Abstract
Background
Persistent infection with high-risk human papillomavirus (HR-HPV) plays a key role in the onset of cervical cancer. This study was designed to examine the epidemiological trends and genotype distribution of HPV from 2014 to 2023 in the plateau region of Southwest China.
Methods
The findings could offer valuable insights for clinical screening of cervical cancer and the formulation of HPV vaccination policies. This retrospective study analyzed 66,000 women who received HPV-DNA testing at the First People’s Hospital of Qujing, Yunnan, China, between 2014 and 2023. The cohort consisted of 33,512 outpatients, 3,816 inpatients, and 28,672 individuals undergoing health examinations. Cervical cells were collected for DNA extraction, and PCR amplification along with Luminex xMAP technology were used to detect 27 HPV genotypes. The data analysis was conducted using GraphPad Prism and IBM SPSS Statistics 27 software.
Results
The overall HPV infection rate at the First People’s Hospital of Qujing declined from 24.92% in 2014 to 16.29% in 2023, averaging 16.02%. Specific infection rates were 18.50% among outpatients, 12.97% among inpatients, and 13.53% for health examination attendees. The predominant high-risk HPV genotypes identified were HPV52 (2.61%), HPV16 (2.06%), HPV58 (1.81%), HPV53 (1.55%), and HPV39 (1.09%). Meanwhile, the most frequent low-risk HPV genotypes were HPV6 (1.30%), HPV61 (1.21%), and HPV11 (0.85%). In HPV-positive cases, the distribution of single, double, triple, and quadruple or more infections were 79.90%, 15.17%, 3.59%, and 1.33%, respectively. The proportions of pure LR-HPV, pure HR-HPV, and mixed infections were 22.16%, 67.82%, and 10.02%, respectively. Age-specific analysis revealed a bimodal distribution of HPV infection, with the infection rate rapidly decreasing from 44.02% in the ≤ 19 age group to 19.55% in the 20–29 age group and 13.84% in the 30–39 age group, followed by a gradual increase to 14.64% in the 40–49 age group, 16.65% in the 50–59 age group, and 22.98% in the ≥ 60 age group. The coverage rates of the three available vaccines are all below 50%. The results of this study indicated a declining trend in HPV prevalence in the plateau region of Southwest China over the period from 2014 to 2023, especially in the reduction of genotypes targeted by vaccines.
Conclusion
There were significant variations in the genotypes prevalent among different age groups, years, and patient sources within the same region. The underwhelming vaccination rates emphasize the critical need for developing either a multivalent vaccine or a personalized vaccine that targets the HPV genotypes common in the Chinese population. Furthermore, vaccinating adolescents to curb HPV infection and ensuring regular cervical cancer screenings for postmenopausal women are crucial steps.
Similar content being viewed by others
Introduction
Human papillomaviruses (HPVs) are non-enveloped, double-stranded, circular DNA viruses, 8 kb in size, that infect basal keratinocytes of mucosal and cutaneous epithelia. The HPV genome consists of an upstream regulatory region (URR), a non-coding region (NCR), and eight open reading frames (ORFs) that encode major proteins. According to their approximate time of expression during the viral life cycle, the ORFs are termed early transcription regions (E6, E7, E1, E2, E4, and E5), late transcription regions (L2 and L1), and long control regions (LCRs) [1, 2]. Sustained expression of E6 and E7 is the most important and necessary mechanism underlying the development of cervical cancer. The proteins encoded by the E6 and E7 regions promote uncontrolled cellular proliferation as they inactivate the tumor suppressor proteins p53 and pRB, respectively [3]. Different pathways are affected by HPV, including the PI3K/Akt, Wnt/β-catenin, ERK/MAPK, and JAK/STAT pathways, associated with signaling by active molecules such as MEK (pMEK), ERK (pERK), and Akt (pAkt). The abnormal activation of these pathways leads eventually to the development of cancer [1]. E5 is an auxiliary oncogene, while E1 (helicase) and E2 (DNA-binding protein) are core viral proteins involved in the replication and maintenance of the genome. E4 assists with genome amplification and viral release and is one of the most highly expressed ORFs, involved in viral spread through keratin filaments. L1 and L2 are, respectively, the main and secondary structural proteins of the viral icosahedral capsid. Prophylactic HPV vaccines target the HPV major capsid L1 proteins that self-organize into empty capsid-like structures, termed virus-like particles (VLPs) [3]. As L1 is generally the most conserved ORF, its sequence is used, on the one hand, to identify HPV types. On the other hand, it also contains five highly variable fragments, each of about 10–30 codons, that encode the outward-facing ring. These rings contain the epitopes recognized by the neutralizing antibodies, which are necessary for the vaccine to induce immunity [4]. Thus, the genetic differences used to define different L1 types correspond to antigenic differences and may reflect natural selection for immune escape. The L1 protein can self-assemble into VLPs even without the assistance of L2; while these multiprotein structures can mimic the organization and conformation of authentic native viruses, they lack the viral genome, potentially yielding safer and cheaper vaccine candidates and forming the molecular basis for the development of vaccines against different HPV genotypes [5].
Prior studies have indicated that most sexually active individuals will contract at least one genital HPV infection during their lifetime [6]. So far, approximately 450 HPV genotypes have been isolated and sequenced [7]. The World Health Organization (WHO) classifies HPV types based on their cancer risk, labeling HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 59 as Group 1 carcinogens (carcinogenic to humans), HPV 68 as a Group 2 A carcinogen (probably carcinogenic to humans), and HPV types 26, 30, 34, 53, 66, 67, 69, 70, 73, 82, 85, 97, and types 5, 8 (in epidermodysplasia verruciformis patients) as Group 2B carcinogens (possibly carcinogenic to humans) [8]. HPV types are also divided into low-risk (LR-HPV) and high-risk (HR-HPV) categories, based on their potential to cause either benign or malignant lesions [9]. LR-HPV types such as 6, 11, 40, 42, 43, 44, 55, 61, and 81 typically cause benign growths on anal, perianal, and genital mucosa, known as Condyloma acuminatum (CA). Conversely, persistent infection with HR-HPV is the primary cause of cervical cancer [10], which ranks as the fourth most common cancer among women worldwide, with 97.7% of patients with cervical cancer being HPV-positive [11]. Additionally, HR-HPV infection is also linked to other cancers, including those of the head and neck, anus, oropharynx, vagina, vulva, and penis [12].
