Abstract
The Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop was held on July 25 and 26, 2016 at the National Institutes of Health. The workshop brought together a diverse group of researchers including pediatric neurosurgeons, neurologists, and neuropsychologists with scientists in the fields of brain injury and development, cerebrospinal and interstitial fluid dynamics, and the blood–brain and blood–CSF barriers. The goals of the workshop were to identify areas of opportunity in posthemorrhagic hydrocephalus research and encourage scientific collaboration across a diverse set of fields. This report details the major themes discussed during the workshop and research opportunities identified for posthemorrhagic hydrocephalus. The primary areas include (1) preventing intraventricular hemorrhage, (2) stopping primary and secondary brain damage, (3) preventing hydrocephalus, (4) repairing brain damage, and (5) improving neurodevelopment outcomes in posthemorrhagic hydrocephalus.
Similar content being viewed by others
Background
The Hydrocephalus Association hosted a workshop on July 25 and 26, 2016 at the National Institutes of Health, Neuroscience Center, to build research capacity and identify areas of opportunity for research around posthemorrhagic hydrocephalus (PHH). The Hydrocephalus Association was founded in 1983 by parents of children with hydrocephalus and developed a research program in 2009. Since then the Association has committed over $7 million to research, making it the largest non-profit, non-governmental funder of hydrocephalus research in the United States. The mission of the Hydrocephalus Association is to promote a cure for hydrocephalus and improve the lives of those affected by the condition. The Association strives to accomplish this mission by collaborating with patients, caregivers, researchers and industry, raising awareness, and funding innovative, high impact research to prevent, treat, and ultimately cure hydrocephalus.
The 2016 Hydrocephalus Association PHH Workshop was developed through the Hydrocephalus Association PHH Initiative, a multiyear initiative focused on increasing research efforts focused on PHH. The workshop agenda was developed by the workshop planning committee which was led by Hydrocephalus Association staff and included both an investigator in the Hydrocephalus Clinical Research Network (HCRN) and a family member of a person with hydrocephalus. The workshop brought together a diverse group of researchers including pediatric neurosurgeons, neurologists, and neuropsychologists together with scientists in the fields of brain injury and development, cerebrospinal and interstitial fluid dynamics, and the blood–brain and blood–CSF barriers. Workshop attendees also included Hydrocephalus Association staff and family members of people affected by hydrocephalus.
The primary focus of the workshop was on PHH of prematurity, although PHH can develop at any age, including in utero, after preterm birth, and in children and adults who have had a brain hemorrhage [1]. PHH develops after intraventricular extension of a hemorrhage [intraventricular hemorrhage, (IVH)] (Fig. 1). IVH grade (I–IV) is classified according to the extension (periventricular germinal tissue, ventricle, parenchyma) of hemorrhage and presence of ventricular dilation according to the Papile scale [2]. Both the source of the hemorrhage (e.g. periventricular vs. choroid plexus) and the degree of tissue injury related to the extension of the hemorrhage are linked to outcomes. Neonatal IVH occurs in up to 25% of preterm neonates [3,4,5,6,7,8,9,10,11,12] and results in hydrocephalus in 10% of these neonates, including 25% of neonates with grade III/IV IVH [13]. 38% of neonates with PHH require long term CSF diversion; the remaining either die or do not require a permanent shunt [13].
Cranial Ultrasounds of Premature Infant after IVH. a Cranial ultrasound performed in a 5 day old 24 week gestation male showing grade IV intraventricular hemorrhage with intraventricular extension. b Cranial ultrasound performed in the same infant 12 days later showing interval development of hydrocephalus
Advances in neonatology have improved survival rates for preterm neonates in recent decades [14]. In the early 1980 s, the rates of IVH decreased from 40–50 to 20% for premature neonates < 1500 g [15, 16]. However, for premature neonates 500–750 g, the rate of IVH remained high at 40–50% [15, 17, 18], and the trend in recent years shows a relative increase in IVH rates [13, 19, 20]. In the United States, the incidence of PHH of prematurity after IVH remained steady (8–10%) between 2000 and 2010; however, annual admissions for both IVH and PHH increased approximately 60% during the same time period [13]. The increase in IVH and PHH comes despite a recent decline in overall premature birth rate between 2007 and 2010 [13, 21].
PHH of prematurity is a common form of pediatric hydrocephalus, accounting for 20% of the shunted hydrocephalus cases in the United States [22] and is associated with significant morbidity and mortality [13]. This report details the major themes and the research opportunities discussed during the 2016 Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop. The views and recommendations in this report were developed by the listed authors and subsequently distributed to all workshop attendees for commentary. All feedback was then discussed and integrated into the report.
PHH of prematurity
PHH of prematurity is a common and particularly insidious form of pediatric hydrocephalus [22]. During the workshop, an overview of our current knowledge about PHH risks, pathophysiology, and treatments was presented.
Maternal and neonatal risk and protective factors
Many maternal factors can alter the risk of IVH in premature neonates. Some protective factors are related to health care including access to prenatal care, administration of antenatal corticosteroid regimens, and cesarean delivery [23]. Maternal health care disparities likely interact with other factors such as maternal race and education level which have also been associated with risk of IVH in preterm neonates. Unexpectedly, preeclampsia has been associated with a decreased risk of IVH [23,24,25,26,27,28].
Neonates born at term rarely develop IVH or PHH [29]. For premature neonates, the risk of IVH, and subsequently PHH, increases with decreased gestational age and weight [7, 13, 14]. Furthermore, the development of PHH is directly related to IVH grade, with over 75% of PHH patients having Grade III/IV IVH [13]. Male sex is also associated with an increased risk of PHH. Prenatal infection, specifically chorioamnionitis, can increase the risk of IVH and is related to gestational age [5, 23, 30,31,32,33,34,35]. Asian ethnicity seems to be protective [36].
Physiological risk factors
Premature neonates are especially vulnerable to IVH within the subependymal germinal matrix, a highly vascularized region consisting of neural and glial precursor cells [19, 30, 37, 38]. During early development, the germinal matrix undergoes rapid cellular proliferation and angiogenesis, but the thickness of the germinal matrix peaks and subsequently declines after 24 gestational weeks and is nearly absent by 36–37 gestational weeks [3, 19, 39,40,41]. This corresponds to the time-dependent risk of developing IVH and subsequent PHH. At developmental time points when premature birth is survivable, the germinal matrix is located along the walls of the lateral ventricles, primarily within the ganglionic eminence and over the developing caudate nucleus.
In preterm neonates, the germinal matrix is susceptible to hemorrhaging due to the immaturity of the vasculature, [3, 15, 19, 39, 42, 43] and sudden fluctuations in cerebral blood flow due to respiratory and hemodynamic instability [37, 38, 44]. The combination of immature vasculature and rapid changes in cerebral blood flow may lead to rupture of the germinal matrix vasculature and IVH [3, 19, 30].
Pathophysiology of PHH
Hydrocephalus represents an alteration in fluid balance within the brain and cranial cavity. It is traditionally held that under normal conditions cerebrospinal fluid (CSF) is primarily secreted into the cerebral ventricles by the choroid plexus (site of the blood–CSF barrier) and moves via bulk flow through the ventricular system and subarachnoid space before being absorbed at the arachnoid villi/granulations although it should be noted that these develop at about week 35 and 39, respectively [45]. In addition, some fluid secretion into brain parenchyma occurs across the cerebral microvasculature (site of the blood–brain barrier) and through Virchow-Robins spaces (also recently termed the “glymphatic” system) at the surface of the cerebral cortex in animal models [46,47,48]. Parenchymal interstitial fluid also enters the cerebral ventricles across the ependymal lining [49]. CSF can also be absorbed via cranial nerve lymphatics [50,51,52] and may pass retrogradely into cerebral microvessels [53,54,55,56,57]. An increase in CSF production or reduction in CSF absorption may result in ventriculomegaly if the system cannot compensate for the changes.
Secondary injury mechanisms occur following ventriculomegaly (reviewed in [58,59,60]). A detailed discussion of these secondary mechanisms is beyond the scope of this manuscript, but they include cerebral (mostly periventricular) edema, demyelination, axonal degeneration and impaired axoplasmic transport in periventricular white matter, cerebral hypoxia and ischemia, reduced metabolite levels, altered blood–brain and blood–CSF barriers, loss of cilia and junctional complexes on ependymal cells, ependymal denudation, changes in aquaporin channels, and altered neurodevelopmental trophic factors. These cytopathologies are found in most forms of congenital and acquired hydrocephalus and most likely overlap with the pathogenetic mechanisms involved in PHH.
As detailed above, the pathophysiology of hydrocephalus is multifactorial in nature, and the precise mechanisms underlying PHH of prematurity remain unclear [3]. PHH is traditionally thought to occur due to impediments in the CSF flow or absorption pathways. Acute, obstructive hydrocephalus can occur soon after IVH and may be due to blood physically blocking the most-narrow portions of the CSF spaces, i.e. the cerebral aqueduct, the foramina of Monro, the outlets of the fourth ventricle, or the subarachnoid spaces.
Multiple theories have been proposed to explain the development of “communicating” hydrocephalus after IVH including blockage of the arachnoid villi and arachnoid granulations due to microthrombi [61] or scarring [62]. Other theories include the CSF bulk flow hypothesis and the hydrodynamic theory. These theories are based on postulated changes in pressure gradients within the CSF or CSF and vascular systems, respectively [63, 64]. Few studies, however, have been conducted to test any of these theories.
Surprisingly, there have also been very few studies addressing the impact of IVH on the choroid plexus [65]. One recent study reports CSF hypersecretion occurs after IVH in a rodent model. This hypersecretion is caused by an upregulation in choroid plexus Na/K/Cl cotransporter activity associated with Toll-like receptor 4 activation [66].
In contrast, there is much evidence that IVH damages the ependymal cells that line the cerebral ventricles. Alterations in this CSF–brain interface may impact bulk fluid flow via ciliopathy and disrupt neurodevelopment by exposing the subventricular zone to CSF. An emerging mechanism appears to involve impaired junctional proteins, such as N-cadherin and connexin that not only provide structure for the ependymal lining of the ventricles but also influence progenitor cell proliferation, migration, and differentiation [67,68,69,70]. Recent evidence from preterm neonates with PHH also indicates that the neurogenic niche is compromised following IVH [71], and this primary effect could subsequently evolve into a type of hydrocephalus ex vacuo, in which the ventricles expand subsequent to impaired neurogenesis and neuronal differentiation [71].
Current treatments for PHH of prematurity
Treatments for PHH of prematurity fall into one of three categories: temporary non-surgical, temporary surgical, and permanent surgical. Temporary non-surgical treatments, including thrombolytic agents and diuretics, have been tested [72,73,74,75,76,77]; however, none of these interventions are currently recommended for use in neonates with PHH [78]. Temporary surgical treatments include ventricular access devices (VADs), external ventricular drains (EVDs), ventriculosubgaleal (VSG) shunts, and lumbar punctures. All four temporary surgical treatments are options in the management of PHH [79]; however, lumbar puncture is only recommended for immediate short-term removal of CSF [78]. Serial lumbar punctures are not recommended [78, 80].
Emerging treatments include endoscopic lavage with early removal of IVH. In one study, Schulz et al. reported a decrease in the rates of hydrocephalus and need for permanent shunt placement [81]. However, this treatment remains under investigation and long-term outcomes remain unclear.
If hydrocephalus persists despite temporary CSF diversion, placement of a ventriculoperitoneal (VP) shunt has been the treatment of choice. VP shunting has been the mainstay of long-term surgical management of hydrocephalus for over six decades. However, VP shunts frequently fail. In children, approximately 30-50% of shunts fail within the first 2 years [82,83,84] and 80% of shunt fail within 4 years [83], necessitating revision, externalization, or removal, all of which have associated costs and complications. Endoscopic third ventriculostomy (ETV), with or without choroid plexus cauterization (ETV-CPC), is an alternative treatment option and can obviate the need for a shunt. However, for treating PHH, the success rate in children less than 1 year of age is approximately 50% [85,86,87,88,89,90]. Evaluations of long-term neurological outcomes of ETV-CPC or ETV versus shunt are ongoing.
Review of clinical trials
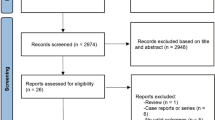
Past clinical trials inform future clinical, translational, and basic science research. The workshop, reviewed clinical trials conducted in both premature neonates and adults with intracranial hemorrhage to identify areas of promise and obstacles that limit our ability to interpret and compare results.
Interventions that alter risk of IVH
Premature and/or (extremely) low birth weight neonates are vulnerable populations at risk for multiple co-morbidities such as IVH and neurological deficits. To improve survival rates and decrease such co-morbidities, interventions based on a variety of biological mechanisms have been tested and adopted by the medical community. These interventions can be broadly grouped into antenatal interventions, birth-related procedural interventions, and postnatal interventions (Table 1).
Antenatal interventions include administration of corticosteroids, phenobarbital, magnesium sulfate, and vitamin K. Antenatal corticosteroids administration is perhaps the most established intervention and has been shown to reduce severe grades of IVH as well as reduce mortality and respiratory distress syndrome [91, 92]. In extremely premature infants, improved outcomes in neonatal mortality and neurodevelopmental outcomes were dose dependent with an indication that these results were mediated by reduced rates of severe IVH [93]. Antenatal vitamin K administration also reduced IVH risk during the first 7 days of life in a small randomized trial [94]; however, an earlier meta-analysis concluded that antenatal vitamin K did not reduce risk of IVH or improve neurodevelopmental outcomes [95]. A recent meta-analysis indicated that, antenatal magnesium sulfate did not reduce the rates of IVH in preterm infants but may have beneficial effects on the rates of moderate to severe cerebral palsy [96]. In addition, antenatal phenobarbital had no effect on IVH risk in preterm infants (NCT00009620; [97, 98]).
Procedural interventions occurring at or close to the time of birth include mode of delivery and the timing of umbilical cord clamping. In many studies comparing vaginal and cesarean deliveries in preterm and very low birth weight infants, there did not appear to be IVH risk reduction associated with one form of delivery over the other [99,100,101]. By contrast, a study showed planned cesarean delivery is associated with a reduced risk of IVH in extremely preterm infants compared to vaginal delivery and emergency cesarean delivery [102]. A study comparing both antenatal corticosteroid administration and cesarean delivery reported that antenatal corticosteroid administration independently reduced IVH risk [103]. The choice of immediate/early vs. delayed cord clamping balances the desire to have neonatologists care for the preterm infant as soon as possible compared with the thought that additional blood flow from the placenta (placental transfusion) may minimize IVH and decrease the need for subsequent transfusions. An early study and a meta-review appeared to show a reduction in IVH with delayed clamping [104, 105], although subsequent primary and meta-analysis studies showed no difference in the rate of IVH [106,107,108]. Encouraging, there may be some neurological and motor benefits to the infants when examined after 18 months [106].
