Abstract
Background
Evaluating muscle spasticity in children with cerebral palsy (CP) is essential for determining the most effective treatment strategies. This scoping review assesses the current methods used to evaluate muscle spasticity, highlighting both traditional and innovative technologies, and their respective advantages and limitations.
Methods
A search (to April 2024) used keywords such as muscle spasticity, cerebral palsy, and assessment methods. Selection criteria included articles involving CP children, assessing spasticity objectively/subjectively, comparing methods, or evaluating method effectiveness.
Results
From an initial pool of 1971 articles, 30 met our inclusion criteria. These studies collectively appraised a variety of techniques ranging from well-established clinical scales like the modified Ashworth Scale and Tardieu Scale, to cutting-edge technologies such as real-time sonoelastography and inertial sensors. Notably, innovative methods such as the dynamic evaluation of range of motion scale and the stiffness tool were highlighted for their potential to provide more nuanced and precise assessments of spasticity. The review unveiled a critical insight: while traditional methods are convenient and widely used, they often fall short in reliability and objectivity.
Conclusion
The review discussed the strengths and limitations of each method and concluded that more reliable methods are needed to measure the level of muscle spasticity more accurately.
Similar content being viewed by others
Introduction
Cerebral palsy (CP) is a group of permanent, nonprogressive neurological disorders that affect movement, posture, and muscle coordination and limit the activities of daily living, leading to dysmorphisms [1,2,3]. The incidence rate of CP is 2–2.5% per 1000, making it the most common disorder leading to physical disability in children [1,2,3,4,5]. It is caused by damage or abnormalities in the developing brain, usually occurring before or during birth, but can also occur during early childhood. The condition is characterized by varying degrees of motor impairment, which can range from mild to severe. Specifically, damage to the motor cortex, which is responsible for planning, executing, and controlling voluntary movements, can lead to muscle spasticity in CP. Spasticity is a condition with a constant state of muscle contraction, resulting in stiffness and difficulty in movement [6]. The motor cortex is located in the brain's frontal lobe, and damage to this area can result in abnormalities in muscle tone, posture, and other motor-related symptoms. However, it is worth noting that CP can result from damage to different parts of the brain, and the specific location of the brain injury can affect the severity and type of motor symptoms that develop, including muscle spasticity [1, 7].
Complications of CP include communication difficulties, gastrointestinal abnormalities, and bone conditions such as osteopenia [1, 8]. Individuals with CP often experience difficulties with muscle tone, control, balance, and coordination, leading to challenges in walking, speaking, eating, and performing everyday activities. The specific symptoms and severity of CP can vary from person to person, as the location and extent of the brain damage determine the areas of the body affected. Muscle spasticity in children with CP can also cause a wide variety of discomforts ranging from pain to hip displacement, which requires medical intervention to improve the dynamics and quality of life of patients [5, 7, 8].
Among different treatment options, such as physical therapy, medication, the Bobath neurodevelopmental method, and surgical procedures used to manage spasticity, the appropriate remedy is selected according to each individual’s specific symptoms [1, 8]. Botulinum toxin type A and baclofen are the medications commonly administered for managing spasticity in children with CP [1, 3]. Botulinum toxin (Botox), a formulation of botulinum toxin type A from the bacterium Clostridium botulinum, can prevent acetylcholine release from nerve terminals and relax muscles [3, 4]. Although Botulinum neurotoxin type A (BoNT A) is not an FDA-approved treatment option for children with CP, it is still considered one of the best options due to its long-lasting effect, noninvasiveness, cost-effectiveness, and accessibility [3]. For over 2 decades, BoNT A has been used to treat spasticity in individuals with CP younger than 19 years [9, 10]. Different clinicians use varying dosages, measured in units of activity and injected volumes, to treat muscle spasticity based on their evaluation of spasticity [10].
Developing a spasticity management plan and finding the optimal procedure for each individual is highly dependent on the level of spasticity. A central challenge, in assessing muscle spasticity in children with CP, is the lack of a universally accepted definition of spasticity, an issue highlighted in an interdisciplinary workshop held at the National Institutes of Health in April 2001 [11]. Current methods for scaling the level of spasticity, such as the modified Ashworth Scale and the modified Tardieu Scale, add some insight but do not provide accurate information physicians need to define the dosage and timing of therapeutic interventions. In recent years, several quantitative scales such as pendulum test, Australian Spasticity Assessment Scale and real-time sonoelastography have been proposed for objective assessment and scaling of spasticity but have yet to gain widespread use in clinical applications.
The works of Scholtes et al. [12], and Aloraini et al. [13]. collectively underline the complexity and diversity in spasticity measurement methods. While these studies emphasize the critical role of precise and comprehensive assessment tools, they also reveal significant gaps in the development and validation of these tools, particularly concerning their reliability and validity across varied clinical settings. Our scoping review was conceived in response to these gaps, aiming to provide an updated and thorough overview of the latest methodologies and technologies in the field. We specifically targeted the integration of novel, objective measures and the standardization of assessment protocols. Our study not only enriches the existing body of knowledge by cataloging and critiquing current methodologies but also pioneers in identifying and recommending future directions for research.
