Abstract
Purpose
The aim of this study is to find a new method for femoral side preservation positioning in anterior cruciate ligament (ACL) reconstruction and test the accuracy and precision of this method.
Method
Fifty patients with isolated ACL rupture (42 males and 8 females) who underwent single-bundle ACL reconstruction in our hospital between July 2022 and July 2023 were included. The lowest point of the cartilage margin of the lateral wall of the intercontinental fossa and the tibial plateau plumb line at 120° of knee flexion were used as the anatomical landmarks for positioning of the femoral tunnel for ACL reconstruction surgery. Femoral side remnant preservation was performed in all cases. Three-dimensional CT was performed 3 days postoperatively to collect the data, which were analyzed using Mimics 21.0 software. We measured the posterior cortical distance of the femoral condyle at 90° of knee flexion and the vertical distance from the center of the bone tunnel to the cortical extension line behind the femur. All femoral tunnel positions were marked on a 4 × 4 grid and visualized using the quadrant method.
Results
Using the new positioning method in 50 knees, the average distance of x was 25.26 ± 2.76% of t and the average distance of y was 23.69 ± 6.19% of h. This is close to the results of previous studies, where x was 24.2 ± 4.0% of t and the average distance of y was 21.6 ± 5.2% of h. Most femoral tunnel positions were located in the same area. The D values were distributed as follows: 60% in the range of 0 to 2 mm, 24% in the range of 2 to 4 mm, and 16% more than 4 mm. The E values were distributed as follows: 80% in the range of 0 to 4 mm and 20% more than 4 mm.
Conclusion
In arthroscopic ACL reconstruction, the knee was flexed at 120° and the lowest point of the cartilage edge of the lateral wall of the intercondylar fossa and the tibial plateau plumb line were used as anatomical landmarks for the positioning of the femoral bone tunnel, which resulted in more accurate femoral bone tunnel positioning, better reproducibility, and better preservation of the femoral stump compared to traditional positioning methods.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
The anterior cruciate ligament (ACL) is an important structure for the stability of knee motion, and its tear is one of the most common knee joint injuries. Injuries to the ACL, which afflict more than 200,000 individuals yearly in the United States, account for more than half of all knee injuries [1]. The most important treatment method for ACL tears is ligament reconstruction [1, 2]. Approximately 130,000 ACL reconstruction surgeries are performed annually in the United States [3, 4]. Although positive outcomes of ACL reconstruction surgery have been reported, a review article indicates that a sizable minority of patients experience negative results and knee instability [5]. The effect of ACL reconstruction is affected by the location of the bone tunnel, the way of graft fixation, etc. A multicenter study of ACL revision reported that technique errors were the main cause of atraumatic ACL reconstruction failures, the majority of which were due to malpositioning of the tunnel socket [6].
The concept of ACL femoral bone tunnel positioning has gone through a process from isometric reconstruction to anatomical reconstruction. Biomechanical studies based on cadaveric specimens and clinical follow-up studies have found that isometric reconstruction is not effective in restoring knee rotational stability [7]. Therefore, anatomical reconstruction was favored at the beginning of the twenty-first century. Subsequent clinical studies demonstrated that anatomical reconstruction results in better rotational stability than isometric reconstruction, and isometric reconstruction of the footprint region has also been shown to have good isometric properties in a study by Forsythe et al. [8]. The clinical outcomes of anatomical single-bundle reconstruction and anatomical double-bundle reconstruction are still controversial, and most studies have concluded that there is no significant difference between anatomical double-bundle and anatomical single-bundle reconstruction of the ACL [9]. However, the anatomical single-bundle reconstruction technique is still the mainstream technique in clinical practice because of its advantage of simple operation. In recent years, with a deeper understanding of the histology and biomechanics of the ACL femoral stump, the concept of anatomical reconstruction has also made new advances. It has been claimed [10] that ACL single-bundle reconstruction centered on the anteromedial bundle results in better mechanical stability of the knee.
