Abstract
Background
Human adenoviruses (HAdV) have been known to cause a range of diseases, including respiratory tract infections (RTIs). However, there is limited information available regarding the genotype diversity and epidemiology of HAdV associated with RTIs in Nanning.
Methods
Between June 2019 and December 2021, throat swab, nasal swab, or nasopharyngeal swab samples were obtained from individuals hospitalized with respiratory tract infections (RTIs). Statistical software was used to analyze the epidemiological data. The highly conserved 132-bp gene region of the HAdV hexon was targeted for the detection of HAdV using a qPCR assay. An 875-bp hexon gene fragment was subjected to phylogenetic analysis.
Results
Significant variations were observed in the age and gender distribution of HAdV-positive patients (P = 0.004 and P = 0.025, respectively). The age distribution of HAdV-positive patients showed that 67.89% of those who tested positive were the age group of 0–6 years. Furthermore, the prevalence of HAdV detection was highest during spring and autumn, with a peak in February. Additionally, genotyping of the 36 HAdV-positive samples with 875-bp fragments identified the presence of circulating HAdV species B, C, and E in Nanning between 2019 and 2021.
Conclusions
This study identified an association between HAdV prevalence and age as well as season. Among hospitalized patients with RTIs in Nanning, HAdV-B, HAdV-C, and HAdV-E were found to be co-circulating. The most commonly detected genotypes were HAdV-C1, HAdV-C6, and HAdV-E4.
Similar content being viewed by others
Background
Human adenoviruses (HAdV) are DNA viruses that belong to the Adenoviridae family and lack an enveloped structure. Their genome is approximately 36Kb in size and encodes about 40 proteins, including Penton base, Hexon, and Fiber proteins [1]. HAdV can infect various tissues and organs, causing a range of illnesses with varying severity, such as sore throat, rhinitis, fever, pneumonia, and bronchitis [2, 3]. While anyone can be affected by HAdV, individuals with weakened immune systems, cardiovascular disease, and young children are at a higher risk of developing severe forms of the disease [4, 5].
HAdV infections are often underreported worldwide, and the distribution of adenovirus types can vary across different geographic regions and human populations. To date, approximately 110 HAdV genotypes have been identified and classified into seven species (A-G) within the Mastadenovirus genus based on their physical, chemical, and biological properties [6]. Among these, genotypes 3, 4, 7, 14, 21, and 55 are known to cause severe infections and have been linked to global outbreaks [7,8,9]. In recent years, new HAdV genotypes with novel pathogenicity and epidemic characteristics have emerged, posing new threats and challenges to public health [10]. Therefore, it is essential to investigate the molecular epidemiological characteristics of HAdV-induced acute respiratory tract infections.
HAdV particles are composed of 252 putamens, including 240 hexons, 12 pentons, and 12 fibers. Hexons play a critical role as type-specific and species-specific antigens that are highly susceptible to immune selection. The hypervariable regions (HVR1-7) within hexons contain numerous antigen epitopes, making them particularly sensitive to immune selection. A recent study conducted in Nanning, China, from June 2019 to December 2021 aimed to investigate the epidemiological, clinical, and molecular characteristics of HAdV infections among patients with respiratory tract infections (RTIs) who tested negative for influenza. The study also explored the link between HAdV infection and RTI symptoms to provide insights into controlling and preventing HAdV infection in China.
Materials and methods
Patient specimens
In this study, a total of 8,315 samples were collected from patients with respiratory tract infections (RTIs) at Nanning First People’s Hospital and Nanning Maternal and Child Health Care Hospital in Nanning, China, between June 2019 and December 2021. All participants were fully informed about this influenza epidemiological surveillance and provided written informed consent prior to enrollment in the study enrollment in the study. An average of 280 samples were collected per month during the study. RTI illness was defined as the presence of at least two of the following influenza-like symptoms within three days: fever, cough, nasal obstruction, expectoration, sneezing, and dyspnea. The collected specimens were stored in Yocon virus preservation solution (MT0301), which contained Hank’s medium with streptomycin, antifungal antibiotics, BSA (V), cryoprotectant, biological buffer, and amino acids. The samples were transported to the laboratory on ice and stored at -80℃ until further processing. Clinical data of the patients were obtained from the hospital database.
