Abstract
Background
Hip fractures are common in elderly patients, in whom it is important to monitor blood loss; however, unnecessary transfusions should be avoided. The primary objective of this study was to assess whether the employment of a dedicated orthogeriatrician in an Orthopaedic Department allows to optimise the clinical conditions of patients, influencing blood loss and consequently the number of transfusions. The secondary objective was to determine whether the influence of the orthogeriatrician differs according to the type of surgical treatment.
Methods
A total of 620 elderly patients treated for hip fracture were included in the study. These patients were divided into two groups according to the presence or not of the orthogeriatrician. For each patient, age, sex, comorbidities, type of fracture, surgical treatment, length of hospital stay, time from hospitalisation and surgery, time from surgery to discharge, haemoglobin (Hb) values (admission, 24h post-surgery, lowest Hb reached, discharge) and the number of transfusions were recorded.
Results
Regardless of the surgical procedure performed, in patients managed by the orthogeriatrician, the Hb at discharge was significantly higher (p = 0.003). In addition to the highest Hb at discharge, in patients who underwent hemiarthroplasty, the number of transfusions per patient is significantly reduced (p = 0.03).
Conclusion
The introduction of the orthogeriatrician in an orthopaedic ward for the management of elderly patients treated for hip fracture allows to discharge the patients with higher Hb values, reducing the risk of anemisation and the costs related to possible re-admission.
Similar content being viewed by others
Introduction
Hip fractures are common in elderly patients [1,2,3,4,5,6]. They can be classified as medial, or intracapsular fractures, related to an increased risk of osteonecrosis of the femoral head [7,8,9,10,11,12] and lateral, or extracapsular fractures [13,14,15,16]. The main risk factor for hip fractures is osteoporosis [2, 17,18,19,20]. Type II osteoporosis, which is age-related, is a risk factor for both female and male patients [2, 17, 18, 20]; type I, postmenopausal, is responsible for the increased incidence of hip fractures in female patients [21,22,23]. Most patients report an accidental fall, often the result of a bone failure related to advanced osteoporosis [1, 2, 4, 6]. These patients often have comorbidities, especially cardiovascular [1, 4, 16, 24,25,26]. In patients with hip fractures, it is important to monitor blood loss caused by both trauma and subsequent surgical treatment. Therefore, it is necessary to constantly examine laboratory tests, such as haematocrit and haemoglobin (Hb), so as to intervene promptly with blood transfusions to restore acceptable values [27,28,29,30]. However, unnecessary transfusions should be avoided because they represent both a risk factor for adverse outcomes and unjustified expenditure [27,28,29,30]. In this perspective, a close collaboration between orthopaedic and orthogeriatrician may provide both clinical and economic advantages. The orthogeriatrician plays a crucial role enhancing and stabilising medical conditions to allow faster access to the actual surgery and reduce the postoperative length of the hospital stay [2].
The primary objective of the present study is to assess whether, in the interdisciplinary management of elderly patients with hip fracture, the employment of a dedicated orthogeriatrician allows to optimise the clinical conditions of patients, influencing blood loss and consequently the number of transfusions. The secondary objective was to determine whether the influence of the orthogeriatrician differs according to the type of surgical treatment: cephalomedullary nail, hip hemiarthroplasty (HHA) or total hip arthroplasty (THA).
Materials and methods
Study design
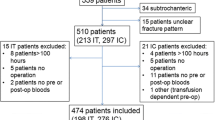
Data were collected from the Academic Department of Trauma and Orthopaedics of the San Giovanni di Dio e Ruggi d’Aragona Hospital of Salerno database. Data were collected for elderly patients undergoing hip fracture surgery for 2 years. From February 1, 2017, to January 31, 2018, before a dedicated orthogeriatrician started to work in the department; and from February 1, 2018, to January 31, 2019, with the employment of the orthogeriatrician in the department. The inclusion criteria were age ≥ 65, intra- and extra-capsular femoral fractures, fragility fractures and low energy trauma. Patients < 65 years with hip fractures resulting from high-energy trauma and/or pathological fractures were excluded. Considering the inclusion and exclusion criteria, a total of 620 patients were included in the study. These patients were divided into two groups according to the presence or not of the orthogeriatrician: 296 patients were included in the Pre-O group (February 1, 2017–January 31, 2018), and 324 patients in the Post-O group (February 1, 2018–January 31, 2019). Two orthopaedic residents worked on data collection and statistical analysis. For each patient, we recorded age, sex, comorbidities, type of fracture (intra/extra-capsular), surgical treatment performed, length of hospital stay (LOS), time from hospitalisation and surgery, time from surgery to discharge, haemoglobin (Hb) values (admission, 24h post-surgery, lowest Hb reached, discharge) and the number of transfusions.