Numerous studies have shown significant differences in HPV infection rates and genotype distribution across various countries, regions, ethnic groups, and age categories. The specific age-related patterns of infection are still debated, with rates in China varying between 8.16% and 37.62% [13,14,15,16,17,18,19]. Vaccination against HPV and cervical cancer screening are universally acknowledged as the most effective, economical, and impactful strategies for preventing cervical cancer [20, 21]. Currently, three types of HPV vaccines are available on the market in China: HPV 2-Valent (Types 16, 18) Vaccine, HPV 4-Valent (Types HPV 6, 11, 16, 18) Vaccine, and HPV 9-Valent (Types HPV 6, 11, 16, 18, 31, 33, 45, 52, 58) Vaccine. However, these vaccines were developed primarily based on the epidemiological data from Western countries, which may not completely align with the needs of the Chinese population [22, 23]. However, regrettably, due to factors such as lack of awareness, limited availability, concerns about potential side effects, and high costs, the cumulative coverage of HPV vaccination in the female population between the ages of 9 and 45 years in China was 6.21% at the end of 2022, far below the WHO target of 90%. Fortunately, initiatives such as China’s “Healthy China 2030” plan and the WHO “Global Strategy to Accelerate the Elimination of Cervical Cancer” [24], are bringing increased attention to HPV vaccination and cervical cancer screening. While HPV vaccination is not yet part of China’s national immunization program, the government supports pilot projects in selected areas. Wealthier provinces like Guangdong and Jiangsu are leading the way by offering free HPV vaccinations to eligible girls and providing free HPV-DNA and Thin-Cytologic Test (TCT) screening for eligible women.
Yunnan Province, situated in the Southwestern plateau of China and neighboring countries like Myanmar, Vietnam, Laos, Thailand, and Cambodia, is known for its high altitude, less developed economy, and the coexistence of diverse ethnic groups. The region possesses an intricate cultural background, ethnic customs, and genetic diversity. Currently, there is a lack of long-term large-scale studies on HPV infection among women in this region. Through a retrospective study, our objective was to assess HPV infection data among women in this region over the past decade. This study also sought to understand the characteristics of HPV prevalence in this region, analyze changes following the introduction of vaccines, and establish baseline data for future comparisons after enhancing screening efforts and expanding HPV vaccination. Additionally, it aimed to provide scientific evidence for clinical cervical cancer screening, HPV vaccine implementation, and research and development strategies, thereby advancing the goals outlined in the “Healthy China 2030” plan and WHO “Global Strategy to Accelerate the Elimination of Cervical Cancer”.
Materials and methods
Study population
This study analyzed data from 66,000 female patients who visited the First People’s Hospital of Qujing between January 2014 and October 2023. The participants included 28,672 healthy individuals undergoing routine physical examinations, 33,512 patients from gynecological and dermato-venereological outpatient clinics, and 3,816 inpatients from various hospital departments, primarily gynecology, along with those from opportunistic screenings in other departments. The reasons for undergoing HPV testing varied and included gynecological exams, menstrual disorders, vaginitis, cervicitis, urethritis, pelvic inflammatory disease, pelvic and ovarian cysts, cervical polyps, irregular vaginal bleeding, infertility, retained miscarriage, unexplained abdominal pain, undiagnosed genital warts, cervical intraepithelial neoplasia, and other opportunistic screenings. Patients were advised to refrain from sexual activity as well as genital washing at least 48 h before sampling, and to schedule their tests outside of their menstrual periods. Since 2014, our hospital has initiated the 27-type HPV-DNA genotyping test. This retrospective study analyzed all complete and available patient data in the existing database.
Cervical specimen collection and management
Gynecologists used a speculum to access the cervix, cleaned the cervical secretions with a cotton swab, and then inserted a cervical brush (manufactured by Jiangsu Jianyou Medical Technology Co., Ltd., SuXieZhuN20182660365) into the cervical canal. The brush was rotated clockwise for 4–5 turns to ensure thorough collection of cervical cells. After collection, the brush was gently removed and placed into a collection tube filled with cell preservation solution. At the mouth of the tube, the cervical brush was broken off at the handle’s crease, leaving the brush head inside the tube. The cap was then securely tightened, the patient’s identification was attached, and the sample was transported to the laboratory at room temperature within 4 h. The samples were stored at -20 °C and processed for HPV testing within one week.
HPV DNA extraction, PCR amplification and genotyping
The HPV DNA genotyping test kit which includes DNA extraction reagents, nucleic acid amplification reagents, and hybridization reagents was purchased from Shanghai Tellgen Biotech Co., Ltd. (Registration No. 20173404697 with China Food and Drug Administration).
DNA extraction reagents were used to extract DNA from cervical exfoliated cells. Initially, the collection tube containing the cervical brush head was vigorously shaken to release the exfoliated cells from the brush. 1 mL of eluent is transferred to a 1.5 mL centrifuge tube, centrifuged at 13,000 rpm for 5 min, and the supernatant was discarded. The cell pellet was then treated with 200 µL of nucleic acid releasing agent, thoroughly mixed, and incubated at 100 °C for 15 min in a metal bath. Following another centrifugation at 13,000 rpm for 5 min, the supernatant, which now contained the DNA template, was ready for the next step of DNA amplification.
