Abstract
Background
Osteosynthesis for geriatric femoral pertrochanteric fractures using the linear compression integrated screw intramedullary nail system (INTERTAN™) has become popular. Nonetheless, cases of perioperative peri-implant fractures have been reported following this surgical technique. The factors responsible for this complication remain unclear. Therefore, we investigated perioperative peri-implant fracture risk factors and incidence, as well as overall outcomes, using the INTERTAN™ system for geriatric femoral pertrochanteric fractures.
Methods
We retrospectively reviewed 98 consecutive patients with geriatric femoral pertrochanteric fractures after INTERTAN™ fixation, with at least a 12-month follow-up period between May 2020 and April 2022 at a single medical institute. The patients’ demographic characteristics, fracture pattern, quality of reduction, quality of fixation, nail length, morphology of the femur, and perioperative complications were recorded and analyzed.
Results
Among the 98 patients, 92 achieved union during follow-up. Twelve perioperative peri-implant fractures (12.2%) were recorded, all of which occurred during or within 1 month of osteosynthesis. Except for one patient who underwent re-osteosynthesis, the others underwent nonoperative treatment, and all achieved union. Multiple regression analysis revealed morphology of the femur with low-lesser trochanter width (odds ratio (OR) 0.532, 95% confidence interval (CI) 0.33–0.86, p = 0.01) to be the only factor contributing to perioperative peri-implant fractures. When the Youden index was used, the optimal cut-off value was 20.2 mm of low-lesser trochanter width. Low-lesser trochanter width < 20.2 mm was found to be a potential factor causing perioperative peri-implant fractures (OR 17.81, 95% CI 1.67–19.76, p = 0.017).
Conclusions
Morphology of the femur with a low-lesser trochanter width smaller than 20.2 mm was found to be the only potential contributor to perioperative peri-implant fractures when using INTERTAN™ for geriatric femoral pertrochanteric fractures. Care should be taken during osteosynthesis, focusing not only on the fracture site but also on the femoral cortex around the implant. Although perioperative peri-implant fractures were observed within one month following osteosynthesis, the majority of these cases were effectively treated without surgical intervention.
Similar content being viewed by others
Introduction
Geriatric femoral pertrochanteric fractures (GFPF) are among the most common operatively treated fractures in the geriatric population [1, 2]. The estimated global annual incidence of GFPF exceeds 1.6 million fractures, with a rising trend [3,4,5]. While the risk associated with anesthesia is a concern for older individuals, surgical intervention offers significant benefits over nonoperative treatment, particularly in terms of preventing complications arising from extended periods of immobility, facilitating the recovery of mobility, and reducing one-year mortality rates [6,7,8,9,10].
Traditionally, the preferred method for treating GFPFs has been the use of a sliding hip screw (SHS), owing to its high union rate, easy application, and cost-effectiveness [11,12,13]. However, there is a growing trend toward the use of intramedullary nails (IMN) for osteosynthesis [14,15,16]. Biomechanical studies and clinical evidence indicate that IMN surpass SHS in various aspects, including a shorter lever arm, better control over femoral shaft medialization, prevention of varus collapse, and reduced soft tissue dissection [17,18,19,20].
Over the years, advancements have been made in the design of IMN for treating GFPFs [21,22,23,24,25]. One such new IMN design is the linear compression integrated screw intramedullary nail system (INTERTAN™, Smith-Nephew Company), which incorporates a dual screw system that aims to provide anti-rotation of the femoral head (2-screw design) and achieve linear compression of the fracture gap (integrated screw design), thereby promoting bone union and avoiding complications such as proximal screw cut-off or cut-out from the femoral head [26, 27]. Studies have demonstrated that this new IMN design exhibits superior biomechanical outcomes compared with those of a single-lag screw nailing system [28,29,30].
However, as the utilization of IMN for GFPF treatment has increased, certain complications such as implant cut-out, implant breakage, and secondary femoral fractures have been documented [31,32,33]. Among them, perioperative peri-implant fractures (PPIF) are a notable concern. The reported incidence of PPIF ranges from 1 to 3%, varying depending on the specific implant design [34]. PPIF is a troublesome complication characterized by the occurrence of a new fracture shortly after the initial fracture, often necessitating repeated osteosynthesis. Despite its significance, few studies have evaluated the potential risk factors associated with PPIF following IMN treatment of GFPF.
