Abstract
Background
This study aimed to demonstrate that the genomic material of SARS-CoV-2 can be isolated from strips of COVID-19 rapid diagnostic test cassettes.
Method
It was a prospective cross-sectional study involving patients admitted to treatment centers and sampling sites in the city of Conakry, Guinea. A total of 121 patients were double sampled, and 9 more patients were tested only for RDT. PCR was conducted according to the protocol of the RunMei kit. Sequencing was performed by using the illumina COVIDSeq protocol. Nine COVID-19 RDTs without nasopharyngeal swabs were in addition tested.
Result
Among the 130 COVID-19 RDTs, forty-seven were macroscopically positive, whereas seventy-two were positive according to PCR using RDT strip, while among the 121 VTM swabs, sixty-four were positive. Among eighty-three negative COVID-19 RDTs, twenty-seven were positive by PCR using RDT strip with a geometric mean Ct value of 32.49 cycles. Compared to those of PCR using VTM, the sensitivity and specificity of PCR using RDT strip were estimated to be 100% and 85.96%, respectively, with 93.39% test accuracy. Among the fifteen COVID-19 RDT extracts eligible for sequencing, eleven had sequences identical to those obtained via the standard method, with coverage between 75 and 99.6%.
Conclusion
These results show that COVID-19 RDTs can be used as biological material for the genomic surveillance of SARS-CoV-2.
Similar content being viewed by others
Background
At the end of 2019, an epidemic of pneumonia of unknown etiology broke out worldwide. A pathogen was isolated and named 2019 novel coronavirus (2019-nCoV), which causes coronavirus disease 2019 (COVID-19) [1].
By January 2024, a total of 774,291,287 confirmed cases of COVID-19 had caused 7,019,704 deaths worldwide [2]. The Reverse Transcription Polymerase Chain Reaction (RT-PCR) of nasopharyngeal swabs has become the gold standard for diagnosis [3,4,5]. Other studies have shown that antigen tests are convenient for the rapid diagnosis of COVID-19 [3, 4, 6, 7]. Indeed, the use of the COVID-19 rapid diagnostic test (RDT) antigen test can contribute to reducing the circulation of the virus through rapid detection of positive cases [1, 7,8,9,10]. On the other hand, the fight against respiratory viral diseases such as COVID-19 cannot be effective without genomic surveillance of different variants of SARS-CoV-2. This surveillance provides information on circulating variants, their impact on viral transmissibility, the occurrence of outbreaks, disease severity, and the effectiveness of vaccines, treatments, and disease diagnostics.
Regardless of whether it is diagnostic or genomic surveillance, it is necessary to collect samples, and nasopharyngeal swabs are highly recommended in the context of COVID-19 [1, 11]. Nasopharyngeal swabs are stored in tubes containing viral transport medium (VTM) [1, 6, 12]. One study showed that for SARS-CoV-2, several transport media, such as Dulbecco's modified Eagle's medium (DMEM), 100% ethanol or phosphate-buffered saline (PBS), can be used [7]. This nasopharyngeal swab for the COVID-19 RDT is stirred into a buffer within a tube before migrating onto the cassette. Studies have shown that residual extraction solution can be used to isolate viral RNA for diagnostic purposes [8].
The main problem that African laboratories faced during the COVID-19 epidemic was the storage of nasopharyngeal swabs in the VTM for an extended period. Thus, retrospective studies for genotyping are a challenge for countries that do not have sequencing tools available at each laboratory. One study showed an alternative preservation method using filter paper as a source of viral RNA [9]. This method has been shown to preserve SARS-CoV-2 viral RNA for at least 1 month. Other studies have shown that the strip in the tested RDT cassette can be used as a source of nucleic acid for Plasmodium [10, 13,14,15,16,17,18] and arboviruses such as dengue [19]. A study conducted in Belgium using fifteen RDT samples demonstrated the feasibility of utilizing RDT strips as a source of viral nucleic acid. This study employed two sequencing technologies and confirmed that these RDT strips can indeed serve as a valuable resource for extracting viral RNA [20].