Orthopaedic surgeon-orthogeriatrician: coordinated activity
Every day, each patient admitted is evaluated with the close collaboration between the staff of the orthopaedic surgeon and the orthogeriatrician. The orthogeriatrician evaluates and manages the general health conditions of the patients, while the orthopaedic deals with the clinical and surgical aspects of the fracture. Following the evaluation of laboratory parameters, management is reassessed and changed if indicated. The levels of Hb are followed to intervene promptly with transfusions, thus avoiding the risk of anaemia. The threshold values of Hb to start the transfusion are debated; often, the decision to transfuse is related to the clinical conditions of patients and associated comorbidities and not to the actual absolute value of haemoglobin concentration.
Statistical analysis
Descriptive statistic was used for data related to the demographic characteristics of the two groups (mean, range, standard deviation, and percentages). The statistical analysis of continuous variables was performed using the Student t test, while categorical variables were analysed with the chi-square test. The test is considered statistically significant if the p value is < 0.05.
Results
A total of 620 patients were identified and included in the study; 479 (77.3%) were women and 141 (22.7%) men. The average age was 83.85 years (SD 7.35; range from 53 to 99 years). The Pre-O group includes 296 (47.7%) patients, 71 (23.9%) males and 225 (76.1%) females, with an average age of 84.1 years (SD 7.02; range from 63 to 98). One hundred ninety-eight (66.89%) patients were managed surgically with a cephalomedullary nail; 90 (30.41%) with HHA and the remaining 8 (2.7%) patients with THA. The Post-O group includes 324 (52.26%) patients, 70 (21.6%) males and 254 (78.4%) females; the average age was 83.6 years (SD 7.64; range from 53 to 99). In this group, 210 (64.81%) patients were managed with a cephalomedullary nail, 97 (29.95%) with HHA and 17 (5.24%) with THA.
Table 1 summarises the demographic characteristics of the two groups.
Hb and transfusions
Analysing the values of Hb for each group, regardless of the surgical procedure performed, we obtained data reported in Table 2. No complications related to the blood transfusions were recorded. The mean haemoglobin values at admission did not differ statistically between the two groups (p = 0.9), with 11.96 mg/dL (SD 1.76; range from 7 to 16.2) in the Pre-O group and 11.97 mg/dL (SD 1.7; range from 5 to 18.2) in the Post-O group. The day after surgery (24 h), the mean values of Hb decreased respectively to 9.43 mg/dL (SD 1.29; range from 5.7 to 13.5) and 9.56 mg/dL (SD 1.31; range from 5.6 to 14.6) (p = 0.21). The lowest Hb is achieved after 2.08 days (SD 2.02; range from −7 to 9) in the Pre-O group with average values of 8.33 mg/dl (SD 0.95; range from 5.1 to 13.1); while in the Post-O group is reached after 1.96 days (SD 2.14; range from −12 to 13) with average values of 8.42 mg/dL (SD 1; range from 3.5 to 13.1). However, there are no significant differences related to the day (p = 0.5) and the lowest Hb value reached (p = 0.3). There was a significant difference between the two groups in the Hb at discharge (p = 0.003), with 10.07 mg/dl (SD 0.82; range from 8.2 to 13.3) in the Pre-O group and 10.27 mg/dl (SD 0.84; range from 8.5 to 14.5) in the Post-O group. A total of 541 transfusions were performed in the Pre-o Group, with a mean of 1.84 (SD1.4; range from 0 to 8) transfusions per patient; 551 transfusions were performed in the Post-O group with a mean of 1.7 (SD 1.46; range from 0 to 8) transfusions per patient (p = 0.2). No significant difference was found in relation to LOS, pre- and post-surgical days.
