Abstract
Background
To analyze the growth disturbance after distal tibia physeal fracture in children.
Methods
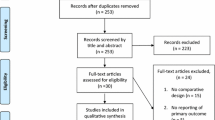
Data about children with distal tibia physeal fractures between September 2015 to September 2018 were collected, including age, gender, affected side, Salter–Harris classification, initial maximal displacement, with or without fibula fracture, open or closed reduction, the method of fixation, time to surgery, blood loss, duration of operation, and complications. Patients were placed in the growth disturbance group when leg length discrepancy was equal to or greater than 1.5 cm, or when they had more than 5 degrees of varus or valgus deformity. Others were placed in the no-growth disturbance group.
Results
A total of 143 patients (96 boys and 47 girls) were enrolled in this study. The length of the follow-up periods averaged 29.34 ± 7.46 months (26 to 61 months). Among the total of 143 patients, the incidence of growth disturbance was 15.39% (22/143). The no-growth disturbance group consisted of 121 patients (84 boys and 37 girls), with a mean age of 11.50 ± 3.20 years, and there were 68, 52, and 1 injuries to the left, right, and bilateral sides, respectively. The average maximal displacement was 5.51 ± 3.18 mm, and 27.27% (33/121) of patients also had a fibula fracture. The growth disturbance group contained 22 patients (12 boys and 10 girls) with a mean age of 9.32 ± 3.56 years, and there were 12, 10, and 0 injuries on the left, right, and bilateral sides, respectively. The average maximal displacement was 5.77 ± 4.89 mm, and 45.45% (10/22) of patients also had a fibula fracture. There was a significant difference in age (p = 0.004) and fibula fracture (p = 0.011) between the two groups. More patients had Salter–Harris types III and IV fractures in the growth disturbance group than in the no-growth disturbance group (p = 0.043).
Conclusions
Children with Salter–Harris types III and IV fractures, younger children, and children with fibula fractures all have a higher incidence of growth disturbance after distal tibia physeal fractures.
Level of evidence
Level III-Prognostic study.
Similar content being viewed by others
Introduction
Distal tibia physeal fractures are a relatively common physeal injury and are the second most common injury in children after the distal radius physis [1, 2]. Distal tibia physeal fractures account for approximately 11–20% of all physeal fractures [3, 4]. The stronger ligamentous attachments make the physis more vulnerable to injury and more likely to be accompanied by subsequent premature growth arrest, which causes angular deformity and differences in leg length 1–2 years after injury [1, 5, 6]. Growth disturbance is defined as differences in leg length equal to or greater than 1.5 cm or varus or valgus deformity more than 5 degrees [7]. According to different studies, the incidence of growth disturbance varies as between 2 and 40% [8,9,10].
Multiple factors, including the cause of injury, fracture type and location, initial displacement, Salter–Harris classification, number of attempted reductions, open or closed reduction, and residual displacement after the intervention, are thought to be associated with growth disturbance [6, 11,12,13]. However, the factors affecting growth disturbance are still unclear. Therefore, this study aims to assess the factors related to growth disturbance after distal tibia physeal fractures in children.
Patients and methods
Data about children with distal tibia physeal fractures who were treated in Fuzhou Second Hospital Affiliated with Xiamen University between September 2015 to September 2018 were collected. All patient files were reviewed with the approval of the hospital. Patients were placed in the growth disturbance group when the difference in their leg lengths was equal to or greater than 1.5 cm or more than 5 degrees of varus or valgus deformity. Otherwise, they were placed in the no-growth disturbance group.
All patients were further divided into early and delayed operation groups. According to Rang and Salter [14, 15], patients were classified in the early operation group when the time from injury to operation was equal to or less than 7 days, and classified in the delayed operation group when it exceeded 7 days.
The following data were extracted from the database: age, gender, affected side, Salter–Harris classification, initial maximal displacement, the presence of fibula fracture, open or closed reduction, method of fixation, time to surgery, blood loss, duration of operation, and complications.