Existing methods of femoral tunnel localization, such as transtibial femoral offset guidance and the clock face technique, are inaccurate and outdated. Adam et al. [11] proposed to use the apex of the deep cartilage as an anatomical landmark to guide anatomical single-bundle ACL reconstruction. During surgery, clear visualization of the posterior cartilage margin of the lateral femoral condyle requires shaving the ACL femoral side stump cleanly, which loses the advantage of preserving the ACL stump. In recent years, authors such as Pearle et al. [12] have proposed the I.D.E.A.L. femoral tunnel, which refers to the placement of the femoral tunnel in a position that reproduces the isometry of the native ACL, covers the fibers of the direct insertion histologically, is eccentrically located in the anterior (high) and proximal (deep) regions of the footprint, anatomically (within the footprint), and replicates the low tension flexion pattern of the natural ACL throughout its range of flexion and extension. The idea of the I.D.E.A.L. femoral bone tunnel is now accepted by most scholars, but there is currently no consensus on the method of locating the I.D.E.A.L. femoral bone tunnel. A simple technique to assist in I.D.E.A.L. femoral tunnel positioning is therefore needed.
Femoral bone tunnel localization is traditionally performed with the knee joint flexed at 90°, but anatomical studies showed that at 90° of flexion, the socket of the posterior lateral bundle of the femoral ACL located anteriorly and inferiorly will obscure the femoral footprint area of the anteromedial bundle located posteriorly and superiorly. However, when the knee joint is flexed at 120°, due to the rotation of the femoral condyles, after the posterior lateral bundle moves anteriorly and superiorly, the anteromedial bundle moves anteriorly and inferiorly, and the latter is no longer obscured, which is more conducive to observation and localization. Therefore, by performing the procedure at 120° of knee flexion, better femoral socket exposure of the anteromedial bundle can be obtained without shaving off the posterior lateral femoral stump of the ACL. However, current studies [13,14,15] have mainly focused on the tibial side for stump preservation, and the femoral side is usually extensively cleaned to reveal the posterior cartilaginous margin of the lateral femoral condyle as an anatomical landmark. In the present study, the lowest point of the cartilage margin of the lateral wall of the intercondylar fossa of the knee and the tibial plateau drape were used as anatomical landmarks without revealing the posterior femoral wall, which can effectively preserve the femoral stump of the ACL. Thus, a simple and effective method of positioning the femoral bone tunnel that preserves the femoral side remnant of the ACL was explored.
The purpose of the present study was to investigate the use of the lowest point of the cartilaginous margin of the lateral femoral condyle and the tibial plateau as anatomical landmarks at 120° of knee flexion to guide femoral tunnel placement during anatomical single-bundle ACL reconstruction. This method can be used intraoperatively for arthroscopy.
Materials and methods
All procedures were performed by the same experienced surgeon, who performs more than 200 ACL reconstruction procedures per year. Fifty patients with unilateral ACL injuries who underwent primary single-bundle ACL reconstruction between July 2022 and December 2022 were included in this study (42 male and 8 female patients).
Inclusion criteria were as follows: the patient had a clear history of injury and instability in the affected knee; complete ACL rupture confirmed by preoperative magnetic resonance imaging (MRI) and intraoperative arthroscopy; initial ACL reconstruction; no surgical or invasive operations had previously been performed on either knee of the patient; all participants provided informed consent.
Exclusion criteria were as follows: revision ACL reconstruction, reconstruction of multiple ligament injuries, joint allograft meniscus graft, contralateral knee ACL reconstruction, combined severe cartilage injury, combined intercondylar fracture, tibial plateau fracture, etc. ACL reconstruction was performed using an autologous hamstring graft (including semitendinosus and gracilis).
The diameter of the tendon graft was kept between 8 and 9 mm [16]. The tibial bone graft was fixed with an absorbable interfacial extrusion screw (Smith & Nephew Inc, USA), while the femoral end was fixed with an Endobutton belt loop titanium plate (Smith & Nephew Inc, USA). The transpotal technique was used when drilling the femoral tunnel, as the postoperative ACL angle on the MRI of the knee is closer to the healthy side [17]. The type of ACL rupture was determined during the arthroscopic diagnosis and a decision was made whether to preserve the ACL stump. The following are some of the possible benefits of preserving the ACL stump [2, 18]: it orients native collagen in the direction of the ACL graft; advantages of standard anatomical ACL reconstruction are not lost; no loose stump in the notch; cyclops lesions are prevented; better healing and ligamentization; and no additional implants are needed.
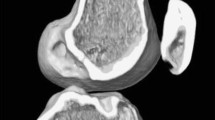
Graft harvest and preparation
Standard anteromedial and anterolateral incisions were made. The patient was placed in the supine position and epidural or general anesthesia was administered. The anteromedial approach was used for exploration and the anterolateral approach was used for standard arthroscopy. At 90° of flexion, the synovial membrane and part of the infrapatellar fat pad were removed to fully expose the medial anterior aspect of the lateral femoral condyle for easy visualization and localization. ACL rupture was confirmed (Fig. 1), and the arthroscope was withdrawn. A 2-cm skin incision was made superiorly on the medial tibia to reveal the goose foot tendon. The semitendinosus and gracilis were then removed with a tendon retriever.