Hb and transfusion: cephalomedullary nail
The data on patients who underwent cephalomedullary nailing are reported in Table 3. The Pre-O group includes 198 patients with an average age of 84.6 years (SD 6.52; range from 65 to 98); the Post-O group includes 210 patients with a mean of 84.9 years (6.4; from 66 to 99) (p = 0.6). The mean Hb at admission was 11.73 mg/dL (SD 1.69; range from 7 to 15.6) in the Pre-O group and 11.61 mg/dL (SD 1.66; range from 5 to 15.3) in the Post-O group (p = 0.5). Twenty-four hours after surgery, the Hb was 9.21 mg/dl (SD 1.28; range from 5.7 to 13.5) and 9.25 mg/dL (SD 1.17; range from 5.6 to 13.1), respectively (p = 0.7). Hb at discharge was 10.1 mg/dL (SD 0.82; range from 8.2 to 9.9) in the Pre-O group and 10.2 mg/dL (SD 0.8; range from 8.5 to 13.1) in the Post-O group (p = 0.3). In the Pre-O group, the lowest value of Hb is 1.9 days (SD 2.09; range from −7 to 9) after surgery with an average of 8.31 mg/dl (SD 0.94; range from 5.1 to 13.1); in the Post-O group, it is 1.54 days (SD 2.17; range from −12 to 13) later, with average values of 8.36 mg/dl (SD 1.02; range from 3.5 to 12.5). Again, there are no significant differences. The number of transfusions was 379 in the Pre-O group with a mean of 1.93 (SD 1.45; range from 0 to 8) transfusions per patient; 393 in the Post-O group with 1.87 (SD 1.56; range from 0 to 8) transfusions per patient (p = 0.7).
Hb and transfusions: HHA
The data related to patients who underwent hemiarthroplasty (HHA) are reported in Table 4. The Pre-O group includes 90 patients with a mean age of 83.8 years (SD 7.2; range from 65 to 96); the Post-O group included 97 patients with a mean age of 82.5 years (SD 7.96; range from 55 to 99) (p = 0.2). Hb at admission was 12.36 mg/dL (SD 1.85; range from 8 to 16.2) in the Pre-O group and 12.61 mg/dL (SD 1.56; range from 8.8 to 18.2) in the Post-O group (p = 0.31). Twenty-four hours after surgery, the Hb did not differ significantly between the two groups (p = 0.1). In these patients, the Hb at discharge differs significantly in the two groups (p = 0.0001), 9.96 mg/dL (SD 0.82; range from 8.6 to 9.4) in the Pre-O group and 10.43 mg/dL (SD 0.8; range from 8.9 to 12.9) in the Post-O group. In the Pre-O group, the lowest peak of Hb is 8.39 mg/dl (SD 0.97; range from 6 to 11.5), reached 2.43 days (SD 1.84; range from −7 to 9) after surgery, while in the Post-O group is 8.62 mg/dl (SD 0.9; range from 6.5 to 10.9), 2.71 days (SD 1.92; range from −5 to 11) after surgery. A further significant difference is the average number of transfusions per patient (p = 0.03). Indeed, 153 transfusions were performed in the Pre-O group with an average of 1.7 (SD 1.31; range from 0 to 6) transfusions per patient; in the Post-O group 127 transfusions were performed with an average of 1.31 (SD 1.13; range from 0 to 6) transfusions per patient. In these patients, the LOS and the pre-surgery days do not differ, while in the Pre-O group, the time between surgery and discharge is significantly reduced (p = 0.008).
