Abstract
Background
Surgical treatment of finger nerve injury is common for hand trauma. However, there are various surgical options with different functional outcomes. The aims of this study are to compare the outcomes of various finger nerve surgeries and to identify factors associated with the postsurgical outcomes via a systematic review and meta-analysis.
Methods
The literature related to digital nerve repairs were retrieved comprehensively by searching the online databases of PubMed from January 1, 1965, to August 31, 2021. Data extraction, assessment of bias risk and the quality evaluation were then performed. Meta-analysis was performed using the postoperative static 2-point discrimination (S2PD) value, moving 2-point discrimination (M2PD) value, and Semmes–Weinstein monofilament testing (SWMF) good rate, modified Highet classification of nerve recovery good rate. Statistical analysis was performed using the R (V.3.6.3) software. The random effects model was used for the analysis. A systematic review was also performed on the other influencing factors especially the type of injury and postoperative complications of digital nerve repair.
Results
Sixty-six studies with 2446 cases were included in this study. The polyglycolic acid conduit group has the best S2PD value (6.71 mm), while the neurorrhaphy group has the best M2PD value (4.91 mm). End-to-side coaptation has the highest modified Highet’s scoring (98%), and autologous nerve graft has the highest SWMF (91%). Age, the size of the gap, and the type of injury were factors that may affect recovery. The type of injury has an impact on the postoperative outcome of neurorrhaphy. Complications reported in the studies were mainly neuroma, cold sensitivity, paresthesia, postoperative infection, and pain.
Conclusion
Our study demonstrated that the results of surgical treatment of digital nerve injury are generally satisfactory; however, no nerve repair method has absolute advantages. When choosing a surgical approach to repair finger nerve injury, we must comprehensively consider various factors, especially the gap size of the nerve defect, and postoperative complications.
Type of study/level of evidence Therapeutic IV.
Similar content being viewed by others
Background
Finger nerve laceration is one of the most common injuries in hand trauma, and its incidence rate is high in the peripheral nerve injuries of the upper limbs [1]. Most hand injuries with nerve damage require surgical treatment [2]. Potential common complications from either surgical or non-surgical treatments include numbness, paresthesia, neuroma, and cold intolerance [3].
Finger nerve repair currently has two main surgical approaches. End-to-end tension-free neurorrhaphy has traditionally been the preferred repair method in lesions with a gap smaller than 5 mm [2]. When the nerve ends cannot be approximated without tension, nerve reconstruction becomes the most commonly used method. [4] Various materials are available for reconstruction, such as autograft, nerve autograft, nerve allograft, and artificial conduit. End-to-side anastomosis is also commonly used to reconstruct large nerve defects. The repair materials of autograft mainly include veins and muscle-in-vein [5]. The autologous nerve graft is the historical gold standard for nerve reconstruction [2]. However, the autologous nerve graft damages the patient’s own tissue, which can increase operative time for harvesting donor nerve and increase potential donor site morbidity [6]. With the improvement of technology and repair materials, nerve duct repair technology and allogeneic nerve repair technology are now available. These two techniques avoid donor site complications caused by autologous nerve transplantation [5]. Synthetic nerve conduits have polyglycolic acid (PGA) tubes and collagen tubes. However, potential complications of allogeneic transplantation include the transmission of infectious diseases [5]. For large-segment defects or proximal nerve damage, some scholars have tried the technique of end-to-side nerve anastomosis. This method can bridge the damaged nerve to the healthy nerve [7].
In addition to the surgical method that may affect the functional outcomes, other predictors of sensory recovery have been evaluated in several studies, such as mechanism of injury gender, age, involved digit, level of injury, time from injury till repair, and gap length. The main one is the type of injury, which can affect the severity of the nerve damage, the gap between the nerve defects, and the recovery after surgery. According to Kusuhara et al. [8], avulsion injuries had significantly lower levels of meaningful recovery when compared with those of clean-cut and crush types of injury. However, Schmauss et al.’s study [9] suggested that it did not observe significant differences in sharp versus crush injuries.
Few systematic reviews and meta-analyses have been conducted to compare surgical approaches and factors associated with sensory outcomes of digital nerve repair. [2, 3, 5, 10,11,12,13] In 2013 Paprottka et al.’s research, some of the included studies were low quality, and they did not compare allogeneic nerve repairs [5]. Herman et al. and Mauch et al.’s research in 2019 [8] included fewer studies and performed limited subgroups analyzed due to small sample size [2, 10]. Thus, we aimed to perform a comprehensive meta-analysis and systematic review of finger nerve repair to include high-quality studies with large sample sizes and conduct detailed subgroup analysis to compare different surgical approaches. We also aimed to identify factors associated with the functional outcomes of finger nerve repair.
Methods
We performed and reported this review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Search strategy and inclusion/exclusion criteria
We performed systematic literature search in PubMed. The search terms “digital nerve,” “operation,” “surgery,” “nerve injury,” “nerve repair,” were combined using Boolean operators. Both “free-text term” and “MeSH term” searches were completed. We did not impose any restrictions on the language. The publication date was set from January 1, 1965, to August 31, 2021, because the clinical implementation of the surgical microscope started around 1965. The previous surgeries without microscopes were not included in the study [14]. Additionally, we reviewed the reference lists of the included papers and previously published reviews to ensure relevant studies had been considered. We merged all search results and discarded duplicate citations [2, 3, 5, 10,11,12,13].
Two authors screened the articles independently based on the titles and abstracts, and each author independently retrieved and examined the full texts of the relevant papers for inclusion/exclusion based on predefined stratified criteria. Finally, we included all prospective and retrospective studies on surgical treatment of finger nerve injuries, including observational cohort studies, randomized controlled trials, and case reports with detailed data. We included patients of all ages with finger nerve injuries. The data published on the included studies were analyzed for the outcomes. We included results with at least 6-month follow-up. Exclusion criteria were peripheral nerve lesions not localized to the digital nerves in the hand, duplicated data, without appropriate data analysis methods, inconsistent data, reviews, unpublished literature, conference papers, studies without adequate information. The PRISMA flowchart is shown in Fig. 1.
