Abstract
Background
To ensure the long-term sustainability of its Community-Based Health Insurance scheme, the Government of Rwanda is working on using Health Technology Assessment (HTA) to prioritize its resources for health. The objectives of the study were to rapidly assess (1) the cost-effectiveness and (2) the budget impact of providing PD versus HD for patients with acute kidney injury (AKI) in the tertiary care setting in Rwanda.
Methods
A rapid cost-effectiveness analysis for patients with AKI was conducted to support prioritization. An ‘adaptive’ HTA approach was undertaken by adjusting the international Decision Support Initiative reference case for time and data constraints. Available local and international data were used to analyze the cost-effectiveness and budget impact of peritoneal dialysis (PD) compared with hemodialysis (HD) in the tertiary hospital setting.
Results
The analysis found that HD was slightly more effective and slightly more expensive in the payer perspective for most patients with AKI (aged 15–49). HD appeared to be cost-effective when only comparing these two dialysis strategies with an incremental cost-effectiveness ratio of 378,174 Rwandan francs (RWF) or 367 United States dollars (US$), at a threshold of 0.5 × gross domestic product per capita (RWF 444,074 or US$431). Sensitivity analysis found that reducing the cost of HD kits would make HD even more cost-effective. Uncertainty regarding PD costs remains.
Budget impact analysis demonstrated that reducing the cost of the biggest cost driver, HD kits, could produce significantly more savings in five years than switching to PD. Thus, price negotiations could significantly improve the efficiency of HD provision.
Conclusion
Dialysis is costly and covered by insurance in many countries for the financial protection of patients. This analysis enabled policymakers to make evidence-based decisions to improve the efficiency of dialysis provision.
Similar content being viewed by others
Introduction
Background
Rwanda’s community-based health insurance (CBHI) scheme covers more than 80% of the population, most of whom are in the informal sector [1]. The scheme has three main funding sources: member contributions, government subsidies, and donors, and operates mostly on a fee-for-service basis [2]. Members are entitled to a comprehensive benefits package covering drugs and medical services, and their contributions vary based on income level [3]. Co-payments are 200 Rwandan francs (RWF) at the health post level, and 10% of the total bill at higher levels of care [3]. As part of the scheme’s success, the government continues to face growing demand for a wide range of healthcare services, which it must balance with an estimated $58 per capita expenditure on health [4].
To strengthen the financial sustainability of the CBHI scheme, health technology assessment (HTA) is being introduced to support explicit, evidence-informed priority setting [5]. As a first step, a rapid cost-effectiveness analysis on dialysis for acute kidney injury (AKI) was undertaken [6].
Dialysis is a common topic of interest for low- and middle-income countries (LMICs) facing a growing burden of non-communicable diseases due to its high costs [7]. Across LMICs, only 2–5% of patients needing treatment receive it; for many, it is unaffordable [8]. At the time of analysis, six weeks of dialysis was covered by CBHI in Rwanda with a 10% co-pay, averaging 218,000 RWF out of pocket per patient [9]. For scale, this represents 25% of GDP per capita [10].
Some LMICs have conducted cost-effectiveness analyses on dialysis to inform their coverage decisions [11, 12]. However, these have been disproportionately focused on dialysis for patients with end-stage renal disease (ESRD) [13,14,15,16]. ESRD is the last stage of chronic kidney disease (CKD), which permanently impairs kidney function and renders patients ‘dialysis dependent’ to survive.
Dialysis is also used to treat AKI, which, unlike ESRD, temporarily impairs kidney function. AKI is reversible if diagnosed and treated early. Depending on the severity of a kidney injury, patients may only need dialysis for a limited period to allow for at least partial, and sometimes full recovery of kidney function.
LMICs bear a disproportionate amount of the globally estimated burden of AKI [17], and in these countries, it is commonly a disease of the young, often caused by a single, curable condition [17,18,19,20]. In Rwanda, the most common comorbidities include malaria; pneumonia; sepsis; pregnancy-related conditions such as eclampsia and hypertension; intoxication caused by treatment from traditional healers; and diabetes [21]. The median age for AKI patients in Rwanda is 38 years old, and the mortality rate is 34% [21]. However, barriers to optimal management of AKI in Rwanda remain. These include knowledge gaps among healthcare providers, sub-optimal diagnostic capacity, particularly in sub-tertiary hospitals, and limited treatment options [22].