The inclusion criteria were as follows:
-
1.
Age less than 16 years.
-
2.
Diagnosed with distal tibia physeal fracture.
-
3.
Residual displacement less than 2 mm after surgery, measured by scale with a 2 mm diameter steel ball or K-wire nest to the ankle joint.
-
4.
Follow-up more than 12 months.
The exclusion criteria were as follows:
-
1.
Peripheral vascular diseases.
-
2.
Neuromuscular diseases.
-
3.
Metabolic bone disorders.
-
4.
Pathological fractures.
-
5.
Residual displacement more than 2 mm after surgery.
SPSS 22.0 software was used for all statistical analyses. Descriptive statistics were conducted for continuous variables using mean ± standard error (SE). A comparison test between two independent or more than two groups was made using a two-sided Student’s t-test or one-way analysis of variance at a 5% significance level (2.5% on each side). Descriptive statistics of categorical variables were represented as frequency and percentage. A Chi-square test was used to compare the differences in rates among different groups at a 5% significance level (2.5% on each side).
Results
A total of 143 patients (96 boys and 47 girls), with an average age of 11.19 ± 3.34 (range from 2.8 to 16) years, were enrolled in this study. The follow-up periods averaged 29.34 ± 7.46 months (26 to 61 months). The overall incidence of growth disturbance was 15.39% (22/143); among them, 21 cases had varus or valgus deformities greater than 5 degrees, and 1 case had a limb shortening exceeding 1.5 cm. However, no infection, nonunion, or osteonecrosis was observed in any patient.
The no-growth disturbance group contained 121 patients (84 boys and 37 girls), with a mean age of 11.50 ± 3.20 years, and 68, 51, and 1 cases on the left, right, and bilateral sides, respectively. The average maximal displacement was 5.51 ± 3.18 mm. The growth disturbance group contained 22 patients (12 boys and 10 girls) with a mean age of 9.32 ± 3.56 years, and 12, 10, and 0 cases on the left, right, and bilateral sides, respectively. The average maximal displacement was 5.77 ± 4.89 mm, and the average comprehensive displacement was 5.05 ± 2.38 mm. There was a significant difference in age between the two groups (p = 0.004), but no significant difference in the factors described above (Table 1).
According to Salter–Harris classification, patients with type I/II/III/IV fracture were 7/59/9/9 in the normal group and 3/7/4/4 in the growth disturbance group. As transitional fractures, there were 31 Triplane fractures and 6 Tillaux fractures in the no-growth disturbance group, and 4 Triplane fractures and 0 Tillaux fractures in the growth disturbance group (Table 2). More Salter–Harris types III and IV patients were in the growth disturbance group than in the no-growth disturbance group (p = 0.043) (Fig. 1). The SH grade analysis showed that growth disturbance occurred 3/10 (30%) in SH grade I, 7/66 (10.61%) in SH grade II, 4/13 (30.77%) in SH Grade III, and 4/13 (30.77%) in SH grade IV (Table 2).
Among the no-growth disturbance group, 27.27% (33/121) of patients also had fibula fractures, while 45.45% (10/22) of patients in the growth disturbance group also had fibula fractures, which was significantly different (p = 0.011). Differences in open or closed reduction, type of fixation, duration of operation, and blood loss were not significant between the two groups. Forty-four cases received K-wires, 76 received screws, and 1 received plates in the no-GD group; 8 cases received K-wires, 14 received screws, and 0 received plates in the GD group. Differences between the two groups were not significant.
