Abstract
Antifungal resistance remains a significant public health threat, yet poorly investigated. This study for the first time investigated the antifungal profile of moulds isolated from groundwaters in a rural community of Osun State, Southwest Nigeria. Groundwater samples were collected during dry and rainy seasons, and processed for mould isolation using standard methods. The isolates were presumptively identified and screened for in vitro susceptibility using 4 antifungals conventionally employed in clinical cases. Multiple antifungal resistance phenotypes and indices were equally evaluated. Representative of each putatively identified species were confirmed using molecular techniques. A total of 29 and 27 moulds were obtained during the dry and rainy seasons, respectively. Genus Aspergillus was the most prevalent (30.4%). Of the 56 isolates subjected to antifungal susceptibility testing, 55(98%) were resistant to fluconazole, followed by flucytosine 49(88%), ketoconazole 45(80%) and amphotericin B 31(55%). Exactly 46 isolates were multidrug-resistant, 23(50%) each, to 3 and 4 drugs, respectively. The multiple antifungal resistance index (MARI) evaluated was 1 in all the samples A-Q, except C (0.75), transcending the threshold limit of 0.2, indicating the isolates to be of high antifungal usage origin. The molecularly identified species had 99–100% similarity with reference strains from GenBank and evolutionary relationship of taxa revealed 10 distinct clades. The outcome of this study reveals a rise in the frequency of antifungal resistance in moulds towards standard drugs, thus, advocating for adequate investigations targeted at monitoring antifungal resistance in groundwater milieus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The availability and accessibility of clean potable water, an essential resource for well-being and sustainable human living, in many developing countries, especially in rural communities remains grossly inadequate [1]. In rural settings, it is estimated that 8 out of 10 people are without access to potable water. This is occasioned by deteriorating condition of existing pipelines, lengthy years of misuse, mismanagement, overexploitation and contamination of freshwater sources, coupled with climate change [2]. This situation threatens Sustainable Development Goal 6 (clean water and sanitation for all) attainment by 2030, with an estimated annual death of 800,000, if the current trend progresses unchecked [3].
Water for human consumption must satisfy the threshold limits by different regulatory bodies to be considered safe [4]. Several studies reported microorganisms including bacteria, viruses and parasites as major waterborne contaminants [5, 6]. On the other hand, fungi are rarely mentioned [7]. The public health implications of fungal contaminated water are largely unknown, and there is paucity of knowledge on standards to employ in routine water quality checks [8]. Recently, fungi began to receive recognition as an emerging chronic water quality challenge [6].
Fungi are ubiquitous in diverse aquatic milieus, comprising surface, ground and tap water proposed for anthropogenic use [8]. Different species of Acremonium, Acrostalagmus, Alternaria, Arthrinium, Arthrographis, Ascochyta, Aspergillus, Asteroma, Astermella, Aureobasidium, Beauveria, Bionectria, Bipolaris, Cadophora, Candida, Cephalosporium, Chaetomium, Cytospora, Dactylaria, Discosporium, Epicoccum, Exophiala, Fusarium, Gibberella, Gliocladium, Kluyveromyces, Microsporum, Paecilomyces, Penicillium, Sarocladium, Talaromyces, Trichoderma, Mucor, Rhizopus etc. have been isolated from water sources in different countries of the world [8].Their distribution in aquatic milieu results in objectionable conditions in taste and odour [5], allergies and meningitis [9]. Some species produce mycotoxins or other secondary metabolites capable of causing respiratory disorders, cancer and opportunistic infections in immmunocompromised individuals [10, 11].
In the last two decades, potential health challenges associated with fungal water pollution, propelled investigations on bottled mineral water [12, 13], tap water [14,15,16], and water supply systems [17, 18] towards safeguarding public health. Of greater concern is the evolution of resistance to commercially available antifungal agents [19, 20], coupled with the limited discovery of new drugs. Antifungals, including azoles (ketoconazole and fluconazole), pyrimidine analog (flucytosine), and polyenes (amphotericin B) are important in modern clinical practice and extensive agriculture [21, 22], and their application brought appreciable progress to the treatment of animal, human and plant fungal infections [23]. Conversely, their efficacy is being confronted by the increasing rise in drug resistance [24]. In recent times, high level resistance i.e. 100% to ketoconazole and fluconazole [25], 75% to fluconazole [26], 47% to flucytosine [28], and 91% [27] and 67% [25] to amphotericin B have been reported.
In the most populous black African nation Nigeria, it is common for communities that do not have access to treated pipe-borne water to rely heavily on alternative sources, such as groundwater which is perceived clean and safe [2]. When groundwater is polluted with antimicrobial-resistant organisms, they impact health and financial burdens on individuals who rely on the water source for daily survival [2, 29]. In Osun State, Southwestern Nigeria, literatures reveal less represented information on antifungal resistance and dearth of data on the genetic relatedness of fungi in groundwater supplies [30, 31]. Previous studies documented mould contaminants using the phenotypic approach only in water sources in Osun State [30, 31]. In this light, the present investigation, being the first of its kind, investigated the antifungal resistance profile and phylogenetic relationship of moulds isolated from groundwater sources in a rural community of the state.
