Abstract
Background
Predicting pathological complete response (pCR) in patients affected by locally advanced rectal cancer (LARC) who undergo neoadjuvant chemoradiotherapy (nCRT) is a challenging field of investigation, but many of the published models are burdened by a lack of reliable external validation. Aim of this study was to evaluate the applicability of a magnetic resonance imaging (MRI) radiomic-based pCR model developed and validated in Europe, to a different cohort of patients from an intercontinental cancer center.
Methods
The original model was based on two clinical and two radiomics features extracted from T2-weighted 1.5 T MRI of 161 LARC patients acquired before nCRT, considered as training set. Such model is here validated using the T2-w 1.5 and 3 T staging MRI of 59 LARC patients with different clinical characteristics consecutively treated in mainland Chinese cancer center from March 2017 to January 2018. Model performance were evaluated in terms of area under the receiver operator characteristics curve (AUC) and relative parameters, such as accuracy, specificity, negative and positive predictive value (NPV and PPV).
Results
An AUC of 0.83 (CI 95%, 0.71–0.96) was achieved for the intercontinental cohort versus a value of 0.75 (CI 95%, 0.61–0.88) at the external validation step reported in the original experience. Considering the best cut-off threshold identified in the first experience (0.26), the following predictive performance were obtained: 0.65 as accuracy, 0.64 as specificity, 0.70 as sensitivity, 0.91 as NPV and 0.28 as PPV.
Conclusions
Despite the introduction of significant different factors, the proposed model appeared to be replicable on a real-world data extra-European patients’ cohort, achieving a TRIPOD 4 level.
Similar content being viewed by others
Background
Medical imaging plays to date a crucial role in tumour staging, clinical workflow definition and prognostic stratification of oncological patients. Radiological findings, integrated with histopathology, blood exams and numerous other clinical parameters, usually determine the optimal therapeutic strategy for each patient affected by a tumour [1]. The opportunity to take fully advantage of quantitative parameters extracted from medical imaging, could provide a more comprehensive characterisation of the tumour, suggesting a more tailored clinical pathway [2]. In the field of quantitative analysis of medical imaging, radiomics represents a topic of growing interest, relying on the biological assumption that the tumours properties (biological aggressiveness) could be described by the phenotypic heterogeneity, and radiological images could allow to successfully quantify it, paving the way to more effective approaches in terms of treatment personalization [3].
Unfortunately, radiomics features are still burdened by several methodological and biological vulnerabilities that hamper their fully aware and effective integration in multidimensional clinical interpretation and translational applications [4, 5].
Rectal cancer represents a significant field of application for radiomics [6], as several grey areas still persist in the management of these patients [7], especially considering the complex interaction among different specialties required to define the optimal therapeutic approach [8, 9]. Neoadjuvant radio-chemotherapy (nCRT) followed by total mesorectal excision (TME) is the current standard of care for locally advanced rectal cancer (LARC) [10, 11] patients and presents variable tumour responses, with nearly 20–30% of pathological complete response (pCR).
Different experiences highlighted that patients showing pCR generally show favourable survival outcomes [12, 13]. The definition of new parameters able to early predict the biological behaviour of rectal cancer in terms of response to the neoadjuvant treatments, represents an innovative strategy to better define organ preservation and less invasive surgical approaches, especially for patients who have overall good prognostic factors [14,15,16].
Even if promising evidence has been produced so far, radiomics still does not represent the standard to characterise rectal cancer behaviour and a growing number of studies is oriented to identify and define a radiomic signature able to predict clinical outcomes [17,18,19,20] or response to neoadjuvant treatment [20,21,22,23]. Promising advances about the role of radiomic biomarkers have also been made thanks to the recent introduction of hybrid MR radiotherapy delivery units (MR-Linac) that make available unprecedented quantities of images [24,25,26].
A robust methodology needs to be pursued in order to allow a full integration of radiomic tools into clinical practice, and existing models need to be validated using external cohorts of patients with the aim to test their replicability [27].