In Guinea, in response to the swift spread of COVID-19 within the population, the Ministry of Health has firmly advocated for the utilization of RDTs during mass testing campaigns. These campaigns are conducted at sampling sites established in health facilities, public spaces, and high-traffic locations such as bus stations. The aim is to enhance testing accessibility and identify cases promptly. This approach reduced the workload of health professionals and the cost of the response. These rapid tests also help resolve the difficulties associated with the implementation of PCR using VTM in rural areas [16]. On the other hand, since the appearance of the first case of COVID-19, surveillance of SARS-CoV-2 variants has focused on samples collected in the city of Conakry [18].
Genotyping studies require tools that are available only in some laboratories across the country. The preservation of the quality of samples and their safe transportation from rural areas to these laboratories is a matter of concern. The difficulties related to the proper storage and transportation of samples from rural areas to the capital constitute an obstacle to conducting a retrospective study to determine the SARS-CoV-2 variants circulating in these areas. This explains the underestimation of the sequencing data produced in the country since the data were collected only in the Conakry region, which is only 16% of the general population of Guinea [19]. To find an alternative way to collect sample for molecular COVID-19 surveillance across the country, we decided to compare the RT-qPCR and sequencing results from direct nasopharyngeal swab sample versus sample collected from COVID-19 RDT cassettes already used for rapid diagnosis for the same patients.
Methods
Study site and sample collection
During the active pandemic of COVID-19 in Guinea, we conducted a prospective study from October 6 to 21, 2022 in Conakry at the epidemic treatment centers of Gbessia, municipal medical center of Matam, and Centre de Recherche et de Formation en Infectiologie de Guinée (CERFIG). Two types of samples source (nasopharyngeal swabs stored in tubes containing VTM and antigen RDT cassettes) were taken from suspected patients, hospitalized patients or international travelers. Both positive and negative cassettes, as well as nasopharyngeal samples stored in the VTM, were sent to the laboratory for analysis.
RNA extraction and quantification by RT-qPCR
RNA was extracted from both sample source using a RunMei kit (Human RunMei Gene Technology Co., Ltd.) following the manufacturer’s instructions. Regarding the extraction of viral RNA from COVID-19 RDTs, we opened each cassette and removed the strip. The protocol was modified at the lysis step for sample from RDT, and the incubation time was extended from 10 to 20 min at room temperature. The extracted RNA was then stored at − 20 °C until use and at − 40 °C for long term use.
Quantification of the samples was performed using the RunMei RT-qPCR SARS-CoV-2 kit (Human RunMei Gene Technology Co., Ltd.), which detects the ORF1ab and N genes. For each PCR, we included an extraction control, a mix control, and used the CY5 fluorescence marker as an internal control for the detection kit. This quantification was conducted for nasopharyngeal extracts stored in VTM and those obtained from COVID-19 RDT strip. For sequencing, SARS-CoV-2-positive samples with a cycle threshold (Ct) value less than 30 were selected. The results obtained were then compared with each other depending on the source of the nucleic acid.
Library preparation
To proceed to the sequencing, we selected only samples with a cycle threshold (Ct) value less than 30. Sequencing library was prepared using the Illumina COVIDSeq Assay (96 samples) protocol. After reverse transcription and first strand synthesis, multiplex tiled PCR was conducted using primers specific for SARS-CoV-2 (Pools 1&2). The PCR-amplified product was processed for tagmentation and adapter ligation using IDT for Illumina Set B indexes (96 indexes for ninety-six samples). The samples were grouped into batches of twelve and quantified using a Qubit 3.0 fluorometer (Invitrogen, Inc.). The pools obtained were normalized and then diluted to obtain a final concentration of 75 pM for loading on Illumina ISeq 100 platform. We introduced one or two negative controls into each library.
Data analysis
All data were recorded as variables of concern, such as test category (suspect, contact or control), sex (male or female), age, date of collection, macroscopic RDT result (positive or negative), the result of PCR using VTM (positive, negative, Ct for the N and ORF1ab genes) and PCR from an RDT strip (positive, negative, Ct for the N and ORF1ab genes). We compared the efficiency of PCR conducted using viral RNA extracts from COVID-19 RDT (PCR using RDT strip) to that of PCR conducted using viral RNA extracts obtained from nasopharyngeal swabs on viral transport medium (PCR using VTM).
