Abstract
Background
The use of intrapartum interventions is becoming increasingly common globally. Interventions during birth, including caesarean section (CS), epidural analgesia and synthetic oxytocin infusion, can be important in optimizing obstetric care, but have the potential to impact breastfeeding. This study aimed to identify whether women who have certain intrapartum interventions have greater odds of unfavourable breastfeeding outcomes, both the immediate post-partum period and in the months after birth.
Methods
This was a population-based cohort study of singleton livebirths at ≥37 weeks’ gestation between 2010 and 2018 in Victoria, Australia using routinely-collected state-wide data from the Victorian Perinatal Data Collection (VPDC) and the Child Development Information System (CDIS). The interventions included were pre-labour CS, in-labour CS, epidural analgesia, and synthetic oxytocin infusion (augmentation and/or induction of labour). Outcomes were formula supplementation in hospital, method of last feed before hospital discharge and breastfeeding status at 3-months and 6-months. Descriptive statistics and multivariable logistic regression models adjusting for potential confounders were employed.
Results
In total, 599,191 women initiated breastfeeding. In-labour CS (aOR 1.96, 95%CI 1.93,1.99), pre-labour CS (aOR 1.75, 95%CI 1.72,1.77), epidural analgesia (aOR 1.45, 95%CI 1.43,1.47) and synthetic oxytocin infusion (aOR 1.24, 95%CI 1.22,1.26) increased the odds of formula supplementation in hospital. Long-term breastfeeding data was available for 105,599 infants. In-labour CS (aOR 0.79, 95%CI 0.76,0.83), pre-labour CS (aOR 0.73, 95%CI 0.71,0.76), epidural analgesia (aOR 0.77, 95%CI 0.75,0.80) and synthetic oxytocin infusion (aOR 0.89, 95%CI 0.86–0.92) decreased the odds of exclusive breastfeeding at 3-months post-partum, which was similar at 6-months. There was a dose-response effect between number of interventions received and odds of each unfavourable breastfeeding outcome.
Conclusion
Common intrapartum interventions are associated with less favourable breastfeeding outcomes, both in hospital and in the months after birth. This confirms the importance of only undertaking interventions when necessary. When interventions are used intrapartum, an assessment and identification of women at increased risk of early discontinuation of breastfeeding has to be performed. Targeted breastfeeding support for women who have intrapartum interventions, when they wish to breastfeed, is important.
Similar content being viewed by others
Background
Despite more than 95% of women initiating breastfeeding after birth in Australia [1], early discontinuation and supplementation with infant formula, a known influence on long-term breastfeeding success [2]. is common [3] At 6 months of age, fewer than 15% of infants are exclusively breastfeeding and only half of infants receive any breastmilk [4]. The likelihood that a mother will breastfeed after birth, and sustain that breastfeeding until her child is at least 6 months of age, is influenced by a number of complex factors including maternal sociodemographic characteristics, professional and peer support networks, physiological state and intention to breastfeed [5,6,7]. There are several known barriers to successful breastfeeding including smoking, obesity, diabetes, multiple births and pre-term births. One factor that has garnered attention in recent years is the influence of perinatal interventions. Intrapartum interventions, specifically caesarean section (CS), epidural analgesia, and synthetic oxytocin infusion, have been proposed to interfere with optimal breastfeeding success through various mechanisms. For example, reduced skin-to-skin contact after CS has been shown to affect lactation by limiting infant pre-feeding behaviours, maternal-infant bonding and maternal oxytocin release [8]. Skin-to-skin contact, which involves positioning the dried, naked infant prone on the mother’s bare chest, and zero separation between the newborn baby and the mother immediately after birth, are well-known protective factors for breastfeeding establishment [9] particularly after CS [10, 11]. Opioid analgesia, such as those in epidurals, can cross the blood brain barrier in the fetus and affect feeding reflexes [12]. Additionally, it is hypothesised that oxytocin infusions desensitise oxytocin receptors in the breast, weakening the milk-ejection reflex [13].
