Abstract
Local skin flaps are frequently employed for wound closure to address surgical, traumatic, congenital, or oncologic defects. (1) Despite their clinical utility, skin flaps may fail due to inadequate perfusion, ischemia/reperfusion injury (IRI), excessive cell death, and associated inflammatory response. (2) All of these factors contribute to skin flap necrosis in 10–15% of cases and represent a significant surgical challenge. (3, 4) Once flap necrosis occurs, it may require additional surgeries to remove the entire flap or repair the damage and secondary treatments for infection and disfiguration, which can be costly and painful. (5) In addition to employing appropriate surgical techniques and identifying healthy, well-vascularized tissue to mitigate the occurrence of these complications, there is growing interest in exploring cell-based and pharmacologic augmentation options. (6) These agents typically focus on preventing thrombosis and increasing vasodilation and angiogenesis while reducing inflammation and oxidative stress. Agents that modulate cell death pathways such as apoptosis and autophagy have also been investigated. (7) Implementation of drugs and cell lines with potentially beneficial properties have been proposed through various delivery techniques including systemic treatment, direct wound bed or flap injection, and topical application. This review summarizes pharmacologic- and cell-based interventions to augment skin flap viability in animal models, and discusses both translatability challenges facing these therapies and future directions in the field of skin flap augmentation.
Similar content being viewed by others
Introduction
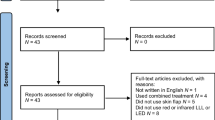
Local skin flaps are frequently employed for wound closure to address surgical, traumatic, congenital, or oncologic defects [1]. Despite their clinical utility, skin flaps may fail due to inadequate perfusion, ischemia/reperfusion injury (IRI), excessive cell death, and associated inflammatory response [2]. All of these factors contribute to skin flap necrosis in 10–15% of cases and represent a significant surgical challenge [3, 4]. Once flap necrosis occurs, it may require additional surgeries to remove the entire flap or repair the damage and secondary treatments for infection and disfiguration, which can be costly and painful [5]. In addition to employing appropriate surgical techniques and identifying healthy, well-vascularized tissue to mitigate the occurrence of these complications, there is growing interest in exploring cell-based and pharmacologic augmentation options [6]. These agents typically focus on preventing thrombosis and increasing vasodilation and angiogenesis while reducing inflammation and oxidative stress. Agents that modulate cell death pathways such as apoptosis and autophagy have also been investigated [7]. Implementation of drugs and cell lines with potentially beneficial properties have been proposed through various delivery techniques including systemic treatment, direct wound bed or flap injection, and topical application (Fig. 1).
This review summarizes pharmacologic- and cell-based interventions to augment skin flap viability in animal models, and discusses both translatability challenges facing these therapies and future directions in the field of skin flap augmentation.
Pharmacologic treatments
First-line interventions for improving flap viability typically include surgical technique optimization and hemodynamic support, usually followed by pharmacological or cell-based therapies as second-line interventions to ensure the best flap survival. Insufficient blood supply and IRI are the two main causes of distal flap necrosis [2]. To improve blood supply and decrease the incidence and effects of IRI, a variety of pharmacologic interventions have been explored for their observed or theoretical utility in improving skin flap viability. While many medications have several benefits, they will be discussed broadly as antithrombotic agents, vasodilators, pro-angiogenic therapies, antioxidants and anti-apoptotics, upregulators of autophagy, and anti-inflammatory drugs.
Antithrombotic agents
Arterial or venous thrombosis can impair capillary circulation and nutrient supply to the flaps [2, 8]. Venous obstruction occurs more frequently than arterial obstruction due to lower flow rate and thin, friable nature of veins. Thrombosis could be induced via two mechanisms: (1) increased platelet and neutrophil adhesivity due to local injury that releases free radicals, enzymes, and cytokines to obstruct the capillaries and (2) activation of the coagulation cascade to form a clot [8]. Anti-thrombotic drugs can reduce thrombotic risk and improve blood circulation to reduce tissue necrosis and improve flap viability (Table 1). They can be categorized into two groups: anti-platelet agents or antithrombin activator/clotting factor inhibitors. Clinically, both aspirin and heparin are given empirically to patients prior to undergoing skin flap surgery with the goal of improving circulation and thereby flap survival.
Aspirin is an irreversible inhibitor of the enzyme cyclooxygenase, the key enzyme in metabolizing arachidonic acid. Aspirin has been shown to be highly effective in improving skin flap viability, hence its frequent use in clinical settings. While some studies indicate that this effect is mediated by inflammation modulation and improvement of flap circulation through direct vasodilation more so than an anti-platelet aggregation effect [15], others indicate all three of these effects contribute meaningfully to aspirin’s benefits [16]. Clopidogrel (an irreversible platelet aggregation inhibitor), alternatively, has also been shown to improve skin flap viability but through a primarily antiaggregatory effect [17].
Several anticoagulants have been studied in animal local skin flap survival models, many of which are also employed clinically. Key differences among these agents are their mechanisms of action, routes of administration, and clinical indications. Low molecular weight Heparin (LMWH) and Hirudin are subcutaneously administered anticoagulants, while Bivalirudin and Activated Protein C can be administered intraperitoneally or intravenously. In contrast, Hirudoid is a topical anti-inflammatory, antithrombotic, and fibrinolytic drug with reduced systemic effects. A study in 2019 by Livaoğlu et al. showed that daily topical Hirudoid application on random dorsal skin flaps in rats resulted in significantly lower inflammation, edema, and intravascular thrombosis scores, as well as a smaller flap necrosis area (31.7% vs. 48.9%) compared to control animals [8]. Subcutaneous injection of natural and recombinant Hirudin and intraperitoneal injection of Bivalirudin following creation of random flaps in rats also both increased flap survival rates. The mechanisms underlying this effect may involve reducing thrombosis, improving flap blood supply, and upregulation of vascular endothelial growth factor (VEGF) activity, which promotes formation of new blood vessels in the flap [11, 10].
Another study investigated subcutaneous use of LMWH—which acts by enhancing antithrombin III—in four pedicled-flap models in rabbits and found that LMWH had a rapid therapeutic effect on flap circulation and survival length [9]. All of the congested flaps survived when treated with LMWH, while the control group showed necrosis in one-sixth of the flap area [9]. Finally, intravenous administration of Activated Protein C in rats also showed significantly improved flap survival in the experimental group compared to the control (68.9% vs. 39.3%, respectively) 1 week after the injection [12]. Interestingly, potentially due to time-sensitive transcriptional changes, earlier Activated Protein C injections prior to elevation of the flap were associated with higher flap survival [12]. However, disadvantages of Activated Protein C treatment include increased risk for significant hemorrhage during flap dissection when administered preoperatively, short half-life of the drug, and potential need for supraphysiologic doses as much as 1000-fold higher than those safely used in patients [12].