Data extraction and outcome measures
The primary author extracted data onto a predefined electronic data extraction form, and then, the other author checked all the data. Any disagreements were resolved through discussion, if necessary, with the involvement of a third reviewer. We extract the following data from each included literature, the characteristics of the literature (author, nationality, research type, hospital, date), population characteristics (age, gender, sample size, number of lost follow-up, number of injured nerves, smoking, type of injury), damage and repair status (nerve gap, repair time, type of surgery, follow-up time), complications (postoperative neuroma, cold stimulation, paresthesia, postoperative infection, pain).
The outcome measurements we used included: static 2-point discrimination (S2PD), moving 2-point dis crimination (M2PD), Semmes–Weinstein monofilament testing (SWMF), and modified Highet classification of nerve recovery [3]. Weber first described S2PD in 1835 which was the most widely used outcome measure. Normal values of S2PD in an uninjured fingertip range from 2 to 6 mm. M2PD was described by Dellon, and we used it as the second outcome indicator to evaluate the recovery of the finger nerves after surgery. S2PD and M2PD use actual measurement distance to evaluate the degree of nerve recovery. They are both continuous variables. The shorter the measurement distance, the better the response.
We used a modified classification system derived from Imai et al. to group SWMF outcomes. The SWMF scores ≤ 2.83 mean “normal” for sensation, scores from 2.83 to 4.31 mean “diminished light touch,” scores from 4.31 to 4.56 mean “diminished protective sensation,” scores from 4.56 to 6.10 mean “loss of protective sensation,” and scores > 6.10 mean “anesthetic” [15]. We counted the number of people with a score less than 4.31 (full sensation and diminished light touch) to calculate the excellent rate for the degree of recovery.
Medical Research Council scoring system from 1954, modified by MacKinnon and Dellon often referred to as modified Highet, grouped a range of values into subjective headings [3]. This scoring system was often used to evaluate the recovery after nerve repair. The specific evaluation criteria are shown in Table 1. We extracted the sensory recovery as good and excellent nerve numbers in the table to evaluate the effect of the treatment.
In the S2PD and Highet data sets, there were many accounting articles, large amounts of data, and more detailed data. Therefore, we divided artificial catheters into two subgroups: collagen tubes and polyglycolic acid catheters. We divided venous catheters and muscle-in-vein grafts into groups in the autograft method. Direct suture and end-to-side anastomosis were split into two subgroups of neurorrhaphy for analysis. For these two data groups, we divided them into artificial conduit: polyglycolic acid, artificial conduit: collagen, nerve allograft, autograft repair: muscle-in-vein graft, autograft repair: vein graft, autologous nerve graft, end-to-end coaptation, end-to-side coaptation, total 8 repair types.
There were fewer articles in the M2PD and SWMF data sets, so the data we extracted were limited. When summarizing and analyzing the data, we did not conduct a detailed subgroup analysis but merged them into five repair Types for analysis. They were: artificial conduit (collagen tubes/polyglycolic acid catheters), nerve allograft, autograft repair (muscle-in-vein graft/vein graft), autologous nerve graft, and neurorrhaphy (end-to-end coaptation/end-to-side coaptation).
In addition, to evaluate the outcomes of the surgical repair methods, we also summarized and analyzed other factors associated with the result. These factors mainly included age, never gap, injury type, repair time, and smoking. Of course, the most important of these factors is the type of injury, which affects the degree of nerve damage, the choice of the surgical method, and postoperative recovery. We analyzed 25 articles [1, 7, 16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38] with specific injury descriptions through further screening of the included literature. We divided the injury types into sharp injury and crush injury. Sharp injuries include cutting injuries, acute or semi-sharp injuries, and stab injuries. Crush injuries include serious crush injuries, mangled injuries, and lacerated injuries. We analyzed patients with two types of injury in four types of surgery, and the analysis indexes were S2PD and modified Highet score excellent rate.
Complications reported in the studies were mainly neuroma, cold sensitivity, paresthesia, postoperative infection, and pain. We also conducted a summary analysis.
Statistical analysis, risk of bias, and study quality assessment
Our meta-analysis was performed by R (V.3.6.3) and package of meta. Heterogeneity variance parameter I2 test was used to assess the heterogeneity of the model. However, in order to reduce the difference between the parameters and avoid error of the results caused by heterogeneity, the random effects model was used to merge the statistics. For postoperative S2PD and M2PD of various surgical methods, we use a combined statistical analysis of mean and standard deviation. For the SWMF excellent rate and modified Highet score excellent rate, we adopted a combined statistical analysis of the rates. The results of the merger were displayed in a forest diagram, and the statistics were compared in the form of a table. We used funnel chart and egger test for publication bias. In the analysis by surgical method and injury type, the continuous variables of S2PD were compared by T test, and the excellent and good rates were compared using the chi-square test.
We used standardized critical appraisal instruments from the JBI Meta-Analysis of Statistics Assessment and Review Instrument (JBI-MAStARI) (Appendix II) to evaluate all included literature. Because all the included studies were case series or cohort studies, we used JBI Critical Appraisal Checklist for Descriptive/Case Series to evaluate the quality of the literature. This evaluation checklist includes 9 quality items, and the judging options include yes, no, unclear, and not applicable. Studies that blinded the evaluators and had “yes” scores of 80% were considered high quality; those with “yes” scores of 60–80% were rated as medium, and the quality of studies with a score of less than 60% was considered low. Any disagreements that arose between the reviewers were resolved through discussion.
Results
Study selection
We searched the PubMed database using keywords and got 403 different publications. At the same time, we examined the reference lists of the included papers and previous reviews to add 45 records. Sixty-six articles were included in the final data analysis [1, 7,8,9, 16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76, 86] (Fig. 1).
Study characteristics
The 66 articles included a total of 2446 cases. Fifty studies [1, 7, 16, 19, 21, 25,26,27,28,29,30,31,32,33,34,35,36,37,38,39, 41, 42, 45,46,47,48,49,50,51,52, 59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76, 86] were retrospective case series, and 16 [8, 9, 17, 18, 20, 22,23,24, 40, 43, 44, 53,54,55,56,57] were prospective. Of these studies, 16 control studies were available [20, 21, 28, 29, 38, 40,41,42, 53,54,55,56,57,58,59,60]. There were 3 papers that we only extracted part of the data because they included other nerve injuries in addition to the finger nerves [7, 32, 61]. The age range of patients included in these studies was 1–81 years old. The time from injury to surgical repair ranged between 0 and 37 months, and follow-up time ranged between 6 and 202 months. The detailed characteristics of eligible studies are shown in Table 2.