The main treatment options for AKI in Rwanda are hemodialysis (HD) and peritoneal dialysis (PD). Evidence suggests little difference when comparing HD and PD in terms of their clinical outcomes or the risk of complications – though the evidence base remains moderate to poor [23].
Currently, all dialysis provision in Rwanda is exclusively delivered in the hospital setting. Most of this provision is HD, with a small proportion being PD. While in other settings, HD is often provided in hospitals and PD in smaller facilities or at home this type of PD was discontinued a few years ago in Rwanda. This was partially because of challenges in sourcing dialysate and difficulty in guaranteeing hygienic conditions for at-home PD.
Aim and objectives
At the time of writing, Rwanda’s CBHI benefits package officially covered up to six weeks of dialysis per patient with AKI. Dialysis for ESRD was not covered. However, the diagnosis of AKI versus CKD can sometimes be challenging, especially when there is a previously undiagnosed kidney dysfunction. Due to the considerable cost of providing dialysis, this study aimed to help the Rwandan CBHI scheme decide on the optimal delivery of dialysis services.
The objectives of the study were to rapidly assess (1) the cost-effectiveness and (2) the budget impact of providing PD versus HD for patients with AKI in the tertiary care setting in Rwanda. This may be the first study of its kind comparing dialysis modalities for AKI in LMICs where both HD and PD are provided exclusively at the tertiary care level.
Methods
Our rapid cost-effectiveness analysis used an ‘adaptive’ HTA (aHTA) approach, which adjusts HTA methods for time, data, and capacity constraints [24]. To respond to policy makers’ demand, the aim was to complete the assessment in six weeks. It was thus decided to use a rapid cost-effectiveness analysis which builds basic economic models using opportunistically or rapidly sourced local data [24]. The assessment used the international decision support initiative (iDSI) reference case for economic evaluation as a guide [6, 25]. Table 1 summarizes the application of the eleven iDSI reference case principles. Highlighted rows indicate principles that were adapted for time and data constraints.
Population and subgroups
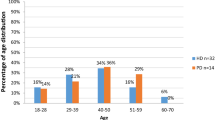
The population for this analysis were dialysis-eligible patients with AKI in a tertiary care facility in Rwanda. Two age groups were considered: patients aged 15–49 and patients aged 50 and above.
Comparators
The intervention was tertiary care delivered PD, compared with tertiary care delivered HD. In the base case, the model assumed that patients receive the maximum allotted care covered by CBHI. This included three sessions per week for six weeks of HD or six weeks of continuous ambulatory PD for hospitalized patients.
Model structure and assumptions
A de novo Markov model was used to reflect the costs and effects of the initial acute condition of AKI combined with the long-term health effects that can follow the condition. The cycle length was one year (Appendix 1). The model was informed by the published literature and validated through consultation with local and international nephrology specialists. Patients enter the model at the tertiary care facility, starting on hospital HD or hospital PD. Over time, patients may stay with the same modality or switch modalities. They may develop complications or not, and subsequently fully recover rendering them dialysis independent or partially recover with no further treatment. They may then die from AKI progressing to CKD, from co-morbidities, or from natural causes.
Modelling perspective and scenarios
A payer perspective was used. The payer perspective included all direct medical costs to Rwanda Social Security Board (RSSB) plus salaries, overhead, and depreciation of the HD machines paid by the Ministry of Health. A ‘decreased provision’ scenario was also explored, which assumed the actual number of sessions patients receive on average was five instead of the full eighteen sessions [9].
Evidence for model parameters
Given an initially short timeline, a pragmatic approach was taken to select data to inform the model. Available local data was supplemented by a rapid literature search and sources known to the authors (Appendix 2). Where needed, gaps were addressed based on personal communication involving Rwandan nephrologists and international experts.
