [9]. In recalcitrant cases, surgery is an accepted therapy, with several minimal incision techniques published in recent years [14, 15]. Other regenerative therapies appear to offer promising results [16].
The most common sonographic findings of plantar fasciitis are fusiform thickening, fiber disorganization, surrounding soft tissue edema and entheseal bone formation [17]. Static and dynamic ultrasound assessment is currently considered the first-line diagnostic approach to accurately differentiate the fasciosis from focal disruption of the plantar fascia. Dynamic ultrasound evaluation is mandatory to evaluate the fascial gliding and displacement of fascial ends, but also for differential diagnosis (e.g., nerve entrapment and stress fracture) [18].
Ultrasound-guided multipuncture (MP) for plantar fasciitis was described by Luca Maria Sconfienza [19, 20]. The author describes performing 10 to 20 punctures of the plantar fascia under local anesthesia with a 20-gauge beveled needle, guided by ultrasound, and adding a corticosteroid to minimize post-procedure pain.
Our study aimed to compare ultrasound-guided multipuncture without post-treatment corticosteroid for plantar fasciitis with a well-established technique in the literature, GCI. We hypothesize that MP is effective for the treatment ofplantar fasciitis.
Materials and methods
Study design and patients
Inclusion Criteria: To be included in the study, (1) patients had to be adults, (2) present with symptoms consistent withplantar fasciitis, (3) exhibit a plantar fascia thickness greater than 0.4 centimeters as described by McMillan et al. [21], and (4) consent to participate in the study.
Exclusion Criteria: Exclusion criteria were: (1) having systemic diseases or non-podiatric morphofunctional changes that could affect the ankle and foot, potentially leading to significant clinical discrepancies in the lower limbs, asymmetries, or evident clinical scoliosis; (2) having received any treatment (medical, orthopedic, and/or invasive) for the foot in the past 3 months; (3) plantar fasciitis associated with another condition such as nerve entrapment; and (4) difficulties understanding the instructions to be followed during the treatment.
All patients underwent a clinical and ultrasound evaluation before treatment and after 30, 60, and 120 days. Clinical evaluation was based on a visual analog scale (VAS) [22] (0–10) and the Foot Function Index (FFI) [23, 24], which assesses function on a scale of 0 to 100. In the pre-treatment evaluation, patients were classified as sedentary, active, or athletic based on their daily physical activity, as well as whether it was the first occurrence of the disease, a recurrence, or chronic [25]. Other factors evaluated included sex, body mass index, the presence of vascularization in the plantar fascia as seen on ultrasound at the initial evaluation, and whether the plantar fascia was biconvex [26] or flattened (Fig. 1).
Plantar fascia with normal morphology (a) (b) and plantar fascia with biconvex morphology. The dotted lines show the plantar fascia thickness measurement [26]
Our clinical trial was performed in accordance with the principles of the Declaration of Helsinki of 1964 (2013 revision) [27] and was approved by the Research Ethics Committee of our center (2093-N-21). All participants provided informed consent to participate in the study and for the reproduction of their clinical and radiological data.
We performed the clinical trial on 81 patients diagnosed with plantar fasciitis who voluntarily participated in the study. These patients were randomly treated with either GCI or MP without knowing which treatment they were receiving between April 2018 and April 2023. The minimum follow-up period post-treatment was 120 days. Regarding sample size calculation, considering a 95% confidence level, 80% statistical power, and a standardized difference of 0.65, at least 38 patients per group were required to meet the study requirements.
All patients had experienced the classic symptoms of plantar fasciitis, including pain upon taking the first steps after waking up or after sitting for prolonged periods. Patients reported tenderness on palpation of the proximal plantar fascia and indicated that the pain worsened as the day progressed.
The diagnosis was established based on symptoms and confirmed by ultrasound using high-resolution equipment (Alpinion Ecube 9) with a 6 to 12 MHz linear transducer (Fig. 2).
