Abstract
Introduction
The best treatment yielding clinical benefits was still equivocal and controversial for the treatment of recalcitrant plantar fasciitis (PF). This study aimed to propose a novel combination strategy of ultrasound-guided percutaneous radiofrequency ablation (RFA) and corticosteroid injection (CI) for recalcitrant PF, and to compare its therapeutic effects with CI alone and continued conservative management.
Methods
We retrospectively reviewed consecutive patients with recalcitrant PF who underwent combined strategy (RFA + CI), CI alone, and continue conservative treatment at our institution between October 2021 and February 2023. The technical pearls were described elaborately. A comparison of demographic data and clinical outcomes, including visual analog scale (VAS), Ankle–Hindfoot Scale (AOFAS-AHS), and plantar fascia thickness, were conducted among the three groups.
Results
Seventy-one eligible patients were enrolled in this study, with 17 in the combined strategy group, 25 in the CI group, and 29 in the continued conservative treatment group. Both the combined strategy group and the CI group showed significant improvements in VAS scores, AOFAS-AHS scores, and significant reductions in plantar fascia thickness during the 12-month follow-up period compared to those preoperatively (P < 0.05). The combined strategy group achieved comparable immediate pain relief to the CI group after the intervention ([25.7 ± 15.7] vs. [20.6 ± 17.6], P = 0.850). However, the combined strategy group demonstrated superior improvement in symptom and function compared to the CI group at the 3-month (VAS: [21.9 ± 13.5] vs. [39.6 ± 20.4]; AOFAS-AHS: [77.9 ± 12.4] vs. [60.5 ± 17.4], P < 0.05) and 12-month follow-up (VAS: [15.7 ± 12.0] vs. [56.8 ± 17.5]; AOFAS-AHS: [84.5 ± 10.7] vs. [53.8 ± 12.4], P < 0.05). Obvious adverse effects or complications were not identified in either group, while two cases (11.8%) in the combined strategy group and five cases (20.0%) in the CI group experienced unsatisfactory symptom remission.
Conclusions
We introduced and detailed a novel combination strategy involving ultrasound-guided percutaneous RFA and CI for treating recalcitrant PF. The strategy is both effective and safe in alleviating pain and enhancing function throughout the entire treatment course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Plantar fasciitis (PF) is the most common cause of plantar heel pain, which has become a worldwide public health issue with an annual incidence of more than 2 million people and an estimated prevalence of 9.6% in the whole elderly population. |
A significant proportion of patients with PF still suffer from residual symptoms after original conservative treatment, and the best treatment yielding clinical benefits was still equivocal and controversial for the treatment of recalcitrant PF. |
We proposed a novel combination strategy of ultrasound-guided percutaneous radiofrequency ablation and corticosteroid injection for treating recalcitrant PF. |
What was learned from the study? |
The combination strategy was both effective and safe in alleviating pain and enhancing function throughout the entire treatment course, and the present results may provide new insights for optimizing the treatment options for recalcitrant PF. |
Introduction
Plantar heel pain (PHP) is a condition characterized by pain under the plantar heel, which has become a worldwide public health issue with an annual incidence of more than 2 million people and an estimated prevalence of 9.6% in the whole elderly population [1,2,3]. Plantar fasciitis (PF) is the most common cause of PHP, accounting for over 1 million patient visits in the United States annually [4, 5]. Since PF is generally a self-limiting disease, a recent best-practice guide recommended noninvasive conservative interventions, such as plantar fascia stretching and low dye taping, as the primary core management [6]. However, a significant proportion of patients still suffer from residual symptoms for at least 6 months, which was generally regarded as recalcitrant PF. A cohort study with long-term follow-up reported up to 44% of patients presented with symptoms for > 15 years from onset [7]. For individuals with recalcitrant PF, while several invasive interventions, including corticosteroid injection (CI), radiofrequency ablation (RFA), plantar fascial release surgery and so on, have been proposed and proven to be effective, current high-level evidence showed that the best treatment yielding clinical benefits was still equivocal and controversial [8].