The DNA amplification system consisted of 20.8 µl, including 10.0 µl of pre-mixed PCR mix (containing dATP, dTTP, dCTP, dGTP, and MgCl2 in Tris-HCl buffer), 5.0 µl of primer mix (containing multiple primers), 0.8 µl of polymerase, and 5 µl of DNA template. The DNA amplification conditions used were as following: first stage: 95 °C for 5 min, 1 cycle; second stage: 95 °C for 30 s, 58 °C for 30 s, 72 °C for 30 s, 5 cycles; third stage: 95 °C for 30 s, 55 °C for 30 s, 72 °C for 30 s, 35 cycles; fourth stage: 72 °C for 3 min, 1 cycle. Gene amplification was performed using an Eppendorf Mastercycler Gradient instrument.
According to the kit instructions, 27 HPV genotypes were detected, including 17 h-HPV genotypes (HPV 16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68, and 82) and 10 LR-HPV genotypes (HPV 6, 11, 40, 42, 43, 44, 55, 61, 81, and 83). During hybridization, 22 µl of mixed microsphere hybridization solution and 3 µl of HPV DNA amplification product were added to each hybridization well, sequentially mixed, and sealed. Denaturation was performed at 95 °C for 5 min, followed by hybridization at 48 °C for 30 min, and further incubation at 48 °C for 15 min. Streptavidin-phycoerythrin (75 µl) was then added to each well, followed by resealing and continued incubation at 48 °C for 15 min. HPV genotyping was analyzed using the Luminex 200 multiplex flow cytometer. The limit of detection (LOD) for HPV DNA is 100 copies/test. Negative quality control (sterile water) and positive quality control (containing cloned HPV16 and HPV18 genomic plasmid DNA fragments) were used as independent templates for PCR amplification, hybridization, and genotyping processes. Quality control of HPV genotyping included both internal quality control and external quality assessment.
Statistical analysis
The data analysis was conducted using GraphPad Prism and IBM SPSS Statistics 27 software. Frequency and prevalence rates (n(%)) were used as indicators to perform statistical analysis on the distribution of HPV genotypes. The chi-square test was utilized to compare infection rates among various groups and assess differences in vaccine coverage rates across different types. Binomial distribution analysis was employed to determine the 95% confidence interval (95% CI). Statistical significance was denoted by two-tailed P < 0.05. In instances where the expected value was ≤ 5 or the P-value approached 0.05, Fisher’s exact test was applied.
Results
The overall prevalence of HPV infection among 66,000 women
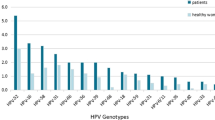
This study conducted HPV-DNA testing on 66,000 women from the Southwest plateau region of China spanning the years 2014 to 2023. The ages of the participants ranged from 14 to 87 years, with a mean age of (40.21 ± 10.93) years. A total of 10,574 cases of HPV-positive infections were detected, resulting in an overall infection rate of 16.02% (Fig. 1A). Among the positive cases, they were classified based on the number of infecting genotypes: single infection accounted for 79.90% (8449/10,574), double infection for 15.17% (1604/10,574), triple infection for 3.59% (380/10,574), and four or more infections for 1.33% (141/10,574) (Fig. 1B). According to the risk of infecting genotypes, they were categorized as follows: pure LR-HPV infection at 22.16% (2343/10,574), pure HR-HPV infection at 67.82% (7171/10,574), and Mixed LR-and HR-HPV infection at 10.02% (1060/10,574) (Fig. 1C). The highest infection rates among HR-HPV genotypes were observed for HPV52 (2.61%), followed by HPV16 (2.06%), HPV58 (1.81%), HPV53 (1.55%), HPV39 (1.09%), HPV56 (0.85%), HPV59 (0.80%), HPV18 (0.74%), HPV51 (0.74%), and HPV66 (0.54%). As for LR-HPV genotypes, the top 5 with the highest infection rates were HPV6 (1.30%), HPV61 (1.21%), HPV11 (0.85%), HPV81 (0.68%), and HPV43 (0.53%) (Fig. 1D; Table 1, and Fig. 2A).
Age specificity of HPV infection
Among patients undergoing HPV testing, the 30–39 age group and the 40–49 age group exhibited the highest proportions, constituting 32.83% and 30.74% respectively. Following closely were the 20–29 age group and the 50–59 age group, representing 16.01% and 15.83% respectively. The lowest proportions were observed in the ≥ 60 age group and the ≤ 19 age group, accounting for merely 3.83% and 0.75% respectively (Table 2). The age-specific pattern of HPV infection displayed a “bimodal” distribution, with the peak declining notably from 44.02% (217/493) in the ≤ 19 age group to 19.55% (2066/10,568) in the 20–29 age group, and further decreasing to the lowest point in the 30–39 age group at 13.84% (3000/21,671). Subsequently, it gradually rose to 14.64% (2970/20,290) in the 40–49 age group, 16.65% (1740/10,450) in the 50–59 age group, and 22.98% (581/2,528) in the ≥ 60 age group (Fig. 1E; Table 1). Moreover, significant variations were observed among different age groups in the top 5 HPV genotypes with the highest infection rates. While the ≤ 19 age group exhibited the highest infection rate, it was primarily dominated by LR-HPV, with HPV6 (13.18%) and HPV11 (10.75%) being the most prevalent. The most common HR-HPV infections were HPV59 (4.87%), HPV52 (4.67%), and HPV16 (4.06%). In all other age groups, HPV52 and HPV16 were the predominant genotypes. The details regarding genotype infections in each age group can be found in (Table 1; Fig. 2D).
The distribution of single and multiple infections
In the study, the proportion of patients with multiple infections decreased as the number of infecting genotypes increased. Specifically, the rates of single, double, triple, quadruple, and higher-order infections were 12.80% (8449/66000), 2.43% (1604/66000), 0.58% (380/66000), and 0.21% (141/66000) respectively (Table 2). Single infection of each genotype was dominant, followed by co-infection with other genotypes (Figs. 1D and 2B). Additionally, among HPV-positive individuals, both younger and older age groups showed a higher propensity for multiple infections, while the middle-aged group tended to experience single infections more frequently (Fig. 1F).