To assess the effectiveness of PCR using RDT strips compared to PCR using VTM, we determined the Cohen’s Kappa coefficient (https://www.jstor.org/stable/2529310) [21, 22]. The Cohen’s Kappa is a statistical test that uses the positive and negative results from two different tests. The test yields a coefficient that ranges from 0 to 1. This allowed us to measure the degree of agreement between the two tests. The closer this coefficient is to 1, the higher the degree of agreement. Student t test was calculated to compare the Ct value obtain from both PCR tests. P value was less than 0.05 was considered significant (Fig. 1).
Implementation of the viral RNA extraction protocol from the rapid diagnostic test for SARS-CoV-2. (1) Quality of the PCR curves made from the sample placement area. The CT values were: Gene N = 24.19; Gene ORF1ab = 30.29 and Internal Control (C. Int) Cy5 = 29.64. (2) Quality of the PCR curves made from the reading area of the RDT, with CT values of: Gene N = 28.12; ORF1ab gene = 32.24 and C. Int Cy5 = 32.53. (3) Quality of the PCR curves made from the distal end of the RDT, with CT values of: Gene N = 30.45; ORF1ab gene = 33.34 and C. Int Cy5 = 34.55. (4) Positive control curves. N gene = 19.09; ORF1ab gene = 21.49 and C. Int Cy5 = 22.25. This result indicates that the sample placement zone curves closely resemble those of the positive control
For bioinformatic analyses, we used the GeVarLi pipeline (GEnome assembly, VARiants calling, and Lineages assignment) developed for the AFROSCREEN network (https://forge.ird.fr/transvihmi/nfernandez/GeVarLi). The pipeline includes the quality control, alignment, variant calling, mapping to the reference genome and consensus sequence building. Lineages was assigned using pangolin version 4.3 developed by Andrew Rambaut and col. (https://doi.org/https://doi.org/10.1093/ve/veab064) and the quality of the sequences was double check on Nextclade. All sequences that passed the quality control was consider good sequences and was submitted to GISAID. The identifiers for the 5 genomes submitted to GISAID are: EPI_ISL_15581444, EPI_ISL_15581445, EPI_ISL_15581450, EPI_ISL_15581457, and EPI_ISL_15581458.
Results
Distribution of samples
From a total, 121 patients were sampled simultaneously for a PCR using VTM and an RDT COVID-19. Nine other patients solely underwent the RDT COVID-19. The maximum time between the collection of the samples where we had the results of the antigen test and the PCR from the RDT strip was 1 week. The PCR using VTM test yielded sixty-four positives from 121 tests. Macroscopic examination of the RDTs revealed forty-seven positive results, but the PCR using RDT strip results revealed at seventy-two (72) out of 130 positive results (Fig. 2). Overall, 75.38% (n = 98) were men, and the median age was 41 years (range, 3 to 89 years). Study participants were mostly cases or contacts of cases (81.5%; n = 106).
The sample distribution flowchart for PCR conducted using COVID-19 RDT extract is called PCR using RDT strip and PCR conducted with nasopharyngeal samples contained in a viral transport medium is called PCR using VTM (PCR). The macroscopic results of the COVID-19 antigen RDT are simply called the RDT
Technical implementation
We started by performing extraction from cassettes to determine whether the genetic material can be isolated and to determine which part of the strip gives the best concentration of virus RNA. For this purpose, ten samples were used. The strip was divided into three (3) parts: the proximal part where the sample was deposited, the middle part where the sample was deposited, the reading window and the distal part where the migration ended. Each part was cut into 3–4 pieces and placed in a 1.5 ml Eppendorf tube. To develop the strategy, we evaluated each of the three parts of the strip to determine which one was best shown. The results obtained (Fig. 1) revealed that the viral RNA was more concentrated in the deposited parts than in the other two parts (the window reading and distal parts).