Interventional procedures
Study subjects were randomized based on their phone number; if the last digit was even, the GCI technique was performed, and if it was odd, the MP technique was used. The treatment was performed in the prone position without the patient knowing which therapeutic technique was being administered by a therapist with 10 years of experience (RMS) in ultrasound-guided treatments of the foot and ankle.
All subjects received posterior tibial nerve block anesthesia with 2% mepivacaine prior to the procedure. The following steps were followed: the ultrasound probe was covered with a 3 M TEGARDERM sterile transparent dressing to maintain skin asepsis, and 2% aqueous chlorhexidine was sprayed on it. The patient’s foot and ankle were also cleaned with aqueous chlorhexidine. With the patient in the prone position (Fig. 3), after waiting for the antiseptic to take effect, the posterior tibial nerve was located with the ultrasound in the area proximal to the medial malleolus. A syringe loaded with local anesthetic and a 27G needle was inserted through the skin to reach the perineurium under ultrasound guidance in-plane needle insertion, and 5 ml of 2% mepivacaine was subsequently injected [28] (Figs. 4 and 5).
With the patient remaining in the prone position, in the case of the multipuncture technique, the depth of the puncture was measured using ultrasound. Approaching from the medial side of the foot, a 21G needle was inserted through the skin under ultrasound visualization, using the in-plane technique in a medial-to-lateral approach, ensuring the entire needle was visible (Figs. 6 and 7). The plantar fascia was punctured multiple times, covering the entire area of abnormality with several punctures. The number of punctures needed to cover the affected area was recorded, with an average of 10.2 ± 1.9 punctures (Table 1).
In the case of GCI, with the patient in the prone position, the depth of the medication injection was also measured using ultrasound. From a medial approach, using an in-plane technique in a medial-to-lateral approach, ensuring the entire needle was visible, 1 mL of Celestone® Cronodose®, which is a marketed drug containing a mixture composed of 5.7 mg of betamethasone, 3 mg of betamethasone (as sodium phosphate), and 2.7 mg of betamethasone (as 3 mg of betamethasone acetate), plus 1 mL of 2% mepivacaine, were injected. Two-thirds of the volume was injected deep into the fascia and one-third superficially to the fascia under ultrasound visualization of the entire needle (Fig. 8). The decision on the injection site was based on the premise that deep injection of the plantar fascia seems to be more effective for pain reduction and improving fascia function [29], although the literature is heterogeneous regarding the injection site, with perifascial injection being common. This approach considers both aspects found in the literature on the subject [30].
Statistical analysis
A descriptive analysis was performed for all quantitative and qualitative data. The normality of the variables was assessed using the Shapiro-Wilk test, with the variables following a normal distribution (p > 0.05) except for the variables of previous treatment (p < 0.05) and body mass (p < 0.05).
The T-test or Mann-Whitney U test for independent samples was used in the comparative analysis of the two techniques. The Friedman two-way analysis of variance by ranks for related samples or repeated measures ANOVA was applied to study the progression over time of the study variables. Statistical analysis was performed using the IBM SPSS Statistics 25 software package with a 95% confidence level.
Results
In the group of patients who underwent multipuncture, the sample consisted of 40 (49.4%) subjects, while in the group of patients who received corticosteroid injection, there were 41 (50.6%) subjects (Table 2). The mean age of patients was 48.4 ± 10.3 years in the multipuncture group and 47.2 ± 15 years in the corticosteroid group. Most (62.5%) of the patients in the multipuncture group were male, while 37.5% were female, compared to 46.3% male and 53.7% female in the corticosteroid group. Pain on the VAS scale before treatment was 6.9 ± 1.3 in the multipuncture group and 6.9 ± 1.3 in the corticosteroid group. Function on the FFI scale was 62.8 ± 15.9 in the multipuncture group and 63 ± 14.7 in the corticosteroid group. There were no significant differences between the two procedure groups in pain and function variables, but there was a significant difference in the thickness of the plantar fascia, which was thicker on average in the corticosteroid group (Table 3).