Australia, similar to other high-income countries, has seen rapid rises in rates of intervention use [14]. In Victoria in 2019, 37.2% of women had a CS, 40.1% used epidural analgesia and 46.6% had labour either induced or augmented, rates that have significantly increased from previous decades [15]. So far, studies assessing the impact of such birth interventions on breastfeeding show mixed results. Though various studies have associated these interventions with unfavourable early breastfeeding outcomes, few explore the ongoing impact on breastfeeding. In particular, the impact of receiving multiple interventions on breastfeeding outcomes in hospital is poorly considered. Identification of women at increased risk of early discontinuation of breastfeeding would enable provision of targeted breastfeeding supports for these women so that the benefits of breastfeeding are not lost to the increasing iatrogenesis in maternity care.
In this study, we aimed to explore the association between CS, epidural analgesia, and synthetic oxytocin infusion, both individually and when used in combination, and short and longer-term breastfeeding outcomes.
Methods
Data sources and study population
This retrospective population-based cohort study used deidentified data from the Victorian Perinatal Data Collection (VPDC), a validated dataset [16] of routinely collected state-wide information for every birth in Victoria, Australia, of ≥20 weeks’ gestation (or ≥ 400 g birth weight if gestation is unknown). Variables include mode of birth, type of intrapartum analgesia, use of oxytocin infusions in labour, initiation of breastfeeding, use of infant formula in hospital and feeding status at discharge from hospital. We analysed all singleton term livebirths at ≥37 weeks gestation whose mother initiated breastfeeding in hospital between 1 January 2010 and 31 December 2018. Breastfeeding initiation refers to whether the baby was put to the breast at least once or whether any attempt was made to express breastmilk during the hospital stay.
A subset of this population, namely those term singleton livebirths born between 1 January 2015 and 31 December 2017, were linked to the Child Development Information System (CDIS) containing information on infant feeding status at 3-month and 6-months. These dates were chosen because of the availability of linked data within this timeframe. The CDIS is a centralised dataset reporting ongoing breastfeeding outcomes through the Maternal and Child Health (MCH) service. The MCH service is a universal primary health service that provides all Victorian families with 10 consultations with MCH nurses between birth and school age, with additional as required. At each consultation parents report their child’s feeding status as exclusively breastfeed, partially breastfed or formula-fed. The most recent total participation rates for the MCH service were shown to be 94.1% at 4-months and 85.8% at 8-months [17], when parents report their child’s feeding status at 3-months and 6-months, respectively. Almost all Local Government Areas reported their MCH information to CDIS by the study period, 2015–17, enabling linkage with births in 2015–17. The linkage was conducted by the Centre for Victorian Data Linkage based on a concordance of predetermined identifiers.
Outcomes, exposures and covariates
The primary short-term breastfeeding outcomes were formula supplementation in hospital, defined as breast-fed babies receiving any amount of formula during the initial hospital stay, and last feed at the breast, defined as having the last feed before hospital discharge directly and exclusively from the breast, and therefore excludes expressed breast milk. These were assessed using the total study population.
The primary long-term breastfeeding outcomes were breastfeeding status at 3-months and 6-months of age, which was recorded as either exclusive, any or no breastfeeding. Exclusive breastfeeding is defined as receiving only breastmilk as the source of nutrition and includes expressed breast milk. Any breastfeeding includes receiving any breastmilk, in addition to artificial milk sources, water-based drinks or solid food. Long-term breastfeeding outcomes were assessed using the linked VPDC-CDIS dataset sub-study population for births in 2015–17.
The exposure variables were four intrapartum interventions: pre-labour CS, in-labour CS, epidural analgesia, and synthetic oxytocin infusion. Method of birth was categorised as either pre-labour CS, in-labour CS, or vaginal birth. Epidural analgesia included epidural block, spinal block and combined spinal/epidural block used to relieve pain in labour. We did not assess epidural anaesthesia provided de novo to facilitate operative birth because of the brief fetal exposure. Synthetic oxytocin infusion includes that which was used for induction and/or augmentation of labour.
Several covariates were assessed. These included socioeconomic status, parity (primiparous, multiparous), hospital admissions status (public, private), birthweight (< 2500 g, 2500-3999 g, ≥4000 g), maternal region of birth, maternal age, maternal body mass index (BMI), smoking status during pregnancy, marital status (married, de facto, single), and gestation at birth. Socioeconomic status was defined using the Socio-Economic Indexes for Areas (SEIFA) indices [18]. The indices are based on information from the five-yearly Census of Population and Housing and are divided into quintiles, with 1 being the most disadvantaged and 5 being the least disadvantaged. The SEIFA used here is based on the smallest available residential neighbourhood level (SA1). Maternal region of birth was classified by the Standard Australian Classification of Countries (SACC) [19]. Marital status information was available for the total population but not for the linked VPDC-CDIS sub-population.