Vasodilators
Vasoconstriction following skin flap elevation is a common cause of flap necrosis [18]. Release of norepinephrine from flap dissection and injured sympathetic neurons produces a local hyperadrenergic environment [19]. Consequently, nutrient-rich blood flow to the distal aspect of the flap may become restricted, and blood is redirected through low-pressure arteriovenous shunts, increasing the risk of irreversible ischemic necrosis [18, 19]. Vasodilators to improve flap viability (Table 2) act directly on arteriolar smooth muscle and can be categorized into three groups: those that target the nitric oxide synthase (NOS) pathway to release nitric oxide (NO), those that target the NOS pathway in combination with other mechanisms, and those that induce vasodilation through non-NOS-mediated mechanisms.
Examples of agents that target the NOS pathway include sodium nitroprusside (SNP), diethylenetriamine NONOate (DETA-NO), sildenafil, and metformin. Transdermal iontophoretic delivery of NO donors such as SNP and DETA-NO showed significantly improved perfusion in rat skin flaps [20, 26]. Similarly, pre-operative administration of metformin, a primary therapeutic option for type 2 diabetes, has been shown to enhance NOS activity via the 5′ adenosine monophosphate-activated protein kinase pathway, resulting in significant improvements in vasodilation and flap viability in rats [18].
Vasodilating therapies that target NOS signaling in concert with other pathways include vasonatrin peptide (VNP) and a combination treatment of Azelaic acid, minoxidil, and caffeine (AMC). VNP, a synthetic natriuretic peptide derived from the combination of atrial natriuretic peptide and C-type natriuretic peptide, induces smooth muscle vasodilation. In rats, Wang et al. demonstrated these combined effects resulted in a significant increase in mean vessel diameter, blood perfusion volume, and flap viability while reducing thrombosis, inflammatory mediators, and oxidative injury [23]. Like VNP, studies with AMC on rat skin flaps have shown a significant increase in NOS activity [22]. This effect has been attributed to the 5α-reductase inhibitory properties of azelaic acid—a dermatological treatment for skin conditions—which promotes NOS expression and NO production by inhibiting dihydrotestosterone (DHT) synthesis [22]. Azelaic acid has also been found to enhance levels of the anti-apoptotic protein B-cell lymphoma 2 [22]. Multiple animal studies have underscored the utility of NOS pathway modulators in enhancing local flap perfusion and survival, supported by the ubiquitous reduction in flap necrosis observed [18, 20–22].
Agents that facilitate vasodilation through non-NOS pathways that have been studied to promote flap survival include calcitonin gene-related peptide (CGRP), an endogenous hormone known for its potent vasodilatory effects, and nifedipine, a selective calcium channel blocker commonly prescribed for hypertension [19, 25]. While the precise mechanism of CGRP has not been fully elucidated, some of its effect has been attributed to CGRP receptor binding on smooth muscle cells, while nifedipine's effect is associated with the inhibition of the α-2 receptor. Calcitonin gene-related peptide also exhibits anti-inflammatory properties, while nifedipine possesses antioxidant properties, prevents calcium influx, and inhibits platelet aggregation [19, 25, 24]. These multifaceted therapeutic mechanisms highlight the utility of CGRP and nifedipine in optimizing local skin flap survival in rats [19, 25, 24].
Pro-angiogenic therapies
In addition to anti-thrombotic agents and vasodilation to promote blood flow, viability of the distal flap can also be enhanced through vascular formation and remodeling (Table 3) [33]. In ischemic skin flaps, angiogenesis is typically mediated by VEGF and basic fibroblast growth factor (bFGF), which is secreted by keratinocytes and fibroblasts in response to hypoxia [27]. VEGF binds to receptors on the surface of the dermal vascular endothelium to stimulate mitosis, inhibit endothelial cell apoptosis, and enhance vascular permeability and cell migration [27]. Direct injection of VEGF into rat skin flaps has been shown to significantly increase flap viability area (38.9% in the control vs. 80.4% in the VEGF-treated group) [10]. Similarly, upregulation of bFGF expression in the flap bed using plasmid-based methods significantly decreased the area of flap necrosis and enhanced vascularity in dorsal skin flaps. Although both VEGF and bFGF are promising agents to improve vascularization in ischemic flaps, their short half-life, expensive costs, instability requiring complicated storage, and uncertainty regarding effective/safe dosage remain significant limitations which have prompted researchers to investigate alternative angiogenic therapeutics [28, 29].
Atorvastatin, a HMG-CoA reductase inhibitor used clinically in the treatment of dyslipidemia, has also been shown to have biphasic VEGF-mediated angiogenic effects [37]. At high doses, studies have suggested atorvastatin to reduce VEGF expression in various human tissues [38]. However, murine studies have shown lower concentrations to enhance endothelial cell proliferation, migration, and differentiation through upregulation of VEGF [37]. A study by Chen et al. showed 7 days of oral atorvastatin administration after dorsal skin flap elevation in rats enhanced VEGF expression and vascular density, reducing necrosis area by 20% [35].
Finally, some angiogenic therapies possess dual angiogenic and anti-inflammatory/anti-oxidant properties, such as memantine, calcitriol, and vinpocetine. Intraperitoneal injection of memantine, an excitatory amino acid receptor antagonist, calcitriol, a metabolite of vitamin D, and vinpocetine, a derivative of the alkaloid vincamine, have all been demonstrated to promote flap vascularization in rats through upregulation of VEGF production [2, 27, 36]. In addition, these therapeutics may also attenuate oxidative stress, mitigate IRI, and suppress inflammatory responses [2, 27, 36].
Antioxidants and anti-apoptotics
Even in the setting of adequate circulation, transient ischemia can still result in partial flap necrosis due to IRI. IRI can generate excess reactive oxygen free radicals and decrease anti-oxidant defenses, leading to endothelial cell swelling, vasoconstriction, and increased capillary permeability [39]. These changes result in damage to the mitochondrial wall and activate apoptotic pathways [2, 40–43]. Therefore, antioxidant, anti-inflammatory, and autophagic agents have been studied for their utility in reducing oxidative stress and preventing cell death in ischemic flaps.
By interacting with radicals to form less reactive products, anti-oxidant agents have shown promise in reducing IRI as well as increasing flap vascularization and survival in rat abdominal skin flaps (Table 4) [2, 27, 36, 44]. During IRI, lipid peroxidation generates malondialdehyde (MDA) which can crosslink proteins and DNA to damage cells [2, 45]. Superoxide dismutase (SOD) is a metalloprotein that can scavenge superoxide radicals to reduce oxidative stress and is one of the body’s best defenses against free radicals [2]. Angiogenic agents such as memantine, calcitriol, vinpocetine (discussed above in “Pro-angiogenic Therapies” section) have been shown to reduce flap tissue damage and oxidative stress in skin flaps by downregulating MDA and glutathione while increasing SOD levels.