Quality assessment and publication bias
All 66 articles were evaluated for the quality assessment using the JBI-MAStARI evaluation tool, and the research evaluation levels were high or medium. The specific evaluation results are shown in Tables 2, 3 and 4. The P values derived from Egger’s test indicated their inexistence of the publication bias in most meta-analyses. The results of the Egger test are summarized in Tables 5, 6, 7, 8 and 9.
Synthesis of results
All the data extracted from the literature are shown in Table 2. The S2PD, Highet score, M2PD, and SWMF sensory results are summarized in Tables 5, 6, 7 and 8.
A total of 51 articles reported the S2PD data [8, 9, 16,17,18,19,20,21,22,23,24, 27,28,29,30,31, 35,36,37,38,39,40, 42, 44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71, 76, 86]. After a summary analysis, the polyglycolic acid conduit group was 6.71 mm (95% CI 4.46; 8.96), which was the smallest discrimination distance, the end-to-end coaptation group was 8.80 mm (95% CI 7.63; 9.97), and the postoperative discrimination distance was the largest. The values of the other groups were distributed between them, but they have yet to reach excellent (2–6 mm), just at the good level (7–15 mm) (Table 5, Figs. 2, 3).
Forest plot of static 2-point discrimination results for each repair technique. a Forest plot of S2PD—Artificial conduit: polyglycolic acid; b Forest plot of S2PD—Artificial conduit: collagen; c Forest plot of S2PD—nerve allografts; d Forest plot of S2PD—autograft repair: muscle-in-vein graft; e Forest plot of S2PD—autograft repair: vein graft; f Forest plot of S2PD—autologous nerve graft; g Forest plot of S2PD—end-to-end coaptation; and h Forest plot of S2PD—end-to-side coaptation
The excellent rate of modified Highet’s scoring includes 61 articles [1, 7,8,9, 16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39, 41, 43,44,45,46,47,48,49,50,51,52,53,54,55,56, 58,59,60,61,62, 64,65,66,67,68,69, 71,72,73,74,75,76, 86]. The end-to-side coaptation group was 98% (95% CI 0.85, 1.00), and the postoperative felt the excellent rate was the highest. The polyglycolic acid conduit group was 74% (95% CI 0.53; 0.91), and the excellent rate was the lowest (Table 6, Figs. 4, 5).
Forest plot of modified Highet classification good rate for each repair technique. a Forest plot of modified Highet classification good rate—Artificial conduit: polyglycolic acid; b Forest plot of modified Highet classification good rate—Artificial conduit: collagen; c Forest plot of modified Highet classification good rate—nerve allograft; d Forest plot of modified Highet classification good rate—autograft repair: muscle-in-vein graft; e Forest plot of modified Highet classification good rate—autograft repair: vein graft; f Forest plot of modified Highet classification good rate—autologous nerve graft; g Forest plot of modified Highet classification good rate—end-to-end coaptation; and h Forest plot of modified Highet classification good rate—end-to-side coaptation
The M2PD group included 19 articles [17, 20, 23, 24, 27, 28, 36, 37, 39,40,41, 45, 47, 50, 54, 57, 60, 68, 69]. The neurorrhaphy group was 4.91 mm (95% CI 3.72, 6.09), and the discrimination distance was the smallest; the autograft repair group was 7.06 mm (95% CI 5.58, 8.54), and the postoperative discrimination distance was the largest. The five data sets have yet to reach excellent (2–3 mm) but at a good level (4–7 mm) (Table 7, Figs. 6, 7).
There were 29 documents included in the SWMF data set [9, 16, 18,19,20, 22, 23, 25, 27,28,29,30, 36, 45,46,47, 49, 52, 53, 64,65,66,67,68,69,70,71, 73, 76, 86]. The highest excellent and good rate was 91% (95% CI 0.80, 0.99) in the autologous nerve graft group. The lowest was 61% (95% CI 0.40, 0.80) in the autograft repair group (Table 8, Figs. 8, 9).
Forest plot of Semmes–Weinstein monofilament testing good rate for each repair technique. a Forest plot of Semmes–Weinstein monofilament testing good rate—artificial conduit; b Forest plot of Semmes–Weinstein monofilament testing good rate—nerve allografts; c Forest plot of Semmes–Weinstein monofilament testing good rate—autograft repair; d Forest plot of Semmes–Weinstein monofilament testing good rate—autologous nerve graft; and e Forest plot of Semmes–Weinstein monofilament testing good rate—neurorrhaphy
Finally, we conducted a summary analysis of all the data in the 4 outcome indicators. S2PD was 8.18 mm (95% CI 7.66, 8.70), M2PD was 5.90 mm (95% CI 5.34, 6.46), Highet score excellent and good rate was 80% (95% CI 0.74, 0.86), and SWMF excellent and good rate was 81% (95% CI 0.72, 0.88) (Table 9, Figs. 10, 11, 12, 13).
We extracted data from 25 articles for statistical analysis in subgroups by injury type. In terms of S2PD values, there was no significant difference in sharp and blunt injuries among the four surgical methods (P > 0.05). In terms of the excellent and good rate, the recovery effect of sharp injury was better than that of blunt injury only in the surgical method of neurorrhaphy (P = 0.00004472), and there was no statistical difference in the other methods (Tables 12, 13).
We performed statistics on the analysis of other influencing factors in the included literature and completed a summary analysis of complications. In the study of influencing factors, in terms of age factor, 13 articles considered it to have an impact [1, 21, 32,33,34, 36, 55, 57, 60, 67, 72,73,74], and nine assumed it to have no effect [9, 20, 43, 45, 63, 65, 66, 71, 75]. In terms of nerve injury interval, 11 papers were deemed to be influential [9, 21, 26, 40, 43, 44, 51, 52, 71, 72, 74], and five pieces that have no influence [20, 32, 60, 65, 67]; four articles were considered to be compelling, [8, 27, 52, 60], and ten articles were considered to be unaffected by the repair time factor [9, 32, 35, 43, 63, 65, 66, 71, 73, 75]; in terms of smoking factors, three papers were supposed to be affected [33, 40, 73], and four pieces were not affected [9, 43, 45, 63] (Table 10).