2 Materials and methods
2.1 Description of the study area
Seke is a rural community located along the Dagbolu-Ikirun axis in Ifelodun Local Government Area of Osun State, Nigeria (Fig. 1). It has vast open land, and majority of the dwellers are farmers. They engage in cultivation of major food crops including cowpea, rice, maize, cassava and yam; and cash crops such as cocoa, kolanut and oil palm, amongst others. Some of Seke inhabitants are into poultry farming, and also hunt games. The community lacks basic infrastructures for potable water, forcing the rural settlers to depend on hand-dug wells to meet their daily water needs.
2.2 Sample collection
Grab water sampling technique was adopted in the collection of 17 hand-dug well water sources, once, during the dry (November 2022) and rainy (March 2023) seasons. All samples were designated A-Q. Water samples were aseptically collected in 1 L capacity germ-free plastic containers and conveyed to the laboratory on ice packs for fungal analysis in not more than 6 h of collection. A brand of hygienically packed bottled water served as a negative control.
2.3 Isolation and enumeration of moulds from groundwater samples
The pour-plate technique was used for fungal enumeration. Exactly 1 mL of each water sample was dispensed into sterile Petri dishes, and 20 mL of potato dextrose agar (PDA) medium (Oxoid, UK) supplemented with chloramphenicol was added, gently swirled and allowed to gel. The inoculated agar plates were incubated at 27 ± 2 °C for 5–7 days. Filamentous fungal colonies were counted and expressed as CFU/mL. Individual colonies were subcultured on PDA until pure cultures were obtained and stored on slants at 4 °C until needed. The occurrence (%) of isolates was calculated following Eq. 1.
where, OC = occurrence of fungal isolates; a = number of fungal isolates; and b = total number of fungal isolates [2].
2.4 Phenotypic characterisation of filamentous fungal isolates
Morphological identification was done using macroscopic and microscopic approaches [32]. Macroscopic description of the isolates was done by observing the shape, size, colour and texture of pure fungal colonies on PDA. For microscopic characterisation, a pure colony of 5—7 days old was stained in lactophenol blue on a clean slide and examined under a microscope (X40). The fungal isolates were presumptively named by comparing observed features with those outlined [32].
2.5 Antifungal susceptibility testing
Susceptibility of the recovered fungal isolates to four antifungals comprising ketoconazole, 15 µg; fluconazole, 25 µg; flucytosine, 10 µg; and amphotericin B, 20 µg (Liofilchem, Italy) was determined following the standardized disc diffusion assay as described [29]. The 7-day-old fungal isolates were suspended in physiological saline and precisely 100 µl of 0.5 McFarland standard spore suspension was inoculated by spreading on PDA plates and allowed to dry. Antifungal discs were carefully positioned on the inoculated plates using a disc dispenser (Oxoid, UK) and incubated at 27 ± 2 °C for 2 days. The diameters of clear zones of inhibition were measured, recorded in the nearest millimetres and interpreted as susceptible (S), intermediate (I) and resistant (R) following standard interpretive guideline [33].
The frequency of antifungal-resistant isolates was estimated using Eq. 2.
where ‘E’ is the total of number isolates resistant to a drug and ‘F’ is the total number of isolates involved in the study [2].
2.6 Multiple antifungal-resistant phenotypes and indexing of the isolates
Multiple antifungal-resistant phenotypes (MARP) for each sample were generated for isolates exhibiting resistance to three or more antifungals according to Wose et al. [34]. Multiple antifungal resistance indexes (MARI) for individual hand-dug wells were also assessed using Eq. 3.
where ‘x’ represents the number of antifungal agents to which the isolate was resistant and ‘y’ is the number of antifungal agents tested against one isolate [2].
Likewise, the antifungal resistance index (ARI) for each sampling location was evaluated using Eq. 4.
where ‘A’ is the total number of resistant isolates recorded, ‘N’ is the number of isolates and ‘Y’ represents the total number of antifungals tested [29].
2.7 Molecular confirmation of isolates
2.7.1 DNA extraction
Fungal DNA was extracted from a 5-day-old broth culture using the ZR Fungal/Bacterial DNA kit™ (Zymo Research, USA) according to the manufacturer’s instructions. Quantification and purity of DNA were done using NanoDrop™ One spectrophotometer (Thermo Scientific, UK).
2.7.2 Polymerase chain reaction and gel electrophoresis
The nuclear ribosomal internal transcribed spacer (ITS) region was amplified by PCR with previously described universal primers ITS4 (5′-TCC TCC GCT TAT TGA TATGC-3) and ITS5 (5′-GGA AGT AAA AGT CGT AAC AAGG -3′) [35]. PCR amplicons were analysed using 1.5% (w/v) agarose gel electrophoresis. The gel image was visualized with a Vilber Lourmat E-Box gel documentation imaging to confirm the size of PCR products. The expected amplicon size of the primers is between 300 and 600 bp.
2.7.3 Amplicon sequencing, deposition into GenBank
PCR products were cleaned up using an enzymatic method (ExoSAP-IT™ PCR Product Cleanup Reagent (Thermofisher, UK)) according to the manufacturer’s instructions. Sanger sequencing was performed using the Nimagen, Brilliant Dye™ Terminator Cycle Sequencing Kit V3.1, following the manufacturer’s instructions. Sequence similarities of the generated ITS region were calculated using the Basic Local Alignment Search Tool (BLASTn), for homology to identify the fungal isolates [36]. Sequences were deposited in the GenBank® and for accession numbers assignment.