Screening for influenza viruses in initial RTI patients
To exclude RTI patients who tested positive for influenza, all RTI patients underwent initial screening. Total viral nucleic acids were extracted from 200 µL of each clinical specimen using the Prefill Viral Total NA Kit 4 × 48 preps for KingFisher FLEX (Fisher Scientific LabServ), following the manufacturer’s instructions. The detection of influenza viruses was carried out using a qPCR assay that targeted specific primers for A type (Forward: 5’-GAC CRA TCC TGT CAC CTC TGA C-3’; Reverse: 5’-GGG CAT TYT GGA CAA AKC GTC TAC G-3’) and B type (Forward: 5’-TCC TCA ACT CAC TCT TCG AGC G-3’; Reverse: 5’-CGG TGC TCT TGA CCA AAT TGG-3’), with a common probe for A and B types (5’HEX-CCA ATT CGA GCA GCT GAA ACT GCG GTG-BHQ2 3’). The qPCR cycling program included 50 °C for 30 min, 95 °C for 15 min, 5 cycles of 95 °C for 15 s, and 50 °C for 30 s, 72 °C for 1 min, followed by 40 cycles of 95 °C for 15 s, and 55 °C for 45 s. Samples with a cycle threshold (Ct) value < 38 were considered positive for influenza virus.
The inspection method of HAdV in influenza-negative specimens
The total nucleic acid of each clinical specimen was extracted by using the Prefill Viral Total NA Kit 4 × 48 preps for KingFisher FLEX(Fisher Scientific LabServ)according to the manufacturer’s instructions. HAdV detection was performed using qPCR assay targeting the highly conserved gene region (132-bp) of the HAdV hexon. QuantiTect Probe RT-PCR Kit (200)(QIAGEN) (AppliedBiosystems, USA) was used to amplify HAdV hexon DNA using specific primers (Forward:5’-CAGGACGCCTCGGRGTAYCTSAG-3’; Reverse: 5’-GGAGCCACVGTGGGRTT-3’) and probe (5’FAM-CCGGGTCTGGTGCAGTTTGCCCGC-BHQ1-3’). The qPCR cycling program included 50 °C for 30 min, 95 °C for 15 min, followed by 5 cycles of 95 °C for 15 s, 50 °C for 30 min, and 72 °C for 1 min, follow by 40 cycles of 95 °C for 15 s, and 60 °C for 45s. Samples with acycle threshold (Ct) < 38 were regarded as positive.
HAdV genotyping and phylogenetic analysis
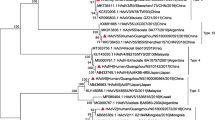
HAdV genotyping was performed using nested PCR targeting the hypervariable region [11]. The primers used were forward 5’-TTCCCCATGGCNCACAACAC-3’ and reverse 5’-GCCTCGATGACGCCGCGGTG-3’. Samples that failed to amplify were defined as untyped. The nested-PCR products were sequenced by TaKaRa LA Taq with GC Buffer(Takara Code No.RR02) and the acquired hexon gene sequences were used together with 26 HAdV strain sequences downloaded from GenBank to construct the phylogenetic tree. The Maximum Likelihood (ML) method in MEGA 7.0 software was used for phylogenetic analysis. The evolutionary tree was evaluated using 1000 bootstrap replicates to verify the HAdV genotypes.
Statistical analysis
The percentage of HAdV-positive specimens was calculated by dividing the number of positive samples by the total samples collected during the same time period. The detection rates of HAdV among different populations and seasons were evaluated using the Chi-square and Fisher’s exact tests, with P-values < 0.05 considered statistically significant. Sequence alignment and phylogenetic analysis were conducted using MEGA7.0. Epidemiological data analysis and graph drawing were performed using SPSS26.0 and R 4.2.0 software.