To ensure the reliable development and validation of predictive models, the international scientific community recently established a group of recommendations, known as TRIPOD statements, proposing a standardized methodology where the independent model validation using an external dataset plays a crucial role. Within this framework, also radiomics studies need to fully meet the TRIPOD requirements [22, 28]. The aim of this study was to evaluate the replicability of a radiomic model for pCR prediction, developed and firstly validated in Europe (as TRIPOD 3), on a cohort of patients enrolled in an Asian cancer centre having different clinical characteristics and following different treatment workflows, therefore reaching a TRIPOD 4 evidence score [20].
Methods
Radiomic model for pCR prediction
The magnetic resonance imaging (MRI) based radiomics model object of this study aimed to early identify patients who will undergo pCR. This vendor-independent model was set up in Italy using a single-center training set composed by 162 patients and an external validation set composed by 59 cases provided by two other European centers. All the patients included in the training and validation cohorts underwent diagnostic 1.5 T MRI prior to the neoadjuvant chemoradiotherapy (nCRT) treatment.
External beam radiation therapy (EBRT) was delivered to the whole mesorectum and the drainage nodal stations (total dose of 45 Gy, 1.8 Gy per fraction) and a boost of 50.4 or 55.0 Gy to the gross tumour volume (GTV), if delivered with sequential boost or simultaneous integrated boost respectively. Patients then underwent TME surgery 8–12 weeks after the end of nCRT. Different concomitant chemotherapy regimens were allowed: oral capecitabine 1650 mg/m2 * die (d1-7, q7); 5-fluorouracil 225 mg/m2 * die (d1-7, q7) or CapOx 60 mg/m2 of iv oxaliplatin (d1, q7) plus oral capecitabine 1300 mg/m2 * die (d1-7, q7) according to staging and general conditions of the patients.
Response to nCRT was evaluated by histopathological examination of surgical resected specimens: tumour responses were classified using tumour regression grade (TRG) according to Mandard et al. [29] and pCR was defined as the absence of tumour disease on surgical specimen (ypT0N0).
The radiomics analysis was performed using standard staging MR images acquired before the start of nCRT.
Radiomic features were extracted from T2-weighted MR images as suggested in Dinapoli et al. after the application of the Laplacian of Gaussian (LoG) filter. In particular the entropy was calculated using a kernel width (σ) equal to 0.344 mm, while the skewness using a σ of 0.485 mm [20].
The significant features and the corresponding coefficient values of the linear regression logistic model are summarised in Table 1.
The multivariable model obtained in [20] was based on four covariates: two clinical parameters (clinical tumour and nodal staging, cT and cN) and two radiomics features (skewness and entropy). Its stability was confirmed on both internal and external validation cohorts showing an area under curve (AUC) receiver operating characteristic (ROC) values of 0.73 (95% CI, 0.65–0.82) and 0.75 (CI 95%, 0.61–0.88), respectively. For further details regarding the MRI radiomics-based model set up and results obtained in the training and validation steps, we address the reader to the previous publication [20].
Intercontinental cohort workflow
Patients affected by pathologically proven LARC and treated at Sichuan Cancer Hospital between March 2017 and January 2018 were retrospectively enrolled in this validation study.
Inclusion criteria were: pathologically proven LARC, absence of artefacts in the pelvic MR staging image and availability of tumour regression grade (TRG) classification in the pathologic report.
Patients with distant metastases at diagnosis, younger than 18 years or denying informed consent for retrospective data collection, were excluded from the study.
All the patients meeting the inclusion criteria and consecutively treated during the period under investigation were considered for this study.
All the patients underwent diagnostic MRI with two different scanners available in the radiation oncology department: a Siemens Magnetom Skyra and a Siemens Magnetom Avanto systems (Siemens Medical Systems, Erlangen, Germany), having a static magnetic field strength B0 of 3 Tesla (27 patients), and 1.5 Tesla (32 patients), respectively.
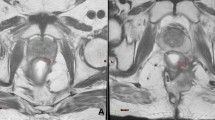
T2-weighted fast spin echo 2D-oblique images acquired on a transversal plan orthogonal to the tumour longitudinal axis were used for the radiomics analysis, in order to be consistent with the original experience reporting the model.
The GTV was firstly contoured by a radiation oncologist of the lower gastro intestinal malignancies department, and then an independent validation was performed by a senior radiation oncologist of the same department.