2.7.4 Phylogenetic analysis
Evolutionary history was inferred between 44 nucleotide sequences using the Neighbor-Joining method [37, 38]. The evolutionary distances were computed using the Maximum Composite Likelihood method [39] and are in the units of the number of base substitutions per site. All ambiguous positions were removed for each sequence pair (pairwise deletion option). There were a total of 1166 positions in the final dataset. Evolutionary analyses were conducted in MEGA X [40].
3 Results
3.1 Enumeration of moulds
The frequency of moulds in the samples ranged from 0 to 4 CFU/ml across both seasons. Moulds were detected in all the samples except A, D and E in the rainy season. Overall, 29 and 27 moulds were recovered from dry and rainy seasons respectively (Table 1). The negative control showed no growth.
3.2 Presumptive identification of the isolates
Morphologically, 6 genera of fungi belonging to 10 species were identified as follows: Aspergillus flavus, A. fumigatus, A. niger, A. welwitschiae, Fusarium equiseti, F. falciforme, Mucor sp., Penicillium citrinum, Rhizopus delemar and Trichoderma longibrachiatum following macroscopic and microscopic description. Representative pictures of the isolates are shown in Fig. 2.
3.3 Occurrence of fungal species in the groundwater samples
The prevalence of moulds in the water samples is as follows: Penicillium citrinum (13;21.43%), Trichoderma longibrachiatum, Aspergillus welwitschiae (11;19.64%), Aspergillus niger (8;14.29%), Fusarium falciforme (4;7.14%), Rhizopus delemar, Aspergillus flavus, Fusarium equiseti (2;3.57%), and Aspergillus fumigatus, Mucor sp. (1;1.79%) (Table 2).
3.4 Antifungal susceptibility pattern
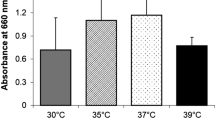
Antifungal susceptibility testing was performed on representative 56 isolates, randomly selected across the sampling points (Fig. 3). Resistance of the isolates to the different antifungal agents approximately ranged from 55 to 98%. The highest resistance was against fluconazole 55(98%), followed by flucytosine 49(88%), ketoconazole 45(80%) and amphotericin B 31(55%). Susceptibility was in descending order amphotericin 25(45%), flucytosine 5(9%) ketoconazole 4(7%) and fluconazole 1(2%) (Fig. 3).
3.5 Multiple antifungal resistance phenotypes and indices of moulds from groundwaters
The results generated for MARP are presented in Table 3. Forty-six (46) of the 56 isolates were multidrug resistant ranging from 3 to 4 drugs. Other isolates (10) were resistant to 1 or 2 antifungal agent(s). In terms of percentage frequency, 23(50%) each of the isolates were resistant to 3 and 4 drugs, respectively (Table 3). In the same vein, the antifungal resistance index (ARI) ranged from 0.17 to 1.00, whereas the multiple antifungal resistance index (MARI) evaluated was 1 except sample D with 0.75 (Table 4).
3.6 Molecular confirmation of fungal isolates
3.6.1 Amplicon size obtained after PCR
The gel electrophoresis image, confirming the amplification of ITS 4 and 5 of the isolates is in Fig. 4. The amplicon sizes ranged between 400 and 600 bp.
Gel electrophoresis of PCR amplified ITS region of the representative isolates. L—Molecular weight marker; 1—Trichoderma longibrachiatum; 2—Aspergillus welwitschiae; 3—A. flavus; 4—Penicillium citrinum; 5—A. niger; 6—Mucor sp.; 7—Fusarium equiseti; 8—F. falciforme; 9—A. fumigatus; 10—Rhizopus delemar
3.6.2 BLASTn analysis
BLASTn analysis of the ITS region of 10 fungal strains from this study was obtained and identified accordingly (Table 5). Our isolates showed between 90% and 100% similarity with their reference species. Aspergillus flavus, A. fumigatus, A.niger, Fusarium equiseti, F. falciforme and Penicillium citrinum had 100% identity with reference strains MK091395, OW985950, MN474007, MN559437, OW985200, and MN069574 respectively. Likewise, Aspergillus welwitschiae, Mucor sp. BAB-3377 and Rhizopus delemar recorded 99% similarity with MK450669, KU504304, and LC514303. Only Trichoderma longibrachiatum had 90% with GenBank strain OQ402425 (Table 5).
3.6.3 Phylogenetic analysis
The evolutionary relationship of taxa as revealed by MEGA-X is shown in Fig. 5. The result revealed the presence of 10 clades. All the investigated strains in this work clustered with selected reference strains from the GenBank (Fig. 5). Aspergillus flavus (OR350638), A. niger (OR743924), A. welwitschiae (OR743925), A. fumigatus (OR74392), Penicillium citrinum (OR743923), Trichoderma longibrachiatum (OR345452), Fusarium falciforme (OR350641), F. equiseti (OR350640), Mucor sp. (OR350639), Rhizopus delemar (OR350642) exhibited close genetic relationship with A. flavus (MT447545), A. aculeatus (KY859793), A. welwitschiae (MK450669), A. fumigatus (OM802836), P. citrinum (MN634544), Trichoderma longibrachiatum (MF967326) and Trichoderma sp. (MK645995), F. oxysporum (EU888922), F. equiseti (MW812252), M. indicus (MT993845) and M. nederlandicus (MZ433254) and Rhizopus sp. (OR304274), respectively (Fig. 5).