This study aimed to accomplish the following objectives: (1) determine the incidence of PPIF, (2) analyze the potential risk factors associated with PPIF, and (3) report the outcomes following the occurrence of PPIF in osteosynthesis procedures for GFPF utilizing the linear compression integrated screw intramedullary nail system.
Methods
We retrospectively reviewed the medical and radiological records from the institutional trauma registry of patients with GFPF who underwent osteosynthesis using the INTERTAN nail with the linear compression integrated screw intramedullary nail system (TRIGEN™ INTERTAN) between May 2020 and April 2022 at our institute. The review process was approved by our Institutional Review Board (IRB No. 202301241B0).
The INTERTAN nail was introduced in our institution in 2018. The available diameters of the INTERTAN nail were 10 mm, 11.5 mm, and 13 mm, with the 10 mm diameter being the smallest size. The inclusion criteria were patients aged > 60 years old who experienced femoral pertrochanteric fractures and underwent osteosynthesis using an INTERTAN nail, with complete medical and radiological follow-up for at least 12 months or until union. Fractures requiring revision osteosynthesis, those involving more than 2 parts of the femur, and those of pathological origin were excluded. Radiological follow-ups were conducted for all patients immediately after the surgery and at 1-, 3-, 6-, and 12-month intervals. The patients’ demographic profiles, fracture patterns, quality of reduction (QoR), quality of fixation (QoF), nail length (NL), morphology of the femur (MoF), and complications were recorded and analyzed.
Applied classification
The pertrochanteric fracture was classified based on the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification system (2018 revision), including A1: simple pertrochanteric fracture; A2: multifragmentary pertrochanteric fracture or incompetence of the lateral wall (thickness ≤ 20.5 mm); and A3: intertrochanteric or reverse oblique fracture [26, 35]. Patients presenting with AO 31-A1 and -A2 fractures were primarily treated with short nails, specifically 180 mm and 200 mm in length. Conversely, individuals with fractures located in the intertrochanteric region accompanied by subtrochanteric extension, falling under the classification of AO 31-A3, were typically recommended for treatment using long nails as the standard implant option.
Radiological evaluations
The QoR was assessed by comparing the neck-shaft angle of the operated site to that of the contralateral healthy hip on pelvic anteroposterior radiography and was classified as: “good” with less than 5 degrees difference from the normal side, “acceptable” with between 5 and 10 degrees of variation, and “poor” with more than 10 degrees of variation [36]. Other radiological parameters included varus (neck-shaft angle < 125°) or valgus reduction (neck-shaft angle > 125°) [37]. Positive, neutral, and negative medial femoral cortical supports were also evaluated [38, 39].
QoF was assessed based on the position of the lag screw using the tip-apex distance (TAD) and the Cleveland index [40, 41]. A critical TAD of 25 mm was established, as a TAD value of < 25 mm was considered protective against screw cut-out of the femoral head or failure [42]. The position of the lag screw tip was assessed using the Cleveland index [40]. As these evaluations were based on the single lag screw design of the implants, evaluations using the INTERTAN™ implant were conducted based on the upper screw in terms of the lag screw.
Because the geometry of the proximal femur may influence the PPIF, the MoF was also measured according to the radiographs, including the diameter of the isthmus (DI), lesser trochanter width (LTW), low-lesser trochanter width (LLTW) (cavity width 20 mm below the mid-lesser trochanter line), and canal flare index (the ratio of the DI in the anteroposterior view to the LTW) (Fig. 1) [43,44,45,46].
All the selected parameters were calibrated by using the corresponding nail size on the X-ray on the PACS system (Centricity Enterprise Web V3.0; GE Healthcare, Chicago, USA).
Rehabilitation protocol
Immediate walker-assisted weight-bearing ambulation is usually advised for GFPF. However, the rehabilitation protocol shifted more conservatively when a PPIF was identified. First, we considered whether the new fracture was stable or unstable with a nail present. If the fracture was unstable, re-do osteosynthesis with a long nail was necessary. In contrast, conservative treatment was chosen when the PPIF was stable. For patients with stable PPIF, a non-weight-bearing rehabilitation program was suggested for at least 6 weeks after the operation. When callus was detected on the follow-up X-ray, walker-assisted partial weight-bearing ambulation was begun. Finally, full weight-bearing ambulation was allowed when more callus formed, usually 3 months after the index surgery.