Cost and resource use
Costs and resource use data were sourced primarily from a 2018 RSSB Utilization and Expenditure Review on Dialysis made available by RSSB [9]. These were supplemented by published data from other jurisdictions and assumptions made by co-authors on this study. The total cost for HD, PD, and palliative care are expressed as per patient unit costs and reflect the cost of providing HD and PD at the tertiary care level (Table 2). Direct medical costs (including catheters, drugs, lab tests, kits, dialysate, other consumables, and palliative care) were sourced from an average across four facilities for HD and one facility for PD. Direct non-medical costs (costs of healthcare professionals, overheads, and depreciation) were estimated by combining local reports, peer-reviewed literature, and personal communication and allocated per patient based on patient volumes. Only one facility provides a minimal amount of PD, and thus there remain uncertainties regarding the PD unit costs. All costs are incurred during the six weeks of treatment; no additional costs of complications were included. For further details of costs included, see Appendix 3.
Costs in the model are expressed in RWF and are inflated to 2022 prices using the Consumer Price Index [26]. They are converted to current US dollars using the latest available exchange rate of 1 United States dollar (US$):1030 RWF [27].
Effectiveness
Clinical effectiveness parameters were drawn from several sources. Population mortality rates were sourced from the World Health Organization’s Global Health Observatory Data repository[28]. Mortality rates for AKI patients undergoing dialysis were from a local observational study [21]. Transition probabilities were from an Indonesian study that compared HD and PD for patients with ESRD [14], and on assumptions made by co-authors of this study.
Quality-adjusted life years (QALYs) were the primary health outcome in this study. Utility values for dialysis patients with AKI were sourced from two studies from Argentina and Canada, which used the EuroQoL EQ-5D-3L [29, 30]. Utility values for dialysis independence was sourced from Garay et al. [30].
Discounting
Costs and outcomes were discounted at a standard 3% per annum after the first year following the iDSI Reference Case, though most costs are incurred in the first year[25]. The impact of varying the discount rate between 0 to 5% was explored in a sensitivity analysis [31].
Thresholds
The base case analysis uses a cost-effectiveness threshold of 0.5 × GDP per capita (RWF 444,074 or US$431). This is broadly in line with recently estimated values for Rwanda based on cross-country studies of US$325 to US$426 (2022), or 39%–51% of GDP per capita[32,33,34].
Analyses
The cost-effectiveness analysis was completed in TreeAge software (version 2023 R1.2), and the budget impact analysis in Microsoft Excel. Uncertainty was analyzed using one-way sensitivity analysis and probabilistic sensitivity analysis (PSA), with distributions set according to standard practice for different parameter types.
Results
Base-case results
Overall, the intervention (PD) was less expensive and less effective relative to the comparator (HD). Table 3 presents the incremental costs and QALYs for the intervention (PD) and status quo (HD), stratified by age. The total estimated per patient cost for PD was RWF 1,824,886 (US$1,771) compared with a total estimated cost of HD of RWF 2,059,354 (US$1,999). The expected net QALYs lost in delivering PD compared with HD were -0.62 for patients aged 15–49 and -0.27 for those over 50, the latter due to the older cohort’s increased mortality rate.
At a threshold of 0.5 × GDP per capita (RWF 444,074 or US$431), the analysis suggests that HD provision, as the standard of care, was cost-effective compared with PD provision for patients aged 15–49, with an ICER below the threshold at RWF 378,174 (US$367). Notably, the interpretation of the ICER (Table 3) is reversed, because incremental costs and effects are both negative[35]. In other words, the ICER falls below the threshold, and thus the comparator (HD) is considered cost-effective.
For patients above 50, the analysis suggests that PD was the preferred option compared with HD with an ICER of RWF 868,399 (US$843). The same reverse interpretation of the ICER also applies to this scenario; as the ICER is above the threshold, PD is the preferred option (Table 3).
