Abstract
Background
The unilaterally extrapedicular approach is adopted increasingly to perform balloon kyphoplasty in treating osteoporotic lumbar fractures, which is intended to improve radiological and clinical efficacy. We compared the efficacy and safety of this method with a unilaterally transpedicular approach.
Methods
We conducted a single-center, randomized controlled trial enrolling participants with a one-level osteoporotic lumbar fracture in less than 1 month. Patients were randomly assigned to undergo kyphoplasty via either a unilaterally extrapedicular approach (treatment group) or a unilaterally transpedicular approach (control group). The primary outcome was the difference in change from baseline to 1 month in visual analog scale (VAS) scores between the two groups. Secondary outcome measures included vertebral height ratio, operation time, fluoroscopic times, hemoglobin loss, and cement leakage between groups. Data were analyzed by intention to treat principle.
Results
A total of 80 participants were assigned to the treatment group (n = 40) and control group (n = 40), with three and two patients lost to follow-up during 12 months in the two groups, respectively. At 1 month postoperatively, the treatment group showed a greater reduction in VAS score from baseline, compared with the control group (mean difference between groups = 0.63, 95%CI 0.19–1.06). There were no significant between-group differences in restoration in anterior, middle, and posterior vertebral body (P > 0.05). No significant differences were found in the rate of cement leakage and perioperative hemoglobin loss (P > 0.05).
Conclusion
Compared with balloon kyphoplasty via the unilaterally transpedicular approach in treating lumbar OVCFs, the unilaterally extrapedicular approach appears to be promising in achieving effective pain relief, adequate cement infusion, short operation time, less fluoroscopy exposure, and comparable risk of cement leakage and vessel injury. It is an alternative approach for lumbar OVCFs treated with kyphoplasty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Osteoporotic vertebral compression fractures (OVCFs) have become one of the most common fragility fractures in the elderly population [1]. Symptomatic OVCFs can result in substantial pain and eventuate in decreased quality of life [2]. Percutaneous cement augmentation procedure, consisting of vertebroplasty and kyphoplasty, has exhibited superiority in pain relief over conservative management [3]. The balloon kyphoplasty is more frequently performed due to the advantage of vertebral height restoration and a lower rate of cement leakage [4, 5]. For osteoporotic thoracic fractures, the approach to injecting polymethylmethacrylate (PMMA) has evolved from bilaterally transpedicular, to unilaterally transpedicular, and further to unilaterally extrapedicular route [6,7,8]. The unilaterally extrapedicular approach has proven superiority in short operation time, symmetrical cement distribution, and a lower rate of cement leakage [9,10,11]. In recent years, several studies have reported the application of a unilaterally extrapedicular approach in treating lumbar OVCFs [12,13,14]. However, there are few prospective studies on the comparison between unilaterally extrapedicular versus unilaterally transpedicular approaches. Thus, we conducted the present randomized controlled study, aiming to clarify the clinical efficacy and safety of this emerging approach to carrying out balloon kyphoplasty for lumbar OVCFs. We hypothesized that the unilaterally extrapedicular approach would yield better clinical efficacy with a comparable complication rate compared to the unilaterally transpedicular approach.
Methods
This randomized controlled trial was approved by the Institutional Review Board of the Chongqing Orthopedic Hospital of Traditional Chinese Medicine. Written informed consent was obtained from all participants involved in the present study.
Participants
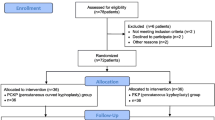
From May 2020 to May 2022 in a single institute, all patients with back pain within 1 month were screened for eligibility (Fig. 1). Magnetic resonance imaging (MRI) and dual-energy X-ray absorptiometry (DEXA) scans were performed to identify OVCFs. The presence of vertebral marrow edema on MRI imaging indicates an acute fracture. Only patients with one-level acute lumbar OVCF were included in this trial. The severity of osteoporosis was assessed by bone mineral density T score. Exclusion criteria were patients (1) with myeloma, osteoblastic metastases, or osteolytic metastatic tumors, (2) with a back pain score of fewer than 4 points on a 0–10 visual analog scale (VAS) scores, (3) with canal narrowing or radicular pain, (4) younger than 50 years old.