This scoping review aims to map the available subjective scales and objective measures for assessing spasticity in children with CP.
Method
This scoping review was conducted according to the framework outlined by Arksey and O’Malley [14] and extended by Levac et al. [15]. In addition, this review is reported according to the PRISMA extension for a scoping review [16]. We did not develop a protocol for this scoping review.
Research question
The primary research question for this article review was: “What are the most effective methods for assessing muscle spasticity in children with CP?”.
To further clarify and support this primary question, we identified two sub-questions that guide the scope of our review. These questions were:
-
1.
How do various subjective and objective methods compare in accuracy and reliability for assessing muscle spasticity in children with CP?
-
2.
What are the strengths and limitations of current spasticity assessment tools in clinical and research settings?
Inclusion criteria
Participants
Studies involving children and adolescents (0–18 years of age) with CP. This includes all types and severities of CP.
Concept
The focus of studies must be on assessing muscle spasticity using either objective or subjective measures. Studies should either compare different assessment methods or evaluate the effectiveness, reliability, or validity of a particular assessment method.
Context
Included studies conducted in any clinical or research setting, including hospitals, rehabilitation centers, outpatient clinics, and research laboratories. The review is interested in studies conducted in diverse geographical locations and healthcare settings to understand the global applicability of the assessment methods.
Type of sources
The review includes original research articles, systematic reviews, meta-analyses, cohorts, and clinical trials. Case studies, editorials, commentaries, and letters are excluded. The review considers studies published in English, given the language capabilities of the research team.
Search strategy
We searched PubMed, Web of Science Core Collection and Google Scholar. The search strategy did not place limitations. The search included a combination of keywords related to muscle spasticity, CP, and assessment methods the date of the last search was April 2024. See Supplement 1 for the search strategy used in databases. To ensure that we located all relevant sources of evidence, we consulted Dr. Shadgan and Dr. Mulpuri who are experts on our team for suggestions of papers that may have been missed by our search, and we performed hand-searching of reference lists of relevant articles to identify studies related to our objective.
Study selection
To determine eligibility, we used a two-step process. First, we assessed the titles and abstracts followed by the full text against the inclusion criteria. At each stage, each reference was screened by two members independently and in duplicate. To remove duplicates, references were imported to Covidence, duplicate entries were automatically detected and highlighted. To ensure accuracy, a manual review has been done, following which duplicates were excluded. Any disagreements were resolved through consultation with a third senior investigator.
Data extraction
After identifying the final articles, two independent investigators carefully examined each article's findings, methods, and the specific assessment scales they utilized. The key findings of the articles, participants, and the method of spasticity assessment were extracted, and summaries of information extracted from studies were provided. Any disagreements were resolved through consultation with a third senior investigator.
Evaluation of the levels of evidence?
The Oxford Centre for Evidence-Based Medicine (OCEBM) criteria were also used to critically evaluate the levels of evidence of the included research [17]. The OCEBM guidelines are divided into five levels, from Level 1 (highest) to Level 5, each corresponding to a particular study design [18]. For example, case studies or expert opinions are located at the bottom of the hierarchy (Level 5), whereas randomized controlled trials (RCTs) are found at the top (Level 1). Table 1 illustrates various levels of OCEBM.
Two independent reviewers from our research team were involved in this evaluation process. Each study was individually assessed by these reviewers, who then compared their evaluations to ensure consistency and objectivity. The involvement of two reviewers aimed to minimize bias and enhance the reliability of our evidence grading.
In cases where the two reviewers had differing opinions on a study's level of evidence, a structured discussion was held to reach a consensus. If a consensus could not be achieved through discussion, a third senior investigator was consulted to provide an additional perspective and facilitate a resolution.
Results
Study selection
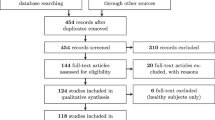
Initially, 1971 primary titles were identified, which were narrowed down to 94 papers related to CP and assessments of muscle spasticity. Additional articles were found by reviewing references. Ultimately, 30 articles were deemed relevant to evaluating muscle spasticity in children with CP and were used as the basis for the review. Figure 1 describes the methodology used for the selection and inclusion of articles.
Study characteristics and quality assessment
The 30 included studies and their characteristics are summarized in Table 2. All the articles included in the qualitative analysis were published from 1999 to April 2024. All studies included children with CP, both male and female, with ages ranging from 1 to 19 years old. The mean sample size was 29.86, ranging from 10 to 168. Various CP subtypes were explored, prominently focusing on spastic hemiplegia and spastic diplegia, and the studies involved a range of clinical and instrumented techniques to assess qualitative and quantitative aspects.