The results of the pooled analysis of complications are shown that there were 12 articles of the literature reporting neuroma [21, 29, 32, 38, 44, 47, 56, 57, 62,63,64, 68], and 14 cases can be counted (artificial conduit: 2 articles, 3 cases; autograft repair: 7 articles, 7 cases; and nerve sutures: 3 articles, 4 cases); 13 publications reporting cold stimulation [27, 29, 30, 32, 37, 38, 49, 58, 63, 67,68,69,70], and 50 cases were counted (autograft repair: 10 articles, 47 cases; nerve sutures: 3 articles, 3 cases); 17 papers reporting paresthesia [1, 9, 21, 27, 29, 30, 32, 33, 38, 44, 49, 62, 63, 65, 67, 71, 76], and 15 cases were counted (artificial conduit: 3 articles, 1 case; autograft repair:11 articles,14 cases; and nerve sutures: 3 articles); 6 articles reporting postoperative infections [20, 21, 40, 45, 53, 69], and 10 cases were counted (artificial conduit: 3 articles, 5 cases; nerve allograft: 2 articles, 4 cases; autograft repair: 1 articles, 1 case); 13 articles reported pain [20, 21, 23, 29, 37,38,39, 49, 50, 53, 58, 67, 70], and 23 cases were counted (artificial conduit: 2 articles, 1 cases; nerve allograft: 3 articles, 9 cases; autograft repair: 6 articles, 12 cases; and nerve sutures: 2 articles, 1 cases) (Table 10).
We analyzed the maximum extent of neurological defects treated by various surgical methods in the literature. The direct suture is the minimum tension-free suture required to repair the defect within 0.5 cm. The largest defect was repaired by autogenous nerve graft, ranging from 0.5 to 9.0 cm. The end-to-side anastomosis technique had no limitation on the length of the defect and was a method of nerve transplantation or bridging (Table 11).
Discussion
It has been reported that among all peripheral nerve injuries, the digital nerves were the most common peripheral nerves injured [77]. In the published literature, there were many ways to repair digital nerve injury. However, the clinical practice of digital nerve repair has been lack of consensus. Thus, we analyzed the published literature on finger nerve injury .
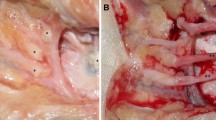
Using the S2PD and modified Highet’s scoring systems, tension-free end-to-end coaptation was the most common method for nerve repair. We found that compared with the other nerve defect repair methods, it seemed that there was no obvious advantage. Autologous nerve transplantation also showed no absolute advantage. As a new material to repair nerve defects, allogeneic nerves have been widely used. Compared with the autologous nerves, it has no obvious advantages. However, it can avoid other postoperative complications caused by nerve extraction and has the same effect as autologous nerve in nerve regeneration. There were some differences between PGA tubes and collagen tubes. In 2003, Laroas et al. published their results on 28 PGA-conduit repairs that with sensory re-education, the success rate could be increased to 100% [78]. In 2007, Waitayawinyu et al. study found better results with collagen conduits than with PGA conduits [79]. Our statistical results showed that there was no significant difference between the two catheters. Vein graft and muscle-in-vein graft as autografts also needed to be obtained from the donor site, but they were not as damaging to the donor site as autologous nerves. The two surgical methods had equivalent results, and there was no absolute advantage when compared with other methods. For large-segment defects or proximal nerve damage, the end-to-side anastomosis technique was an effective method. Its excellent rate was the highest among the 8 methods. Experimental end-to-side nerve suture was first introduced by Kennedy [80], but somehow it was not widely used clinically then. Viterbo et al., the creators of the modern approach of end-to-side neurorrhaphy without harming the donor’s nerve, something that broke paradigm, against all acknowledges, conducted their research by rats, in which they had the peroneal nerve sectioned, the distal ending sutured to the lateral face of the tibial nerve after removing a small epineural window, demonstrating that the anastomosed nerve endings had electrophysiological functions and successfully proving that the end-to-side nerve anastomosis technique was feasible [81,82,83]. Mennen first reported the use of this technique in humans in 1996 with good results [84]. In the 2003 literature, Mennen reported 56 cases of end-to-side anastomosis, including 5 cases of digital nerve repair, with a good level of neurological functional recovery [7]. Since then, four other scholars have reported related studies, but the number of cases they reported was very small. Recently, new techniques and materials have been used as variants for end-to-side coaptation; however, Geuna S et al. proposed that the bioactive materials as conduits or gene therapy, the role of Schwann cells, and attracting factors derived from the severed trunk should be on the way with further studies [85]. As a new surgical method of nerve repair, there are few studies on the repair of digital nerve. A total of 5 articles [7, 37, 64, 70, 86] and 49 cases were included in our study, and some data could not be extracted. Thus, there may be publication bias.
The data on the excellent rate of SWMF and M2PD of the autograft (muscle-in-vein graft/vein graft) were the worst. These 2 techniques have disadvantages for longer distances such as the collapse of the vein or dispersion of the regenerating axons out of the muscle [47]. We found that none of these methods had significantly different results. Our results were similar as shown in the meta-analysis performed by [11,12,13].
Through a summary analysis of all the data in the 4 outcome measures, we found that most patients had a good recovery after nerve injury repair. According to the modified Highet classification of nerve recovery, both S2PD and M2PD achieved S3 + or better. The Highet score and SWMF excellent and good rate were all above 80% (Table 1). We found that surgical repair was significantly better than no repair. Our results are consistent with the study performed by Chow et al., which had the same conclusion. [56] In Chow’s literature, 2-year follow-up outcomes were compared between digital nerve repair and no repair. 90% of the 76 patients with nerve repair achieved S3 + or better at 2 years, compared with only 6% of the 36 patients with unrepaired digital nerves. On the other hand, the meta-analysis of Dunlop et al. found that there were little difference between repair and non-repair. The differences in conclusions may be due to different studies included in the analysis [3].