Statistical analysis
Descriptive statistics were used to summarize cohort characteristics, with means and standard deviations reported for continuous variables, and frequencies and percentages for categorical variables. Continuous variables were compared using the Student’s t-test. Categorical variables were compared using Chi-square and Fisher’s exact tests. All analyses were performed using SPSS software (version 23.0; IBM Corp., Armonk, NY, USA). Statistical significance was determined using a two-tailed p-value less than 0.05.
Results
Ninety-eight patients who met the inclusion criteria during the study period were enrolled; their demographic data are shown in Table 1. While six patients showed nonunion of the fracture and required re-osteosynthesis, the union rate reached 93.9% (92 out of 98). Twelve patients experienced PPIF (incidence: 12.2%). Among the 12 cases of PPIF, 10 were identified during intraoperative fluoroscopic examination. The other 2 cases of PPIF were observed without new trauma by X-ray follow-up within 1 month postoperatively. One patient with an PPIF required revised osteosynthesis owing to the long extension of the fracture distal to the implant (Fig. 2). For the remaining 11 patients, union of the PPIF was achieved by nonoperative treatment within 9 months (Fig. 3).
An illustration of perioperative peri-implant fracture (PPIF) that underwent revision osteosynthesis. A A femoral intertrochanteric fracture underwent osteosynthesis. B Nonoperative treatment for PPIF (arrow). C The fracture extended to the diaphysis 2 months later. D and E Revised osteosynthesis was performed
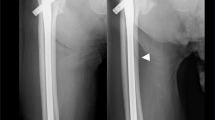
Illustrations of perioperative peri-implant fracture (PPIF) and related nonoperative treatment. A and D Femoral intertrochanteric fractures underwent osteosynthesis. B and E PPIF was noted over the lateral femoral cortex (arrow). C and F Cortical continuity achieved 6 months later by nonoperative treatment
Table 2 compares selected factors between patients with (PPIF group) and without (NPPIF group) PPIF. The PPIF group had a higher BMI than the NPPIF group (23.2 versus 27.3, p = 0.005). The other significant finding was the MoF: the PPIF group had a smaller LTW (30.8 mm versus 28.0 mm, p = 0.026), smaller LLTW (23.2 mm versus 18.7 mm, p = 0.001), and smaller DI (14.4 versus 12.1, p = 0.002).
Because a relatively small number of patients was enrolled, a stepwise method of multivariate logistic regression analysis was applied (Table 3), which resulted in only one significant independent predictor: LLTW (odds ratio (OR): 0.532, 95% confidence interval (CI) = 0.33–0.86, p = 0.01). The area under the curve was 0.874 (OR 17.81, 95% CI 1.67–19.76, p = 0.017) on the receiver operating characteristic curve. The Youden index revealed that the optimal cutoff value of LLTW was 20.2 mm (Fig. 4).
Discussion
Only a few studies have addressed the occurrence of PPIF and its associated factors in Asian populations using a single implant for GFPF [47]. With reference to this gap in the literature, our study revealed that the incidence of PPIF in patients with GFPF after INTERTAN™ fixation was 12.2%, which was relatively higher than the rates reported by other studies (1 to 3%) [34, 47, 48]. Moreover, through femoral morphology analysis, we identified a specific potential factor, namely, the width of the LLTW, which might be responsible for causing PPIF. We found that a critical LLTW width of less than 20.2 mm could significantly increase the risk of PPIF.
Although employing the SHS system to treat GFPF has a long history, using a proximal femoral intramedullary nail for such fractures has been shown to offer several advantages [14, 18]. However, accompanying complications such as PPIF after nailing may increase. A systematic review reported that the incidence of secondary fractures around the nail is 1.7% [34]. Additionally, Muller et al. reported that peri-implant fractures occur within the proximal femoral nails much more frequently than in dynamic hip screws [33], and the position of the lag screw is a potential factor associated with PPIF. Helwig et al. conducted a laboratory study using finite element analysis and discovered that cranial positioning of the lag screw increased stress on the proximal femur, contributing to a higher risk of peri-implant fracture [49]. In this study, the lag screws were positioned at the center-center or inferior-center in the femoral head, adhering to the criteria of TAD (less than 25 mm) and the Cleveland index, which aimed to prevent migration of the lag screw and facilitate fracture union. Consequently, the present study did not find evidence supporting the influence of an inappropriate lag screw position on PPIF occurrence.