Interventions
Based on computer-generated random numbers, we randomly assigned enrolled patients to undergo unilateral balloon kyphoplasty either by an extrapedicular approach (treatment group) or a transpedicular approach (control group). Individuals were blinded to the assigned group throughout their hospital stay and follow-up. All surgical interventions were performed by the same surgeon aware of patient information and corresponding assignment.
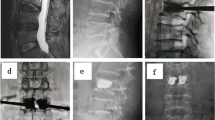
For the treatment group, the highlight of the extrapedicular approach was that the insertion site was located on the superolateral periosteum relative to the pedicle, which could provide a higher puncture angle on both the sagittal and horizontal plane (Fig. 2). The detailed procedures were as follows. Based on the preoperative MRI imaging, the insertion site and angle on the skin could be measured and noted (Fig. 2A, B). During the surgical procedure, patients were placed in the prone position on a radiolucent table. A C-arm or G-arm was placed on the contrary side to carry out intraoperative fluoroscopy. One or two metallic markers were used to identify the pedicle of the target vertebrae. Then, the puncture site and angle on the skin were marked with the usage of pre-measured data (Fig. 2C). After the infiltration with 1% lidocaine or 0.25% bupivacaine, a needle was inserted in the predesigned direction. It was essential to confirm the needle reached the correct periosteum under fluoroscopic guidance (Fig. 2D–G). After that, an inflatable bone tamp (IBT) was inserted inside the middle third of the vertebral body on both anterior–posterior and lateral images. The balloon was then inflated and the cement was injected slowly until satisfactory infiltration was achieved (Fig. 2H, I). Generally, the volume of cement was controlled up to 6 mL for each vertebra. The injection was also stopped if cement leakage occurred (e.g., extraosseous and spinal leakage).
Kyphoplasty by unilaterally extrapedicular approach. A On the axial MRI film, a indicates the distance between the spinous process and the puncture site. B On the sagittal MRI film, b indicates the distance between the puncture site and the line crossing pedicles. C The puncture site on skin based on preoperative MRI measurements. D, E the entry site is located on the superolateral periosteum relative to the pedicle. F, G, H, I the surgical procedure of kyphoplasty by the unilaterally extrapedicular approach
For the control group, all patients received unilaterally transpedicular balloon kyphoplasty. We did not allow conversion to bipedicular kyphoplasty even if the unilateral injection failed to achieve adequate instillation of cement, which could improve the comparability between groups. The surgical procedures were done according to standard practices of introducer instruments.
Following the surgery, all patients stayed in the hospital for 1–2 days and received ancillary care (e.g., osteoporosis drugs, back braces, analgesics, and physiotherapy) when necessary. A subsequent vertebral fracture was treated as the initial assignment.
Outcome assessment
Radiological assessment was done by a blinded radiologist while functional assessment was done by another blinded assessor. Baseline data included gender, age, body mass index (BMI), bone mineral density (BMD), the time from injury to surgery, affected lumbar level, vertebral body height ratio, and VAS scores. If injury time was uncertain, the onset of back pain was recorded. Vertebral height was presented as anterior, middle, and posterior vertebral body height ratios, which were measured on lateral radiographs. Assessment during operation involved operation time, fluoroscopic times, injected cement volume, and occurrence of cement leakage. The cement leakage was defined as leakage in any direction extraosseously. The hidden blood loss was evaluated as the reduction of perioperative hemoglobin value. Following the surgery, all patients underwent both functional (VAS scores) and radiological (anterior–posterior and lateral images) assessments at postoperative 1 day, 1, 3, 6, and 12 months of follow-up. If a participant failed to visit assessors in our hospital, telephone contact was carried out. Radiographs could be performed at local hospitals and sent to us via WeChat or Email. The intention to treat principle was used for missing data.