Postnatal interventions that decrease the risk of IVH, but may not improve long-term neurological outcomes, include treatment with prophylactic indomethacin, ibuprofen, inositol, or ethamsylate [31, 109,110,111,112,113,114]. Early indomethacin or ibuprofen decreased IVH rates in preterm and very low birth weight infants [115,116,117,118,119,120]. In addition, indomethacin reduced the incidence of patent ductus arteriosus and the risk of severe periventricular and intraventricular hemorrhage, although rates of shunted hydrocephalus were not changed (NCT00009646; [120]). Inositol treatment reduced the risk of severe IVH as well as neonatal deaths, infant deaths, and retinopathy of prematurity [121,122,123,124,125]. In a systematic review of ethamsylate treatment in preterm and very low birth rate infants, Hunt and Hey found lower rates of IVH in treated infants who were born at less than 35 weeks gestation [113]. However, there were no differences in neonatal mortality or neurodevelopmental outcomes at 2 years.
Other postnatal interventions, such as inhaled nitrous oxide, phenobarbital, prophylactic surfactant, and corticosteroids, have had no effect on IVH rates [5, 126,127,128,129] but some were associated with other positive outcomes [5, 126, 128]. In contrast, multiple interventions for premature neonates increase the risk of IVH, which include red blood cell transfusions and rapid volume expansion [130,131,132]. Encouragingly, vitamin E supplementation in preterm infants reduces the risk of germinal matrix/intraventricular hemorrhage in a meta-analysis of 26 studies, though there was an associated higher risk of sepsis [133].
Neonatal interventions to stop development of progressive PHH
Pharmaceutical agents, drainage and irrigation of the ventricles, and temporizing devices have been tested to stop the development or progression of PHH after IVH. In these studies, the primary outcome is usually permanent shunt placement.
To date, pharmaceutical treatments have not been effective in stopping the development of PHH or its neurological disability [78, 134, 135]. These therapies include the use of diuretics to reduce CSF production [76, 77, 136] and fibrinolytic agents. The International Posthemorrhagic Ventricular Dilation (PHVD) Drug Trial Group tested acetazolamide plus furosemide treatment. In that trial, the combination resulted in higher rates of morbidity and did not decrease the need for a permanent shunt placement [76]. At the 1 year follow up, there was no difference in shunt placements but the group did report an increase in neurological morbidity [77]. A definitive Cochrane database review by Whitelaw et al. [43] and another study reported no difference in mortality or permanent shunt placement [78, 137]. Intraventricular thrombolytic agents, including recombinant tissue plasminogen activator (rtPA) [138], streptokinase [73, 75, 139], and urokinase [140], have been tested but are also not recommended for clinical use [78]. The two randomized studies testing streptokinase reported no difference in rates of shunt dependent hydrocephalus and also increased concerns about the development of meningitis and secondary IVH [75, 139].
Recently, a phase one clinical trial for the use of PNEUMOSTEM®, human umbilical cord blood derived mesenchymal stem cells, in preterm infants with grade III–IV IVH was completed. The primary outcome is unexpected death or anaphylactic shock and the secondary outcome is death or the development of shunt dependent hydrocephalus; results are pending (NCT02274428). The same group is now enrolling infants in a follow up study (NCT02673788). In related work, multiple clinical trials are underway or being analyzed to determine the effects of mesenchymal stem cells on the development of bronchopulmonary dysplasia in preterm infants (NCT01828957; NCT01897987; NCT02381366; NCT0244396).
In contrast to pharmaceutical treatments, trials that have attempted to physically wash out blood and other substances have shown more positive results [72, 141, 142]. Drainage and irrigation of the ventricles in the DRIFT (Drainage, Irrigation, and Fibrinolytic Therapy) randomized control trial did not decrease mortality or the need for permanent shunt insertion at 6 months, and the study was stopped early due to an increase the incidence of secondary intraventricular bleeding [72]. However, at 2 years, the DRIFT group had reduced rates of severe cognitive disability and death compared to the standard care group [141]. These results underscore the need for long term cognitive assessments in addition to near term outcomes such as shunt placement.
At this time, short-term temporizing procedures are often the first step in the clinical treatment of PHH, since the longevity of the condition may still be in question and, from a technical standpoint, the size of the neonate may preclude longer-term strategies such as permanent CSF shunting. Temporary surgical treatments include VADs, EVDs, VSG shunts, and lumbar punctures. Many studies have compared these treatment options but no clear results have emerged (reviewed in [78, 143, 144]). A recent prospective cohort study by the Hydrocephalus Clinical Research Network (HCRN) reported no difference in the rate of permanent shunt placement between EVDs or VSG shunts (SOPHH, NCT01480349) [145].
In future studies, morbidity, mortality, permanent shunt placement, and infection risk should all be considered as important factors. However, the timing of these interventions may have a greater impact on outcomes than the type of treatment. In one study, early treatment (based on ventricular index) with either reservoir placement or lumbar puncture was safe, effective, resulted in lower rates of permanent shunt placement, and reduced moderate-to-severe disability [146]. The results of a randomized control trial, the Early versus Late Ventricular Intervention Study (ELVIS, NCT00875758), are currently being analyzed.
Lessons from adult intracerebral and intraventricular hemorrhage clinical trials
In adults, IVH occurs as an extension of an initial intracerebral hemorrhage (ICH) with IVH occurring in about 40% of ICH cases [147, 148]. IVH size and degree of extension through the ventricular system predict poor outcomes and mortality [11, 149, 150]. Hydrocephalus develops in two-thirds of adult IVH cases and is an independent risk factor for poor neurological outcome [11, 12]. While both neonatal and adult IVH arise from parenchymal hemorrhage, the underlying causes differ between premature neonates (rupture of immature germinal matrix blood vessels) and adults (e.g., hypertension, amyloid angiopathy, anti-coagulant use; [151]). However, information from IVH in adults may inform neonatal studies.
In adults, ICH/IVH treatment has focused on three main approaches: limiting bleeding, clot removal, and reducing secondary brain injury. Hemostatic therapy (e.g., Factor VIIa, FAST trial NCT00127283; Tranexamic acid, TRAIGE trial, NCT02625948; platelet transfusion, PATCH trial, NCT02187120) and reducing blood pressure (e.g., ATACH, NCT01176565; INTERACT, NCT00716079) have undergone clinical trials to limit continued bleeding (clot expansion) in the early phase (< 24 h) after ICH. Although some of these studies have reported statistically significant effects on limiting bleeding, there has yet to be definitive evidence of improved outcomes [152,153,154,155,156,157,158,159,160].
The second therapeutic approach has centered on parenchymal or intraventricular clot removal. For ICH, standard surgical evacuation has not shown statistical benefit (e.g. STICH II trial, NCT01320423) and there is interest in using minimally invasive surgery (MIS) with or without tissue rtPA to lyse the clot (MISTIE II trial, NCT01827046; ICES trial, NCT00224770; ENRICH trial, NCT02880878) [161,162,163]. Evidence indicates that MIS is safe but whether it improves outcomes after ICH is still uncertain [162].
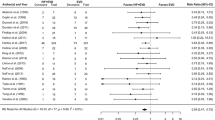
As in the premature population, a number of trials for adult ICH patients with IVH have combined EVD placement with administration of thrombolytic agents. A number of systematic meta-analyses have reported decreased mortality using this combination versus external ventricular drain (EVD) alone [164, 165]. Khan et al. [165] also reported a reduction in permanent shunt placement with the combination therapy while a non-significant reduction was reported by Gaberel et al. [164]. The recent large CLEAR III trial (NCT00784134) evaluated EVD with rtPA administration vs. EVD with saline in IVH patients. There was no significant improvement in the primary outcome measure (modified Rankin Score), but there was a significant reduction in mortality compared to EVD + saline [166]. There is debate about whether the particular thrombolytic (urokinase vs. rtPA) used to remove the clot is important [164, 165]. Two subsequent meta-analyses have been performed which include the results of the CLEAR trial [167, 168]. Wang et al. [88] reported that benefit of intraventricular thrombolysis (IVT) + EVD vs. EVD alone is limited to a reduction in mortality at the expense of an increased number of survivors with moderately-severe to severe disability; subgroup analyses did not suggest an advantage of urokinase over rtPA. In a recent meta-analysis and systematic review, Baker et al. [167] reported that intraventricular thrombolytic therapy for IVH resulted in reduced mortality and potentially better functional outcomes as measured by the modified Rankin Scale or Glasgow outcome scale.
Other newer minimally invasive approaches to adult IVH studied in small clinical trials include endoscopic surgery and controlled lumbar drainage for prevention of permanent shunt dependency. A randomized trial of combined IVT with lumbar drainage vs. IVT alone for prevention of permanent shunt dependency after ICH with severe IVH was stopped following interim analysis after 30 patients due to significant efficacy of the tested intervention [169]. A meta-analysis comparing neuroendoscopic surgery combined with EVD versus combination EVD plus IVT reported significant benefits in survival, functional outcomes, hematoma evacuation rates, and need for shunt placement in favor of endoscopic techniques [170]. These promising techniques will require large-scale validation with standardized protocols.
Compared to cerebral ischemia [171], there have been relatively few clinical trials of neuroprotectants to reduce ICH/IVH-induced secondary brain injury including hydrocephalus [151, 152]. As yet, those trials have not shown any statistical benefit. Iron, from hemoglobin, is one potential clot-derived neurotoxic factor [151]. Currently, there is a phase II clinical trial for deferoxamine, an iron chelator (iDEF; NCT02175225) and minocycline (MACH; NCT01805895, [172]), an anti-inflammatory agent that also chelates iron [173]. Additional promising therapies tested in small pilot clinical trials include fingolimod, which may reduce progression of perihematomal edema [174], and transcription factor peroxisome proliferator-activated receptor gamma (pioglitazone) which augments phagocytosis and modulates oxidative stress and inflammation (SHRINC; NCT00827892) [175].
With the exception of early clot expansion, where there is little data in the neonate, there are similarities in the approaches being examined in the adult and neonate. It is hoped that information from each age group may help in devising better ways for hematoma removal and reducing the impact of clot-induced, or derived, harmful factors.
Workshop recommendations: key areas for research and intervention
The development of PHH of prematurity involves a series of events resulting in multiple, simultaneous injury processes. Correctly predicting who is at risk, determining key time-points and targets for early interventions, and understanding the long-term effects of PHH are essential for preventing, minimizing, or reversing the development of hydrocephalus and improving long-term outcomes. During the workshop, key areas for research and interventions were identified and discussed (Fig. 2).
Early identification
To optimize clinical management, it is essential to identify the premature neonates who are at highest risk of developing IVH and subsequently PHH. This is a key area for future research (Table 2). Many demographic and physiological factors are associated with IVH and PHH, but there are currently no established predictive models of PHH [176,177,178,179,180]. Predicting IVH and PHH with a high degree of sensitivity and specificity will improve clinical management and prognostication of high risk neonates and could be an essential component in the development and testing of new therapies. Identified biomarkers may provide insights to the pathophysiology of PHH and provide new therapeutic targets to prevent or minimize the condition. These tools could also be used as selection criteria for clinical trials testing the efficacy of new therapies.
Prevention of hemorrhage
Premature neonates are uniquely susceptible to germinal matrix hemorrhage (GMH) and the germinal matrix vasculature is a major target for research (Table 3). Determining the tolerance of the germinal matrix to fluctuations in cerebral blood flow and the interplay between respiratory and cardiac instability and cerebral blood flow will help guide clinical management of premature neonates to reduce the risk of GMH. In addition, a more in depth understanding of germinal matrix development and physiology will provide new targets for prophylactic therapies aimed at strengthening or otherwise modifying the germinal matrix to make it less susceptible to hemorrhage. Determining how these therapies affect corticogenesis is a critical component and potential barrier to success.
Prevention of blood-induced injury
Once IVH occurs, blood and blood-derived products cause damage to the surrounding tissue. Developing methods to reduce such injury is a major research target (Table 4). Multiple labs have already identified key blood components, such as iron and lysophosphatidic acid (LPA), that can independently cause ventriculomegaly and progressive hydrocephalus [3, 67, 181,182,183,184,185,186]. Determining the mechanism(s) of action on both the ventricular ependyma and choroid plexus epithelia may allow the development of targeted therapies, such as iron chelation, LPA receptor antagonism, or reducing LPA production. Ependymal damage after IVH may be a cause of further injury by allowing blood and blood components direct access to underlying tissue and by affecting fluid flow within the brain [71]. As stated earlier, the choroid plexus is the site of the blood–CSF barrier and the primary site of CSF secretion. Alterations in either of these functions may exacerbate brain injury and alter fluid dynamics in the brain after IVH [66].
Careful time-series experimentation will be required to determine if there is a critical time window post-IVH in which these therapies are effective and if the timing can be achieved in a clinical setting. In addition, early blood evacuation with or without the use of thrombolytic agents may reduce damage and improve outcomes. Forthcoming results from the ELVIS trial should help clinical decision making. Active clearance of the blood clot remains a promising avenue for research. It may also be possible to speed up endogenous processes, such as macrophage clearance of the clot, that do not result in the release of additional blood products.
Prevention of secondary injury
Prevention or reduction of secondary injury processes and the damage caused by hydrocephalus are active areas of research, with multiple research targets (Table 5), and may have broad implications for preventing or minimizing the effects of hydrocephalus for many etiologies. Immediately after hemorrhage, blood coagulation begins through a cascade that activates thrombin [187, 188] and results in subarachnoid fibrosis and disruption of cerebrospinal fluid dynamics [58, 189,190,191,192,193,194]. Modulation of neuro-inflammatory pathways has thus been suggested as a strategy for mitigating the effects of IVH and potentially preventing the development of PHH. CSF levels of interleukin (IL)-1β, IL-6, IL-8, IL-18, transforming growth factor (TGF)-β1 and -β2, tumor necrosis factor (TNF)-α, and other cytokines and chemokines have all been implicated in PHH [194,195,196,197,198,199,200]. In a recent study by Habiyaremye et al. [201], XCL-1 was decreased in the CSF of neonates with PHH. Levels of CCL-19, IL-1α, IL-1β, IL-12, and CCL-3 were elevated but only absolute CCL-19 levels correlated with levels of CSF nucleated cells, neutrophils, and lymphocytes [201]. In addition, non-protein bound iron likely remains a source of injury well after the initial bleed [3, 182, 185, 202].
Recent studies have focused on reducing subarachnoid fibrosis and periventricular astrogliosis by targeting inflammatory and other signaling cascades and have had positive results in animal models [194, 203,204,205]. Other neuroprotective attempts to modulate calcium cytopathology have shown limited improvements [134, 206, 207]. As opposed to molecular targets, the results of the DRIFT trial suggest that ventricular drainage and irrigation to remove toxic substances, such as free iron and pro-inflammatory cytokines, provides long-term benefits [141]. To date, this is the only intervention that has improved outcomes in PHH in a randomized trial.