The potential effect of short or long intramedullary nails on PPIF remains uncertain. Frisch et al. conducted a comparative study involving 169 patients and reported a higher peri-implant fracture rate in short nails than in long nails [50]. However, other studies have indicated no difference in the incidence of PPIF between short and long nails [34, 47, 51]. In our study, there was no significant difference in the PPIF rates between short and long nails. Of the 12 PPIFs, 11 occurred near the subtrochanteric area and were effectively treated using nonoperative methods. However, in one case, re-osteosynthesis was necessary because the short nail lost its stability. This observation leads us to advocate for the use of long nails in high-risk patients (those with a narrow LLTW measuring less than 20.2 mm). This can improve stability and reduce the need for re-do surgery if PPIF occurs.
Irrespective of the design and geometry of the intramedullary nail, patient factors such as increased BMI might have influenced the PPIF. However, the cause of the relatively high incidence of PPIF after intramedullary nail fixation remains unclear. Based on our analysis, a potential factor contributing to PPIF could be the discrepancy between the bone mineral density and the INTERTAN™ design. Notably, Asian populations have been observed to possess a greater cortical thickness in the proximal femur compared to that in Caucasian individuals [52]. Thiesen et al. reported that the proximal isthmus distance was relatively consistent but was more proximal in Asians than in Caucasians [53]. The INTERTAN™ nail is specifically designed with a proximal trapezoidal shape to enhance strength and stability during flexion and extension of the femur. However, due to the proximity of the isthmus and thickness of the femoral cortex in the Asian population, the insertion of a trapezoidal proximal nail may add additional stress to the proximal femoral cortex, theoretically leading to an increased risk of PPIF in this population.
Despite efforts to minimize bias, our study has certain limitations. First, its retrospective design introduced the risk of recall bias, and the relatively small sample size from a single institution may have led to potential bias. The limited sample size also constrained our ability to identify the independent risk factors for PPIF. Additionally, the inclusion of several orthopedic surgeons in the study might have introduced bias owing to variations in surgical techniques. Furthermore, quantification of femoral geometry relies on radiography instead of more precise methods, such as computed tomography. The position of the patient during the X-ray examinations may have also influenced the results. Moreover, certain anatomical details, such as femoral bowing, were not obtained, and these anatomical variations may play a role in PPIF development. Finally, the fracture pattern of PPIF was evaluated only by X-rays. A computed tomography scan would be a better examination tool to clarify the pattern and orientation of the fracture. This would allow for better assessment of treatment options (conservative treatment or re-do osteosynthesis). Further prospective studies with larger sample sizes and well-designed image interpretations, such as computed tomography, should be conducted. This would help gain a deeper understanding of the condition and its potential risk factors.
Conclusions
While INTERTAN™ has shown a high union rate in treating GFPF, it is crucial to be vigilant regarding the occurrence of PPIF. A narrow LLTW measuring less than 20.2 mm emerges as a potential risk factor for an unforeseen fracture. Care should be taken during osteosynthesis, especially during insertion of the nail, not only concentrating on the fracture site but also considering the entire femur surrounding or distal to the implant. Despite the occurrence of PPIF, most cases can be effectively managed without surgical intervention. Nonoperative approaches have shown promise in managing PPIF with favorable outcomes.
Availability of data and material
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AO:
-
Arbeitsgemeinschaft für Osteosynthesefragen
- CI:
-
Confidence interval
- DI:
-
Diameter of the isthmus
- GFPF:
-
Geriatric femoral pertrochanteric fractures
- IMN:
-
Intramedullary nails
- INTERTAN:
-
Integrated screw intramedullary nail system
- LLTW:
-
Low-lesser trochanter width
- LTW:
-
Lesser trochanter width
- MoF:
-
Morphology of the femur
- NL:
-
Nail length
- NPPIF:
-
Without PPIF
- OR:
-
Odds ratio
- PPIF:
-
Perioperative peri-implant fractures
- QOF:
-
Quality of fixation
- QoR:
-
Quality of reduction
- SHS:
-
Sliding hip screw
- TAD:
-
Tip–apex distance
References
Womble TN, Kirk A, Boyle M, Comadoll SM, Su L, Srinath A, et al. Comparison of short, intermediate, and long cephalomedullary nail length outcomes in elderly intertrochanteric femur fractures. J Am Acad Orthop Surg Glob Res Rev. 2022;6:e2100322.