Comparison between PCR using VTM, PCR using RDT strip and COVID-19 antigen RDT results
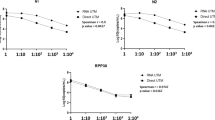
All samples (n = 46) positive for COVID-19 RDT were also positive for PCR using VTM and PCR using RDT strip (Table 1). For these forty-six samples, the Ct distribution (Fig. 3a) was greater for PCR using RDT strip than for PCR using VTM. However, these values did not exceed thirty cycles, and the difference between the two distributions was significant (p = 0.0006). Indeed, 88.88% (64/72) of samples positive for PCR using VTM were also positive for PCR using RDT strip, with a significant difference (p = 0.0011) in Ct value distributions (Fig. 3b). Eight samples with Ct values greater than thirty cycles were therefore negative according to PCR using VTM. Twenty-six RDT-negative samples were detected as positive by PCR using RDT strip with a geometric mean Ct value of 32.43 cycles. Thus, only four samples had a Ct < 30 cycles. Eighteen samples were negative by RDT and positive by PCR using VTM and PCR using RDT strip (Fig. 3c). Among these eighteen samples, 9 and 4 had Ct values below 30 for PCR using VTM and PCR using RDT strip, respectively.
Ct value distribution for PCRVTM and PCRStrip. a Designates the distribution of forty-six (46) samples positive for the COVID-19 RDT, PCR using VTM (PCRVTM) and PCR DRT strip (PCRStrip). b Represents the distribution of sixty-four PCRStrip and PCRVTM positive samples. c Designates the distribution of Ct values of eighteen samples positive for PCRVTM and PCRStrip and negative for the COVID-19 RDT. d Represent the eight samples negative for PCRStrip and RDT COVID-19 tests
Concordance between PCR using RDT strip and PCR using VTM.
PCR using VTM, which involves the use of nasopharyngeal swabs extracted from viral transport media, was used as the reference test in this study. For the PCR using RDT strip, there were sixty-four true positives, eight false positives, zero (0) negatives, and forty-nine true negatives. However, we had 64 positives compared to 57 negatives in the PCR using viral transport medium (VTM), the Cohen’s Kappa is equal to 0.8 (Table 2). This value indicates almost perfect concordance between the PCR using VTM and the PCR using RDT strips.
Concordance of variants found by whole-genome sequencing:
A total of fifteen samples extracted from COVID-19 RDTs were sequenced. The sequences were compared to those of nasopharyngeal swabs (NPS) from VTM from the same patients. The SARS-CoV-2 variants found were BA.5.2.1 (n = 6), BQ.1 (n = 3), BQ.1.1 (n = 5), and recombinant XAS (n = 1). The results showed that eleven (11) sequences yielded the same variant for both sample sources. These variants were BA.5.2.1 (n = 6) and BQ.1.1 (n = 4), with coverage between 75 and 99.6%, and BQ.1 (n = 1), with 39% coverage for the COVID-19 extract of RDT and 54.44% coverage for the VTM extract of NPS. Regarding this difference between these two variants, we observed that the greater the coverage was, the more we obtained the BQ1.1 variant and the lower the coverage was; thus, we obtained the BQ.1 variant for the same samples. Three samples gave variants (BQ.1 and BQ.1.1) that did not correspond to each other. For those sample sequences, the difference was related to low coverage or lack of sequences for the nasopharyngeal swab samples on the VTM (Table 3).
Discussion
To combat emerging infectious diseases, low-income countries must develop innovative strategies for transporting and storing biological samples. The main objective of this study was to demonstrate that RNA can be extracted from the virus using rapid diagnostic tests, which are commonly employed for SARS-CoV-2 testing. This extracted RNA can then be utilized to confirm diagnoses via RT-PCR and to conduct sequencing as part of epidemiological surveillance. Therefore, this approach facilitates the decentralization of sampling in rural regions and extends surveillance coverage of virus circulation in areas that are typically inaccessible to molecular diagnostic technology. Additionally, it permits the conducting of retrospective studies on alternative sampling methods beyond those recommended under normal circumstances while ensuring sufficient technical platform availability.