For treatment of both blood-induced injury and secondary injuries, the specificity of the compounds, mode of administration, dosing, toxicity, and proof of target engagement will become extremely important as therapies move toward first in human trials (see section: “Moving basic science discoveries into clinical practice”). The identification of potential therapeutic agents would be accelerated if appropriate in vitro preparations were developed that could be used for high-throughput screening of new or repurposed compounds.
Targeting brain fluid dynamics
IVH in premature neonates can result in altered brain fluid dynamics and hydrocephalus. Increased intracranial pressure (ICP) and hydrocephalus can cause additional damage through hypoxia, ischemia, and mechanical stress [58, 207,208,209,210,211,212,213,214]. This damage is especially apparent in white matter tracts [214,215,216,217,218,219,220,221]. Temporizing devices and permanent shunting can, at least partially, relieve these insults, but are only implemented after ventriculomegaly is apparent. Non-surgical methods that alter CSF dynamics could be used at earlier time points in isolation or later in conjunction with temporizing devices. Current targets for these interventions include pharmaceutical reduction of CSF production by the choroid plexus (reviewed in [134, 222]), increased CSF absorption (e.g., increase absorption through aquaporin channels [223,224,225], especially following IVH [226], as well as cranial nerve lymphatics [227]), and improved CSF flow (e.g., enhancement of natural processes that repair motile cilia). This list, however, also highlights the need for a better understanding of the choroid plexus response after IVH, alternative routes of CSF production and absorption, and the role of motile cilia in the development of hydrocephalus after hemorrhage. Strengthening cell–cell junctions between ependymal cells might also prevent or delay ventriculomegaly by maintaining ependymal integrity and increasing the total resistance of the ependymal layer [71, 228].
Although much research is still needed on CSF dynamics (Table 6), IVH and subsequent injury may also impact interstitial flow within the brain parenchyma. The recently proposed brain glymphatic system describes a pathway for fluid movement between CSF and brain parenchyma and within the parenchyma itself [229]. How IVH affects such movement is an important research question.
Understanding brain development and long-term outcomes after IVH
Premature neonates with Grade III or IV IVH are at a higher risk of poor neurodevelopmental and cognitive outcomes than preterm neonates without IVH or who have Grade I or II IVH [7, 230]. It is not clear if the development of progressive hydrocephalus significantly adds to this burden [30], but it is likely that the injury mechanisms involved in the development of PHH overlap with those related to neurodevelopmental and cognitive outcomes.
For the PHH population, improving long-term neurodevelopmental and cognitive outcomes is very important and should be a primary focus in clinical trials [231]. Understanding how blood products, destruction of the ependymal layer, and inflammatory processes alter brain maturation will be important for the development of rehabilitation strategies. Normalized brain development and function after therapeutic interventions could serve as additional markers of efficacy beyond the primary outcome measure of permanent shunt placement. For example, recent findings of altered CSF proteins [129,130,131, 152] and impaired adherens junctions in disrupted ventricular and subventricular zones [71] could be targeted and have long-lasting neurodevelopmental consequences. In the near term, ventricular drainage and irrigation may minimize the secondary damage that occurs soon after and in the months following a brain bleed, minimizing the need for additional therapies [141].
Improving functional outcomes is a priority for the hydrocephalus community and must become a priority in research [231]. Longitudinal clinical studies are needed to investigate the long-term neurobehavioral outcomes of PHH, ranging from the infant/toddler stage through adulthood. For patients with shunted hydrocephalus, it is important to study the longer term, cumulative effects of altered CSF dynamics along with periodic brain compression and increased ICP due to shunt malfunction on cognition and other measures of quality of life. Other areas of particular interest include the impact of non-surgical (e.g., occupational, speech, physical therapies) and surgical (CSF shunt management) treatments. For such long-term studies, the development of optimal psychometric and imaging-based instruments is a logical priority. Research priorities in relation to brain development and long-term outcomes after IVH are given in Table 7.
Improving clinical management and clinical trials
Focus on the clinical management of preterm neonates has intensified in recent years in parallel with advances in obstetrics and newborn medicine. Identifying and implementing best practices as well as testing the benefit, or lack thereof, of new techniques and therapies is an essential part of this process. However, in published work, substantial variability exists in the study populations as well as diagnosis and treatment thresholds, making comparisons between studies difficult.
Standardizing clinical protocols through quality improvement methodologies and/or clinical trials has become a priority for the field but more work needs to be done. An early report from the HCRN demonstrated substantial variation in the treatment of PHH, even within this coordinated network [232]. In 2014, evidence-based guidelines for the management of PHH were published and provided specific recommendations while also identifying larger areas of uncertainty [78]. Wellons et al. [145] recently published the results of the HCRN’s Shunting Outcomes in Post-Hemorrhagic Hydrocephalus (SOPHH), which compared two of the most common neurosurgical treatments for PHH, and, while no difference was found between the two treatments, SOPHH provides an excellent starting point for standardizing the diagnosis and treatment of PHH [145].
Study protocols also need to be standardized. Currently, research groups use different study populations and inclusion criteria (e.g., preterm vs. very preterm, low birth weight, very low birth weight, or IVH grade) as well as different diagnosis and treatment thresholds. As a first step, common classification data including gestational age at birth, weight at birth, and IVH grade should be collected in every study and, when possible, standard inclusion and exclusion criteria should be used.
Establishing standardized criteria for PHH diagnosis and treatment thresholds (e.g., physical criteria, ventricular size parameters, CSF and imaging biomarkers, etc.) will also help simplify the interpretation of comparative effectiveness research examining available treatments (e.g., CSF shunting versus ETV ± CPC) and studies testing emerging therapeutics. Outcome measures (e.g., ventriculomegaly, progressive hydrocephalus, symptomatic hydrocephalus, or permanent shunt placement) also need to be standardized and used consistently.
Standardizing clinical management and study protocols for preterm neonates is essential as new surgical and non-surgical strategies are developed. With powerful, multi-institutional and multi-dimensional clinical trial infrastructure, the collective efforts of committed investigators can be leveraged to address critical clinical questions relevant to the diagnosis and treatment of PHH over both the short- and long-term. Research priorities in relation to clinical management and clinical studies after IVH are given in Table 8.
Moving basic science discoveries into clinical practice
The workshop was designed to identify areas of opportunity and spur research efforts for PHH of prematurity, but the ultimate goal is to prevent IVH and PHH of prematurity or prevent associated brain injury. The process of moving basic science discoveries into clinical trials and then standard clinical practice, however, is slow and inefficient. During the workshop, participants identified multiple areas that could be improved and opportunities to speed up the transition from basic research to clinical trials.
Choosing the appropriate model
There is a wide range of animal models used for research in PHH of prematurity and germinal matrix hemorrhage (reviewed in [233, 234]), and no single animal model will be suitable for all biological questions. Most studies involve experimental induction of IVH in mice [67, 191, 235], rats [182, 185, 202, 236,237,238,239,240,241,242,243], rabbits [244,245,246,247,248,249,250], cats [251], dogs [252, 253], sheep [254], and pigs [255,256,257,258]. While the majority of these in vivo studies have employed intraventricular injection of whole blood or blood products, others have used alternative approaches [67, 247, 259,260,261]. In vitro models of IVH have also been used [262, 263]. Before studies begin, animal models should be reviewed to determine the model most suitable for the outcomes being measured, the clinical relevance of each model, and whether multiple animal models will be needed if the initial studies are positive [233, 234]. In addition, experimental parameters such as mode of IVH induction, intraventricular volume changes, and developmental age of animal models should be addressed when interpreting the results.
Streamlining preclinical research
There is a paucity of studies on non-surgical therapies in PHH and one goal is to increase this number and move these therapies into clinical trial. However, the literature is littered with clinical trials that proved to be costly failures. To avoid these mistakes, it is imperative that investigators conduct preclinical research at the highest standards of scientific rigor and demonstrate robust reproducibility. It is difficult for one lab or investigator to conduct all of the experiments necessary, but it is possible to streamline these efforts through the use of standardized protocols and active collaboration. In addition, publication of negative data would benefit the entire research community.
In addition to the success or failure of an experiment or series of experiments, there are other common stumbling blocks in the development of novel treatments. Many are related to the compound itself including its safety profile, metabolism, and tissue distribution. Mode of delivery can also prevent promising therapies from moving forward. On the business side, compound manufacturing, licensing, and commercialization are issues in which many investigators are not versed but can prevent a therapy from coming to market [264, 265]. Early identification of these issues can help investigators design meaningful translational studies.
Available resources for preclinical research
Private and public organizations provide useful resources to guide preclinical research. The Operation Brain Trauma Therapy (OBTT) consortium has published a framework for preclinical drug screening and could be a useful model for PHH research [266]. In addition, the National Institutes of Health (NIH) have developed general guidelines to improve scientific rigor and reproducibility (https://www.nih.gov/research-training/rigor-reproducibility/principles-guidelines-reporting-preclinical-research). The RIGOR guidelines and Stroke Therapy Academic Industry Roundtable (STAIR) recommendations have been developed for preclinical studies focused on stroke therapies [267,268,269]. These guidelines and recommendations are highly applicable to PHH research.
The National Institute of Neurological Disorders and Stroke (NINDS) has also developed programs to streamline preclinical therapeutic development (https://www.ninds.nih.gov/Current-Research/Research-Funded-NINDS/Translational-Research). For early-stage development, NINDS has created the IGNITE (Innovation Grants to Nurture Initial Translational Efforts) Program that include: (1) funding opportunities for assay development and screening potential therapeutic agents, (2) therapeutic agent characterization (pharmacokinetics, pharmacodynamics and in vivo efficacy studies for small molecules, biologics and biotechnology products and (3) the development and validation of animal models, model systems and/or pharmacodynamic markers. Additional information about this program can be found here: https://www.ninds.nih.gov/Current-Research/Research-Funded-NINDS/Translational-Research/Funding-Programs-Researchers/IGNITE.
For later-stage biologic and biotechnology products, NINDS has established the CREATE Bio (Cooperative Research to Enable and Advance Translational Enterprises for Biologics) program that includes an optimization track (agent optimizations) and a development track (IND enabling and optional small first in human Phase 1 clinical trials) funding opportunities (https://www.ninds.nih.gov/Current-Research/Research-Funded-NINDS/Translational-Research/CREATE-BIO). For later-stage drug development, NIH established the NIH Blueprint Neurotherapeutics Network (BPN) providing support for small molecule discovery and development (https://neuroscienceblueprint.nih.gov/bpdrugs/).
The Food and Drug Administration (FDA) also provides guidelines for good laboratory practices (GLP) which need to be followed for medical product development for preclinical trials (http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=58). Researchers should understand the guidelines and work with their institutions to establish GLP practices early in the drug development process. Resources are also available through the Alzheimer’s Drug Discovery Foundation that cover topics from central nervous system drug discovery through commercialization (https://www.scienceexchange.com/group/addf-access/resources#catList).
Conducting clinical trials
Conducting clinical trials in PHH of prematurity present a number unique challenges. Extreme prematurity, very low birthweight, and medical comorbidities as well as often complex social issues all contribute to the vulnerability of this population. Thus, clinical studies must be held to the highest standards of good clinical practice (GCP), institutional human research protection offices, and federal agencies such as the NIH and FDA.
Despite its high prevalence within newborn medicine and hydrocephalus in general, PHH is relatively uncommon at any individual institution. Multi-institutional platforms are therefore critical to conducting meaningful human studies research in PHH. In addition to the HA-supported HCRN, the NIH has worked to develop infrastructure for clinical studies for conditions like PHH. NINDS established the Network for Excellence in Neuroscience Clinical Trials (NeuroNext) that consists of one Clinical Coordinating Center (CCC), a Data Coordinating Center (DCC), and 25 Clinical Sites located throughout the United States (https://www.neuronext.org/). The standardized and accessible infrastructure of NeuroNext was designed to efficiently and rapidly conduct exploratory phase I and II clinical trials as well as biomarker validation studies.
Through the National Center for Advancing Translational Sciences (NCATS), the NIH also has important resources for early and late phase studies designed to repurpose drugs developed for other conditions (https://ncats.nih.gov/preclinical/repurpose). For example, the Molecular Libraries Small Molecule Repository (MLSMR) has over 350,000 compounds. Taking advantage of these resources can accelerate the process of therapy development.
Role of the Hydrocephalus Association
The HA can play a central role in accelerating hydrocephalus research by serving as a link between the two HA-supported clinical networks, the Hydrocephalus Clinical Research Network (HCRN.org) and Adult HCRN (AHCRN.org), the basic and translational researchers involved with the HA Network for Discovery Science (HANDS, HANDS.hydroassoc.org), and the patient community through the HA Patient Powered Interactive Engagement Registry (HAPPIER, hydroassoc.org/happier). HANDS is designed to support basic and translational research by directly funding research studies, building shared infrastructure, and convening workshops and conferences. HANDS is also a platform for improving communication between researchers and developing new research collaborations. HAPPIER is a patient reported database. The survey data generated through HAPPIER can be used by researchers. In addition, researchers can work with HA to send out new surveys and also to recruit patients for clinical trials. The HA will continue to develop and modify research programs to best serve the hydrocephalus research community as well as continue advocacy efforts to increase the availability of federal funding for hydrocephalus research.
Conclusions
Intraventricular hemorrhage and posthemorrhagic hydrocephalus is a potentially devastating condition in premature neonates with no effective non-surgical therapies. The Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop identified many important areas for future research to help produce a pathway for reducing the occurrence and effects of PHH.