There was no significant difference in growth disturbance between the early group (18/123) and the delayed operation group (3/20) (p > 0.05) (Figs. 2, 3).
a An 11-year-old patient, Salter–Harris type II, distal tibia physeal fracture accompanied by fibula fracture, accepted open reduction 17 days after injury, osteotyluss growth can be seen in CT scan showed in the red frame. Growth disturbance has not been observed during 39 month follow-up. b An 11-year-old boy, Salter–Harris type III Distal tibia physeal fracture, accepted open reduction 4 days after injury. Growth disturbance has been observed at 13-month follow-up, the lateral angle of the distal tibia was 98° at 26-month follow-up
Discussion
Like some fractures, physeal injuries can be complicated by malunion, infections, neurovascular problems, or osteonecrosis. The incidence of growth disturbance after distal tibia physeal fractures was variable based on previously published findings, ranging from 2% [8] to almost 40% [9]. In this study, the overall incidence of growth disturbance was 15.39% (22/143), which was within the range of previous research [8, 9, 16].
Growth disturbance has been related to many different factors, including the cause of injury, fracture type and location, initial displacement, Salter–Harris classification, number of attempted reductions, open or closed reduction, quality of reduction, and the different composition characteristics of patients. However, few articles have reported the effects of age on growth disturbance after distal tibia physeal fractures. Our study found that age was an important factor affecting growth disorders. The average age of the growth disturbance group was significantly lower than that of the no-growth disturbance group. This could be due to the greater growth potential of younger children and a greater effect on growth after a fracture. Additionally, there were 4 Triplane fractures and 0 Tillaux fractures among the 22 patients with malformations, which could occur in older adolescents. This suggests that age was an important factor in growth disorders after distal tibia physeal fractures.
The growth disturbance in grade I was similar to that in grade III/IV, probably because there were so few cases in grade I. Salter–Harris types III and IV fractures displayed a higher growth disturbance, which could be due to injuries to the germinal layer of the physis [17]. Our study also found that there were more Salter–Harris types III and IV patients in the growth disturbance group than in the no-growth disturbance group (p = 0.043) (Fig. 1).
We also found that the growth disturbance group (12/22) (Table 3) was more likely to also have fibula fractures than the normal group (33/121) (p = 0.011). Patients with fibula fractures could have suffered more significant injuries. Significant injuries often manifest as larger initial displacements but can also be accompanied by other fractures.
Patients were classified either into an early operation group or a delayed operation group based on the methods used by Rang and Salter [13, 14]. They suggested that delayed reduction makes it more difficult to achieve fracture reduction and places the viability of the physis at risk when forceful reduction is required. However, Egol KA reported that delayed reduction showed no evidence of physeal damage, physeal growth disturbance, or radiographic bar formation in a rat model study [18]. Our study included closed or open reduction in 20 delayed operation patients (mean 12.8 ± 6.68 days, range from 8 to 37 days). Differences in growth disturbance were not significant compared with early operation patients (Fig. 2).
This study had some limitations. It was a retrospective study, and the number of cases was limited. Growth disturbance from a physeal fracture is typically evident 2 to 6 months after the injury, but it may not become obvious for up to 2 or more years after the injury. Therefore, follow-ups should be extended to near skeletal maturity. However, Stenroos et al. [19] suggested that routine radiographic follow-up is unnecessary after physeal fractures of the distal tibia in children. We believe this study will significantly improve prognosis in children after distal tibia physeal fractures.
Conclusion
Patients in the growth disturbance group were significantly younger and more likely to be Salter–Harris types III and IV than patients in the no-growth disturbance group. Patients who also had fibula fractures could have a higher incidence of growth disorders.
Availability of data and materials
The data used for analysis in our study are available from the corresponding author on reasonable request.
References
Kraus R, Kaiser M. Growth disturbances of the distal tibia after physeal separation—what do we know, what do we believe we know? A review of current literature. Eur J Pediatr Surg. 2008;18:295–9.
Peterson HA, Brewster RC, Johnson KA. Epiphyseal growth plate injuries of the distal tibia. Minn Med. 1977;60:44–50.
Oh WH, Craig C, Banks HH. Epiphyseal injuries. Pediatr Clin North Am. 1974;21:407–22.
Stefanich RJ, Lozman J. The juvenile fracture of Tillaux. Clin Orthop Relat Res. 1986;210:219–27.