Hb and transfusion: THA
In patients undergoing THA, there are no significant differences between the two groups (Table 5). The Pre-O group includes 8 patients with a mean age of 74 years (SD 7.38; range from 63 to 87); the Post-O group comprises 17 patients with an average age of 72 years (SD 9.5; range from 53 to 93) (p = 0.6). Hb on admission was 13.52 mg/dL (SD 0.94; range from 11.5 to 14.7) in the Pre-O group; 12.94 mg/dL (SD 1.68; range from 10.3 to 15.8) in the Post-O group (p = 0.37). Twenty-four hours after THA, Hb was 10.62 mg/dL (SD 0.61; range from 10 to 11.6) and 10.16 mg/dL (SD 1.35; range from 7.8 to 12.6), respectively (p = 0.4). On discharge, the values were 10.23 mg/dl (SD 0.68; range from 9.5 to 11.8) for the Pre-O group and 10.36 mg/dl (SD 1.37; range from 8.7 to 14.5) with for the Post-O group. The lowest level of Hb was 3.17 days (SD 1.6; range from 2 to 6) after surgery, with 8.57 mg/dL (SD 0.58; range from 7.7 to 9.3) in the Pre-O group; and after 2.87 days (SD 1.75; range from 0 to 11) with 8.1 mg/dL (SD 0.86; range from 6.4 to 9.7) in the Post-O group (p = 0.7). The patients of the Pre-O group received a total of 9 transfusions, 1.12 (SD 0.64; range from 0 to 2) transfusions per patient; 31 transfusion were performed in the Post-O group, 1.82 (SD 1.42; range from 0 to 5) transfusions per patient (p = 0.12).
Discussion
A significant health care burden is related to the management of elderly patients with hip fractures [31,32,33]. Indeed, the incidence of hip fractures, as well as the incidence of all age-related fractures, is progressively increasing given the increase of life expectancy [31, 33,34,35]. Treating the fracture is not enough, and a comprehensive management of the patient is needed. Multiple comorbidities in the elderly population are extremely common [36, 37]. Consequently, these patients take multi-therapies that need to be considered before administering further drugs [36, 37].
In elderly patients with a hip fracture, it is important to monitor blood loss; they are often anaemic, regardless of the fracture [38]. Anaemia may delay surgical treatment, resulting in further blood loss. In these patients, transfusions are needed. However, the threshold value of Hb to begin the transfusion is debated. Some studies report that, in such patients, transfusions are associated with an increased risk of post-surgical complications and long-term mortality [39]; others report a decreased rate of delirium and a faster post-surgical functional recovery [40,41,42]. In others still, no association between the number of transfusions and the risk of mortality is recognised [43]. Some studies proposed a threshold value of Hb < 7 mg/dL as a trigger for transfusions in hemodynamically stable patients [44]. However, elderly patients with hip fractures often have different comorbidities, especially cardiovascular; in addition, it must also be considered the age-related fragility of these patients, in whom the fracture can lead to rapid hemodynamic imbalance even if they may be initially stable. In the Orthopaedic Department of the San Giovanni di Dio e Ruggi d’Aragona Hospital of Salerno, patients are monitored every day to maintain Hb to adequate levels. Since February 1, 2018, an orthogeriatrician works in the Orthopaedic Department, to promote functional recovery, reducing pre- and post-surgical complications and both short- and long-term mortality of the patients, thus reducing LOS, re-hospitalisations and related costs [45, 46]. The present study assessed whether the presence of an orthogeriatrician affects the blood management and the number of transfusions in patients with hip fractures. Regardless of the surgical treatment performed, there are no significant differences related to Hb at admission and 24 h after surgery, and the number of transfusions per patient does not differ significantly despite the involvement of the orthogeriatrician.
However, Hb at discharge was significantly higher in the Post-O group (p = 0.003). This difference probably results from a more comprehensive management provided by the orthogeriatrician, which also allows a faster recovery of the values of the Hb. Analysing the data according to the surgical procedure performed, there are some differences. Indeed, there are no differences related to Hb levels and the number of transfusions in the patients treated with an intramedullary nail and with THA. Differently, in the patients undergoing HHA, Hb at discharge was significantly higher in the patients managed by the orthogeriatrician (p = 0.0001); in addition, in these patients, the number of transfusions per patient was reduced (p = 0.03), although the post-surgical LOS was increased (p = 0.008). Despite the lack of significant differences in the number of transfusions performed, the higher Hb value at discharge may have a significant impact. Low levels of Hb can increase the LOS and thus hospital-related costs. In addition, although the risk of morbidity and mortality may not be affected, higher values of Hb at discharge reduce the risk of re-admission [47]. This allows to prevent further costs related to both the hospitalisation and the need for transfusions in case of hemodynamic imbalance of patients, in particular those with associated cardiovascular diseases.