After an initial cycle of chemotherapy CapOx lasting about 3 weeks and foreseeing capecitabine 1000 mg/m2 at d1-14 concurrently with oxaliplatinum 130 mg/m2 d1, patients followed two different treatment schedules prior to TME. The first treatment scheme involved a 1-week short course of external beam radiotherapy (EBRT, 25 Gy in 5 fractions of 5 Gy per fraction) followed directly after 1-week gap by TME; the second treatment scheme involved nCRT administering EBRT for 5–6 weeks (50.4 Gy in 28 fractions of 1.8 Gy each) concurrently with chemotherapy (Capecitabine 825 mg/m2 die), at the end of which two more cycle of CapOx were foreseen.
Evaluation of the model performance
The clinical and treatment parameters of the intercontinental patients-cohort were compared with those reported in the previous experience [20] using the Mann Whitney test for continue variables and the chi-square test for categorical ones [23, 28,29,30].
The in house developed radiomics platform MODDICOM [25, 31] used to build the model, was used to process the MR images of the Asian cohort, applying the LoG filter and extracting the radiomic features required by the radiomic model.
Response to nCRT was determined following the same procedure adopted in the training cohort of LARC patients [20], both in terms of tumour classification and definition of complete responders.
The evaluation of the model performance was performed in terms of the area under the curve (AUC) of the receiver operator characteristics (ROC) curve; accuracy sensitivity, specificity, negative and positive predictive value (NPV and PPV) calculated at the optimal threshold identified considering the Youden Index on the original data reported. The statistical analysis was carried out using R software (version 3.3.1).
Results
59 patients were lastly enrolled.
The patient characteristics of both the original cohort (European patients, used for training and validation of the model) and of the new cohort enrolled in the Sichuan Cancer Hospital are reported in Table 2.
The original and new cohort of patients reported different magnetic field strength of the MR scanner used for imaging, different nCRT treatment schedules, with subsequent different interval between MRI and CRT and the end of CRT and surgery; no statistical differences in the patients age (p = 0.67), sex (p = 0.56), T staging (p = 0.98) were observed.
The proportion of T staging and sex are very similar between training and validation set, while the median age of validation cases (56 years, range 34–75) is lower than the corresponding training ones (65, range 28–83). No difference has been recorded for N stage.
The total number of pCR cases observed in the Chinese cohort was 10, corresponding to a pCR rate of 16.9% (10/59).
When analysing the intercontinental cohort, the model reported a ROC curve with an AUC value of 0.83 and a 95% confidence interval of 0.71–0.96. The ROC curve is shown in Fig. 1. The applicability of the model tested analysing separately the patients of the intercontinental cohort imaged with a 1.5 T and 3.0 T scanner, gave AUC 0.82 (95% CI 0.61–1.00) and 0.86 (95% CI 0.70–1.00), respectively; the ROC curves obtained are reported in Fig. 2.
Moreover, the best cut-off value was 0.267 in the original experience, corresponding to a Youden index of 0.39 (specificity: 0.63, sensitivity: 0.76); the predictive performance observed for the intercontinental patient dataset considering this threshold are reported in Table 3.
Relative confusion matrices are available as Additional file 1.
Discussion
The predictive role of MRI in rectal cancer has been widely investigated [32] but, to the best of our knowledge, the introduction of radiomic models in clinical practice is still limited, mainly due to the lack of the independent validation studies.
Omics studies in general, and radiomic ones particularly, specifically lack ethnographic information in the models and the possibilities to test this aspect are pretty uncommon, leaving this interesting question unresolved. As far as the authors know, this study represents the first experience of external validation of a rectal cancer radiomic model on an extra-European population, while a previous validation on Asian cohort of patients has been performed for predictive models not including radiomics, with good results in terms of generalisation and overall stability [33].
During the last years, several authors tested MRI radiomics to evaluate its reliability in terms of nCRT response prediction for rectal cancer, including also the analysis of MR images acquired during or at the end of the course of treatment, investigating how the quantitative analysis can support clinicians in the choice of the optimal therapeutic strategy [34,35,36,37,38,39,40,41]. It should be noted that these models were generally trained and validated on very homogeneous clinical trial populations, reaching in the best-case scenario a TRIPOD 3 robustness score, with their possible generalization to a world population being still far to be thoroughly described [42,43,44].