Most of the sequences obtained in Africa originated from cases diagnosed in major cities (capital cities) and were exclusively supplied by research laboratories located in those capitals [23]. This proves the importance of our study, considering our main goal to show the possibility of viral RNA isolation from strips of RDT cassettes used for COVID-19 screening in addition to conducting genomic investigations. The first idea was to show that the genetic material of the virus can be isolated from previously used COVID-19 RDTs. The need to include macroscopically negative COVID-19 RDTs in the tests was investigated, and finally, some sequences obtained from COVID-19 RDT extracts and those obtained from nasopharyngeal swab extracts on the VTM were compared to determine the concordance between them. The COVID-19 RDT is a rapid test that allows immediate treatment of the disease. It is easy to deploy and widely accessible to help limit the spread of the virus. Therefore, even in the most remote corners of the country, this test can be used. This study shows that SARS-CoV-2, the virus responsible for COVID-19, can be isolated from the strip of an already used RDT. The PCR using RDT strip proved to be effective with a sensitivity of 100% and a specificity of 85.96% compared to the PCR using VTM. However, we also observed that the PCR using RDT strip while the RDT itself was macroscopically negative, had a Ct value higher than 30. This suggests that negative RDTs are ineffective for genomic surveillance. Studies conducted in this context have shown the performance of using filter paper soaked in the dilution buffer of the COVID-19 RDT kit stored at room temperature for 1 month to perform molecular studies [24]. This was also supported by authors from Belgium [20] who tested this hypothesis by sequencing respiratory viruses such as influenza virus and SARS-CoV-2 from 10 RDT strips. Thus, all these studies highlight the possibility of using RDTs as a source of nucleic acid for genomic surveillance of respiratory viruses such as SARS-CoV-2. We should also add that this strategy was applied to Plasmodium [14, 16] and Dengue virus [19].
To decide whether to include the COVID-19 RDT in testing and not just limit it to positive RDTs, we evaluated all positive and negative COVID-19 RDTs with PCR using RDT strip to determine whether there would be any difference between the results obtained and those of the RDT seen by eye. The results of the PCR using RDT strip were then compared to those of the PCR using VTM. Thus, all RDT-positive samples were positive by PCR using RDT strip and PCR using VTM. We also noted that COVID-19 RDT-negative samples were negative by PCR using RDT strip. The sensitivity and specificity of the COVID-19 RDT compared to PCR using RDT strip were 71% and 100%, respectively. These results thus affirm that all positive and negative RDTs must be collected and subjected to the same molecular analyses.
We highlighted the possibility of performing sequencing using SARS-CoV-2-positive samples whose viral RNA was extracted from COVID-19 RDTs. For sequences with good coverage, we noted no differences between the sequences obtained from extracts used for PCR using VTM and those obtained from extracts used for PCR using RDT strip. In the study of [20], the authors sequenced samples with RNA extracted from strips of antigen RDT conserved for 1 month and used Sanger and whole-genome sequencing (WGS). They found the same variant event, although the coverage of some samples in WGS was 75%. However, the good conservation of samples and viral RNA extracts is a key factor to consider, not only to maintain the first characteristics of the samples but also to obtain good coverage of the sequences. We also observed that the detection of BQ.1.1 and BQ.1 was dependent on sequence coverage due to their close genetic proximity [25].
Although the use of rapid diagnostic strips as a source of nucleic acid is an innovative approach that is well suited for low-resource countries, their storage conditions could impact the biological quality of samples. In this study, the strips were stored at room temperature, but the effect of storage duration on sample quality was not evaluated.
Conclusions
The field of genomic surveillance for viruses plays a crucial role in understanding virus evolution and transmission dynamics. This knowledge informs decisions related to epidemic response, medical care, and vaccination strategies. The more data we gather, the deeper our understanding becomes.
In this study, we propose an innovative approach: utilizing RDT cassettes to collect additional samples and expand genomic surveillance in rural areas of the country. Our findings demonstrate the high sensitivity and specificity of PCR conducted with RNA extracted from these RDT cassettes. Notably, all symptomatic individuals who tested positive for RDT antigen could be confidently considered COVID-19 patients.
However, it is essential to note that the Ct value was greater for the PCR using RDT strip method than for PCR using VTM. Despite this difference, our results indicate that all positive samples suitable for sequencing using the standard protocol were also compatible with the alternative procedure. Given these results, we recommend expanding the use of this approach for broader epidemiological and molecular surveillance of potentially epidemic diseases.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request. Sequencing data including in this study are available on GISAID (https://gisaid.org/).