Both techniques yielded different results at various time points regarding several evaluated variables. Both MP for plantar fasciitis and GCI were associated with significant functional and echographic improvements at 120 days post-treatment (p < 0.001)(Table 4 and 5). The pain did not significantly improve at 120 days with ultrasound-guided corticosteroid injection, but it did with ultrasound-guided multipuncture of the plantar fascia. Corticosteroid injection provided better pain outcomes on the VAS scale and function on the FFI scale at 30 days post-treatment (p < 0.001). At 60 days, there were no statistically significant differences between treatments (p < 0.001) (Table 6).
No adverse events were reported during the procedure. Data on perceived pain during treatment were collected from the patients, with slightly higher pain perception reported during multipuncture treatment, likely due to increased manipulation of the area by the clinician.
There were no statistically significant differences (p > 0.05) between the two procedures regarding patient classification based on daily physical activity, onset of the disease (first occurrence/recurrence/chronic), sex, presence of vascularization in the plantar fascia visualized on ultrasound at the initial evaluation, or the biconvex or flattened shape of the plantar fascia.
Statistically significant differences (p < 0.05) were found regarding previous treatment, with the multipuncture group having more prior treatments. The duration of the condition prior to intervention was longer in patients treated with multipuncture, and the body mass index was higher in the multipuncture group. The thickness of the plantar fascia was greater in the corticosteroid group.
Discussion
The present study aimed to evaluate the efficacy of MP by comparing it with GCI in patients diagnosed with plantar fasciitis from the clinical, functional and plantar fascia thickness points of view.
In light of the results obtained, the present study demonstrated that GCI provides better VAS and FFI pain outcomes at 30 days (p < 0.001), and MP provides better VAS and FFI pain outcomes at 120 days (p < 0.001). Regarding fascial thickness, the results are similar at 120 days (p < 0.001).
Both GCI and MP were associated with significant improvements in function (FFI scale) and plantar fascia thickness as measured by ultrasound. The plantar fascia thickness does not reach normal values, even if the symptoms disappear. With respect to pain measured with the VAS scale, they present different results, with GCI being more effective than MP in the short term and less effective in the long term [31,32,33,34,35,36].
In the present study, both treatments were guided by ultrasound. There is evidence to suggest that ultrasound-guided corticosteroid puncture is more effective than blind corticosteroid puncture [37]. Ultrasound has been routinely used in the authors’ clinic because it allows precise needle placement and thus minimizes potential damage to healthy tissue [38]. In fact, a number of adverse effects of GCI have been reported in the literature, including fascia rupture and plantar fat atrophy [39, 40], which could be avoided with ultrasound guidance. In the present study, no patient treated with either technique had any adverse effects at 120 days.
Some of the adverse reactions to injection of the plantar fascia with glucocorticoids are alterations in the fascia, including complete or partial tear and necrosis of adipose tissue [41].
Indeed, during the follow-up phase (after the injection), a focal hypoechoic gap of TPF with protrusion of the hyperechoic heel fat pad inside can be accurately observed using high-resolution ultrasound. Ultrasound examination is the first-line modality to localize the tissue lesion and measure its extension. Furthermore, dynamic maneuvres facilitate confirmation of a complete tear by verifying the presence of a gap between the two torn parts of the plantar fascia [42].
Multiple perforations of the heel fat pad with a 21G needle (coupled with the steroid injection) should be performed with caution to avoid iatrogenic injuries to the fat tissue. Indeed, excessive disruption of the heel fat pad during the interventional procedure may lead to minor “fat fractures” known as heel fat pad syndrome [43]. This potential and unintentional complication can be assessed during the ultrasound examination in the follow-up phase.
Several authors have presented papers in which they claim that the simple puncture of the fascia is curative, or they combine it with drugs or other products as part of their therapy. This fact is more studied in tendons. Evidence suggests that simple multipuncture of the tendon improves pain and function outcomes reported by patients with tendinopathy [44]. There is limited data on the benefits of this technique (also known as percutaneous needle tenotomy or tendon fenestration) as a stand-alone treatment for tendinopathy, although there are encouraging results in case series in the literature [45,46,47,48].