This innovative external intercontinental validation experience has been realised on real-world imaging data of patients enrolled in a different continent, with MRI scans acquired on scanners characterised by different vendor and field strength with respect to those reported in the original model, significantly increasing data heterogeneity and critically stressing the original two-radiomics features model.
High predictive values were reported on the whole external dataset (AUC = 0.83, NPV 0.91), representing a significant result in the context of radiomics-models replicability and translational robustness. Interestingly, the relative subgroup analysis (AUC 0.82 on 1.5 T and 0.86 on 3 T patients) suggests that magnetic field intensity variability can be overcome by means of selecting appropriate image features, as also reported in a previous study [23].
It has to be noted that the PPV observed in the whole cohort is low 0.28 (0.18–0.40), with slightly better results for the 1.5 T cases (0.29, range 0.20–0.41) if compared to the 3 T ones, which reached only 0.22 (0.08–0.48).
This results could be explained by the limited absolute number of pCR in the Chinese cohort and the original design of the Dinapoli et al. model, set on 1.5 T images. Nevertheless, the very high NPV 0.91 (0.80–0.97) observed in the whole cohort represents a stimulating result in order to guide a more tailored treatment approach in patients predicted as “not responding” to nCRT. Similar experiences represent the rationale for new radiomics driven trials, where dose intensification is foreseen for patients predicted as not responding [41, 45].
Futhermore, the observed results suggest the applicability of the original model by Dinapoli et al. also for LARC patients undergoing short course radiotherapy, supporting the hypothesis of an intrinsic biological signature of the tumor that could be correlated with different radiomic features [20].
Besides the limited patients sample for the intercontinental validation (59 patients, representing the 36.4% of the original model sample), one of the possible limitations of this study maybe identified in the lack of a multi observer based segmentation to test the robustness of radiomic features, to which we preferred an expertise based segmentation (revision by a senior staff member). Nevertheless, this choice reflects the fact that decisions are generally taken on single operator’s segmentations in daily clinical practice and that the model object of this study is based on two first order radiomic features, which were recently categorised as the least sensitive to manual tumour delineation in a recent experience performed on MRI in LARC patients [46].
Despite the heterogeneity of the treatments offered to patients of the different cohorts (i.e. type of neoadjuvant treatment; EBRT administered in short versus long course; different MR vendors and field strength used; patient clinical and ethnic characteristics), the proposed model appeared to be overall replicable on a real-world data extra-European patients’ cohort, offering an innovative hint for radiomics validation procedures.
New experiences including larger cohorts of patients are encouraged to further validate the proposed model with tighter confidence intervals, confirming the generalizability of the model to the entire world population.
The next validation step will be represented by the setup of a prospective study in order to confirm the advantages of using these innovative imaging based predictive models supporting clinical decision making and personalised cancer care especially considering the innovative applications of MRI in radiation oncology, thanks to the promising applications of MR-Linacs in the management of rectal cancer [47].
Conclusion
The intercontinental external validation of this model confirmed the robustness and replicability of the original model with a TRIPOD 4 level. The promising results obtained encourage further investigations for the application of radiomics modelling in the framework of complex multivariable decision support systems for LARC.
Availability of data and materials
The data are fully available and will be included within the article and in its additional files.
Abbreviations
- pCR:
-
Pathological complete response
- LARC:
-
Locally advanced rectal cancer
- nCRT:
-
Neoadjuvant chemoradiotherapy
- MR:
-
Magnetic resonance
- AUC:
-
Area under the curve
- ROC:
-
Receiver operating characteristics
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- TME:
-
Total mesorectal excision
- EBRT:
-
External beam radiation therapy
- GTV:
-
Gross target volume
- TRG:
-
Tumour regression grade
- LoG:
-
Laplacian of Gaussian
- cT:
-
Clinical tumour
- cN:
-
Nodal staging
References
Giger ML. Machine learning in medical imaging. J Am Coll Radiol JACR. 2018;15(3 Pt B):512–20.
Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data. Radiology. 2016;278(2):563–77.
Gatenby RA, Grove O, Gillies RJ. Quantitative imaging in cancer evolution and ecology. Radiology. 2013;269(1):8–14.
Yip SSF, Aerts HJWL. Applications and limitations of radiomics. Phys Med Biol. 2016;61(13):R150–66.