Abbreviations
- nCoV:
-
Novel coronavirus
- COVID-19:
-
Coronavirus Disease 2019
- RDT:
-
Rapid diagnostic test
- RT-qPCR:
-
Real-time quantitative reverse transcription polymerase chain reaction
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- VTM:
-
Viral transport medium
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- RNA:
-
Ribonucleic acid
- CERFIG:
-
Centre de Recherche et de Formation en Infectiologie de Guinée
- Ct:
-
Cycle threshold
- pM:
-
Pico molaire
- N:
-
Nucleocapsid protein
- ORFab:
-
Reading frame of 1ab
References
Sharma K, Aggarwala P, Gandhi D, Mathias A, Singh P, Sharma S, et al. Comparative analysis of various clinical specimens in detection of SARS-CoV-2 using rRT-PCR in new and follow up cases of COVID-19 infection: quest for the best choice. PLoS ONE. 2021;16:e0249408. https://doi.org/10.1371/journal.pone.0249408.
WHO. COVID-19 cases|WHO COVID-19 dashboard [Internet]. 2024 [Cited 2024 Jan 31]. https://data.who.int/dashboards/covid19/cases?n=c.
Pan American Health Organization (PAHO). Laboratory guidelines for the detection and diagnosis of COVID-19 virus infection [Internet]. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/laboratory.
CDC. Interim guidelines for clinical specimens for COVID-19|CDC [Internet]. [Cited 2023 Jul 18]. https://www.cdc.gov/coronavirus/2019-ncov/lab/guidelines-clinical-specimens.html.
Machhi J, Herskovitz J, Senan AM, Dutta D, Nath B, Oleynikov MD, et al. The natural history, pathobiology, and clinical manifestations of SARS-CoV-2 infections. J Neuroimmune Pharmacol. 2020;15:359–86.
WHO. WHO|SARS-CoV-2 variants [Internet]. 2020 [Cited 2021 Apr 11]. https://www.who.int/csr/don/31-december-2020-sars-cov2-variants/en/.
Baek YH, Park MY, Lim HJ, Jung HS, Yang JH, Sohn YH, et al. Evaluation of alternative transport media for RT-qPCR-based SARS-CoV-2 testing. Int J Anal Chem. 2022;7.
Sitoe N, Sambo J, Nguenha N, Chilaule J, Chelene I, Loquiha O, et al. Performance evaluation of the STANDARDTM Q COVID-19 and PanbioTM COVID-19 antigen tests in detecting SARS-CoV-2 during high transmission period in Mozambique. Diagnostics. 2022;12:475.
Durand GA, Amroun A, Grard G, Badaut C. Positive SARS-CoV-2 RT-qPCR of a nasal swab spot after 30 days of conservation on filter paper at room temperature. J Med Virol. 2023;95:e28165. https://doi.org/10.1002/jmv.28165.
Nabet C, Doumbo S, Jeddi F, Sagara I, Manciulli T, Tapily A, et al. Analyzing deoxyribose nucleic acid from malaria rapid diagnostic tests to study Plasmodium falciparum genetic diversity in Mali. Am J Trop Med Hyg. 2016;94:1259–65.
Kevadiya BD, Machhi J, Herskovitz J, Oleynikov MD, Blomberg WR, Bajwa N, et al. Diagnostics for SARS-CoV-2 infections. Nat Mater. 2021;20:593–605.
Martinez RM. Clinical samples for SARS-CoV-2 detection: review of the early literature. Clin Microbiol Newsl. 2020;42:121–7.
Ishengoma DS, Lwitiho S, Madebe RA, Nyagonde N, Persson O, Vestergaard LS, et al. Using rapid diagnostic tests as source of malaria parasite DNA for molecular analyses in the era of declining malaria prevalence. Malar J. 2011;10:6.
Papa Mze N, Ahouidi AD, Diedhiou CK, Silai R, Diallo M, Ndiaye D, et al. Distribution of Plasmodium species on the island of Grande Comore on the basis of DNA extracted from rapid diagnostic tests. Parasite. 2016;23:34.
Srisutham S, Suwannasin K, Mathema VB, Sriprawat K, Smithuis FM, Nosten F, et al. Utility of Plasmodium falciparum DNA from rapid diagnostic test kits for molecular analysis and whole genome amplification. Malar J. 2020;19:1–8. https://doi.org/10.1186/s12936-020-03259-9.