Statistical analysis
The primary endpoint was the difference in change from baseline to 1 month in VAS scores between the treatment and control groups. With the usage of PASS software, we calculated that per group would include at least 34 participants (90% power, 5% type 1 error rate, 1.24 standard deviation, a change of 1 point on VAS score). We used SAS software version 9.4 to conduct the statistical data analysis. Mixed effects modeling was used to analyze repeated measures (VAS scores and vertebral height ratio). The Chi-square test or Fisher’s exact test was used for categorical variables. Continuous data were tested for normality using the Shapiro–Wilk test. For data matching normal distribution, a two-sample t test was used to detect statistical differences between groups. The Mann–Whitney U test was used for continuous variables with non-normal distribution. The differences between groups were presented with 95% confidence intervals. A P value of < 0.05 was considered significant. We produced statistical figures with the use of GraphPad Prism software version 9.5.1.
Results
A total of 142 participants were assessed for eligibility. Finally, 80 patients were randomly allocated to the treatment group (n = 40) or control group (n = 40). At baseline, the characteristics between the two groups were similar (Table 1). From randomization to 12-month follow-up, 37 patients in the treatment group and 38 patients in the control group had complete data. A total of six patients encountered a second OVCF (three in each group) and received the same protocol as the initial assignment. All 80 participants were taken into the intention to treat analysis.
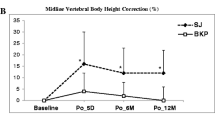
For the primary outcome, a significant interaction was detected between the intervention effect and follow-up time. The treatment group showed a greater reduction in the VAS score from baseline to 1 month, compared with the control group (adjusted MD = 0.63, 95%CI 0.19–1.06). At 1 day postoperatively, there were also significant differences in the VAS score reduction between groups (adjusted MD = 1.13, 95%CI 1.02–1.23). At 3, 6, and 12 months, no between-group differences were found in the VAS score reduction (Fig. 3).
Functional and radiological assessment during preoperation and 12-month follow-up (1 day, 1, 3, 6, and 12 months postoperatively). Means with 95% confidence intervals were presented. The first measurement in each figure indicates baseline data. A visual analog scale (VAS) scores. B, C, D anterior, middle, and posterior vertebral body height ratios (VBHR), indicating height loss of vertebral body, were measured on lateral radiographs
In the radiological assessment, no interaction was found significant between treatment and follow-up time (Fig. 3). There were no significant differences in anterior, middle, and posterior vertebral body height ratios between groups (all P > 0.05).
The treatment group exhibited shorter operation time of 2.85 min than the control group (95%CI 1.54–4.16, P < 0.001). More cement could be injected into the target vertebral body in the treatment group (MD = 5 ml, 95%CI 0.98–0.92, P < 0.001). Six and nine patients encountered cement leakage in the treatment group and control group, respectively. No significant associations were found between groups and the incidence of cement leakage (relative risk = 0.67, 95%CI 0.26–1.70, P > 0.05). There were no significant between-groups differences in hemoglobin loss (Table 2).
Discussion
The most important finding of the present randomized controlled trial was that in patients with lumbar OVCFs, balloon kyphoplasty by unilaterally extrapedicular approach could yield effective pain relief, adequate cement infusion, short operation time, less fluoroscopy exposure, and comparable risk of cement leakage and vessel injury, compared with the procedure by the unilaterally transpedicular approach.
The unilaterally extrapedicular approach for kyphoplasty has prevailed over the past years in treating thoracic OVCFs [6]. A myriad of studies has stated that both extrapedicular and transpedicular approaches are equally effective and safe in relieving pain for patients undergoing thoracic kyphoplasty [15,16,17]. In recent years, some attempts were made to use the unilaterally extrapedicular approach to perform kyphoplasty in treating lumbar OVCFs. Zhu et al. [14] retrospectively analyzed 76 lumbar OVCFs treated with the percutaneous kyphoplasty by either a bilateral transpedicular approach or unilateral extrapedicular approach. The results found that there were no between-group significant differences in both VAS and Oswestry Disability Index scores throughout a mean follow-up of 16.6 months. However, to our best knowledge, there were still no randomized controlled trials to compare the extrapedicular and transpedicular approach in performing unilateral kyphoplasty for lumbar OVCFs. In the current study, the treatment group showed a significantly greater reduction in the VAS score than the control group within 1 month of follow-up. However, the differences were no longer significant at 3, 6, and 12 months postoperatively. An explanation is that the extrapedicular approach could more easily access the center of the fractured vertebra and provide more symmetric cement filling than the transpedicular approach. This was possibly attributed to greater pain relief in the extrapedicular approach group. The finding of this study was consistent with prior evidence that symmetric cement infusion is more effective than asymmetric filling in pain relief [18]. Although there is still a lack of randomized controlled trials comparing the unilaterally extrapedicular approach with the bilaterally transpedicular approach in lumbar kyphoplasty, based on clinical practices; however, we believe that the two approaches are comparable to achieve symmetric cement infusion and pain relief. Another possible benefit of the extrapedicular approach in pain relief is the avoided injury of facet joint and capsule, which is reported to be associated with residual pain after transpedicular kyphoplasty [19].
