Abstract
Glioblastoma (GBM) comprises 45.6% of all primary malignant brain cancers and is one of the most common and aggressive intracranial tumors in adults. Intratumoral heterogeneity with a wide range of proteomic, genetic, and epigenetic dysregulation contributes to treatment resistance and poor prognosis, thus demanding novel therapeutic approaches. To date, numerous clinical trials have been developed to target the proteome and epigenome of high-grade gliomas with promising results. However, studying RNA modifications, or RNA epitranscriptomics, is a new frontier within neuro-oncology. RNA epitranscriptomics was discovered in the 1970s, but in the last decade, the extent of modification of mRNA and various non-coding RNAs has emerged and been implicated in transposable element activation and many other oncogenic processes within the tumor microenvironment. This review provides background information and discusses the therapeutic potential of agents modulating epitranscriptomics in high-grade gliomas. A particular emphasis will be placed on how combination therapies that include immune agents targeting hERV-mediated viral mimicry could improve the treatment of GBM.
Key points
-
In vivo studies link epitranscriptomic dysregulation with glioma pathogenesis.
-
TCGA shows elevated regulator expression is associated with increased mortality in GBM patients.
-
RNA modifications negatively correlate with GBM immunogenicity and thus reduce the efficacy of immunotherapies in GBM patients.
-
RNA modification regulators represent promising therapeutic agents for reducing mortality and immunotherapy adjuvants for enhancing tumor immunogenicity.
Similar content being viewed by others
Introduction
Glioblastoma (GBM) comprises 45.6% of all primary malignant brain cancers and is one of the most common and aggressive intracranial tumors in adults [1]. Due to its highly aggressive nature and inevitable recurrence, its disease course has one of the highest mortalities, with a 5-year survival rate of only 5% despite maximal surgical resection and adjuvant chemoradiation [2].
GBM is a highly heterogeneous neoplasm with a wide range of proteomic, genetic, and epigenetic dysregulation [3]. Many enzymes responsible for regulating protein and DNA modifications are currently targets of cancer trials and therapies. However, studying RNA modifications, or RNA epitranscriptomics, is a new frontier within neuro-oncology [4]. Simply put, epitranscriptional modifications include dynamic, covalent modifications that can affect the stability, translation, and function of RNA. Although eukaryotic RNA modifications have been known since the 1970s, most studies focused on transfer RNA (tRNA) and ribosomal RNA (rRNA). Only within the last decade has there been extensive characterization of modifications of mRNA and various non-coding RNAs. RNA modifications have steadily moved towards the limelight as scientists appreciated that RNA does not only act as an effector molecule (tRNA and rRNA) or intermediate in protein synthesis (mRNA) but also directly affects gene expression via non-coding RNAs such as microRNA (miRNA) and long ncRNA (lncRNA) [5,6,7].
Few dedicated studies of posttranscriptional modifications and their potential as therapeutic targets occurred initially. Still, in the past few years, this field has become an active field of investigation for brain tumors [4]. Several lines of evidence suggest that epitranscriptomic dysregulation contributes to glioma pathogenesis [4, 8,9,10]. The three major epitranscriptomic players implicated in both physiologic regulation and disease include “writers” that add a specific modification, “erasers” that remove a specific modification, and “readers” that identify and bind modified nucleotides.
A common consequence of pretranscriptional (i.e., epigenetics) and posttranscriptional (i.e., epitranscriptomic) dysregulation is the activation of transposable elements (TEs). Interestingly, in the last decade of cancer research, a form of TEs known as endogenous retroviruses (ERVs) has been shown to play a dichotomous role in driving oncogenesis and serving as potential antigens for immunotherapy [11]. First described in 1981, human ERVs (hERVs) are relics of retroviral infection of the ancestral germline. hERV genes account for nearly 9% of the human genome and are transcriptionally silent in normal cells. hERV expression is associated with many cancers. hERV expression also is related to autoimmune and neurodegenerative diseases. Augmenting hERV inflammatory effects through a cellular state known as “viral mimicry” is being explored to sensitize tumors to immunotherapy [12]. Viral mimicry enhances hERV expression by reversing silencing marks that suppress hERV gene expression. The fundamental premise is that a transient increase in hERV expression may induce an innate antiviral and adaptive immune response that sensitizes and homogenizes tumor cells for immunotherapy.
Recent publications extensively reviewed how RNA modifications participate in cancer and glioma development/progression, regulate the tumor microenvironment (TME), and encourage the development of drug resistance [4, 9]. This review aims to provide background information about epitranscriptomics and discuss the therapeutic potential of modulating epitranscriptomics in high-grade gliomas and GBM. We will also further discuss the rationale for using a hERV-mediated viral mimicry strategy as part of a combination immunotherapy for GBM.
Aberrant RNA modifications in GBM
In the context of glioma pathogenesis and progression, the most relevant RNA modifications are N6-methyladenosine (m6A), 5-methylcytidine (m5C), N1-methyladenosine (m1A), hydroxymethylcytidine (hm5C), pseudouridine (Ψ), and adenosine-to-inosine (A-to-I) RNA editing [9]. Elevated transcript levels of RNA modification writers/readers have been associated with increased mortality in GBM patients, as illustrated in Fig. 1. One notable exception is ADAR3, whose transcript levels have oddly been found to be inversely correlated to its protein expression [13].
Select RNA modification regulators and glioma survival. A Kaplan–Meier curves shown for RNA B modification regulators YTHDF2, NSUN4, PUS7, WTAP, and ADAR3. Note both IDH wildtype and mutant status are included. GlioVis data portal for visualization and analysis of brain tumor expression datasets [123]. B PDB images of each protein or protein complex [131] is shown adjacent to the respective modification involved. Of note, YTHDF2 has been shown to be a reader molecule for both m1A and m6A [124, 125]. C mRNA modifications are shown in the most probable area based on its respective transcriptome-wide distribution [8]. CDS, coding sequence; UTR, untranslated region
The following subsections will review the physiologic role of each RNA modification on gene regulators. Furthermore, Table 1 summarizes the findings of dysfunction associated with each modification in glioma, and Fig. 2 illustrates major pathways where mechanistic studies have been completed.
major Oncogenic Pathways in Glioma Epitranscriptome. Following the color scheme established in Fig. 1, major oncogenic pathways proceeding through the m6A writer complex, m6A eraser ALKBH5, A-to-I RNA editors ADAR1/2/3, m1A writer TRMT6-TRMT61A, and pseudouridine writer PUS7 are illustrated
M6A
Methylation of the adenosine at the N6 position (m6A) is the most common modification of mRNA and is primarily found in the 3’ untranslated region (UTR) [14]. The writers that catalyze this modification include methyltransferase enzymes methyltransferase-like 3 (METTL3), METTL14, and Wilms tumor 1-associated protein (WTAP) [14]. Examples of erasers that remove them are fat mass and obesity-associated protein (FTO) and alkB homolog 5 (ALKBH5) [15]. Readers involved in the m6A physiologic functions usually comprise the YT521-B homology (YTH) domain family of proteins or the heterogeneous nuclear ribonucleoprotein (HNRNP) proteins [9].