The assessment of the included papers based on the OCEBM scoring system revealed the following distribution of scores: five papers obtained a score of 4, one paper obtained a score of 3b, twenty papers obtained a score of 2b, one paper obtained a score of 1b, two papers obtained a score of 2a, and one paper obtained a score of 1.
Methods for muscle spasticity assessment
Identified methods to scale muscle spasticity included clinical qualitative and instrumented quantitative techniques. Quantitative approaches are further classified into neurophysiological response and biomechanical response methods. The methods identified from the selected articles are explained in the following section.
Hofmann’s reflex
The Hoffman's reflex, commonly known as the H-reflex, is a neurophysiological technique widely used to assess muscle spasticity. This method involves stimulating a mixed peripheral nerve—usually the nerve that serves the muscles being tested—with a mild electrical current. The H-reflex is similar to the natural reflex that occurs when a muscle tendon is tapped (like in a knee-jerk reflex), but it is elicited in a controlled manner using electrical stimulation [46].
When the nerve is stimulated, it causes a response in the muscle, which is then recorded. The key aspect of the H-reflex is the measurement of the reaction time (latency) and the size (amplitude) of the muscle response. Typically, in spastic muscles, as seen in conditions like CP, the reflex response is exaggerated—meaning the muscles respond more quickly and with greater force than normal [46].
Additionally, the ratio of the maximum reflex response to the maximum direct muscle response (known as Hmax/Mmax ratio) is calculated. This ratio provides valuable information about the excitability of the spinal motor neurons controlling the muscle. However, it's important to note that there is an overlap in the values of this scale between healthy and spastic muscles, which can sometimes limit its diagnostic efficiency [46]. Furthermore, obtaining the maximum direct muscle response, which is essential for the Hmax/Mmax calculation, requires a strong stimulus that can be uncomfortable, making it less frequently used in children [46].
Modified Ashworth Scale (MAS)
The MAS is a clinical assessment tool used to evaluate spasticity in patients with neurological conditions such as CP, stroke, or spinal cord injury. The MAS measures the resistance of a muscle group to passive stretching on a six-point ordinal scale, ranging from 0 (no increase in muscle tone) to 4 (rigidity). A score of 1 indicates a mild increase in muscle tone with a catch and release, while a score of 2 represents a more marked increase in muscle tone through the entire range of motion, but the limb can still be easily moved. A score of 3 indicates a considerable increase in muscle tone; passive movement is complex, and there is a “catch” at a certain point in the range of motion. A score of 4 represents rigid flexion or extension [47].
The MAS is a common method of muscle spasticity assessment since it does not require any equipment and can be performed rapidly, efficiently, and in a daycare clinic [48]. The test is performed manually to assess the muscle resistance to passive stretching and was primarily defined as a scale of spasticity [48]. However, its result depends on the speed at which the test is done [48]. This drawback limits the reliability of this test and increases the chances of error in assessments. Therefore, the results of spasticity evaluations obtained with this scale should be interpreted cautiously. The other limitation of the MAS is that it only provides a subjective assessment of spasticity based on the clinician’s interpretation of the resistance to passive stretching [21]. Additionally, the MAS does not provide information on the underlying neural mechanisms of spasticity, such as changes in muscle fibre properties or altered reflex pathways [21].
Tardieu Scale (TS)
This test evaluates muscle resistance to both slow and fast passive motions [48]. TS assessment is simple and relatively easy to carry out. Moreover, the results of this assessment, i.e., the spasticity angle X and the spasticity grade Y, can be correlated with gait analysis if needed [22].
The Tardieu scale has excellent intra- and interrater reliability when measured at the elbow and ankle joints of children with CP. Moreover, no difference was noted between visual and goniometric assessments. The Tardieu Scale is commonly used during the evaluation of children with CP; nevertheless, it is associated with several drawbacks, such as lack of standardization, precise control over stimulation, and poor reliability and validity for qualitative and subjective assessments of all muscle groups [48].
Electromyography (EMG)
Electromyography (EMG) is a technique used to measure the electrical activity of muscles. It involves the placement of surface or fine wire electrodes on the skin overlying the muscle of interest, which then records the electrical activity generated by the muscle during movement [23]. EMG determines muscle activation patterns, timing and coordination, and muscle recruitment during functional tasks. In children with CP, EMG can be used to assess muscle spasticity by measuring the level of muscle activity during passive or active movement [49].
One limitation of EMG is that it only measures muscle activity on the surface, so it may not accurately reflect deep muscle activity [50]. Additionally, EMG cannot distinguish between spasticity and other factors contributing to increased muscle activity, such as compensation strategies or pain [51].