The surgical approach significantly impacts nerve injury and is a critical factor in surgical intervention. The mechanism of injury is another important factor that may affect the degree of damage, the length of nerve defect, the choice of the surgical method, and the outcome of postoperative recovery. Many scholars have researched this factor in the literature included in our study. Kusuhara et al.’s nine studies [8, 18, 21, 33, 43, 52, 60, 72, 74] suggested that the type of injury had an impact on postoperative neurological recovery. Schmauss et al.’s nine studies [1, 9, 34, 45, 57, 63, 66, 73, 75] reported that the type of injury did not affect nerve recovery. We also did a statistical analysis of the data for this factor; through further screening of the included literature, we analyzed 25 kinds of literature with specific injury descriptions. Regarding S2PD value, sharp injury recovered better than blunt injury after four types of surgery, but there was no apparent absolute advantage. In terms of the excellent and reasonable rate, sharp injury has apparent benefits in the recovery of blunt injury after neurorrhaphy, and there is no significant difference between the other three surgical methods. This should be related to the fact that blunt injury can lead to large nerve damage, so only conduit or nerve transplantation can be selected for treatment. After the damaged nerve segment is removed, the nerve stumps become healthy. At this time, there is no significant difference in the effect of the two injury mechanisms on the nerve. However, if the damaged nerve segment is not resected but directly anastomosed, the blunt injury of the nerve is unhealthy and will affect the postoperative recovery. Sharp injury has less damage to the nerve, and the recovery effect after neurorrhaphy is good, while the blunt injury is poor. Therefore, when dealing with blunt nerve injury, the damaged nerve segment should be removed, and the appropriate surgical method should be selected according to the length of the nerve defect.
There are other factors that may affect the postoperative recovery of neuroremediation. In the 5 studies included, it has been shown that age was a factor that affected nerve recovery, especially in children, whose recovery after nerve repair was better than that of adults and the elderly [1, 33, 34, 36, 74]. Repair time, smoking, and follow-up time may have little effect on the recovery after nerve repair. In 2015, a study by Fakin et al. found that the experience of the surgeon was also one of the predicting factors of the outcomes. The repair of the finger artery accompanying the finger nerve had little effect on the postoperative recovery, which was also concluded by Hohendorff et al. [63, 87] In 1985, Sullivan et al. and Murakami et al. found that the number of finger nerve repairs had no difference in the effect of restoration [35, 88]. In a 2016 study done by Bulut et al., it was found that the recovery after finger nerve injury repair was independent of gender and which finger [73]. In 1981, Young et al. compared simple epineurium repair versus perineurium repair, and there was no significant difference in the recovery [55]. In a 2016 study by Sladana et al., it was deemed necessary to use splints after nerve repair [72]. Thomas et al. found that the result of using a microscope was significantly better than using a magnifying glass [89].
Our analysis of the postoperative complications in the included literature found that neuroma, cold stimulation, paresthesia, and pain were the most reported after autograft surgeries. This may be due to the damage to the donor site and poor recovery of the recipient site after transplantation. For complications, the application of allogeneic nerves and nerve conduits was better than autograft.
Our analysis has shown that the length of the nerve defect would affect the postoperative recovery, as well as limit the choice of surgical methods. Of course, we must also consider other factors, such as complications, economic conditions, local hospital technology, repair materials, etc. When there were multiple options to choose from for the optimal repair gap, we had to consider clinical factors associated with recovery when making the decision. There were no significant differences in the outcomes of various surgical methods, and the surgeon should choose a reasonable treatment plan based on the clinical scenario.
There were several limitations of our study. First, the quality of our study is limited by the quality of the included studies, which were mostly case series (level 4 evidence). Second, the strength of our conclusions was limited by the heterogeneous and incomplete outcome data reported across the included studies, and publication bias for the individual studies analyzed. In addition, when analyzing the excellent rate of Highet score, not every study reported outcomes in the same manner. We were forced to use S2PD and M2PD classification systems to group the results into categories that were comparable across sensory outcomes.
Conclusions
Our study demonstrated that the results of surgical treatment of digital nerve injury are generally satisfactory; however, no nerve repair method has absolute advantages. When choosing a surgical method to repair finger nerve injury, we must comprehensively consider various factors, especially the type of injury, the gap size of the nerve defect, the injury to the patient’s donor site, postoperative complications, the patient’s economic conditions, and the medical level of the local hospital. Whenever tension-free nerve coaptation was possible, end-to-end nerve coaptation was still the method of choice. In the case of nerve defects, the advantages of nerve conduits and allogeneic nerves were relatively high. When the proximal nerve was damaged and could not be connected, the end-to-side anastomosis technique could be selected for bridging to repair. Simultaneously, age, the size of the gap, and the type of injury were also factors that may affect recovery. Certainly, in consideration of the limitations of the study, such as the low qualities, the high heterogeneous, incomplete outcome data reported, and publication bias for the individual studies, conclusions in our study should be interpreted with caution. Therefore, more high-quality randomized controlled studies were definitely needed in order to give a conclusive statement.
Availability of data and materials
This study included articles which are available via PubMed. All information analyzed in this study was collected in a data set, and this is available from the corresponding author on reasonable request.
Abbreviations
- S2PD:
-
Static 2-point discrimination
- M2PD:
-
Moving 2-point discrimination
- SWMF:
-
Semmes–Weinstein monofilament testing
- PGA:
-
Polyglycolic acid tubes
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- CI:
-
Confidence intervals
- JBI-MAStARI:
-
JBI Meta-Analysis of Statistics Assessment and Review Instrument
- JBI:
-
Australia’s Joanna Briggs Institute
References
Efstathopoulos D, Gerostathopoulos N, Misitzis D, Bouchlis G, Anagnostou S, Daoutis NK. Clinical assessment of primary digital nerve repair. Acta Orthop Scand Suppl. 1995;264:45–7.
Herman ZJ, Ilyas AM. Sensory outcomes in digital nerve repair techniques: an updated meta-analysis and systematic review. Hand. 2019;15(2):157–64.
Dunlop RLE, Wormald JCR, Jain A. Outcome of surgical repair of adult digital nerve injury: a systematic review. BMJ Open. 2019;9(3):e025443.
Griffin JW, Hogan MV, Chhabra AB, Deal DN. Peripheral nerve repair and reconstruction. J Bone Jt Surg Am. 2013;95(23):2144–51.
Paprottka FJ, Wolf P, Harder Y, Kern Y, Paprottka PM, Machens HG, Lohmeyer JA. Sensory recovery outcome after digital nerve repair in relation to different reconstructive techniques: meta-analysis and systematic review. Plast Surg Int. 2013;2013: 704589.