The strength of this study is related to a large number of patients included. The demographic characteristics of patients and comorbidities do not differ significantly, except for patients with heart failure, who presented less often in the Post-O period (p = 0.007). In addition, the surgical procedures were performed in both groups by the same surgical team; therefore, the experience of surgeons should not affect the outcomes. The limitations are related to the retrospective nature of the study. The included patients were at least ASA III, as assessed by a consultant anaesthetist with a special interest in hip fracture management in the elderly. The computerised data collection and retrieval system in our health care system does not allow us to dwell further in this field; this would have made it possible to define more precisely the work of the orthogeriatrician. Furthermore, no data are available on the patient after discharge, so it is not possible to assess the long-term outcomes of the two groups of patients.
Conclusion
The introduction of the orthogeriatrician in an orthopaedic ward in which elderly patients are treated for hip fracture does not significantly change the number of transfusions per patient performed during the LOS. However, it allows to discharge the patients with significantly higher Hb values. In patients undergoing HHA, in addition to the highest Hb at discharge, the number of average transfusions per patient is significantly reduced. The increased values of Hb at discharge and the decreased number of transfusions in patients undergoing HHA indicate the involvement of an orthogeriatrician in the management of elderly patients with hip fractures. Indeed, with a higher Hb at discharge, the risk of anemisation of patients is reduced; consequently, also the costs related to possible re-admission and further transfusions are reduced.
Availability of data and materials
This study does not contain any third materials.
Abbreviations
- HHA:
-
Hip hemiarthroplasty
- THA:
-
Total hip arthroplasty
- LOS:
-
Length of hospital stay
- Hb:
-
Haemoglobin
References
Koso RE, Sheets C, Richardson WJ, Galanos AN. Hip fracture in the elderly patients: a sentinel event. Am J Hosp Palliat Care. 2018;35(4):612–9. https://doi.org/10.1177/1049909117725057.
Aletto C, Aicale R, Pezzuti G, Bruno F, Maffulli N. Impact of an orthogeriatrician on length of stay of elderly patient with hip fracture. Osteoporos Int. 2020;31(11):2161–6. https://doi.org/10.1007/s00198-020-05510-0.
Ramponi DR, Kaufmann J, Drahnak G. Hip fractures. Adv Emerg Nurs J. 2018;40(1):8–15. https://doi.org/10.1097/TME.0000000000000180.
de Miguel AM, Roca Chacón O, Martínez-Alonso M, et al. Hip fracture in the elderly patient: prognostic factors for mortality and functional recovery at one year. Rev Espanola Geriatr Gerontol. 2018;53:247–54.
Magaziner J, Chiles N, Orwig D. Recovery after hip fracture: interventions and their timing to address deficits and desired outcomes--evidence from the Baltimore Hip Studies. Nestle Nutr Inst Workshop Ser. 2015;83:71–81. https://doi.org/10.1159/000382064.
Pareja Sierra T, Bartolomé Martín I, Rodríguez Solís J, et al. Predictive factors of hospital stay, mortality and functional recovery after surgery for hip fracture in elderly patients. Rev Espanola Cirugia Ortop Traumatol. 2017;61:427–35.
Glimcher MJ, Kenzora JE. The biology of osteonecrosis of the human femoral head and its clinical implications: II. The pathological changes in the femoral head as an organ and in the hip joint. Clin Orthop. 1979;139:283–312.
Koo K-H, Mont MA, Jones LC. Osteonecrosis. Berlin: Springer Berlin Heidelberg; 2014. https://doi.org/10.1007/978-3-642-35767-1.
Yamamoto T, DiCarlo EF, Bullough PG. The prevalence and clinicopathological appearance of extension of osteonecrosis in the femoral head. J Bone Joint Surg Br. 1999;81:328–32.
Mehlhoff T, Landon GC, Tullos HS. Total hip arthroplasty following failed internal fixation of hip fractures. Clin Orthop. 1991;269:32–7.
Pavelka T, Salášek M, Bárta P, Fridrich F, Džupa V. Avascular necrosis of femoral head and coxarthrosis progression after acetabular fractures. Acta Chir Orthop Traumatol Cech. 2019;86(6):381–9.
Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82(5):679–83. https://doi.org/10.1302/0301-620X.82B5.0820679.