Analyses
We first described the rates of intrapartum interventions and breastfeeding outcomes in our populations. Categorical variables were reported as absolute numbers and percentages and compared using Pearson’s Chi-square test. To assess the association between each intervention and breastfeeding outcomes, we then performed univariable and multivariable logistic regression models to obtain adjusted odds ratios (aOR) with 95% confidence intervals (CI), adjusting for available confounders. Given that the use of each intervention was not always mutually exclusive, each intrapartum intervention was first assessed regardless of whether other interventions were also used, then each was assessed when used in isolation, and finally cumulatively. A two-tailed P-value of < 0.05 was deemed statistically significant.
Missing data were excluded case-wise. Data were missing for 8676 (1.4%) cases regarding formula supplementation in hospital, 3808 (0.6%) cases regarding last feed at breast and 41 cases (< 0.1%) regarding method of birth. There was no missing data on epidural analgesia and synthetic oxytocin infusion. Data were missing for < 0.1% of mothers regarding parity, maternal age, sex of baby and hospital admission status, 53,029 (8.9%) cases regarding smoking status, 39,181 (6.5%) cases regarding maternal BMI, 7744 (1.3%) cases regarding marital status, 37,224 (6.2%) cases regarding SEIFA quintile, and 3681 (0.6%) cases regarding country of birth region. Within the linked population, feeding status information was missing for 16,269 (15.4%) of infants at 3-months and 10,072 (9.5%) of infants at 6-months. A ‘missing’ category was created for covariates with substantial missing data in order to include cases with valid data on other variables in multivariable analyses.
Statistical analyses were performed using Statistical Package for the Social Science Version 26 (SPSS, IBM Corp., Armonk, New York, USA) and Stata SE Version 16 (Stata, 2020, release 16, StataCorp, Texas, USA).
Results
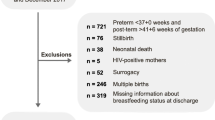
Breastfeeding was initiated by 95.1% (n = 599,191) of all singleton livebirths at ≥37 weeks gestation in hospital between 2010 and 2018. Thus, our total study population was n = 599,191Of these, 197,775 infants were born between 2015 and 2017, of which 105,599 (53.4%) of infants had VPDC data that linked to long-term feeding status in the CDIS dataset. The characteristics of the total population and the restricted population with linked long-term breastfeeding outcomes were largely similar, though infants in the linked population were more likely to be born at 37 weeks and in a private hospital, mothers were more likely to have a higher SES and less likely to have smoked in pregnancy (Table 1).
Within the total birth population, 19.1% (n = 114,251) had a pre-labour CS, 12.8% (n = 76,516) had an in-labour CS, 26.1% (n = 156,395) had epidural analgesia and 31.0% (n = 185,628) had synthetic oxytocin infusion (augmentation and/or induction of labour). Overall, 38.0% (n = 227,499) had none of the assessed interventions, 40.4% had one (n = 242,083), 16.4% had two (n = 98,158) and 5.2% (n = 31,451) had all three intrapartum interventions. The demographic information of women within each intervention group is presented in Table 2. Intervention use was more common among primiparous women, with the exception of pre-labour CS, where significantly more women were multiparous compared to primiparous (72.2% vs 27.8%, P < 0.001). Intervention use was also more common with increasing SEIFA quintile, at private hospitals and with increasing maternal BMI (all P < 0.001). Infant gestational age and birth weight was relatively similar for all groups, except for pre-labour CS, where infants were born approximately 1 week earlier than those born by vaginal birth or in-labour CS.
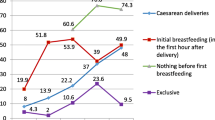
Formula supplementation was used by 28.2% (n = 166,642) of infants in hospital and 78.2% (n = 465,695) of infants had their last feed at the breast. The proportion of infants who had formula in hospital was significantly higher following in-labour CS and pre-labour CS compared to vaginal birth (41.7 and 38.0% vs 23.0%, both P < 0.001), following epidural compared to no epidural (35.4% vs 25.7%, P < 0.001) and following oxytocin infusion compared to no oxytocin infusion (33.3% vs 25.9%, P < 0.001) (Table 3). As the number of interventions received increased, the proportion of infants who received formula in hospital increased, from 18.0% for women who had none of the assessed interventions to 45.7% for women who had all three interventions (P < 0.001). The inverse was true for receiving the last feed before discharge directly at the breast.