4 Discussion
Fungi occur ubiquitously in diverse environments, including aquatic milieus [41, 42]. In this present study, 29 and 27 moulds were isolated from groundwater samples across dry and rainy seasons respectively, suggesting the unsuitability of the water sources for drinking, with its attendant threat to public health [43]. Previous studies isolated 35 and 2 moulds from bottled mineral and tap waters, respectively [44] and 55 from the water distribution system [17]. The widespread distribution of fungi in water has been attributable to factors including location, solar radiation, temperature, ion composition and pH [8]. Additionally, the existence of carbon-based matter, dissolved oxygen concentration, type of water treatment, and biofilm formation influence occurrence of fungi in water environment [8].
Globally, fungal pathogens account for at least 13 million infections resulting in about 1.5 million mortalities annually [45, 46].The moulds detected in the groundwater samples (Table 2) are of a public health concern as they are causative agents of respiratory, mucosal, rhinocerebral, cutaneous and subcutaneous infections [47]. Earlier investigations documented species belonging to Alternaria, Aspergillus, Aureobasidium, Beauveria, Botrytis, Chaetomium, Cladosporium, Epicoccum, Exophiala, Fusarium, Paecilomyces, Penicillium, Purpureocillium, Sarcocladium, Scopulariopsis, Stachybotrys, Trichoderma, Mucor and Rhizopus from different water sources including groundwaters [8, 17, 48, 49]. In the current study, the genera Aspergillus was the most predominant (Table 2), agreeing with previous investigations [50,51,52]. Aspergillus plays important roles in the maintenance of the freshwater environment through the degradation of dead plant litters and animal parts; however, some exist as pathogens or endophytes of aquatic lives [51].
The existence of antifungal resistance in environmental samples is well reported [53,54,55,56,57], but its incidence is scarcely reported in groundwater samples. In the present study, resistance observed amongst isolates ranged from 55 to 98%. The detection of drug resistance suggests the contamination of the environment with antifungal agents. Generally, the natural environment is the main reservoir for moulds, but antifungals used in agriculture may drive resistance development [58]. Seke village is characterized by intense agricultural activities, almost all the hand-dug wells sampled are either/both rarely treated or/and uncovered. This exposes humans to antifungal-resistant pathogens and poses a risk for patients who acquire an infection from environmental antifungal-resistant strains [58].
Microorganisms develop resistance to drugs in a quest to outcompete and persist in their natural ecological systems [60]. The greater than 80% resistance observed for fluconazole, flucytosine and ketoconazole (Fig. 1) was comparable with Shittu et al. [11] who reported resistance to fluconazole (76.19%), ketoconazole (73.80%), clotrimazole (92.86%), griseofulvin (88.09%) and nystatin (100%). This suggests indiscriminate and inappropriate use of the drug in that environment. Antifungal compounds are widely used as therapeutics in clinical and/or veterinary medicine; as antimycotic in body care products [60]; and in agricultural settings as fungicides for plant protection [61]. Once antifungals are in the environment, some accumulate and persist for long periods [62] encouraging the development of resistant strains. Most of the villagers are farmers and regular users of chemicals on their farmlands for prophylaxis purposes. The direct use of fungicides in crops serves as a route of antifungal entry to the environment [63], and subsequently through agricultural runoff [64].
The highest susceptibility recorded in amphotericin B 25(44.64%) suggests it is the therapeutic option in treating fungal infections arising from contaminated groundwater. Generally, amphotericin B resistance is rare unlike the azoles and flucytosine [65]. Currently, there are few therapeutic antifungal alternative drug targets. Antifungal agents consistently damage cell structure and rigidity by interacting with either cell wall or cell membrane constituents. As a result, resistance to one or more classes of antifungals drastically reduces viable treatment options for potentially life-threatening infections [63]. Amphotericin B is the most known member of the antifungal class, polyene. Although the class acts synergistically with some of the most effective antifungal compounds, they are associated with severe nephrotoxicity [66] and low water solubility [67], which limits their use as antifungal drugs [68].
In vitro and in vivo multiple drug resistances are of great therapeutic consequences [29]. The current study elucidated multiple antifungal resistance patterns and found MARI ranging from 0.75–1.00 across both seasons. Fundamentally, diverse human activities and other associated events within the village might be responsible for the observed MARI values (0.75 to 1.00) which denote a high-risk source contamination of the groundwater samples. This reveals that the isolates originated from sources where antifungals are frequently applied [2], possibly from the farmlands in Seke Village where fungicides are frequently applied. Overuse of antifungals in either agriculture or humans exert pressure on fungi, selecting those that have developed resistance, encouraging their survival and proliferation [68, 70]. However, the environment may drive the evolution of antifungal resistance, and may also play a role in human exposure to drug-resistant opportunistic fungal pathogens [71].
The mechanism of resistance in fungi could either be intrinsic or acquired [72]. While intrinsic resistance is inherent, acquired resistance is influenced by antimicrobial selective pressures, and may be caused by mutations, genome rearrangements and/or overexpression of resistance gene products, changes in ergosterol synthesis and aneuploidy [73,74,75,76,77,78].