The cement infiltration by the unilaterally extrapedicular approach brought out additional advantages over the transpedicular approach. In this study, compared to the control group, more cement was injected inside the target vertebral body in the treatment group. We deduce that the achievement of satisfactory cement infusion is highly associated with an advantageous puncture site and angle. In previous studies, several extrapedicular approaches have been proposed. Ryu et al. [20] proposed a far-lateral extrapedicular approach, by which the needle penetrated the transverse process with a puncture angle of 45 to 50 degrees on the horizontal plane. Cho et al. [21] introduced a personalized approach measured before surgery, in which the puncture was advanced superiorly to the upper edge of the transverse process. Wang et al. [22] suggested performing a puncture through Kambin’s triangle. The entry point was located at the junction between the pedicle and vertebral body. In the present study, we proposed a modified extrapedicular approach. Specifically, the insertion site and angle were based on the anatomical landmarks on radiographs preoperatively. In the surgical procedure, the needle tip reached the bottom of Kambin’s triangle at a puncture angle of 45 degrees from the sagittal plane. The puncture trajectory could easily access the center of the fractured vertebra. A single balloon was sufficient to produce symmetrical expansion and achievement of adequate return of kyphotic angle. In this trial, the majority of the unilaterally extrapedicular injection has produced similar cement infusion with traditional bilaterally transpedicular kyphoplasty. Moreover, although a mean of 4.83 ml cement was injected into a fractured lumbar vertebra, the risk of cement leakage did not differ between the extrapedicular and transpedicular approaches. The overall rate of cement leakage accounted for 15.0% (6/40), which coincided with prior studies [23, 24].
The most common concerns about the extrapedicular approach are puncture-related injuries involving segmental artery injury and nerve root lesions. Heo et al. [25] performed a spinal computed tomographic angiography and found that the segmental arteries predominantly passed below the midline of the pedicle. By the extrapedicular approach in the present study, the insertion site was located superior-laterally to the pedicle. The needle tip was controlled to slip on the periosteum and pass through the posterolateral lamina. Theoretically, the injury of segmental arteries could be avoided by this method. We calculated perioperative hemoglobin reduction to assess hidden blood loss. Between the extrapedicular and transpedicular approaches, no significant differences were found in perioperative hemoglobin loss. However, the definitive identification of retroperitoneal hematoma could be confirmed by an abdominal CT scan, especially for patients with hypovolemic shock and progressive hemoglobin loss after an extrapedicular kyphoplasty [8, 25]. Concerning the nerve root injury, which could be identified easily by the occurrence of radicular pain, both extrapedicular and transpedicular approaches in our study were proven to be equally safe in performing lumbar kyphoplasty.
As all kyphoplasty procedures in this study were carried out by an experienced surgeon, no significant clinical differences have been shown between the two approaches. Actually, the learning curve of the extrapedicular approach is much longer than that of the transpedicular approach for inexperienced practitioners. It will take more time and fluoroscopy to reach the optimal insertion point on the periosteum and verify the occurrence of malposition and cement leakage. As the experience begins to accumulate, the procedure of kyphoplasty by extrapedicular approach could be performed with much shorter time and less fluoroscopy exposure.
This study had several limitations. First, the surgeon involved in the surgical procedure was unblinded to participants, which may lead to performance bias. Second, there was no assessment of the quality of life (e.g., Roland-Morris disability questionnaire scores, short-form 36 physical component summary score), which may reach insufficient conclusions. Third, this study compared only unilaterally extrapedicular and transpedicular approaches. The clinical significance would be elevated if the bilaterally transpedicular approach could be taken into comparison.