Femoral tunnel preparation
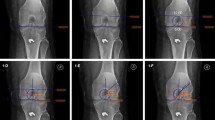
Most surgeons accept the theory of I.D.E.A.L. femoral location (Fig. 2). The I.D.E.A.L. location is located a little below the footprint of the direct fiber insertion of the anteromedial ACL bundle.The flexion mode arthroscopic femoral tunnel is positioned by first flexing the knee 120° using the anterolateral approach as the observation approach and identifying the lowest point of the cartilage margin of the femoral condyle, through which a vertical line is made with a plasma device perpendicular to the tibial plateau, which is the bifurcate ridge between the anteromedial bundle and the posterolateral bundle. A hollow drill with the same diameter as the weave was selected. The hollow drill was introduced through an anterolateral medial inferior approach in the following position: the anterior edge of the drill was tangential to the vertical line, and the underside of the drill was located approximately 2 mm from the edge of the femoral condylar cartilage. The hollow drill was used to guide a 2 mm K wire and drill through the lateral femoral cortex. Then a fine bone tunnel was drilled with a 4.5 mm hollow drill, and the depth of the tunnel was measured; according to the length of the bone tunnel and the length of the graft, a coarse bone tunnel with suitable depth was created. This is called the high flexion femur preservation and residual positioning method (Figs. 3a and b).
Tibial tunnel preparation and fixation of the graft
The tibial locator was placed in the center of the ACL stump through the anteromedial entrance, then the tibia was drilled with a 2 mm K wire, and finally, the appropriate tibial drill was selected according to the diameter of the tendon. Finally, the tendon was introduced into the bone tunnel, and it was confirmed that the Endobutton was turned and fit well at the outer opening of the bone tunnel. Arthroscopic examination confirmed that the previous markings on the graft were flush with the entrance to the femoral bone tunnel, indicating complete entry of the graft into the femoral tunnel. The squeeze screw was placed at 15° of knee flexion to maintain pressure on the graft when the reconstructed ligament tension was closest to the original ACL tension [19]. Graft impingement was assessed during the procedure with the knee fully extended (Figs. 4a and b).
Measurements
Three days after the operation, all patients underwent 3D CT in a knee extension position. The Digital Imaging and Communications Medicine (DICOM) data (Siemens 64-layer spiral CT, 1 mm thick) of the patients' postoperative knee CT images were imported into Mimics 21.0 software (Materialise, Leuven, Belgium) to reconstruct knee models (distal femur and proximal tibia), which were used to assess the position of the femoral tract of the ACL. The sagittal cut surface of the knee can be constructed as follows: first, the condylar axis is determined and the posterior and distal femoral condyles are approximated cylindrically to provide a true lateral image of the femur. This is because the intercondylar notch is different for each individual, so the axial length of the condylar axis is fixed at 100%. We used the same cutting plane for all reconstructed knee joints according to a related study [20]: at the apex of the intercondylar notch, we established a single cutting plane perpendicular to this condylar axis (C-plane). After resection of the medial femoral condyle in the C-plane, an image of the lateral femoral condyle in true lateral position was obtained. This view was used to measure the position of the femoral tunnel. The cortical extension line behind the femur was approximately regarded as the direct fiber insertion point of the ACL [21, 22]. The data were merged using Bernard and Hertel's quadrant approach [23], which has been widely used for evaluating the position of the ACL femoral footprint [23]. In the quadrant approach, there are four distances: the total sagittal diameter of the lateral condyle along the Blumensaat line (distance t), the maximum intercondylar notch height perpendicular to the Blumensaat line (distance h), the distance from the center of the footprint to the proximal border along line t (distance x), and the distance between the Blumensaat line and the center of the footprint (distance y). The distances x and y are expressed as percentages of t and h, respectively. All femoral bone tunnels were marked on a 4 × 4 grid, and the quadrant method was used to visualize the area of these tunnels. Next, dots were created to show the centers of all the bone tunnels using Photoshop (Fig. 6). The distance from the center of the circle to the t and h axes was measured as the location of the femoral bone tunnels. Finally, we utilized the sagittal plane of the lateral condyle of the knee obtained from the Mimics software for the measurement of D and E values (Fig. 5). The D value represents the thickness of the posterior wall of the bone tunnel; the E value represents the distance of the center of the bone tunnel from the posterior femoral cortical extension. The D and E values are represented as a scatterplot. The data for the location of the femoral tunnel centers are expressed as mean and standard deviation. Data were measured twice by the same surgeon at intervals greater than 1 week.