Abbreviations
- AHCRN:
-
Adult Hydrocephalus Clinical Research Network
- BPN:
-
Blueprint Neurotherapeutics Network
- CCC:
-
Clinical Coordinating Center
- CPC:
-
choroid plexus cauterization
- CREATE Bio:
-
Cooperative Research to Enable and Advance Translational Enterprises for Biologics
- DCC:
-
Data Coordinating Center
- DRIFT:
-
Drainage, Irrigation, and Fibrinolytic Therapy
- ELVIS:
-
Early versus Late Ventricular Intervention Study
- ETV:
-
endoscopic third ventriculostomy
- CPC:
-
choroid plexus cauterization
- EVD:
-
external ventricular drain
- FDA:
-
Food and Drug Administration
- GCP:
-
good clinical practice
- HA:
-
Hydrocephalus Association
- HANDS:
-
Hydrocephalus Association Network for Discovery Science
- HAPPIER:
-
Hydrocephalus Association Patient Powered Interactive Engagement Registry
- HCRN:
-
Hydrocephalus Clinical Research Network
- ICH:
-
intracerebral hemorrhage
- ICP:
-
intracranial pressure
- IGNITE:
-
Innovation Grants to Nurture Initial Translational Efforts
- IL:
-
interleukin
- IND:
-
investigational new drug
- IVH:
-
intraventricular hemorrhage
- IVT:
-
intraventricular thrombolysis
- LPA:
-
lysophosphatidic acid
- MIS:
-
minimally invasive surgery
- MLSMR:
-
Molecular Libraries Small Molecule Repository
- NCATS:
-
National Center for Advancing Translational Sciences
- NeuroNext:
-
Network for Excellence in Neuroscience Clinical Trials
- NICHD:
-
National Institute of Child Health and Human Development
- NIH:
-
National Institutes of Health
- NINDS:
-
National Institute of Neurological Disorders and Stroke
- PATCH:
-
Pre-hospital Anti-fibrinolytics for Traumatic Coagulopathy and Haemorrhage
- PHH:
-
posthemorrhagic hydrocephalus
- PHVD:
-
posthemorrhagic ventricular dilation
- rtPA:
-
recombinant tissue plasminogen activator
- SOPHH:
-
Shunting Outcomes in Post-Hemorrhagic Hydrocephalus
- STAIR:
-
Stroke Therapy Academic Industry Roundtable
- TGF:
-
transforming growth factor
- TNF:
-
tumor necrosis factor
- VAD:
-
ventricular access device
- VSG:
-
ventriculosubgaleal
References
Rodriguez EM, Guerra MM. Neural stem cells and fetal-onset hydrocephalus. Pediatr Neurosurg. 2017;52:446–61.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
Strahle J, Garton H, Maher C, Muraszko K, Keep R, Xi G. Mechanisms of hydrocephalus after neonatal and adult intraventricular hemorrhage. Transl Stroke Res. 2012;3(Suppl 1):25–38.
Kazan S, Gura A, Ucar T, Korkmaz E, Ongun H, Akyuz M. Hydrocephalus after intraventricular hemorrhage in preterm and low-birth weight infants: analysis of associated risk factors for ventriculoperitoneal shunting. Surg Neurol. 2005;64:S77–81.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56.
Limbrick DD Jr, Mathur A, Johnston JM, Munro R, Sagar J, Inder T, Park TS, Leonard JL, Smyth MD. Neurosurgical treatment of progressive posthemorrhagic ventricular dilation in preterm infants: a 10-year single-institution study. J Neurosurg Pediatr. 2010;6:224–30.
Radic JA, Vincer M, McNeely PD. Temporal trends of intraventricular hemorrhage of prematurity in Nova Scotia from 1993 to 2012. J Neurosurg Pediatr. 2015;15:573–9.
Romero L, Ros B, Arraez MA, Rius F, Gonzalez L, Martin A, Carrasco A, Segura M. Analysis of risk factors for hydrocephalus development in newborn infants with germinal matrix hemorrhage. Minerva Pediatr. 2015;67:401–6.
Bassan H. Intracranial hemorrhage in the preterm infant: understanding it, preventing it. Clin Perinatol. 2009;36:737–62.
Murphy BP, Inder TE, Rooks V, Taylor GA, Anderson NJ, Mogridge N, Horwood LJ, Volpe JJ. Posthaemorrhagic ventricular dilatation in the premature infant: natural history and predictors of outcome. Arch Dis Child Fetal Neonatal Ed. 2002;87:F37–41.
Bhattathiri PS, Gregson B, Prasad KS, Mendelow AD, Investigators S. Intraventricular hemorrhage and hydrocephalus after spontaneous intracerebral hemorrhage: results from the STICH trial. Acta Neurochir Suppl. 2006;96:65–8.
Hwang BY, Bruce SS, Appelboom G, Piazza MA, Carpenter AM, Gigante PR, Kellner CP, Ducruet AF, Kellner MA, Deb-Sen R, et al. Evaluation of intraventricular hemorrhage assessment methods for predicting outcome following intracerebral hemorrhage. J Neurosurg. 2012;116:185–92.
Christian EA, Jin DL, Attenello F, Wen T, Cen S, Mack WJ, Krieger MD, McComb JG. Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000–2010. J Neurosurg Pediatr. 2016;17:260–9.
Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, Laptook AR, Sanchez PJ, Van Meurs KP, Wyckoff M, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314:1039–51.
Ballabh P. Intraventricular hemorrhage in premature infants—mechanism of disease. Pediatr Res. 2010;67:1–8.
Philip AG, Allan WC, Tito AM, Wheeler LR. Intraventricular hemorrhage in preterm infants: declining incidence in the 1980s. Pediatrics. 1989;84:797–801.
Jain NJ, Kruse LK, Demissie K, Khandelwal M. Impact of mode of delivery on neonatal complications: trends between 1997 and 2005. J Matern Fetal Neonatal Med. 2009;22:491–500.
Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M. Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics. 2005;115:997–1003.
Ballabh P. Pathogenesis and prevention of intraventricular hemorrhage. Clin Perinatol. 2014;41:47–67.
Sherlock RL, Anderson PJ, Doyle LW, Victorian Infant Collaborative Study G. Neurodevelopmental sequelae of intraventricular haemorrhage at 8 years of age in a regional cohort of ELBW/very preterm infants. Early Hum Dev. 2005;81:909–16.
Martin JA, Osterman MJ, Centers for Disease C, Prevention. Preterm births—United States, 2006 and 2010. MMWR Suppl. 2013;62:136–8.
Riva-Cambrin J, Kestle JR, Holubkov R, Butler J, Kulkarni AV, Drake J, Whitehead WE, Wellons JC 3rd, Shannon CN, Tamber MS, et al. Risk factors for shunt malfunction in pediatric hydrocephalus: a multicenter prospective cohort study. J Neurosurg Pediatr. 2016;17:382–90.
Shankaran S, Lin A, Maller-Kesselman J, Zhang H, O’Shea TM, Bada HS, Kaiser JR, Lifton RP, Bauer CR, Ment LR, Gene Targets for Intraventricular Hemorrhage S. Maternal race, demography, and health care disparities impact risk for intraventricular hemorrhage in preterm neonates. J Pediatr. 2014;164(1005–1011):e1003.
McCrea HJ, Ment LR. The diagnosis, management, and postnatal prevention of intraventricular hemorrhage in the preterm neonate. Clin Perinatol. 2008;35:777–92.
Gagliardi L, Rusconi F, Da Fre M, Mello G, Carnielli V, Di Lallo D, Macagno F, Miniaci S, Corchia C, Cuttini M. Pregnancy disorders leading to very preterm birth influence neonatal outcomes: results of the population-based ACTION cohort study. Pediatr Res. 2013;73:794–801.
Linder N, Haskin O, Levit O, Klinger G, Prince T, Naor N, Turner P, Karmazyn B, Sirota L. Risk factors for intraventricular hemorrhage in very low birth weight premature infants: a retrospective case–control study. Pediatrics. 2003;111:e590–5.
Kent AL, Wright IM, Abdel-Latif ME, New South W, Australian Capital Territory Neonatal Intensive Care Units Audit G. Mortality and adverse neurologic outcomes are greater in preterm male infants. Pediatrics. 2012;129:124–31.
Volpe JJ. The encephalopathy of prematurity–brain injury and impaired brain development inextricably intertwined. Semin Pediatr Neurol. 2009;16:167–78.
Szpecht D, Frydryszak D, Miszczyk N, Szymankiewicz M, Gadzinowski J. The incidence of severe intraventricular hemorrhage based on retrospective analysis of 35939 full-term newborns-report of two cases and review of literature. Childs Nerv Syst. 2016;32:2447–51.
Robinson S. Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts. J Neurosurg Pediatr. 2012;9:242–58.
Been JV, Rours IG, Kornelisse RF, Lima Passos V, Kramer BW, Schneider TA, de Krijger RR, Zimmermann LJ. Histologic chorioamnionitis, fetal involvement, and antenatal steroids: effects on neonatal outcome in preterm infants. Am J Obstet Gynecol. 2009;201(587):e581–8.
Malaeb S, Dammann O. Fetal inflammatory response and brain injury in the preterm newborn. J Child Neurol. 2009;24:1119–26.
Moscuzza F, Belcari F, Nardini V, Bartoli A, Domenici C, Cuttano A, Ghirri P, Boldrini A. Correlation between placental histopathology and fetal/neonatal outcome: chorioamnionitis and funisitis are associated to intraventricular haemorrage and retinopathy of prematurity in preterm newborns. Gynecol Endocrinol. 2011;27:319–23.
Shatrov JG, Birch SC, Lam LT, Quinlivan JA, McIntyre S, Mendz GL. Chorioamnionitis and cerebral palsy: a meta-analysis. Obstet Gynecol. 2010;116:387–92.
Soraisham AS, Singhal N, McMillan DD, Sauve RS, Lee SK, Canadian Neonatal N. A multicenter study on the clinical outcome of chorioamnionitis in preterm infants. Am J Obstet Gynecol. 2009;200(372):e371–6.
Tully HM, Traudt CM, Rue T, Oron AP, Simon TD, Kukull WA, Doherty D. Risk factors for post-hemorrhagic hydrocephalus among infants with intraventricular hemorrhage. Fluids Barriers CNS. 2015;12:O18.
du Plessis AJ. Cerebrovascular injury in premature infants: current understanding and challenges for future prevention. Clin Perinatol. 2008;35:609–41.
du Plessis AJ. The role of systemic hemodynamic disturbances in prematurity-related brain injury. J Child Neurol. 2009;24:1127–40.
Gould SJ, Howard S. Glial differentiation in the germinal layer of fetal and preterm infant brain: an immunocytochemical study. Pediatr Pathol. 1988;8:25–36.
Ballabh P, Braun A, Nedergaard M. The blood–brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol Dis. 2004;16:1–13.
Del Bigio MR. Cell proliferation in human ganglionic eminence and suppression after prematurity-associated haemorrhage. Brain. 2011;134:1344–61.
Braun A, Xu H, Hu F, Kocherlakota P, Siegel D, Chander P, Ungvari Z, Csiszar A, Nedergaard M, Ballabh P. Paucity of pericytes in germinal matrix vasculature of premature infants. J Neurosci. 2007;27:12012–24.
Whitelaw A. Intraventricular haemorrhage and posthaemorrhagic hydrocephalus: pathogenesis, prevention and future interventions. Semin Neonatol. 2001;6:135–46.
Vela-Huerta MM, Amador-Licona M, Medina-Ovando N, Aldana-Valenzuela C. Factors associated with early severe intraventricular haemorrhage in very low birth weight infants. Neuropediatrics. 2009;40:224–7.
Gomez DG, DiBenedetto AT, Pavese AM, Firpo A, Hershan DB, Potts DG. Development of arachnoid villi and granulations in man. Acta Anat. 1982;111:247–58.
Iliff JJ, Wang M, Zeppenfeld DM, Venkataraman A, Plog BA, Liao Y, Deane R, Nedergaard M. Cerebral arterial pulsation drives paravascular CSF-interstitial fluid exchange in the murine brain. J Neurosci. 2013;33:18190–9.
Ratner V, Gao Y, Lee H, Elkin R, Nedergaard M, Benveniste H, Tannenbaum A. Cerebrospinal and interstitial fluid transport via the glymphatic pathway modeled by optimal mass transport. Neuroimage. 2017;152:530–7.
Yang L, Kress BT, Weber HJ, Thiyagarajan M, Wang B, Deane R, Benveniste H, Iliff JJ, Nedergaard M. Evaluating glymphatic pathway function utilizing clinically relevant intrathecal infusion of CSF tracer. J Transl Med. 2013;11:107.
Spector R, Keep RF, Robert Snodgrass S, Smith QR, Johanson CE. A balanced view of choroid plexus structure and function: focus on adult humans. Exp Neurol. 2015;267:78–86.
Nagra G, Li J, McAllister JP 2nd, Miller J, Wagshul M, Johnston M. Impaired lymphatic cerebrospinal fluid absorption in a rat model of kaolin-induced communicating hydrocephalus. Am J Physiol Regul Integr Comp Physiol. 2008;294:R1752–9.
Koh L, Zakharov A, Johnston M. Integration of the subarachnoid space and lymphatics: is it time to embrace a new concept of cerebrospinal fluid absorption? Cerebrospinal Fluid Res. 2005;2:6.
Johnston M, Zakharov A, Papaiconomou C, Salmasi G, Armstrong D. Evidence of connections between cerebrospinal fluid and nasal lymphatic vessels in humans, non-human primates and other mammalian species. Cerebrospinal Fluid Res. 2004;1:2.
Greitz D. Radiological assessment of hydrocephalus: new theories and implications for therapy. Neuroradiol J. 2006;19:475–95.
Greitz D, Greitz T, Hindmarsh T. A new view on the CSF-circulation with the potential for pharmacological treatment of childhood hydrocephalus. Acta Paediatr. 1997;86:125–32.
Miyajima M, Arai H. Evaluation of the production and absorption of cerebrospinal fluid. Neurol Med Chir. 2015;55:647–56.
Mori E, Yamada S. A hypothesis of cerebrospinal fluid formation and absorption: from the clinical viewpoint of idiopathic normal pressure hydrocephalus. Rinsho Shinkeigaku. 2014;54:1190–2.
Hladky SB, Barrand MA. Mechanisms of fluid movement into, through and out of the brain- evaluation of the evidence. Fluids Barriers CNS. 2014;11:26.
Del Bigio MR. Cellular damage and prevention in childhood hydrocephalus. Brain Pathol. 2004;14:317–24.
McAllister JP 2nd, Williams MA, Walker ML, Kestle JR, Relkin NR, Anderson AM, Gross PH, Browd SR, Hydrocephalus Symposium Expert P. An update on research priorities in hydrocephalus: overview of the third National Institutes of Health-sponsored symposium “Opportunities for Hydrocephalus Research: Pathways to Better Outcomes”. J Neurosurg. 2015;123:1163–6.
Williams MA, McAllister JP, Walker ML, Kranz DA, Bergsneider M, Del Bigio MR, Fleming L, Frim DM, Gwinn K, Kestle JR, et al. Priorities for hydrocephalus research: report from a National Institutes of Health-sponsored workshop. J Neurosurg. 2007;107:345–57.
Hill A, Shackelford GD, Volpe JJ. A potential mechanism of pathogenesis for early posthemorrhagic hydrocephalus in the premature newborn. Pediatrics. 1984;73:19–21.
Motohashi O, Suzuki M, Yanai N, Umezawa K, Shida N, Yoshimoto T. Thrombin and TGF-beta promote human leptomeningeal cell proliferation in vitro. Neurosci Lett. 1995;190:105–8.
Greitz D. The hydrodynamic hypothesis versus the bulk flow hypothesis. Neurosurg Rev. 2004;27:299–300.
Greitz D. Paradigm shift in hydrocephalus research in legacy of Dandy’s pioneering work: rationale for third ventriculostomy in communicating hydrocephalus. Childs Nerv Syst. 2007;23:487–9.
Xiang J, Routhe LJ, Wilkinson DA, Hua Y, Moos T, Xi G, Keep RF. The choroid plexus as a site of damage in hemorrhagic and ischemic stroke and its role in responding to injury. Fluids Barriers CNS. 2017;14:8.