In adjusted analyses, all interventions were significantly associated with less favourable breastfeeding outcomes in hospital, including when separated into mutually exclusive groups (Table 3). In-labour CS was the strongest predictor of formula supplementation in hospital (aOR 1.96, 95% CI 1.93–1.99), followed by pre-labour CS (aOR 1.75, 95% CI 1.72–1.77), epidural analgesia (aOR 1.45, 95% CI 1.43–1.47) and then oxytocin infusion (aOR 1.24, 95% CI 1.22–1.26). When performed in isolation, both pre-labour CS and in-labour CS equally predicted formula supplementation (aOR 2.17, 95% CI 2.13–2.21 and aOR 2.17, 95% CI 2.10–2.24). There was a dose response relationship between the number of interventions received and formula supplementation in hospital. Compared to no interventions, having one (aOR 1.77, 95% CI 1.74–1.79), two (aOR 2.08, 95% CI 2.04–2.12) or all three (aOR 2.90 95% CI 2.83–2.98) interventions significantly increased the odds of formula supplementation in hospital. The inverse was true for receiving the last feed before discharge directly at the breast.
In the linked population, 52.4% (n = 46,703) and 14.5% (n = 13,713) were exclusively breastfeeding at 3-months and 6-months, respectively, and 70.8% (n = 63,088) and 55.4% (n = 52,400) of mothers were breastfeeding at all at 3-months and 6-months, respectively. Exclusive and any breastfeeding were less common at each time point for those who received each intervention compared to those who did not. After adjusting for confounders, each intervention remained associated with less favourable breastfeeding outcomes at 3-months and 6-months, and this persisted when the interventions were explored as mutually exclusive groups (Table 4a, b). The association was strongest for women who had pre-labour CS, which decreased the odds of exclusive and any breastfeeding at 3 months (aOR 0.73, 95% CI 0.71–0.76 and aOR 0.70, 95% CI 0.68–0.73, respectively); and of exclusive and any breastfeeding at 6 months (aOR 0.81, 95% CI 0.77–0.86 and aOR 0.72, 95% CI 0.69–0.74, respectively). There was a dose-response relationship between number of interventions received and the adjusted odds of exclusive and any breastfeeding at 3-months and 6-months.
Discussion
In this study we demonstrated that the use of each of the intrapartum interventions investigated was associated with less favourable breastfeeding outcomes, both in hospital and in the months after birth. The associations persisted when each intervention was assessed independently from other interventions in mutually exclusive groups. In-labour CS was the strongest predictor of formula supplementation in hospital, though pre-labour CS was the strongest predictor of not breastfeeding at 3 and 6-months. Importantly, the associations increased in strength with increasing number of interventions received in a dose-response fashion. These findings suggest the need for targeted breastfeeding support in hospital and after discharge for women who receive these intrapartum interventions.
The use of intrapartum interventions was common in our study, with nearly two thirds of women receiving at least one intervention. This was not surprising given rates of intrapartum intervention use have rapidly increased in Australia over the last decade [15]. This highlights the need for greater discussion about limiting intervention use when not medically indicated or necessary. Moreover, women should be well-informed about the potential risks vs benefits of having an intervention to aid in shared and informed decision-making during birth. Alongside this, despite all women in our study population initiating breastfeeding, rates of formula supplementation in hospital were high and discontinuation of exclusive and any breastfeeding in the months after birth was common. Only one in two infants were exclusively breastfeeding at 3-months, and this decreased to one in seven infants at 6-months. These rates fall far short of the national targets for breastfeeding, such as those produced by the Australian National Breastfeeding Strategy, which aim for 40% of infants to be exclusively breastfeeding until around 6 months of age by 2022 [20] and international targets set by the World Health Organisation for at least 50% of infants to be exclusively breastfeeding to 6 months by 2025 [21].