Staniforth P, Fisher TR. The effects of sural nerve excision in autogenous nerve grafting. Hand. 1978;10(2):187–90.
Mennen U. End-to-side nerve suture in clinical practice. Hand Surg Int J Devoted Hand Upper Limb Surg Relat Res J Asia-Pac Fed Soc Surg Hand. 2003;8(1):33–42.
Kusuhara H, Hirase Y, Isogai N, Sueyoshi Y. A clinical multi-center registry study on digital nerve repair using a biodegradable nerve conduit of PGA with external and internal collagen scaffolding. Microsurgery. 2019;39(5):395–9.
Schmauss D, Finck T, Liodaki E, Stang F, Megerle K, Machens HG, Lohmeyer JA. Is nerve regeneration after reconstruction with collagen nerve conduits terminated after 12 months? The long-term follow-up of two prospective clinical studies. J Reconstr Microsurg. 2014;30(8):561–8.
Mauch JT, Bae A, Shubinets V, Lin IC. A systematic review of sensory outcomes of digital nerve gap reconstruction with autograft, allograft, and conduit. Ann Plast Surg. 2019;82:S247–55.
Rinkel WD, Huisstede BM, van der Avoort DJ, Coert JH, Hovius SE. What is evidence based in the reconstruction of digital nerves? A systematic review. J Plast Reconstr Aesthet Surg. 2013;66(2):151–64.
Kim JS, Bonsu N-Y, Leland HA, Carey JN, Patel KM, Seruya M. A systematic review of prognostic factors for sensory recovery after digital nerve reconstruction. Ann Plast Surg. 2018;80:S311–6.
Mermans JF, Franssen BB, Serroyen J, Van der Hulst RR. Digital nerve injuries: a review of predictors of sensory recovery after microsurgical digital nerve repair. Hand (N Y). 2012;7(3):233–41.
Smith JW. Microsurgery of peripheral nerves. Plast Reconstr Surg. 1964;33:317–29.
Imai H, Tajima T, Natsuma Y. Interpretation of cutaneous pressure threshold (Semmes–Weinstein monofilament measurement) following median nerve repair and sensory reeducation in the adult. Microsurgery. 1989;10(2):142–4.
Bushnell BD, McWilliams AD, Whitener GB, Messer TM. Early clinical experience with collagen nerve tubes in digital nerve repair. J Hand Surg. 2008;33(7):1081–7.
Taras JS, Jacoby SM, Lincoski CJ. Reconstruction of digital nerves with collagen conduits. J Hand Surg Am. 2011;36(9):1441–6.
Arnaout A, Fontaine C, Chantelot C. Sensory recovery after primary repair of palmar digital nerves using a Revolnerv ((R)) collagen conduit: a prospective series of 27 cases. Chir Main. 2014;33(4):279–85.
Thomsen L, Bellemere P, Loubersac T, Gaisne E, Poirier P, Chaise F. Treatment by collagen conduit of painful post-traumatic neuromas of the sensitive digital nerve: a retrospective study of 10 cases. Chir Main. 2010;29(4):255–62.
Means KR, Rinker BD, Higgins JP, Payne SH, Merrell GA, Wilgis EFS. A multicenter, prospective, randomized, pilot study of outcomes for digital nerve repair in the hand using hollow conduit compared with processed allograft nerve. Hand. 2016;11(2):144–51.
Rbia N, Bulstra LF, Saffari TM, Hovius SER, Shin AY. Collagen nerve conduits and processed nerve allografts for the reconstruction of digital nerve gaps: a single-institution case series and review of the literature. World Neurosurg. 2019;127:e1176–84.
Guo Y, Chen G, Tian G, Tapia C. Sensory recovery following decellularized nerve allograft transplantation for digital nerve repair. J Plast Surg Hand Surg. 2013;47:1–3.
Taras JS, Amin N, Patel N, McCabe LA. Allograft reconstruction for digital nerve loss. J Hand Surg Am. 2013;38(10):1965–71.
Karabekmez FE, Duymaz A, Moran SL. Early clinical outcomes with the use of decellularized nerve allograft for repair of sensory defects within the hand. Hand (N Y). 2009;4(3):245–9.
Tos P, Battiston B, Ciclamini D, Geuna S, Artiaco S. Primary repair of crush nerve injuries by means of biological tubulization with muscle-vein-combined grafts. Microsurgery. 2012;32(5):358–63.
Risitano G, Cavallaro G, Merrino T, Coppolino S, Ruggeri F. Clinical results and thoughts on sensory nerve repair by autologous vein graft in emergency hand reconstruction. Chir Main. 2002;21(3):194–7.
Alligand-Perrin P, Rabarin F, Jeudy J, Cesari B, Saint-Cast Y, Fouque PA, Raimbeau G. Vein conduit associated with microsurgical suture for complete collateral digital nerve severance. Orthop Traumatol Surg Res. 2011;97(4 Suppl):S16-20.
Laveaux C, Pauchot J, Obert L, Choserot V, Tropet Y. Retrospective monocentric comparative evaluation by sifting of vein grafts versus nerve grafts in palmar digital nerves defects. Report of 32 cases. Ann Chir Plast Esthet. 2010;55(1):19–34.
Chen C, Tang P, Zhang X. Reconstruction of proper digital nerve defects in the thumb using a pedicle nerve graft. Plast Reconstr Surg. 2012;130(5):1089–97.
Pilanci O, Ozel A, Basaran K, Celikdelen A, Berkoz O, Saydam FA, Kuvat SV. Is there a profit to use the lateral antebrachial cutaneous nerve as a graft source in digital nerve reconstruction? Microsurgery. 2014;34(5):367–71.
Inoue S, Ogino T, Tsutida H. Digital nerve grafting using the terminal branch of posterior interosseous nerve: a report of three cases. Hand Surg Int J Devot Hand Upper Limb Surg Relat Res J Asia-Pac Fed Soc Surg Hand. 2002;7(2):305–7.
Meek MF, Coert JH, Robinson PH. Poor results after nerve grafting in the upper extremity: Quo vadis? Microsurgery. 2005;25(5):396–402.
Al-Ghazal SK, McKiernan M, Khan K, McCann J. Results of clinical assessment after primary digital nerve repair. J Hand Surg (Edinburgh, Scotland). 1994;19(2):255–7.