Karimy JK, Zhang J, Kurland DB, Theriault BC, Duran D, Stokum JA, Furey CG, Zhou X, Mansuri MS, Montejo J, et al. Inflammation-dependent cerebrospinal fluid hypersecretion by the choroid plexus epithelium in posthemorrhagic hydrocephalus. Nat Med. 2017;23:997–1003.
Yung YC, Mutoh T, Lin ME, Noguchi K, Rivera RR, Choi JW, Kingsbury MA, Chun J. Lysophosphatidic acid signaling may initiate fetal hydrocephalus. Sci Transl Med. 2011;3:99ra87.
Guerra M, Henzi R, Ortloff A, Lictin N, Vio K, Jiminez AJ, Dominguez-Pinos MD, Gonzalez C, Bioch MCJ, Hinostroza F, et al. A cell junction pathology of neural stem cells is associated with ventricular zone disruption, hydrocephalus and abnormal neurogenesis. J Neuropathol Exp Neurol. 2015;74:653–71.
Rodriguez EM, Guerra MM, Vio K, Gonzalez C, Ortloff A, Batiz LF, Rodriguez S, Jara MC, Munoz RI, Ortega E, et al. A cell junction pathology of neural stem cells leads to abnormal neurogenesis and hydrocephalus. Biol Res. 2012;45:231–42.
Jimenez AJ, Garcia-Verdugo JM, Gonzalez CA, Batiz LF, Rodriguez-Perez LM, Paez P, Soriano-Navarro M, Roales-Bujan R, Rivera P, Rodriguez S, et al. Disruption of the neurogenic niche in the subventricular zone of postnatal hydrocephalic hyh mice. J Neuropathol Exp Neurol. 2009;68:1006–20.
McAllister JP, Guerra MM, Ruiz LC, Jimenez AJ, Dominguez-Pinos D, Sival D, den Dunnen W, Morales DM, Schmidt RE, Rodriguez EM, Limbrick DD. Ventricular zone disruption in human neonates with intraventricular hemorrhage. J Neuropathol Exp Neurol. 2017;76:358–75.
Whitelaw A, Evans D, Carter M, Thoresen M, Wroblewska J, Mandera M, Swietlinski J, Simpson J, Hajivassiliou C, Hunt LP, Pople I. Randomized clinical trial of prevention of hydrocephalus after intraventricular hemorrhage in preterm infants: brain-washing versus tapping fluid. Pediatrics. 2007;119:e1071–8.
Whitelaw A, Odd DE. Intraventricular streptokinase after intraventricular hemorrhage in newborn infants. Cochrane Database Syst Rev. 2007;4:CD000498.
Whitelaw A, Rivers RP, Creighton L, Gaffney P. Low dose intraventricular fibrinolytic treatment to prevent posthaemorrhagic hydrocephalus. Arch Dis Child. 1992;67:12–4.
Yapicioglu H, Narli N, Satar M, Soyupak S, Altunbasak S. Intraventricular streptokinase for the treatment of posthaemorrhagic hydrocephalus of preterm. J Clin Neurosci. 2003;10:297–9.
Group IPDT. International randomised controlled trial of acetazolamide and furosemide in posthaemorrhagic ventricular dilatation in infancy. International PHVD Drug Trial Group. Lancet. 1998;352:433–40.
Kennedy CR, Ayers S, Campbell MJ, Elbourne D, Hope P, Johnson A. Randomized, controlled trial of acetazolamide and furosemide in posthemorrhagic ventricular dilation in infancy: follow-up at 1 year. Pediatrics. 2001;108:597–607.
Mazzola CA, Choudhri AF, Auguste KI, Limbrick DD Jr, Rogido M, Mitchell L, Flannery AM, Pediatric Hydrocephalus Systematic R, Evidence-Based Guidelines Task F. Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: management of posthemorrhagic hydrocephalus in premature infants. J Neurosurg Pediatr. 2014;14(Suppl 1):8–23.
Perlman JM, Lynch B, Volpe JJ. Late hydrocephalus after arrest and resolution of neonatal post-hemorrhagic hydrocephalus. Dev Med Child Neurol. 1990;32:725–9.
Chaplin ER, Goldstein GW, Myerberg DZ, Hunt JV, Tooley WH. Posthemorrhagic hydrocephalus in the preterm infant. Pediatrics. 1980;65:901–9.
Schulz M, Buhrer C, Pohl-Schickinger A, Haberl H, Thomale UW. Neuroendoscopic lavage for the treatment of intraventricular hemorrhage and hydrocephalus in neonates. J Neurosurg Pediatr. 2014;13:626–35.
Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J Jr, Haines S, Schiff SJ, Cochrane DD, Steinbok P, MacNeil N. Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery. 1998;43:294–303.
Kestle JR, Drake JM, Cochrane DD, Milner R, Walker ML, Abbott R III, Boop FA. Lack of benefit of endoscopic ventriculoperitoneal shunt insertion: a multicenter randomized trial. J Neurosurg. 2003;98:284–90.
Naftel RP, Safiano NA, Falola MI, Shannon CN, Wellons JC 3rd, Johnston JM Jr. Technology preferences among caregivers of children with hydrocephalus. J Neurosurg Pediatr. 2013;11:26–36.
Stone SS, Warf BC. Combined endoscopic third ventriculostomy and choroid plexus cauterization as primary treatment for infant hydrocephalus: a prospective North American series. J Neurosurg Pediatr. 2014;5:439–46.
Zandian A, Haffner M, Johnson J, Rozzelle CJ, Tubbs RS, Loukas M. Endoscopic third ventriculostomy with/without choroid plexus cauterization for hydrocephalus due to hemorrhage, infection, Dandy–Walker malformation, and neural tube defect: a meta-analysis. Childs Nerv Syst. 2014;30:571–8.
Kulkarni AV, Riva-Cambrin J, Browd SR, Drake JM, Holubkov R, Kestle JR, Limbrick DD, Rozzelle CJ, Simon TD, Tamber MS, et al. Endoscopic third ventriculostomy and choroid plexus cauterization in infants with hydrocephalus: a retrospective Hydrocephalus Clinical Research Network study. J Neurosurg Pediatr. 2014;14:224–9.
Wang S, Stone S, Weil AG, Fallah A, Warf BC, Ragheb J, Bhatia S, Kulkarni AV. Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization: a propensity score-matched cohort and survival analysis. J Neurosurg Pediatr. 2017;19:585–91.
Chamiraju P, Bhatia S, Sandberg DI, Ragheb J. Endoscopic third ventriculostomy and choroid plexus cauterization in posthemorrhagic hydrocephalus of prematurity. J Neurosurg Pediatr. 2014;13:433–9.
Warf BC, Campbell JW, Riddle E. Initial experience with combined endoscopic third ventriculostomy and choroid plexus cauterization for post-hemorrhagic hydrocephalus of prematurity: the importance of prepontine cistern status and the predictive value of FIESTA MRI imaging. Childs Nerv Syst. 2011;27:1063–71.
Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2017;3:CD004454.
Deshmukh M, Patole S. Antenatal corticosteroids for neonates born before 25 weeks—a systematic review and meta-analysis. PLoS ONE. 2017;12:e0176090.
Chawla S, Natarajan G, Shankaran S, Pappas A, Stoll BJ, Carlo WA, Saha S, Das A, Laptook AR, Higgins RD, et al. Association of neurodevelopmental outcomes and neonatal morbidities of extremely premature infants with differential exposure to antenatal steroids. JAMA Pediatr. 2016;170:1164–72.
El-Ganzoury MM, El-Farrash RA, Saad AA, Ali MS, El-Bhbiti AR, Selem AM. Antenatal administration of vitamin K1: relationship to vitamin K-dependent coagulation factors and incidence rate of periventricular-intraventricular hemorrhage in preterm infants; Egyptian randomized controlled trial. J Matern Fetal Neonatal Med. 2014;27:816–20.
Crowther CA, Crosby DD, Henderson-Smart DJ. Vitamin K prior to preterm birth for preventing neonatal periventricular haemorrhage. Cochrane Database Syst Rev. 2010;1:CD000229.
Zeng X, Xue Y, Tian Q, Sun R, An R. Effects and safety of magnesium sulfate on neuroprotection: a meta-analysis based on PRISMA guidelines. Medicine. 2016;95:e2451.
Shankaran S, Papile LA, Wright LL, Ehrenkranz RA, Mele L, Lemons JA, Korones SB, Stevenson DK, Donovan EF, Stoll BJ, et al. The effect of antenatal phenobarbital therapy on neonatal intracranial hemorrhage in preterm infants. N Engl J Med. 1997;337:466–71.
Crowther CA, Crosby DD, Henderson-Smart DJ. Phenobarbital prior to preterm birth for preventing neonatal periventricular haemorrhage. Cochrane Database Syst Rev. 2010;1:CD000164.
Barzilay E, Gadot Y, Koren G. Safety of vaginal delivery in very low birthweight vertex singletons: a meta-analysis. J Matern Fetal Neonatal Med. 2016;29:3724–9.
Riskin A, Riskin-Mashiah S, Bader D, Kugelman A, Lerner-Geva L, Boyko V, Reichman B. Delivery mode and severe intraventricular hemorrhage in single, very low birth weight, vertex infants. Obstet Gynecol. 2008;112:21–8.
Wylie BJ, Davidson LL, Batra M, Reed SD. Method of delivery and neonatal outcome in very low-birthweight vertex-presenting fetuses. Am J Obstet Gynecol. 2008;198:640.e641–7 (discussion e641–644).
Humberg A, Hartel C, Paul P, Hanke K, Bossung V, Hartz A, Fasel L, Rausch TK, Rody A, Herting E, et al. Delivery mode and intraventricular hemorrhage risk in very-low-birth-weight infants: observational data of the German Neonatal Network. Eur J Obstet Gynecol Reprod Biol. 2017;212:144–9.
Hubner ME, Ramirez R, Burgos J, Dominguez A, Tapia JL. Mode of delivery and antenatal steroids and their association with survival and severe intraventricular hemorrhage in very low birth weight infants. J Perinatol. 2016;36:832–6.
Mercer JS, Vohr BR, McGrath MM, Padbury JF, Wallach M, Oh W. Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late-onset sepsis: a randomized, controlled trial. Pediatrics. 2006;117:1235–42.
Rabe H, Diaz-Rossello JL, Duley L, Dowswell T. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev. 2012;8:CD003248.
Mercer JS, Erickson-Owens DA, Vohr BR, Tucker RJ, Parker AB, Oh W, Padbury JF. Effects of placental transfusion on neonatal and 18 month outcomes in preterm infants: a randomized controlled trial. J Pediatr. 2016;168(50–55):e51.
Tarnow-Mordi W, Morris J, Kirby A, Robledo K, Askie L, Brown R, Evans N, Finlayson S, Fogarty M, Gebski V, et al. Delayed versus immediate cord clamping in preterm infants. N Engl J Med. 2017;377:2445–55.
Fogarty M, Osborn DA, Askie L, Seidler AL, Hunter K, Lui K, Simes J, Tarnow-Mordi W. Delayed vs early umbilical cord clamping for preterm infants: a systematic review and meta-analysis. Am J Obstet Gynecol. 2018;218:1–18.
Dani C, Poggi C, Bertini G, Pratesi S, Di Tommaso M, Scarselli G, Rubaltelli FF. Method of delivery and intraventricular haemorrhage in extremely preterm infants. J Matern Fetal Neonatal Med. 2010;23:1419–23.
Fulkerson DH, Vachhrajani S, Bohnstedt BN, Patel NB, Patel AJ, Fox BD, Jea A, Boaz JC. Analysis of the risk of shunt failure or infection related to cerebrospinal fluid cell count, protein level, and glucose levels in low-birth-weight premature infants with posthemorrhagic hydrocephalus. J Neurosurg Pediatr. 2011;7:147–51.
Linder N, Bello R, Hernandez A, Rosen C, Birk E, Sirota L, Pushkov Y, Klinger G. Treatment of patent ductus arteriosus: indomethacin or ibuprofen? Am J Perinatol. 2010;27:399–404.
Garay RP, Chiavaroli C, Hannaert P. Therapeutic efficacy and mechanism of action of ethamsylate, a long-standing hemostatic agent. Am J Ther. 2006;13:236–47.
Hunt R, Hey E. Ethamsylate for the prevention of morbidity and mortality in preterm or very low birth weight infants. Cochrane Database Syst Rev. 2010;1:CD004343.
Liebowitz M, Clyman RI. Antenatal betamethasone: a prolonged time interval from administration to delivery is associated with an increased incidence of severe intraventricular hemorrhage in infants born before 28 weeks gestation. J Pediatr. 2016;177(114–120):e111.
Ment LR, Vohr B, Allan W, Westerveld M, Sparrow SS, Schneider KC, Katz KH, Duncan CC, Makuch RW. Outcome of children in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics. 2000;105:485–91.
Ment LR, Oh W, Ehrenkranz RA, Philip AG, Vohr B, Allan W, Duncan CC, Scott DT, Taylor KJ, Katz KH, et al. Low-dose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial. Pediatrics. 1994;93:543–50.
Luque MJ, Tapia JL, Villarroel L, Marshall G, Musante G, Carlo W, Kattan J, Neocosur Neonatal N. A risk prediction model for severe intraventricular hemorrhage in very low birth weight infants and the effect of prophylactic indomethacin. J Perinatol. 2014;34:43–8.
Kalani M, Shariat M, Khalesi N, Farahani Z, Ahmadi S. A comparison of early ibuprofen and indomethacin administration to prevent intraventricular hemorrhage among preterm infants. Acta Med Iran. 2016;54:788–92.
Johnston PG, Gillam-Krakauer M, Fuller MP, Reese J. Evidence-based use of indomethacin and ibuprofen in the neonatal intensive care unit. Clin Perinatol. 2012;39:111–36.
Schmidt B, Davis P, Moddemann D, Ohlsson A, Roberts RS, Saigal S, Solimano A, Vincer M, Wright LL, Trial of Indomethacin Prophylaxis in Preterms I. Long-term effects of indomethacin prophylaxis in extremely-low-birth-weight infants. N Engl J Med. 2001;344:1966–72.
Hallman M, Bry K, Hoppu K, Lappi M, Pohjavuori M. Inositol supplementation in premature infants with respiratory distress syndrome. N Engl J Med. 1992;326:1233–9.
Hallman M, Jarvenpaa AL, Pohjavuori M. Respiratory distress syndrome and inositol supplementation in preterm infants. Arch Dis Child. 1986;61:1076–83.
Howlett A, Ohlsson A, Plakkal N. Inositol in preterm infants at risk for or having respiratory distress syndrome. Cochrane Database Syst Rev. 2015;2:CD000366.
Phelps DL, Ward RM, Williams RL, Nolen TL, Watterberg KL, Oh W, Goedecke M, Ehrenkranz RA, Fennell T, Poindexter BB, et al. Safety and pharmacokinetics of multiple dose myo-inositol in preterm infants. Pediatr Res. 2016;80:209–17.