Although the exact pathogenesis of PF remains poorly understood, microscopic tears in plantar fascia caused by mechanical overload was believed to be the trigger, leading to further degenerative changes including collagen fiber disorientation, mucoid ground substance accumulation, angiofibroblastic hyperplasia, and calcification [9]. Regarding the corresponding pharmacological effects including inhibition of fibroblast proliferation and ground substance protein expression, CI was widely used and achieved certain efficacy in the treatment of PF [10, 11]. However, a systematic review in the Cochrane database revealed that CI may only reduce heel pain for 1 month but not in subsequent longer-term follow-up [12]. RFA is another alternative minimally invasive approach for PF, which mainly focuses on promoting angiogenesis and degenerative tissue repair through varied growth factors [13]. Although RFA gained promising long-term clinical outcomes, symptom improvement seemed to be a gradual process [14,15,16,17]. A prospective study indicated that only 33.3% of patients experienced satisfactory pain relief within 1 month after RFA treatment for recalcitrant PF [14].
Accordingly, we speculated that a combination therapy strategy of RFA and CI may achieve favorable efficacy in the whole course of PF treatment. This notion was also inspired by the combination therapy of CI and peppering technique [18,19,20]. The mechanism of peppering, similar to RFA, leads to the creation of new channels and bleeding in degenerative tissue, promoting revitalization [21]. A prospective randomized study performed four different local injection modalities for the treatment of PF and found that CI combined with peppering provided the best short- and mid-term pain relief [18]. In addition, the current RFA for treating PF was mainly based on a grid-like pattern mark at the area of maximum tenderness, followed by a blind perpendicular puncture approach [14, 16, 17, 22, 23]. This process can result in inaccuracy and additional damage to the weight-bearing area of the plantar fat pad and plantar dermis. Hence, we proposed a novel ultrasound-guided RFA technique, based on an oblique puncture longitudinally, which may provide a precise navigation to lesions and minimize additional damage. The technique was expected to promote rapid recovery post intervention.
Therefore, this study aimed to propose a novel combination strategy of ultrasound-guided percutaneous bipolar RFA and CI for the treatment of recalcitrant PF, and to compare its therapeutic effects with CI alone and continue conservative treatment. We hypothesized that the combination strategy will be both effective and safe in alleviating pain and enhancing function throughout the entire treatment course.
Methods
Patient Population
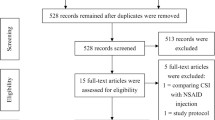
We reviewed 96 consecutive patients with recalcitrant PF treated with combined strategy (RFA + CI) and CI alone at our center between October 2021 and February 2023. PF was diagnosed based on symptoms and physical examination and imaging findings, which included pain at the plantar heel, tenderness at the plantar medial heel, and a sonographic sign of > 4 mm fascia thickness with hypoechoic areas. The inclusion criteria were as follows: (1) diagnosis of PF, (2) failure of noninvasive conservative treatment for at least 6 months. The exclusion criteria were as follows: (1) previous trauma or invasive treatments at the heel, including any injection therapy, (2) heel pain suspected to be related to systemic diseases or nerve entrapment, (3) allergy to local anesthetics or corticosteroid, (4) patients who underwent further invasive treatments for PF after the present intervention during follow-up, (5) patients with incomplete data or lost data within at least 1-year follow-up. Both types of interventions were performed in the inpatient department, and intervention selection was determined by the surgeon together with the patient, after an elaborate explanation of the procedures and sufficient understanding. In addition, the outpatients, who had undergone failed conservative treatment yet still declined invasive interventions and opted for noninvasive conservative treatment for at least 1 year, were identified and served as the control group. The research conducted has been performed in accordance with the Declaration of Helsinki. Approval for the study was obtained from the ethics committees of the Beijing Chaoyang Hospital (2024-KE-364). Written informed consent was obtained from all patients before the procedures.
Intervention Technique
All interventions were performed by a senior orthopedic surgeon with sufficient experience (YZ, with 24 years of experience). Sonographic procedures were performed with a Sonimage HS1 system (Konica Minolta Corp., Tokyo, Japan), and RFA was performed using the HLZ-SC-H-26 unit (LuangZ Corp., Hunan, China). Ultrasound-guided percutaneous RFA was conducted by oblique punctures along the longitudinal axis of the foot, generally consistent with the orientation of the fiber bundles of plantar fascia (Fig. 1B and C). This technique aimed to minimize additional iatrogenic damage to the plantar fascia and the weight-bearing area of the plantar fat pad and plantar dermis.