This multipuncture is similar to the peppering procedure that has been analyzed in other studies both in the plantar fascia [49, 50] with good results and in other anatomical regions [51]. Pruce et al. [52] first introduced the peppering technique in 1964. In this technique, after needle insertion, the needle is removed, redirected, and reinserted several times without leaving the skin, resulting in the formation of a hematoma that helps speed up the healing of the degenerated structure.
We believe that the multi-needling procedure breaks up the scar tissue that has formed in the plantar fascia and stimulates a healing response. In addition, multi-needling can cause bleeding in the fascia, where platelets release growth factors. Platelets contain a large number of physiologically active substances, which include growth factors that have local action, such as platelet-derived growth factor, transforming growth factor, platelet factor interleukin, platelet-derived angiogenesis factor, vascular endothelial growth factor, epidermal growth factor, insulin-like growth factor, and fibronectin [53]. These substances have anabolic protein properties, including the ability to remodel bones and blood vessels and promote angiogenesis, chondrogenesis, and collagen synthesis [54]. Growth factors bind to transmembrane receptors and initiate a signal within the cell that ultimately results in protein formation. Protein expression regulates multiple pathways involved in cell proliferation, cell chemotaxis, angiogenesis, cell differentiation, and extracellular matrix production. Cytokines, chemokines, and many other proteins were found within platelet alpha granules, which are also involved in stimulating chemotaxis, cell proliferation, and maturation, modulating inflammatory molecules, and attracting leukocytes [53]. In addition to alpha granules, other bioactive components within platelets are dense granules containing serotonin, histamine, dopamine, calcium, and adenosine. In 2015, Andia et al. [55] concluded that PRP injections into pathological and adjacent tissue can help restore homeostasis of injured tissue.
Perhaps the reason why many injectable treatments, diverse in their pharmacological properties, are effective for the treatment of plantar fasciitis is because of the simple fact that the puncture on the plantar fascia tissue is curative.
Study limitations
One of the limitations of the study is that the follow-up is only 120 days. Some of the subjects have been studied for 360 days, with data continuing to be gathered, but more long-term follow-up studies of the investigated subjects are needed.
Because some of the patients had undergone treatment 3 months prior to entering the study, the present study cannot show how effective either technique could be as a first-line treatment.
Patients have not been assessed with magnetic resonance imaging. Indeed, in some recalcitrant cases of “plantar fasciopathy” the pain may be partially related to the fascia-bone junction (enthesis) with abnormal imaging findings of the bone tissue (e.g., bone marrow edema/lesion).
The present results should be understood with caution since all patients attended the same center and were treated by the same therapist. The blinded study was simple, as the patient did not know about the treatment, but the health professional who performed it did. Double-blind studies should be performed in the future.
We do not know if needle size has significant clinical relevance. More studies should be done in the future. Nor do we know if the number of punctures is relevant. In our study, the essential tests were performed to cover the area of greatest irregularity of the plantar fascia under continuous ultrasound visualization.
Another limitation of the study is that in our sample, more subjects in the multipuncture group had had previous treatment. Patients in the multipuncture group also had a higher body mass on average.
Conclusion
In conclusion, corticosteroid injection provides better short-term VAS and FFI pain outcomes, and ultrasound-guided multipuncture provides better VAS and FFI pain outcomes at 120 days. Regarding the thickness of the fascia, the results are similar at 120 days, without the fascia reaching a thickness considered normal in most patients.
Data availability
Sequence data that support the findings of this study have been deposited are available from the corresponding author upon reasonable request.