Pendulum test
The pendulum test, also known as the Wartenberg test, is a biomechanical method that measures muscle tone by using gravity to stimulate the muscle stretch reflex during passive swinging of the lower leg. Studies that used this method to assess spasticity in children with CP report that it may provide an objective assessment distinguishing various degrees of spasticity in this population [19, 24]. However, it needs to be clarified whether the outcomes of the pendulum test correlate with the results of other spasticity assessment methods in children with CP [19]. The pendulum test is simple, quick, and noninvasive, with reproducible results. Furthermore, it is nonintimidating to children or people with cognitive deterioration. However, its main drawback is that the test outcomes are thoroughly influenced by the level of muscle relaxation and sitting position [24].
Acoustic radiation force impulse (ARFI) elastography
ARFI elastography is a recently developed technique that overlays tissue elasticity data on standard images obtained with commercial ultrasound scanners. ARFI elastography systems either show a map displaying spatial differences in tissue spasticity or report tissue elasticity quantitatively as shear wave velocity (SWV), normally measured in meters per second (m/s) [52].
ARFI elastography-based quantification of tissue spasticity is a noninvasive, inexpensive, safe, and quick imaging tool with reliable and reproducible results that can improve the precision of ultrasound tests in determining muscle spasticity [52]. However, ARFI elastography is an operator skill-dependent technique that requires precision mechanical equipment, which is not easily applicable at the bedside [53].
Real-time sonoelastography (RTS)
Real-time sonoelastography (RTS) is another novel ultrasound-based technique that assesses the elasticity of the tissue in real time. RTS is based on the principle that tissue strain (displacement) is lower in hard tissue and higher in soft tissue [25]. However, RTS involves tissue compression, leading to imprecise outcomes and limiting interoperator reproducibility. Therefore, it can be considered a semiquantitative assessment [26].
Dynamic evaluation of range of movement (DAROM)
The DAROM evaluation method considers muscle stiffness, movement velocity, and adjacent joint positions to assess spasticity. The DAROM, a simplified form of the modified Tardieu Scale, demonstrated good intra- and interrater reliability when passive muscle stretching was repeated at two different speeds. The range of movement in this test is defined as slow and quick passive stretching to assess a dynamic component of muscle spasticity. Unlike standard clinical examinations, the DAROM represents a “range of movement deficit” (DROM), a value from the minimal muscle stretch position. In this test, two joint angles are measured: DROM I, described as the passive range of movement (PROM) deficiency following a slow velocity stretch, and DROM II, defined as the angle of catch after a quick velocity stretch. The difference between DROM II and DROM I demonstrates the examined muscle group’s level of spasticity and is called the angle of spasticity (AOS) [27]. The DAROM examination is a simultaneous accelerometric assessment of the range of motion ROM deficiency and the corresponding passive motion angular velocity, which enables the observer to assess the static contractures and dynamic spastic components. However, its drawback is that this measure is not an objective test [27].
Australian spasticity assessment scale (ASAS)
ASAS is a recently developed method to assess muscle spasticity [34]. The ASAS determines the presence of spasticity by identifying a velocity-dependent increased response to rapid passive movement. An ordinal scale is used to quantify this method. No instrument is required to perform this tool, and it is easy to apply in the clinical setting [34]. Although Sarah Love and her colleagues demonstrated promising reliability between raters, further research needs to be conducted to clarify the responsiveness of the ASAS to detect change after specific spasticity interventions [34].
Ely test
The Ely test (Duncan-Ely) is a clinical technique for evaluating rectus femoris spasticity [35]. It is a velocity-dependent test measured as positive or negative by quickly flexing the knee while lying prone in a relaxed state [35]. The Root-Ely test, a modified version of the Duncan-Ely test, is a 5-point numerical rating system that determines where the catch happens in the quick arc of knee flexion [35].
There are some limitations associated with this study including the lack of standardized velocity in measuring spasticity which potentially affects the consistency and accuracy of measurements [35]. Furthermore, differences in how each clinician performs the measurements may lead to inconsistencies and biases in the results [35]. Lastly, the possibility of a learned effect by the children, whereby repeated measurements influence their responses, is a challenge in reliability studies and may confound the results, and we cannot control this effect [35].
Hypertonia assessment tool
The hypertonia assessment tool has seven components: items one, two, and six assess dystonia, items three and four measure spasticity, and items five and seven examine rigidity [36]. The items are graded as either positive or negative [36]. One or more positive scores on one hypertonia item indicate the presence of this subtype [36]. Each limb is examined and given an individual diagnosis of hypertonia [36].
Since this method is a subjective test, to improve the quality of the results, the test procedure (e.g., hand positioning) needs to be standardized and assessors should be trained properly [36].
Numeric rating scale
The 0–10 numeric rating scale (NRS) is utilized to assess spasticity [37]. NRS is a self-reported outcome measure in which 0 represents no spasticity and 10 denotes the greatest spasticity [37]. This rating instrument is commonly used in clinical settings to promptly evaluate pain [37].