An illustration of ultrasound-guided percutaneous radiofrequency ablation (RFA). A The plantar fascia was divided into nine approximately equal quadrants (Quadrants 1–9: 1–3, the lateral region; 4–6, the intermediate region; and 7–9, the medial region). Yellow asterisk represents the primary target quadrant with maximum tenderness. The yellow circles represent the secondary quadrants with minor tenderness, consistent with increased plantar fascia thickness. The three black points represent the entry sites; B the schematic view of the ultrasound-guided percutaneous RFA procedure. Each insertion of the radiofrequency cutter was responsible for ablating the corresponding region, and the insertion angle could be adjusted slightly to adapt to the pathologic locations; C the sagittal view of the ultrasound-guided percutaneous RFA procedure. The procedure was guided by a long-axis ultrasound, and the intervention approach avoids the weight-bearing area of the plantar fat pad and plantar dermis
RFA + CI Group: All patients were placed in the prone position. Before the interventions, palpation and ultrasound examination were performed to identify the plantar fascia and mark its area on the skin. Followed by recognizing and marking the distal edge with tenderness in the plantar fascia area, the region was divided into nine approximately equal quadrants (Quadrants 1–9: 1–3, the lateral region; 4–6, the intermediate region; and 7–9, the medial region), and the quadrant with maximum tenderness was marked by an asterisk, served as the primary target. Other quadrants with minor tenderness, consistent with plantar fascia thickness and hypoechogenicity/mixed echogenicity by ultrasound examination, were marked by a circle. The remaining quadrants without tenderness or with normal ultrasonography results were not marked (Fig. 1A). Moreover, three horizontal points were marked with an interval of 0.5 cm and 1 cm distal to the plantar fascia area as entry sites (Figs. 1A and 2E). Standard routine iodine and alcohol disinfection for skin prep and sterilized towel spreading were applied. A sterile cover was placed on the ultrasound probe, and sterile ultrasound gel was used. Entering from the entry sites, an intradermal and subcutaneous 2 ml of 1% lidocaine was administered for local anesthesia. Next, percutaneous ultrasound-guided injection of a mixed solution of 5 ml of 1% lidocaine and 1 ml of diprospan (containing 2 mg of betamethasone disodium phosphate and 5 mg of betamethasone dipropionate) was performed surrounding and superior to the marked area (Figs. 2A and C). In line with the region to which the primary target belonged, a corresponding entry site (lateral, intermediate, or medial) was chosen to be the initial entry site. Whereafter, the radiofrequency cutter was inserted into the primary target quadrant, with the tip penetrating the lesion, to ablate at a power level of 180 V (level 4) and a pulse duration of 500 ms, followed by other quadrants in this region (Fig. 2B). Each insertion of radiofrequency cutter ablated the corresponding region, and the insertion angle could be adjusted slightly to adapt to the pathologic locations (Fig. 1B). In general, 1–5 times of ablation were performed for each region in one insertion, and the procedure was repeated at the remaining regions. The whole procedure was mainly guided by a long-axis ultrasound, assisted with a short-axis view (Figs. 1C, 2C, and D). The puncture site was wrapped with sterilized dressing at the end of the procedure. Postoperatively, the sterilized dressing was left for 2 days. Patients were asked to practice stretching exercises mildly and to weight bear as tolerated on the second postoperative day.
Perioperative photographs of the combination strategy of ultrasound-guided percutaneous radiofrequency ablation (RFA) and corticosteroid injection (CI). A CI procedure; B RFA procedure; C long-axis sonogram showed the needle tip was placed surrounding the plantar fascia followed by injection of mixed solution. The asterisks indicate the edge of the plantar fascia; D long-axis sonogram showed the radiofrequency cutter was inserted into the target plantar fascia. Asterisks indicate the edge of the plantar fascia; E hindfoot at 3 days post-intervention
CI Group: With patients placed in the prone position, the position with maximum tenderness was marked as the target. Disinfection, ultrasound-guided CI, and postoperative management approaches were the same as those in the RFA + CI group.