Abbreviations
- CI:
-
Confidence Interval
- FFI:
-
Foot Function Index
- GCI:
-
Glucocorticosteroid injections
- ICC:
-
Intraclass correlation coefficient
- IQR:
-
Interquartile range
- MDC:
-
Minimal change detectable
- MP:
-
Ultrasound-guided multipuncture
- SD:
-
Standard Deviation
- SEM:
-
Standard error of measurement
- TPF:
-
Thickness of the plantar fascia
- VAS:
-
Visual Analog Scale
References
McNally EG, Shetty S. Plantar fascia: imaging diagnosis and guided treatment. Semin Musculoskelet Radiol. 2010;14(3):334–43.
Tong KB, Furia J. Economic burden of plantar fasciitis treatment in the United States. Am J Orthop (Belle Mead NJ). 2010;39(5):227–31.
Rasenberg N, Bierma-Zeinstra SMA, Bindels PJ, van Middelkoop M, van der Lei J. Incidence, prevalence, and management of plantar heel pain: a retrospective cohort study in Dutch primary care. Br J Gen Pract. 2019;69(688):E801–8.
Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95–101.
Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93(3):234–7.
Lee WCC, Wong WY, Kung E, Leung AKL. Effectiveness of adjustable dorsiflexion night splint in combination with accommodative foot orthosis on plantar fasciitis. J Rehabil Res Dev. 2012;49(10):1557–64.
Petraglia F, Ramazzina I, Costantino C. Plantar fasciitis in athletes: diagnostic and treatment strategies. A systematic review. Muscles Ligaments Tendons J. 2017;7(1):107–18.
Luffy L, Grosel J, Thomas R, So E. Plantar fasciitis: a review of treatments. JAAPA. 2018;31(1):20–4.
Rhim HC, Kwon J, Park J, Borg-Stein J, Tenforde AS. A systematic review of systematic reviews on the epidemiology, evaluation, and treatment of plantar fasciitis. Life. 2021;11(12).
Beeson P. Plantar fasciopathy: revisiting the risk factors. Foot Ankle Surg. 2014;20(3):160–5.
Rompe JD, Furia J, Cacchio A, Schmitz C, Maffulli N. Radial shock wave treatment alone is less efficient than radial shock wave treatment combined with tissue-specific plantar fascia-stretching in patients with chronic plantar heel pain. Int J Surg. 2015;24(Pt B):135–42.
Maffulli G, Padulo J, Iuliano E, Furia J, Rompe J, Maffulli N. Extracorporeal shock wave therapy in the management of insertional plantar fasciitis: the assert database. Muscles Ligaments Tendons J. 2019;8(3):402–8.
Rompe JD, Cacchio A, Weil L, Furia JP, Haist J, Reiners V, et al. Plantar fascia-specific stretching versus radial shock-wave therapy as initial treatment of plantar fasciopathy. J Bone Joint Surg Am. 2010;92(15):2514–22.
Nery C, Raduan F, Mansur N, Baunfeld D, Del Buono A, Maffulli N. Endoscopic approach for plantar fasciopathy: a long-term retrospective study. Int Orthop. 2013;37(6):1151–6.
Oliva F, Piccirilli E, Tarantino U, Maffulli N. Percutaneous release of the plantar fascia. New surgical procedure. Muscles Ligaments Tendons J. 2017;7(2):338–40.
Melo SNS, Ezekwesili A, Yurdi NA, Murrell WD, Maffulli N. Gold-induced cytokine (GOLDIC®) injection therapy in patient with plantar fasciosis: a case report. Indian J Orthop. 2020;54(3):348–51.
Filippini C, Teh J. Ultrasound features of sole of foot pathology: a review. J Ultrason. 2019;19(77):145–51.
Pirri C, Stecco C, Güvener O, Mezian K, Ricci V, Jačisko J, et al. EURO-MUSCULUS/USPRM dynamic ultrasound protocols for ankle/foot. Am J Phys Med Rehabil. 2024;103(3):E29–34.
Sconfienza LM, Orlandi D, Silvestri E. Ultrasound-guided musculoskeletal procedures: the lower limb. 1st ed. Springer; 2015.