Results
Characteristics of patients
During the period from June 2019 to December 2021, a total of 2838 samples were collected from Nanning First People’s Hospital,1405 (49.51%) were male and 1433 (50.49%) were female, resulting in a sex ratio of 0.98:1 (Additional file 1: Table S1). A total of 5477 samples were collected from Nanning Maternal and Child Health Care Hospital,3240 (59.16%) were male and 2237 (40.84%) were female, resulting in a sex ratio of 1.45:1 (Additional file 1: Table S2). A total of 8315 samples were collected from the two hospitals; among them, 4645 (55.86%) were males, and 3670 (44.14%) were females, resulting in a sex ratio of 1.27:1. The age range was from 1 month old to 95 years old with an average age of 12 years and a median age of 4 years old (IQR: 1–20 years old). HAdV is prone to infect immunocompromised people, especially in young children who lack humoral immunity [3, 12, 13]. For further comparison, patients were categorized into five age groups: infants (0 ~ 6 year), youth (~ 20 year), prime of life (~ 40 year), middle age (~ 60 year) and the elderly (~ 95year). Out of all patients, 218 (2.62%) tested positive for HAdV infection, and there was a significantly different detection rate among age groups (P = 0.004). Among the 218 HAdV-positive patients, 138 (63.30%) were male, and 80 (36.70%) were female, with a sex ratio of 1.725:1 (Table 1). Additionally, we randomly selected 100 influenza positive patients to dest HAdV, and found 3.39% HAdV-positive patients.
Epidemiology of HAdV
The 0–6 age group had the highest rates of HAdV infection, followed by the 7–20 age group, then the 21–40 age group. The lowest rates were observed in the 71–95 age group (Fig. 1A). There was a significant variation in the prevalence of HAdV infection throughout the years 2020 and 2021 (P < 0.001), with the highest detection rate occurring from August to February (71.43%, 100 out of 140 cases), and a peak in February (15.71%, 22 out of 140 cases) (Fig. 1B). The infection of HAdV in different periods is shown in Fig. 1C. The prevalence of HAdV infection across all four age groups mirrored the overall prevalence over the months from June 2019 to December 2021 (Fig. 1D-G). These findings suggest that HAdV infection is seasonal and may be influenced by age.
The distribution of HAdV infections across age groups over different time periods. (A) HAdV Infection Distribution across Age Groups (0–95 years). (B) Monthly HAdV infection status from 2020–2021. (C) HAdV infection in each month from June 2019 to December 2021. (D) Monthly HAdV infection status in the 0–6 years old group from June 2019 to December 2021. (E) Monthly HAdV infection status in the 7–20 years old group from June 2019 to December 2021. (F) Monthly HAdV infection status in the 21–40 years old group from June 2019 to December 2021. (G) Monthly HAdV infection status in the 41–60 years old group from June 2019 to December 2021
HAdV genotyping and phylogenetic analysis
After amplifying the hexon gene using nested-PCR products with Sanger sequencing, 36 HAdV-positive samples with 875-bp fragments were obtained and successfully genotyped. In our research project, we conducted an analysis of 36 samples using phylogenetic methods with maximum likelihood method in MEGA 7.0 based on the hexon gene sequence. Our findings indicate the presence of three distinct HAdV genotypes. The phylogenetic analyses showed that 8 cases belonged to species B (HAdV-B1, HAdV-B7, HAdV-B14), 22 belonged to species C (HAdV-C1, HAdV-C2, HAdV-C5, HAdV-C57, HAdV-C6), and 6 belonged to species E (HAdV-E4). HAdV-C1 was the most prevalent genotype (10/36), followed by HAdV-C6 and HAdV-E4 (Fig. 2). These results indicate that species B, species C and species E was circulated in Nanning from 2019 to 2021, making up 22.22%, 61.11% and 16.67% of the isolates, respectively.
