Abstract
Background
This study aimed to compare surgical outcomes, clinical outcomes, and complications between minimally invasive transforaminal lumbar interbody fusion (MIS TLIF) and midline lumbar interbody fusion (MIDLIF) in patients with spondylolisthesis.
Methods
This study retrospectively compared the patients who underwent MIS TLIF (n = 37) or MIDLIF (n = 50) for spinal spondylolisthesis. Data of surgical outcomes (postoperative one-year fusion rate and time to bony fusion), clinical outcomes (visual analog scale [VAS] for pain and Oswestry Disability Index [ODI] for spine function), and complications were collected and analyzed.
Results
There was more 2-level fusion in MIDLIF (46% vs. 24.3%, p = 0.038). The MIS TLIF and MIDLIF groups had similar one-year fusion rate and time to fusion. The MIDLIF group had significantly lower VAS at postoperative 3-months (2.2 vs. 3.1, p = 0.002) and postoperative 1-year (1.1 vs. 2.1, p = < 0.001). ODI was not significantly different. The operation time was shorter in MIDLIF (166.1 min vs. 196.2 min, p = 0.014). The facet joint violation is higher in MIS TLIF (21.6% vs. 2%, p = 0.009). The other complications were not significantly different including rate of implant removal, revision, and adjacent segment disease.
Conclusion
In this study, postoperative VAS, operation time, and the rate of facet joint violation were significantly higher in the MIS TLIF group. Comparable outcomes were observed between MIDLIF and MIS TLIF in terms of fusion rate, time to fusion, and postoperative ODI score.
Similar content being viewed by others
Introduction
Transforaminal lumbar interbody fusion (TLIF) has been proven to be an effective solution for spinal instability [1, 2]. To minimize surgical trauma and enhance patient’s recovery, minimally invasive techniques are introduced in the past decades such as minimally invasive TLIF (MIS TLIF) [3]. MIS TLIF provides less estimated blood loss, less tissue trauma, and shorter hospital stays compared to traditional open TLIF [4, 5].
Pedicle screws used in MIS TLIF are placed in traditional trajectory. The traditional trajectory screw is inserted parallel to endplate, aims from lateral to medial, and placed convergently. Traditional trajectory screw provides well posterior fixation of spinal fusion. However, some disadvantages of traditional pedicle screw insertion including medial pedicle wall breaching [6], facet joint violation [7], damage of the medial branches of dorsal rami of spinal nerves (MBN) [8, 9], and higher screw loosening rate in osteoporotic patients [10, 11]. The stability of traditional trajectory screws is provided by dorsal cortex and the surrounding cancellous bone. Osteoporosis would attenuate the screw strength and lead to higher screw loosening rate [12,13,14].
In order to enhance the screw strength, screw insertion through cortical bone trajectory (CBT) was first introduced by Santoni et al. in 2009 [15]. CBT increased 30% pull-out strength and 70% insertion torque compared with traditional trajectory [15, 16]. With the new trajectory aims from medial to lateral and from caudal to cephalad, CBT can purchase more cortexes and provides more strength. The different trajectory also brings the advantages of less facet joint violation, less medial pedicle wall breaching, and less surgical trauma [17]. A meta-analysis revealed that CBT and traditional trajectory received similar fusion rate, whereas CBT was associated with less blood loss and shorter hospital stays than traditional trajectory [17]. Additionally, CBT screw insertion could be performed with laminectomy and decompression simultaneously through a posterior midline approach (MIDLIF). Due to the advantages of CBT, MIDLIF is gaining popularity recently. However, few studies directly compare MIDLIF to MIS TLIF. This study aimed to compare surgical outcomes, clinical outcomes, and complications between MIS TLIF and MIDLIF.
Materials and methods
Patients
The retrospective cohort study was approved by the Institutional Review Board of Show Chwan Memorial Hospital (No. 1100706). Eligible patients were those who underwent MIS TLIF between November 2014 and March 2018 (MIS TLIF group) or underwent MIDLIF (MIDLIF group) between April 2018 and April 2021 in the Show Chwan Memorial Hospital, had spinal instability due to degenerative or isthmic spondylolisthesis Meyerding grade I-II [18], fusion levels less than three, and received postoperative follow-up for at least one year. Patients were excluded if they had active infection, malignancy, prior history of spinal surgery, or postoperative follow-up for less than one year. All operations were performed by the one experienced spinal surgeon.