The distribution of HR-HPV and LR-HPV infections
Among all patients, the LR-HPV infection rate stood at 5.16% (3403/66000), whereas that of HR-HPV was 12.47% (8231/66000). Specifically, the rate of pure LR-HPV infection was 3.55% (2343/66000), and pure HR-HPV infection was at 10.87% (7171/66000). The rate of mixed LR-and HR-HPV infection was 1.61% (1060/66000) (Table 2). Furthermore, among HPV-positive individuals, the proportion of HR-HPV infection increased with age overall. Specifically, in the age group ≤ 19 years, it was the lowest at 57.60% (125/217), while in the age group ≥ 60 years, it was the highest at 86.23% (501/581). Thus, among HPV-positive individuals, younger individuals were more susceptible to LR-HPV infection, while older individuals were more prone to HR-HPV infection (Fig. 1G).
The prevalence of HPV in the patients from different sources
In this study, the outpatient HPV infection rate was recorded at 18.50% (6199/33512), surpassing that of inpatients at 12.97% (495/3816) and individuals undergoing physical examinations at 13.53% (3880/28672) (Table 3). The top five HPV genotypes with the highest infection rates among inpatients were HPV16 (3.17%), HPV52 (1.73%), HPV58 (1.62%), HPV53 (1.00%), and HPV61 (0.89%). Among outpatients, the top five HPV genotypes with the highest infection rates were HPV52 (2.66%), HPV16 (2.65%), HPV6 (2.17%), HPV58 (2.06%), and HPV53 (1.47%). For individuals subjected to physical examinations, the top five HPV genotypes with the highest infection rates were HPV52 (2.67%), HPV53 (1.72%), HPV58 (1.55%), HPV16 (1.22%), and HPV61 (1.14%) (Fig. 2C). Notably, the HPV16 positivity rate among inpatients was 2.60 times higher than that among individuals undergoing physical examinations, while the positivity rates of HPV6 and HPV11 among outpatients were 6.38 times and 4.25 times higher, respectively, than those among individuals undergoing physical examinations.
The prevalence of total and major HPV genotypes from 2014 to 2023
Between 2014 and 2023, spanning a decade, the prevalence of HPV demonstrated an overall declining trajectory. The highest prevalence occurred in 2016 at 25.40% (651/2563), while the lowest was observed in 2022 at 10.32% (1269/12297) (Fig. 3A). The prevalence of the nine HPV genotypes covered by the HPV 9-valent vaccine exhibited declines, particularly noticeable in HPV6, 11, 16, and 18 (Fig. 3B-C-D-E), while the prevalence of HPV31, 33, and 45 remained consistently low (Fig. 3F-G-H). Over the decade, HPV52 prevalence increased from the fourth position in 2014 to the top spot in 2018, maintaining this position until 2023 (Fig. 3I). HPV58 prevalence remained relatively stable overall, except for lower rates observed in 2019 at 1.11% (133/11966) and in 2022 at 1.08% (133/12297) (Fig. 3J). However, it is noteworthy that HPV53 and HPV61 currently exhibit high prevalence rates but lack corresponding vaccines. Unlike the nine genotypes covered by the vaccine, HPV53 and HPV61 did not demonstrate a decreasing trend in prevalence between 2014 and 2023; instead, they displayed an upward trend (Fig. 3K-L). Specifically, the prevalence of HPV53 increased from 0.87% (26/2982) in 2014 to 1.87% (168/8965) in 2023, indicating a 2.15-fold increase, with its infection rate ranking second among individuals undergoing physical examinations (Fig. 2C). Additionally, it is also worth highlighting that during the COVID-19 pandemic period from 2020 to 2022, the prevalence of all HPV genotypes showed a continuous downward trend.
Evaluation of the effectiveness of three human papillomavirus vaccines
In this study, the effectiveness of the three HPV vaccines was evaluated under two scenarios. In one scenario, all infected HPV genotypes were encompassed by the vaccine, resulting in coverage rates of 12.37% for the bivalent vaccine, 21.98% for the quadrivalent vaccine, and 46.82% for the nonavalent vaccine. In the other scenario, where at least one of the infected HPV genotypes was covered by the vaccine, the coverage rates were 17.20% for the bivalent vaccine, 26.35% for the quadrivalent vaccine, and 47.57% for the nonavalent vaccine (Table 4). The study found statistically significant differences in effectiveness among the three vaccines (P < 0.05).
Discussion
According to the 2020 WHO global assessment data on cervical cancer incidence and mortality, China ranks second globally in both the incidence and mortality of cervical cancer, following only India [25]. The availability of data on HPV prevalence is essential for informing effective HPV vaccination strategies and cervical cancer screening programs. This research offers insights into HPV infection rates and the distribution of its genotypes among women in the southwestern plateau region of China from 2014 to 2023. With the largest sample size and the longest study period to date, this research used consistent detection methods and included a comprehensive analysis across outpatient, inpatient, and routine physical examination settings in this area. The findings provide robust evidence for understanding HPV epidemiology in the region and could potentially influence future vaccination campaigns, screening programs, and public health policies to better address the burden of cervical cancer in this specific region of China.
