Abstract
Background
We compared the clinical efficacy of mini-open reduction and autologous bone grafting (GM) and closed reduction (GC) using intramedullary nailing for the treatment of tibial shaft fractures.
Methods
This retrospective study included 70 tibial shaft fractures treated with GM or GC between January 2018 and December 2021. The demographic characteristics and clinical outcomes were compared between the two treatment methods.
Results
This study included 70 patients who were followed-up for 12.4 months. In total, 31 and 39 patients were treated with GM and GC, respectively. The operative duration was significantly shorter for GM (95.2 ± 19.3 min) than for GC (105.5 ± 22.2 min, p = 0.0454). The number of radiation times was significantly lower for GM (14.7 ± 6.3) than for GC (22.2 ± 9.2, p < 0.005). There were no statistically significant differences between the groups in terms of the wound complication or infection rates. The malunion and nonunion rates were high after GC than after GM, but there are no significant differences between the groups.
Conclusions
Closed reduction and intramedullary nailing remains the first choice for tibial shaft fractures. GM is a safe and effective treatment worth considering. Future prospective randomized controlled trials are warranted.
Similar content being viewed by others
Introduction
Tibial fractures result from high- and low-energy trauma [1]. The aim of surgical treatment is to promote early postoperative weight-bearing and rehabilitation. The treatments for tibial fractures include intramedullary nailing (IMN), plating, and external fixation [2, 3]. Multiple studies have evaluated the safety and effectiveness of IMN, and have found that it promotes bone healing, early mobilization, and return to function. IMN is commonly performed and effective for the treatment of tibial fractures [4,5,6,7]. Tibial shaft fractures may be treated with IMN for internal fixation using limited open reduction of the fractured point [8, 9] and implanting a bone graft harvested from the opening point of the tibial tuberosity to the fractured end [10]. This method is associated with better reduction, fewer soft tissue operations and X-rays, shortened reduction time, and improved fracture healing rate compared to closed reduction. We retrospectively compared the outcomes of mini-open reduction and autologous bone grafting followed by IMN (GM) and closed reduction (GC) for the treatment of closed tibial fractures. We hypothesized that the former is associated with reduced operation time and improved fracture healing rate without an increased risk of complications.
Methods
Patients
This retrospective study enrolled patients with displaced closed fracture of the tibial shaft who were treated with IMN and presented for regular follow-up for ≥ 6 months or until fracture union between January 2018 and December 2021 at the Department of our hospital. Indications for open reduction include cases where a satisfactory closed reduction could not be achieved or when there is the presence of intramedullary cortical bone debris. Ethical approval was obtained from the Ethics Committee of our hospital. We excluded patients with open or pathological fractures, compartment syndrome, infection, or concomitant diseases. In total, 70 patients with tibial fractures were enrolled. The demographic characteristics of the study variables are presented in Table 1.
Surgical methods
The surgery was performed by a chief surgeon or associate chief surgeon.
Observation group (GM)
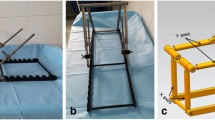
After anesthesia, the patient was placed in supine position on a fluoroscopic surgical bed and a balloon tourniquet was applied. A longitudinal incision 4–5 cm long was made below the patella. The patellar ligament was incised longitudinally, and the point of entry for the tibial IMN was determined. The tibial tuberosity was opened approximately 0.5 cm posteromedial to the tibial tuberosity using a bone awl, and free bone fragments were selected as the opening point (Fig. 1A). A small auxiliary incision of approximately 3–4 cm was made at the displaced end of the bone to reposition and fix the fractured segment using bone-holding forceps (Fig. 1B). After insertion of the guide wire and satisfactory fluoroscopic reduction, the medullary canal was reamed to collect a sample. The medullary canal was expanded to match the IMN diameter. The IMN was inserted from the proximal tibia to lock the distal and proximal ends of the bone. C-arm X-ray was performed to visualize the fracture site, screw length, and anatomical reduction. The harvested bone was grafted onto the fractured site (Fig. 1B). The incision was irrigated and closed in layers.
Control group (GC)
Conventional closed reduction and IMN was performed.