Surgical techniques
MIS TLIF
Operation was performed using Wiltse approach as previously described [19]. A 4 cm incision was made on the cage insertion side. The dissection was made between multifidus and longissimus and down to the lamina and facet. Unilateral approach bilateral decompression was performed to relieve pressure on the spinal nerves in cases of spinal stenosis. The intervertebral body space was carefully prepared including disc material removal, decortication of bony endplate, autograft placement, and cage selection. Superior facet joint was preserved to prevent future adjacent segment disease. Staple wounds were made on the other side to facilitate percutaneous screwing. Pedicle screw was placed with guide pins and dilators under fluoroscopic guidance. Soft tissue around the entry point was not cauterized due to the limited operative field of the staple wound. After the procedure of decompression, cage placement and screw insertion were done, the rod were assembly and secured. Checked the final structure under fluoroscope before wound closure. The wound was closed layer by layer. The screws we used in MIS TLIF were MANTIS (Stryker, Kalamazoo, MI, USA) and Trend I systems (Biomech, Taipei, Taiwan). All polyetheretherketone cage (G cage, Biomech, Taipei, Taiwan) was used in MIS TLIF.
MIDLIF
MIDLIF was performed using CBT screw insertion as previously described [20, 21]. The midline incision was made and dissection was made between spinal process and paraspinal muscles. Exposed the lamina and facet. The bilateral entry point of the screw was exposed with electrocautery, which is different from MIS TLIF. The CBT screw was inserted divergently under fluoroscopy. The decompression was done on the symptomatic side and until the pulsation of the spinal cord restored. After the decompression and screw insertion were done, the rod and crosslink were assembled and secured. The final structure under fluoroscope was checked before wound closure. Wound was closed layer by layer. The CBT screws placed in MIDLIF were Wiltrom (Wiltrom, Hsinchu, Taiwan) and Trend II (Biomech, Taipei, Taiwan) systems. Interbody fusion was done using all polyetheretherketone cage (G cage, Biomech, Taipei, Taiwan).
Data collections
Data were collected through retrospective chart review. Demographics, body mass index (BMI), bone marrow density (BMD), smoking status, comorbidity (including diabetes mellitus, hypertension, and coronary artery disease), diagnosis, perioperative data (i.e., operation time and blood loss), postoperative data (i.e., change in hemoglobin and hospital stay), surgical outcomes, clinical outcomes, and complications were collected.
Surgical outcomes included fusion status at postoperative one-year and time to bony fusion. Fusion status was assessed by computed tomography (CT) scan. The CT was arranged once the lumbar spine flexion extension radiograph showed the angular motion change less than 5 degree at fusion level, trabecular bony bridge formation without radiolucent line, and no implant failure [22, 23].
Clinical outcomes included pain degree and spine function, which were assessed using visual analog scale (VAS) and Oswestry Disability Index (ODI), respectively. The VAS score ranges from 0 to 10 (0 = least pain, 10 = worst pain). The ODI contains 10 patient-completed questions to evaluate spine function. Each question is scored on the scale of 0 to 5 (0 = best outcome, 5 = worst outcome). The overall ODI score ranges from 0 to 100% and a lower score indicates better function [24]. Evaluation of pain and spine function were performed at preoperative, postoperative 3-month, and postoperative 1-year.
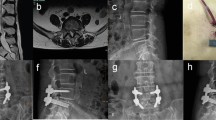
Complications included implant removal due to screw head irritation, revision surgery, screw loosening, and implants related complication. Implants related complications consisted of medial breaching, lateral breaching, and facet joint violation (Fig. 1). Screw loosening was defined as presence of radiolucent area of more than 1 mm surrounding the screw and double halo sign on lumbar spine radiograph [25]. The CT scan was arranged when symptomatic complications occurred. The screw malposition was investigated by authors using the fusion CT as mentioned above. Safe zone was defined as breaching less than 2 mm [26]. Screw breaching more than 2 mm were recorded. All the images were interpreted independently by two orthopedists. Disagreement of the interpretation was resolved by further discussion. Lumbar spine radiography was performed preoperatively, immediate postoperatively, and at postoperative 1-, 2-, 3-, 6, and 12-months.