Clinical and Imaging Evaluation
Follow-up assessments were conducted through regular outpatient visits during a minimum period of 1 year. We evaluated patient-reported outcome measures including the visual analog scale (VAS, ranging from 0 to 100, with higher scores indicating more pain) and American Orthopaedic Foot and Ankle Society Ankle–Hindfoot Scale (AOFAS-AHS, ranging from 0 to 100, with lower scores indicating poorer function) [24]. VAS and AOFAS-AHS in the combined group and CI group were assessed preoperatively and at 3 and 12 months postoperatively. The control group was evaluated at the same time points based on the initial outpatient visit. Distinctively, VAS in intervention groups was also assessed at 7–14 days postoperatively. Further, an objective evaluation of plantar fascia thickness was conducted based on ultrasonography. The plantar fascia thickness was measured longitudinally at the thickest point at the 3- and 12-month follow-up visits routinely. Any complications were identified and recorded during follow-up visits. Clinical baseline data including age, gender, body mass index (BMI), and duration of symptoms (DOS) were also collected from the medical record.
Statistical Analysis
Statistical analyses were performed using SPSS 24.0 (IBM Corp., Armonk, NY, USA). The paired t test was used to determine differences in continuous variables between preoperative and follow-up clinical outcomes. For continuous data, comparisons between two groups were performed with Student’s t test, and comparisons between more than two groups were performed with the one-way ANOVA or the Kruskal–Wallis H test. The chi-square test was used to compare categorical data. Post hoc comparisons were conducted using the Bonferroni post hoc test. Statistical significance was set at a P value of < 0.05.
Results
A total of 71 eligible patients (47 men and 24 women) were enrolled in this study with the mean age and BMI of 54.7 ± 11.2 years and 27.5 ± 4.9 kg/m2, respectively. Among them, 17 underwent combined strategy, 25 underwent CI, and 29 received continued conservative treatment. No significant difference was obtained among the groups in all clinical baseline data, including age, gender, BMI, DOS, preoperative VAS, AOFAS-AHS, and plantar fascia thickness (P > 0.05, Table 1).
During a period of 12 months from interventions or first visit, all enrolled patients underwent regular outpatient visits. For the VAS score, both combined strategy and CI groups showed immediate significant improvements postoperatively compared to their preoperative status. The effect of pain relief was maintained in the combined strategy group, while it weakened gradually in individuals undergoing CI during the follow-up period (3- and 12-months postoperatively). In the control group, significant improvement of the VAS score was achieved at 12 months from the first visit, yet not at 3 months, by continuous noninvasive conservative treatment (Fig. 3). Between-group comparison revealed no significant difference in the VAS score between the combined strategy and CI groups immediately after interventions ([25.7 ± 15.7] vs. [20.6 ± 17.6], P = 0.850). At 3 months postoperatively, pain relief was more outstanding in the combined strategy group than the others ([21.9 ± 13.5] vs. [39.6 ± 20.4]; [21.9 ± 13.5] vs. [70.6 ± 19.2], P < 0.05), and the CI group was better than the control group ([39.6 ± 20.4] vs. [70.6 ± 19.2], P < 0.05). At 12 months postoperatively, the superiority maintained in the combined strategy group ([15.7 ± 12.0] vs. [56.8 ± 17.5]; [15.7 ± 12.0] vs. [59.7 ± 20.0], P < 0.05), whereas no significant difference was observed between the CI and control groups ([56.8 ± 17.5] vs. [59.7 ± 20.0], P > 0.05, Table 2).
For the AOFAS-AHS score, all groups showed significant improvements postoperatively compared to preoperative and first visit status at both follow-up time points (3 and 12 months postoperatively). However, continuous function improvement was shown in the combined strategy and control groups, whereas the function showed a declining trend in the CI group at 12 months compared with 3 months postoperative (Fig. 4). In the between-group comparison, patients achieved better function at 3 months postoperatively in the combined strategy group than the others ([77.9 ± 12.4] vs. [60.5 ± 17.4]; [77.9 ± 12.4] vs. [39.4 ± 10.2], P < 0.05), and the CI group was better than the control group ([60.5 ± 17.4] vs. [39.4 ± 10.2], P < 0.05). At 12 months postoperatively, the superiority was maintained in the combined strategy group ([84.5 ± 10.7] vs. [53.8 ± 12.4]; [84.5 ± 10.7] vs. [50.9 ± 14.6], P < 0.05), whereas no significant difference was observed between the CI and control groups ([53.8 ± 12.4] vs. [50.9 ± 14.6], P > 0.05, Table 2).