The physiologic function of m6A modifications involves pre-mRNA splicing, mature mRNA transport, and translation [9, 16, 17]. The HNRNPC reader regulates mRNA splicing, while the YTHDC1 reader regulates mature mRNA export [18, 19]. The YTHDF2 and YTHDF3 readers work on translation to accelerate and increase efficiency, respectively [20]. The METLL3 writer is involved in mature mRNA export and translation regulation [19]. Regarding m6A erasers, FTO and ALKBH5 both function as splicing-related erasers, with the latter also shown to enhance cellular stability [17, 21].
M1A
Adenosine methylation at the N1 position (m1A) is frequently found in the 5’ UTR of mRNA and tRNA. The tRNA methyltransferase 6/61A (TRMT6/61A) and tRNA methyltransferase 10C (TRMT10C) writers and YTHDF1/2/3 and YTHDC1 readers function to influence mRNA structural stability and increase translation [9, 22]. Additionally, m1A methylation may negatively impact the translation of coding sequences (CDS) in mitochondrial mRNA (mt-mRNA) [22]. AlkB homologs 1 and 3 (ALKBH1/3) act as erasers.
M5C
In addition to being found on DNA, the methylation of cytosine at the N5 position (m5C) is frequently found in the UTRs of mRNA [23]. Writers include NOL1/NOP2/SUN domain (NSUN) proteins and the DNA methyltransferase (DNMT) DNMT2 [9]. Only NSUN2 is known to be capable of modifying mRNA, while the rest of the writers solely act on rRNAs and tRNAs. Aly/REF export factor (ALYREF) serves as a reader, participating in transcript transport and translation efficiency regulation [24]. Interestingly, evidence has shown that m5C methylation of 5’UTRs and CDS may limit or altogether abolish translation, respectively, while modification of 3’UTRs may enhance expression [9]. m5C erasers have yet to be identified. Furthermore, m5C can be oxidized into hm5C by the Tet-family enzymes [25]. This most often occurs in coding regions and appears associated with translational activation.
Ψ
Isomerization of uracil (U) yields the pseudouridine (Ψ) modification. This is thought to be the most abundant RNA modification, mainly accumulating in rRNAs and tRNAs [26]. An RNA-dependent pseudouridine synthase (PUS) such as PUS1/3/7 in humans and centromere-binding factor 5 (Cbf5) in yeast usually catalyze this modification [27, 28]. Despite limited investigations on the Ψ modification in biological mRNAs, its ability to prevent pre-mRNA splicing, maintain mRNA stability, and increase mRNA translation is thought to result in improper protein expression [9].
A-to-I editing
Nucleotide base editing of adenosine to inosine is catalyzed by adenosine deaminases (ADARs) [29]. In addition to changing the primary sequence, it appears to affect mRNA native secondary structures [30]. In humans, there are three ADAR proteins: ADAR1 (ADAR), ADAR2 (ADARB1), and ADAR3 (ADARB2) [31]. While ADAR1 and ADAR2 are ubiquitously expressed and catalyze A-to-I RNA editing in many organs and at millions of sites in the human transcriptome [32, 33], ADAR3 expression is restricted to the brain and appears catalytically inactive [34,35,36,37,38]. Interestingly, in addition to dsRNA binding activity, ADAR3 has been shown to bind single-stranded RNA (ssRNA) in vitro [35]. Although not yet fully elucidated, ADAR3 appears to play a role in competitive inhibition of the catalytically active ADARs [39]. Adenosine deaminases are also known to act on tRNAs (ADATs) to catalyze A-to-I editing [40]. These enzymes remain understudied and incompletely characterized, with only 7 related papers on PubMed.
RNA modification patterns in glioma
The role of RNA modification in cancers is incredibly complex and challenging to study, primarily due to limitations in sequencing technologies. Conventional sequencing techniques such as bulk RNA-seq and scRNA-seq quantify and normalize for mRNA expression but are not specifically developed to detect RNA modifications. Taguchi et al. recently reviewed developments in epitranscriptome spatial detection and data analysis [41]. Advancements in de novo sequencing will be discussed later in this review.
RNA modifications, namely m6A methylations, have been found to influence the tumor microenvironment (TME), immune cell-infiltrating characteristics, and, ultimately, patient outcomes [4, 42]. RNA modification patterns are particularly clinically relevant since they may portend responses to immunotherapy [42]. Similarly, Lin et al. utilized the TCGA-GBM and TCGA-LGG databases to explore patterns of differentially expressed m6A regulators in glioma [43]. Using principal component analysis, two glioma subgroups were identified, and one cluster was found to have a worse prognosis, higher WHO classification grade, and higher immune infiltration. Based on the combination of m6A RNA methylation and the landscape of the immune microenvironment, a novel 4-gene (TAGLN2, PDPN, TIMP1, EMP3) prognostic model was developed and validated with a good prediction. In addition, PDPN and TIMP1 were found to be highly expressed in high-grade glioma via The Human Protein Atlas database, and both correlated with m6A and macrophage marker CD68 in glioma tissue samples, which may serve as potential biomarkers for glioma prognosis.
Molecular alterations characterizations such as isocitrate dehydrogenase IDH1/2 mutations, 1p/19q codeletion, and MGMT promoter methylation, have improved the accuracy of diagnostics, prognostics, and prediction of treatment response for glioma patients. However, we have yet to observe any tangible improvement in either clinical management or patient outcomes. A potential utility of epitranscriptomics is to be used in conjunction with known glioma sub-entities to further advance tumor stratification and help guide treatment selection [15]. According to studies mining the Chinese Glioma Genome Atlas (CGGA), The Cancer Genome Atlas (TCGA), and Repository for Molecular Brain Neoplasia Data (REMBRANDT), epitranscriptomic regulators appear to be differentially expressed based upon molecular alterations and clinical attributes. For example, METTL3, FTO, and YTHDC1 are significantly differentially expressed between IDH-mutant and IDH-wildtype high grade gliomas [44]. Additionally, m6A writer METTL3 correlates with poor OS in IDH-wildtype but not in IDH-mutant gliomas [45].
A critical limiting factor of most epitranscriptomic cancer studies has been the scientific indifference towards RNA modifications other than m6A. Given the integrated process of interactions between different RNA methylation modifications, studying a single type of RNA modification in tumors may not comprehensively elucidate epitranscriptomic effects. A recent study by Li and colleagues recognized this. It developed a GBM score’ based on the differentially expressed genes (DEGs) between groups showing RNA modification patterns of writers that catalyze m1A methylation, m6A methylation, APA, and A-to-I RNA editing [46]. Out of the 26 writers analyzed, 15 were found to be more highly expressed in tumor tissue than adjacent normal tissue. Using Spearman’s correlation analysis, positive correlations occurred among several writers, which indicate that crosstalk among RNA modification writers may mediate the formation of distinct RNA modification patterns and GBM progression. After consensus clustering analysis, two clusters emerged, with one having a significantly shorter survival. In this cluster with higher mortality, GSVA was used to estimate the signaling pathways with gene set enrichment. Signaling pathways found to be significantly enriched were those involved in NK cell-mediated cytotoxicity, Toll-like receptor activation, JAK-STAT, and chemokine signaling. Additionally, using CIBERSORT, this same cluster was found to have higher levels of immunosuppressive cells such as M2 macrophages. Of note, several RNA modification writers, including RBM15, RBM15B, TRMT6, CLTP1, PABPN1, ADARB1, and CPSF1, were found to be positively associated with M0 macrophage differentiation.