Molecular characterization provides a way out of misidentification associated with conventional phenotypic identification [79]. Our current investigation employed genetic markers ITS 4 and 5, with amplicon sizes ranging between 400 and 600 bp (Fig. 4). Ezeonuegbu et al. [80] reported an amplicon size of 600 bp in fungi isolated from industrial wastewater. On the other hand, Fujita et al. [81] noted PCR products have band sizes that range from 350–880 bp. Generally, in fungal identification, variance of fungal ITS region and primer combination employed in PCR account for variability in band size [81, 82]. In this study, our isolates recorded 99–100%identity with GenBank strains. Previous works noted 97–99% similarity in fungal isolates from soil and plant parts [83], and 100% in fungal isolates from dumpsite soils [84]. Phylogenetic analysis (Fig. 5) revealed that all the investigated strains are genetically related with previously deposited sequences in the GenBank, including those of environmental sources: soils (MK450669, MW812252, MZ433254), farmland (MF967326), roots (MT447545, KY859793, EU888922), drinking water (MN634544), plant (MK645995), aquaculture water (OR304274), drainage water and sediments (OM802836), oil mill effluent (MT993845)[85].
5 Conclusion
Phenotypic detection and genotypic confirmation of moulds in any groundwater source is indicative of waters not suitable for drinking. The findings of this study signify a high prevalence of drug resistance in the mould contaminants towards standard antifungals. Multiple antifungal-resistant phenotypes and indices assessed imply the presence of antifungal-resistant moulds that can lead to deleterious health complications for individuals who rely heavily on the hand-dug well waters for their domestic purposes. Amphotericin B was identified as a choice drug for infections arising from ingestion of contaminated waters. Groundwaters will continue to experience a rise in the incidence of resistant fungal strains unless indiscriminate use of antifungals in medical (human and veterinary practices) and agricultural fields is restricted. This can be achieved by public awareness and education, legislation and restriction of prescription and dispensing of antifungals to strictly trained and certified specialists. Unrestricted access to fungicides through uncertified retailers should also be discouraged. Good intervention programmes targeted at monitoring antifungal resistance patterns in groundwater is recommended for the Seke rural inhabitants to safeguard public health.
Data availability
All data generated or analysed during this study are included in this published article
References
Milanezi ACM, Witusk JPD, Van Der Sand ST. Antifungal susceptibility of yeasts isolated from anthropogenic watershed. An Acad Bras Ciênc. 2019;91(1): e20170369.
Titilawo MA, Fatoki CO, Titilawo Y, Olaitan JO. Assessment of multidrug-resistant phenotypes and detection of ampicillin-resistant determinants among Escherichia coli isolates of groundwater origin: case study—Osogbo, Southwest Nigeria. Sustain Water Resour Manag. 2023;9:8.
United nations (UN). High-level political forum goals in focus. Goal 6: Ensure availability and sustainable management of water and sanitation for all; 2023. http://unstats.un.org
World Health Organization (WHO). Guidelines for drinking-water quality, WHO, Geneva, Switzerland, 2011. http://apps.who.int/iris/bitstream/10665/44584/1/9789241548151_eng.pdf, 4th edition.
Sonigo P, De Toni A, Reilly K. A review of fungi in drinking water and the implications for human health. Final report WD 0906. Bio Intelligence Service, Paris: France; 2011.
Ashbolt NJ. Microbial contamination of drinking water and human health from community water systems. Curr Environ Health Rep. 2015;2:95–106.
Ren W, Huang T, Wen G. Quantity, species, and origin of fungi in a groundwater-derived water source. Water. 2023;15:1161.
Babič MN, Gunde-Cimerman N, Vargha M, Tischner Z, Magyar D, Veríssimo C, Sabino R, Viegas C, Meyer W, Brandão J. Fungal contaminants in drinking water regulation? a tale of ecology, exposure, purification and clinical relevance. Int J Environ Res Public Health. 2017;14:636.
Oliveira H, Santos C, Paterson R, Gusmão N, Lima N. Fungi from a groundwater-fed drinking water supply system in Brazil. Int J Environ Res Public Health. 2016;13(3):304.
Mhlongo NT, Tekere M, Sibanda T. Prevalence and public health implications of mycotoxigenic fungi in treated drinking water systems. J Water Health. 2019;17(4):517–31.
Shittu OB, Iwaloye OF, Oloyede AR, Oni EO, Ajibola AT, Arowosegbe AO, Oluwasanya GO. Water safety, antifungal-resistant aflatoxigenic Aspergillus flavus and other pathogenic fungi in a community hand-dug wells. J Appl Microbiol. 2022;133:673–82.
Cabral D, Pinto VEF. Fungal spoilage of bottled mineral water. Int J Food Microbiol. 2002;72:73–6.
Ribeiro A, Machado AP, Kozakiewicz Z, Ryan M, Luke B, Buddie AG, Venâncio A, Lima N, Kelley J. Fungi in bottled water: a case study of a production plant. Rev Iberoam Micol. 2006;23:139–44.
Kanzler D, Buzina W, Paulitsch A, Haas D, Platzer S, Marth E, Mascher F. Occurrence and hygienic relevance of fungi in drinking water. Mycoses. 2007;51:165–9.