There are various perspectives on spasticity among children, caretakers, and clinicians, which can lead to challenges in accurately assessing and measuring spasticity using NRS [37]. Children identify spasticity with end range of movement, caretakers with generalized hypertonia, and physicians with a velocity-dependent component of spasticity [37].
Inertial sensors
Inertial sensors, which are lightweight devices containing accelerometers, gyroscopes, and sometimes magnetic sensors, are employed to track the movement of both proximal and distal body segments during rapid passive muscle stretch [40]. These sensors can offer insights into the angle of catch, a significant aspect of spasticity evaluation [41]. Similar to dynamometry, mathematical models have been proposed to create an objective measure of spasticity, utilizing data gathered from these sensors [13].
Stiffness tool (L-STIFF)
Driven Gait Orthosis Lokomat is a device created for robotic-assisted gait rehabilitation that allows patients with neurological movement disorders to simply measure the mechanical stiffness of a joint while performing robotic-assisted gait training with partial body weight support [38]. The L-STIFF tool detects changes in resistive torque in hip and knee joints during predetermined passive motions in both flexion and extension, moving the joint at a constant velocity with a regulated range of motion [38, 42].
The L-STIFF assessment technique is a viable option for automated stiffness testing in children with CP, but it is not sensitive enough to detect minor variations in muscle tone [38].
Tonic stretch reflex threshold
The Tonic Stretch Reflex Threshold (TSRT) is determined by stretching the spastic muscle at various fast paces while measuring the joint angle with an electrogoniometer and the myoelectric response using EMG [39]. The TSRT index is calculated using linear regression (the stretch reflex threshold angle and velocity) [39, 43]. A TSTR angle is estimated by extending the regression line until it intersects with the velocity axis at 0 degrees per second [39, 43].
Discussion
This article aims to review and compare the available subjective scales and objective measures for assessing muscle spasticity in children with CP. Muscle spasticity is a common motor disorder that affects individuals with CP [46]. It occurs due to damage to the part of the brain that controls muscle movement and can affect any part of the body, such as the legs, arms, and trunk [46]. Muscle spasticity significantly impacts a person’s ability to perform daily activities and quality of life; hence, measuring and monitoring the level of muscle spasticity is important [19].
Various methods are used to classify muscle spasticity and aid in its management.44 Current subjective and objective methods to measure the spasticity of muscles include Hofmann’s reflex or H-reflex [46], the Modified Ashworth Scale [21, 47, 48], the Tardieu scale [22, 48], electromyography (EMG) [23, 49,50,51] pendulum tests [19, 24], acoustic radiation force impulse (ARFI) elastography [52, 53], real-time sonoelastographs (RTS) [25, 26], the dynamic evaluation of range of motion (DAROM) scale [27], the Australian spasticity assessment Scale (ASAS) [34]. Ely Test [35], hypertonia assessment tool [36], numeric rating Scale [37], inertial sensors [40, 41], stiffness tool (L-STIFF) [38, 42], and tonic stretch reflex threshold [39, 43].
These methods can be categorized into two main groups: neurophysiological response methods and biomechanical response methods. Neurophysiological response methods include techniques such as the H-reflex and EMG. The H-reflex measures the electrical response of a muscle to low-threshold electrical stimulation, while EMG measures the electrical activity of muscles during movement [23, 46]. Both methods offer insights into muscle activation patterns and motor neuron excitability but may have limitations in distinguishing spasticity from other factors affecting muscle activity.
Biomechanical response methods include clinical assessment tools such as the MAS and the TS, as well as novel techniques such as ARFI and RTS. The MAS and TS are widely used clinical tools to assess spasticity based on resistance to passive stretching, while ARFI and RTS offer noninvasive and real-time imaging approaches to quantify tissue elasticity.
In addition to these methods include the Ely Test and Hypertonia Assessment Tool, which fall under more subjective assessments due to their reliance on clinician interpretation and patient responses. The Numeric Rating Scale, while simple and commonly used, also falls into this subjective category. Conversely, Inertial Sensors and the Stiffness Tool (L-STIFF) provide more objective biomechanical response measurements by analyzing the physical properties of muscle movements and stiffness. Similarly, the Tonic Stretch Reflex Threshold (TSRT) offers an objective approach by quantifying reflex thresholds and muscle dynamics.
Reviewing the selected articles suggests that each assessment method has advantages and limitations. Some methods, such as the MAS and TS, are commonly used in clinical practice due to their simplicity and accessibility [48]. However, they may be subject to subjective interpretation and may not fully capture the underlying neural mechanisms of spasticity [21, 48].
On the other hand, newer techniques such as ARFI elastography and RTS offer more objective and quantitative measures of tissue elasticity but may require specialized equipment and operator skills. The strengths and limitations of each method are listed in Table 3.