The immunosuppressive tumor microenvironment has been identified as the primary reason for the failure of immune therapy in GBM patients; currently, there are no FDA-approved immunotherapies for GBM [47]. Accumulating evidence has shown a strong correlation between RNA modifications, namely m6A, and immunomodulation, and thus the efficacy of immunotherapies in GBM patients [43, 46, 48,49,50]. This correlation does not appear to be unique to primary brain tumors, as similar data has been found in colorectal cancer [51], colon cancer [52], gastric cancer [42], bladder cancer [53], lung adenocarcinoma [54], and head and neck squamous cell carcinoma [55]. This collection of recent investigations indicates that RNA modification shapes the complexity of the TME and its response to immunotherapy. Han et al. provide a more complete review of this field [56]. While exciting, extensive work is needed to understand modifications other than m6A, crosstalk between modifications, and cell types modulated by RNA modification. To fully understand the underlying mechanisms and therapeutic potential, further in vitro and in vivo studies are needed using meticulous methods to dissect RNA modifications and their regulators in tumor cells versus immune cells [56].
Advancements in RNA modification de novo sequencing
Epitranscriptomic sequencing technologies may be divided into four fundamental approaches: antibody-based, reverse-transcription signature-dependent, enzyme-dependent, and chemically assisted [8]. Antibody-based methods are the most widely used modality for m6A, m5C, ac4C, and m7G modifications; however, drawbacks include limited specificity, lack of stochiometric outputs, and high input material requirements. Reverse transcription signature-dependent techniques rely on insertion-deletion mutations (indels), mismatches, and truncations at the modification sites. Still, they are prone to false positives due to errors in library preparation and sequencing or single-nucleotide polymorphisms [57, 58]. Enzyme-dependent sequencing technologies rely on various enzymes such as demethylases, endonucleases, and exonucleases to discriminate regular bases from modified ones [8]. The efficiency and sequence biases of the respective enzyme characterize its limitations. Lastly, chemical-assisted technologies combine chemical treatments with next-generation sequencing [8]. Recent chemical methods have addressed the gap between the dynamics and reversibility of RNA modifications by allowing absolute quantification at single-base resolution for m6A, pseudouridine, m5C, and ac4C.
Novel sequencing technologies that allow simultaneous detection of multiple modifications are vital to understand the crosstalk between modifications further and drive the field of epitranscriptomics. Third-generation methods such as SMRT and Nanopore sequencing hold promise but have faced challenges, including limited signal-to-noise ratios, complex algorithms, and high error rates and costs [59]. In addition, spatial epitranscriptomic elucidation of the mRNA modification profiles of individual cells in both spatial and temporal dimensions is likely to become an important area in developmental and cancer biology [8, 60].
(h)ERVs, post-transcriptional regulation, and GBM
As occurs in pluripotent embryos, many cancers are known to reactivate transposable elements (TE) through chromatin remodeling, DNA hypomethylation, and histone modifications [12]. TEs are fundamentally heterogeneous, comprising two main types: DNA transposons and retrotransposons, which include Long Interspersed Nuclear Elements (LINEs), Short Interspersed Nuclear Elements (SINEs), and Long Terminal Repeat (LTR) Retrotransposons. Our focus in this review will be on LTR retrotransposons or human ERVs (hERVs).
The genome of an intact hERV provirus comprises at least 5’ and 3’ long terminal repeats (LTRs) flanking an internal Gag (group-specific antigen)-Pro (protease)-Pol (polymerase) polyprotein-coding sequence. Gag is cleaved by Pro to generate a virus-like particle that contains the fusion protein and ERV mRNA. hERVs may also contain a remnant envelope (Env) and other accessory genes but are generally not infectious [12]. HERV-K (HML-2), first reported in 1986, is the most recent hERV integrated into genomic DNA. Unlike other hERVs, HERV-K contains a near-full-length transcript in the human genome that includes open reading frames (ORFs) of HERV-K Gag, Pol, and Env, which can be read and translated into functional retroviral proteins [61].
While necessary for mammalian embryologic development, ERV activation and transposition can compromise host health secondary to aberrant transcriptional regulation; thus, constant surveillance is needed to maintain homeostasis [62]. Although the ERV regulatory network mechanisms are poorly understood, recent advancements have helped elucidate how mammals effectively regulate ERV expression.
ERV regulatory networks fundamentally consist of pre-transcriptional and post-transcriptional regulatory networks [63]. Pre-transcriptional regulators include zinc-finger proteins (ZFPs), TRIM28-SETDB1, human silencing hub (HUSH) complex, SWItch-sucrose non-fermentable (SWI-SNF) complex, MORC proteins, Lymphoid-specific helicase (LSH), and P-element-induced wimpy testis (PIWI)-interacting RNAs (piRNAs). Alternatively, piRNAs, nuclear exosome targeting (NEXT) complex, and RNA methylation comprise the post-transcriptional modulators. Table 2 summarizes the proteins and function of the ERV expression regulators.
hERV-mediated Oncogenesis
hERVs may drive oncogenesis in two main ways: (1) indirect transcriptional regulation of oncogenes/tumor suppressors and (2) expression of oncogenic HERV proteins [11].
There is accumulating support for hERVs as an oncogenic driver and emerging target for treatment via epigenetic silencing. On the other hand, the role of post-transcriptional silencing and RNA modifications of hERV transcripts in glioma remains virtually unexplored. This subsection briefly recounts major hERV-mediated oncogenic findings and provides context for the onco-exaptation discussion later in the review.
Akin to its role in development, hERVs may serve as alternative promoters for proximal genes in malignant cells and cryptic transcription start sites to produce aberrant CDS mRNA [12]. Similarly, onco-exaptation may proceed by hERVs acting as enhancers [64]. Moreover, HERV-K-derived sequences appear to interrupt and inactivate tumor suppressor BRCA2 and DNA repair gene XRCC1 in glioma cells [65].
Through c-MYC proto-oncogene activation, HERV-K Env and accessory proteins Rec and Np9 have been linked to tumorigenesis in various cancers [66]. Rec and Np9 have been proposed to bind to the transcriptional repressor promyelocytic leukemia zinc finger (PLZF), which mediates the expression of the protooncogene c-MYC and suppressor genes p53 and p21 [67]. Np9 has also been associated with amplifying Notch signaling via binding to and initiating Ligand of Numb Protein X (LNX) degradation [68]. Interestingly, in glioma cells, LNX protein has been found to be decreased [69]. Therefore, the HERV-K Rec and Np9 represent putative oncogenes and require further investigation as therapeutic targets in gliomas displaying signs of hERV activation.
Finally, hERVs have been proposed to be responsible for the stem-cell phenotype in cancer stem cells (CSCs) [11, 61]. CD133, a common glioma stem-cell marker, strongly correlates with hERV expression in melanoma cell lines. Treatment with reverse transcriptase inhibitors lowers HERV-K expression and CD133 + melanoma cell populations [70]. Moreover, the HERV-K env is overexpressed in pluripotent stem cells (PSC) but downregulated during neuronal differentiation. This same protein interacts with CD98HC, activates the mTOR pathway, and induces epigenetic changes through lysophosphatidylcholine acyltransferase (LPCAT1) [71]. CD98 is widely expressed in astrocytic tumors, where it has been suggested to promote oncogenic transformation by facilitating amino acid transport [72].