Conclusions
The unilaterally extrapedicular approach appears to be a promising method to perform kyphoplasty for patients with lumbar OVCFs. It combines the advantages of unilaterally and bilaterally transpedicular approaches, with effective pain relief, adequate cement infusion, short operation time, less fluoroscopy exposure, and comparable risk of cement leakage and vessel injury. It is a viable option for carefully selected patients with lumbar OVCFs.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OVCFs:
-
Osteoporotic vertebral compression fractures
- VAS:
-
Visual analog scale
- PMMA:
-
Polymethylmethacrylate
- MRI:
-
Magnetic resonance imaging
- DEXA:
-
Dual-energy X-ray absorptiometry
- IBT:
-
Inflatable bone tamp
- BMI:
-
Body mass index
- BMD:
-
Bone mineral density
- VBHR:
-
Vertebral body height ratios
References
Ballane G, Cauley JA, Luckey MM, El-Hajj Fuleihan G. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017;28(5):1531–42.
Rodriguez AJ, Fink HA, Mirigian L, Guañabens N, Eastell R, Akesson K, Bauer DC, Ebeling PR. Pain, quality of life, and safety outcomes of kyphoplasty for vertebral compression fractures: report of a task force of the American Society for bone and mineral research. J Bone Miner Res. 2017;32(9):1935–44.
Wang B, Zhao CP, Song LX, Zhu L. Balloon kyphoplasty versus percutaneous vertebroplasty for osteoporotic vertebral compression fracture: a meta-analysis and systematic review. J Orthop Surg Res. 2018;13(1):264.
Clark W, Bird P, Gonski P, Diamond TH, Smerdely P, McNeil HP, Schlaphoff G, Bryant C, Barnes E, Gebski V. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016;388(10052):1408–16.
Evans AJ, Kip KE, Brinjikji W, Layton KF, Jensen ML, Gaughen JR, Kallmes DF. Randomized controlled trial of vertebroplasty versus kyphoplasty in the treatment of vertebral compression fractures. J Neurointerv Surg. 2016;8(7):756–63.
Ge J, Cheng X, Li P, Yang H, Zou J. The clinical effect of kyphoplasty using the extrapedicular approach in the treatment of thoracic osteoporotic vertebral compression fracture. World Neurosurg. 2019;131:e284–9.
Schupfner R, Koniarikova K, Pfeifer C, Grechenig P, Bakota B, Staresinic M, Kerner MA, Müller M. An anatomical study of transpedicular vs. extrapedicular approach for kyphoplasty and vertebroplasty in the thoracic spine. Injury. 2021;52(Suppl 5):S63-s69.
Zhu D, Hu JN, Wang L, Cui W, Zhu JC, Ma S, Tian BP, Liu BG. A modified unilateral extrapedicular approach applied to percutaneous kyphoplasty to treat lumbar osteoporotic vertebral compression fracture: a retrospective analysis. Pain Physician. 2023;26(3):E191-e201.
Chen W, Xie W, Xiao Z, Chen H, Jin D, Ding J. Incidence of cement leakage between unilateral and bilateral percutaneous vertebral augmentation for osteoporotic vertebral compression fractures: a meta-analysis of randomized controlled trials. World Neurosurg. 2019;122:342–8.
Sun H, Lu PP, Liu YJ, Yang X, Zhou PH, Shen XF, Sun SW, Yang H. Can unilateral kyphoplasty replace bilateral kyphoplasty in treatment of osteoporotic vertebral compression fractures? A systematic review and meta-analysis. Pain Physician. 2016;19(8):551–63.
Zhang W, Liu S, Liu X, Li X, Wang L, Wan Y. Unilateral percutaneous vertebroplasty for osteoporotic lumbar compression fractures: a comparative study between transverse process root-pedicle approach and conventional transpedicular approach. J Orthop Surg Res. 2021;16(1):73.
Qian Y, Li Y, Shen G, Zhong X, Tang C, He S. Comparison of unipedicular and bipedicular kyphoplasty for treating acute osteoporotic vertebral compression fractures in the lower lumbar spine: a retrospective study. BMC Musculoskelet Disord. 2023;24(1):410.