The review also highlights the need for more research to establish the reliability, validity, and responsiveness of newer methods such as the ASAS. Additionally, further studies could explore the correlations between the outcomes of different assessment methods to determine their complementary roles in evaluating muscle spasticity.
Incorporating multiple assessment techniques is essential for a comprehensive understanding of muscle spasticity [54]. While methods like the modified Ashworth Scale (MAS) are easily applied, they can be enhanced with objective tools like electromyography (EMG) or acoustic radiation force impulse (ARFI) elastography. This fusion enhances assessment accuracy, shedding light on neural and biomechanical factors influencing spasticity [54].
Developing standardized protocols and establishing normative data for these techniques is vital. Such standardization facilitates clinical translation of the methods and ensures consistent results across studies [55]. Additionally, longitudinal studies that track changes in muscle spasticity over time and in response to various interventions are essential to establish the responsiveness and reliability of these methods in a clinical context.
Furthermore, considering factors such as age, CP severity, and comorbidities when selecting and interpreting assessment methods is essential. Customizing evaluations to each child’s specific needs can lead to personalized treatment plans and enhanced outcomes.
The limitations of the present article review are related to the limited longitudinal data and heterogeneity of the included studies. The included studies in this review used different populations, assessment protocols, and outcome measures, leading to heterogeneity in the data. This diversity in methodologies may limit direct comparisons and the generalizability of the findings. The review mainly relies on cross-sectional studies, which may not provide comprehensive insights into the effectiveness of different assessment methods over time.
Conclusions
Muscle spasticity assessment in children with CP is essential for an effective treatment/spasticity management plan and follow-up. Current spasticity assessment techniques are primarily subjective and lack sufficient reliability to quantify the level of muscle spasticity in children with CP. New methods that can objectively, accurately and reliably scale muscle spasticity can provide insight into each child’s condition with CP and aid physicians in optimizing personalized treatment plans. Moreover, they can assist in monitoring the efficiency of treatments.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Novak I, Morgan C, Adde L, Blackman J, Boyd RN, Brunstrom-Hernandez J, Cioni G, Damiano D, Darrah J, Eliasson AC, De Vries LS. Early, accurate diagnosis and early intervention in cerebral palsy: advances in diagnosis and treatment. JAMA Pediatr. 2017;171(9):897–907.
Beckung E, Carlsson G, Carlsdotter S, Uvebrant P. The natural history of gross motor development in children with cerebral palsy aged 1 to 15 years. Dev Med Child Neurol. 2007;49(10):751–6.
Krigger KW. Cerebral palsy: an overview. Am Fam Physician. 2006;73(1):91–100.
Pavone V, Testa G, Restivo DA, Cannavò L, Condorelli G, Portinaro NM, Sessa G. Botulinum toxin treatment for limb spasticity in childhood cerebral palsy. Front Pharmacol. 2016;7:29.
Graham HK, Boyd R, Carlin JB, Dobson F, Lowe K, Nattrass G, Thomason P, Wolfe R, Reddihough D. Does botulinum toxin A combined with bracing prevent hip displacement in children with cerebral palsy and “hips at risk”?: A randomized, controlled trial. JBJS. 2008;90(1):23–33.
McDougall J, Chow E, Harris RL, Mills PB. Near-infrared spectroscopy as a quantitative spasticity assessment tool: a systematic review. J Neurol Sci. 2020;412: 116729.
Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, Dan B, Jacobsson B. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109(suppl 109):8–14.
Bjornson K, Hays R, Graubert C, Price R, Won F, McLaughlin JF, Cohen M. Botulinum toxin for spasticity in children with cerebral palsy: a comprehensive evaluation. Pediatrics. 2007;120(1):49–58.
Love SC, Novak I, Kentish M, Desloovere K, Heinen F, Molenaers G, O’flaherty S, Graham HK. Botulinum toxin assessment, intervention and after-care for lower limb spasticity in children with cerebral palsy: international consensus statement. Eur J Neurol. 2010;17:9–37.
Schroeder AS, Berweck S, Lee SH, Heinen F. Botulinum toxin treatment of children with cerebral palsy—a short review of different injection techniques. Neurotox Res. 2006;9:189–96.
Sanger TD, Delgado MR, Gaebler-Spira D, Hallett M, Mink JW, Task Force on Childhood Motor Disorders. Classification and definition of disorders causing hypertonia in childhood. Pediatrics. 2003;111(1):e89–97.
Scholtes VA, Becher JG, Beelen A, Lankhorst GJ. Clinical assessment of spasticity in children with cerebral palsy: a critical review of available instruments. Dev Med Child Neurol. 2006;48(1):64–73.
Aloraini SM, Alassaf AM, Alrezgan MM, Aldaihan MM. Spasticity measurement tools and their psychometric properties among children and adolescents with cerebral palsy: a systematic review. Pediatr Phys Ther. 2022;34(4):449–63.