Epigenetic and m6A epitranscriptomic crosstalk
Chemical modifications on DNA, RNA, and proteins (e.g., histones) impact gene regulation. As discussed above, installing an RNA m6A modification alters mRNA stability and translation. Furthermore, emerging data suggests that m6A methylation influences physiological regulation beyond post-transcriptional mechanisms [73]. While loss of m6A writers and nuclear m6A readers are known to be developmentally lethal, knockout of the YTHDF family, cytoplasmic m6A readers involved in transcript decay, has not been shown to recapitulate lethality [74, 75]. Although alternative explanations, such as compensation from other readers, are undoubtedly reasonable, evidence that suggests m6A methylation feeds back onto epigenetic circuits has rapidly accumulated.
A vital function of heterochromatin is restraining the activity of embedded satellite repeats and transposable elements [76]. Endogenous retroviruses (ERVs) are a prominent class of retrotransposons that necessitate constitutive silencing by regulation machineries, traditionally understood to comprise epigenetic processes. Remarkably, three separate research groups have recently reported a role for m6A in regulating ERVs through an element known as intracisternal A particle (IAP) in mouse embryonic stem cells (mESCs) [77,78,79]. m6A on the 5′UTR of the IAP mRNA recruits YTHDF readers for mRNA degradation. Thus, m6A levels are inversely correlated with mRNA and protein levels of IAP. Knockout of Mettl3 writers and rescue by a catalytically inactive form failed to restore H3K9me3 levels at IAP elements, while knockout of Alkbh5 erasers significantly increased H3K9me3 levels at these sites. Thus, this data suggests a positive link between m6A deposition and levels of H3K9me3, a significant molecular feature of heterochromatin.
The current explanation for these findings is that m6A RNA modifications catalyzed by Mettl3 are known to interact with Ythdc1 readers. This interaction, confirmed via chromatin immunoprecipitation followed by sequencing (ChIP-seq) with enrichment at H3K9me3-rich transposable elements, has a role in mediating retrotransposon silencing and maintaining mESC identity [79]. In addition, Ythdc1 appears to guide Mettl3 and facilitate its interaction with chromatin, tripartite motif containing 28 (TRIM28), and SET-domain-bifurcated histone lysine methyltransferase 1 (SETDB1). This aptly named m6A methyltransferase complex regulates H3K9me3 deposition at IAPs.
Despite some inconsistencies in the proposed mechanism, these studies [77,78,79] provide convincing evidence that m6A directly impacts heterochromatin formation. Furthermore, expanding evidence has revealed the role of m6A methylation on chromosome-associated regulatory RNAs (carRNAs) or mRNA-encoding histone-modifying enzymes and accessible chromatin. There is evidence of reverse feedback of histones on m6A modifications and of the histone elongation mark H3K36me3 guiding m6A deposition [80]. Kan et. Al more extensively discusses these concepts [73].
It is currently unknown if and how RNA modifications other than m6A feedback on epigenetic checkpoints.
Viral mimicry
Viral mimicry describes an active anti-viral cellular state triggered by an endogenous stimulus. It may evoke innate and adaptive immune responses and can be triggered by cytosolic RNA or DNA [81].
Two landmark papers in 2015 describe “viral mimicry” as a process involving inhibition of epigenetic silencing, retrotransposon transcription, and IFN activation. The host cells interpret aberrant repetitive element RNA expression as a viral infection and activate an IFN response [82, 83]. Recognition of retrotransposon-derived duplex RNAs (dsRNA) by cytosolic RNA sensors like MDA5 or endosomal RNA sensors such as Toll-like receptor 3 (TLR3) initiates antiviral signaling. Stimulation of RNA sensors is propagated by mitochondrial antiviral-signaling protein (MAVS) aggregation on the mitochondrial surface, which induces a TBK1-mediated phosphorylation cascade that results in the phosphorylation, dimerization, and nuclear localization of IRF3/7 to activate either type I or III IFN signaling. This pro-inflammatory immune response ultimately suppresses proliferation and induces apoptosis in the affected cell. In addition, viral mimicry enhances adaptive immune responses as hERV-derived peptides form tumor-associated antigens (TAAs) that may elicit CD8 + T-cell responses. Glioblastoma is characteristically considered to be an “immunologically cold” tumor. Using adjunctive agents to enhance intratumoral viral mimicry and its innate and adaptive immune responses could bolster the effects of present immunotherapies.
In glioblastoma cell lines, DNA methyltransferase inhibition (DNMTi) increased the expression of TE and HERV-derived peptides [84]. However, clinical trials utilizing adjuvant DNMTi have been unsuccessful to date. A phase 1 trial using 5-Azacitidine monotherapy in recurrent high-grade IDHm gliomas reached disease stabilization in approximately 40% of patients but failed to accomplish a durable radiographic response [85]. Histone deacetylase inhibitors (HDACi) such as Vorinostat, which has a narrow therapeutic index, have shown safety/tolerability for the treatment of recurrent glioblastoma [86,87,88] but have not yet been combined with immunotherapies for clinical treatment of high-grade gliomas. In addition, the clinical efficacy of HDACi in improving progression-free or overall survival has yet to be demonstrated.
Several recurrent cancer-driving mutations are known to activate TEs that prime tumors for viral mimicry induction. One of the most studied examples is the H3.3K27M mutation in high-grade gliomas [89]. This mutation impairs the recruitment of the Polycomb complex, reduces facultative heterochromatinization, and thus activates DNA transposons, LINEs, and SINEs [81]. However, despite elevated retrotransposon expression, H3.3K27M gliomas do not have elevated IFN signaling, likely secondary to a cancer-specific compensatory mechanism. Treatment of high-grade glioma with either DNMTi or HDACi has been shown to more strongly promote MAVS-dependent induction of IFN and IFN-stimulated genes in H3.3K27M cancers than H3.3 wild-type cancers. The resulting enhanced dsRNA responses promote PKR-mediated cell death [89]. Therefore, although H3.3K27M gliomas lack IFN induction at baseline, H3K27me3 loss results in elevated retrotransposon expression and primes for viral mimicry responses to DNMTi and HDACi treatment.
Aside from ERVs, numerous studies have linked LINEs and SINEs to a viral mimicry response [12]. In fact, the cytosolic dsRNA sensor MDA5, a vital player in viral mimicry, was found to preferentially bind to the stem-loop structure formed by inverted-repeat Alus (IR-Alus) relative to the bidirectionally transcribed dsRNA structures of ERVs and LINEs [90]. IR-Alus is also the primary substrate for the A-to-I mRNA editor ADAR1 [91], which produces a modification that disrupts the RNA duplex and prevents MDA5-mediated dsRNA sensing [92]. Therefore, ADAR1 depletion increases cytosolic dsRNA levels and sensitizes cancer cells to treatment by viral mimicry inducers such as decitabine or CADK4/6 [90]. Furthermore, tumors with intrinsically high IFN signaling have been found to be ADAR1 dependent [93, 94], and thus, ADAR1 inhibition may be exploited for these viral mimicry-primed cells. On the other hand, immune-checkpoint blockade-resistant tumors in mice were found to be sensitive to both IFN and anti-PD1 blockade in ADAR1 deletion [95]. As immune checkpoint blockade resistance is common in high-grade gliomas, combined ADAR and epigenetic therapies may represent a novel path for a synthetic vulnerability to immunotherapies.