Meunier A, Maczynski A, Asgassou S, Baulot E, Manckoundia P, Martz P. Mortality and functional independence one year after hip fracture surgery: extracapsular fracture versus intracapsular fracture. Geriatr Psychol Neuropsychiatr Vieil. 2019;17(2):153–62. https://doi.org/10.1684/pnv.2018.0769.
Butt FF, Hussain AS, Khan AM, Sultan M. Implants for extracapsular neck of femur fracture dynamic hip screw versus intramedullary nailing. J Ayub Med Coll Abbottabad. 2017;29(4):697–701.
Hershkovitz A, Brill S, Sulam LN, Luria T, Heller S. Stability of extracapsular hip fracture: does it affect rehabilitation outcome of post-acute patients? Injury. 2018;49(7):1313–8. https://doi.org/10.1016/j.injury.2018.05.023.
Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2018;19(1):369. https://doi.org/10.1186/s12891-018-2276-3.
Crilly RG, Kloseck M, Chesworth B, Mequanint S, Sadowski E, Gilliland J. Comparison of hip fracture and osteoporosis medication prescription rates across Canadian provinces. Osteoporos Int. 2014;25(1):205–10. https://doi.org/10.1007/s00198-013-2453-z.
Nogués X, Martinez-Laguna D. Update on osteoporosis treatment. Med Clin (Barc). 2018;150(12):479–86. https://doi.org/10.1016/j.medcli.2017.10.019.
Black DM, Geiger EJ, Eastell R, Vittinghoff E, Li BH, Ryan DS, et al. Atypical femur fracture risk versus fragility fracture prevention with bisphosphonates. N Engl J Med. 2020;383(8):743–53. https://doi.org/10.1056/NEJMoa1916525.
Vandenbroucke A, Luyten FP, Flamaing J, Gielen E. Pharmacological treatment of osteoporosis in the oldest old. Clin Interv Aging. 2017;12:1065–77. https://doi.org/10.2147/CIA.S131023.
Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer A, et al. Risk of subsequent fracture after prior fracture among older women. Osteoporos Int. 2019;30(1):79–92. https://doi.org/10.1007/s00198-018-4732-1.
Kanis JA, McCloskey EV, Johansson H, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2013;24(1):23–57. https://doi.org/10.1007/s00198-012-2074-y.
Black DM, Rosen CJ. Clinical practice. Postmenopausal Osteoporosis. N Engl J Med. 2016;374(3):254–62. https://doi.org/10.1056/NEJMcp1513724.
von Friesendorff M, McGuigan FE, Wizert A, et al. Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int. 2016;27(10):2945–53. https://doi.org/10.1007/s00198-016-3616-5.
Guzon-Illescas O, Perez Fernandez E, Crespí Villarias N, Quirós Donate FJ, Peña M, Alonso-Blas C, et al. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg. 2019;14(1):203. https://doi.org/10.1186/s13018-019-1226-6.
Katsoulis M, Benetou V, Karapetyan T, Feskanich D, Grodstein F, Pettersson-Kymmer U, et al. Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med. 2017;281(3):300–10. https://doi.org/10.1111/joim.12586.
Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos D, Elmans L, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421–30. https://doi.org/10.2147/CIA.S115945.
Sim YE, Sim S-ED, Seng C, Howe TS, Koh SB, Abdullah HR. Preoperative anemia, functional outcomes, and quality of life after hip fracture surgery. J Am Geriatr Soc. 2018;66(8):1524–31. https://doi.org/10.1111/jgs.15428.
Pareja Sierra T, Bartolome Martín I, Rodríguez Solis J, Morales Sanz MD, Torralba Gonzalez de Suso M, Barcena Goitiandia LÁ, et al. Results of an anaemia treatment protocol complementary to blood transfusion in elderly patients with hip fracture. Rev Espanola Geriatr Gerontol. 2019;54(5):272–9. https://doi.org/10.1016/j.regg.2019.05.003.
Iliopoulos E, Yousaf S, Watters H, Khaleel A. Hospital stay and blood transfusion in elderly patients with hip fractures. J Perioper Pract. 2017;27(12):288–91. https://doi.org/10.1177/175045891702701203.
Hernlund E, Svedbom A, Ivergård M, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8:136.