Plantar fascia thickness was significantly reduced in both the combined strategy and CI groups at both follow-up time points compared to that preoperatively. No significant change was obtained in the control group during follow-up (Fig. 5). In the between-group comparison, reduction in plantar fascia thickness was significantly greater in the CI group than in the control group at 3 months postoperatively ([4.8 ± 1.0] mm vs. [5.6 ± 1.3] mm, P < 0.05) and in the combined strategy group than the control group at 12 months postoperatively ([4.5 ± 1.0] mm vs. [5.6 ± 1.3] mm, P < 0.05, Table 2).
Obvious adverse effects or complications, such as nerve injury, plantar fascia rupture, or infection, were not identified in either group. In individuals undergoing invasive interventions, a total of seven patients, including two (11.8%) in the combined strategy group and five (20.0%) in the CI group, experienced unsatisfied relief of symptoms.
Discussion
PF is a prevalent worldwide public health issue. When noninvasive conservative treatment fails, which intervention is most beneficial for recalcitrant PF is still equivocal and controversial, especially during the whole rehabilitation period. Therefore, we proposed a novel combination strategy of ultrasound-guided percutaneous bipolar plasma RFA and CI for the treatment of recalcitrant PF. Our findings showed that the combination strategy can significantly improve the symptoms, function, and structural anomaly from the immediate postoperative to 1-year follow-up period. This combination strategy yielded comparable rapid pain relief to CI while sustaining a better efficacy at long-term follow-up. The present results may provide new insights for optimizing the treatment options for recalcitrant PF.
The exact definition of recalcitrant PF remained equivocal, and no widely accepted criteria have been established based on the duration and severity of symptoms. Generally, it is considered a condition that symptoms persist after 6–12 months of conservative treatment. Our results showed that continuous noninvasive conservative treatment showed significant improvements in pain relief and function for patients with recalcitrant PF at a 12-month follow-up. We believe this may be attributed to two major reasons. First, PF is a self-limiting disease, and its process may persist for months to years until recovery [4]. In this study, the median DOS of the control group was only 10 months, indicating a still hopeful and promising improvement subsequently. Besides, the efficacy of conservative treatment may be revealed gradually even up to 2 years. A prospective study evaluated the 2-year outcomes of patients with chronic PF treated by extracorporeal shock wave therapy and conventional conservative treatment and found a continuous reduction of VAS from 24 weeks to 2 years [25]. Second, a great portion of patients in the control group received individualized and standard education by experts during outpatient visits and adjusted to several alternative conservative treatment approaches subsequently in follow-up periods, which may be beneficial to the therapy. However, the present study found the general improvement of symptoms, function, and structural anomaly in continuous noninvasive conservative treatment was more inconspicuous than in intervention groups. A survey was conducted among surgeons in the American Orthopaedic Foot and Ankle Society in 2012 to investigate the preferred management of recalcitrant PF, and more than half (55%) of the members preferred surgery, especially open surgery like gastrocnemius recession, partial plantar fascia release, or nerve decompression, for patients with 10-month symptom duration [26]. With the rapid development of techniques and concepts in the last decade, a more optimal strategy for recalcitrant PF was desired to balance clinical outcomes and surgical trauma.
CI is prevalently used for recalcitrant PF after the failure of noninvasive conservative treatments, based on its corresponding effects including inhibition in fibroblast proliferation and ground substance protein expression [12]. Nonetheless, there is indelible concern about the serious adverse events related to CI including plantar fascia ruptures and injection site infections, despite being under-reported generally [27,28,29]. Besides, pooled data from meta-analysis indicated that CI showed exact short-term effects of pain relief for treating recalcitrant PF [12], even more, superior than autologous blood injection and foot orthoses [30]. However, the efficacy may not be sustained for the medium or long-term [12]. As an echo of such evidence, our results showed a recurrence of symptoms and disability from short-term to 1-year follow-up. Therefore, we believe that CI alone may not be the most ideal regimen for recalcitrant PF.