Phelps DL, Ward RM, Williams RL, Watterberg KL, Laptook AR, Wrage LA, Nolen TL, Fennell TR, Ehrenkranz RA, Poindexter BB, et al. Pharmacokinetics and safety of a single intravenous dose of myo-inositol in preterm infants of 23–29 wk. Pediatr Res. 2013;74:721–9.
Barrington KJ, Finer N. Inhaled nitric oxide for respiratory failure in preterm infants. Cochrane Database Syst Rev. 2010;12:CD000509.
Whitelaw A, Odd D. Postnatal phenobarbital for the prevention of intraventricular hemorrhage in preterm infants. Cochrane Database Syst Rev. 2007;4:CD001691.
Soll R, Ozek E. Prophylactic protein free synthetic surfactant for preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2010;1:CD001079.
Halliday HL, Ehrenkranz RA, Doyle LW. Early (< 8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev. 2010;1:CD001146.
Baer VL, Lambert DK, Henry E, Snow GL, Butler A, Christensen RD. Among very-low-birth-weight neonates is red blood cell transfusion an independent risk factor for subsequently developing a severe intraventricular hemorrhage? Transfusion. 2011;51:1170–8.
Volpe JJ. Neurology of the newborn. Philadelphia: Saunder Elsevier; 2008.
Christensen RD, Baer VL, Lambert DK, Ilstrup SJ, Eggert LD, Henry E. Association, among very-low-birthweight neonates, between red blood cell transfusions in the week after birth and severe intraventricular hemorrhage. Transfusion. 2014;54:104–8.
Brion LP, Bell EF, Raghuveer TS. Vitamin E supplementation for prevention of morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2003;4:CD003665.
Del Bigio MR, Di Curzio DL. Nonsurgical therapy for hydrocephalus: a comprehensive and critical review. Fluids Barriers CNS. 2016;13:3.
Shooman D, Portess H, Sparrow O. A review of the current treatment methods for posthaemorrhagic hydrocephalus of infants. Cerebrospinal Fluid Res. 2009;6:1.
Libenson MH, Kaye EM, Rosman NP, Gilmore HE. Acetazolamide and furosemide for posthemorrhagic hydrocephalus of the newborn. Pediatr Neurol. 1999;20:185–91.
Whitelaw A, Kennedy CR, Brion LP. Diuretic therapy for newborn infants with posthemorrhagic ventricular dilatation. Cochrane Database Syst Rev. 2001;2:CD002270.
Whitelaw A, Saliba E, Fellman V, Mowinckel MC, Acolet D, Marlow N. Phase I study of intraventricular recombinant tissue plasminogen activator for treatment of posthaemorrhagic hydrocephalus. Arch Dis Child Fetal Neonatal Ed. 1996;75:F20–6.
Luciano R, Velardi F, Romagnoli C, Papacci P, De Stefano V, Tortorolo G. Failure of fibrinolytic endoventricular treatment to prevent neonatal post-haemorrhagic hydrocephalus. A case-control trial. Childs Nerv Syst. 1997;13:73–6.
Hudgins RJ, Boydston WR, Hudgins PA, Morris R, Adler SM, Gilreath CL. Intrathecal urokinase as a treatment for intraventricular hemorrhage in the preterm infant. Pediatr Neurosurg. 1997;26:281–7.
Whitelaw A, Jary S, Kmita G, Wroblewska J, Musialik-Swietlinska E, Mandera M, Hunt L, Carter M, Pople I. Randomized trial of drainage, irrigation and fibrinolytic therapy for premature infants with posthemorrhagic ventricular dilatation: developmental outcome at 2 years. Pediatrics. 2010;125:e852–8.
Whitelaw A, Pople I, Cherian S, Evans D, Thoresen M. Phase 1 trial of prevention of hydrocephalus after intraventricular hemorrhage in newborn infants by drainage, irrigation, and fibrinolytic therapy. Pediatrics. 2003;111:759–65.
Badhiwala JH, Hong CJ, Nassiri F, Hong BY, Riva-Cambrin J, Kulkarni AV. Treatment of posthemorrhagic ventricular dilation in preterm infants: a systematic review and meta-analysis of outcomes and complications. J Neurosurg Pediatr. 2015;16(5):545–55.
Whitelaw A, Lee-Kelland R. Repeated lumbar or ventricular punctures in newborns with intraventricular haemorrhage. Cochrane Database Syst Rev. 2017;4:CD000216.
Wellons JC 3rd, Shannon CN, Holubkov R, Riva-Cambrin J, Kulkarni AV, Limbrick DD Jr, Whitehead W, Browd S, Rozzelle C, Simon TD, et al. Shunting outcomes in posthemorrhagic hydrocephalus: results of a Hydrocephalus Clinical Research Network prospective cohort study. J Neurosurg Pediatr. 2017;20:19–29.
de Vries LS, Liem KD, van Dijk K, Smit BJ, Sie L, Rademaker KJ, Gavilanes AW, Dutch Working Group of Neonatal N. Early versus late treatment of posthaemorrhagic ventricular dilatation: results of a retrospective study from five neonatal intensive care units in The Netherlands. Acta Paediatr. 2002;91:212–7.
Hanley DF. Intraventricular hemorrhage: severity factor and treatment target in spontaneous intracerebral hemorrhage. Stroke. 2009;40:1533–8.
Gregson BA, Broderick JP, Auer LM, Batjer H, Chen XC, Juvela S, Morgenstern LB, Pantazis GC, Teernstra OP, Wang WZ, et al. Individual patient data subgroup meta-analysis of surgery for spontaneous supratentorial intracerebral hemorrhage. Stroke. 2012;43:1496–504.
Tuhrim S, Horowitz DR, Sacher M, Godbold JH. Volume of ventricular blood is an important determinant of outcome in supratentorial intracerebral hemorrhage. Crit Care Med. 1999;27:617–21.
Andrews CO, Engelhard HH. Fibrinolytic therapy in intraventricular hemorrhage. Ann Pharmacother. 2001;35:1435–48.
Keep RF, Hua Y, Xi G. Intracerebral haemorrhage: mechanisms of injury and therapeutic targets. Lancet Neurol. 2012;11:720–31.
Thabet AM, Kottapally M, Hemphill JC 3rd. Management of intracerebral hemorrhage. Handb Clin Neurol. 2017;140:177–94.
Mayer SA, Brun NC, Begtrup K, Broderick J, Davis S, Diringer MN, Skolnick BE, Steiner T, Investigators FT. Efficacy and safety of recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2008;358:2127–37.
Qureshi AI, Palesch YY, Suarez JI. Intensive blood-pressure lowering in cerebral hemorrhage. N Engl J Med. 2016;375:e48.
Morotti A, Brouwers HB, Romero JM, Jessel MJ, Vashkevich A, Schwab K, Afzal MR, Cassarly C, Greenberg SM, Martin RH, et al. Intensive blood pressure reduction and spot sign in intracerebral hemorrhage: a secondary analysis of a randomized clinical trial. JAMA Neurol. 2017;74:950–60.
Morotti A, Boulouis G, Romero JM, Brouwers HB, Jessel MJ, Vashkevich A, Schwab K, Afzal MR, Cassarly C, Greenberg SM, et al. Blood pressure reduction and noncontrast CT markers of intracerebral hemorrhage expansion. Neurology. 2017;89:548–54.
Delcourt C, Sato S, Zhang S, Sandset EC, Zheng D, Chen X, Hackett ML, Arima H, Hata J, Heeley E, et al. Intracerebral hemorrhage location and outcome among INTERACT2 participants. Neurology. 2017;88:1408–14.
Delcourt C, Zheng D, Chen X, Hackett M, Arima H, Hata J, Heeley E, Al-Shahi Salman R, Woodward M, Huang Y, et al. Associations with health-related quality of life after intracerebral haemorrhage: pooled analysis of INTERACT studies. J Neurol Neurosurg Psychiatry. 2017;88:70–5.
Wang X, Arima H, Al-Shahi Salman R, Woodward M, Heeley E, Stapf C, Lavados PM, Robinson T, Huang Y, Wang J, et al. Rapid blood pressure lowering according to recovery at different time intervals after acute intracerebral hemorrhage: pooled analysis of the INTERACT studies. Cerebrovasc Dis. 2015;39:242–8.
Baharoglu MI, Cordonnier C, Al-Shahi Salman R, de Gans K, Koopman MM, Brand A, Majoie CB, Beenen LF, Marquering HA, Vermeulen M, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016;387:2605–13.
Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM, Investigators SI. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013;382:397–408.
Hanley DF, Thompson RE, Muschelli J, Rosenblum M, McBee N, Lane K, Bistran-Hall AJ, Mayo SW, Keyl P, Gandhi D, et al. Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open-label, phase 2 trial. Lancet Neurol. 2016;15:1228–37.
Vespa P, Hanley D, Betz J, Hoffer A, Engh J, Carter R, Nakaji P, Ogilvy C, Jallo J, Selman W, et al. ICES (Intraoperative Stereotactic Computed Tomography-Guided Endoscopic Surgery) for brain hemorrhage: a multicenter randomized controlled trial. Stroke. 2016;47:2749–55.
Gaberel T, Magheru C, Parienti JJ, Huttner HB, Vivien D, Emery E. Intraventricular fibrinolysis versus external ventricular drainage alone in intraventricular hemorrhage: a meta-analysis. Stroke. 2011;42:2776–81.
Khan NR, Tsivgoulis G, Lee SL, Jones GM, Green CS, Katsanos AH, Klimo P Jr, Arthur AS, Elijovich L, Alexandrov AV. Fibrinolysis for intraventricular hemorrhage: an updated meta-analysis and systematic review of the literature. Stroke. 2014;45:2662–9.
Hanley DF, Lane K, McBee N, Ziai W, Tuhrim S, Lees KR, Dawson J, Gandhi D, Ullman N, Mould WA, et al. Thrombolytic removal of intraventricular haemorrhage in treatment of severe stroke: results of the randomised, multicentre, multiregion, placebo-controlled CLEAR III trial. Lancet. 2017;389:603–11.
Baker AD, Rivera Perla KM, Yu Z, Dlugash R, Avadhani R, Mould WA, Ziai W, Thompson RE, Staykov D, Hanley DF. Fibrinolytic for treatment of intraventricular hemorrhage: a meta-analysis and systematic review. Int J Stroke. 2018;13:11–23.
Wang D, Liu J, Norton C, Liu M, Selim M. Local fibrinolytic therapy for intraventricular hemorrhage: a meta-analysis of randomized controlled trials. World Neurosurg. 2017;107(1016–1024):e1011.
Staykov D, Kuramatsu JB, Bardutzky J, Volbers B, Gerner ST, Kloska SP, Doerfler A, Schwab S, Huttner HB. Efficacy and safety of combined intraventricular fibrinolysis with lumbar drainage for prevention of permanent shunt dependency after intracerebral hemorrhage with severe ventricular involvement: a randomized trial and individual patient data meta-analysis. Ann Neurol. 2017;81:93–103.
Li Y, Zhang H, Wang X, She L, Yan Z, Zhang N, Du R, Yan K, Xu E, Pang L. Neuroendoscopic surgery versus external ventricular drainage alone or with intraventricular fibrinolysis for intraventricular hemorrhage secondary to spontaneous supratentorial hemorrhage: a systematic review and meta-analysis. PLoS ONE. 2013;8:e80599.
Ginsberg MD. Neuroprotection for ischemic stroke: past, present and future. Neuropharmacology. 2008;55:363–89.
Fouda AY, Newsome AS, Spellicy S, Waller JL, Zhi W, Hess DC, Ergul A, Edwards DJ, Fagan SC, Switzer JA. Minocycline in acute cerebral hemorrhage: an early phase randomized trial. Stroke. 2017;48(10):2885–7.
Zhao F, Hua Y, He Y, Keep RF, Xi G. Minocycline-induced attenuation of iron overload and brain injury after experimental intracerebral hemorrhage. Stroke. 2011;42:3587–93.
Fu Y, Hao J, Zhang N, Ren L, Sun N, Li YJ, Yan Y, Huang D, Yu C, Shi FD. Fingolimod for the treatment of intracerebral hemorrhage: a 2-arm proof-of-concept study. JAMA Neurol. 2014;71:1092–101.
Gonzales NR, Shah J, Sangha N, Sosa L, Martinez R, Shen L, Kasam M, Morales MM, Hossain MM, Barreto AD, et al. Design of a prospective, dose-escalation study evaluating the safety of pioglitazone for hematoma resolution in intracerebral hemorrhage (SHRINC). Int J Stroke. 2013;8:388–96.
Galbreath E, Kim SJ, Park K, Brenner M, Messing A. Overexpression of TGF-beta 1 in the central nervous system of transgenic mice results in hydrocephalus. J Neuropathol Exp Neurol. 1995;54:339–49.
McAllister JP II. Experimental hydrocephalus. In: Winn HR, editor. Youmans textbook of neurological surgery, vol. 6. New York: Elsevier; 2011. p. 2002–8.
Morales DM, Townsend RR, Malone JP, Ewersmann CA, Macy EM, Inder TE, Limbrick DD Jr. Alterations in protein regulators of neurodevelopment in the cerebrospinal fluid of infants with posthemorrhagic hydrocephalus of prematurity. Mol Cell Proteom. 2012;11(M111):011973.
Morales DM, Holubkov R, Inder TE, Ahn HC, Mercer D, Rao R, McAllister JP 2nd, Holtzman DM, Limbrick DD Jr. Cerebrospinal fluid levels of amyloid precursor protein are associated with ventricular size in post-hemorrhagic hydrocephalus of prematurity. PLoS ONE. 2015;10:e0115045.
Morales DM, Silver SA, Morgan CD, Mercer D, Inder TE, Holtzman DM, Wallendorf MJ, Rao R, McAllister JPI, Limbrick DD Jr. Lumbar cerebrospinal fluid biomarkers of post-hemorrhagic hydrocephalus of prematurity—amyloid precursor protein, soluble APPα, and L1 cell adhesion molecule. Neurosurgery. 2017;80(1):82–90.
Yung YC, Stoddard NC, Mirendil H, Chun J. Lysophosphatidic acid signaling in the nervous system. Neuron. 2015;85:669–82.
Gao C, Du H, Hua Y, Keep RF, Strahle J, Xi G. Role of red blood cell lysis and iron in hydrocephalus after intraventricular hemorrhage. J Cereb Blood Flow Metab. 2014;34:1070–5.
Garton T, Keep RF, Wilkinson DA, Strahle JM, Hua Y, Garton HJ, Xi G. Intraventricular hemorrhage: the role of blood components in secondary injury and hydrocephalus. Transl Stroke Res. 2016;7(6):447–51.
Okubo S, Strahle J, Keep RF, Hua Y, Xi G. Subarachnoid hemorrhage-induced hydrocephalus in rats. Stroke. 2013;44:547–50.