Lambin P, van Stiphout RGPM, Starmans MHW, Rios-Velazquez E, Nalbantov G, Aerts HJWL, et al. Predicting outcomes in radiation oncology—multifactorial decision support systems. Nat Rev Clin Oncol. 2013;10(1):27–40.
Dinapoli N, Casà C, Barbaro B, Chiloiro GV, Damiani A, Matteo MD, et al. Radiomics for rectal cancer. Transl Cancer Res. 2016;5(4):424–31.
Valentini V, Marijnen C, Beets G, Bujko K, De Bari B, Cervantes A et al. The 2017 Assisi think tank meeting on rectal cancer: a positioning paper. Radiother Oncol. 2019; S0167814019329809.
Maas M, Nelemans PJ, Valentini V, Das P, Rödel C, Kuo L-J, et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol. 2010;11(9):835–44.
Breugom AJ, Swets M, Bosset J-F, Collette L, Sainato A, Cionini L, et al. Adjuvant chemotherapy after preoperative (chemo)radiotherapy and surgery for patients with rectal cancer: a systematic review and meta-analysis of individual patient data. Lancet Oncol. 2015;16(2):200–7.
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351(17):1731–40.
Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet. 2009;373(9666):811–20.
Vecchio FM, Valentini V, Minsky BD, Padula GDA, Venkatraman ES, Balducci M, et al. The relationship of pathologic tumour regression grade (TRG) and outcomes after preoperative therapy in rectal cancer. Int J Radiat Oncol. 2005;62(3):752–60.
Valentini V, van Stiphout RGPM, Lammering G, Gambacorta MA, Barba MC, Bebenek M, et al. Nomograms for predicting local recurrence, distant metastases, and overall survival for patients with locally advanced rectal cancer on the basis of European randomized clinical trials. J Clin Oncol Off J Am Soc Clin Oncol. 2011;29(23):3163–72.
Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U, Silva e Sousa AH, et al. Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg. 2004;240(4):711–7 (discussion 717-718).
Habr-Gama A, São Julião GP, Fernandez LM, Vailati BB, Andrade A, Araújo SEA, et al. Achieving a complete clinical response after neoadjuvant chemoradiation that does not require surgical resection: it may take longer than you think! Dis Colon Rectum. 2019;62(7):802–8.
Rizzo G, Zaccone G, Magnocavallo M, Mattana C, Pafundi DP, Gambacorta MA, et al. Transanal endoscopic microsurgery after neoadjuvant radiochemotherapy for locally advanced extraperitoneal rectal cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Br Assoc Surg Oncol. 2017;43(8):1488–93.
Ng F, Ganeshan B, Kozarski R, Miles KA, Goh V. Assessment of primary colorectal cancer heterogeneity by using whole-tumour texture analysis: contrast-enhanced CT texture as a biomarker of 5-year survival. Radiology. 2013;266(1):177–84.
Jeon SH, Song C, Chie EK, Kim B, Kim YH, Chang W, et al. Delta-radiomics signature predicts treatment outcomes after preoperative chemoradiotherapy and surgery in rectal cancer. Radiat Oncol. 2019;14(1):43.
Boldrini L, Cusumano D, Chiloiro G, Casà C, Masciocchi C, Lenkowicz J, et al. Delta radiomics for rectal cancer response prediction with hybrid 0.35 T magnetic resonance-guided radiotherapy (MRgRT): a hypothesis-generating study for an innovative personalized medicine approach. Radiol Med (Torino). 2019;124(2):145–53.
Dinapoli N, Barbaro B, Gatta R, Chiloiro G, Casà C, Masciocchi C, et al. Magnetic resonance, vendor-independent, intensity histogram analysis predicting pathologic complete response after radiochemotherapy of rectal cancer. Int J Radiat Oncol Biol Phys. 2018;102(4):765–74.
Cusumano D, Dinapoli N, Boldrini L, Chiloiro G, Gatta R, Masciocchi C, et al. Fractal-based radiomic approach to predict complete pathological response after chemo-radiotherapy in rectal cancer. Radiol Med (Torino). 2018;123(4):286–95.