Postoperative management
Postoperative antibiotics were administered routinely for 24–48 h to prevent infection. The patients were advised to perform functional exercises from three days after the surgery.
Observational indices
We recorded the operative duration, radiation time, intraoperative blood loss, and postoperative complications, such as nonunion, infection, and malunion. Malunion is characterized by an excess of 5° of deviation in any plane, 15° of internal rotation, 20° of external rotation, a foreshortening exceeding 1 cm, or over 50% dislocation involving any fracture site.
Statistical analysis
Data were analyzed using SPSS software (version 22.0; IBM Corp., Armonk, NY, USA). Continuous variables are presented as means ± standard deviations and were analyzed using an independent samples t test. Qualitative data were analyzed using the Chi-square test. P < 0.05 was considered to be statistically significant.
Results
This study enrolled 70 patients with a mean age of 40.6 years; 31 were treated with GM and 39 were treated with GC. The patients were followed-up for 12.4 months. The characteristics of the study participants are presented in Table 1.
Surgical outcomes
The operative duration was significantly shorter for GM (95.2 ± 19.3 min) than for GC (105.5 ± 22.2 min, p = 0.0454). The number of radiation times were significantly lower for GM (14.7 ± 6.3) than for GC (22.2 ± 9.2, p < 0.005). The intraoperative blood losses were 46.8 ± 28.6 ml and 49.5 ± 25.2 ml in the GM and GC groups, respectively, with no significant differences between the groups (Table 2). Figure 2 shows postoperative X-rays in GM. A perfectly fracture reduction was achieved and the fracture was healing well.
Postoperative complications
No statistically significant differences were observed in the wound complication or infection rate between the groups. Malunion and nonunion were common in the GC group than in the GM group, but there are no significant differences between the groups (Table 3).
Discussion
We compared the safety and efficacy of GM and GC for the treatment of tibial shaft fractures. There were significant differences between the groups in terms of the operative duration and the number of radiation times. Besides low malunion and nonunion rates were found in GM, indicating favorable results of GM compared to GC.
Tibial fractures are common and have been treated using several different methods. Malunion, nonunion, and wound infection are common postoperative complications after the treatment of tibial fractures [11]. IMN is performed for most cases of tibial fractures because it is minimally invasive, avoids soft tissue stripping, causes less bleeding, and preserves the vascular supply [6, 7]. However, it is associated with a high rate of malunion [12]. During closed reduction, it is difficult to reestablish the appropriate tibial length, alignment, and rotation before inserting the guidewire, thereby necessitating frequent X-ray use. In addition, the soft tissues near the fracture site are damaged during multiple reduction attempts [13]. Several studies have evaluated the effectiveness of open reduction and IMN for the treatment of tibial shaft fractures. Bishop et al. [8] found that open reduction through a small incision with careful soft tissue manipulation was safe and effective. It was associated with high-quality reduction, which promoted fracture healing. There were no significant differences in the nonunion or infection rates between this technique and closed reduction. Our results are in line with a retrospective study [9] that found similar outcomes between open and closed reduction. Open reduction significantly reduces the operation time and improves patient satisfaction. The operation time and the number of radiation times were significantly shorter and lower with GM than with GC. There were no significant differences in the intraoperative blood loss between the two groups, which may be explained by the use of a tourniquet. GM was associated with improved fracture healing and low malunion rate.
Although most tibial shaft fractures are treated successfully, nonunion is a common complication because of small muscle tissue attached to the distal tibia and insufficient blood supply. The nonunion rate after tibial fractures is 5–17% [14,15,16]. Autologous bone grafting is the gold-standard treatment for nonunion [17]. IMN is associated with excessive removal of bone at the point of nail insertion during reaming. We collected the excess bone and implanted it onto the fracture site to promote fracture healing. Autologous bone grafting improves the local biological factors at the fracture site to promote healing. During GM, bone harvesting was convenient and required no additional incision or costs. Bone grafts are usually obtained from the iliac crest, which requires an additional procedure [18]. Other implants that promote fracture healing, such as bone morphogenetic proteins [19] and platelet-rich plasma [20], are associated with additional costs [21, 22]. However, GM overcomes these problems. The small incision at the fracture site allowed adequate fracture reduction and alignment, as well as bone grafting to promote fracture healing without the need for an additional procedure (Fig. 2). As a result, there is none nonunion after GM.