The finding that each intrapartum intervention increased the likelihood of formula supplementation in hospital and decreased the likelihood of exclusive breastfeeding at discharge is in keeping with the results of several studies [22,23,24]. Novel to our findings, however, is that even when used in isolation, each intervention still negatively affected early breastfeeding outcomes. The underlying explanation for these findings is likely to be multifactorial. In respect to pre-labour CS, it has been suggested that the absence of labour may interfere with normal hormonal changes required for successful lactation [25]. However we observed that in-labour CS was a stronger predictor of less favourable early breastfeeding outcomes than pre-labour CS. This suggests that the stress and pain associated with operative birth also plays a role, possibly related to post-partum opiate pain relief, reduced skin-to-skin contact and poor mobility [26]. Physiologically, both fentanyl in epidural analgesia and synthetic oxytocin have the potential to transfer to the fetal circulation and depress newborn feeding behaviours, [12, 27] which is a key reason for formula supplementation in hospital [2]. Each intervention has also been shown to interfere with the normal production of lactation hormones, oxytocin and prolactin [28]. Despite these proposed mechanisms, some studies have found no association between each intervention and early breastfeeding outcomes [29,30,31]. Interestingly, these studies tend to be conducted in hospitals accredited under the Baby Friendly Hospital Initiative, a program that encourages breastfeeding [32], and include populations of women who have strong intentions to breastfeed. Our findings recommend the need for enhanced breastfeeding support following intervention use for women birthing in hospitals without such initiatives and facilitators.
Importantly, we also found that each intervention decreased the odds of exclusive and any breastfeeding at 3-months and 6-months when compared to no intervention. Of note, associations between each intervention and exclusive breastfeeding at 6-month were weak compared to other long-term breastfeeding outcomes. This may be because many infants commence solid food introduction by 6-months of age. Exclusive breastfeeding at 6-months of age is therefore not necessarily the most appropriate indicator of ongoing breastfeeding success in the local setting. While many studies have associated intervention use with reduced long-term breastfeeding success [22, 24, 33], others have contrastingly found no impact [29, 34, 35]. The complex nature of ongoing feeding choices likely explains such varied findings; attitudes towards breastfeeding and intervention use differ significantly across the globe, as does the availability of ongoing supports and return-to-work policies. Our findings of reduced long-term breastfeeding in women who underwent interventions are unlikely to be entirely a direct physiological consequence of the interventions themselves. Rather, they will be explained, at least in part, by the well-known associations between successful establishment of breastfeeding and long-term breastfeeding maintenance [2]. In particular, women who successfully initiate breastfeeding immediately after birth are more likely to sustain that breastfeeding when their child is 6-months old [2]. This highlights the importance of optimising early and ongoing breastfeeding support for mothers who have multiple interventions given their long-term association with breastfeeding success. Such supports may include increased uptake of the Baby Friendly Hospital Initiative in hospitals around Australia and improved access to professional and lay lactation support, such as MCH nurses, lactation consultants, the Australian Breastfeeding Association and peer-support [7].
To our knowledge, our study is the first to demonstrate a dose-response relationship between increasing numbers of interventions used and the odds of receiving formula in hospital. This relationship persisted for breastfeeding outcomes in the months after birth, where increasing numbers of intrapartum interventions were associated with decreased odds of both exclusive and any breastfeeding at 3-months and 6-months, which is consistent with other studies [36, 37]. These results are important because intervention use often occurs in a cascade, with more than one in five women in the present study receiving multiple interventions during birth. The dose-response relationship may be explained by amplification of the physiological burden when interventions are used in combination, the fact that women who have multiple interventions are more likely to have complicated births, and that women who opt for intervention use, at least when done so electively, may be less concerned about having “unnatural” feeding sources.