Global distribution of HPV varies due to regional differences, population demographics, and the methods used for HPV DNA detection. The highest rates of HPV infection globally are seen in young women, with South America (Brazil) reporting 54.6%, North America (Mexico) at 54.17%, and the United States at 40%. Additionally, sub-Saharan Africa has an infection rate of 24.0%, and Asia (China) reports a rate of 19.12%. [15, 26,27,28,29]. In this study, the overall HPV positivity rate was 16.02%, consistent with the reported overall HPV infection rate in China (15.54%) [30]. Similar findings include 14.02% in Xinjiang [17], 15.13% in Xiamen [31], 17.35% in Wenzhou [32], 18.10% in Guangxi [33], and 18.71% in Chen Zhou [34]. However, the HPV infection rate in this study was lower than in Liaocheng, Shandong, at 22.13% [35], Weifang at 23.64% [19], Beijing at 24.14% [36], and Inner Mongolia (Ordos) at 23.36% [37], but higher than 8.16% in Shannan City, Tibet Autonomous Region [13]. Variations in HPV prevalence can be attributed to differences in geographic locations, economic conditions, and detection methods used. In comparison to other findings from Yunnan Province, the prevalence rates from this study are generally lower than the 27.4% observed among the Tibetan population in northwestern Yunnan [16] and 22.03% in Kunming [38], but higher than 11.9% among the Naxi population in northwestern Yunnan [16] and 9.88% among the Dai population in southern Yunnan [39]. However, in the same region of Qujing, the HR-HPV prevalence was reported as 8.32% in 2012 [40], which was significantly lower than the HR-HPV prevalence of 12.47% in this study [40]. These discrepancies in results could be due to the earlier study detecting fewer HPV genotypes, as well as variations in the study periods, populations studied, and the sensitivity of detection methods employed. Some of the domestic research findings published from 2021 to 2024 have been summarized in Table 5.
The relationship between single and multiple HPV infections and their impact on cervical cancer risk is a critical area of study. For instance, few prior studies have indicated that multiple HPV infections might exhibit a synergistic effect among different HPV genotypes, potentially complicating immune clearance mechanisms. This complexity could lead to a higher probability of persistent HPV infections, subsequently elevating the risk for cervical cytological abnormalities and the development of cervical cancer [23, 41, 42]. Conversely, other reports suggests that there may be competition or equilibrium among various HPV subtypes, which could result in a greater risk of cervical cancer in cases of single infections compared to multiple infections. For example, it has been observed that the incidence of cervical intraepithelial neoplasia grades 2–3 (CIN2-3) and cervical squamous cell carcinoma (SCC) is higher in patients with a sole HPV 16 infection (62.2%) than in those with multiple HPV genotype infections (52.4%) [43, 44]. Additionally, another study found that 91.8% of HPV-positive tumors harbored a single viral type, whereas 7% exhibited multiple viral types [45]. Multiple infections were more frequently noted in younger and older age groups, whereas single infections predominated in the middle-aged cohort. Thus, further evidence is required to ascertain whether multiple HPV infections contribute to an increased risk of cervical cancer. However, understanding the dynamics of multiple HPV infections is essential for the development of the next generation of multivalent HPV vaccines.
In this study, the age-specific pattern of HPV infection was characterized by a “bimodal” distribution (Fig. 1E), with peaks observed in younger and older age groups. Similar age distribution patterns have been reported in Tibet and Xiamen [13, 31]. In contrast, Xinjiang showed two infection peaks among those aged ≤ 25 years and 36–40 years [17], whereas in Jilin, the peaks were observed in individuals aged ≤ 24 years and 55–59 years, with rates declining after 60 [12]. Further analysis revealed that different HPV genotypes predominantly infect individuals in different age groups (Table 2; Fig. 2D). For example, in the ≤ 19-year-old group, where infection rates are highest, low-risk HPV types (LR-HPV), particularly HPV6 and 11, predominate. However, the highest rates of high-risk HPV (HR-HPV) infections, notably HPV59 and 52, occur in this group as well. In contrast, HPV52 and 16 are the most prevalent among women in all other age groups, with women aged ≥ 60 years experiencing not only high infection rates but also a tendency towards multiple infections primarily involving HR-HPV. Several factors contribute to these patterns. Younger women, who often have more frequent sexual activity and unstable sexual partnerships prior to full immune system development, lack adequate protection partly due to insufficient sexual health education [46]. Additionally, immature cervixes may not produce sufficient cervical mucus, increasing the risk of HPV infection [47]. However, infections in younger individuals, particularly LR-HPV, tend to be transient as the immune system matures. In contrast, older women are more vulnerable to persistent or reactivated HPV infections due to hormonal and immune changes post-menopause, with HR-HPV types evading immune surveillance over time. This increase in infection rates among older women poses a significant risk for the development of cervical cancer [48]. Therefore, adolescent vaccination to reduce HPV infections and regular cervical cancer screening for postmenopausal women are crucial strategies.
Differences in the predominant circulating HPV genotypes have been reported across various regions (Table 5). In this study, the most common HR-HPV genotypes were HPV52, 16, 58, 53, and 39, while the most common LR-HPV genotypes were HPV6, 61, and 11. Between 2014 and 2023, there was a marked reduction in the prevalence of HPV6, 11, 16, and 18, all of which are targeted by the 9-valent vaccine (HPV 9-Valent (Types 6, 11, 16, 18, 31, 33, 45, 52, 58) Vaccine-targeted genotypes) (Fig. 3B-C-D-E). This decrease could be linked to the earlier and broader availability, more affordable pricing, and increased access to bivalent and quadrivalent vaccines. HPV16 is not only highly oncogenic but also universally susceptible across all populations, with reports indicating that 49.8% of cervical adenocarcinoma patients are infected with HPV16 [49]. Consequently, managing HPV16 infections should be a high priority, necessitating prompt and consistent treatment and monitoring strategies. Although HPV18 also exhibits high oncogenicity, with reports indicating that 45.3% of cervical adenocarcinoma patients are infected with HPV18 [49], its prevalence in this study was relatively low, ranking only eleventh. Additionally, international studies have identified HPV31, 33, and 45 as the next most frequent genotypes in cancer cases after HPV16 and 18 [45, 49]. Although the prevalence of HPV31, 33, and 45 is lower in the Chinese population [31, 32], there is a need for further evidence on the cost-effectiveness of developing domestic vaccines targeting these genotypes. Reports within China indicate that, in addition to HPV16 and 18, HPV52 and 58 are significant carcinogenic factors responsible for inducing intraepithelial neoplasia [50]. These two genotypes, HPV52 and 58, are currently the most prevalent high-risk HPV (HR-HPV) genotypes. This prominence is likely due to the delayed availability, higher cost, and lower vaccination rates of the 9-valent vaccine, as well as potential influences from the immune clearance mechanisms of these genotypes, making them particularly noteworthy. Furthermore, HPV53, which ranks second in infection rates among those undergoing physical examinations, is associated with slower disease progression, and single HPV53 infections are considered less pathogenic [51]. Currently, HPV53, 39, and 61 maintain relatively high infection rates in the Chinese population but do not have targeted vaccines, highlighting a clear direction for the development of domestically produced vaccines.