Statistical analysis
Continuous variables were presented as mean (standard deviation) and categorical variables as count (percentage). To compare the MIS TLIF and MIDLIF groups, Mann-Whitney U test and Fisher’s Exact test were used for continuous variables and categorical variables, respectively. One-year fusion rate was compared using log-rank test. A two-tailed p < 0.05 indicated statistical significance. All analyses were performed using IBM SPSS Statistics for Windows, version 24 (IBM Corporation, Armonk, NY, USA).
Results
A total of 87 patients were included in this study, 37 in the MIS TLIF group and 50 in the MIDLIF group. There were no significant differences between the two groups regarding age, gender, BMI, smoking, chronic diseases, pathology, and preoperative spondylolisthesis grade. There were lower BMD (0.885 vs. 0.697, p = 0.002) and more 2-level fusion (24.3 vs. 46%, p = 0.038) in MIDLIF (Table 1).
As presented in Table 2, the operation time (196.2 vs. 166.1, p = 0.014) was shorted in MIDLIF. No significant differences in blood loss, change in hemoglobin, and hospital stay were observed. These two groups had similar time to fusion and one-year fusion rate (Table 2).
Both groups had improved VAS and ODI postoperatively. The MIDLIF group had significantly lower VAS at postoperative 3-months (2.2 vs. 3.1, p = 0.002) and postoperative 1-year (1.1 vs. 2.1, p < 0.001). ODI was not significantly different between the two groups during postoperative follow-up (Fig. 2).
Complications
No significant difference was observed between the two groups regarding implant removal, revision, and adjacent segment disease. The facet joint violation (21.6% vs. 2%, p = 0.009) was higher in MIS TLIF (Table 3). Medial breaching was also higher in MIS TLIF, but the difference was not statistically significant.
Five patients experienced reoperation, four in the MIS TLIF group and one in the MIDLIF group. The duration until reoperation ranged from 2 days to 34.4 months. The indications of reoperation included symptomatic medial screw breaching, facet joint violation with nonunion, and screw head irritation. Two patients received revision at postoperative 2-day due to symptomatic screw breaching, one in each group. Three patients presented with chronic low back pain postoperatively in MIS TLIF. Two were diagnosed screw head irritation and one facet joint violation with nonunion. The symptoms were resolved after the operations (Table 4).
Discussion
Although both MIS TLIF and MIDLIF are common surgical approaches for spinal disorders, evidence of directly comparing MIS TLIF and MIDLIF is limited. In this study, there were no significant differences in one-year fusion rate, time to fusion, and improvement of spinal function between MIS TLIF and MIDLIF, except that MIDLIF provided better effect of pain relief than MIS TLIF at postoperative 3-month and one-year. Other complications were comparable. The MIS TLIF group had numerical higher incidence of implant removal, and revision than the MIDLIF group.
The higher postoperative pain score and incidence of implant removal in the MIS TLIF group may be related with MBN-induced back pain after spinal instrumentation [27, 28]. MBN lies between facet and transverse process [29, 30] and is fixed by the strong fibers of mammillo-accessory ligament, which extends between the mammillary process and accessory process (Fig. 3A) [9]. A cadaveric study by Regev et al. compared MBN injury after mini-open versus percutaneous pedicle screw insertion [8]. MBN transection was observed in 84% of the pedicles when using mini-open technique and in 20% of the pedicles when the screw was placed via percutaneous approach (P < 0.01). When the MBN is transected or ablated during pedicle screw insertion, there would be less MBN-related postoperative pain. Conversely, when performing percutaneous screw insertion via traditional trajectory, the screw head is just beside the intact MBN. Thus, it might result in nerve impingement or irritation, contributing to postoperative back pain (Fig. 3B). In MIDLIF, soft tissues around the entry point are ablated, which may damage the MBN. In MIS TLIF, the MBN is relatively preserved due to percutaneous insertion technique. The difference in entry points and soft tissue preservation around entry points may lead to greater postoperative pain with MIS TLIF.