Discussion
HAdV is associated with various clinical manifestations, including hepatitis,gastroenteritis, meningitis, cystitis, conjunctivitis, upper and lower respiratory tract infections, and myocarditis etc. [14,15,16,17,18,19,20]. Moreover, HAdV infection spreads easily, is highly contagious in some cases, can cause local outbreaks, is associated with a severe course, and occasionally leads to fatal outcomes even in immunocompetent individuals [21,22,23,24,25]. Most HAdV species are observed to have a global circulation, but the predominant types vary among countries or geographic regions and undergo changes over time [26,27,28]. An increased number of HAdV types are now emerging from genomic analyses. Most importantly, there is no standardized clinical treatment, HAdV is also difficult to prevent,and the ECIL does not recommend prophylactic antiviral therapy with currently available virustatic drugs [29]. Therefore, our objective was to ascertain the distribution of HAdV infections by age and gender in these hospitals and to monitor the prevalence of HAV. Additionally, we examined the genetic diversity of HAV among different age groups and months.
Human adenovirus (HAdV) can cause respiratory tract infections (RTIs) with clinical symptoms that resemble those caused by other respiratory pathogens such as influenza and parainfluenza viruses [30]. This makes it challenging to diagnose HAdV infections based solely on symptoms. Therefore, rapid and effective diagnostic methods are crucial for identifying and genotyping HAdV. In this study, a qPCR assay was developed to detect and quantify HAdV in nasal and pharyngeal aspirate (NPA) specimens collected from 8,315 individuals. Out of the total specimens screened, 218 (2.62%) tested positive for HAdV, which is lower than the reported prevalence of HAdV in conjunction with avian influenza (ranging from 1.70 to 13.90%) [11, 31, 32]. In addition, the detection rate of HAdV varied across different regions in China. For instance, in Zhejiang province from 2006 to 2012, the detection rate of HAdV in hospitalized children with acute lower respiratory tract infections was 0.63%, while in Shenzhen city from 2012 to 2015, it was 2.24% [33, 34]. This study also found differences in the detection rate based on sex composition, age distribution, and seasonal effects.
Our study found that the highest prevalence of HAdV occurred during the autumn and winter seasons (71.43% from August to February), and the peak prevalence was observed in February. Similar seasonal patterns have been observed in other studies conducted in Northern China and Mexico [35, 36]. However, some previous studies have suggested that the detection rates of HAdV are positively associated with the monthly mean temperature and sunshine duration, while being negatively correlated with wind speed [7]. It should be noted that Nanning experiences a prolonged period of high temperatures from May to October, with the average daily maximum temperature exceeding 30 °C. From November to April, the average temperature is around 15 °C. This may account for differences in the results of this study compared to those conducted in other cities.
This study indicates that HAdV infections are predominantly observed in children under the age of 6, accounting for 67.89% of cases, highlighting the importance of HAdV as a pediatric pathogen. These findings are consistent with previous studies that have also reported HAdV infections to be common in young children [32, 37, 38]. HAdV can be easily transmitted through fomites contaminated with infectious bodily fluids. Interestingly, our study found that the detection rate of HAdV was lowest among individuals over the age of 60 (0.45%). However, these findings need to be interpreted with caution as the sample size was small, and longer observation periods may be required to confirm the results.
Our study employed nested-PCR to genotype 218 HAdV samples, resulting in 36 hexon 875-bp sequence. Phylogenetic analysis of these sequences revealed that 8 cases belonged to species B (B1, B7 and B14), 22 cases belonged to species C (C1, C2, C5, C6, C57), and 6 cases belonged to species E(E4). The most commonly found genotype was HAdV-C1 (10/36), followed by HAdV-C6 and HAdV-E4. Several studies have previously reported that the most common HAdV species causing respiratory tract infections (RTIs) in children worldwide are B (B3, B7, B21), C (C1, C2, C5, C6), and E (E4) [39,40,41]. In China, HAdV species B, C, and E are associated with severe pneumonia and are also the most prevalent species. In this study, phylogenetic analysis of 36 samples based on the hexon gene sequence revealed three HAdV genotypes. The results showed that HAdV species B and C were the most commonly found, accounting for 22.22% and 61.11% of isolates, respectively.