D represents the thickness of the posterior wall of the bone tunnel, E represents the distance of the center of the bone tunnel from the posterior femoral cortical extension, the red dashed line represents the posterior femoral cortical extension (intercondylar ridge), and the red dot represents the center point of the bone tunnel
Statistical analysis
Statistical analysis was carried out using SPSS software version 25.0 (SPSS Inc., Chicago, IL, USA). The mean and standard deviation were calculated. Scatterplots of D and E values were generated using Microsoft Excel 2016 (Fig. 7).
Results
As shown in Fig. 6, with the new localization method, the average distance x was 25.26 ± 2.76% of t and the average distance of y was 23.69 ± 6.19% of h. As shown in Fig. 7, the D values were distributed as follows: 60% in the range of 0 to 2 mm, 24% in the range of 2 to 4 mm, and 16% more than 4 mm. The E values were distributed as follows: 80% in the range of 0 to 4 mm and 20% more than 4 mm. Our results are in agreement with Table 1, which was obtained from Xu et al. [24]. Eight studies have shown that the theoretical center of the anteromedial bundle is 24.2 ± 4.0 × 21.6 ± 5.2. Based on Mimics measurements, these results are close to the location of the I.D.E.A.L. point reported in the present study. We believe that with the new localization method, our femoral tract is very close to the I.D.E.A.L. point. Therefore, the new positioning method can be used as a simple method to place the I.D.E.A.L. femoral tunnel in clinical ACL reconstruction and significantly shorten the operation time.
\(x\), distance from the center of the footprint to the proximal border along line \(t\); \(y\), distance from the center of the footprint to the Blumensaat line; \(x\) and \(y\) are expressed as percentages of \(t\) and \(h\). \(t\), total sagittal diameter of lateral condyle along the Blumensaat line; \(h\), maximum intercondylar notch height.
Discussion
A variety of factors have an impact on the outcome of ACL reconstruction surgery, and we are still searching for the ideal approach. The clinical results of stump-preserving reconstruction with an I.D.E.A.L. femoral tunnel have been documented in previous clinical studies [2]. The anteromedial and posterolateral bundles of the ACL have different functions. However, biomechanical studies have shown that the anteromedial bundle is the main factor associated with knee stability [25]. Several recent studies have shown that tunnel reconstruction in the center of the anteromedial bundle is desirable [26, 27]. In the present study, we performed anteromedial bundle reconstruction of the ACL.
In the present study, we performed the operation with the knee joint flexed at 120°, and the lowest point of the cartilaginous margin of the lateral femoral condyle (at 120° of flexion) and the tibial plateau were used arthroscopically as anatomical landmarks. In this way, we were able to obtain better femoral side exposure of the anteromedial bundle without extensively cleaning the posterior lateral femoral bundle stump of the ACL, and we could achieve better stump-preserving reconstruction of the femoral side of the ACL. Recent studies of residual preservation have mainly focused on the tibial side, and the femoral side is usually extensively cleaned to reveal the posterior femoral wall as an anatomical landmark. In arthroscopic surgery, removal of the ACL stump helps to improve visualization of bony landmarks on the tibia and femur and helps to localize the bone tunnel, thus making the procedure easier.
From the eight studies in Table 1, we can see that the center of the anteromedial bundle of the ACL that was ultimately derived was 24.2 ± 4.0 × 21.6 ± 5.2, whereas the center of the anteromedial bundle of the ACL in our present study was 25.26 ± 2.76 × 23.69 ± 6.19. In the present study, in 84% of the cases, the posterior wall of the femoral bone tunnel was maintained at 0–4 mm, of which 0–2 mm accounted for 60%, and our femoral bone tunnel position was very close to the posterior cartilaginous margin of the lateral condyle of the femur. The high flexion femoral side remnant preservation positioning technique is safe and avoids breaking the posterior wall of the femoral osseous tract. This is similar to the findings of authors such as Smith et al. [28], who placed the femoral bone tunnel less than 2 mm posterior to the posterior wall of the bone tunnel. In the present study, there was not one case of posterior wall rupture of the femoral bone tunnel, which indicates the safety of our high flexion femoral side remnant preservation positioning technique. Moreover, we created the femoral bone tunnel with the knee kept in flexion at 120° during the procedure, which also reduced the risk of posterior wall rupture to a certain extent. Chung et al. [29] indicated that creating the femoral osseous tract by keeping the knee flexion angle between 120° and 130° can avoid posterior wall rupture and achieve an appropriate femoral channel length.