In the present study, we did not record fracture healing time as an outcome. Patients generally present for follow-up visits at almost 1 month postoperatively, which made it difficult to determine the fracture healing time accurately. To reduce the influence of confounding factors, we included patients with only closed fractures and excluded patients with open or pathological fractures, compartment syndrome, infection, or severe concomitant disease.
This study had several limitations. First, this was a retrospective study with a short follow-up duration. Second, we enrolled a small number of participants and did not evaluate their functional outcomes. Third, we excluded patients with open fractures. Therefore, it is unclear whether bone harvesting on open fracture sites reduce the risk of infection and other complications.
In conclusion, GM is safe and effective for the treatment of tibial shaft fracture. While closed reduction and intramedullary nailing continue to be the preferred approach for managing tibial shaft fractures, the utilization of mini-open reduction combined with autologous bone grafting may be taken into consideration when closed techniques are unsuccessful. Future prospective randomized controlled trials are warranted.
References
Larsen P, Elsoe R, Hansen SH, Graven-Nielsen T, Laessoe U, Rasmussen S. Incidence and epidemiology of tibial shaft fractures. Inj-Int J Care Inj. 2015;46:746–50. https://doi.org/10.1016/j.injury.2014.12.027.
Li Y, Jiang X, Guo Q, Zhu L, Ye T, Chen A. Treatment of distal tibial shaft fractures by three different surgical methods: a randomized, prospective study. Int Orthop. 2014;38:1261–7. https://doi.org/10.1007/s00264-014-2294-1.
Toivanen JAK, Honkonen SE, Koivisto AM, Jarvinen MJ. Treatment of low-energy tibial shaft fractures: plaster cast compared with intramedullary nailing. Int Orthop. 2001;25:110–3. https://doi.org/10.1007/s002640000083.
Lin ZQ, Zhang HZ, Luo GG, Yao JC, Xie HF, Zhang X, Zhu YZ. Comparison of 3 treatment methods for distal tibial fractures: a network meta-analysis. Med Sci Monit. 2019;25:7480–7. https://doi.org/10.12659/msm.917311.
Guo C, Ma J, Ma X, Wang Y, Sun L, Lu B, Tian A, Wang Y, Dong B. Comparing intramedullary nailing and plate fixation for treating distal tibail fractures: a meta-analysis of randomized controlled trials. Int J Surg. 2018;53:5–11. https://doi.org/10.1016/j.ijsu.2018.03.026.
Johal H, Bhandari M, Tornetta P III. Cochrane in CORR®: intramedullary nailing for tibial shaft fractures in adults (review). Clin Orthop Relat Res. 2017;475:585–91. https://doi.org/10.1007/s11999-016-5202-8.
Nork SE, Schwartz AK, Agel J, Holt SK, Schrick JL, Winquist RA. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Jt Surg-Am Vol. 2005;87A:1213–21. https://doi.org/10.2106/jbjs.c.01135.
Bishop JA, Dikos GD, Mickelson D, Barei DP. Open reduction and intramedullary nail fixation of closed tibial fractures. Orthopedics. 2012;35:E1631–4. https://doi.org/10.3928/01477447-20121023-21.
Auston DA, Meiss J, Serrano R, Sellers T, Carlson G, Hoggard T, Beebe M, Quade J, Watson D, Simpson RB, Kistler B, Shah A, Sanders R, Mir HR. Percutaneous or open reduction of closed tibial shaft fractures during intramedullary nailing does not increase wound complications, infection or nonunion rates. J Orthop Trauma. 2017;31:215–9. https://doi.org/10.1097/bot.0000000000000777.
Meiser S, Arora R, Petersen J, Keiler A, Liebensteiner MC, Pallua JD, Wurm A. Radiographic and clinical outcome of tibial plateau fractures treated with bone allograft. Arch Orthop Trauma Surg. 2022. https://doi.org/10.1007/s00402-022-04461-x.
Joveniaux P, Ohl X, Harisboure A, Berrichi A, Labatut L, Simon P, Mainard D, Vix N, Dehoux E. Distal tibia fractures: management and complications of 101 cases. Int Orthop. 2010;34:583–8. https://doi.org/10.1007/s00264-009-0832-z.