Similarly, enhanced activity of natural cellular defense mechanisms against free radicals through topical/oral administration of tocopherols (vitamin E) and retinoids (vitamin A) or injection of ascorbate (vitamin C) and glutathione have been shown to improve flap survival significantly in rats [49]. Interestingly, various studies have also demonstrated an association between hyperthyroidism and oxidant-mediated tissue damage [50, 51]. In a study by Rahimpour et al. use of anti-thyroid medications propylthiouracil and methimazole were both found to significantly improve random-pattern dorsal skin flap survival in rats by promoting cellular antioxidant activity [46].
Aside from lipid peroxidation, the xanthine oxidase (XO) system in endothelial cells is another major source of free radicals. A study by Rasti-Ardakani et al. showed that treatment pre- and post-skin flap elevation in dogs with an XO inhibitor such as allopurinol allowed flaps to tolerate a longer period of ischemia, with reduced inflammation and smaller areas of necrosis [47]. Importantly, the efficacy of allopurinol to enhance viability may be dependent on tissue- and species-specific XO activity, as this intervention was found to be less successful in preserving skin flap survival in pigs [47, 52].
Upregulators of autophagy
Autophagy is a highly conserved cellular degradation process to protect against metabolic stress, cellular damage, and programmed cell death [53]. Upregulation of autophagy can reduce oxidative stress‐mediated damage, enhance angiogenesis in endothelial cells Ak strain transforming (Akt) pathway activation, and thus improve the survival rate of skin flaps (Table 5) [54].
As discussed earlier, calcitriol has been shown to upregulate VEGF production and attenuate oxidative stress, and this active form of vitamin D has been one of the best studied medications for stimulation of autophagy and relief of IRI. Intraperitoneal injection of calcitriol for 7 days postoperatively was effective in promoting autophagy-mediated angiogenesis and reducing oxidative injury in rat dorsal skin flaps, with 67.6% area of tissue survival compared to 46.8% in control animals [53]. In other rat studies, gastrodin, a chemical compound derived from the orchid Gastrodia elata, has also been shown to upregulate autophagy, resulting in enhanced angiogenesis and reduced cellular apoptosis [56, 55]. Similar injection for 7 days following flap elevation improved survival and increased expression of both VEGF and multiple antioxidant markers including SOD, endothelial NOS, and heme oxygenase-1 [55].
Other compounds capable of stimulating autophagy have also been shown to be effective at promoting skin flap survival in various mouse and rat studies. These include catapol, a biologically active compound found in the flowering plant Rehmannia glutinosa, andorgrapholide, a diterpenoid isolated from the stem and leaves of Andrographis paniculata, and nobiletin, a flavonoid found in citrus fruits [56, 58–57]. Each of these have been shown to positively regulate autophagy, through sirtuin 1, phophosoinositide 3-kinase/Akt, and 5′ adenosine monophosphate-activated protein kinase (AMPK) activation, respectively. Murine flap studies have shown these agents to decrease levels of pro-apoptotic markers, and promote angiogenesis, resulting in improved tissue survival [57]. Collectively, these studies highlight the protective role autophagy may play in promoting tissue survival and spotlight the promise several plant-derived compounds may possess in enhancing random skin flap survival outcomes.
Anti-inflammatory agents
With tissue ischemia, activation of several inflammatory signals occurs [41] which can potentiate evolution of coagulative necrosis and inflammatory cell infiltration [64]. As the extent of necrosis increases, so too does the intensity of inflammation [64]. Agents limiting the inflammatory process may thus be useful to lessen tissue damage and improve flap viability (Table 6).
Interestingly, many members of the most well-known class of anti-inflammatory medications, non-steroidal anti-inflammatory drugs (NSAIDs), have been shown repeatedly to either have unequivocal or negative effects in the setting of skin flaps [70–72]. Indeed, NSAID treatment following skin flap elevation has been associated with poor wound healing, increased incidence of infections and other complications, as well as decreased neovascularization [71]. Despite this finding, anti-inflammatory effects of a number of other therapies have been cited in their success at achieving increased skin flap viability.
Gamma-aminobutyric acid (GABA) receptors, expressed in immune cells, play a role in regulating cytokine secretion and immune cell migration [68]. Elevated GABA levels, primarily synthesized from glutamate, have also demonstrated cytoprotective capabilities, likely due to GABA's inhibitory role as a neurotransmitter [69]. Several GABA-modulating medications have been investigated as potential treatments for enhancing skin flap viability by reducing inflammation. Ivermectin (IVM), originally used as an antiparasitic agent, demonstrated enhanced flap survival in animal studies by upregulating the expression of GABA a1 subunit and GABAB R1 receptor in immune cells [69]. Sodium valproate (SV), commonly prescribed as an anticonvulsant medication, also exerts its effects through the GABA pathway, and SV administration led to increased GABA receptors and inhibition of histone deacetylase (HDAC) signaling. The application of IVM and SV both resulted in suppressed proinflammatory cytokine secretion, significantly reduced necrosis areas, and improved flap viability, indicating the potential clinical value of these agents [68, 69].
Colchicine, a decades-old anti-inflammatory drug used to treat gout, has similarly shown promise in mitigating inflammation and IRI-mediated necrosis through the glutamate pathway, ultimately resulting in enhanced skin flap survival [67]. The application of colchicine to ischemia/reperfusion injured rats reduced proinflammatory cytokines IL-6 and TNF-α and mildly increased glutamate and N-methyl-D-aspartate subunit 2A receptor expression, a glutamate receptor found on nerve cells and keratinocytes of the skin with known cytoprotective capabilities [67]. Furthermore, colchicine inhibited microtubule polymerization, which affects neutrophil adhesion, mobilization, and recruitment. Inflammation was attenuated through increased induction of the M2 macrophage phenotype, which is known for dampening of the immune response [67].
Cell-based therapies
Cell-based therapies harness the self-renewing and regenerative capabilities of living stem cells to improve viability of skin flaps (Table 7). Cell-based therapies are a relatively new strategy to improve flap viability compared to pharmaceutical drugs and may act through various mechanisms, including direct tissue repair, immune modulation, and release of growth factors and cytokines (Fig. 2). They can potentially provide a longer therapeutic effect window due to the self-renewing and differentiating capability of the cells. Additionally, mesenchymal stem cells (MSCs) can differentiate into endothelial cells to form new vessels and significantly lower necrosis rates in rat dorsal skin flaps in ischemia–reperfusion conditions, as shown by Foroglou et al. [76].
Cell-based therapies require the harvest of cells from relevant tissue type and processing prior to usage as a therapy for skin flaps. The most common sources of these cells are adipose tissue, bone marrow, placental amniotic membrane, and the umbilical cord. These cells are typically applied to preclinical murine models via subcutaneous injection, as depicted in a McFarlane flap
MSCs, and particularly adipose-derived stem cells (ADSCs), are the most frequently studied cell types [3], and have been associated with anti-oxidant, vasodilatory, anti-inflammatory, and angiogenic effects [76]. Several sources of MSCs, including ADSCs from lipoaspirate, bone marrow, and human umbilical cord matrix stem cells (hUCMs), have been studied and demonstrate different benefits and drawbacks in terms of therapeutic potential and ease of harvest/isolation.