According to the publicly available China CDC Weekly data, the cumulative vaccination rates for the first, second, and third doses of the HPV vaccine among women aged 9–45 years in China were 10.15, 8.69, and 6.21%, respectively, at the end of 2022. Specifically, the three-dose vaccination rates were 0.31, 2.21, 8.34, 9.39, 7.68, 7.88, and 5.37% in the age groups 9–14, 15–19, 20–24, 25–29, 30–34, 35–39, and 40–45 years, respectively [52]. Therefore, it is speculated that the trends of vaccine coverage and HPV prevalence are opposed. While the vaccination rate was low in the younger age groups (≤ 19 years), the HPV prevalence was high. In contrast, the prevalence of HPV infection was relatively high in the middle groups (20–39 years old) accompanied by a higher vaccination rate, with high prevalence in the older groups without vaccination. In Yunnan, while there were no data on vaccinations before 2018, the three-dose vaccination rates were 0.08, 0.41, 1.03, and 3.66% for the years between 2019 and 2022, with an accumulated vaccination rate of only 5.18% [52]. Unfortunately, the present study was retrospective in design and we were thus unable to collect data on the distribution of HPV genotypes and antibody titers in vaccinated and unvaccinated patients; this will be the focus of our future studies. However, relevant research shows that HPV vaccination generates high and prolonged antibody titers, represented mostly by IgG antibodies against the respective HPV L1 proteins. Notably, HPV vaccination has been found to produce 10 to 100-fold higher titers of L1-specific neutralizing antibodies compared to natural infection, thus preventing viral infection and subsequently the development of premalignant dysplasias [3].
Research has shown that HPV vaccines can prevent up to 82.5% (for bivalent vaccine) and up to 95.3% (for nonavalent vaccine) of HPV-positive cervical adenocarcinomas [45]. However, in this study, the coverage rates of all three HPV vaccines were below 50%, suggesting that the current vaccines may not fully meet the needs of this group. In line with the “Healthy China 2030” plan and the World Health Organization’s global objective to eliminate cervical cancer, it is critical for China, where cervical cancer incidence and mortality rates are among the highest globally to advance domestic vaccine production and develop HPV vaccines that are tailored to the epidemiological trends of its population. One innovative approach could be the development of monovalent HPV vaccines for each prevalent genotype, allowing individuals to select a vaccine combination that aligns with their financial capacity, age, ethnicity, regional epidemiological nuances, and other personal factors, thus personalizing the vaccination process. Such a strategy could enhance patient satisfaction, meet diverse needs more effectively, and reduce prevention costs, presenting a promising avenue for the future.
Although this study provides valuable insights into HPV infection rates and genotype distribution in the southwestern plateau region of China, it also has several notable limitations. First, the study relies solely on the results from single HPV-DNA detections, which do not account for the dynamics of ongoing infections in patients. Second, the absence of integration with pathological findings limits our understanding of how different HPV genotypes correlate with specific cervical abnormalities. Third, due to the retrospective nature of the study, information on the number and distribution of HPV genotypes in vaccinated and unvaccinated patients could not be obtained. Furthermore, critical sociodemographic information such as the patients’ educational levels, economic status, occupations, cultural backgrounds, ethnicity, parity, and number of sexual partners was not collected. This omission restricts our ability to fully evaluate how these factors might influence HPV infection rates. Hence, future research could not only address the various limitations of the current study but also significantly contribute to the global efforts in preventing and managing HPV-related diseases. For instance, conducting longitudinal studies to track individuals over time could enhance our understanding of the persistence of HPV infections and their evolution from infection to cervical abnormalities and cancer. Additionally, integrating HPV genotype information with pathological findings from cervical screenings could help clarify the relationship between specific HPV genotypes and the development of cervical lesions or cancer. Considering the variety of HPV genotypes detected, it would also be beneficial to develop and evaluate new multivalent or personalized vaccines tailored to cover the most prevalent and high-risk types specific to the region. In addition, analysis of the HPV infection rate and differences in genotype distribution between vaccinated and unvaccinated patients would be helpful in evaluating the preventive value of the vaccine. Furthermore, collecting and thoroughly analyzing demographic and behavioral data, such as education level, economic status, cultural background, ethnicity, and sexual history, could provide insights into the socio-economic and cultural factors that influence HPV prevalence and vaccine acceptance, thereby facilitating targeted public health measures.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- HPV:
-
Human Papillomavirus
- HR-HPV:
-
High-risk human papillomavirus
- LR-HPV:
-
Low-risk human papillomavirus
References
Lien K, Mayer W, Herrera R, et al. HIV-1 proteins gp120 and Tat promote epithelial-mesenchymal transition and invasiveness of HPV-Positive and HPV-Negative neoplastic genital and oral epithelial cells. Microbiol Spectr. 2022;10(6):e0362222.
Nelson CW, Mirabello L. Human papillomavirus genomics: understanding carcinogenicity. Tumour Virus Res. 2023;15:200258.
Tsakogiannis D, Nikolaidis M, Zagouri F, et al. Mutation Profile of HPV16 L1 and L2 genes in different Geographic areas. Viruses. 2022;15(1):141.
Roldão A, Mellado MC, Castilho LR, et al. Virus-like particles in vaccine development. Expert Rev Vaccines. 2010;9(10):1149–76.