Percutaneous RFA, actually a specific pattern of microfasciotomy, is another alternative minimally invasive approach for treating recalcitrant PF. This technique was performed by implementing multipoint ablations in the plantar fascia area, stimulating angiogenesis and further degenerative tissue repair through several growth factors [21]. The idea was first proposed by Weil et al. in 2008 [16] and validated and modified in several studies subsequently [14, 15, 17, 22, 23]. However, a typical RFA procedure conducted in most studies included drawing a grid-like pattern mark at the area of maximum tenderness, followed by blind perpendicular multipoint punctures and ablations [14, 16, 17, 22, 23]. Such an approach cannot ensure precise guidance to the lesion area and may result in additional damage to the weight-bearing area of the plantar fat pad and plantar dermis. Although the technique gained satisfactory pain relief and functional improvement in the treatment of PF generally, there is still a lack of high-level evidence to report a persuasive efficacy and safety, especially at the early stage postoperatively. Sorensen et al. conducted a prospective study and found that only 33.3% of patients experienced satisfactory pain relief within 1 month after RFA treatment for recalcitrant PF [14]. Therefore, we proposed a novel RFA technique, based on a percutaneous oblique puncture longitudinally by ultrasound guidance. It can provide precise real-time navigation to lesions and minimize additional damages in the weight-bearing area, which may improve efficacy as well as safety and promote rapid recovery. As this procedure was a novel technique, all patients in this study were managed under inpatient care and performed in the operating room. However, it has the potential to apply in the outpatient department as the low-cost and convenient features of ultrasound and RFA.
Further, we proposed a combined strategy of ultrasound-guided percutaneous bipolar RFA and CI for the treatment of recalcitrant PF. This idea was inspired and supported by three main aspects below. First, although RFA was proven to result in rapid pain reduction by inducing the degeneration of the nerve fibers in rat models [31], this effect may be short-lived and insufficient. The symptom improvement in patients with PF treated with RFA seemed to be gradual [14,15,16,17]. Tasto et al. performed a prospective study to evaluate the effectiveness of RFA microtenotomy for treating chronic tendinosis and reported a reduction of the median VAS score from 8 to 3 (preoperative to postoperative 7–10 days). However, the median VAS score further decreased to 0.7 at 2 years postoperatively, and the ratio of patients who reported minimal to no pain (VAS ≤ 1) was 0 vs. 100% (postoperative 7–10 days vs. 2 years) [32]. They speculated the mechanism of pain relief switched from antinociceptive response to histological improvement including revascularization and reorganization of collagen, which occurs at least 2–3 weeks after RFA and contributed to longer-term and better symptom improvement [32]. Therefore, given the superiority of the short-term effects of CI for recalcitrant PF, complementing their strengths with a combined strategy was reasonable and attractive. Second, the procedure of the proposed combined strategy was similar to the combination therapy of CI and peppering technique, which has been proven to be effective in high-level evidence [18,19,20]. Third, we believe CI will not contribute to additional damage and burden on the routine RFA workflow. Based on the target point of needle placement, the CI modality can be divided into injections within or surrounding the plantar fascia [30]. We chose to mix the corticosteroid with local anesthetics, followed by an injection at the periphery of the plantar fascia. Collectively, the results showed that this combination strategy can significantly improve the symptoms, function, and structural anomaly from immediate postoperative to 1-year period. Furthermore, no obvious adverse effect or complication was observed during follow-up.
Our study had certain limitations. First, the study was subject to the retrospective and single-center design with a small sample size; thus, we could not exclude selection bias. Further validation with prospective, multicenter, and large sample size studies is required. Second, whether the superiority of pain relief at the early stage postoperatively was attributed to the modification of the RFA technique or the additional effect of corticosteroid could not be determined because we did not build a control group consisting of patients treated by modified RFA alone. We speculated that both the modified RFA technique and CI contributed to the immediate improvement postoperatively, yet it still needed to be proven by further well-designed studies. Finally, we did not collect the detail of nonsteroidal anti-inflammatory drugs use of the study individuals during the treatment course, which may cause unexpected bias.