Conclusions
This three-year study investigated the prevalence, age distribution, seasonality, and molecular epidemiology of human adenovirus (HAdV) infections associated with respiratory tract infections (RTIs) in Nanning, China, excluding avian influenza. The findings suggest recent changes in the circulating HAdV genotypes associated with RTIs in Nanning. These changes could aid in improving the diagnosis of HAdV-related diseases and developing new detection, treatment, and prevention strategies for clinical settings. However, only 36 sequences of the hexon gene were amplified from 218 HAdV samples in this study. Therefore, further analysis of the full-length genome is necessary to understand the extent of genetic variation and any potential recombination that occurred in the strains identified in this study.
Data Availability
Condensed anonymized data are available from the corresponding author on reasonable request.
Abbreviations
- Ct:
-
cycle threshold
- HAdV:
-
Human adenoviruses
- ML:
-
Maximum Likelihood
- MEGA:
-
Molecular evolutionary genetics analysis
- NPA:
-
nasal and pharyngeal aspirate
- RTIs:
-
respiratory tract infections
- qPCR:
-
quantitative real-time polymerase chain reaction
- SPSS:
-
Statistical product and service solutions
References
Davison AJ, Benkő M, Harrach B. Genetic content and evolution of adenoviruses. J Gen Virol. 2003;84(Pt 11):2895–908. https://doi.org/10.1099/vir.0.19497-0.
Radke JR, Cook JL. Human adenovirus infections: update and consideration of mechanisms of viral persistence. Curr Opin Infect Dis. 2018;31(3):251–6. https://doi.org/10.1097/qco.0000000000000451.
Lion T. Adenovirus infections in immunocompetent and immunocompromised patients. Clin Microbiol Rev. 2014;27(3):441–62. https://doi.org/10.1128/cmr.00116-13.
Huang Y, Wang C, Ma F, et al. Human adenoviruses in paediatric patients with respiratory tract infections in Beijing, China. Virol J. 2021;18(1):191. https://doi.org/10.1186/s12985-021-01661-6.
Sawires R, Osowicki J, Clothier H, et al. Pediatric Hepatitis and respiratory viruses: a spatiotemporal ecologic analysis. Pediatr Infect Dis J. 2023;42(4):276–80. https://doi.org/10.1097/inf.0000000000003828.
Greber UF. Adenoviruses - infection, pathogenesis and therapy. FEBS Lett. 2020;594(12):1818–27. https://doi.org/10.1002/1873-3468.13849.
Liu MC, Xu Q, Li TT, et al. Prevalence of human infection with respiratory adenovirus in China: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2023;17(2):e0011151. https://doi.org/10.1371/journal.pntd.0011151.
Salama M, Amitai Z, Amir N, et al. Outbreak of adenovirus type 55 infection in Israel. J Clin virology: official publication Pan Am Soc Clin Virol. 2016;78:31–5. https://doi.org/10.1016/j.jcv.2016.03.002.
Philo SE, Anderson BD, Costa SF et al. Adenovirus Type 21 Outbreak Among Lung Transplant Patients at a Large Tertiary Care Hospital. Open forum infectious diseases 2018;5(8):ofy188.10.1093/ofid/ofy188.
Mennechet FJD, Paris O, Ouoba AR et al. A review of 65 years of human adenovirus seroprevalence. Expert review of vaccines 2019;18(6):597-613.10.1080/14760584.2019.1588113.
Ahmad S, Malik A, Ullah I, et al. Prevalence of human adenovirus in paediatric patients presenting with Acute respiratory symptoms at different hospitals of Pakistan. J Ayub Med Coll Abbottabad: JAMC. 2023;35(1):37–42.
Nair H, Simões EA, Rudan I et al. Global and regional burden of hospital admissions for severe acute lower respiratory infections in young children in 2010: a systematic analysis. Lancet (London, England) 2013;381(9875):1380-1390.10.1016/s0140-6736(12)61901-1.