This study is strengthened by its use of linked population-level data that has strong statistical power and is representative of all births in Victoria, Australia, eliminating selection bias. The VPDC dataset has been reported as having high accuracy in internal validation studies [16]. There are important limitations. Firstly, the CDIS dataset has not had any validation studies. Second, as an observational study, we were not able to adjust for all potential confounders of breastfeeding success. One important confounder that was not accounted for was return to work commitments for women, which is known to influence long-term infant feeding choices [38,39,40]. We also had no information about previous breastfeeding experience, indication for the intrapartum interventions or indication for formula supplementation in hospital, all of which may influence feeding methods in hospital and after discharge. We did not have access to data about admission to special care nursey or neonatal intensive care unit after birth. Nonetheless, we know that factors such as Apgar score and SCN/NICU admission likely lie on the causal pathway between intervention use and breastfeeding outcome. While only half of infants in the sub-study population had information regarding long-term feeding status, this was not unexpected. Some families do not attend the MCH consultations where feeding status is obtained, either because infants born in Victoria live interstate or have moved elsewhere and are not eligible to receive MCH consultations, or because parents choose not to participate. The movement of MCH data from state Local Government Areas to the centralised CDIS database has been gradual, and between 2015 and 2017, several Local Government Areas had not reported MCH data to the centralised database. Some of the infants born between 2015 and 2017 also would not have reached 4 or 8 months by the end of data collection and so feeding status for these time points would not have been available. Nonetheless, our restricted linked population was shown to be similar in many characteristics as the total Victorian infant population, indicating that the sub-study population can be considered representative of the total birth population Due to the exclusion of pre-term births and multiple births, the findings of our study are not generalisable to these groups. Future studies that examine the impact of intrapartum interventions on primiparous women, pre-term births and multiple births, would further the understanding of this topic.
Conclusion
Women who have intrapartum interventions, particularly multiple interventions, are at increased risk of less favourable early and long-term breastfeeding outcomes, and therefore should be carefully considered for additional breastfeeding support, if they wish to breastfeed. Limiting intrapartum interventions when not medically indicated or necessary while ensuring women remain informed about potential risks is essential.
Availability of data and materials
This study is based on Victorian population perinatal and developmental data. These data do not belong to the authors but to the Consultative Council on Obstetric and Paediatric Mortality and Morbidity and the Municipal Association of Victoria, respectively. The authors are not permitted to share them, except in aggregate (as, for example, in a publication). However, interested parties can obtain the deidentified data on which this study is based by submitting a research protocol to the Victorian Agency for Health Information Data Request Hub at: https://vahi.freshdesk.com/support/home.
Abbreviations
- aOR:
-
Adjusted Odds Ratio
- CCOPMM:
-
Consultative Council on Obstetric and Paediatric Mortality and Morbidity
- CDIS:
-
Child Development Information System
- CS:
-
Caesarean Section
- CI:
-
Confidence Interval
- MCH:
-
Maternal and Child Health
- SEIFA:
-
Socio-Economic Indexes for Areas
- SACC:
-
Standard Australian Classification of Countries
- WHO:
-
World Health Organisation
- VPDC:
-
Victorian Perinatal Data Collection
References
National Health and Medical Research Council. Infant Feeding Guidelines. Canberra: National Health and Medical Research Council; 2012.
Chantry CJ, Dewey KG, Peerson JM, Wagner EA, Nommsen-Rivers LA. In-hospital formula use increases early breastfeeding cessation among first-time mothers intending to exclusively breastfeed. J Pediatr. 2014;164(6):1339–45 e5.
Hunt RW, Ryan-Atwood TE, Davey M-A, Gaston J, Wallace E, Anil S, et al. Victorian perinatal service performance indicators: 2018–19. Melbourne: Safer Care Victoria, Victorian Government; 2019.
Australian Institute of Health and Welfare. 2010 Australian National Infant Feeding Survey: Indicator results Canberra, ACT: AIHW; 2011.
Amir LH, Donath S. A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy Childbirth. 2007;7:9.
Amir LH, Donath SM. Socioeconomic status and rates of breastfeeding in Australia: evidence from three recent national health surveys. Med J Aust. 2008;189(5):254–6.
Forster DA, McLardie-Hore FE, McLachlan HL, Davey MA, Grimes HA, Dennis CL, et al. Proactive peer (mother-to-mother) breastfeeding support by telephone (ringing up about breastfeeding early [RUBY]): a multicentre, unblinded, randomised controlled trial. EClinicalMedicine. 2019;8:20–8.
Matthiesen AS, Ransjo-Arvidson AB, Nissen E, Uvnas-Moberg K. Postpartum maternal oxytocin release by newborns: effects of infant hand massage and sucking. Birth. 2001;28(1):13–9.
Cooijmans KHM, Beijers R, Rovers AC, de Weerth C. Effectiveness of skin-to-skin contact versus care-as-usual in mothers and their full-term infants: study protocol for a parallel-group randomized controlled trial. BMC Pediatr. 2017;17(1):154.