Zhang T, Deng Y. A design of a targeted puncture trajectory applied to unilateral extrapedicular percutaneous vertebroplasty. BMC Musculoskelet Disord. 2023;24(1):268.
Zhu D, Hu J, Wang L, Zhu J, Ma S, Liu B. A comparison between modified unilateral extrapedicular and bilateral transpedicular percutaneous kyphoplasty in the treatment of lumbar osteoporotic vertebral compression fracture. World Neurosurg. 2022;166:e99–108.
He H, Tan Y, Yang S, Zhang C, Luo X. Study of unilateral extrapedicular and bilateral pedicle approach percutaneous kyphoplasty for osteoporotic vertebral compression fracture. J Coll Phys Surg Pak. 2022;32(7):924–7.
Rebolledo BJ, Gladnick BP, Unnanuntana A, Nguyen JT, Kepler CK, Lane JM. Comparison of unipedicular and bipedicular balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures: a prospective randomised study. Bone Joint J. 2013;95-b(3):401–6.
Wang W, Duan K, Ma M, Jiang Y, Liu T, Liu J, Hao D. Can an unipedicular approach replace bipedicular percutaneous vertebroplasty for osteoporotic vertebral compression fracture? J Back Musculoskelet Rehabil. 2019;32(2):261–7.
Lv B, Ji P, Fan X, Yuan J, Xu T, Yao X, Huang A, Zou T. Clinical efficacy of different bone cement distribution patterns in percutaneous kyphoplasty: a retrospective study. Pain Physician. 2020;23(4):E409-e416.
Wang R, Xu Y, Ma X. Risk factors and strategies for recovery quality, postoperative pain, and recurrent fractures between percutaneous kyphoplasty and percutaneous vertebroplasty in elderly patients with thoracolumbar compression fractures: a retrospective comparative cohort study. Ann Transl Med. 2023;11(2):122.
Ryu KS, Park CK, Kim MK, Kim DH. Single balloon kyphoplasty using far-lateral extrapedicular approach: technical note and preliminary results. J Spinal Disord Tech. 2007;20(5):392–8.
Cho SM, Nam YS, Cho BM, Lee SY, Oh SM, Kim MK. Unilateral extrapedicular vertebroplasty and kyphoplasty in lumbar compression fractures : technique, anatomy and preliminary results. J Korean Neurosurg Soc. 2011;49(5):273–7.
Wang YF, Shen J, Li SY, Yu X, Zou TM. Kambin triangle approach in percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures. Medicine (Baltimore). 2019;98(44): e17857.
Palm HG, Riesner HJ, Lang P, Haentzsch M, Friemert B, Hackenbroch C. Diagnostic accuracy of fluoroscopy, radiography, and computed tomography in detecting cement leakage in kyphoplasty. J Neurol Surg A Cent Eur Neurosurg. 2018;79(6):502–10.
Zhan Y, Jiang J, Liao H, Tan H, Yang K. Risk factors for cement leakage after vertebroplasty or kyphoplasty: a meta-analysis of published evidence. World Neurosurg. 2017;101:633–42.
Heo DH, Cho YJ. Segmental artery injury following percutaneous vertebroplasty using extrapedicular approach. J Korean Neurosurg Soc. 2011;49(2):131–3.
Acknowledgements
Not applicable.
Funding
This research is supported by the Chongqing Yuzhong District Fundamental Research and Frontier Exploration Project (Grant No. 20210150).
Author information
Authors and Affiliations
Contributions
HH designed the study and wrote the article. JL, HD, YD, and QJ participated in the analysis of the data and contributed to the interpretation of results. HH and ZD are mainly responsible for this project. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
This randomized controlled trial was approved by the Institutional Review Board of the Chongqing Orthopedic Hospital of Traditional Chinese Medicine. All experiments were performed in accordance with the Declaration of Helsinki. All methods were carried out in accordance with relevant guidelines and regulations. Written informed consent was obtained from all participants involved in the present study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hong, H., Li, J., Ding, H. et al. Unilaterally extrapedicular versus transpedicular kyphoplasty in treating osteoporotic lumbar fractures: a randomized controlled study. J Orthop Surg Res 18, 801 (2023). https://doi.org/10.1186/s13018-023-04267-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04267-6