Conclusions
We introduced and detailed a novel combination strategy involving ultrasound-guided percutaneous RFA and CI for the treatment of recalcitrant PF. The combination strategy is both effective and safe in alleviating pain and enhancing function throughout the entire treatment course of PF.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Riel H, Cotchett M, Delahunt E, Rathleff MS, Vicenzino B, Weir A, et al. Is ‘plantar heel pain’ a more appropriate term than ‘plantar fasciitis’? Time to move on. Br J Sports Med. 2017;51(22):1576–7.
Tu P. Heel pain: diagnosis and management. Am Fam Physician. 2018;97(2):86–93.
Thomas MJ, Whittle R, Menz HB, Rathod-Mistry T, Marshall M, Roddy E. Plantar heel pain in middle-aged and older adults: population prevalence, associations with health status and lifestyle factors, and frequency of healthcare use. BMC Musculoskelet Disord. 2019;20(1):337.
Cooper MT. Common painful foot and ankle conditions: a review. JAMA. 2023;330(23):2285–94.
Guimarães JS, Arcanjo FL, Leporace G, Metsavaht LF, Conceição CS, Moreno MVMG, et al. Effects of therapeutic interventions on pain due to plantar fasciitis: a systematic review and meta-analysis. Clin Rehabil. 2023;37(6):727–46.
Morrissey D, Cotchett M, Said J’Bari A, Prior T, Griffiths IB, Rathleff MS, et al. Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values. Br J Sports Med. 2021;55(19):1106–18.
Hansen L, Krogh TP, Ellingsen T, Bolvig L, Fredberg U. Long-term prognosis of plantar fasciitis: a 5- to 15-year follow-up study of 174 patients with ultrasound examination. Orthop J Sports Med. 2018;6(3):2325967118757983.
Babatunde OO, Legha A, Littlewood C, Chesterton LS, Thomas MJ, Menz HB, et al. Comparative effectiveness of treatment options for plantar heel pain: a systematic review with network meta-analysis. Br J Sports Med. 2019;53(3):182–94.
Wearing SC, Smeathers JE, Urry SR, Hennig EM, Hills AP. The pathomechanics of plantar fasciitis. Sports Med. 2006;36(7):585–611.
McMillan AM, Landorf KB, Gilheany MF, Bird AR, Morrow AD, Menz HB. Ultrasound guided corticosteroid injection for plantar fasciitis: randomised controlled trial. BMJ. 2012;344: e3260.
Erden T, Toker B, Cengiz O, Ince B, Asci S, Toprak A. Outcome of corticosteroid injections, extracorporeal shock wave therapy, and radiofrequency thermal lesioning for chronic plantar fasciitis. Foot Ankle Int. 2021;42(1):69–75.
David JA, Sankarapandian V, Christopher PR, Chatterjee A, Macaden AS. Injected corticosteroids for treating plantar heel pain in adults. Cochrane Database Syst Rev. 2017;6(6):CD009348.
Tasto JP, Cummings J, Medlock V, Harwood F, Hardesty R, Amiel D. The tendon treatment center: new horizons in the treatment of tendinosis. Arthroscopy. 2003;19(Suppl 1):213–23.
Sorensen MD, Hyer CF, Philbin TM. Percutaneous bipolar radiofrequency microdebridement for recalcitrant proximal plantar fasciosis. J Foot Ankle Surg. 2011;50(2):165–70.
Chou AC, Ng SY, Su DH, Singh IR, Koo K. Radiofrequency microtenotomy is as effective as plantar fasciotomy in the treatment of recalcitrant plantar fasciitis. Foot Ankle Surg. 2016;22(4):270–3.
Weil L Jr, Glover JP, Weil LS Sr. A new minimally invasive technique for treating plantar fasciosis using bipolar radiofrequency: a prospective analysis. Foot Ankle Spec. 2008;1(1):13–8.
Tay KS, Ng YC, Singh IR, Chong KW. Open technique is more effective than percutaneous technique for TOPAZ radiofrequency coblation for plantar fasciitis. Foot Ankle Surg. 2012;18(4):287–92.
Kalaci A, Cakici H, Hapa O, Yanat AN, Dogramaci Y, Sevinç TT. Treatment of plantar fasciitis using four different local injection modalities: a randomized prospective clinical trial. J Am Podiatr Med Assoc. 2009;99(2):108–13.