Sconfienza LM, Lacelli F, Piccazzo R, Muda A, Serafini G, Silvestri E. One-year outcome of ultrasound-guided percutaneous treatment of plantar fasciitis: a randomized controlled trial. In: Radiological Society of North America 2009 Scientific Assembly and Annual Meeting. 2009.
McMillan AM, Landorf KB, Barrett JT, Menz HB, Bird AR. Diagnostic imaging for chronic plantar heel pain: a systematic review and meta-analysis. J Foot Ankle Res. 2009;2(1):1–11.
Thong ISK, Jensen MP, Miró J, Tan G. The validity of pain intensity measures: what do the NRS, VAS, VRS, and FPS-R measure? Scand J Pain. 18(1):99–107.
Paez-Moguer J, Budiman-Mak E, Cuesta-Vargas AI. Cross-cultural adaptation and validation of the foot function index to Spanish. Foot Ankle Surg. 2014;20(1):34–9.
Budiman-Mak E, Conrad KJ, Roach KE. The foot function index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44(6):561–70.
Pardo y Camps F. Eficacia de la infiltración de Plasma Rico en Plaquetas (PRP) en pacientes diagnosticados del Síndrome de la Fascia Plantar (SFP) desde el punto de vista clínico y funcional. [Master’s thesis, Universidad Complutense de Madrid]. Teseo. 2016.
Fleischer AE, Albright RH, Crews RT, Kelil T, Wrobel JS. Prognostic value of diagnostic sonography in patients with plantar fasciitis. J Ultrasound Med. 2015;34(10):1729–35.
World Medical Association Declaration. Of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Redborg KE, Antonakakis JG, Beach ML, Chinn CD, Sites BD. Ultrasound improves the success rate of a tibial nerve block at the ankle. Reg Anesth Pain Med. 2009;34(3):256–60.
Gurcay E, Kara M, Karaahmet OZ, Ata AM, Onat ŞŞ, Özçakar L. Shall we inject superficial or deep to the plantar fascia? An Ultrasound Study of the Treatment of Chronic Plantar Fasciitis. J Foot Ankle Surg. 2017;56(4):783–7.
Whittaker GA, Munteanu SE, Menz HB, Bonanno DR, Gerrard JM, Landorf KB. Corticosteroid injection for plantar heel pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1).
Schulhofer SD. Short-term benefits of ultrasound-guided corticosteroid injection in plantar fasciitis. Clin J Sport Med. 2013;23(1):83–4.
Li Z, Yu A, Qi B, Zhao Y, Wang W, Li P, et al. Corticosteroid versus placebo injection for plantar fasciitis: a meta-analysis of randomized controlled trials. Exp Ther Med. 2015;9(6):2263–8.
Grice J, Marsland D, Smith G, Calder J. Efficacy of foot and ankle corticosteroid injections. Foot Ankle Int. 2017;38(1):8–13.
Fei X, Lang L, Lingjiao H, Wei C, Zhou X. Platelet-rich plasma has better mid-term clinical results than traditional steroid injection for plantar fasciitis: a systematic review and meta-analysis. Orthopaedics & Traumatology: Surgery & Research. 2021;107(6):103007.
Mcmillan AM, Landorf KB, Gilheany MF, Bird AR, Morrow AD, Menz HB. Ultrasound guided corticosteroid injection for plantar fasciitis: randomised controlled trial. 2012;3260(May):1–12.
Li Z, Xia C, Yu A, Qi B. Ultrasound- versus palpation-guided injection of corticosteroid for plantar fasciitis: a meta-analysis. PLoS ONE. 2014;9(3).
Chen CM, Chen JS, Tsai WC, Hsu HC, Chen KH, Lin CH. Effectiveness of device-assisted ultrasound-guided steroid injection for treating plantar fasciitis. Am J Phys Med Rehabil. 2013;92(7):597–605.
Fox TP, Oliver G, Wek C, Hester T. Plantar fascia calcification a sequelae of corticosteroid injection in the treatment of recalcitrant plantar fasciitis. BMJ Case Rep. 2013;bcr2013200303.