Lynch JP 3rd, Kajon AEAdenovirus. Epidemiology, Global Spread of Novel Serotypes, and Advances in Treatment and Prevention. Seminars in respiratory and critical care medicine 2016;37(4):586-602.10.1055/s-0036-1584923.
Shauer A, Gotsman I, Keren A, et al. Acute viral myocarditis: current concepts in diagnosis and treatment. Isr Med Association journal: IMAJ. 2013;15(3):180–5.
de Ory F, Avellón A, Echevarría JE et al. Viral infections of the central nervous system in Spain: a prospective study. Journal of medical virology 2013;85(3):554-562.10.1002/jmv.23470.
Chhabra P, Payne DC, Szilagyi PG et al. Etiology of viral gastroenteritis in children < 5 years of age in the United States, 2008–2009. The Journal of infectious diseases 2013;208(5):790-800.10.1093/infdis/jit254.
Rocholl C, Gerber K, Daly J et al. Adenoviral infections in children: the impact of rapid diagnosis. Pediatrics 2004;113(1 Pt 1):e51-56.10.1542/peds.113.1.e51.
Mameli C, Zuccotti GV. The impact of viral infections in children with community-acquired pneumonia. Current infectious disease reports 2013;15(3):197-202.10.1007/s11908-013-0339-z.
Lynch JP 3rd, Fishbein M, Echavarria M, Adenovirus. Seminars in respiratory and critical care medicine 2011;32(4):494-511.10.1055/s-0031-1283287.
Adenovirus-associated epidemic keratoconjunctivitis outbreaks–four states, 2008–2010. MMWR Morbidity and mortality weekly report 2013;62(32):637–41.
Lewis PF, Schmidt MA, Lu X et al. A community-based outbreak of severe respiratory illness caused by human adenovirus serotype 14. The Journal of infectious diseases 2009;199(10):1427-1434.10.1086/598521.
Savón C, Acosta B, Valdés O et al. A myocarditis outbreak with fatal cases associated with adenovirus subgenera C among children from Havana City in 2005. Journal of clinical virology: the official publication of the Pan American Society for Clinical Virology 2008;43(2):152-157.10.1016/j.jcv.2008.05.012.
Alharbi S, Van Caeseele P, Consunji-Araneta R et al. Epidemiology of severe pediatric adenovirus lower respiratory tract infections in Manitoba, Canada, 1991–2005. BMC infectious diseases 2012;12(55.10.1186/1471-2334-12-55.
Chen SP, Huang YC, Chiu CH et al. Clinical features of radiologically confirmed pneumonia due to adenovirus in children. Journal of clinical virology: the official publication of the Pan American Society for Clinical Virology 2013;56(1):7-12.10.1016/j.jcv.2012.08.021.
Berciaud S, Rayne F, Kassab S et al. Adenovirus infections in Bordeaux University Hospital 2008–2010: clinical and virological features. Journal of clinical virology: the official publication of the Pan American Society for Clinical Virology 2012;54(4):302-307.10.1016/j.jcv.2012.04.009.
Ishiko H, Shimada Y, Konno T et al. Novel human adenovirus causing nosocomial epidemic keratoconjunctivitis. Journal of clinical microbiology 2008;46(6):2002-2008.10.1128/jcm.01835-07.
Ampuero JS, Ocaña V, Gómez J et al. Adenovirus respiratory tract infections in Peru. PloS one 2012;7(10):e46898.10.1371/journal.pone.0046898.
Lin KH, Lin YC, Chen HL et al. A two decade survey of respiratory adenovirus in Taiwan: the reemergence of adenovirus types 7 and 4. Journal of medical virology 2004;73(2):274-279.10.1002/jmv.20087.
Matthes-Martin S, Feuchtinger T, Shaw PJ et al. European guidelines for diagnosis and treatment of adenovirus infection in leukemia and stem cell transplantation: summary of ECIL-4 (2011). Transplant infectious disease: an official journal of the Transplantation Society 2012;14(6):555-563.10.1111/tid.12022.