Altissimi M, Mancini GB, Azzarà A. Results of primary repair of digital nerves. J Hand Surg (Edinburgh, Scotland). 1991;16(5):546–7.
Sullivan DJ. Results of digital neurorrhaphy in adults. J Hand Surg (Edinburgh, Scotland). 1985;10(1):41–4.
Segalman KA, Cook PA, Wang BH, Theisen L. Digital neurorrhaphy after the age of 60 years. J Reconstr Microsurg. 2001;17(2):85–8.
Voche P, Ouattara D. End-to-side neurorrhaphy for defects of palmar sensory digital nerves. Br J Plast Surg. 2005;58(2):239–44.
Pereira JH, Bowden RE, Gattuso JM, Norris RW. Comparison of results of repair of digital nerves by denatured muscle grafts and end-to-end sutures. J Hand Surg (Edinburgh, Scotland). 1991;16(5):519–23.
Mackinnon SE, Dellon AL. Clinical nerve reconstruction with a bioabsorbable polyglycolic acid tube. Plast Reconstr Surg. 1990;85(3):419–24.
Rinker B, Liau JY. A prospective randomized study comparing woven polyglycolic acid and autogenous vein conduits for reconstruction of digital nerve gaps. J Hand Surg. 2011;36(5):775–81.
Battiston B, Geuna S, Ferrero M, Tos P. Nerve repair by means of tubulization: literature review and personal clinical experience comparing biological and synthetic conduits for sensory nerve repair. Microsurgery. 2005;25(4):258–67.
Neubrech F, Heider S, Otte M, Hirche C, Kneser U, Kremer T. Nerve tubes for the repair of traumatic sensory nerve lesions of the hand: review and planning study for a randomised controlled multicentre trial. Handchir Mikrochir Plast Chir. 2016;48(3):148–54.
Lohmeyer JA, Kern Y, Schmauss D, Paprottka F, Stang F, Siemers F, Mailaender P, Machens HG. Prospective clinical study on digital nerve repair with collagen nerve conduits and review of literature. J Reconstr Microsurg. 2014;30(4):227–34.
Lohmeyer J, Zimmermann S, Sommer B, Machens HG, Lange T, Mailander P. Bridging peripheral nerve defects by means of nerve conduits. Chirurg. 2007;78(2):142–7.
Buncke G, Safa B, Thayer W, Greenberg J, Ingari J, Rinker B. Outcomes of short-gap sensory nerve injuries reconstructed with processed nerve allografts from a multicenter registry study. J Reconstr Microsurg. 2015;31(05):384–90.
Rinker B, Zoldos J, Weber RV, Ko J, Thayer W, Greenberg J, Leversedge FJ, Safa B, Buncke G: Use of Processed Nerve Allografts to Repair Nerve Injuries Greater Than 25 mm in the Hand. Ann Plast Surg 2017, 78(6S Suppl 5):S292-s295.
Marcoccio I, Vigasio A. Muscle-in-vein nerve guide for secondary reconstruction in digital nerve lesions. J Hand Surg Am. 2010;35(9):1418–26.
Norris RW, Glasby MA, Gattuso JM, Bowden RE. Peripheral nerve repair in humans using muscle autografts. A new technique. J Bone Jt Surg Br. 1988;70(4):530–3.
Laveaux C, Pauchot J, Obert L, Choserot V, Tropet Y. Emergency management of traumatic collateral palmar digital nerve defect inferior to 30 mm by venous grafting. Report on 12 clinical cases. Chir Main. 2011;30(1):16–9.
Lee Y-H, Shieh S-J. Secondary nerve reconstruction using vein conduit grafts for neglected digital nerve injuries. Microsurgery. 2008;28(6):436–40.
Tang JB, Gu YQ, Song YS. Repair of digital nerve defect with autogenous vein graft during flexor tendon surgery in zone 2. J Hand Surg (Edinburgh, Scotland). 1993;18(4):449–53.
Walton RL, Brown RE, Matory WE Jr, Borah GL, Dolph JL. Autogenous vein graft repair of digital nerve defects in the finger: a retrospective clinical study. Plast Reconstr Surg. 1989;84(6):944–9 (discussion 950–942).
He B, Zhu Q, Chai Y, Ding X, Tang J, Gu L, Xiang J, Yang Y, Zhu J, Liu X. Safety and efficacy evaluation of a human acellular nerve graft as a digital nerve scaffold: a prospective, multicentre controlled clinical trial. J Tissue Eng Regen Med. 2015;9(3):286–95.
Chiu DT, Strauch B. A prospective clinical evaluation of autogenous vein grafts used as a nerve conduit for distal sensory nerve defects of 3 cm or less. Plast Reconstr Surg. 1990;86(5):928–34.
Young L, Wray RC, Weeks PM. A randomized prospective comparison of fascicular and epineural digital nerve repairs. Plast Reconstr Surg. 1981;68(1):89–93.
Chow SP, Ng C. Can a divided digital nerve on one side of the finger be left unrepaired? J Hand Surg (Edinburgh, Scotland). 1993;18(5):629–30.
Calcagnotto GN, Braga Silva J. The treatment of digital nerve defects by the technique of vein conduit with nerve segment. A randomized prospective study. Chir Main. 2006;25(3–4):126–30.
Chen C, Tang P, Zhang X. Finger sensory reconstruction with transfer of the proper digital nerve dorsal branch. J Hand Surg. 2013;38(1):82–9.
Oruç M, Ozer K, Çolak Ö, Kankaya Y, Koçer U. Does crossover innervation really affect the clinical outcome? A comparison of outcome between unilateral and bilateral digital nerve repair. Neural Regen Res. 2016;11(9):1499–505.
Wang WZ, Crain GM, Baylis W, Tsai TM. Outcome of digital nerve injuries in adults. J Hand Surg Am. 1996;21(1):138–43.
Young VL, Wray RC, Weeks PM. The results of nerve grafting in the wrist and hand. Ann Plast Surg. 1980;5(3):212–5.
Stang F, Stollwerck P, Prommersberger KJ, van Schoonhoven J. Posterior interosseus nerve vs. medial cutaneous nerve of the forearm: differences in digital nerve reconstruction. Arch Orthop Trauma Surg. 2013;133(6):875–80.