Anatomy of medial branch of dorsal ramus nerve (A) and anatomical relationship among entry point of cortical bone trajectory, entry point of traditional trajectory, and medial branch of dorsal ramus nerve (B). Gray line: L4 nerve root; yellow line: medial branch of dorsal ramus of spinal nerve; M: mamillary process; A: accessory process; C: entry point of cortical bone trajectory; T: entry point of traditional trajectory
Our results revealed that both MIDLIF and MIS TLIF groups had one-year fusion rate of over 90%, which were comparable with previous reports [31,32,33]. Several studies also observed higher fusion rate in MIDLIF than in MIS TLIF [31,32,33]. The greater proportion of two-level fusion in the MIDLIF versus MIS TLIF group (40.7% vs. 24.3%) lead to lower one-year fusion rate and longer time to fusion but none of these were statistically significant. Most of previous studies focused on the patient undergoing one-level spinal fusion [32,33,34,35] or included only a few patient with two-level fusion [31]. By contrast, this study included more patients with two-level fusion, which indicated more complicated nature of the patients.
This study revealed similar blood loss between two groups. The operation time was statistically faster in the MIDLIF group even with a larger proportion of two-level fusion. Previous reports [32,33,34] also showed shorter operation time in MIDLIF. The narrow surgical field of view and high technical demands of MIS TLIF increase operation time, especially when resecting contralateral lesions. On the other hand, MIDLIF is performed via a posterior midline incision and bilateral lesions could be approached more easily.
Our study observed a trend towards a lower complication rate for MIDLIF compared to MIS TLIF, although the difference was not statistically significant. The study by Wu et al. revealed similar results that overall complication rate was lower in MIDLIF than in MIS TILF (18.75% vs. 29.4%, P = 0.423). Kasukawa et al. reported higher rate of correct screw positioning in MIDLIF than in MIS TILF (90% vs. 84.1%). The higher malposition rate in MIS TILF might be related with the instinct characteristic of traditional trajectory, in which screws are placed convergently and entry points are just nearby the facet joints.
A meta-analysis published by Hu et al. indicated that no difference was found in VAS score when comparing MIDLIF and other posterior fusion technique [17]. A study published by Wu et al. better VAS leg pain at post operative 6 months but no difference found at 1 year follow up [33]. In our study, we revealed the same tendency and the better VAS score at post operative 3 months and 1 year were noted.
This study had limitations. The first one came from the retrospective study design. Potential selection bias and reporting bias could not be avoided. All patients were operated in the same hospital. The single-institutional results may not be applicable in other institutions, which limited the external validity of this study. Additionally, all patients were postoperatively followed for at least one year. However, some long-term complications, such as adjacent segment disease, might not be thoroughly observed. Furthermore, there were more two-level fusion done in MIDLIF, which indicated the severity of the patient was not evenly distributed and may produce bias.
In conclusion, this study observed comparable one-year fusion rate, time to fusion, function improvement, and complications between the patients receiving MIS TLIF and MIDLIF. MIDLIF provided better pain relief at postoperative 3-months and one-year. Further large-scale studies are warranted for identifying the patients who would benefit most from MIS TLIF and MIDLIF respectively.
Data availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- BMD:
-
Bone marrow density
- BMI:
-
Body mass index
- CBT:
-
Cortical bone trajectory
- CT:
-
Computed tomography
- MIDLIF:
-
Midline lumbar interbody fusion
- MIS TLIF:
-
Minimally invasive transforaminal lumbar interbody fusion
- ODI:
-
Oswestry Disability Index
- TLIF:
-
Transforaminal lumbar interbody fusion
- VAS:
-
Visual analog scale
References
Lenz M, Mohamud K, Bredow J, Oikonomidis S, Eysel P, Scheyerer MJ. Comparison of different approaches in lumbosacral spinal Fusion surgery: a systematic review and Meta-analysis. Asian Spine J. 2022;16(1):141–9.