Yao LH, Wang C, Wei TL et al. Human adenovirus among hospitalized children with respiratory tract infections in Beijing, China, 2017–2018. Virology journal 2019;16(1):78.10.1186/s12985-019-1185-x.
Lu MP, Ma LY, Zheng Q et al. Clinical characteristics of adenovirus associated lower respiratory tract infection in children. World journal of pediatrics: WJP 2013;9(4):346-349.10.1007/s12519-013-0431-3.
Liu C, Xiao Y, Zhang J et al. Adenovirus infection in children with acute lower respiratory tract infections in Beijing, China, 2007 to 2012. BMC infectious diseases 2015;15(408.10.1186/s12879-015-1126-2.
Feng L, Li Z, Zhao S et al. Viral etiologies of hospitalized acute lower respiratory infection patients in China, 2009–2013. PloS one 2014;9(6):e99419.10.1371/journal.pone.0099419.
Wang H, Zheng Y, Deng J et al. Prevalence of respiratory viruses among children hospitalized from respiratory infections in Shenzhen, China. Virology journal 2016;13(39.10.1186/s12985-016-0493-7.
Li Y, Zhou W, Zhao Y et al. Molecular typing and epidemiology profiles of human adenovirus infection among paediatric patients with severe acute respiratory infection in China. PloS one 2015;10(4):e0123234.10.1371/journal.pone.0123234.
Rosete DP, Manjarrez ME, Barrón BL. Adenoviruses C in non-hospitalized Mexican children older than five years of age with acute respiratory infection. Memorias do Instituto Oswaldo Cruz 2008;103(2):195-200.10.1590/s0074-02762008000200012.
Koren MA, Arnold JC, Fairchok MP et al. Type-specific clinical characteristics of adenovirus-associated influenza-like illness at five US military medical centers, 2009–2014. Influenza and other respiratory viruses 2016;10(5):414-420.10.1111/irv.12392.
Demian PN, Horton KC, Kajon A et al. Molecular identification of adenoviruses associated with respiratory infection in Egypt from 2003 to 2010. BMC infectious diseases 2014;14(50.10.1186/1471-2334-14-50.
Pollio AR, Fries AC, Yang Y et al. Clustered cases of human adenovirus types 4, 7, and 14 infections in US Department of Defense Beneficiaries during the 2018–2019 season. Journal of medical virology 2023;95(2):e28571.10.1002/jmv.28571.
Shimada Y, Ariga T, Tagawa Y et al. Molecular diagnosis of human adenoviruses d and e by a phylogeny-based classification method using a partial hexon sequence. Journal of clinical microbiology 2004;42(4):1577-1584.10.1128/jcm.42.4.1577-1584.2004.
Ishiko H, Aoki K. Spread of epidemic keratoconjunctivitis due to a novel serotype of human adenovirus in Japan. Journal of clinical microbiology 2009;47(8):2678-2679.10.1128/JCM.r00313-09.
Acknowledgements
We thank the Nanning First People’s Hospital and Nanning Maternal and Child Health Care Hospital for providing the NPA specimens.
Funding
This work was supported by Nanning science and technology development program(20206124) and Guangxi Key Research and Development Program (GuiKeAB22035027).
Author information
Authors and Affiliations
Contributions
YLH, BX, HQ, CY, and JQQ: designed the study and provided the correlative knowledge. LJY, HQ, LW, BX and JQQ: collected and provided the data. JQQ and TYY extracted data and cleaned data. LJY and TYY generated the figures and tables. YLH, BX, JQQ and TYY: wrote and edited the manuscript. All of the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The project was approved by the Ethics Committee of Nanning Center for Disease Control and Prevention, and the committee’s reference number is 2023004.
Consent for publication
Written informed consent for specimen collection, testing and publication was obtained from all individuals (or their parents) in the study population.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qin, J., Yan, T., Yin, L. et al. Detection of human adenoviruses in influenza-negative patients with respiratory tract infections in Nanning, China. Virol J 20, 171 (2023). https://doi.org/10.1186/s12985-023-02093-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12985-023-02093-0