The role of stump preservation in ACL reconstruction has been extensively studied. However, preserving the ACL stump has its drawbacks. Preservation of the stump has been shown to be a risk factor for arthrofibrosis and the formation of cyclops lesions in the knee joint.
We believe that a new method is needed to ensure the correct placement of the femoral tunnel. In the present study, the lowest point of the cartilage margin of the lateral wall of the intercondylar fossa of the knee and the vertical line between the tibial plateau and the lowest point were used as anatomical landmarks to create the ACL femoral bone tunnel at 120° of knee flexion, which enables the reconstruction of the preserved femoral stump while accurately positioning the femoral bone tunnel.
There are some limitations to this study. First, only one surgeon confirmed the location of the femoral bone tunnel during ACL reconstruction. There is currently no golden standard for the intraoperative localization of the I.D.E.A.L. femoral bone tunnel. Second, the number of cases in our study was small. For subsequent studies, we aim to include more patients to confirm our conclusions. Finally, there are anatomical differences in the knee joint that may lead to incorrect positioning.
Conclusions
In this study, during ACL reconstruction, the lowest point of the cartilage margin of the lateral wall of the intercondylar fossa of the knee and the vertical line between the tibial plateau and the lowest point were used as anatomical landmarks, and the ACL femoral tunnel was established at 120° of knee flexion, which could achieve stump-preserving reconstruction of the femur while accurately locating the femoral bone tunnel. This technique would not sacrifice the ideal position of the femoral tunnel and is able to retain the possible benefits of the ACL stump.
Availability of data and materials
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med. 2017;36(1):1–8. https://doi.org/10.1016/j.csm.2016.08.001.
Su C, Kuang SD, Liu WJ, Li YS, Xiong YL, Zhao X, Gao SG. Clinical outcome of remnant-preserving and I.D.E.A.L. femoral tunnel technique for anterior cruciate ligament reconstruction. Orthop Surg. 2020;12(6):1693–702. https://doi.org/10.1111/os.12791.
Cooper JD, Lorenzana DJ, Heckmann N, McKnight B, Mostofi A, Gamradt SC, Rick Hatch GF. The effect of obesity on operative times and 30-day readmissions after anterior cruciate ligament reconstruction. Arthroscopy. 2019;35(1):121–9. https://doi.org/10.1016/j.arthro.2018.07.032.
Griffin LY, Albohm MJ, Arendt EA, Bahr R, Beynnon BD, Demaio M, Dick RW, Engebretsen L, Garrett WE Jr, Hannafin JA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34(9):1512–32. https://doi.org/10.1177/0363546506286866.
Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW. Factors associated with revision following anterior cruciate ligament reconstruction: a systematic review of registry data. Knee. 2020;27(2):287–99. https://doi.org/10.1016/j.knee.2019.12.003.
Wright RW, Huston LJ, Spindler KP, Dunn WR, Haas AK, Allen CR, Cooper DE, DeBerardino TM, Lantz BB, Mann BJ, et al. Descriptive epidemiology of the multicenter ACL revision study (MARS) cohort. Am J Sports Med. 2010;38(10):1979–86. https://doi.org/10.1177/0363546510378645.
Fleming B, Beynnon BD, Johnson RJ, McLeod WD, Pope MH. Isometric versus tension measurements. A comparison for the reconstruction of the anterior cruciate ligament. Am J Sports Med. 1993;21(1):82–8. https://doi.org/10.1177/036354659302100115.
Forsythe B, Lansdown D, Zuke WA, Verma NN, Cole BJ, Bach BR Jr, Inoue N. Dynamic 3-dimensional mapping of isometric anterior cruciate ligament attachment sites on the tibia and femur: is anatomic also isometric? Arthroscopy. 2018;34(8):2466–75. https://doi.org/10.1016/j.arthro.2018.03.033.