Wang JW, Roden RB. Virus-like particles for the prevention of human papillomavirus-associated malignancies. Expert Rev Vaccines. 2013;12(2):129–41.
Chesson HW, Dunne EF, Hariri S, Markowitz LE. The estimated lifetime probability of acquiring human papillomavirus in the United States. Sex Transm Dis. 2014;41(11):660–4.
McBride AA. Human papillomaviruses: diversity, infection and host interactions. NAT Rev Microbiol. 2022;20(2):95–108.
International Agency for Research on Cancer of World Health Organization. IARC MONOGRAPHS ON THE IDENTIFICATION OF CARCINOGENIC HAZARDS TO HUMANS. List of Classifications, Agents classified by the IARC Monographs, Volumes 1-135.
Wang R, Pan W, Jin L, et al. Human papillomavirus vaccine against cervical cancer: opportunity and challenge. Cancer Lett. 2020;471:88–102.
Sawaya GF, Smith-McCune K, Kuppermann M. Cervical Cancer screening: more choices in 2019. JAMA. 2019;321(20):2018–9.
Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J Clin. 2021;71(3):209–49.
Hao S, Wang C, Liu S, et al. HPV genotypic spectrum in Jilin Province, China, where nonvaccine-covered HPV53 and 51 are prevalent, exhibits a bimodal age-specific pattern. PLoS ONE. 2020;3(15):e230640.
Feng D, Wei S, Chen J, et al. Human papillomavirus prevalence and genotype distribution landscapes in Shannan City, Tibet Tibetan Autonomous Region, China. Virol J. 2022;19(1):46.
Zhang W, Guo N, Li B, et al. Prevalence and genotype distribution of human papillomavirus infections in Beijing, China between 2016 and 2020. Virol J. 2023;20(1):11.
Zeng Z, Austin RM, Wang L, et al. Nationwide prevalence and genotype distribution of high-risk human papillomavirus infection in China. Am J Clin Pathol. 2022;157(5):718–23.
Baloch Z, Yuan T, Wang B, et al. Ethnic and geographic variations in HPV prevalence and genotype distribution in north-western Yunnan, China. J Med Virol. 2016;88(3):532–40.
Wang J, Tang D, Wang K, et al. HPV genotype prevalence and distribution during 2009–2018 in Xinjiang, China: baseline surveys prior to mass HPV vaccination. BMC Womens Health. 2019;19(1):90.
Li S, Zhang K, Yang L, et al. Distribution patterns of human papillomavirus genotypes among women in Guangzhou, China. Infect Agent Cancer. 2023;18(1):67.
Liu M, Zhang X, Guo L, et al. HPV prevalence and genotype distribution among 38 056 women in Weifang, China: a cross-sectional study. BMJ Open. 2023;13(9):e073332.
Bruni L, Serrano B, Roura E, et al. Cervical cancer screening programmes and age-specific coverage estimates for 202 countries and territories worldwide: a review and synthetic analysis. Lancet Glob Health. 2023;11(7):e1011.
Simms KT, Keane A, Nguyen DTN, et al. Benefits, harms and cost-effectiveness of cervical screening, triage and treatment strategies for women in the general population. Nat Med. 2023;29(12):3050–58.
Huang W, Xu H, Hu H, et al. The prevalence of human papillomavirus among women in northern Guangdong Province of China. Sci Rep. 2022;12(1):13353.
Li L, Chen Y, Chen J, et al. Prevalence and genotype distribution of high-risk human papillomavirus among Chinese women in Sichuan Province. Jpn J Infect Dis. 2020;73(2):96–101.
World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. https://www.who.int/publications/i/item/9789240014107 (2020).
Singh D, Vignat J, Lorenzoni V, et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO global cervical cancer elimination initiative. Lancet Glob Health. 2023;11(2):e197–e206.
Wendland EM, Villa LL, Unger ER, et al. Prevalence of HPV infection among sexually active adolescents and young adults in Brazil: the POP-Brazil study. Sci Rep. 2020;10(1):4920.
Alarcón-Romero LDC, Organista-Nava J, Gómez-Gómez Y, et al. Prevalence and distribution of human papillomavirus genotypes (1997–2019) and their association with cervical cancer and precursor lesions in women from Southern Mexico. Cancer Control. 2022;29:10732748221103331.
Bhattacharya M, Reiter PL, McRee AL. Nativity status and genital HPV infection among adults in the U.S. Hum Vaccin Immunother. 2019;15(7–8):1897–1903.
Kutz JM, Rausche P, Gheit T, et al. Barriers and facilitators of HPV vaccination in sub-saharan Africa: a systematic review. BMC Public Health. 2023;23(1):974.
Zhu B, Liu Y, Zuo T, et al. The prevalence, trends, and geographical distribution of human papillomavirus infection in China: the pooled analysis of 1.7 million women. Cancer Med. 2019;8(11):5373–85.
Shen Y, Huang Y, Wang W, et al. Prevalence and genotype distribution of HPV infection among women in Xiamen, China. Front Microbiol. 2023;14:1130226.
Chen Q, Qu W, Zhao Y, et al. The prevalence of HPV among 164,137 women in China exhibited some unique epidemiological characteristics. Infect Agent Cancer. 2023;18(1):72.
Wei L, Ma L, Qin L, Huang Z. The prevalence and genotype distribution of human papillomavirus among women in Guangxi, southern China. Infect Agent Cancer. 2022;17(1):19.
Luo LP, He P, Liu QT, et al. Prevalence and genotype distribution of HPV infection among 214,715 women from Southern China, 2012–2018: baseline measures prior to mass HPV vaccination. BMC Infect Dis. 2021;21(1):328.
Zheng LL, Chen SF, Yang F, et al. High-risk HPV prevalence and genotype distribution among women in Liaocheng, Shandong Province, China from 2016 to 2022. Front Public Health. 2023;11:1145396.