Arksey H, O’malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:1–9.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Durieux N, Vandenput S, Pasleau F. OCEBM levels of evidence system. Rev Med Liege. 2013;68(12):644–9.
Oxford Centre for Evidenced-based Medicine-Level of Evidence. Centre for evidenced based medicine (CEBM). Available at: http://www.cebm.net/. Updated 2009. Accessed 3 May 2013.
Szopa A, Domagalska-Szopa M, Kidoń Z, Syczewska M. Quadriceps femoris spasticity in children with cerebral palsy: measurement with the pendulum test and relationship with gait abnormalities. J Neuroeng Rehabil. 2014;11:1.
Ceyhan Bilgici M, Bekci T, Ulus Y, Bilgici A, Tomak L, Selcuk MB. Quantitative assessment of muscle stiffness with acoustic radiation force impulse elastography after botulinum toxin A injection in children with cerebral palsy. J Med Ultrason. 2018;45:137–41.
Pandyan AD, Johnson GR, Price CI, Curless RH, Barnes MP, Rodgers H. A review of the properties and limitations of the Ashworth and modified Ashworth Scales as measures of spasticity. Clin Rehabil. 1999;13(5):373–83.
Gracies JM, Burke K, Clegg NJ, Browne R, Rushing C, Fehlings D, Matthews D, Tilton A, Delgado MR. Reliability of the Tardieu Scale for assessing spasticity in children with cerebral palsy. Arch Phys Med Rehabil. 2010;91(3):421–8.
Tedroff K, Knutson LM, Soderberg GL. Synergistic muscle activation during maximum voluntary contractions in children with and without spastic cerebral palsy. Dev Med Child Neurol. 2006;48(10):789–96.
Rahimi F, Eyvazpour R, Salahshour N, Azghani MR. Objective assessment of spasticity by pendulum test: a systematic review on methods of implementation and outcome measures. BioMed Eng OnLine. 2020;19:1–8.
Park GY, Kwon DR. Application of real-time sonoelastography in musculoskeletal diseases related to physical medicine and rehabilitation. Am J Phys Med Rehabil. 2011;90(11):875–86.
Kwon DR, Kwon DG. Botulinum toxin a injection combined with radial extracorporeal shock wave therapy in children with spastic cerebral palsy: shear wave sonoelastographic findings in the medial gastrocnemius muscle, preliminary study. Children. 2021;8(11):1059.
Domagalska M, Szopa A, Syczewska M, Pietraszek S, Kidoń Z, Onik G. The relationship between clinical measurements and gait analysis data in children with cerebral palsy. Gait Posture. 2013;38(4):1038–43.
Alhusaini AA, Dean CM, Crosbie J, Shepherd RB, Lewis J. Evaluation of spasticity in children with cerebral palsy using Ashworth and Tardieu Scales compared with laboratory measures. J Child Neurol. 2010;25(10):1242–7.
Fosang AL, Galea MP, McCoy AT, Reddihough DS, Story I. Measures of muscle and joint performance in the lower limb of children with cerebral palsy. Dev Med Child Neurol. 2003;45(10):664–70.
Mutlu A, Livanelioglu A, Gunel MK. Reliability of Ashworth and Modified Ashworth scales in children with spastic cerebral palsy. BMC Musculoskelet Disord. 2008;9:1–8.
Fowler EG, Nwigwe AI, Ho TW. Sensitivity of the pendulum test for assessing spasticity in persons with cerebral palsy. Dev Med Child Neurol. 2000;42(3):182–9.
Park GY, Kwon DR. Sonoelastographic evaluation of medial gastrocnemius muscles intrinsic stiffness after rehabilitation therapy with botulinum toxin a injection in spastic cerebral palsy. Arch Phys Med Rehabil. 2012;93(11):2085–9.
Jang DH, Sung IY, Kang YJ. Usefulness of the tendon reflex for assessing spasticity after botulinum toxin-a injection in children with cerebral palsy. J Child Neurol. 2013;28(1):21–6.
Love S, Gibson N, Smith N, Bear N, Blair E, Australian Cerebral Palsy Register Group. Interobserver reliability of the Australian spasticity assessment scale (ASAS). Dev Med Child Neurol. 2016;58:18–24.
Drefus LC, Clarke S, Resnik K, Koltsov J, Dodwell ER, Scher DM. The root-ely modified test of rectus femoris spasticity has reliability in individuals with cerebral palsy. HSS J. 2018;14(2):143–7.
Marsico P, Frontzek-Weps V, Balzer J, van Hedel HJ. Hypertonia assessment tool: reliability and validity in children with neuromotor disorders. J Child Neurol. 2017;32(1):132–8.
Tsai S, Blackburn J, Gaebler-Spira D. Validation of the 0–10 numeric rating scale measure of spasticity in children with cerebral palsy. J Pediatr Neurol. 2016;14:012–6.