Gonçalves AB, Santos IM, Paterson RRM, Lima N. FISH and calcofluor staining techniques to detect in situ filamentous fungal biofilms in water. Rev Iberoam Micol. 2006;23:194–8.
Hageskal G, Gaustad P, Heier B, Skaar I. Occurrence of moulds in drinking water. J Appl Microbiol. 2006;102:774–80.
Grabińska-Łoniewska A, Koniłłowicz-Kowalska T, Wardzy´nska G, Boryn K. Occurrence of fungi in water distribution system. Pol J Environ Stud. 2007;16:539–47.
Ma X, Vikram A, Casson LW, Bibby K. Centralized drinking water treatment operations shape bacterial and fungal community structure. Environ Sci Technol. 2017;51:7648–57.
Giri S, Kindo AJ. Evaluation of antifungal susceptibility testing in Candida isolates by Candifast and disk-diffusion method. Indian J Pathol Microbiol. 2014;57:595–7.
Caicedo-Bejarano LD, Osorio-Vanegas LS, Ramírez-Castrillón M, Castillo JE, Martínez-Garay CA, Chávez-Vivas M. Water quality, heavy metals, and antifungal susceptibility to fluconazole of yeasts from water systems. Int J Environ Res Public Health. 2023;20:3428.
O’Neill J. Antimicrobials in agriculture and the environment: reducing unnecessary use and waste (the review on antimicrobial resistance) London:Wellcome Trust; 2015. p.40. www.amr-review.org
Fisher MC, Alastruey-Izquierdo A, Berman J, Bicanic T, Bignell EM, Bowyer P, et al. Tackling the emerging threat of antifungal resistance to human health. Nat Rev Microbiol. 2022;2022:1–15.
Vanreppelen G, Wuyts J, Van Dijck P, Vandecruys P. Sources of antifungal drugs. J Fungi. 2023;9:171.
Ashbolt NJ, Amezquita A, Backhaus T, Borriello P, Brandt KK, Collignon P, et al. Human health risk assessment (HHRA) for environmental development and transfer of antibiotic resistance. Environ Health Perspect. 2013;121(9):993–1001.
dos Santos Júnior CJ, de Lima Melo AR, do Nascimento JM, da Silva SM, dos Santos Araújo MA, Souza AK. Evaluation of susceptibility and response in the surface of agents of surface mycoses (Trichophyton mentagrophytes; T. tonsurans) to antifungal drugs of interest in a medical clinic. ABCS Health Sci. 2021;46:e021203.
Sriramajayam L, Kaur R, Dhakad MS, Gulati A. Antifungal resistance profile of fungal isolates from fungal Rhinosinusitis patients: a study from tertiary care hospital. J Lab Physician. 2023;15(4):488–92.
Li Y, Wang H, Zhao Y-P, Xu Y-C, Hsueh P-R. Antifungal susceptibility of clinical isolates of 25 genetically confirmed Aspergillus species collected from Taiwan and Mainland China. J Microbiol Immunol Infect. 2020;53(1):125–32.
Frías-De-León MG, Hernández-Castro R, Vite-Garín T, Arenas R, Bonifaz A, Castañón-Olivares L, Acosta-Altamirano G, Martínez-Herrera E. Antifungal resistance in Candida auris: molecular determinants. Antibiotics. 2020;9(9):568.
Titilawo Y, Sibanda T, Obi L. Okoh A Multiple antibiotic resistance indexing of Escherichia coli to identify high-risk sources of faecal contamination of water. Environ Sci Pollut Res. 2015;22:10969–80.
Bisi-Johnson MA, Adediran KO, Akinola SA, Popoola EO, Okoh AI. Comparative physicochemical and microbiological qualities of source and stored household waters in some selected communities in Southwestern Nigeria. Sustainability. 2017;9:454.
Adeyemi FM, Wahab AA, Oyelami CA, Oyedara OO, Titilawo MA, Adebunmi AA, Awoniyi IO. Hydrology survey and water qualityassessment of water sources in three selected towns in Osun State, Southwest Nigeria. Int J Energ Water Res. 2022;7:271–84.
Barnett HL, Hunter BB. Illustrated genera on imperfect fungi. 4th ed. St. Paul, Minnessota, USA: The American Phytopathological Society; 1999.
Clinical and Laboratory Standards Institute (CLSI). Methods for antifungal disk diffusion susceptibility testing of filamentous fungi. CLSI document M51-P (ISBN 1-58238-702-2), Wayne, Pennsylvania: USA; 2009.
Wose KCN, Ateba N, Kawadza TD. Antibiotic resistance profiles of Escherichia coli isolated from different water sources in the Mmabatho locality, North-West Province. South Africa Res Lett. 2010;106(1–2):44–9.
White TJ, Bruns TD, Lee SS, Taylor JW. Amplification and direct sequencing of fungal ribosomal RNA genes for phylogenetics. In: Innis MA, Gelf DH, Sninsky JJ, White TJ, editors. PCR protocols: a guide to methods and application. Academic Press: San Diego; 1990. p. 315–22.
Altshul SF, Madden TL, Schäfer AA, Zhang Z, Miller W, Lipman DJ. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 1997;25:3389–402.
Saitou N, Nei M. The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol. 1987;4:406–25.
Felsenstein J. Confidence limits on phylogenies: an approach using the bootstrap. Evolution. 1985;39:783–91.