Guner S, Onder H, Guner SI, Ceylan MF, Gökalp MA, Keskin S. Effectiveness of local tenoxicam versus corticosteroid injection for plantar fasciitis treatment. Orthopedics. 2013;36(10):e1322–6.
Mahindra P, Yamin M, Selhi HS, Singla S, Soni A. Chronic plantar fasciitis: effect of platelet-rich plasma, corticosteroid, and placebo. Orthopedics. 2016;39(2):e285–9.
Altay T, Günal I, Oztürk H. Local injection treatment for lateral epicondylitis. Clin Orthop Relat Res. 2002;398:127–30.
Yuan Y, Qian Y, Lu H, Kou Y, Xu Y, Xu H. Comparison of the therapeutic outcomes between open plantar fascia release and percutaneous radiofrequency ablation in the treatment of intractable plantar fasciitis. J Orthop Surg Res. 2020;15(1):55.
Hormozi J, Lee S, Hong DK. Minimal invasive percutaneous bipolar radiofrequency for plantar fasciotomy: a retrospective study. J Foot Ankle Surg. 2011;50(3):283–6.
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–53.
Hammer DS, Adam F, Kreutz A, Kohn D, Seil R. Extracorporeal shock wave therapy (ESWT) in patients with chronic proximal plantar fasciitis: a 2-year follow-up. Foot Ankle Int. 2003;24(11):823–8.
DiGiovanni BF, Moore AM, Zlotnicki JP, Pinney SJ. Preferred management of recalcitrant plantar fasciitis among orthopaedic foot and ankle surgeons. Foot Ankle Int. 2012;33(6):507–12.
Canyilmaz E, Canyilmaz F, Aynaci O, Colak F, Serdar L, Uslu GH, et al. Prospective randomized comparison of the effectiveness of radiation therapy and local steroid injection for the treatment of plantar fasciitis. Int J Radiat Oncol Biol Phys. 2015;92(3):659–66.
Tsai WC, Hsu CC, Chen CP, Chen MJ, Yu TY, Chen YJ. Plantar fasciitis treated with local steroid injection: comparison between sonographic and palpation guidance. J Clin Ultrasound. 2006;34(1):12–6.
Sellman JR. Plantar fascia rupture associated with corticosteroid injection. Foot Ankle Int. 1994;15(7):376–81.
Whittaker GA, Munteanu SE, Menz HB, Bonanno DR, Gerrard JM, Landorf KB. Corticosteroid injection for plantar heel pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1):378.
Takahashi N, Tasto JP, Ritter M, Ochiai N, Ohtori S, Moriya H, et al. Pain relief through an antinociceptive effect after radiofrequency application. Am J Sports Med. 2007;35(5):805–10.
Tasto JP, Cummings J, Medlock V, Hardesty R, Amiel D. Microtenotomy using a radiofrequency probe to treat lateral epicondylitis. Arthroscopy. 2005;21(7):851–60.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Yinfeng Zheng and Tianyi Wang contributed equally to this work. Conceptualization: Yinfeng Zheng, Tianyi Wang, and Lei Zang; methodology: Yinfeng Zheng, Tianyi Wang, and Peng Du; formal analysis and investigation: Tianyi Wang and Peng Du; writing—original draft preparation: Yinfeng Zheng and Tianyi Wang; writing—review and editing: Xiaochuan Kong, Gang Hong, Le Zhang, Jian Li; resources: Lei Zang; supervision: Lei Zang.
Corresponding author
Ethics declarations
Conflict of Interest
Yinfeng Zheng, Tianyi Wang, Lei Zang, Peng Du, Xiaochuan Kong, Gang Hong, Le Zhang, and Jian Li declare that they have no conflicts of interest.
Ethical Approval
The research conducted has been performed in accordance with the Declaration of Helsinki. Approval for the study was obtained from the ethics committees of the Beijing Chaoyang Hospital (2024-KE-364). Written informed consent was obtained from all patients before the procedures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zheng, Y., Wang, T., Zang, L. et al. A Novel Combination Strategy of Ultrasound-Guided Percutaneous Radiofrequency Ablation and Corticosteroid Injection for Treating Recalcitrant Plantar Fasciitis: A Retrospective Comparison Study. Pain Ther (2024). https://doi.org/10.1007/s40122-024-00629-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40122-024-00629-y