Gatta R, Vallati M, Dinapoli N, Masciocchi C, Lenkowicz J, Cusumano D, et al. Towards a modular decision support system for radiomics: a case study on rectal cancer. Artif Intell Med. 2018;96:145–53.
Cusumano D, Meijer G, Lenkowicz J, Chiloiro G, Boldrini L, Masciocchi C, et al. A field strength independent MR radiomics model to predict pathological complete response in locally advanced rectal Cancer. Radiol Med (Torino). 2020;126:421–9.
Chiloiro G, Boldrini L, Elisa Meldolesi E, Alessia Re A, Cellini F, Cusumano D, Corvari B, Mantini G, Mario Balducci M, Valentini V, Gambacorta MA. MR-guided radiotherapy in rectal cancer: first clinical experience of an innovative technology. Clin Transl Radiat Oncol. 2019;12(18):80–6.
Boldrini L, Intven M, Bassetti M, Valentini V, Gani C. MR-guided radiotherapy for rectal cancer: current perspective on organ preservation. Front Oncol. 2021;11:619852.
Corradini S, Alongi F, Andratschke N, Belka C, Boldrini L, Cellini F, Debus J, Guckenberger M, Hörner-Rieber J, Lagerwaard FJ, Mazzola R. MR-guidance in clinical reality: current treatment challenges and future perspectives. Radiat Oncol. 2019;14(1):92.
Lambin P, Leijenaar R, Deist T, Peerlings J, de Jong E, Van Timmeren V, Sanduleanu S, Larue R, Even A, Arthur Jochems A. Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol. 2017;14(12):749–62.
Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med. 2015;162(1):55.
Mandard AM, Dalibard F, Mandard JC, Marnay J, Henry-Amar M, Petiot JF, et al. Pathologic assessment of tumour regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer. 1994;73(11):2680–6.
Parmar C, Grossmann P, Bussink J, Lambin P, Aerts HJWL. Machine learning methods for quantitative radiomic biomarkers. Sci Rep. 2015;17(5):13087.
Dinapoli N, Alitto AR, Vallati M, Gatta R, Autorino R, Boldrini L, et al. Moddicom: a complete and easily accessible library for prognostic evaluations relying on image features. Conf Proc Annu Int Conf IEEE Eng Med Biol Soc IEEE Eng Med Biol Soc Annu Conf. 2015;2015:771–4.
Barbaro B, Vitale R, Valentini V, Illuminati S, Vecchio FM, Rizzo G, et al. Diffusion-weighted magnetic resonance imaging in monitoring rectal cancer response to neoadjuvant chemoradiotherapy. Int J Radiat Oncol. 2012;83(2):594–9.
Shen L, van Soest J, Wang J, Yu J, Hu W, Gong YUT, et al. Validation of a rectal cancer outcome prediction model with a cohort of Chinese patients. Oncotarget. 2015;6(35):38327–35.
Nie K, Shi L, Chen Q, Hu X, Jabbour SK, Yue N, et al. Rectal cancer: assessment of neoadjuvant chemoradiation outcome based on radiomics of multiparametric MRI. Clin Cancer Res Off J Am Assoc Cancer Res. 2016;22(21):5256–64.
Liu Z, Zhang X-Y, Shi Y-J, Wang L, Zhu H-T, Tang Z, et al. Radiomics analysis for evaluation of pathological complete response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Clin Cancer Res Off J Am Assoc Cancer Res. 2017;23(23):7253–62.
Horvat N, Veeraraghavan H, Khan M, Blazic I, Zheng J, Capanu M, et al. MR imaging of rectal cancer: radiomics analysis to assess treatment response after neoadjuvant therapy. Radiology. 2018;287(3):833–43.
Li Y, Liu W, Pei Q, Zhao L, Güngör C, Zhu H, et al. Predicting pathological complete response by comparing MRI-based radiomics pre- and postneoadjuvant radiotherapy for locally advanced rectal cancer. Cancer Med. 2019;8(17):7244–52.
Shi L, Zhang Y, Nie K, Sun X, Niu T, Yue N, et al. Machine learning for prediction of chemoradiation therapy response in rectal cancer using pre-treatment and mid-radiation multi-parametric MRI. Magn Reson Imaging. 2019;61:33–40.