ADSCs have the benefits of abundant reserves with high proliferating ability, simple harvest with liposuction, and low donor site morbidity. However, the harvested lipoaspirate is initially impure and requires either a large volume or a long period of in vitro expansion to produce a sufficient number of ADSCs for transplantation [73]. ADSCs have been found to effectively reduce distal skin flap necrosis, with a meta-analysis finding that treatment resulted in an absolute risk reduction in necrotic skin area of 22.37% [77]. Augmentation of ADSCs with exosomes stimulated by hydrogen peroxide [78] and preconditioning of ADSCs with hypoxia [79] have been shown to amplify these therapeutic effects. Several studies have isolated various components of ADSCs, such as extracellular vesicles and exosomes and have shown these to independently improve skin flap survival, suggesting contribution of these components to the therapeutic value of these cells [80–83].
MSCs can be isolated from bone marrow and used in cell-based therapies to improve flap viability. Interestingly, while these cells have been shown to stimulate VEGF activity, neovascularization, and collagen density in rat random-pattern skin flaps, they do not appear to have a beneficial effect on the fibroblast number or other biomechanical parameters in flap wound healing [75]. The limited supply and invasive harvesting procedures necessitated by stem cell therapies from the bone marrow are an important limitation their clinical tranlatability [28].
Human umbilical cord matrix stem cells (hUCMs) are derived from human umbilical cord Wharton’s jelly and are more easily isolated in a large number. Compared to BM-MSCs, hUCsM may have more robust proliferation and differentiation capabilities, greater plasticity, and lower immunogenicity. A study by Leng et al. showed that hUCMs promote vascularization by increasing capillary density, enhancing angiogenic growth factors such as VEGF and bFGF levels, and improving the survival of ischemic epigastric mouse flap models [28].
Tissue engineering approaches have also been applied to the field of cell-based therapies for skin flap survival, with a 2022 study by Nazanin et al. exploring the use of placental amniotic membrane as a scaffold source to improve flap viability. From the amniotic membrane, researchers have studied the utility of amniotic membrane sheet (AMS) and micronized amniotic membrane (MAM) products, which contain human amniotic MSCs, a number of angiogenic growth factors, and ECM components to impart tensile strength [74]. While both products were found to be effective treatments to improve rat flap survival, each imparted different therapeutic benefits [74]. Specifically, transplantation of MAM improved the organization of collagen tissue and angiogenesis rate, while AMS had more profound anti-inflammatory effects [74]. AMS treatment was also found to increase epithelialization of keratinocytes and the in-growth of fibroblasts during wound healing [74].
In summary, cell-based therapies offer a promising avenue for enhancing skin flap viability through the utilization of various stem cell types, including mesenchymal stem cells (MSCs), adipose-derived stem cells (ADSCs), and human umbilical cord matrix stem cells (hUCMs). Additionally, the incorporation of tissue engineering approaches, such as placental amniotic membrane, adds further depth to this innovative field of research and presents diverse avenues for improving the survival and quality of skin flaps. While evidence suggests promising utility for stem cells in improving skin flap viability, many factors produced by these cells and their specific effects remain poorly understood. Further characterization of the factors produced by distinct cell lines and their impact on the post-operative skin flap environment will provide a more granular understanding of the possible clinical utility of stem cells for improvement of skin flap viability.
Translatability challenges and future directions
Preclinical investigation of pharmacologic and cell-based therapies has attempted to improve viability through a variety of pathways, drug classes, and stem-cell types. Despite promising results, the translation of these therapies to common clinical practice has yet to be seen. The reasons for this are complex, though several include negative drug side effects, complicated treatment regimens, and high economic/logistic costs. Calcium channel blockers like Nifedipine, for example, can cause palpitations, edema, and constipation, while the antiepileptic Sodium valproate can impede hair growth and amplify weight gain when administered systemically. On the topic of administration, treatment protocols may often be demanding, with some drugs requiring daily injections due to short half-lives and low plasma concentrations. The cost of these agents can also be prohibitive for practical translatability, particularly for growth factors like VEGF and cell-based therapies. Cell-based options are accompanied by several logistical barriers which contribute to their high costs, such as sourcing, expansion, and delivery. Clinical limitations such as immuno-rejection and genetic stability exist as well.
The future of clinical practices to enhance skin flap viability requires clear understanding of pro-survival pathways, as well as validation of results in more rigorous studies. Many of the experiments conducted in this field have utilized small animal models, and large animal models as well as clinical trials with long-term follow-up will ultimately be needed [77].
Furthermore, with promising results demonstrated by induction of ischemia [84] to promote angiogenesis prior to creating a skin flap, interest in preconditioning treatments to prepare a skin region for use as a skin flap has emerged. Studies have reported promising results with hyperbaric oxygen therapy [85, 86] and local warming of the skin using a heat blanket prior to surgery, which have been shown to enhance skin flap survival in pigs [87]. Additionally, advances in flap care are moving toward the direction of combination therapies that promote viability by addressing a variety of pathways simultaneously [22, 88, 89]. For example, one study simultaneously used hyperbaric oxygen therapy to promote angiogenesis and nitroglycerin to promote vasodilation [90]. Another study investigated the synergistic action of azelaic acid, minoxidil, and caffeine to protect against IRI by targeting parallel anti-apoptotic, anti-inflammatory, and antioxidant pathways [22].
As techniques advance, so, too has drug delivery technology. Novel delivery mechanisms for pharmaceutical therapies such as an injectable thermosensitive hydrogel [64] and photocrosslinked gelatin hydrogel implants [91] have been introduced for optimized drug delivery. These gel-based biomaterials allow for controlled release platforms that can be applied directly to the wound bed prior to flap closure, topically to the flap site, injected directly into the flap, or incorporated into dressings [64]. Nanoparticles that encapsulate drugs and target specific tissues or cells within a flap offer controlled release and drug protection, ultimately enhancing delivery and reducing systemic side effects [92].
Since survival rate of compromised skin flaps correlate inversely with time, treatment following the first signs of necrosis—particularly within the first 72-h window—is important to provide timely interventions to minimize the risk of flap necrosis [93, 94]. A recent paper reported bioengineering sensors that use non-invasive electrical measurements to monitor biochemical parameters, such as pH value or dissolved oxygen concentration, and biophysical parameters, like blood flow and temperature, to relay real-time information regarding flap viability may thus be of future value [92]. These sensors allow for timely detection of signs of flap failure, allowing an opportunity for intervention and, ultimately, improved survival [95].