Strahle JM, Garton T, Bazzi AA, Kilaru H, Garton HJ, Maher CO, Muraszko KM, Keep RF, Xi G. Role of hemoglobin and iron in hydrocephalus after neonatal intraventricular hemorrhage. Neurosurgery. 2014;75:696–705 (discussion 706).
Guo J, Chen Q, Tang J, Zhang J, Tao Y, Li L, Zhu G, Feng H, Chen Z. Minocycline-induced attenuation of iron overload and brain injury after experimental germinal matrix hemorrhage. Brain Res. 2015;1594:115–24.
Klebe D, Flores JJ, McBride DW, Krafft PR, Rolland WB, Lekic T, Zhang JH. Dabigatran ameliorates post-haemorrhagic hydrocephalus development after germinal matrix haemorrhage in neonatal rat pups. J Cereb Blood Flow Metab. 2017;37:3135–49.
Babu R, Bagley JH, Di C, Friedman AH, Adamson C. Thrombin and hemin as central factors in the mechanisms of intracerebral hemorrhage-induced secondary brain injury and as potential targets for intervention. Neurosurg Focus. 2012;32:E8.
Crews L, Wyss-Coray T, Masliah E. Insights into the pathogenesis of hydrocephalus from transgenic and experimental animal models. Brain Pathol. 2004;14:312–6.
Paul DA, Leef KH, Stefano JL. Increased leukocytes in infants with intraventricular hemorrhage. Pediatr Neurol. 2000;22:194–9.
Xue M, Del Bigio MR. Immune pre-activation exacerbates hemorrhagic brain injury in immature mouse brain. J Neuroimmunol. 2005;165:75–82.
Ballabh P, Xu H, Hu F, Braun A, Smith K, Rivera A, Lou N, Ungvari Z, Goldman SA, Csiszar A, Nedergaard M. Angiogenic inhibition reduces germinal matrix hemorrhage. Nat Med. 2007;13:477–85.
Dummula K, Vinukonda G, Xu H, Hu F, Zia MT, Braun A, Shi Q, Wolk J, Ballabh P. Development of integrins in the vasculature of germinal matrix, cerebral cortex, and white matter of fetuses and premature infants. J Neurosci Res. 2010;88:1193–204.
Botfield H, Gonzalez AM, Abdullah O, Skjolding AD, Berry M, McAllister JPI, Logan A. Decorin prevents the development of juvenile communicating hydrocephalus. Brain. 2013;136:2842–58.
Chow LC, Soliman A, Zandian M, Danielpour M, Krueger RC Jr. Accumulation of transforming growth factor-beta2 and nitrated chondroitin sulfate proteoglycans in cerebrospinal fluid correlates with poor neurologic outcome in preterm hydrocephalus. Biol Neonate. 2005;88:1–11.
Heep A, Stoffel-Wagner B, Bartmann P, Benseler S, Schaller C, Groneck P, Obladen M, Felderhoff-Mueser U. Vascular endothelial growth factor and transforming growth factor-beta1 are highly expressed in the cerebrospinal fluid of premature infants with posthemorrhagic hydrocephalus. Pediatr Res. 2004;56:768–74.
Merhar S. Biomarkers in neonatal posthemorrhagic hydrocephalus. Neonatology. 2012;101:1–7.
Savman K, Blennow M, Hagberg H, Tarkowski E, Thoresen M, Whitelaw A. Cytokine response in cerebrospinal fluid from preterm infants with posthaemorrhagic ventricular dilatation. Acta Paediatr. 2002;91:1357–63.
Schmitz T, Heep A, Groenendaal F, Huseman D, Kie S, Bartmann P, Obladen M, Felderhoff-Muser U. Interleukin-1beta, interleukin-18, and interferon-gamma expression in the cerebrospinal fluid of premature infants with posthemorrhagic hydrocephalus–markers of white matter damage? Pediatr Res. 2007;61:722–6.
Limbrick DD Jr, Castaneyra-Ruiz L, Han RH, Berger D, McAllister JP, Morales DM. Cerebrospinal fluid biomarkers of pediatric hydrocephalus. Pediatr Neurosurg. 2017;52(6):426–35.
Habiyaremye G, Morales DM, Morgan CD, McAllister JP, CreveCoeur TS, Han RH, Gabir M, Baksh B, Mercer D, Limbrick DD Jr. Chemokine and cytokine levels in the lumbar cerebrospinal fluid of preterm infants with post-hemorrhagic hydrocephalus. Fluids Barriers CNS. 2017;14:35.
Garton T, He Y, Garton HJ, Keep RF, Xi G, Strahle JM. Hemoglobin-induced neuronal degeneration in the neonatal hippocampus after intraventricular hemorrhage. Brain Res. 2016;1635:86–94.
Aojula A, Botfield H, McAllister JP 2nd, Gonzalez AM, Abdullah O, Logan A, Sinclair A. Diffusion tensor imaging with direct cytopathological validation: characterisation of decorin treatment in experimental juvenile communicating hydrocephalus. Fluids Barriers CNS. 2016;13:9.
Klebe D, Krafft PR, Hoffmann C, Lekic T, Flores JJ, Rolland W, Zhang JH. Acute and delayed deferoxamine treatment attenuates long-term sequelae after germinal matrix hemorrhage in neonatal rats. Stroke. 2014;45:2475–9.
McAllister JP, Miller JM. Minocycline inhibits glial proliferation in the H-Tx rat model of congenital hydrocephalus. Cerebrospinal Fluid Res. 2010;7:7.
Di Curzio DL, Turner-Brannen E, Mao X, Del Bigio MR. Magnesium sulfate treatment for juvenile ferrets following induction of hydrocephalus with kaolin. Fluids Barriers CNS. 2016;13:7.
Khan OH, McPhee LC, Moddemann LN, Del Bigio MR. Calcium antagonism in neonatal rats with kaolin-induced hydrocephalus. J Child Neurol. 2007;22:1161–6.
Del Bigio MR. Neuropathology and structural changes in hydrocephalus. Dev Disabil Res Rev. 2010;16:16–22.
Del Bigio MR, Khan OH, da Silva Lopes L, Juliet PA. Cerebral white matter oxidation and nitrosylation in young rodents with kaolin-induced hydrocephalus. J Neuropathol Exp Neurol. 2012;71:274–88.
Del Bigio MR, Wilson MJ, Enno T. Chronic hydrocephalus in rats and humans: white matter loss and behavior changes. Ann Neurol. 2003;53:337–46.
Di Curzio DL, Buist RJ, Del Bigio MR. Reduced subventricular zone proliferation and white matter damage in juvenile ferrets with kaolin-induced hydrocephalus. Exp Neurol. 2013;248C:112–28.
McAllister JP 2nd. Pathophysiology of congenital and neonatal hydrocephalus. Semin Fetal Neonatal Med. 2012;17:285–94.
McAllister JP 2nd, Chovan P. Neonatal hydrocephalus. Mechanisms and consequences. Neurosurg Clin N Am. 1998;9:73–93.
Yuan W, McKinstry RC, Shimony JS, Altaye M, Powell SK, Phillips JM, Limbrick DD Jr, Holland SK, Jones BV, Rajagopal A, et al. Diffusion tensor imaging properties and neurobehavioral outcomes in children with hydrocephalus. AJNR Am J Neuroradiol. 2013;34:439–45.
Yuan W, Air E, Altaye M, Holland S, Jones B, Bierbrauer K, Mangano F. Abnormal fractional anisotropy in hydrocephalic children: a DTI study. Cerebrospinal Fluid Res. 2009;6:S14.
Eskandari R, Abdullah O, Mason C, Lloyd KE, Oeschle AN, McAllister JP 2nd. Differential vulnerability of white matter structures to experimental infantile hydrocephalus detected by diffusion tensor imaging. Childs Nerv Syst. 2014;30:1651–61.
Eskandari R, McAllister JP 2nd, Miller JM, Ding Y, Ham SD, Shearer DM, Way JS. Effects of hydrocephalus and ventriculoperitoneal shunt therapy on afferent and efferent connections in the feline sensorimotor cortex. J Neurosurg. 2004;101:196–210.
Yuan W, Deren KE, McAllister JP 2nd, Holland SK, Lindquist DM, Cancelliere A, Mason M, Shereen A, Hertzler DA, Altaye M, Mangano FT. Diffusion tensor imaging correlates with cytopathology in a rat model of neonatal hydrocephalus. Cerebrospinal Fluid Res. 2010;7:19.
Yuan W, Holland SK, Shimony JS, Altaye M, Mangano FT, Limbrick DD, Jones BV, Nash T, Rajagopal A, Simpson S, et al. Abnormal structural connectivity in the brain networks of children with hydrocephalus. Neuroimage Clin. 2015;8:483–92.
Yuan W, McAllister JP 2nd, Lindquist DM, Gill N, Holland SK, Henkel D, Rajagopal A, Mangano FT. Diffusion tensor imaging of white matter injury in a rat model of infantile hydrocephalus. Childs Nerv Syst. 2012;28:47–54.
Yuan W, McAllister JPI, Mangano FT. Neuroimaging of white matter abnormalities in pediatric hydrocephalus. J Pediatr Neuroradiol. 2013;2:119–28.
Karimy JK, Duran D, Hu JK, Gavankar C, Gaillard JR, Bayri Y, Rice H, DiLuna ML, Gerzanich V, Marc Simard J, Kahle KT. Cerebrospinal fluid hypersecretion in pediatric hydrocephalus. Neurosurg Focus. 2016;41:E10.
Uldall M, Botfield H, Jansen-Olesen I, Sinclair A, Jensen R. Acetazolamide lowers intracranial pressure and modulates the cerebrospinal fluid secretion pathway in healthy rats. Neurosci Lett. 2017;645:33–9.
Schmidt MJ, Rummel C, Hauer J, Kolecka M, Ondreka N, McClure V, Roth J. Increased CSF aquaporin-4, and interleukin-6 levels in dogs with idiopathic communicating internal hydrocephalus and a decrease after ventriculo-peritoneal shunting. Fluids Barriers CNS. 2016;13:12.
Castaneyra-Ruiz L, Gonzalez-Marrero I, Castaneyra-Ruiz A, Gonzalez-Toledo JM, Castaneyra-Ruiz M, Perez-Molto FJ, Carmona-Calero EM, Castaneyra-Perdomo A. The neuroepithelium disruption could generate autoantibodies against AQP4 and cause neuromyelitis optica and hydrocephalus. Int Sch Res Notices. 2014;2014:580572.
Sveinsdottir S, Gram M, Cinthio M, Sveinsdottir K, Morgelin M, Ley D. Altered expression of aquaporin 1 and 5 in the choroid plexus following preterm intraventricular hemorrhage. Dev Neurosci. 2014;36:542–51.
Kim H, Moore SA, Johnston MG. Potential for intranasal drug delivery to alter CSF outflow via the nasa turbinate lymphatics. Fluids Barriers CNS. 2014;11:4.
Ballabh P, Hu F, Kumarasiri M, Braun A, Nedergaard M. Development of tight junction molecules in blood vessels of germinal matrix, cerebral cortex, and white matter. Pediatr Res. 2005;58:791–8.
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, Benveniste H, Vates GE, Deane R, Goldman SA, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci Transl Med. 2012;4:147ra111.
Mukerji A, Shah V, Shah PS. Periventricular/intraventricular hemorrhage and neurodevelopmental outcomes: a meta-analysis. Pediatrics. 2015;136:1132–43.
Koschnitzky JEW, Wright JM, White M, Garzon A, Bechard J, Unguru Y, Walker M, Williams MA. Incorporating the patient voice in hydrocephalus research: translation to transform project. Hydroceph Assoc. 2017;1:1–22.
Riva-Cambrin J, Shannon CN, Holubkov R, Whitehead WE, Kulkarni AV, Drake J, Simon TD, Browd SR, Kestle JR, Wellons JC 3rd, Hydrocephalus Clinical Research N. Center effect and other factors influencing temporization and shunting of cerebrospinal fluid in preterm infants with intraventricular hemorrhage. J Neurosurg Pediatr. 2012;9:473–81.
Del Bigio MR. Future directions for therapy of childhood hydrocephalus: a view from the laboratory. Pediatr Neurosurg. 2001;34:172–81.
Balasubramaniam J, Del Bigio MR. Animal models of germinal matrix hemorrhage. J Child Neurol. 2006;21:365–71.
Zhu W, Gao Y, Chang CF, Wan JR, Zhu SS, Wang J. Mouse models of intracerebral hemorrhage in ventricle, cortex, and hippocampus by injections of autologous blood or collagenase. PLoS ONE. 2014;9:e97423.
Xue M, Del Bigio MR. Comparison of brain cell death and inflammatory reaction in three models of intracerebral hemorrhage in adult rats. J Stroke Cerebrovasc Dis. 2003;12:152–9.
Lodhia KR, Shakui P, Keep RF. Hydrocephalus in a rat model of intraventricular hemorrhage. Acta Neurochir Suppl. 2006;96:207–11.
Balasubramaniam J, Xue M, Buist RJ, Ivanco TL, Natuik S, Del Bigio MR. Persistent motor deficit following infusion of autologous blood into the periventricular region of neonatal rats. Exp Neurol. 2006;197:122–32.
Aquilina K, Chakkarapani E, Love S, Thoresen M. Neonatal rat model of intraventricular haemorrhage and post-haemorrhagic ventricular dilatation with long-term survival into adulthood. Neuropathol Appl Neurobiol. 2011;37:156–65.
Chen Z, Zhang J, Chen Q, Guo J, Zhu G, Feng H. Neuroprotective effects of edaravone after intraventricular hemorrhage in rats. Neuroreport. 2014;25:635–40.
Marinkovic I, Strbian D, Mattila OS, Abo-Ramadan U, Tatlisumak T. A novel combined model of intracerebral and intraventricular hemorrhage using autologous blood-injection in rats. Neuroscience. 2014;272:286–94.
Chen Q, Zhang J, Guo J, Tang J, Tao Y, Li L, Feng H, Chen Z. Chronic hydrocephalus and perihematomal tissue injury developed in a rat model of intracerebral hemorrhage with ventricular extension. Transl Stroke Res. 2015;6:125–32.
Gu W, Li F, Zhang W, Jia P. Expression and significance of aquaporin protein in Sprague–Dawley rats after experimental intraventricular hemorrhage. Cell Mol Biol. 2016;62:59–62.
Sugimoto T, Yasuhara A, Matsumura T. Intracranial hemorrhage following administration of sodium bicarbonate in rabbits. Brain Dev. 1981;3:297–303.
Lorenzo AV, Welch K, Conner S. Spontaneous germinal matrix and intraventricular hemorrhage in prematurely born rabbits. J Neurosurg. 1982;56:404–10.