Buijze GA, Richardson S, Jupiter JB. Successful reconstruction for complex malunions and nonunions of the tibia and femur. J Bone Jt Surg-Am Vol. 2011;93A:485–92. https://doi.org/10.2106/jbjs.j.00342.
Kwok CS, Crossman PT, Loizou CL. Plate versus nail for distal tibial fractures: a systematic review and meta-analysis. J Orthop Trauma. 2014;28:542–8.
Padilla-Eguiluz NG, Gomez-Barrena E. Epidemiology of long bone non-unions in Spain. Inj-Int J Care Inj. 2021;52:S3–7. https://doi.org/10.1016/j.injury.2021.02.053.
Chloros GD, Kanakaris NK, Vun JSH, Howard A, Giannoudis PV. Scoring systems for early prediction of tibial fracture non-union: an update. Int Orthop. 2021;45:2081–91. https://doi.org/10.1007/s00264-021-05088-0.
Zura R, Xiong Z, Einhorn T, Watson JT, Ostrum RF, Prayson MJ, Della Rocca GJ, Mehta S, McKinley T, Wang Z, Steen RG. Epidemiology of fracture nonunion in 18 human bones. JAMA Surg. 2016. https://doi.org/10.1001/jamasurg.2016.2775.
Baldwin P, Li DJ, Auston DA, Mir HS, Yoon RS II, Koval KJ. Autograft, allograft, and bone graft substitutes: clinical evidence and indications for use in the setting of orthopaedic trauma surgery. J Orthop Trauma. 2019;33:203–13. https://doi.org/10.1097/bot.0000000000001420.
Pountos I, Georgouli T, Kontakis G, Giannoudis PV. Efficacy of minimally invasive techniques for enhancement of fracture healing: evidence today. Int Orthop. 2010;34:3–12. https://doi.org/10.1007/s00264-009-0892-0.
Moghaddam A, Elleser C, Biglari B, Wentzensen A, Zimmermann G. Clinical application of BMP 7 in long bone non-unions. Arch Orthop Trauma Surg. 2010;130:71–6. https://doi.org/10.1007/s00402-009-0982-x.
Cevolani L, Bianchi G, Costantino E, Staals E, Lucarelli E, Spazzoli B, Frisoni T, Donati DM. Minimally invasive treatment of long bone non-unions with bone marrow concentrate, demineralized bone matrix and platelet-rich fibrin in 38 patients. J Tissue Eng Regen Med. 2021;15:831–40. https://doi.org/10.1002/term.3231.
Valdes MA, Thakur NA, Namdari S, Ciombor DM, Palumbo M. Recombinant bone morphogenic protein-2 in orthopaedic surgery: a review. Arch Orthop Trauma Surg. 2009;129:1651–7. https://doi.org/10.1007/s00402-009-0850-8.
Antonova E, Le TK, Burge R, Mershon J. Tibia shaft fractures: costly burden of nonunions. BMC Musculoskeletal Disord. 2013. https://doi.org/10.1186/1471-2474-14-42.
Acknowledgements
This study was supported by Keqiao Clinical Funding (NO.2022KZ68, 2022KZ71, and 2022KZ80). We thank textcheck.com for its linguistic assistance during the preparation of this manuscript (http://www.textcheck.com/certificate/index/JxAspx).
Author information
Authors and Affiliations
Contributions
DX and ZL contributed to the study’s conception and design. Data collection was performed by JX, YZ, and YH. Data were analyzed by Bing Wu. The first draft of the manuscript was written by JX and BW. DX and ZL edited the draft and revised it. All the authors commented on previous versions of the manuscript and revised it. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The protocols of study were approved by the Ethics Committee of The Central Hospital Affiliated to Shaoxing University, Shaoxing, People’s Republic of China.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, D., Xie, J., Wu, B. et al. Comparison of mini-open reduction and autologous bone grafting with closed reduction and intramedullary device insertion for tibial shaft fractures: a retrospective study. J Orthop Surg Res 18, 519 (2023). https://doi.org/10.1186/s13018-023-04024-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-023-04024-9