The mechanisms that dictate whether elevated dsRNAs induce sublethal or lethal IFN responses remain unclear. Survival of the subset of cancer cells with both high dsRNA levels and ADAR1 deficiency suggests that ADAR1-mediated editing is not the only mechanism cancer cells utilize to evade immunogenic cell death. As we strive to develop more robust and clinically relevant drugs, other RNA regulators and editors providing compensatory immunosuppression must also be explored. One recently found example is the RNA helicase DHX9 in breast cancer cells [96].
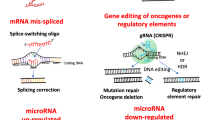
Long read methylome data indicates that hERV CpG methylation is lower at baseline than other TEs and the remaining genome in normal tissues [97]. Thus, it is probable that in many tumor cells, DNA methylation may not be the principal mechanism limiting ERV activation [98]. Though HDAC inhibitors and lysine methyltransferase inhibitors have been shown to synergize with DNMTis to activate ERVs [99, 100], other repressive and less characterized pathways likely provide compensatory effects. Further studies and improvements in epitranscriptomic mapping of gliomas are necessary to identify specific cancer-driving mutations in RNA modification regulators that prime tumors for viral mimicry. With crosstalk to epigenetic silencing already established, it is probable such mutations exist and may represent promising targets for novel high-grade glioma treatment in combination with immunotherapies and pre-transcriptional ERV regulation inhibitors (i.e., DNMTi and HDACi). Though several small molecule inhibitors of RNA modification regulators already exist, many must be redesigned to improve their BBB penetrance and levels in GBM. CRISPR-Cas systems developed for programmable RNA modification editing [101] and nucleotide-specific editing [102] expand the scope of RNA engineering and facilitate mechanistic understanding of the epitranscriptome. Like their DNA-targeting counterparts, RNA-targeting CRISPR-Cas systems may begin to be translated into the clinic in the coming years.
Post-transcriptional methods of viral mimicry induction are undergoing further study for recurrent cancers like glioblastoma. Despite its promise, the potential benefits of leveraging inducible hERV activity against solid tumors must be closely balanced with possible unintended consequences such as ERV onco-exaptation.
Future directions & translational endeavors
Several drugs, such as 5-azacytidine and decitabine inhibiting DNA methylation, are FDA-approved for hematological tumors. Of the many similarities and parallels between DNA and RNA methylation, the most similar is m5A. Interestingly, studies show the clinical response to hypomethylating therapies do not correlate with DNA methylation status, and approximately 90% of 5-azacytidine is incorporated into RNA [103]. Thus, these therapies’ antiproliferative effects, either RNA- or DNA-mediated, and drug-repurposing potential remain hotly debated, with further mechanistic studies needed.
Though no FDA-approved drugs currently target epitranscriptomic regulators, there is preclinical evidence of the anti-tumor effects of RNA-modifying therapy and a growing cadre of interested biotech companies [103]. Most small molecule inhibitors for RNA-modifying therapy have been developed against m6A regulators. For example, the METTL3–METTL14 catalytic activity inhibitor STM2457 has been validated in vitro and in vivo for hematological tumors [9]. Additionally, inhibitors against FTO, ALKBH5, IGF2BP1, and ADAR1 have shown promising anti-tumor properties in vitro and in vivo [104]. However, as mentioned previously, these inhibitors will likely require chemical modification to improve their BBB penetration for glioma treatment.
Utilizing glioblastoma stem cells (GSCs) and xenograft mice, MA2, the ethyl ester form of meclofenamic acid (MA), an FDA-approved non-steroidal anti-inflammatory drug, was identified as a selective inhibitor of FTO that increases m6A mRNA levels and suppresses GSC-initiated tumor progression [105, 106]. Similarly, small-molecule compounds inhibiting pseudouridine synthase 7 impair GSC growth in vitro and, in mouse xenografts, improve prognosis [107]. Lastly, inhibition of TYK2, a mediator of both PUS7- and ADAR1-containing pathways in GSCs, demonstrated impaired GSC self-renewal and stemness [108]. As these molecules enter clinical trials, how they affect the landscape of cancer therapies targeting gene expression dysregulation and impact GBM patient outcomes will be exciting.
Availability of data and materials
Not applicable.
References
Wirsching, H.-G., E. Galanis, and M. Weller. 2016 Chapter 23 – Glioblastoma. In Handbook of Clinical Neurology, M.S. Berger and M. Weller, Editors., Elsevier.
Fedele M, et al. Proneural-mesenchymal transition: phenotypic plasticity to acquire multitherapy resistance in glioblastoma. Int J Mol Sci. 2019;20(11):2746.
Yekula A, et al. Extracellular vesicles in glioblastoma tumor microenvironment. Front Immunol. 2020. https://doi.org/10.3389/fimmu.2019.03137.
Barbieri I, Kouzarides T. Role of RNA modifications in cancer. Nat Rev Cancer. 2020;20(6):303–22.
Zhao BS, Roundtree IA, He C. Post-transcriptional gene regulation by mRNA modifications. Nat Rev Mol Cell Biol. 2017;18(1):31–42.
Shelton SB, Reinsborough C, Xhemalce B. Who watches the watchmen: roles of RNA modifications in the RNA interference pathway. PLoS Genet. 2016;12(7):e1006139.
Esteller M, Pandolfi PP. The epitranscriptome of noncoding RNAs in cancer. Cancer Discov. 2017;7(4):359–68.
Sun H, et al. Regulation and functions of non-m(6)A mRNA modifications. Nat Rev Mol Cell Biol. 2023. https://doi.org/10.1038/s41580-023-00622-x.
Piperi C, et al. Deciphering glioma epitranscriptome: focus on RNA modifications. Oncogene. 2023;42(28):2197–206.
Tang Q, et al. RNA modifications in cancer. Br J Cancer. 2023;129(2):204–21.
Shah AH, et al. The role of human endogenous retroviruses in gliomas: from etiological perspectives and therapeutic implications. Neuro Oncol. 2021;23(10):1647–55.
Jansz N, Faulkner GJ. Endogenous retroviruses in the origins and treatment of cancer. Genome Biol. 2021;22(1):147.
Wang R, et al. CircNT5E Acts as a sponge of miR-422a to promote glioblastoma tumorigenesis. Can Res. 2018;78(17):4812–25.
Shi H, et al. Novel insight into the regulatory roles of diverse RNA modifications: Re-defining the bridge between transcription and translation. Mol Cancer. 2020;19(1):78.
Tűzesi Á, et al. Understanding the epitranscriptome for avant-garde brain tumour diagnostics. Cancers (Basel). 2023. https://doi.org/10.3390/cancers15041232.
Finkel D, Groner Y. Methylations of adenosine residues (m6A) in pre-mRNA are important for formation of late simian virus 40 mRNAs. Virology. 1983;131(2):409–25.
Bartosovic M, et al. N6-methyladenosine demethylase FTO targets pre-mRNAs and regulates alternative splicing and 3’-end processing. Nucleic Acids Res. 2017;45(19):11356–70.
Liu N, et al. N(6)-methyladenosine-dependent RNA structural switches regulate RNA-protein interactions. Nature. 2015;518(7540):560–4.