Fakin RM, Calcagni M, Klein HJ, Giovanoli P. Long-term clinical outcome after epineural coaptation of digital nerves. J Hand Surg (Eur Vol). 2015;41(2):148–54.
Artiaco S, Tos P, Conforti LG, Geuna S, Battiston B. Termino-lateral nerve suture in lesions of the digital nerves: clinical experience and literature review. J Hand Surg Eur. 2010;35(2):109–14.
McFarlane RM, Mayer JR. Digital nerve grafts with the lateral antebrachial cutaneous nerve. J Hand Surg. 1976;1(3):169–73.
Poppen NK, McCarroll HR, Doyle JR, Niebauer JJ. Recovery of sensibility after suture of digital nerves. J Hand Surg. 1979;4(3):212–26.
Chevrollier J, Pedeutour B, Dap F, Dautel G. Evaluation of emergency nerve grafting for proper palmar digital nerve defects: a retrospective single centre study. Orthop Traumatol Surg Res. 2014;100(6):605–10.
Rose EH, Kowalski TA, Norris MS. The reversed venous arterialized nerve graft in digital nerve reconstruction across scarred beds. Plast Reconstr Surg. 1989;83(4):593–604.
Kim J, Lee YH, Kim MB, Lee SH, Baek GH. Innervated reverse digital artery island flap through bilateral neurorrhaphy using direct small branches of the proper digital nerve. Plast Reconstr Surg. 2015;135(6):1643–50.
Landwehrs GM, Brüser P. Clinical results of terminolateral neurorrhaphy in digital nerves. Handchir Mikrochir Plast Chir. 2008;40(5):318–21.
Unal MB, Gokkus K, Sirin E, Cansü E. Lateral antebrachial cutaneous nerve as a donor source for digital nerve grafting: a concept revisited. Open Orthop J. 2017;11(1):1041–8.
Andelkovic SZ, Lesic AR, Bumbasirevic MZ, Rasulic LG. The outcomes of 150 consecutive patients with digital nerve injuries treated in a single center. Turk Neurosurg. 2017;27(2):289–93.
Bulut T, Akgun U, Citlak A, Aslan C, Sener U, Sener M. Prognostic factors in sensory recovery after digital nerve repair. Acta Orthop Traumatol Turc. 2016;50(2):157–61.
Vahvanen V, Gripenberg L, Nuutinen P. Peripheral nerve injuries of the hand in children. A follow-up study of 38 patients. Scand J Plast Reconstr Surg. 1981;15(1):49–51.
Acar E, Turkmen F, Korucu IH, Karaduman M, Karalezli N. Outcomes of primary surgical repair of zone 2 dDigital nerve injury. Acta Orthop Belg. 2018;84(1):84–93.
Nunley JA, Ugino MR, Goldner RD, Regan N, Urbaniak JR. Use of the anterior branch of the medial antebrachial cutaneous nerve as a graft for the repair of defects of the digital nerve. J Bone Jt Surg Am. 1989;71(4):563–7.
Asplund M, Nilsson M, Jacobsson A, von Holst H. Incidence of traumatic peripheral nerve injuries and amputations in Sweden between 1998 and 2006. Neuroepidemiology. 2009;32(3):217–28.
Laroas G, Battiston B, Sard A, Ferrero M, Dellon AL. Digital nerve reconstruction with the bioabsorbable neurotube. Rivista Italiana di Chirurgia Plastica. 2003;35:125–8.
Waitayawinyu T, Parisi DM, Miller B, Luria S, Morton HJ, Chin SH, Trumble TE. A comparison of polyglycolic acid versus type 1 collagen bioabsorbable nerve conduits in a rat model: an alternative to autografting. J Hand Surg Am. 2007;32(10):1521–9.
Kennedy R. On the restoration of co-ordinated movements after nerve section. Proc R Soc Edinb. 1901;22:636–40.
Viterbo F, Trindade JC, Hoshino K, Mazzoni Neto A. Latero-terminal neurorrhaphy without removal of the epineural sheath. Experimental study in rats. Rev Paul Med. 1992;110(6):267–75.
Viterbo F, Trindade JC, Hoshino K, Mazzoni Neto A. End-to-side neurorrhaphy with removal of the epineurial sheath: an experimental study in rats. Plast Reconstr Surg. 1994;94(7):1038–47.
Viterbo F, Trindade JC, Hoshino K, Mazzoni A. Two end-to-side neurorrhaphies and nerve graft with removal of the epineural sheath: experimental study in rats. Br J Plast Surg. 1994;47(2):75–80.
Mennen U. End-to-side nerve suture in the human patient. Hand Surg. 1998;3(1):7–15.
Geuna S, Papalia I, Ronchi G, d’Alcontres FS, Natsis K, Papadopulos NA, Colonna MR. The reasons for end-to-side coaptation: How does lateral axon sprouting work? Neural Regen Res. 2017;12(4):529–33.
Li Q, Liu Z, Lu J, Shao W, Feng X. Transferring the ulnaris proper digital nerve of index finger and its dorsal branch to repair the thumb nerve avulsion. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31(8):992–5.
Hohendorff B, Staub L, Fritsche E, Wartburg U. Sensible Nervenfunktion nach unilateraler digitaler Gefäß-Nerven-Verletzung: Nervennaht mit und ohne Arterienanastomose. Handchir Mikrochir Plast Chir. 2009;41(05):306–11.
Murakami T, Ikuta Y, Tsuge K. Relationship between the number of digital nerves sutured and sensory recovery in replanted fingers. J Reconstr Microsurg. 1985;1(4):283–6.
Thomas PR, Saunders RJ, Means KR. Comparison of digital nerve sensory recovery after repair using loupe or operating microscope magnification. J Hand Surg Eur. 2015;40(6):608–13.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
XT and YZ contributed to conception and design of the study, literature search, data extraction, methodological quality assessment, writing, and final approval; and XT and KW were involved in literature search, data extraction, methodological quality assessment, analysis, interpretation of data, and final approval; NH and JZ contributed to revision and final approval, and BX, JL, and XC were involved in supervision and final approval. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Y., Hou, N., Zhang, J. et al. Treatment options for digital nerve injury: a systematic review and meta-analysis. J Orthop Surg Res 18, 675 (2023). https://doi.org/10.1186/s13018-023-04076-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04076-x