Dong Z, Niu Y, Qi J, Song Y, Wang F. Long term results after double and single bundle ACL reconstruction: Is there any difference? A meta-analysis of randomized controlled trials. Acta Orthop Traumatol Turc. 2019;53(2):92–9. https://doi.org/10.1016/j.aott.2018.12.004.
Iriuchishima T, Goto B. Systematic review of surgical technique and tunnel target points and placement in anatomical single-bundle ACL reconstruction. J Knee Surg. 2021;34(14):1531–8. https://doi.org/10.1055/s-0040-1710521.
Hart A, Han Y, Martineau PA. The apex of the deep cartilage: a landmark and new technique to help identify femoral tunnel placement in anterior cruciate ligament reconstruction. Arthroscopy. 2015;31(9):1777–83. https://doi.org/10.1016/j.arthro.2015.03.026.
Pearle AD, McAllister D, Howell SM. Rationale for strategic graft placement in anterior cruciate ligament reconstruction: I.D.E.A.L. femoral tunnel position. Am J Orthop (Belle Mead NJ). 2015;44(6):253–8.
Kosy JD, Walmsley K, Gordon EA, Heddon SV, Anaspure R, Schranz PJ, Mandalia VI. Remnant preservation does not affect accuracy of tibial tunnel positioning in single-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2021;29(4):1157–63. https://doi.org/10.1007/s00167-020-06125-y.
Crain EH, Fithian DC, Paxton EW, Luetzow WF. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005;21(1):19–24. https://doi.org/10.1016/j.arthro.2004.09.015.
Masuda T, Kondo E, Onodera J, Kitamura N, Inoue M, Nakamura E, Yagi T, Iwasaki N, Yasuda K. Effects of remnant tissue preservation on tunnel enlargement after anatomic double-bundle anterior cruciate ligament reconstruction using the hamstring tendon. Orthop J Sports Med. 2018;6(12):2325967118811293. https://doi.org/10.1177/2325967118811293.
Marchand JB, Ruiz N, Coupry A, Bowen M, Robert H. Do graft diameter or patient age influence the results of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2998–3004. https://doi.org/10.1007/s00167-015-3608-6.
Jamsher M, Ballarati C, Viganò M, Hofbauer M, Togninalli D, Lafranchi S, de Girolamo L, Denti M. Graft inclination angles in anterior cruciate ligament reconstruction vary depending on femoral tunnel reaming method: comparison among transtibial, anteromedial portal, and outside-in retrograde drilling techniques. Arthroscopy. 2020;36(4):1095–102. https://doi.org/10.1016/j.arthro.2019.09.040.
Singh I, Singh A. Remnant-preserving anterior cruciate ligament reconstruction: remnant envelope technique. Arthrosc Tech. 2020;9(11):e1805–12. https://doi.org/10.1016/j.eats.2020.08.002.
Kent RN 3rd, Amirtharaj MJ, Berube EE, Imhauser CW, Thein R, Voleti PB, Wickiewicz TL, Pearle AD, Nawabi DH. Anterior cruciate ligament graft forces are sensitive to fixation angle and tunnel position within the native femoral footprint during passive flexion. Knee. 2021;33:266–74. https://doi.org/10.1016/j.knee.2021.08.003.
Miyaji N, Araki D, Hoshino Y, Kanzaki N, Nagai K, Matsumoto T, Niikura T, Kuroda R, Matsushita T. The sagittal cutting plane affects evaluation of the femoral bone tunnel position on three-dimensional computed tomography after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2021;29(2):398–404. https://doi.org/10.1007/s00167-020-05963-0.
Śmigielski R, Zdanowicz U, Drwięga M, Ciszek B, Ciszkowska-Łysoń B, Siebold R. Ribbon like appearance of the midsubstance fibres of the anterior cruciate ligament close to its femoral insertion site: a cadaveric study including 111 knees. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3143–50. https://doi.org/10.1007/s00167-014-3146-7.
Śmigielski R, Zdanowicz U, Drwięga M, Ciszek B, Williams A. The anatomy of the anterior cruciate ligament and its relevance to the technique of reconstruction. Bone Jt J. 2016;98-b(8):1020–6. https://doi.org/10.1302/0301-620x.98b8.37117.
Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg. 1997;10(1):14–21 (discussion 21–12).
Xu H, Zhang C, Zhang Q, Du T, Ding M, Wang Y, Fu SC, Hopkins C, Yung SH. A systematic review of anterior cruciate ligament femoral footprint location evaluated by quadrant method for single-bundle and double-bundle anatomic reconstruction. Arthroscopy. 2016;32(8):1724–34. https://doi.org/10.1016/j.arthro.2016.01.065.