Fustin JM, et al. RNA-methylation-dependent RNA processing controls the speed of the circadian clock. Cell. 2013;155(4):793–806.
Wang X, et al. N(6)-methyladenosine modulates messenger RNA translation efficiency. Cell. 2015;161(6):1388–99.
Zheng G, et al. ALKBH5 is a mammalian RNA demethylase that impacts RNA metabolism and mouse fertility. Mol Cell. 2013;49(1):18–29.
Li X, et al. Transcriptome-wide mapping reveals reversible and dynamic N(1)-methyladenosine methylome. Nat Chem Biol. 2016;12(5):311–6.
Squires JE, et al. Widespread occurrence of 5-methylcytosine in human coding and non-coding RNA. Nucleic Acids Res. 2012;40(11):5023–33.
Yang X, et al. 5-methylcytosine promotes mRNA export - NSUN2 as the methyltransferase and ALYREF as an m(5)C reader. Cell Res. 2017;27(5):606–25.
Zhang HY, et al. The existence of 5-hydroxymethylcytosine and 5-formylcytosine in both DNA and RNA in mammals. Chem Commun (Camb). 2016;52(4):737–40.
Horowitz S, et al. Mapping of N6-methyladenosine residues in bovine prolactin mRNA. Proc Natl Acad Sci U S A. 1984;81(18):5667–71.
Kumar S, Mohapatra T. Deciphering epitranscriptome: modification of mrna bases provides a new perspective for post-transcriptional regulation of gene expression. Front Cell Dev Biol. 2021;9:628415.
Keszthelyi TM, Tory K. The importance of pseudouridylation: human disorders related to the fifth nucleoside. Biologia Futura. 2023;74(1):3–15.
Galeano F, et al. ADAR2-editing activity inhibits glioblastoma growth through the modulation of the CDC14B/Skp2/p21/p27 axis. Oncogene. 2013;32(8):998–1009.
Nigita G, Veneziano D, Ferro A. A-to-I RNA editing: current knowledge sources and computational approaches with special emphasis on non-coding rna molecules. Front Bioeng Biotechnol. 2015;3:37.
Mannion N, et al. New insights into the biological role of mammalian ADARs; the RNA editing proteins. Biomolecules. 2015;5(4):2338–62.
Wang Y, Zheng Y, Beal PA. Adenosine Deaminases That Act on RNA (ADARs). Enzymes. 2017;41:215–68. https://doi.org/10.1016/bs.enz.2017.03.006.
Samuel CE. ADARs: viruses and innate immunity. Curr Top Microbiol Immunol. 2012;353(1):163–95.
Melcher T, et al. RED2, a Brain-specific member of the RNA-specific adenosine Deaminase family*. J Biol Chem. 1996;271(50):31795–8.
Chen CX, et al. A third member of the RNA-specific adenosine deaminase gene family, ADAR3, contains both single- and double-stranded RNA binding domains. RNA. 2000;6(5):755–67.
Cho D-SC, et al. Requirement of dimerization for RNA editing activity of adenosine deaminases acting on RNA*. J Biol Chem. 2003;278(19):17093–102.
Licht K, et al. A high resolution A-to-I editing map in the mouse identifies editing events controlled by pre-mRNA splicing. Genome Res. 2019;29(9):1453–63.
Chalk AM, et al. The majority of A-to-I RNA editing is not required for mammalian homeostasis. Genome Biol. 2019. https://doi.org/10.1186/s13059-019-1873-2.
Raghava Kurup R, et al. RNA binding by ADAR3 inhibits adenosine-to-inosine editing and promotes expression of immune response protein MAVS. J Biol Chem. 2022;298(9):102267.
Torres AG, et al. A-to-I editing on tRNAs: biochemical, biological and evolutionary implications. FEBS Lett. 2014;588(23):4279–86.
Taguchi Y-H. Bioinformatic tools for epitranscriptomics. Am J Physiol Cell Physiol. 2023;324(2):C447–57.
Zhang B, et al. m6A regulator-mediated methylation modification patterns and tumor microenvironment infiltration characterization in gastric cancer. Mol Cancer. 2020;19(1):53.
Lin S, et al. Prognosis analysis and validation of m(6)A signature and tumor immune microenvironment in glioma. Front Oncol. 2020;10:541401.
Chai RC, et al. m(6)A RNA methylation regulators contribute to malignant progression and have clinical prognostic impact in gliomas. Aging (Albany NY). 2019;11(4):1204–25.
Chang YZ, et al. METTL3 enhances the stability of MALAT1 with the assistance of HuR via m6A modification and activates NF-κB to promote the malignant progression of IDH-wildtype glioma. Cancer Lett. 2021;511:36–46.
Li G, et al. RNA modification patterns based on major RNA modifications define tumor microenvironment characteristics in glioblastoma. Sci Rep. 2022;12(1):10278.
McGranahan T, et al. Current state of immunotherapy for treatment of glioblastoma. Curr Treat Options Oncol. 2019;20(3):24.
Pan Y, et al. RNA N6-methyladenosine regulator-mediated methylation modifications pattern and immune infiltration features in glioblastoma. Front Oncol. 2021. https://doi.org/10.3389/fonc.2021.632934.
Zhu J, et al. Pan-cancer molecular characterization of m6a regulators and immunogenomic perspective on the tumor microenvironment. Front Oncol. 2021. https://doi.org/10.3389/fonc.2020.618374.
Xu S, et al. Expression of m6A regulators correlated with immune microenvironment predicts therapeutic efficacy and prognosis in gliomas. Front Cell Dev Biol. 2020. https://doi.org/10.3389/fcell.2020.594112.
Chen H, et al. Cross-talk of four types of RNA modification writers defines tumor microenvironment and pharmacogenomic landscape in colorectal cancer. Mol Cancer. 2021;20(1):29.
Chong W, et al. m(6)A regulator-based methylation modification patterns characterized by distinct tumor microenvironment immune profiles in colon cancer. Theranostics. 2021;11(5):2201–17.
Zheng B, et al. A new m6A methylation-related gene signature for prognostic value in patient with urothelial carcinoma of the bladder. 2021. Biosci Rep. https://doi.org/10.1042/BSR20204456.
Li Y, et al. Molecular characterization, biological function, tumor microenvironment association and clinical significance of m6A regulators in lung adenocarcinoma. Brief Bioinform. 2020. https://doi.org/10.1093/bib/bbaa225.
Yi L, et al. Comprehensive analysis of the PD-L1 and immune infiltrates of m<sup>6</sup>A RNA Methylation regulators in head and neck squamous cell carcinoma. Mol Ther Nucleic Acids. 2020;21:299–314.
Han D, Xu MM. RNA modification in the immune system. Annu Rev Immunol. 2023;41(1):73–98.
Zhou H, et al. Evolution of a reverse transcriptase to map N(1)-methyladenosine in human messenger RNA. Nat Methods. 2019;16(12):1281–8.
Ramaswami G, et al. Accurate identification of human Alu and non-Alu RNA editing sites. Nat Methods. 2012;9(6):579–81.
Begik O, Mattick JS, Novoa EM. Exploring the epitranscriptome by native RNA sequencing. RNA. 2022;28(11):1430–9.