Schmartz AC, Meyer-Heim AD, Müller R, Bolliger M. Measurement of muscle stiffness using robotic assisted gait orthosis in children with cerebral palsy: a proof of concept. Disabil Rehabil Assist Technol. 2011;6(1):29–37.
Jobin A, Levin MF. Regulation of stretch reflex threshold in elbow flexors in children with cerebral palsy: a new measure of spasticity. Dev Med Child Neurol. 2000;42(8):531–40.
Van den Noort JC, Scholtes VA, Harlaar J. Evaluation of clinical spasticity assessment in cerebral palsy using inertial sensors. Gait Posture. 2009;30(2):138–43.
Lynn BO, Erwin A, Guy M, Herman B, Davide M, Ellen J, Anne C, Kaat D. Comprehensive quantification of the spastic catch in children with cerebral palsy. Res Dev Disabil. 2013;34(1):386–96.
Cherni Y, Ballaz L, Girardin-Vignola G, Begon M. Intra-and inter-tester reliability of spasticity assessment in standing position in children and adolescents with cerebral palsy using a paediatric exoskeleton. Disabil Rehabil. 2021;43(7):1001–7.
Germanotta M, Taborri J, Rossi S, Frascarelli F, Palermo E, Cappa P, Castelli E, Petrarca M. Spasticity measurement based on tonic stretch reflex threshold in children with cerebral palsy using the PediAnklebot. Front Hum Neurosci. 2017;11:277.
Wang X, Teh SH, Du XG, Wang XH. Acupuncture and tuina treatment for gross motor function in children with spastic cerebral palsy: a monocentric clinical study. Neuropsychiatr Dis Treat. 2023;19:1875–86.
Stergiou ΑN, Varvarousis DN, Tzoufi M, Markozannes G, Plyta P, Vasileiadis G, Beris A, Ploumis A. Equine-assisted intervention in children with spastic quadriplegia: the effect on function and balance A prospective study. Arch Hell Med Arheia Ell Iatr. 2024;41(2):1–10.
Bar-On L, Molenaers G, Aertbeliën E, Van Campenhout A, Feys H, Nuttin B, Desloovere K. Spasticity and its contribution to hypertonia in cerebral palsy. BioMed Res Int. 2015;2015: 317047.
Boyd RN, Graham HK. Objective measurement of clinical findings in the use of botulinum toxin type A for the management of children with cerebral palsy. Eur J Neurol. 1999;6:s23-35.
Sarathy K, Doshi C, Aroojis A. Clinical examination of children with cerebral palsy. Indian J Orthop. 2019;53:35–44.
Wang H, Wang L, Xiang Y, Zhao N, Li X, Chen S, Lin C, Li G. Assessment of elbow spasticity with surface electromyography and mechanomyography based on support vector machine. In: 2017 39th annual international conference of the IEEE engineering in medicine and biology society (EMBC) 2017 Jul 11. IEEE, pp 3860–3863
Kellis E, Katis A. Reliability of EMG power-spectrum and amplitude of the semitendinosus and biceps femoris muscles during ramp isometric contractions. J Electromyogr Kinesiol. 2008;18(3):351–8.
Basmajian JV. Muscles alive. Their functions revealed by electromyography. Acad Med. 1962;37(8):802.
Bruno C, Minniti S, Bucci A, Pozzi Mucelli R. ARFI: from basic principles to clinical applications in diffuse chronic disease—a review. Insights Imaging. 2016;7:735–46.
Mikami Y, Ushio K, Matsumoto A, Kouda K, Kimura H, Adachi N. Quantitative assessment of muscle stiffness using tensiomyography before and after Injection of botulinum toxin type an in patients after stroke. Phys Med. 2019;4:1–5.
Luo Z, Lo WL, Bian R, Wong S, Li L. Advanced quantitative estimation methods for spasticity: a literature review. J Int Med Res. 2020;48(3):0300060519888425.
He J, Luo A, Yu J, Qian C, Liu D, Hou M, Ma Y. Quantitative assessment of spasticity: a narrative review of novel approaches and technologies. Front Neurol. 2023;14:1121323.
Funding
No funding was used for the writing of the article.
Author information
Authors and Affiliations
Contributions
I confirm that all authors of this manuscript, including Mehdi Nourizadeh, Babak Shadgan, Samin Abbasidezfouli, Maria Juricic, and Kishore Mulpuri, made Substantial contributions to: design the work, the acquisition, analysis, or interpretation of data, draft the work or revise it critically for important intellectual content, final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All of the authors give their consent to publish this article.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nourizadeh, M., Shadgan, B., Abbasidezfouli, S. et al. Methods of muscle spasticity assessment in children with cerebral palsy: a scoping review. J Orthop Surg Res 19, 401 (2024). https://doi.org/10.1186/s13018-024-04894-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04894-7