Date A, Panthula M, Bolina A. Comparison of clinical and radiological outcomes in intertrochanteric fractures treated with InterTAN nail against conventional cephalomedullary nails: a systematic review. Future Sci OA. 2020;7:FSO668.
Huette P, Abou-Arab O, Djebara AE, Terrasi B, Beyls C, Guinot PG, et al. Risk factors and mortality of patients undergoing hip fracture surgery: a 1-year follow-up study. Sci Rep. 2020;10:9607.
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22:465–75.
Maffulli N, Aicale R. Proximal femoral fractures in the elderly: a few things to know, and some to forget. Medicina. 2022;58(10):1314.
Quaranta M, Miranda L, Oliva F, Migliorini F, Pezzuti G, Maffulli N. Haemoglobin and transfusions in elderly patients with hip fractures: the effect of a dedicated orthogeriatrician. J Orthop Surg Res. 2021;16(1):387.
Tay E. Hip fractures in the elderly: operative versus nonoperative management. Singapore Med J. 2016;57:178–81.
Lee J, Shin KY, Nam HW, Oh M, Shim GS. Mortality rates of hip fracture patients with non-operative treatment. Jt Dis Relat Surg. 2022;33:17–23.
Hwang KT, Moon JK, Kim YH. Do we really need a surgery for hip fractures in elderly patients? Mortality rate and influencing factors. Arthroplasty. 2019;1:7.
Chen YP, Kuo YJ, Hung SW, Wen TW, Chien PC, Chiang MH, et al. Loss of skeletal muscle mass can be predicted by sarcopenia and reflects poor functional recovery at one year after surgery for geriatric hip fractures. Injury. 2021;52(11):3446–52.
Stern R. Are there advances in the treatment of extracapsular hip fractures in the elderly? Injury. 2007;38(Suppl 3):S77-87.
Alessio-Mazzola M, Traverso G, Coccarello F, Sanguineti F, Formica M. Dynamic hip screw versus intramedullary nailing for the treatment of A1 intertrochanteric fractures: a retrospective, comparative study and cost analysis. Jt Dis Relat Surg. 2022;33:314–22.
Lee YS, Huang HL, Lo TY, Huang CR. Dynamic hip screw in the treatment of intertrochanteric fractures: a comparison of two fixation methods. Int Orthop. 2007;31:683–8.
Werner BC, Fashandi AH, Gwathmey FW, Yarboro SR. Trends in the management of intertrochanteric femur fractures in the United States 2005–2011. Hip Int. 2015;25:270–6.
Anglen JO, Weinstein JN. American board of orthopaedic surgery research committee nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice a review of the American board of orthopaedic surgery database. J Bone Joint Surg Am. 2008;90:700–7.
Marsillo E, Pintore A, Asparago G, Oliva F, Maffulli N. Cephalomedullary nailing for reverse oblique intertrochanteric fractures 31A3 (AO/OTA). Orthop Rev. 2022;14(6):38560.
Horwitz DS, Tawari A, Suk M. Nail length in the management of intertrochanteric fracture of the femur. J Am Acad Orthop Surg. 2016;24:e50–8.
Bonnaire F, Lein T, Bula P. Trochanteric femoral fractures: anatomy, biomechanics and choice of implants. Der Unfallchirurg. 2011;114:491–500.
Matre K, Vinje T, Havelin LI, Gjertsen JE, Furnes O, Espehaug B, et al. TRIGEN INTERTAN intramedullary nail versus sliding hip screw: a prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up. J Bone Joint Surg Am. 2013;95:200–8.
Grønhaug KML, Dybvik E, Matre K, Östman B, Gjertsen JE. Intramedullary nail versus sliding hip screw for stable and unstable trochanteric and subtrochanteric fractures: 17,341 patients from the Norwegian hip fracture register. Bone Joint J. 2022;104-B:274–82.