Karwacki Z, Kowianski P, Morys J, Dziewiatkowski J, Suchorzewska J. The influence of the intraventricular hemorrhage on the intracranial pressure and hemodynamic changes in the experimental intracerebral hemorrhage in the rabbits. Folia Neuropathol. 2000;38:55–9.
Georgiadis P, Xu H, Chua C, Hu F, Collins L, Huynh C, Lagamma EF, Ballabh P. Characterization of acute brain injuries and neurobehavioral profiles in a rabbit model of germinal matrix hemorrhage. Stroke. 2008;39:3378–88.
Chua CO, Chahboune H, Braun A, Dummula K, Chua CE, Yu J, Ungvari Z, Sherbany AA, Hyder F, Ballabh P. Consequences of intraventricular hemorrhage in a rabbit pup model. Stroke. 2009;40:3369–77.
Vinukonda G, Zia MT, Bhimavarapu BB, Hu F, Feinberg M, Bokhari A, Ungvari Z, Fried VA, Ballabh P. Intraventricular hemorrhage induces deposition of proteoglycans in premature rabbits, but their in vivo degradation with chondroitinase does not restore myelination, ventricle size and neurological recovery. Exp Neurol. 2013;247:630–44.
Dohare P, Zia MT, Ahmed E, Ahmed A, Yadala V, Schober AL, Ortega JA, Kayton R, Ungvari Z, Mongin AA, Ballabh P. AMPA-kainate receptor inhibition promotes neurologic recovery in premature rabbits with intraventricular hemorrhage. J Neurosci. 2016;36:3363–77.
Rudy TA, Westergaard JL, Yaksh TL. Hyperthermia produced by simulated intraventricular hemorrhage in the cat. Exp Neurol. 1978;58:296–310.
Ment LR, Stewart WB, Duncan CC. Local cerebral glucose utilization in the beagle puppy model of intraventricular hemorrhage. J Neurosurg. 1982;57:384–9.
Johnson DL, Getson P, Shaer C, O’Donnell R. Intraventricular hemorrhage in the newborn beagle puppy. A limited model of intraventricular hemorrhage in the premature infant. Pediatr Neurosci. 1987;13:78–83.
Reynolds ML, Evans CA, Reynolds EO, Saunders NR, Durbin GM, Wigglesworth JS. Intracranial haemorrhage in the preterm sheep fetus. Early Hum Dev. 1979;3:163–86.
Farstad T, Odden JP, Bratlid D. Effect of intraventricular hemorrhage on pulmonary function in newborn piglets. Biol Neonate. 1994;66:238–46.
Mayfrank L, Kim Y, Kissler J, Delsing P, Gilsbach JM, Schroder JM, Weis J. Morphological changes following experimental intraventricular haemorrhage and intraventricular fibrinolytic treatment with recombinant tissue plasminogen activator. Acta Neuropathol. 2000;100:561–7.
Aquilina K, Hobbs C, Cherian S, Tucker A, Porter H, Whitelaw A, Thoresen M. A neonatal piglet model of intraventricular hemorrhage and posthemorrhagic ventricular dilation. J Neurosurg. 2007;107:126–36.
Tang T, Weiss MD, Borum P, Turovets S, Tucker D, Sadleir R. In vivo quantification of intraventricular hemorrhage in a neonatal piglet model using an EEG-layout based electrical impedance tomography array. Physiol Meas. 2016;37:751–64.
Alles YCJ, Greggio S, Alles RM, Azevedo PN, Xavier LL, DaCosta JC. A novel preclinical rodent model of collagenase-induced germinal matrix/intraventricular hemorrhage. Brain Res. 2010;1356:130–8.
Goddard J, Lewis RM, Alcala H, Zeller RS. Intraventricular hemorrhage–an animal model. Biol Neonate. 1980;37:39–52.
Ment LR, Stewart WB, Duncan CC, Pitt BR, Cole JS. Beagle puppy model of perinatal cerebral infarction. J Neurosurg. 1986;65:851–5.
Juliet PA, Frost EE, Balasubramaniam J, Del Bigio MR. Toxic effect of blood components on perinatal rat subventricular zone cells and oligodendrocyte precursor cell proliferation, differentiation and migration in culture. J Neurochem. 2009;109:1285–99.
Juliet PA, Mao X, Del Bigio MR. Proinflammatory cytokine production by cultured neonatal rat microglia after exposure to blood products. Brain Res. 2008;19(1210):230–9 (Epub 2008 Mar 18).
Gamo NJ, Birknow MR, Sullivan D, Kondo MA, Horiuchi Y, Sakurai T, Slusher BS, Sawa A. Valley of death: a proposal to build a “translational bridge” for the next generation. Neurosci Res. 2017;115:1–4.
Yu HW. Bridging the translational gap: collaborative drug development and dispelling the stigma of commercialization. Drug Discov Today. 2016;21:299–305.
Kochanek PM, Bramlett HM, Dixon CE, Shear DA, Dietrich WD, Schmid KE, Mondello S, Wang KK, Hayes RL, Povlishock JT, Tortella FC. Approach to modeling, therapy evaluation, drug selection, and biomarker assessments for a multicenter pre-clinical drug screening consortium for acute therapies in severe traumatic brain injury: operation brain trauma therapy. J Neurotrauma. 2016;33:513–22.
Fisher M, Feuerstein G, Howells DW, Hurn PD, Kent TA, Savitz SI, Lo EH, Group S. Update of the stroke therapy academic industry roundtable preclinical recommendations. Stroke. 2009;40:2244–50.
Stroke Therapy Academic Industry R. Recommendations for standards regarding preclinical neuroprotective and restorative drug development. Stroke. 1999;30:2752–8.
Lapchak PA, Zhang JH, Noble-Haeusslein LJ. RIGOR guidelines: escalating STAIR and STEPS for effective translational research. Transl Stroke Res. 2013;4:279–85.
Vinukonda G, Dummula K, Malik S, Hu F, Thompson CI, Csiszar A, Ungvari Z, Ballabh P. Effect of prenatal glucocorticoids on cerebral vasculature of the developing brain. Stroke. 2010;41:1766–73.
Schmitz T. Prevention of preterm birth complications by antenatal corticosteroid administration. J Gynecol Obstet Biol Reprod. 2016;45:1399–417.
Romejko-Wolniewicz E, Oleszczuk L, Zareba-Szczudlik J, Czajkowski K. Dosage regimen of antenatal steroids prior to preterm delivery and effects on maternal and neonatal outcomes. J Matern Fetal Neonatal Med. 2013;26:237–41.
Wei JC, Catalano R, Profit J, Gould JB, Lee HC. Impact of antenatal steroids on intraventricular hemorrhage in very-low-birth weight infants. J Perinatol. 2016;36:352–6.
Wapner RJ. Antenatal corticosteroids for periviable birth. Semin Perinatol. 2013;37:410–3.
Ment LR, Vohr BR, Makuch RW, Westerveld M, Katz KH, Schneider KC, Duncan CC, Ehrenkranz R, Oh W, Philip AG, et al. Prevention of intraventricular hemorrhage by indomethacin in male preterm infants. J Pediatr. 2004;145:832–4.
Ment LR, Oh W, Ehrenkranz RA, Phillip AG, Vohr B, Allan W, Makuch RW, Taylor KJ, Schneider KC, Katz KH, et al. Low-dose indomethacin therapy and extension of intraventricular hemorrhage: a multicenter randomized trial. J Pediatr. 1994;124:951–5.
Dani C, Bertini G, Pezzati M, Poggi C, Guerrini P, Martano C, Rubaltelli FF, IntraVentricular Ibuprofen Study G. Prophylactic ibuprofen for the prevention of intraventricular hemorrhage among preterm infants: a multicenter, randomized study. Pediatrics. 2005;115:1529–35.
Schulte J, Osborne J, Benson JW, Cooke R, Drayton M, Murphy J, Rennie J, Speidel B. Developmental outcome of the use of etamsylate for prevention of periventricular haemorrhage in a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2005;90:F31–5.
Benson JW, Drayton MR, Hayward C, Murphy JF, Osborne JP, Rennie JM, Schulte JF, Speidel BD, Cooke RW. Multicentre trial of ethamsylate for prevention of periventricular haemorrhage in very low birthweight infants. Lancet. 1986;2:1297–300.
Hasan SU, Potenziano J, Konduri GG, Perez JA, Van Meurs KP, Walker MW, Yoder BA, Newborns Treated With Nitric Oxide Trial G. Effect of inhaled nitric oxide on survival without bronchopulmonary dysplasia in preterm infants: a randomized clinical trial. JAMA Pediatr. 2017;171:1081–9.
Barrington KJ, Finer N, Pennaforte T, Altit G. Nitric oxide for respiratory failure in infants born at or near term. Cochrane Database Syst Rev. 2017;1:CD000399.
Smit E, Odd D, Whitelaw A. Postnatal phenobarbital for the prevention of intraventricular haemorrhage in preterm infants. Cochrane Database Syst Rev. 2013;8:CD001691.
Ma CC, Ma S. The role of surfactant in respiratory distress syndrome. Open Respir Med J. 2012;6:44–53.
Polin RA, Carlo WA, Committee on F, Newborn, American Academy of P. Surfactant replacement therapy for preterm and term neonates with respiratory distress. Pediatrics. 2014;133:156–63.
McCord FB, Curstedt T, Halliday HL, McClure G, Reid MM, Robertson B. Surfactant treatment and incidence of intraventricular haemorrhage in severe respiratory distress syndrome. Arch Dis Child. 1988;63:10–6.
Doyle LW, Ehrenkranz RA, Halliday HL. Early (< 8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database Syst Rev. 2014;5:CD001146.
Doyle LW, Ehrenkranz RA, Halliday HL. Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Database Syst Rev. 2014;5:CD001145.
Jelin AC, Salmeen K, Gano D, Burd I, Thiet MP. Perinatal neuroprotection update. F1000Res. 2016;5(F1000 Faculty Rev):1939.
Crowther CA, Middleton PF, Voysey M, Askie L, Duley L, Pryde PG, Marret S, Doyle LW, Group A. Assessing the neuroprotective benefits for babies of antenatal magnesium sulphate: an individual participant data meta-analysis. PLoS Med. 2017;14:e1002398.
Horton AL, Lai Y, Rouse DJ, Spong CY, Leveno KJ, Varner MW, Mercer BM, Iams JD, Wapner RJ, Sorokin Y, et al. Effect of magnesium sulfate administration for neuroprotection on latency in women with preterm premature rupture of membranes. Am J Perinatol. 2015;32:387–92.
Petrova A, Mehta R. Magnesium sulfate tocolysis and intraventricular hemorrhage in very preterm infants. Indian J Pediatr. 2012;79:43–7.
Szpecht D, Szymankiewicz M, Nowak I, Gadzinowski J. Intraventricular hemorrhage in neonates born before 32 weeks of gestation-retrospective analysis of risk factors. Childs Nerv Syst. 2016;32:1399–404.
Andersson O, Lindquist B, Lindgren M, Stjernqvist K, Domellof M, Hellstrom-Westas L. Effect of delayed cord clamping on neurodevelopment at 4 years of age: a randomized clinical trial. JAMA Pediatr. 2015;169:631–8.
Committee on Obstetric P. Committee Opinion No. 684: delayed umbilical cord clamping after birth. Obstet Gynecol. 2017;129:e5–10.
Committee on Obstetric Practice ACoO, Gynecologists. Committee Opinion No.543: timing of umbilical cord clamping after birth. Obstet Gynecol. 2012;120:1522–6.
Authors’ contributions
JEK wrote the initial manuscript. RFK, DDL, JPM, JAM, JS, and YCY critically revised the document and significantly contributed to the writing of select sections. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank everyone who participated in the 2016 Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop. A special thanks to the National Institutes of Health for providing the venue and Elizabeth Quartey and Lyna Merzoug for providing planning and logistical support.
Workshop Participants:
Stephen Back, MD, PhD, Oregon Health Sciences University, Andrew Baird, PhD, University of California San Diego, Praveen Ballabh, MD, New York Medical College, Christopher Batterman, Hydrocephalus Association, Craig Brown, Hydrocephalus Association, Vicki Brown, Hydrocephalus Association, Adam Chodobski, PhD, Warren Alpert Medical School of Brown University, Joanne Conover, PhD, University of Connecticut, Marc Del Bigio, MD, PhD, University of Manitoba, Amanda Garzon, MA, Hydrocephalus Association, Paul Gross, Hydrocephalus Association (Planning Committee Member), Diana Gray, MA, Hydrocephalus Association, Carolyn Harris, PhD, Wayne State University, Aisha Heath, MPA, CFRE, Hydrocephalus Association, Terrie Inder, MD, Harvard University (Planning Committee Member), Richard Keep, PhD, University of Michigan (Planning Committee Member), Jenna Koschnitzky, PhD, Hydrocephalus Association (Planning Committee Member), Maria K. Lehtinen, PhD, Boston Children’s Hospital, Harvard Medical School, David Limbrick, MD, PhD, Washington University School of Medicine (Planning Committee Member), James P. (Pat) McAllister, II, PhD, Washington University School of Medicine (Planning Committee Member), Lyna Merzoug, Hydrocephalus Association (Planning Committee Member), Laura Ment, MD, Yale School of Medicine, Jill A. Morris, PhD, NIH, NINDS (Planning Committee Member), Shenandoah (Dody) Robinson, MD, Johns Hopkins University, Joseph Scafidi, DO, Children’s National, Jennifer Strahle, MD, Washington University School of Medicine, Evan Synder, MD, PhD, Sanford Burnham Prebys Medical Discovery Institute, Joanna Szmydynger-Chodobski, PhD, Warren Alpert Medical School of Brown University, Hudson Taylor, PhD, ABPP/CN, Nationwide Children’s Hospital Research Institute, The Ohio State University, Robert Thorne, PhD, University of Wisconsin-Madison School of Pharmacy, Andrew Whitelaw, MD, PhD, University of Bristol, Guohua Xi, MD, University of Michigan, Yun Yung, PhD, Sanford Burnham Prebys Medical Discovery Institute (Planning Committee Member), John Zhang, MD, PhD, Loma Linda University, Wendy Ziai, MD, MPH, Johns Hopkins University.
Competing interests
DDL and JPM receive research funding from Medtronic, Inc., Karl Storz, Inc., and Microbot Medical, Inc. RFK is co-Editor-in-Chief of Fluids Barriers CNS.
Availability of data and materials
The full agenda and speaker abstracts can be found at http://www.hydroassoc.org/conferences-and-workshops/.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
The 2016 Hydrocephalus Association (HA) Posthemorrhagic Hydrocephalus Workshop was funded through the HA Network for Discovery Science (HANDS.hydroassoc.org).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the attendees of the 2016 Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Koschnitzky, J.E., Keep, R.F., Limbrick, D.D. et al. Opportunities in posthemorrhagic hydrocephalus research: outcomes of the Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop. Fluids Barriers CNS 15, 11 (2018). https://doi.org/10.1186/s12987-018-0096-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12987-018-0096-3