Gardner EJ, Noyes FR, Jetter AW, Grood ES, Harms SP, Levy MS. Effect of anteromedial and posterolateral anterior cruciate ligament bundles on resisting medial and lateral tibiofemoral compartment subluxations. Arthroscopy. 2015;31(5):901–10. https://doi.org/10.1016/j.arthro.2014.12.009.
Borton ZM, Yasen SK, Mumith A, Wilson AJ. Mid-bundle positioning of the femoral socket increases graft rupture in anatomic single bundle anterior cruciate ligament reconstruction. Knee. 2018;25(6):1122–8. https://doi.org/10.1016/j.knee.2018.08.007.
Byrne KJ, Hughes JD, Gibbs C, Vaswani R, Meredith SJ, Popchak A, Lesniak BP, Karlsson J, Irrgang JJ, Musahl V. Non-anatomic tunnel position increases the risk of revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2022;30(4):1388–95. https://doi.org/10.1007/s00167-021-06607-7.
Smith CK, Howell SM, Hull ML. Anterior laxity, slippage, and recovery of function in the first year after tibialis allograft anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(1):78–88. https://doi.org/10.1177/0363546510378652.
Chung K, Choi CH, Kim SH, Kim SJ, Choi HC, Jung M. Influence of knee flexion angle on graft bending angle during anterior cruciate ligament reconstruction using the transportal technique. Sci Rep. 2023;13(1):13638. https://doi.org/10.1038/s41598-023-41002-x.
Wang HD, Wang FS, Gao SJ, Zhang YZ. Remnant preservation technique versus standard technique for anterior cruciate ligament reconstruction: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2018;13(1):231. https://doi.org/10.1186/s13018-018-0937-4.
Annear PT, Rohr EJ, Hille DM, Gohil S, Ebert JR. No clinical difference in 10-year outcomes between standard and minimal graft debridement techniques in patients undergoing anterior cruciate ligament reconstruction using autologous hamstrings: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2019;27(2):516–23. https://doi.org/10.1007/s00167-018-5146-5.
Takahashi T, Kimura M, Hagiwara K, Ohsawa T, Takeshita K. The effect of remnant tissue preservation in anatomic double-bundle ACL reconstruction on knee stability and graft maturation. J Knee Surg. 2019;32(6):565–76. https://doi.org/10.1055/s-0038-1660513.
Kim MK, Lee SR, Ha JK, Ra HJ, Kim SB, Kim JG. Comparison of second-look arthroscopic findings and clinical results according to the amount of preserved remnant in anterior cruciate ligament reconstruction. Knee. 2014;21(3):774–8. https://doi.org/10.1016/j.knee.2014.02.011.
Bali K, Dhillon MS, Vasistha RK, Kakkar N, Chana R, Prabhakar S. Efficacy of immunohistological methods in detecting functionally viable mechanoreceptors in the remnant stumps of injured anterior cruciate ligaments and its clinical importance. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):75–80. https://doi.org/10.1007/s00167-011-1526-9.
Lee BI, Min KD, Choi HS, Kwon SW, Chun DI, Yun ES, Lee DW, Jin SY, Yoo JH. Immunohistochemical study of mechanoreceptors in the tibial remnant of the ruptured anterior cruciate ligament in human knees. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1095–101. https://doi.org/10.1007/s00167-009-0831-z.
Adachi N, Ochi M, Uchio Y, Iwasa J, Ryoke K, Kuriwaka M. Mechanoreceptors in the anterior cruciate ligament contribute to the joint position sense. Acta Orthop Scand. 2002;73(3):330–4. https://doi.org/10.1080/000164702320155356.
Kim SJ, Choi CH, Chun YM, Kim SH, Lee SK, Jung WS, Jung M. Anterior cruciate ligament reconstruction using bone-patellar tendon-bone autograft with remnant preservation: comparison of outcomes according to the amount of remnant tissue. J Knee Surg. 2019;32(9):847–59. https://doi.org/10.1055/s-0038-1669902.
Beard DJ, Kyberd PJ, Fergusson CM, Dodd CA. Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Jt Surg Br. 1993;75(2):311–5. https://doi.org/10.1302/0301-620x.75b2.8444956.