Wang J, Li H, Zhang J, et al. Epidemiology and genotypes analysis of human papillomavirus infection in Beijing, China. Virol J. 2024;21(1):19.
Wang S, Liu S, Tan S, et al. Characteristics of human papillomavirus prevalence and infection patterns among women aged 25–64 according to age groups and cytology results in Ordos City, China. Virol J. 2024;21(1):12.
Zhang Y, Xu Y, Dian Z, et al. Prevalence and genotype distribution of human papillomavirus infection among 40,613 women: an outpatient-based population study in Kunming, Yunnan. Front Public Health. 2022;10:922587.
Baloch Z, Yasmeen N, Li Y, et al. Prevalence and risk factors for human papillomavirus infection among Chinese ethnic women in southern of Yunnan, China. Braz J Infect Dis. 2017;21(3):325–32.
Sun LL, Jin Q, Li H, et al. Population-based study on the prevalence of and risk factors for human papillomavirus infection in Qujing of Yunnan province, Southwest China. Virol J. 2012;9:153.
Zhao M, Zhou D, Zhang M, et al. Characteristic of persistent human papillomavirus infection in women worldwide: a meta-analysis. Peer J. 2023;11:e16247.
Kim M, Park NJ, Jeong JY, Park JY. Multiple human papilloma virus (HPV) infections are associated with HSIL and persistent HPV infection status in Korean patients. Viruses. 2021;13(7):1342.
Nie J, Liu J, Xie H, et al. Multiple human papillomavirus infections and type-competition in women from a clinic attendee population in China. J Med Virol. 2016;88(11):1989–98.
Li M, Du X, Lu M, et al. Prevalence characteristics of single and multiple HPV infections in women with cervical cancer and precancerous lesions in Beijing, China. J Med Virol. 2019;91(3):473–81.
Pirog EC, Lloveras B, Molijn A, et al. HPV prevalence and genotypes in different histological subtypes of cervical adenocarcinoma, a worldwide analysis of 760 cases. Mod Pathol. 2014;27(12):1559–1567.
Wissing MD, Louvanto K, Comète E, et al. Human papillomavirus viral load and transmission in Young, recently formed heterosexual couples. J Infect Dis. 2019;220(7):1152–61.
Tounkara FK, Téguété I, Guédou FA, et al. Type-specific incidence, persistence and factors associated with human papillomavirus infection among female sex workers in Benin and Mali, West Africa. Int J Infect Dis. 2021;106:348–57.
Malagón T, Kulasingam S, Mayrand MH, et al. Age at last screening and remaining lifetime risk of cervical cancer in older, unvaccinated, HPV-negative women: a modelling study. Lancet Oncol. 2018;19(12):1569–78.
Reynders C, Lerho T, Goebel EA, et al. Prevalence and genotype distribution of human papillomavirus in cervical adenocarcinoma (usual type and variants): a systematic review and meta-analysis. J Med Virol. 2023;95(10):e29190.
Wang X, Zeng Y, Huang X, Zhang Y. Prevalence and genotype distribution of human papillomavirus in Invasive Cervical Cancer, Cervical Intraepithelial Neoplasia, and Asymptomatic women in Southeast China. Biomed Res Int. 2018;2018:2897937.
Chen R, Fu Y, You B, et al. Clinical characteristics of single human papillomavirus 53 infection: a retrospective study of 419 cases. BMC Infect Dis. 2021;21(1):1158.
Chen J, Zhang Z, Pan W, et al. Estimated human papillomavirus vaccine coverage among females 9–45 years of age - China, 2017–2022. China CDC Wkly. 2024;6(19):413–7.
Wang X, Song Y, Wei X, et al. Prevalence and distribution of human papillomavirus genotypes among women attending gynecology clinics in northern Henan Province of China. Virol J. 2022;19(1):6.
Wang T, Luan L, Deng J, et al. Prevalence and human papillomavirus (HPV) genotype distribution in Suzhou, China. Hum Vaccin Immunother. 2023;19(2):2241309.
Lin B, Zhang F, Liu F, et al. The prevalence and genotype distribution of human papillomavirus in central Fujian Province during the COVID-19 pandemic. Virol J. 2024;21(1):129.
Acknowledgements
We express our gratitude to the medical staff in the departments of gynecology and preventive medicine at the People’s Hospital Affiliated with Kunming Medical University for their assistance in conducting this study.
Funding
This work was supported financially by grants from the Scientific Research Fund of Yunnan Provincial Department of Science and Technology and Kunming Medical University Joint Project (202201AY070001-214; 202301AY070001-071), the Scientific Research Fund of Yunnan Provincial Department of Education (2024J0152; 2024J0392; 2020J0800), the major science and technology special plan of Yunnan Province (202402AD080006).
Author information
Authors and Affiliations
Contributions
Conceptualization, J.P.H. and H.W.L.; methodology, J.L.W., C.J.Y., Y.L. and Y.F.; investigation, C.Q.T. and X.Q.C.; data curation, J.P.H., J.P.H. and H.X.L.; writing—original draft preparation, J.P.H. and X.P.L.; writing—review and editing, J.L.W., G.H.Z., and Q.X.; supervision, H.W.L. and C.J.Y.; project administration, Z.W.F., J.S.Y., Y.X.L., Z.S.W., T.J., L.H.G., J.D.Z., R.Z., J.M.S., Q.C. and S.M.L.; funding acquisition, F.H., H.X.L., C.J.Y. and J.L.W. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical Research Ethics Committee [2023-045(KE)-01] in the Qujing First People’s Hospital. The participants’ informed consent was obtained electronically.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hu, JP., Wang, JL., Li, Y. et al. Prevalence and genotype distribution of human papillomavirus infection among 66000 women from 2014 to 2023 in the plateau region of Southwest China. Virol J 21, 176 (2024). https://doi.org/10.1186/s12985-024-02447-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-024-02447-2