Acevedo JI, Beskin JL. Complications of plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1998;19(2):91–7.
Krey D, Borchers J, McCamey K. Tendon needling for treatment of tendinopathy: a systematic review. Phys Sportsmed. 2015;43(1):80–6.
Sellman JR. Plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1994;15(7):376–81.
Cocco G, Ricci V, Boccatonda A, Abate M, Guagnano MT, Schiavone C. Ultrasound follow-up of spontaneous tears of the plantar fascia treated with conservative therapies: two case reports. Medicine. 2019;98(52).
Ricci V, Abdulsalam AJ, Özçakar L. From plantar fasciitis to heel fat pad syndrome: sonographic kaleidoscope for heel pain. Am J Phys Med Rehabil. 2024.
Housner JA, Jacobson JA, Misko R. Sonographically guided percutaneous needle tenotomy for the treatment of chronic tendinosis. J Ultrasound Med. 28(9):1187–92.
Housner JA, Jacobson JA, Morag Y, Pujalte GGA, Northway RM, Boon TA. Should ultrasound-guided needle fenestration be considered as a treatment option for recalcitrant patellar tendinopathy? A retrospective study of 47 cases. Clin J Sport Med. 2010;20(6):488–90.
Kanaan Y, Jacobson JA, Jamadar D, Housner J, Caoili EM. Sonographically guided patellar tendon fenestration: prognostic value of preprocedure sonographic findings. J Ultrasound Med. 2013;32(5):771–7.
McShane JM, Shah VN, Nazarian LN. Sonographically guided percutaneous needle tenotomy for treatment of common extensor tendinosis in the elbow: is a corticosteroid necessary? J Ultrasound Med. 2008;27(8):1137–44.
Kalaci A, Çakici H, Hapa O, Yanat AN, Dogramaci Y, Sevinç TT. Treatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trial. J Am Podiatr Med Assoc. 2009;99(2):108–13.
Scioli MW. Platelet-rich plasma injection for proximal plantar fasciitis. Techniques Foot Ankle Surg. 2011;10:7–10.
Prakash YR, Dhanda A, Yallapur KL, Inamdar SS, Darshan GT, Ramakrishna M. Peppering versus single injection technique in tennis elbow - a prospective comparative study. Malays Orthop J. 2022;16(1):91–6.
Pruce AM, Miller JA Jr, Berger IR. Anatomic landmarks in joint paracentesis. Clin Symp. 1964;16:19–30.
Sundman EA, Cole BJ, Fortier LA. Growth factor and catabolic cytokine concentrations are influenced by the cellular composition of platelet-rich plasma. Am J Sports Med. 2011;39(10):2135–40.
Katz JN. Platelet-rich plasma for osteoarthritis and achilles tendinitis. JAMA. 2021;326(20):2012–4.
Grambart ST. Sports medicine and platelet-rich plasma: nonsurgical therapy. Clin Podiatr Med Surg. 2015;32(1):99–107.
Andia I, Rubio-Azpeitia E, Maffulli N. Platelet-rich plasma modulates the secretion of inflammatory/angiogenic proteins by inflamed tenocytes. Clin Orthop Relat Res. 2015;473(5):1624–34.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
RMS: Conceptualization, writing and measurement. RMD: Measurement Methodology. AGC: Methodology and design. AFG: Data curation: EGA: original draft preparation. JMCL: writing—reviewing and editing. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by the Research Ethics Committee of Hospital Universitario de Nuestra Señora de Valme under protocol number 2093-N-21. The ethical and human criteria established in the Declaration of Helsinki were followed. Informed, signed consent was obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Montes-Salas, R., Mahillo-Durán, R., Gómez-Carrión, Á. et al. Ultrasound-guided procedures for plantar fasciitis: a randomized clinical study. J Orthop Surg Res 19, 436 (2024). https://doi.org/10.1186/s13018-024-04946-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04946-y