Yi X, Pei Q, Zhang Y, Zhu H, Wang Z, Chen C, et al. MRI-based radiomics predicts tumour response to neoadjuvant chemoradiotherapy in locally advanced rectal cancer. Front Oncol. 2019;26(9):552.
Fiorino C, Gumina C, Passoni P, Palmisano A, Broggi S, Cattaneo GM, et al. A TCP-based early regression index predicts the pathological response in neo-adjuvant radio-chemotherapy of rectal cancer. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2018;128(3):564–8.
Cusumano D, Boldrini L, Yadav P, Yu G, Musurunu B, Chiloiro G, et al. External validation of early regression index (ERITCP) as predictor of pathologic complete response in rectal cancer using magnetic resonance-guided radiation therapy. Int J Radiat Oncol Biol Phys. 2020;108(5):1347–56.
Antunes JT, Ofshteyn A, Bera K, Wang EY, Brady JT, Willis JE, et al. Radiomic features of primary rectal cancers on baseline T2-weighted MRI are associated with pathologic complete response to neoadjuvant chemoradiation: a multisite study. J Magn Reson Imaging. 2020;52(5):1531–41.
Pang X, Wang F, Zhang Q, Li Y, Huang R, Yin X, et al. A pipeline for predicting the treatment response of neoadjuvant chemoradiotherapy for locally advanced rectal cancer using single MRI modality: combining deep segmentation network and radiomics analysis based on “suspicious region.” Front Oncol. 2021;11:711747.
van Griethuysen JJM, Lambregts DMJ, Trebeschi S, Lahaye MJ, Bakers FCH, Vliegen RFA, et al. Radiomics performs comparable to morphologic assessment by expert radiologists for prediction of response to neoadjuvant chemoradiotherapy on baseline staging MRI in rectal cancer. Abdom Radiol (NY). 2020;45(3):632–43.
Chiloiro G, Cusumano D, Boldrini L, Romano A, Placidi L, Nardini M, Meldolesi E, et al. THUNDER 2: THeragnostic Utilities for Neoplastic DisEases of the Rectum by MRI guided radiotherapy. BMC Cancer. 2022;22(1):67.
Traverso A, Kazmierski M, Shi Z, Kalendralis P, Welch M, Dahl Nissen H, Jaffray D, et al. Stability of radiomic features of apparent diffusion coefficient (ADC) maps for locally advanced rectal cancer in response to image pre-processing. Phys Med. 2019;61:44–51.
Gani C, Boldrini L, Valentini V. Online MR guided radiotherapy for rectal cancer. New opportunities. Clin Transl Radiat Oncol. 2019;8(18):66–7.
Acknowledgements
None.
Funding
The authors received funds from Chengdu Science and Technology Project, 2021-YF05-01484-SN; Excellent Youth Foundation Project of Sichuan Cancer Hospital, YB2021037; Foundation Project of Health Commission of Sichuan Province, 20PJ112.
Author information
Authors and Affiliations
Contributions
Study concept and design of the Research: LB, VV, ND; Acquisition of data and images dataset processing: JL, GY, DC, CC, GC; Analysis and interpretation of data: ND, JL, YG, LCO; Manuscript Preparation: JL, DC, PQ; Writing Manuscript LB, LCO, MAG, Manuscript critical revision: LB, VV. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The authors declare that this retrospective study “Applicability of a Pathological Complete Response Magnetic Resonance-based Radiomics model for Locally Advanced Rectal Cancer in intercontinental cohort received the approval of the ethic Committee of Sichuan Cancer Hospital located in 55th Renmin South Road, 4th Section, 610041, Chengdu, China (Approval number SCCHEC 02-2020-008, 28th of April 2020).
Consent for publication
Even if no individual patient data were reported, consensus has been received by every patient for the elaboration of its data and for future scientific publication.
Competing interests
None of the authors have any competing interests (financial and non-financial) in the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Confusion matrices of the predictive performances for the intercontinenental cohort.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Boldrini, L., Lenkowicz, J., Orlandini, L.C. et al. Applicability of a pathological complete response magnetic resonance-based radiomics model for locally advanced rectal cancer in intercontinental cohort. Radiat Oncol 17, 78 (2022). https://doi.org/10.1186/s13014-022-02048-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13014-022-02048-9