Conclusion
Translational work in the field of skin flaps aimed at augmenting viability has demonstrated significant potential through diverse approaches, drug classes, and cell types. Despite promising results, the translation of these therapies to common clinical practice remains elusive. Challenges such as clinical side effects, complex treatment protocols, high economic and logistic costs, dosing regimens, and incomplete understanding of underlying molecular pathways have hindered their widespread adoption. To overcome these obstacles and pave the way for successful clinical implementation, future research must focus on elucidating the intricate mechanisms of action, conducting rigorous and comprehensive preclinical and clinical trials, adopting a holistic approach through combination therapies, exploring novel delivery methods, and leveraging technological advancements for flap monitoring. Moreover, validating results in large animal models and conducting long-term clinical trials will be crucial for establishing the efficacy and safety of these interventions. Recent advances in preconditioning treatments, combination therapies, drug delivery systems, and monitoring technologies offer hope for overcoming the existing challenges and ultimately enhancing skin flap viability in clinical settings. As the safety and efficacy of pharmaceutical agents in flap viability continue to progress, they hold the potential to significantly improve patient outcomes and contribute to advancements in reconstructive surgery.
Availability of data and materials
Not applicable.
References
Deramo P, Rose J. Flaps: muscle and musculocutaneous. In: StatPearls. StatPearls Publishing; 2023. Accessed July 27, 2023. http://www.ncbi.nlm.nih.gov/books/NBK546581/.
Fan W, Liu Z, Chen J, et al. Effect of memantine on the survival of an ischemic random skin flap and the underlying mechanism. Biomed Pharmacother Biomedecine Pharmacother. 2021;143:112163. https://doi.org/10.1016/j.biopha.2021.112163.
Li Y, Jiang QL, Van der Merwe L, Lou DH, Lin C. Preclinical efficacy of stem cell therapy for skin flap: a systematic review and meta-analysis. Stem Cell Res Ther. 2021;12(1):28. https://doi.org/10.1186/s13287-020-02103-w.
Ozturk A, Fırat C, Parlakpınar H, Bay-Karabulut A, Kirimlioglu H, Gurlek A. Beneficial effects of aminoguanidine on skin flap survival in diabetic rats. Exp Diabetes Res. 2012;2012:721256. https://doi.org/10.1155/2012/721256.
Lin R, Lin J, Li S, et al. Effects of the traditional Chinese medicine baicalein on the viability of random pattern skin flaps in rats. Drug Des Devel Ther. 2018;12:2267–76. https://doi.org/10.2147/DDDT.S173371.
Khouri RK, Shaw WW. Reconstruction of the lower extremity with microvascular free flaps: a 10-year experience with 304 consecutive cases. J Trauma. 1989;29(8):1086–94. https://doi.org/10.1097/00005373-198908000-00005.
Hashimoto I, Abe Y, Ishida S, et al. Development of skin flaps for reconstructive surgery: random pattern flap to perforator flap. J Med Investig JMI. 2016;63(3–4):159–62. https://doi.org/10.2152/jmi.63.159.
Livaoğlu M, Kerimoğlu S, Sönmez B, Livaoğlu A, Karaçal N. The effect of Hirudoid on random skin-flap survival in rats. J Plast Reconstr Aesthetic Surg JPRAS. 2010;63(6):1047–51. https://doi.org/10.1016/j.bjps.2009.03.018.
Miyawaki T, Jackson IT, Elmazar H, et al. The effect of low-molecular-weight heparin in the survival of a rabbit congested skin flap. Plast Reconstr Surg. 2002;109(6):1994–9. https://doi.org/10.1097/00006534-200205000-00032.
Yingxin G, Guoqian Y, Jiaquan L, Han X. Effects of natural and recombinant hirudin on VEGF expression and random skin flap survival in a venous congested rat model. Int Surg. 2013;98(1):82–7. https://doi.org/10.9738/CC171.1.
Cai LY, Wang T, Lin DS, Lu D. Effects and related mechanism of bivalirudin on the survival of random skin flap on the back of rat. Zhonghua Shao Shang Za Zhi Zhonghua Shaoshang Zazhi Chin J Burns. 2017;33(4):228–32. https://doi.org/10.3760/cma.j.issn.1009-2587.2017.04.008.
Bezuhly M, Morris SF, Juskevicius R, Currie RW, West KA, Liwski RS. Activated protein C improves ischemic flap survival and modulates proangiogenic and antiinflammatory gene expression. Plast Reconstr Surg. 2009;123(2):502–15. https://doi.org/10.1097/PRS.0b013e318196b87f.
Chai J, Ge J, Zou J. Effect of autologous platelet-rich plasma gel on skin flap survival. Med Sci Monit. 2019;25:1611-1620. doi: 10.12659/MSM.913115.
Wang B, Geng Q, Hu J, Shao J, Ruan J, Zheng J. Platelet-rich plasma reduces skin flap inflammatory cells infiltration and improves survival rates through induction of angiogenesis: an experiment in rabbits. J Plast Surg Hand Surg. 2016;50(4):239-245. doi: 10.3109/2000656X.2016.1
Shalom A, Friedman T, Westreich M. Effect of aspirin and heparin on random skin flap survival in rats. Dermatol Surg. 2008;34(6):785.
Shalom A, Herbert M, Westreich M. Effect of aspirin on random pattern flap survival in rats. Eur J Plast Surg. 2000;23(1):21–4. https://doi.org/10.1007/s002380050005.
Akan M, Çakır B, Mısirlioğlu A, Yildirim S, Taylan G, Aköz T. Effects of clopidogrel and high dose aspirin on survival of skin flaps in rats. Scand J Plast Reconstr Surg Hand Surg. 2005;39(1):7–10. https://doi.org/10.1080/02844310410017951.
Taleb S, Moghaddas P, Rahimi Balaei M, et al. Metformin improves skin flap survival through nitric oxide system. J Surg Res. 2014;192(2):686–91. https://doi.org/10.1016/j.jss.2014.07.012.
Bailet JW, Hoffman LF, Trachy RE, Weymuller EA. The effect of nifedipine on skin flap survival in rats. Laryngoscope. 1994;104(3 Pt 1):253–8. https://doi.org/10.1288/00005537-199403000-00002.
Russell JA, Connor NP, Hartig GK. Iontophoretic delivery of nitric oxide donor improves local skin flap viability. J Rehabil Res Dev. 2010;47(1):61–6. https://doi.org/10.1682/jrrd.2008.10.0144.
Shah A, Pfaff MJ, Assi R, Wu W, Steinbacher DM (2014) PDE-5 inhibition improves skin flap viability in rats that are exposed to nicotine. Microsurgery 34.
Farrokhi M, Gashti MZ, Hoormand M, Bakhtiarian A, Habibi R. Combination therapy profoundly improved skin flap survival by modulating KATP channels and nitric oxide. Adv Med Sci. 2019;64(1):117–23. https://doi.org/10.1016/j.advms.2018.08.015.