Gargano G, Poeta N, Oliva F, Migliorini F, Maffulli N. Zimmer natural nail and ELOS nails in pertrochanteric fractures. J Orthop Surg Res. 2021;16(1):509.
Su Z, Yang M, Luo G, Liang L, Hao Y. Treatment of elderly femoral intertrochanteric fracture by InterTan intramedullary nail and PFNA. Evid Based Complement Alternat Med. 2022;2022:5020960.
Winnock de Grave P, Tampere T, Byn P, Van Overschelde J, Pattyn C, Verdonk R. Intramedullary fixation of intertrochanteric hip fractures: a comparison of two implant designs. A prospective randomised clinical trial. Acta Orthop Belg 2012; 78: 192–8.
Makridis KG, Georgaklis V, Georgoussis M, Mandalos V, Kontogeorgakos V, Badras L. Comparing two intramedullary devices for treating trochanteric fractures: a prospective study. J Orthop Surg Res. 2010;5:9.
Yalın M, Golgelioglu F, Key S. Intertrochanteric femoral fractures: a comparison of clinical and radiographic results with the proximal femoral intramedullary nail (PROFIN), the anti-rotation proximal femoral nail (A-PFN), and the InterTAN nail. Medicina. 2023;59:559.
Ma JX, Kuang MJ, Fan ZR, Xing F, Zhao YL, Zhang LK, et al. Comparison of clinical outcomes with InterTan vs gamma nail or PFNA in the treatment of intertrochanteric fractures: a meta-analysis. Sci Rep. 2017;7:15962.
Luo W, Fu X, Ma JX, Huang JM, Wu J, Ma XL. Biomechanical comparison of INTERTAN nail and Gamma3 nail for intertrochanteric fractures. Orthop Surg. 2020;12:1990–7.
Santoni BG, Nayak AN, Cooper SA, Smithson IR, Cox JL, Marberry ST, et al. Comparison of femoral head rotation and Varus collapse between a single lag screw and integrated dual screw intertrochanteric hip fracture fixation device using a cadaveric hemi-pelvis biomechanical model. J Orthop Trauma. 2016;30:164–9.
Santoni BG, Diaz MA, Stoops TK, Lannon S, Ali A, Sanders RW. Biomechanical investigation of an integrated 2-screw cephalomedullary nail versus a sliding hip screw in unstable intertrochanteric fractures. J Orthop Trauma. 2019;33:82–7.
Nherera L, Trueman P, Horner A, Watson T, Johnstone AJ. Comparison of a twin interlocking derotation and compression screw cephalomedullary nail (InterTAN) with a single screw derotation cephalomedullary nail (proximal femoral nail antirotation): a systematic review and meta-analysis for intertrochanteric fractures. J Orthop Surg Res. 2018;13:46.
Chan LWM, Gardner AW, Wong MK, Chua K, Kwek EBK. Singapore orthopaedic research collaborative (SORCE). Non-prosthetic peri-implant fractures: classification, management and outcomes. Arch Orthop Trauma Surg. 2018;138:791–802.
Lang NW, Joestl J, Payr S, Platzer P, Sarahrudi K. Secondary femur shaft fracture following treatment with cephalomedullary nail: a retrospective single-center experience. Arch Orthop Trauma Surg. 2017;137:1271–8.
Müller F, Galler M, Zellner M, Bäuml C, Marzouk A, Füchtmeier B. Peri-implant femoral fractures: the risk is more than three times higher within PFN compared with DHS. Injury. 2016;47:2189–94.
Norris R, Bhattacharjee D, Parker MJ. Occurrence of secondary fracture around intramedullary nails used for trochanteric hip fractures: a systematic review of 13,568 patients. Injury. 2012;43:706–11.
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32(Suppl 1):S1–170.
Sharma A, Mahajan A, John B. A comparison of the clinico-radiological outcomes with proximal femoral nail (PFN) and proximal femoral nail antirotation (PFNA) in fixation of unstable intertrochanteric fractures. J Clin Diagn Res. 2017;11:RC-05-RC−09.
Hoffmann MF, Khoriaty JD, Sietsema DL, Jones CB. Outcome of intramedullary nailing treatment for intertrochanteric femoral fractures. J Orthop Surg Res. 2019;14:360.
Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg. 2015;135:811–8.
Tian KW, Zhang LL, Liu C, Chen XT, Chen K. The positive, neutral, and negative cortex relationship in fracture reduction of per/inter-trochanteric femur fractures. Int Orthop. 2020;44:2475–6.
Cleveland M, Bosworth DM, Thompson FR, Wilson HJ Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959;41-A:1399–408.
Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–64.
Cai Y, Feng J, Chen Y, Shi M, Yu Z, Fang L, et al. Comparison of the predictive value of tip-apex distance and calcar referenced tip-apex distance in treatment of femoral intertrochanteric fractures with Asian type proximal femoral nail fixation. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2020;34:1359–63.
Sevil-Kilimci F, Kara ME. Canal flare index in the canine femur is influenced by the measurement method. Vet Comp Orthop Traumatol. 2020;33:198–204.
Tawada K, Iguchi H, Tanaka N, Watanabe N, Murakami S, Hasegawa S, et al. Is the canal flare index a reliable means of estimation of canal shape? Measurement of proximal femoral geometry by use of 3D models of the femur. J Orthop Sci. 2015;20:498–506.
de Andrade CR, Minto BW, Dreibi RM, Diogo LMI, Kawamoto FYK, Franco GG, et al. Accuracy in determining canal flare index using different radiographical positions for imaging canine femurs. Vet Comp Orthop Traumatol. 2019;32:234–40.
Zhao R, Cai H, Tian H, Zhang K. Morphological consistency of bilateral hip joints in adults based on the X-ray and CT data. Surg Radiol Anat. 2021;43:1107–15.
Halonen LM, Stenroos A, Vasara H, Kosola J. Peri-implant fracture: a rare complication after intramedullary fixation of trochanteric femoral fracture. Arch Orthop Trauma Surg. 2022;142:3715–20.
Sop A, Kali M, Bishara P, Broce M, Wallace L, Damayanti S. Risk of peri-implant fracture with long versus short cephalomedullary nailing for geriatric patients with intertrochanteric femur fracture. Orthopedics. 2022;45:304–9.
Helwig P, Faust G, Hindenlang U, Hirschmüller A, Konstantinidis L, Bahrs C, et al. Finite element analysis of four different implants inserted in different positions to stabilize an idealized trochanteric femoral fracture. Injury. 2009;40:288–95.
Frisch NB, Nahm NJ, Khalil JG, Les CM, Guthrie ST, Charters MA. Short versus Long cephalomedullary nails for pertrochanteric hip fracture. Orthopedics. 2017;40:83–8.
Shannon SF, Yuan BJ, Cross WW 3rd, Barlow JD, Torchia ME, Holte PK, et al. Short versus long cephalomedullary nails for pertrochanteric hip fractures: a randomized prospective study. J Orthop Trauma. 2019;33:480–6.
Marshall LM, Zmuda JM, Chan BK, Barrett-Connor E, Cauley JA, Ensrud KE, et al. Osteoporotic fractures in men (MrOS). Research group race and ethnic variation in proximal femur structure and BMD among older men. J Bone Miner Res. 2008;23:121–30.
Thiesen DM, Ntalos D, Korthaus A, Petersik A, Frosch KH, Hartel MJ. A comparison between Asians and Caucasians in the dimensions of the femoral isthmus based on a 3D-CT analysis of 1189 adult femurs. Eur J Trauma Emerg Surg. 2022;48:2379–86.
Acknowledgements
Not applicable.
Funding
The authors declare that no funds, grants, or other support was received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
CYL and YHY contributed to conceptualization; CYL, CHL, PJL, and YHH done investigation; CYL, YCC, and YHY helped in writing; YHY contributed to writing-review and supervision. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Institutional Review Board of Chang Gung Memorial Hospital (IRB NO: 20230124B0). The requirement for informed consent was waived because of the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lai, CY., Liu, CH., Lai, PJ. et al. Perioperative peri-implant fracture after osteosynthesis for geriatric femoral pertrochanteric fracture with the linear compression integrated screw intramedullary nail system (INTERTAN™): a retrospective study. J Orthop Surg Res 18, 932 (2023). https://doi.org/10.1186/s13018-023-04441-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04441-w