Fremerey RW, Lobenhoffer P, Zeichen J, Skutek M, Bosch U, Tscherne H. Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study. J Bone Jt Surg Br. 2000;82(6):801–6. https://doi.org/10.1302/0301-620x.82b6.10306.
Takazawa Y, Ikeda H, Kawasaki T, Ishijima M, Kubota M, Saita Y, Kaneko H, Kim SG, Kurosawa H, Kaneko K. ACL reconstruction preserving the ACL remnant achieves good clinical outcomes and can reduce subsequent graft rupture. Orthop J Sports Med. 2013;1(4):2325967113505076. https://doi.org/10.1177/2325967113505076.
Choi S, Kim MK, Kwon YS, Kang H. Clinical and arthroscopic outcome of single bundle anterior cruciate ligament reconstruction: Comparison of remnant preservation versus conventional technique. Knee. 2017;24(5):1025–32. https://doi.org/10.1016/j.knee.2017.05.012.
Ahn JH, Wang JH, Lee YS, Kim JG, Kang JH, Koh KH. Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: clinical and magnetic resonance imaging results. Arthroscopy. 2011;27(8):1079–89. https://doi.org/10.1016/j.arthro.2011.03.002.
Yamamoto Y, Hsu WH, Woo SL, Van Scyoc AH, Takakura Y, Debski RE. Knee stability and graft function after anterior cruciate ligament reconstruction: a comparison of a lateral and an anatomical femoral tunnel placement. Am J Sports Med. 2004;32(8):1825–32. https://doi.org/10.1177/0363546504263947.
Colombet P, Robinson J, Christel P, Franceschi JP, Djian P, Bellier G, Sbihi A. Morphology of anterior cruciate ligament attachments for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy. 2006;22(9):984–92. https://doi.org/10.1016/j.arthro.2006.04.102.
Tsukada H, Ishibashi Y, Tsuda E, Fukuda A, Toh S. Anatomical analysis of the anterior cruciate ligament femoral and tibial footprints. J Orthop Sci. 2008;13(2):122–9. https://doi.org/10.1007/s00776-007-1203-5.
Lorenz S, Elser F, Mitterer M, Obst T, Imhoff AB. Radiologic evaluation of the insertion sites of the 2 functional bundles of the anterior cruciate ligament using 3-dimensional computed tomography. Am J Sports Med. 2009;37(12):2368–76. https://doi.org/10.1177/0363546509341577.
Forsythe B, Kopf S, Wong AK, Martins CA, Anderst W, Tashman S, Fu FH. The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Joint Surg Am. 2010;92(6):1418–26. https://doi.org/10.2106/jbjs.I.00654.
Iriuchishima T, Ingham SJ, Tajima G, Horaguchi T, Saito A, Tokuhashi Y, Van Houten AH, Aerts MM, Fu FH. Evaluation of the tunnel placement in the anatomical double-bundle ACL reconstruction: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2010;18(9):1226–31. https://doi.org/10.1007/s00167-010-1128-y.
Pietrini SD, Ziegler CG, Anderson CJ, Wijdicks CA, Westerhaus BD, Johansen S, Engebretsen L, LaPrade RF. Radiographic landmarks for tunnel positioning in double-bundle ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2011;19(5):792–800. https://doi.org/10.1007/s00167-010-1372-1.
Zantop T, Wellmann M, Fu FH, Petersen W. Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med. 2008;36(1):65–72. https://doi.org/10.1177/0363546507308361.
Acknowledgements
We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Funding
This work was supported by the 2020 Natural Science Foundation of Hubei Province (2020CFB570).
Author information
Authors and Affiliations
Contributions
RD, XL designed the study, RD conceived the study and performed the operations. HL and JS followed up the patients and collected the relevant data. XL analyzed and interpreted the data. XL wrote the manuscript and performed subsequent editing of the manuscript. XL and JL used software to import the original CT data to reconstruct 3D model. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of the General Hospital of Central Theater Command (No. [2023]059-01). All patients signed the informed consent to participate in this study.
Consent for publication
The authors affirm that patients provided informed consent regarding publishing their data and images.
Competing interests
None of the authors have conflicts of interest or commercial relations in regard to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, X., Lu, J., Su, J. et al. High flexion femoral side remnant preservation positioning technique: a new method for positioning the femoral tunnel in anterior cruciate ligament reconstruction. J Orthop Surg Res 19, 189 (2024). https://doi.org/10.1186/s13018-024-04670-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-024-04670-7