Wang SP, Lan ZY, Xia W, et al. The effects of vasonatrin peptide on random pattern skin flap survival. Ann Plast Surg. 2014;72(1):94–9. https://doi.org/10.1097/SAP.0b013e318255a3eb.
Pal S, Khazanchi RK, Moudgil K. An experimental study on the effect of nifedipine on ischaemic skin flap survival in rats. Br J Plast Surg. 1991;44(4):299–301. https://doi.org/10.1016/0007-1226(91)90076-v.
Gherardini G, Gürlek A, Milner SM, et al. Calcitonin gene-related peptide improves skin flap survival and tissue inflammation. Neuropeptides. 1998;32(3):269–73. https://doi.org/10.1016/s0143-4179(98)90047-6.
Tsai SL, Chiang Y, Wang MH, Chen MK, Jang LS. Battery-powered portable instrument system for single-cell trapping, impedance measurements, and modeling analyses. Electrophoresis. 2014;35(16):2392–400. https://doi.org/10.1002/elps.201300591.
Zhou K, Zhang Y, Lin D, Tao X, Xu H. Effects of calcitriol on random skin flap survival in rats. Sci Rep. 2016;6:18945. https://doi.org/10.1038/srep18945.
Leng X, Zhang Q, Zhai X, Chen Z. Local transplant of human umbilical cord matrix stem cells improves skin flap survival in a mouse model. Tohoku J Exp Med. 2012;227(3):191–7. https://doi.org/10.1620/tjem.227.191.
Cai Y, Yu Z, Yu Q, et al. Fat extract improves random pattern skin flap survival in a rat model. Aesthet Surg J. 2019;39(12):NP504–14. https://doi.org/10.1093/asj/sjz112.
Fromes Y, Liu JM, Kovacevic M, Bignon J, Wdzieczak-Bakala J. The tetrapeptide acetyl-serine-aspartyl-lysine-proline improves skin flap survival and accelerates wound healing. Wound Repair Regen. 2006;14(3):306-12. doi:10.1111/j.1743-6109.2006.00125.x.
Vourtsis SA, Papalois AE, Agrogiannis GD, Spyriounis PK, Patsouris E, Ionac M. Improvement of a long random skin flap survival by application of vascular endothelial growth factor in various ways of local administration in a rat model. Indian J Plast Surg. 2012;45(1):102-108. doi: 10.4103/0970-0358.96596.
Fujihara Y, Koyama H, Nishiyama N, Eguchi T, Takato T. Gene transfer of bFGF to recipient bed improves survival of ischemic skin flap. Br J Plast Surg. 2005;58(4):511-517. doi: 10.1016/j.bjps.2004.12.028
Cheon YW, Tark KC, Kim YW. Better survival of random pattern skin flaps through the use of epigallocatechin gallate. Dermatol Surg Off Publ Am Soc Dermatol Surg Al. 2012;38(11):1835–42. https://doi.org/10.1111/j.1524-4725.2012.02566.x.
Lee DW, Hong HJ, Roh H, Lee WJ. The effect of polydeoxyribonucleotide on ischemic rat skin flap survival. Ann Plast Surg. 2015;75(1):84-90. doi: 10.1097/SAP.0000000000000053
Chen JX, Chiu CW, Shih PK. The effect of atorvastatin on survival of rat ischemic flap. Kaohsiung J Med Sci. 2013;29(4):187–93. https://doi.org/10.1016/j.kjms.2012.08.032.
Xiao-Xiao T, Sen-Min W, Ding-Sheng L. Effects of vinpocetine on random skin flap survival in rats. J Reconstr Microsurg. 2013;29(6):393–8. https://doi.org/10.1055/s-0033-1343834.
Weis M, Heeschen C, Glassford AJ, Cooke JP. Statins have biphasic effects on angiogenesis. Circulation. 2002;105(6):739–45. https://doi.org/10.1161/hc0602.103393.
Chen J, Liu B, Yuan J, et al. Atorvastatin reduces vascular endothelial growth factor (VEGF) expression in human non-small cell lung carcinomas (NSCLCs) via inhibition of reactive oxygen species (ROS) production. Mol Oncol. 2012;6(1):62–72. https://doi.org/10.1016/j.molonc.2011.11.003.
Das DK, Maulik N. Antioxidant effectiveness in ischemia-reperfusion tissue injury. Methods Enzymol. 1994;233:601–10. https://doi.org/10.1016/s0076-6879(94)33063-8.
Zheng Y, Li Z, Yin M, Gong X. Heme oxygenase-1 improves the survival of ischemic skin flaps (review). Mol Med Rep. 2021;23(4):235. https://doi.org/10.3892/mmr.2021.11874.
van den Heuvel MGW, Buurman WA, Bast A, van der Hulst RRWJ. Review: ischaemia-reperfusion injury in flap surgery. J Plast Reconstr Aesthetic Surg JPRAS. 2009;62(6):721–6. https://doi.org/10.1016/j.bjps.2009.01.060.
Kayiran O, Cuzdan SS, Uysal A, Kocer U. Ethyl pyruvate improves skin flap survival after ischaemia reperfusion injury. Indian J Med Res. 2017;146(3):369–74. https://doi.org/10.4103/ijmr.IJMR_1428_14.
Hou R, Lu T, Gao W, et al. Prussian blue nanozyme promotes the survival rate of skin flaps by maintaining a normal microenvironment. ACS Nano. 2022;16(6):9559–71. https://doi.org/10.1021/acsnano.2c02832.
Bagdas D, Cam Etoz B, Inan Ozturkoglu S, et al. Effects of systemic chlorogenic acid on random-pattern dorsal skin flap survival in diabetic rats. Biol Pharm Bull. 2014;37(3):361–70. https://doi.org/10.1248/bpb.b13-00635.
Gaschler MM, Stockwell BR. Lipid peroxidation in cell death. Biochem Biophys Res Commun. 2017;482(3):419–25. https://doi.org/10.1016/j.bbrc.2016.10.086.
Rahimpour S, Nezami BG, Karimian N, et al. Hypothyroidism improves random-pattern skin flap survival in rats. J Surg Res. 2012;178(1):524–8. https://doi.org/10.1016/j.jss.2012.03.058.
Rasti Ardakani M, Al-Dam A, Rashad A, Shayesteh MA. Effect of systemic antioxidant allopurinol therapy on skin flap survival. World J Plast Surg. 2017;6(1):54–61.
Hayden RE, Paniello RC, Yeung CST, Bello SL, Dawson SM (1987) The effect of glutathione and vitamins A, C, and E on acute skin flap survival. Laryngoscope 97:1176–1179. https://doi.org/10.1288/00005537-198710000-00011
Hassanpour SE, Rostami K, Azargashb E, et al. The effect of topical vitamin A and E on ischemic random skin flap survival. World J Plast Surg. 2019;8(1):58–61. https://doi.org/10.29252/wjps.8.1.58.