Lee AC, et al. Spatial epitranscriptomics reveals A-to-I editome specific to cancer stem cell microniches. Nat Commun. 2022;13(1):2540.
Rivas SR, et al. The role of HERV-K in cancer stemness. Viruses. 2022;14(9):2019.
Bourque G, et al. Ten things you should know about transposable elements. Genome Biol. 2018;19(1):199.
Dopkins N, et al. A field guide to endogenous retrovirus regulatory networks. Mol Cell. 2022;82(20):3763–8.
Deniz Ö, et al. Endogenous retroviruses are a source of enhancers with oncogenic potential in acute myeloid leukaemia. Nat Commun. 2020;11(1):3506.
Misra A, et al. Alteration of a sequence with homology to human endogenous retrovirus (HERV-K) in primary human glioma: implications for viral repeat mediated rearrangement. Mutat Res. 2001;484(1–2):53–9.
Kessler AF, et al. Expression-analysis of the human endogenous retrovirus HERV-K in human astrocytic tumors. BMC Res Notes. 2014;7:159.
Choi WI, et al. Role of promyelocytic leukemia zinc finger (PLZF) in cell proliferation and cyclin-dependent kinase inhibitor 1A (p21WAF/CDKN1A) gene repression. J Biol Chem. 2014;289(27):18625–40.
Armbruester V, et al. Np9 protein of human endogenous retrovirus K interacts with ligand of numb protein X. J Virol. 2004;78(19):10310–9.
Chen J, et al. Characterization of human LNX, a novel ligand of Numb protein X that is downregulated in human gliomas. Int J Biochem Cell Biol. 2005;37(11):2273–83.
Argaw-Denboba A, et al. HERV-K activation is strictly required to sustain CD133+ melanoma cells with stemness features. J Exp Clin Cancer Res. 2017;36(1):20.
Wang T, et al. Regulation of stem cell function and neuronal differentiation by HERV-K via mTOR pathway. Proc Natl Acad Sci U S A. 2020;117(30):17842–53.
Nawashiro H, et al. The role of CD98 in astrocytic neoplasms. Hum Cell. 2002;15(1):25–31.
Kan RL, Chen J, Sallam T. Crosstalk between epitranscriptomic and epigenetic mechanisms in gene regulation. Trends Genet. 2022;38(2):182–93.
Zaccara S, Ries RJ, Jaffrey SR. Reading, writing and erasing mRNA methylation. Nat Rev Mol Cell Biol. 2019;20(10):608–24.
Geula S, et al. m6A mRNA methylation facilitates resolution of naive pluripotency toward differentiation. Science. 2015;347(6225):1002–6.
Allshire RC, Madhani HD. Ten principles of heterochromatin formation and function. Nat Rev Mol Cell Biol. 2018;19(4):229–44.
Chelmicki T, et al. m6A RNA methylation regulates the fate of endogenous retroviruses. Nature. 2021;591(7849):312–6.
Xu W, et al. METTL3 regulates heterochromatin in mouse embryonic stem cells. Nature. 2021;591(7849):317–21.
Liu J, et al. The RNA m6A reader YTHDC1 silences retrotransposons and guards ES cell identity. Nature. 2021;591(7849):322–6.
Huang H, et al. Histone H3 trimethylation at lysine 36 guides m6A RNA modification co-transcriptionally. Nature. 2019;567(7748):414–9.
Chen R, Ishak CA, De Carvalho DD. Endogenous retroelements and the viral mimicry response in cancer therapy and cellular homeostasis. Cancer Discov. 2021;11(11):2707–25.
Roulois D, et al. DNA-demethylating agents target colorectal cancer cells by inducing viral mimicry by endogenous transcripts. Cell. 2015;162(5):961–73.
Chiappinelli KB, et al. Inhibiting DNA methylation causes an interferon response in cancer via dsRNA including endogenous retroviruses. Cell. 2015;162(5):974–86.
Kong Y, et al. Transposable element expression in tumors is associated with immune infiltration and increased antigenicity. Nat Commun. 2019;10(1):5228.
Federici L, et al. 5-Azacitidine in patients with IDH1/2-mutant recurrent glioma. Neuro Oncol. 2020;22(8):1226–8.
Friday BB, et al. Phase II trial of vorinostat in combination with bortezomib in recurrent glioblastoma: a north central cancer treatment group study. Neuro Oncol. 2012;14(2):215–21.
Lee EQ, et al. Phase I study of vorinostat in combination with temozolomide in patients with high-grade gliomas: North American Brain Tumor Consortium Study 04–03. Clin Cancer Res. 2012;18(21):6032–9.
Peters KB, et al. Phase I/II trial of vorinostat, bevacizumab, and daily temozolomide for recurrent malignant gliomas. J Neurooncol. 2018;137(2):349–56.
Krug B, et al. Pervasive H3K27 acetylation leads to ERV expression and a therapeutic vulnerability in H3K27M gliomas. Cancer Cell. 2019;35(5):782-797.e8.
Mehdipour P, et al. Epigenetic therapy induces transcription of inverted SINEs and ADAR1 dependency. Nature. 2020;588(7836):169–73.
Levanon EY, et al. Systematic identification of abundant A-to-I editing sites in the human transcriptome. Nat Biotechnol. 2004;22(8):1001–5.
Liddicoat BJ, et al. RNA editing by ADAR1 prevents MDA5 sensing of endogenous dsRNA as nonself. Science. 2015;349(6252):1115–20.
Gannon HS, et al. Identification of ADAR1 adenosine deaminase dependency in a subset of cancer cells. Nat Commun. 2018;9(1):5450.
Liu H, et al. Tumor-derived IFN triggers chronic pathway agonism and sensitivity to ADAR loss. Nat Med. 2019;25(1):95–102.
Ishizuka JJ, et al. Loss of ADAR1 in tumours overcomes resistance to immune checkpoint blockade. Nature. 2019;565(7737):43–8.
Cottrell KA, Ryu S, Torres LS, Schab AM, Weber JD. Induction of viral mimicry upon loss of DHX9 and ADAR1 in breast cancer cells. bioRxiv. 2023. https://doi.org/10.1101/2023.02.27.530307.
Ewing AD, et al. Nanopore sequencing enables comprehensive transposable element epigenomic profiling. Mol Cell. 2020;80(5):915-928.e5.
López-Moyado IF, et al. Paradoxical association of TET loss of function with genome-wide DNA hypomethylation. Proc Natl Acad Sci U S A. 2019;116(34):16933–42.
Brocks D, et al. DNMT and HDAC inhibitors induce cryptic transcription start sites encoded in long terminal repeats. Nat Genet. 2017;49(7):1052–60.
Liu M, et al. Dual inhibition of DNA and histone methyltransferases increases viral mimicry in ovarian cancer cells. Cancer Res. 2018;78(20):5754–66.
Liu XM, et al. Programmable RNA N(6)-methyladenosine editing by CRISPR-Cas9 conjugates. Nat Chem Biol. 2019;15(9):865–71.
Lo N, et al. The basis and promise of programmable RNA editing and modification. Front Genet. 2022. https://doi.org/10.3389/fgene.2022.834413.
Berdasco M, Esteller M. Towards a druggable epitranscriptome: Compounds that target RNA modifications in cancer. Br J Pharmacol. 2022;179(12):2868–89.