Cnops L, Boderie M, Gillet P, Van Esbroeck M, Jacobs J. Rapid diagnostic tests as a source of DNA for Plasmodium species-specific real-time PCR. Malar J. 2011;11.
Veron V, Carme B. Recovery and use of Plasmodium DNA from malaria rapid diagnostic tests. Am J Trop Med Hyg. 2006;74:941–3.
Denise *, Mawili-Mboumba P, Louise M, Mbuyi T, Patrick M’bondoukwe N, Bouyou-Akotet MK. Plasmodium falciparum allelic diversity: a comparison of DNA extraction from isolates collected on rapid diagnostic tests (Rdts) and filter paper. Iran J Parasitol. 2021;16:555–9.
Vongsouvath M, Phommasone K, Sengvilaipaseuth O, Kosoltanapiwat N, Chantratita N, Blacksell SD, et al. Using rapid diagnostic tests as a source of viral RNA for dengue serotyping by RT-PCR—a novel epidemiological tool. PLoS Negl Trop Dis. 2016 [Cited 2023 Jul 24];10. https://pubmed.ncbi.nlm.nih.gov/27159058/.
Rector A, Bloemen M, Schiettekatte G, Maes P, Van Ranst M, Wollants E, et al. Sequencing directly from antigen-detection rapid diagnostic tests in Belgium, 2022: a gamechanger in genomic surveillance? Research. 2022 [Cited 2023 Aug 3];1. www.eurosurveillance.org.
Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–60.
Chung E, Romano JP. Exact and asymptotically robust permutation tests. Ann Stat. 2013;41:484–507.
Adepoju P. Challenges of SARS-CoV-2 genomic surveillance in Africa. Lancet Microbe. 2021;2:e139.
Castineiras TMPP, ÉR dos Nascimento S, Faffe DS, Galliez RM, Mariani D, I de Leitão C. Performance of an alternative RT-PCR procedure using residual sample from the PanbioTM Ag COVID-19 test. Braz J Infect Dis. 2021;25:8.
Akash S, Pharm M, Islam MR, Dhama K. Emergence BQ.1 and BQ.1.1 as newly identified omicron subvariants: current scenario and future outlook-an update. 2023 [Cited 2024 Mar 1]. https://doi.org/10.1097/MS9.0000000000000469.
Acknowledgements
We acknowledge all the patients who agreed to participate in the study. We thank all CERFIG personnel and those at the study sites. We would also like to thank members of the AFROSCREEN Consortium (https://www.afroscreen.org/en/network) for their work and support on genomic surveillance in Africa.
Funding
This work was supported by Agence Française de Développement through the AFROSCREEN project (Grant Agreement CZZ3209), coordinated by ANRS Maladies Infectieuses Emergentes in partnership with the Institut Pasteur and IRD.
Author information
Authors and Affiliations
Consortia
Contributions
AKK, AKS, HD, BT, ACTG, JBK, MKP, JLM, BT, and AM carried out the experiments and collected the data. AM, AKK, KJJOK, AT, NV, EG, AA, ED, MP and AKK conceived and designed the study. AM, HD, BT, AS, and ACTG performed the sequencing data analysis. AKK and AM analyzed the data. AM and AKK wrote the original draft. AM, AKK, AKS, KJJOK, HD, ACTG, JBK, MKP, JLM, BT, NV, EG, AA, ED, MP, AT, AKK, AND AFROSCREEN team wrote, reviewed, and edited the last versions. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval to this study was obtained from the National Ethics Review Board (number062/CNERS/22). The protection of confidentiality was promoted to all participants. All participants for whom nasopharyngeal samples were collected provided verbal informed consent to take part in the study.
Consent for publication
This manuscript doesn’t contain any individual person’s data.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Keita, A.K., Mbaye, A., Soumah, A.K. et al. Use of strips of rapid diagnostic tests as a source of ribonucleic acid for genomic surveillance of viruses: an example of SARS-CoV-2. Virol J 21, 171 (2024). https://doi.org/10.1186/s12985-024-02442-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-024-02442-7