Barreiro Arcos ML. Role of thyroid hormones-induced oxidative stress on cardiovascular physiology. Biochim Biophys Acta Gen Subj. 2022;1866(12):130239. https://doi.org/10.1016/j.bbagen.2022.130239.
Fasciolo G, Napolitano G, Aprile M, et al. Hepatic insulin resistance in hyperthyroid rat liver: vitamin E supplementation highlights a possible role of ROS. Antioxid Basel Switz. 2022;11(7):1295. https://doi.org/10.3390/antiox11071295.
Picard-Ami LA, MacKay A, Kerrigan CL. Effect of allopurinol on the survival of experimental pig flaps. Plast Reconstr Surg. 1992;89(6):1098–103. https://doi.org/10.1097/00006534-199206000-00016.
Chen L, Zhou K, Chen H, Li S, Lin D, Zhou D. Calcitriol promotes survival of experimental random pattern flap via activation of autophagy. Am J Transl Res. 2017;9(8):3642–53.
Nyongo A, Huntrakoon M. Microcystic adenoma of the pancreas with myoepithelial cells A hitherto undescribed morphologic feature. Am J Clin Pathol. 1985;84(1):114–20. https://doi.org/10.1093/ajcp/84.1.114.
Chen H, Chen B, Li B, et al. Gastrodin promotes the survival of random-pattern skin flaps via autophagy flux stimulation. Oxid Med Cell Longev. 2021;2021:6611668. https://doi.org/10.1155/2021/6611668.
Jiang R, Lin C, Jiang C, Huang Z, Gao W, Lin D. Nobiletin enhances the survival of random pattern skin flaps: involvement of enhancing angiogenesis and inhibiting oxidative stress. Int Immunopharmacol. 2020;78:106010. https://doi.org/10.1016/j.intimp.2019.106010.
Jiang J, Jin J, Lou J, et al. Positive effect of andrographolide induced autophagy on random-pattern skin flaps survival. Front Pharmacol. 2021;12:653035. https://doi.org/10.3389/fphar.2021.653035.
Jiang R, Dong C, Chen Z, Cheng S, Yang J, Gao W. Catalpol enhances random-pattern skin flap survival by activating SIRT1-mediated enhancement of autophagy. Oxid Med Cell Longev. 2022;2022:5668226. https://doi.org/10.1155/2022/5668226.
Zhang L, Yu G, Yu Q, Wang L, Wu L, Tao Z, Ding J, Lin D (2023) Baicalin promotes random-pattern skin flap survival by inducing autophagy via AMPK-regulated TFEB nuclear transcription. Phytotherapy Res 37(9):3926–3938. https://doi.org/10.1002/ptr.7849.
Li J, Chen H, Lou J, Bao G, Wu C, Lou Z, Wang X, Ding J, Li Z, Xiao J, Xu H, Gao W, Zhou K. Exenatide improves random-pattern skin flap survival via TFE3 mediated autophagy augment. J Cell Physiol. 2021;236(5):3641–3659. https://doi.org/10.1002/jcp.30102.
Wu H, Ding J, Li S, Lin J, Jiang R, Lin C, Dai L, Xie C, Lin D, Xu H, Gao W, Zhou K. Metformin promotes the survival of random-pattern skin flaps by inducing autophagy via the AMPK-mTOR-TFEB signaling pathway. Int J Biol Sci. 2019;15(2):325-340. https://doi.org/10.7150/ijbs.29009.
Wu H, Chen H, Zheng Z et al. Trehalose promotes the survival of random-pattern skin flaps by TFEB mediated autophagy enhancement. 2019;Cell Death Dis 10:483. https://doi.org/10.1038/s41419-019-1704-0.
Ma X, Lin Y, Fang M, et al. Effects of catalpol from Rehmannia glutinosa extract on skin flaps. Plast Reconstr Surg. 2023. https://doi.org/10.1097/PRS.0000000000010650.
Zheng W, Wang J, Xie L, et al. An injectable thermosensitive hydrogel for sustained release of apelin-13 to enhance flap survival in rat random skin flap. J Mater Sci Mater Med. 2019;30(9):106. https://doi.org/10.1007/s10856-019-6306-y.
Cao B, Wang L, Lin D, Cai L, Gao W. Effects of lidocaine on random skin flap survival in rats. Dermatol Surg. 2015;41(1):53-58. https://doi.org/10.1097/DSS.0000000000000241.
Ahmadzadeh M, Esmaeilzadeh Z, Khezri MR, Jafari A, Ghasemnejad-Berenji M. The promising effect of topiramate on random-pattern skin flap survival in rats. Aesthetic Plast Surg. 2022;46(5):2548-2555. https://doi.org/10.1007/s00266-022-02969-6.
Tabary M, Aryannejad A, Noroozi N, et al. The promising effect of colchicine on random-pattern skin flap survival in rats: glutamate pathway. J Surg Res. 2022;275:63–71. https://doi.org/10.1016/j.jss.2022.01.026.
Ala M, Mohammad Jafari R, Nematian H, Ganjedanesh MR, Dehpour AR. Sodium valproate improves skin flap survival via gamma-aminobutyric acid and histone deacetylase inhibitory system. J Surg Res. 2020;246:519–26. https://doi.org/10.1016/j.jss.2019.09.036.
Tabary M, Aryannejad A, Noroozi N, et al. Ivermectin increases random-pattern skin flap survival in rats: the novel role of GABAergic system. J Surg Res. 2021;259:431–41. https://doi.org/10.1016/j.jss.2020.09.010.
Nichter LS, Sobieski MW, Edgerton MT. Augmentation of critical skin flap survival following ibuprofen therapy. Ann Plast Surg. 1986;16(4):305–12. https://doi.org/10.1097/00000637-198604000-00006.
Ren H, Lin D, Mou Z, Dong P. The adverse effect of selective cyclooxygenase-2 inhibitor on random skin flap survival in rats. Li Volti G, ed. PLoS ONE. 2013;8(12):82802. https://doi.org/10.1371/journal.pone.0082802.
Davis RE, Cohen JI, Robinson JE, Urben SL, Cook TA. Ketorolac (Toradol) and acute random-pattern skin flap survival in rat. Arch Otolaryngol Head Neck Surg. 1995;121(6):673–7. https://doi.org/10.1001/archotol.1995.01890060071014.
Yang M, Sheng L, Li H, Weng R, Li QF. Improvement of the skin flap survival with the bone marrow-derived mononuclear cells transplantation in a rat model. Microsurgery. 2010;30(4):275–81. https://doi.org/10.1002/micr.20779.