Kelly M, Kates SL. Geriatric fracture centers-improved patient care and economic benefits : English Version. Unfallchirurg. 2017;120(S1):1–4. https://doi.org/10.1007/s00113-015-0092-x.
Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):131–7. https://doi.org/10.5435/JAAOS-D-14-00432.
Collin PG, D’Antoni AV, Loukas M, et al. Hip fractures in the elderly: a clinical anatomy review. Clin Anat. 2017;30(1):89–97. https://doi.org/10.1002/ca.22779.
Kanis JA. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int. 1994;4(6):368–81. https://doi.org/10.1007/BF01622200.
Roche JJW, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. https://doi.org/10.1136/bmj.38643.663843.55.
Wei J, Zeng L, Li S, Luo F, Xiang Z, Ding Q. Relationship between comorbidities and treatment decision-making in elderly hip fracture patients. Aging Clin Exp Res. 2019;31(12):1735–41. https://doi.org/10.1007/s40520-019-01134-5.
Sim YE, Wee HE, Ang AL, Ranjakunalan N, Ong BC, Abdullah HR. Prevalence of preoperative anemia, abnormal mean corpuscular volume and red cell distribution width among surgical patients in Singapore, and their influence on one year mortality. PloS One. 2017;12(8):e0182543. https://doi.org/10.1371/journal.pone.0182543.
Engoren M, Mitchell E, Perring P, Sferra J. The effect of erythrocyte blood transfusions on survival after surgery for hip fracture. J Trauma. 2008;65(6):1411–5. https://doi.org/10.1097/TA.0b013e318157d9f9.
Johnston P, Wynn-Jones H, Chakravarty D, Boyle A, Parker MJ. Is perioperative blood transfusion a risk factor for mortality or infection after hip fracture? J Orthop Trauma. 2006;20(10):675–9. https://doi.org/10.1097/01.bot.0000249435.25751.e8.
Carson JL, Duff A, Berlin JA, Lawrence VA, Poses RM, Huber EC, et al. Perioperative blood transfusion and postoperative mortality. JAMA. 1998;279(3):199–205. https://doi.org/10.1001/jama.279.3.199.
Blandfort S, Gregersen M, Borris LC, Damsgaard EM. Blood transfusion strategy and risk of postoperative delirium in nursing homes residents with hip fracture. A post hoc analysis based on the TRIFE randomized controlled trial. Aging Clin Exp Res. 2017;29(3):459–66. https://doi.org/10.1007/s40520-016-0587-5.
Potter LJ, Doleman B, Moppett IK. A systematic review of pre-operative anaemia and blood transfusion in patients with fractured hips. Anaesthesia. 2015;70(4):483–500. https://doi.org/10.1111/anae.12978.
Amin RM, DeMario VM, Best MJ, et al. A restrictive hemoglobin transfusion threshold of less than 7 g/dL decreases blood utilization without compromising outcomes in patients with hip fractures. J Am Acad Orthop Surg. 2019;27(23):887–94. https://doi.org/10.5435/JAAOS-D-18-00374.
Pioli G, Giusti A, Barone A. Orthogeriatric care for the elderly with hip fractures: where are we? Aging Clin Exp Res. 2008;20(2):113–22. https://doi.org/10.1007/BF03324757.
Friedman SM, Mendelson DA, Kates SL, McCann RM. Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc. 2008;56(7):1349–56. https://doi.org/10.1111/j.1532-5415.2008.01770.x.
Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J, et al. Effects of blood transfusion on clinical and functional outcomes in patients with hip fracture. Transfusion. 2003;43(10):1358–65. https://doi.org/10.1046/j.1537-2995.2003.00527.x.
Acknowledgements
None.
Funding
No external source of funding was used. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
MQ and LM: the conception and design of the study, acquisition of data, and analysis and interpretation of the data. FO: drafting the article and revising it critically for important intellectual content. FM and NM: final approval of the version to be submitted. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
All the authors approved the manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Quaranta, M., Miranda, L., Oliva, F. et al. Haemoglobin and transfusions in elderly patients with hip fractures: the effect of a dedicated orthogeriatrician. J Orthop Surg Res 16, 387 (2021). https://doi.org/10.1186/s13018-021-02524-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-021-02524-0