Spiegel PG, Cooperman DR, Laros GS. Epiphyseal fractures of the distal ends of the tibia and fibula. A retrospective study of two hundred and thirty-seven cases in children. J Bone Joint Surg Am. 1978;60:1046–50.
Kling TJ, Bright RW, Hensinger RN. Distal tibial physeal fractures in children that may require open reduction. J Bone Joint Surg Am. 1984;66:647–57.
Basener CJ, Mehlman CT, Dipasquale TG. Growth disturbance after distal femoral growth plate fractures in children: a meta-analysis. J Orthop Trauma. 2009;23:663–7.
Dugan G, Herndon WA, Mcguire R. Distal tibial physeal injuries in children: a different treatment concept. J Orthop Trauma. 1987;1:63–7.
Pacicca D, Cramer K, Tornetta P. Is anatomic reduction necessary for displaced physeal fractures of the distal tibia? In: Programs and abstracts of the American Academy of Orthopaedic Surgeons 68th Annual Meeting. 2001; p. 131.
Barmada A, Gaynor T, Mubarak SJ. Premature physeal closure following distal tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop. 2003;23:733–9.
Rohmiller MT, Gaynor TP, Pawelek J, et al. Salter-Harris I and II fractures of the distal tibia: does mechanism of injury relate to premature physeal closure? J Pediatr Orthop. 2006;26:322–8.
Leary JT, Handling M, Talerico M, et al. Physeal fractures of the distal tibia: predictive factors of premature physeal closure and growth arrest. J Pediatr Orthop. 2009;29:356–61.
Russo F, Moor MA, Mubarak SJ, et al. Salter-Harris II fractures of the distal tibia: does surgical management reduce the risk of premature physeal closure? J Pediatr Orthop. 2013;33:524–9.
Rang M. Injuries of the epiphysis, growth plate and perichondral ring. In: Rang M, editor. Children’s Fracture. Philadelphia: Lippincott; 1983. p. 10.
Salter R. Epiphyseal plate injuries. In: Letts R, editor. Management of Pediatric Fracture. New York: Churchill Living-atone; 1994. p. 10.
Wang W, Xiong Z, Li Y, Chen S, et al. Variables influencing radiological fracture healing in children with femoral neck fractures treated surgically: a review of 177 cases. Orthop Traumatol Surg Res. 2022;108(1):103052.
D’Angelo F, Solarino G, Tanas D, et al. Outcome of distal tibia physeal fractures: a review of cases as related to risk factors. Injury. 2017;48:S7–11.
Egol KA, Karunakar M, Phieffer L, et al. Early versus late reduction of a physeal fracture in an animal model. J Pediatr Orthop. 2002;22:208–11.
Stenroos A, Kosola J, Puhakka J, et al. Routine radiographic follow-up is not necessary after physeal fractures of the distal tibia in children. Acta Orthop. 2019;90:610–3.
Acknowledgements
We declare that we have no financial and personal relationships with other people or organizations that can inappropriately influence our work, and there is no professional or other personal interest of any nature or kind in any product, service, and/or company that could be construed as influencing the position presented in, or the review of, the manuscript. The work was performed by Hui Chen, Zhao Chen, Peisheng Chen, Zibing Zheng, and Jinrun Lin.
Funding
This study was financially supported by Startup Fund for scientific research, Fujian Medical University (Grant No. 2019QH1136); Nature Fund of Fujian Province (Grant No. 2020J05274); and Joint Funds for the innovation of science and Technology, Fujian province (Grant No. 2020Y9157).
Author information
Authors and Affiliations
Contributions
All authors made significant contributions to the writing and editing process. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by the Medical Ethical Committee. Informed consent was obtained from all patients before enrolled in the study.
Consent for publication
All the authors listed have approved the manuscript that is enclosed.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, H., Chen, Z., Chen, P. et al. Incidence of growth disturbance after distal tibia physeal fracture in children. J Orthop Surg Res 17, 529 (2022). https://doi.org/10.1186/s13018-022-03427-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13018-022-03427-4