Stevens J, Schmied V, Burns E, Dahlen H. Immediate or early skin-to-skin contact after a caesarean section: a review of the literature. Matern Child Nutr. 2014;10(4):456–73.
Hung KJ, Berg O. Early skin-to-skin after cesarean to improve breastfeeding. MCN Am J Matern Child Nurs. 2011;36(5):318–24.
Beilin Y, Bodian CA, Weiser J, Hossain S, Arnold I, Feierman DE, et al. Effect of labor epidural analgesia with and without fentanyl on infant breast-feeding: a prospective, randomized, double-blind study. Anesthesiology. 2005;103(6):1211–7.
Odent MR. Synthetic oxytocin and breastfeeding: reasons for testing an hypothesis. Med Hypotheses. 2013;81(5):889–91.
OECD. Health at a Glace 2019: OECD Indicators: Paris OECD Publishing; 2019. https://doi.org/10.1787/4dd50c09-en.
Consultative Council on Obstetric and Paediatric Mortality and Morbidity. Victoria's Mothers, Babies and Children: 2019; Supplementary tables - births. Melbourne: safer care Victoria, Victorian Government 2021.
Flood MM, McDonald SJ, Pollock WE, Davey MA. Data accuracy in the Victorian perinatal data collection: results of a validation study of 2011 data. Health Inf Manag. 2017;46(3):113–26.
Department of Health and Human Services. Maternal & Child Health Services Annual Report: 2017–18. Melbourne Victoria State Government; 2019.
Pink B. Socio-economic indexes for areas (SEIFA) 2011 technical paper. Canberra: Australian Bureau of Statistics; 2013.
Australian Bureau of Statistics. Standard Australian classification of countries (SACC): Second Edition Canberra: Australian Bureau of Statistics,; 2008 [Available from: https://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/9A9C459F46EF3076CA25744B0015610A/$File/12690_Second%20Edition.pdf.
COAG Health Council. The Australian National Breastfeeding Strategy: 2019 and beyond. Canberra: ACT: COAG Health Council; 2019.
World Health Organization. Breastfeeding - WHO response Geneva, Switzerland: World Health Organisation,; 2022 [Available from: https://www.who.int/health-topics/breastfeeding#tab=tab_3.
Chen C, Yan Y, Gao X, Xiang S, He Q, Zeng G, et al. Influences of cesarean delivery on breastfeeding practices and duration: a prospective cohort study. J Hum Lact. 2018;34(3):526–34.
Wiklund I, Norman M, Uvnas-Moberg K, Ransjo-Arvidson AB, Andolf E. Epidural analgesia: breast-feeding success and related factors. Midwifery. 2009;25(2):e31–8.
Garcia-Fortea P, Gonzalez-Mesa E, Blasco M, Cazorla O, Delgado-Rios M, Gonzalez-Valenzuela MJ. Oxytocin administered during labor and breast-feeding: a retrospective cohort study. J Matern Fetal Neonatal Med. 2014;27(15):1598–603.
Nissen E, Uvnas-Moberg K, Svensson K, Stock S, Widstrom AM, Winberg J. Different patterns of oxytocin, prolactin but not cortisol release during breastfeeding in women delivered by caesarean section or by the vaginal route. Early Hum Dev. 1996;45(1–2):103–18.
Kealy MA, Small RE, Liamputtong P. Recovery after caesarean birth: a qualitative study of women's accounts in Victoria, Australia. BMC Pregnancy Childbirth. 2010;10:47.
Olza Fernández I, Marín Gabriel M, Malalana Martínez A, Fernández-Cañadas Morillo A, López Sánchez F, Costarelli V. Newborn feeding behaviour depressed by intrapartum oxytocin: a pilot study. Acta Paediatr. 2012;101(7):749–54.
Jonas K, Johansson LM, Nissen E, Ejdeback M, Ransjo-Arvidson AB, Uvnas-Moberg K. Effects of intrapartum oxytocin administration and epidural analgesia on the concentration of plasma oxytocin and prolactin, in response to suckling during the second day postpartum. Breastfeed Med. 2009;4(2):71–82.
Mahomed K, Wild K, Brown C, Green A. Does fentanyl epidural analgesia affect breastfeeding: a prospective cohort study. Aust N Z J Obstet Gynaecol. 2019;59(6):819–24.