Tamura K, Nei M, Kumar S. Prospects for inferring very large phylogenies by using the neighbor-joining method. Proc Natl Acad Sci. 2004;101:11030–5.
Kumar S, Stecher G, Li M, Knyaz C, Tamura K. MEGA X: molecular evolutionary genetics analysis across computing platforms. Mol Biol Evol. 2018;35:1547–9.
Mesquita-Rocha S, Godoy-Martinez PC, Gonçalves SS, et al. Water supply system as a potential source of fungal infection in paediatric haematopoietic stem cell units. BMC Infect Dis. 2013;26(13):289.
Akinde SB, Olaitan JO, Ajayi EI, Adeniyi MA, Ige OO, Adebooye OC. Fungal quality and molecular characterisation of aflatoxin-producing Aspergillus species in irrigation water and fresh vegetables in Southwest Nigeria. Jordan J Agric Sci. 2018;14(1):51–70.
EEC. Council directive 98/83/EC on the quality of water intended for human consumption. Off J Euro Commun. 1998;L330:32–54.
Yamaguchi MU, Rampazzo RCP, Ogatta SFY, Nakamura CV, Ueda-Nakamura T, Filho BPD. Yeasts and filamentous fungi in bottled mineral water and tap water from municipal supplies. Braz Arch Biol Technol. 2007;50(1):1–9.
Brown GD, Denning DW, Gow NA, Levitz SM, Netea MG, White TC. Hidden killers: human fungal infections. Sci Transl Med. 2012;4:165rv13.
Brown GD, Denning DW, Levitz SM. Tackling human fungal infections. Science. 2012;336:647.
De Hoog GS, Guarro J, Gene J, Figueras MJ. Atlas of clinical fungi: electronic version 4.0. Centraalbyreau vour schhimmelculyures: utrecht, The Netherlands; 2014. Accessed 4 April, 2023.
Kinsey GC, Paterson RRM, Kelley J. Methods for the determination of filamentous fungi in treated and untreated waters. J Appl Microbiol. 1999;85:214–24.
Rankovic B. Five Serbian reservoirs contain different fungal propagules. Mycologia. 2005;97:50–6.
Ali EAM, Abdel-Rahman TMA, Sayed MA, Abd AlKhalek SH. Occurrence of fungi in drinking water sources and their treatment by chlorination and UV-irradiation. Egypt J Bot. 2017;7(3):621–32.
Heo H, Hong K, Yang H, Lee HB, Chi Y-J. Diversity of Aspergillus, Penicillium, and Talaromyces species isolated from freshwater environments in Korea. Mycobiology. 2019;47(1):12–9.
Góralska K, Błaszkowska J, Dzikowiec M. The occurrence of potentially pathogenic filamentous fungi in recreational surface water as a public health risk. J Water Health. 2020;18:2.
Bader O, Tunnermann J, Dudakova A, Tangwattanachuleeporn M, Weig M, Gross U. Environmental isolates of azole-resistant Aspergillus fumigatus in Germany. Antimicrob Agents Chemother. 2015;59:4356–9.
Chowdhary A, Meis JF. Emergence of azole resistant Aspergillus fumigatus and one health: time to implement environmental stewardship. Environ Microbiol. 2018;20:1299–301.
Assress HA, Nyoni H, Mamba BB, Msagati TA. Occurrence and risk assessment of azole antifungal drugs in water and wastewater. Ecotoxicol Environ Saf. 2020;187: 109868.
Fisher MC, Hawkins NJ, Sanglard D, Gurr SJ. Worldwide emergence of resistance to antifungal drugs challenges human health and food security. Science. 2018;360(6390):739–42.
Rhodes J, Abdolrasouli A, Dunne K, Sewell TR, Zhang Y, Ballard E, et al. Population genomics confirms acquisition of drug-resistant Aspergillus fumigatus infection by humans from the environment. Nat Microbiol. 2022;7:663–74.
Skaar I, Abdellaue A, Andersen CT, Ardenrup MC, Bjørnholt JV, Christensen E, Divon HH, Ficke A, Gaustad P, Strand E, Sørum H, Verweij PE. Knowledge and knowledge gaps on azole resistance in a One Health perspective. Report. 2019; 3:p.15.
Robbins N, Caplan T, Cowen LE. Annual review of microbiology molecular evolution of antifungal drug resistance. Ann Rev Microbiol. 2017;71:753–75.
Richter E, Wick A, Ternes TA, Coors A. Ecotoxicity of climbazole, a fungicide contained in antidandruff shampoo. Environ Toxicol Chem. 2013;32(12):2816–25.
Stevenson E, Warris A, Usher J, Gow N, Gaze W, Murray A. Scoping review into environmental selection for antifungal resistance and testing methodology. Can the novel SELECT method be modified to enable determination of selective concentrations for antifungal resistance? Environment Agency Horizon House, Deanery Road, Bristol BS1 5AH; 2022a. www.gov.uk/environment-agency p.108.
Bhagat J, Singh N, Nishimura N, Shimada Y. A comprehensive review on environmental toxicity of azole compounds to fish. Chemosphere. 2021;262: 128335.
Stevenson EM, Gaze WH, Gow NAR, Hart A, Schmidt W, Usher J, Warris A, Wilkinson H, Murray AK. Antifungal exposure and resistance development: defining minimal selective antifungal concentrations and testing methodologies. Front Fungal Bio. 2022;3: 918717.