Tang L, Wu Y, Jing D, Xu Y, Wang C, Pan J. A bayesian network meta-analysis of 5 different fusion surgical procedures for the treatment of lumbar spondylolisthesis. Med (Baltim). 2020;99(14):e19639.
Foley KT, Lefkowitz MA. Advances in minimally invasive spine surgery. Clin Neurosurg. 2002;49:499–517.
Miller LE, Bhattacharyya S, Pracyk J. Minimally invasive Versus Open Transforaminal lumbar Interbody Fusion for single-level degenerative disease: a systematic review and Meta-analysis of Randomized controlled trials. World Neurosurg. 2020;133:358–65. e4.
Qin R, Liu B, Zhou P, Yao Y, Hao J, Yang K, et al. Minimally invasive Versus Traditional Open Transforaminal lumbar Interbody Fusion for the treatment of single-level spondylolisthesis grades 1 and 2: a systematic review and Meta-analysis. World Neurosurg. 2019;122:180–9.
El- Desouky A, Silva PS, Ferreira A, Wibawa GA, Vaz R, Pereira P. How accurate is fluoroscopy-guided percutaneous pedicle screw placement in minimally invasive TLIF? Clin Neurol Neurosurg. 2021;205:106623.
Zhang RJ, Zhou LP, Zhang L, Zhang HQ, Ge P, Jia CY et al. The Rates and Risk factors of Intra-pedicular Accuracy and Proximal Facet Joint violation for single-level degenerative lumbar diseases: cortical bone trajectory versus traditional trajectory pedicle screw. Spine (Phila Pa 1976). 2021.
Regev GJ, Lee YP, Taylor WR, Garfin SR, Kim CW. Nerve injury to the posterior rami medial branch during the insertion of pedicle screws: comparison of mini-open versus percutaneous pedicle screw insertion techniques. Spine (Phila Pa 1976). 2009;34(11):1239–42.
Boelderl A, Daniaux H, Kathrein A, Maurer H. Danger of damaging the medial branches of the posterior rami of spinal nerves during a dorsomedian approach to the spine. Clin Anat. 2002;15(2):77–81.
Lee CK, Kim D, An SB, Shin DA, Ha Y, Kim KN et al. An optimal cortical bone trajectory technique to prevent early surgical complications. Br J Neurosurg. 2020:1–7.
Song T, Hsu WK, Ye T. Lumbar pedicle cortical bone trajectory screw. Chin Med J (Engl). 2014;127(21):3808–13.
Formby PM, Kang DG, Helgeson MD, Wagner SC. Clinical and Radiographic Outcomes of Transforaminal Lumbar Interbody Fusion in patients with osteoporosis. Global Spine J. 2016;6(7):660–4.
Weiser L, Huber G, Sellenschloh K, Viezens L, Puschel K, Morlock MM, et al. Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur Spine J. 2017;26(11):2891–7.
Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS 3rd, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994;19(21):2415–20.
Santoni BG, Hynes RA, McGilvray KC, Rodriguez-Canessa G, Lyons AS, Henson MA, et al. Cortical bone trajectory for lumbar pedicle screws. Spine J. 2009;9(5):366–73.
Matsukawa K, Yato Y, Kato T, Imabayashi H, Asazuma T, Nemoto K. In vivo analysis of insertional torque during pedicle screwing using cortical bone trajectory technique. Spine (Phila Pa 1976). 2014;39(4):E240–5.
Hu JN, Yang XF, Li CM, Li XX, Ding YZ. Comparison of cortical bone trajectory versus pedicle screw techniques in lumbar fusion surgery: a meta-analysis. Med (Baltim). 2019;98(33):e16751.
Meyerding HW, Spondyloptosis. Surg Gynaecol Obstet. 1932;54:371–7.
Ge DH, Stekas ND, Varlotta CG, Fischer CR, Petrizzo A, Protopsaltis TS, et al. Comparative analysis of two transforaminal lumbar Interbody Fusion techniques: open TLIF Versus Wiltse MIS TLIF. Spine (Phila Pa 1976). 2019;44(9):E555–60.