Nazanin M, Mahshad M, Mehdi B, Farzaneh C. Enhanced survival and accelerated perfusion of skin flap to recipient site following administration of human amniotic membrane in rat models. J Plast Reconstr Aesthetic Surg JPRAS. 2022;75(11):4321–7. https://doi.org/10.1016/j.bjps.2022.08.028.
Chehelcheraghi F, Chien S, Bayat M. Mesenchymal stem cells improve survival in ischemic diabetic random skin flap via increased angiogenesis and VEGF expression. J Cell Biochem. 2019;120(10):17491–9. https://doi.org/10.1002/jcb.29013.
Foroglou P, Demiri E, Koliakos G, Karathanasis V. Autologous administration of adipose stromal cells improves skin flap survival through neovascularization: an experimental study. Int Wound J. 2019;16(6):1471–6. https://doi.org/10.1111/iwj.13216.
Avila FR, Torres-Guzman RA, Huayllani MT, et al. Human stem cells prevent flap necrosis in preclinical animal models: a systematic review. J Clin Transl Res. 2022;8(2):110–24.
Bai Y, di Han Y, Yan XL, et al. Adipose mesenchymal stem cell-derived exosomes stimulated by hydrogen peroxide enhanced skin flap recovery in ischemia-reperfusion injury. Biochem Biophys Res Commun. 2018;500(2):310–7. https://doi.org/10.1016/j.bbrc.2018.04.065.
Yue Y, Zhang P, Liu D, Yang JF, Nie C, Yang D. Hypoxia preconditioning enhances the viability of ADSCs to increase the survival rate of ischemic skin flaps in rats. Aesthetic Plast Surg. 2013;37(1):159–70. https://doi.org/10.1007/s00266-012-9993-z.
Pu CM, Chen YC, Chen YC, et al. Interleukin-6 from adipose-derived stem cells promotes tissue repair by the increase of cell proliferation and hair follicles in ischemia/reperfusion-treated skin flaps. Mediators Inflamm. 2019;2019:2343867. https://doi.org/10.1155/2019/2343867.
Mayo JS, Kurata WE, O’Connor KM, Pierce LM. Oxidative stress alters angiogenic and antimicrobial content of extracellular vesicles and improves flap survival. Plast Reconstr Surg Glob Open. 2019;7(12):e2588. https://doi.org/10.1097/GOX.0000000000002588.
Pu CM, Liu CW, Liang CJ, et al. Adipose-derived stem cells protect skin flaps against ischemia/reperfusion injury via IL-6 expression. J Invest Dermatol. 2017;137(6):1353–62. https://doi.org/10.1016/j.jid.2016.12.030.
Hu X, Yi Y, Zhu Y, et al. Effect of adipose-derived stem cell derived exosomes on angiogenesis after skin flap transplantation in rats. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi Zhongguo Xiufu Chongjian Waike Zazhi Chin J Reparative Reconstr Surg. 2019;33(12):1560–5. https://doi.org/10.7507/1002-1892.201904023.
Zahir KS, Syed SA, Zink JR, Restifo RJ, Thomson JG. Ischemic preconditioning improves the survival of skin and myocutaneous flaps in a rat model. Plast Reconstr Surg. 1998;102(1):140–50. https://doi.org/10.1097/00006534-199807000-00022. (Discussion 151–152).
Pellitteri PK, Kennedy TL, Youn BA. The influence of intensive hyperbaric oxygen therapy on skin flap survival in a swine model. Arch Otolaryngol Head Neck Surg. 1992;118(10):1050–4. https://doi.org/10.1001/archotol.1992.01880100040011.
Qi Z, Gao C, Wang Y, et al. Effects of hyperbaric oxygen preconditioning on ischemia-reperfusion inflammation and skin flap survival. Chin Med J (Engl). 2013;126(20):3904–9.
Harder Y, Contaldo C, Klenk J, Banic A, Jakob SM, Erni D. Improved skin flap survival after local heat preconditioning in pigs. J Surg Res. 2004;119(1):100–5. https://doi.org/10.1016/j.jss.2003.11.002.
Kretzschmar RM. Panel discussion: placenta previa. Isotope placental localization. J Iowa Med Soc. 1965;55(11):628–9.
Davis RE, Wachholz JH, Jassir D, Perlyn CA, Agrama MH. Comparison of topical anti-ischemic agents in the salvage of failing random-pattern skin flaps in rats. Arch Facial Plast Surg. 1999;1(1):27–32. https://doi.org/10.1001/archfaci.1.1.27.
Chang C, White C, Katz A, Hanna MK. Management of ischemic tissues and skin flaps in re-operative and complex hypospadias repair using vasodilators and hyperbaric oxygen. J Pediatr Urol. 2020;16(5):672.e1-672.e8. https://doi.org/10.1016/j.jpurol.2020.07.034.
Kushibiki T, Mayumi Y, Nakayama E, et al. Photocrosslinked gelatin hydrogel improves wound healing and skin flap survival by the sustained release of basic fibroblast growth factor. Sci Rep. 2021;11(1):23094. https://doi.org/10.1038/s41598-021-02589-1.
Lese I, Graf DA, Tsai C, et al. Bioactive nanoparticle-based formulations increase survival area of perforator flaps in a rat model. PLoS ONE. 2018;13(11):e0207802. https://doi.org/10.1371/journal.pone.0207802.
Chen KT, Mardini S, Chuang DCC, et al. Timing of presentation of the first signs of vascular compromise dictates the salvage outcome of free flap transfers. Plast Reconstr Surg. 2007;120(1):187–95. https://doi.org/10.1097/01.prs.0000264077.07779.50.
Bui DT, Cordeiro PG, Hu QY, Disa JJ, Pusic A, Mehrara BJ. Free flap reexploration: indications, treatment, and outcomes in 1193 free flaps. Plast Reconstr Surg. 2007;119(7):2092–100. https://doi.org/10.1097/01.prs.0000260598.24376.e1.
Abe Y, Hashimoto I, Goishi K, Kashiwagi K, Yamano M, Nakanishi H. Transcutaneous PCO2 measurement at low temperature for reliable and continuous free flap monitoring: experimental and clinical study. Plast Reconstr Surg Glob Open. 2013;1(2):1–8. https://doi.org/10.1097/GOX.0b013e3182936cd0.
Acknowledgements
Not applicable.
Funding
None to disclose.
Author information
Authors and Affiliations
Contributions
CEB and DCW contributed to ideation and conceptualization of the presented manuscript. CEB, TL, NA, CK, AZF, and AAC contributed to manuscript background research and writing. MG, MJ, and DCW assisted in editing and made substantial contributions to the written content included in the final manuscript. CEB and PMP contributed to figure creation.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication has been obtained from all necessary person(s).
Competing interests
All authors declared that there are no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Berry, C.E., Le, T., An, N. et al. Pharmacological and cell-based treatments to increase local skin flap viability in animal models. J Transl Med 22, 68 (2024). https://doi.org/10.1186/s12967-024-04882-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-024-04882-9