Monapathi M, Bezuidenhout C, Rhodes O. Physico-chemical parameters and culturable yeast diversity in surface water: a consequence of pollution. WaterSA. 2020;34(4):593–601.
Vincent BM, Lancaster AK, Scherz-Shouval R, Whitesell L, Lindquist S. Fitness trade-offs restrict the evolution of resistance to amphotericin B. PLOS Biol. 2013;11: e1001692.
Wingard JR, Kubilis P, Lee L, Yee G, White M, Walshe L, Bowden R, Anaissie E, Hiemenz J, Lister J. Clinical significance of nephrotoxicity in patients treated with amphotericin B for suspected or proven aspergillosis. Clin Infect Dis. 1999;29:1402–7.
Lemke A, Kiderlen AF, Kayser O. Amphotericin B. Appl Microbiol Biotechnol. 2005;68:151–62.
Vanreppelen G, Wuyts J, Van Dijck P, Vandecruys P. Sources of antifungal drugs. J Fungi. 2023;9:171.
Aarestrup FM. Occurrence of glycopeptides resistance among Enterococcus faecium isolates from conventional and ecological poultry farms. J Microbial Drug Resist. 1995;1:255–7.
Levin B, Lipsitch M, Pettot V, Schrags S, Anita R, Simonsen L. The population genetics of antibiotics resistance. J Clin Infect Dis. 1997;24:9–16.
Snelders E, Van Der Lee HA, Kuijpers J, Rijs AJ, Varga J, Samson RA, Mellado E, Donders AR, Melchers WJ, Verweij PE. Emergence of azole resistance in Aspergillus fumigatus and spread of a single resistance mechanism. PLoS Med. 2008;5: e219.
Perlin DS, Rautemaa-Richardson R, Alastruey-Izquierdo A. The global problem of antifungal resistance: prevalence, mechanisms, and management. Lancet Infect Dis. 2017;17(12):e383–92.
Lockhart SR, Etienne KA, Vallabhaneni S, Farooqi J, Chowdhary A, Govender NP, et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin Infect Dis. 2017;64(2):134–40.
Chaabane F, Graf A, Jequier L, Coste AT. Review on antifungal resistance mechanisms in the emerging pathogen Candida auris. Front Microbiol. 2019;10:2788.
Berman J, Krysan DJ. Drug resistance and tolerance in fungi. Nat Rev Microbiol. 2020;18(6):319–31.
Young LY, Hull CM, Heitman J. Distruption of ergosterol biosynthesis confers resistance to amphotericin B in Candida lusitaniae. Antimicrob Agents Chemother. 2003;47(9):2717–24.
Kwon-Chung KJ, Chang YC. Aneuploidy and drug resistance in pathogenic fungi. PloS Pathog. 2012;8(11):1003022.
Sionov E, Lee H, Chang YC, Kwon-Chung KJ. Cryptococcus neoformans overcomes stress of azole drugs by formation of disomy in specific multiple chromosomes. PloS Pathog. 2010;6(4): e1000848.
Nilsson RH, Abarenkov K, Larsson KH, Kõljalg U. Molecular identification of fungi: rationale, philosophical concerns, and the UNITE database. Open Appl Informat. 2011;J5:81–6.
Ezeonuegbu BA, Abdullahi MD, Whong CMZ, Sohunago JW, Kassem HS, Yaro CA, Hetta HF, Mostafa-Hedeab G, Zouganelis GD, Batiha GW. Characterization and phylogeny of fungi isolated from industrial wastewater using multiple genes. Sci Rep. 2022;12:2094.
Fujita SI, Senda Y, Nakaguchi S, Hashimoto T. Multiplex PCR using internal transcribed spacer 1 and 2 regions for rapid detection and identification of yeast strains. J Clin Microbiol. 2001;39(10):3617–22.
Krimitzas A, Pyrri I, Kouvelis VN, Kapsanaki-Gotsi E, Typpas MA. A phylogenetic analysis of Greek isolates of Aspergillus species based on morphology and mitochondrial gene sequences. Biomed Res Int. 2013;2013:2603952013.
Alsohaili SA, Bani-Hasan BM. Morphological and molecular identification of fungi isolated from different environmental sources in the Northern Eastern desert of Jordan. Jordan J Biol Sci. 2017;1(3):329–37.
Titilawo MA, Ajani TF, Adedapo SA, Akinleye GO, Ogunlana OE. Aderibigbe D evaluation of lead tolerance and biosorption characteristics of fungi from dumpsite soils. Disc Environ. 2023;1:24.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MAT: Conceptualization, study design, investigation, data interpretation, original draft preparation, and reviewing; POO: Investigation; KKO: Investigation; OOO: Investigation; PDO: Investigation; YT: Investigation, original draft preparation, and reviewing; JOO: Conceptualization, investigation, reviewing, supervision. All authors read and approved the final manuscript draft before submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Titilawo, M.A., Oyebamiji, P.O., Olanipekun, K.K. et al. Antifungal resistance profile and genetic relatedness of moulds from rural groundwater sources. Discov Public Health 21, 109 (2024). https://doi.org/10.1186/s12982-024-00218-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12982-024-00218-6