Fernandez-Canadas Morillo A, Duran Duque M, Hernandez Lopez AB, Muriel Miguel C, Perez Riveiro P, Salcedo Marina A, et al. Cessation of breastfeeding in association with oxytocin administration and type of birth. A prospective cohort study. Women Birth. 2019;32(1):e43–e8.
Fernández-Cañadas Morillo A, Durán Duque M, Hernández López AB, Muriel Miguel C, Martínez Rodríguez B, Oscoz Prim A, et al. A comparison of factors associated with cessation of exclusive breastfeeding at 3 and 6 months. Breastfeed Med. 2017;12(7):430–5.
World Health Organization. Baby-Friendly Hospital Initiative: Revised, updated and expanded for integrated care Geneva, Switzerland: WHO; 2009 [Available from: https://apps.who.int/iris/bitstream/handle/10665/43593/9789241594967_eng.pdf;sequence=1.
Torvaldsen S, Roberts CL, Simpson JM, Thompson JF, Ellwood DA. Intrapartum epidural analgesia and breastfeeding: a prospective cohort study. Int Breastfeed J. 2006;1:24.
Chang ZM, Heaman MI. Epidural analgesia during labor and delivery: effects on the initiation and continuation of effective breastfeeding. J Hum Lact. 2005;21(3):305–14.
Halpern SH, Levine T, Wilson DB, MacDonell J, Katsiris SE, Leighton BL. Effect of labor analgesia on breastfeeding success. Birth. 1999;26(2):83–8.
Bai DL, Wu KM, Tarrant M. Association between intrapartum interventions and breastfeeding duration. J Midwifery Womens Health. 2013;58(1):25–32.
Dozier AM, Howard CR, Brownell EA, Wissler RN, Glantz JC, Ternullo SR, et al. Labor epidural anesthesia, obstetric factors and breastfeeding cessation. Matern Child Health J. 2013;17(4):689–98.
Xiang N, Zadoroznyj M, Tomaszewski W, Martin B. Timing of return to work and breastfeeding in Australia. Pediatrics. 2016;137(6):e20153883.
Burns E, Triandafilidis Z. Taking the path of least resistance: a qualitative analysis of return to work or study while breastfeeding. Int Breastfeed J. 2019;14:15.
Ogbuanu C, Glover S, Probst J, Liu J, Hussey J. The effect of maternity leave length and time of return to work on breastfeeding. Pediatrics. 2011;127(6):e1414–27.
Acknowledgements
We would like to thank the Consultative Council on Obstetric and Paediatric Mortality and Morbidity (CCOPMM) for providing access to the Victorian Perinatal Data Collection. The conclusions drawn from this research are those of the authors and do not necessarily align with the views of CCOPMM. We are grateful to the Victorian Centre for Data Linkage for linking the VPDC and CDIS datasets for use in this study. Thank you to Rei Irawan for providing advice about the CDIS dataset.
Funding
Roshan J Selvaratnam receives financial support from the National Stillbirth Centre of Research Excellence and the Norman Beischer Medical Research Foundation. Miranda Davies-Tuck received financial support by the National Health and Medical Research Council Centre of Research Excellence in Stillbirth.
Author information
Authors and Affiliations
Contributions
Madison S Andrew: formal analysis, data curation, writing and editing original draft visualisation, writing, reviewing and editing final manuscript, project administration, preparation of Tables 1, 2, 3 and 4. Roshan J Selvaratnam: methodology, formal analysis, data curation, writing - review and editing, project administration. Miranda Davies-Tuck: methodology, writing -review and editing, visualisation, supervision. Kim Howland: writing - review and editing, resources. Mary-Ann Davey: conceptualisation, methodology, formal analysis, data curation, writing -review and editing, visualisation, supervision, project administration. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Monash University Human Research Ethics Committee (#23936) on 1st of April 2020 and the Department of Health and Human Services, Human Research Ethics Committee (#45712) on 6th of March 2019. This study design did not require active public or patient involvement as it used routinely collected data, and therefore did not require consent to participate.
Competing interests
None declared.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Andrew, M.S., Selvaratnam, R.J., Davies-Tuck, M. et al. The association between intrapartum interventions and immediate and ongoing breastfeeding outcomes: an Australian retrospective population-based cohort study. Int Breastfeed J 17, 48 (2022). https://doi.org/10.1186/s13006-022-00492-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13006-022-00492-7