Cully M. Chemical inhibitors make their RNA epigenetic mark. Nat Rev Drug Discov. 2019;18(12):892–4.
Cui Q, et al. m6A RNA methylation regulates the self-renewal and tumorigenesis of glioblastoma stem cells. Cell Rep. 2017;18(11):2622–34.
Huang Y, et al. Meclofenamic acid selectively inhibits FTO demethylation of m6A over ALKBH5. Nucleic Acids Res. 2014;43(1):373–84.
Cui Q, et al. Targeting PUS7 suppresses tRNA pseudouridylation and glioblastoma tumorigenesis. Nature Cancer. 2021;2(9):932–49.
Jiang, L., et al., ADAR1-mediated RNA editing links ganglioside catabolism to glioblastoma stem cell maintenance. J Clin Invest, 2022. 132(6).
Li F, et al. N(6)-methyladenosine modulates nonsense-mediated mRNA decay in human glioblastoma. Cancer Res. 2019;79(22):5785–98.
Fang R, et al. EGFR/SRC/ERK-stabilized YTHDF2 promotes cholesterol dysregulation and invasive growth of glioblastoma. Nat Commun. 2021;12(1):177.
Dixit D, et al. The RNA m6A reader YTHDF2 maintains oncogene expression and is a targetable dependency in glioblastoma stem cells. Cancer Discov. 2021;11(2):480–99.
Yin D, Kong C, Chen M. Effect of hnRNPA2/B1 on the proliferation and apoptosis of glioma U251 cells via the regulation of AKT and STAT3 pathways. 2020. Biosci Rep. https://doi.org/10.1042/BSR20190318.
Wang H, Xu B, Shi J. N6-methyladenosine METTL3 promotes the breast cancer progression via targeting Bcl-2. Gene. 2020;722:144076.
Vu LP, et al. The N(6)-methyladenosine (m(6)A)-forming enzyme METTL3 controls myeloid differentiation of normal hematopoietic and leukemia cells. Nat Med. 2017;23(11):1369–76.
Dome A, et al. Post-transcriptional modifications of RNA as regulators of apoptosis in glioblastoma. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23169272.
Liu Z, et al. ALKBH5 promotes the proliferation of glioma cells via enhancing the mRNA stability of G6PD. Neurochem Res. 2021;46(11):3003–11.
Zhang S, et al. m(6)A demethylase ALKBH5 maintains tumorigenicity of glioblastoma stem-like cells by sustaining FOXM1 expression and cell proliferation program. Cancer Cell. 2017;31(4):591-606.e6.
Wang J, Sha Y, Sun T. m(6)A modifications play crucial roles in glial cell development and brain tumorigenesis. Front Oncol. 2021;11:611660.
Su R, et al. R-2HG exhibits anti-tumor activity by targeting FTO/m(6)A/MYC/CEBPA signaling. Cell. 2018;172(1–2):90-105.e23.
Macari F, et al. TRM6/61 connects PKCα with translational control through tRNAi(Met) stabilization: impact on tumorigenesis. Oncogene. 2016;35(14):1785–96.
Wang B, et al. RNA m1A methyltransferase TRMT6 predicts poorer prognosis and promotes malignant behavior in glioma. Front Mol Biosci. 2021;8:692130.
Mongiardi MP, et al. c-MYC inhibition impairs hypoxia response in glioblastoma multiforme. Oncotarget. 2016;7(22):33257–71.
Li X, Meng Y. Expression and prognostic characteristics of m(5) C regulators in low-grade glioma. J Cell Mol Med. 2021;25(3):1383–93.
Paz N, et al. Altered adenosine-to-inosine RNA editing in human cancer. Genome Res. 2007;17(11):1586–95.
Quin J, et al. ADAR RNA modifications, the epitranscriptome and innate immunity. Trends Biochem Sci. 2021;46(9):758–71.
Oakes E, et al. Adenosine deaminase that acts on RNA 3 (ADAR3) binding to glutamate receptor subunit B Pre-mRNA inhibits RNA editing in glioblastoma. J Biol Chem. 2017;292(10):4326–35.
Raghava Kurup R, et al. ADAR3 activates NF-κB signaling and promotes glioblastoma cell resistance to temozolomide. Sci Rep. 2022;12(1):13362.
Hu G, et al. Prognostic markers identification in glioma by gene expression profile analysis. J Comput Biol. 2020;27(1):81–90.
Wang LJ, et al. Gene expression-based predication of rna pseudouridine modification in tumor microenvironment and prognosis of glioma patients. Front Cell Dev Biol. 2021;9:727595.
Miao FA, et al. Increased DKC1 expression in glioma and its significance in tumor cell proliferation, migration and invasion. Invest New Drugs. 2019;37(6):1177–86.
Berman HM, et al. The protein data bank. Nucleic Acids Res. 2000;28(1):235–42.
Turelli P, et al. Interplay of TRIM28 and DNA methylation in controlling human endogenous retroelements. Genome Res. 2014;24(8):1260–70.
Shi H, et al. ZFP57 regulation of transposable elements and gene expression within and beyond imprinted domains. Epigenetics Chromatin. 2019;12(1):49.
Liu N, et al. Selective silencing of euchromatic L1s revealed by genome-wide screens for L1 regulators. Nature. 2018;553(7687):228–32.
Robbez-Masson L, et al. The HUSH complex cooperates with TRIM28 to repress young retrotransposons and new genes. Genome Res. 2018;28(6):836–45.
Tchasovnikarova IA, et al. Epigenetic silencing by the HUSH complex mediates position-effect variegation in human cells. Science. 2015;348(6242):1481–5.
Seczynska M, et al. Genome surveillance by HUSH-mediated silencing of intronless mobile elements. Nature. 2022;601(7893):440–5.
Wilson BG, Roberts CWM. SWI/SNF nucleosome remodellers and cancer. Nat Rev Cancer. 2011;11(7):481–92.
Kim H, et al. The gene-silencing protein MORC-1 topologically entraps DNA and forms multimeric assemblies to cause DNA compaction. Mol Cell. 2019;75(4):700-710.e6.
Chen X, et al. Lymphoid-specific helicase in epigenetics, DNA repair and cancer. Br J Cancer. 2022;126(2):165–73.
Ren J, et al. The ATP binding site of the chromatin remodeling homolog Lsh is required for nucleosome density and de novo DNA methylation at repeat sequences. Nucleic Acids Res. 2015;43(3):1444–55.
Cosby RL, Chang NC, Feschotte C. Host-transposon interactions: conflict, cooperation, and cooption. Genes Dev. 2019;33(17–18):1098–116.
Lubas M, et al. Interaction profiling identifies the human nuclear exosome targeting complex. Mol Cell. 2011;43(4):624–37.
Garland W, et al. Chromatin modifier HUSH co-operates with RNA decay factor NEXT to restrict transposable element expression. Mol Cell. 2022;82(9):1691-1707.e8.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
CKR and AHS conceived the manuscript. CKR wrote the manuscript and prepared the figures. All authors edited and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ramsoomair, C.K., Ceccarelli, M., Heiss, J.D. et al. The epitranscriptome of high-grade gliomas: a promising therapeutic target with implications from the tumor microenvironment to endogenous retroviruses. J Transl Med 21, 893 (2023). https://doi.org/10.1186/s12967-023-04725-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-023-04725-z