Berjano P, Damilano M, Ismael M, Formica C, Garbossa D. Minimally invasive PLIF with divergent, cortical trajectory pedicle screws. Eur Spine J. 2015;24(Suppl 5):654–5.
Matsukawa K, Taguchi E, Yato Y, Imabayashi H, Hosogane N, Asazuma T, et al. Evaluation of the fixation strength of pedicle screws using cortical bone trajectory: what is the Ideal trajectory for optimal fixation? Spine (Phila Pa 1976). 2015;40(15):E873–8.
Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976). 1995;20(12):1410–8.
Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J. 2010;19(10):1780–4.
Fairbank JCT, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25(22):2940–53.
Wu X, Shi J, Wu J, Cheng Y, Peng K, Chen J, et al. Pedicle screw loosening: the value of radiological imagings and the identification of risk factors assessed by extraction torque during screw removal surgery. J Orthop Surg Res. 2019;14(1):6.
Aoude AA, Fortin M, Figueiredo R, Jarzem P, Ouellet J, Weber MH. Methods to determine pedicle screw placement accuracy in spine surgery: a systematic review. Eur Spine J. 2015;24(5):990–1004.
Ellwood S, Shupper P, Kaufman A. A retrospective review of spinal Radiofrequency Neurotomy procedures in patients with metallic posterior spinal instrumentation - is it safe? Pain Physician. 2018;21(5):E477–82.
Klessinger S, editor. Safety and Efficacy of Lumbar Spine Radiofrequency Neurotomy in the Presence of Posterior Pedicle Screws2016.
Lau P, Mercer S, Govind J, Bogduk N. The surgical anatomy of lumbar medial branch neurotomy (facet denervation). Pain Med. 2004;5(3):289–98.
Zhou L. The anatomy of dorsal Ramus nerves and its implications in Lower Back Pain. Neurosci Med. 2012;03:192–201.
Kasukawa Y, Miyakoshi N, Hongo M, Ishikawa Y, Kudo D, Shimada Y. Short-term results of transforaminal lumbar Interbody Fusion using pedicle screw with cortical bone trajectory compared with conventional trajectory. Asian Spine J. 2015;9(3):440–8.
Gonchar I, Kotani Y, Matsui Y, Miyazaki T, Iwasaki N, editors. Clinical Comparison of Cortical Bone Trajectory and Percutaneous Pedicle Screw in Single-Level Minimally Invasive Lumbar Fusion2017.
Wu FL, Dang L, Zhou H, Yu M, Wei F, Jiang L, et al. Two-year outcomes of midline lumbar Fusion Versus minimally invasive transforaminal lumbar Interbody Fusion in the treatment of L4-L5 degenerative disease. Biomed Environ Sci. 2020;33(11):839–48.
Elmekaty M, Kotani Y, Mehy EE, Robinson Y, Tantawy AE, Sekiguchi I, et al. Clinical and radiological comparison between three different minimally invasive Surgical Fusion techniques for single-level lumbar isthmic and degenerative spondylolisthesis: minimally invasive Surgical Posterolateral Fusion versus minimally invasive Surgical Transforaminal lumbar Interbody Fusion versus midline lumbar Fusion. Asian Spine J. 2018;12(5):870–9.
Silva PS, Jardim A, Pereira J, Sousa R, Vaz R, Pereira P. Minimally invasive fusion surgery for patients with degenerative spondylolisthesis and severe lumbar spinal stenosis: a comparative study between MIDLIF and TLIF. Eur Spine J. 2023;32(9):3210–7.
Acknowledgements
None.
Funding
This study did not receive any funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the manuscript writing and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
The retrospective cohort study was approved by the Institutional Review Board of Show Chwan Memorial Hospital (No. 1100706).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, YY., Chung, YH., Huang, CH. et al. Comparison of minimally invasive transforaminal lumbar interbody fusion and midline lumbar interbody fusion in patients with spondylolisthesis. J Orthop Surg Res 19, 286 (2024). https://doi.org/10.1186/s13018-024-04764-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04764-2