One-way sensitivity analysis
One-way deterministic sensitivity analysis was applied to individual parameters that affected the ICER most. Varying the costs of HD kits, HD commodities, HD salaries, and HD overhead by ± 30% increased the ICER when the cost of each parameter increased, and decreased the ICER when the cost of each parameter decreased. When varying the cost of PD dialysate, PD commodities, PD salaries, and PD overhead by ± 30%, increasing the costs of the parameters decreased the ICER, and decreasing the costs increased the ICER. In other words, this suggests that there may be opportunities to reduce HD-related costs and enhance the favorability of the ICER; but the same is not true for PD. See Appendix 4 for a tornado diagram.
Scenario analysis
In the reduced provision scenario, HD appeared to be cost-effective compared with PD. Again, for both age groups, the ICER falls below the threshold (Table 4).
Probabilistic sensitivity analysis
PSA was used to estimate the joint impact of uncertainty in all input parameters. Gamma distributions were applied to costs and beta distributions to health utilities (Table 2). By randomly sampling from each parameter distribution, 10,000 Monte Carlo simulations of incremental costs and incremental effects were obtained. The results of the PSA are presented in two figures. An incremental cost-effectiveness scatterplot (Fig. 1) and a cost-effectiveness acceptability curve (CEAC) (Fig. 2), which both summarize the impact of uncertainty in relation to the threshold[36]. At the threshold of 0.5 × GDP (RWF 444,074 or US$431) and above, HD provision has a 56% probability of being cost-effective relative to PD.
Budget impact analysis
The budget impact analysis rapidly assessed the five-year (2020–2024) costs associated with providing dialysis services in four scenarios. In the baseline scenario, ‘HD preferred,’ a stable distribution of HD (91%) to PD (9%) was maintained (i.e., status quo). Alternative scenarios included scenario 1–5% annual shift to PD provision over 5 years; scenario 2–10% annual shift to PD provision over 5 years; and scenario 3—HD provision maintained at 91% but with reduced costs for HD kits. Compared to an ‘HD preferred’ baseline scenario, shifting to PD coverage would generate some savings. Maintaining an HD-preferred strategy and decreasing the cost of HD kits could achieve significantly more savings because HD kits represent more than half of the overall baseline cost of dialysis (Table 5).
Discussion
At a threshold of 0.5 × GDP per capita, the analysis suggests that HD is cost-effective compared with PD for most AKI patients receiving dialysis in Rwanda, i.e., those aged 15–49 years. The budget impact analysis suggests that shifting to PD would cost less than maintaining the status quo over five years. However, it also suggests that maintaining the HD status quo and decreasing the cost of the HD kit, which is a major cost driver in providing HD, would save even more than shifting to PD. A reduction in the cost of the kit could also reduce the overall co-pay for the patient.
One-way sensitivity analysis suggests that decreasing the cost of HD commodities and kits decreases the ICER. This may be achievable, as one hospital, Rwanda Military Hospital (RMH), procures HD kits directly from a local supplier and pays about half the price of those procured for other hospitals providing dialysis [9]. If all hospitals were to get the RMH price for kits, the ICER would decrease to below the threshold for all ages, and HD would be more cost-effective relative to PD. Indeed, this information has led to ongoing price negotiations for the kits for all facilities.
This study contributes to a sparse literature on dialysis for AKI. A recent systematic review published after the time of analysis identified only seven other studies on dialysis for patients with AKI, with mixed results and a recent increase in industry-sponsored studies [37]. Our study is thus a valuable, independent contributor to this sparse literature.
From a cost-effectiveness perspective, this analysis should be seen only as a starting point for discussion rather than a policy recommendation. Indeed, results of the PSA illustrate that HD is slightly more cost-effective at the threshold compared with PD, but there is still uncertainty. Moreover, policymakers raise several issues that the analysis cannot address. These include the cost or requirements for changing or expanding services; the cost-effectiveness of service delivery at lower levels of care; and the impact of removing patient co-pays.
Additionally, since the time of analysis, dialysis policies have changed in Rwanda. More coverage of dialysis is now available, as is kidney transplantation. Our analysis reflects the coverage at the time of analysis, and further analyses could be conducted to reflect current available health services.
Limitations
Our rapid cost-effectiveness analysis has several important limitations.
The study team’s approach to data collection was largely pragmatic, given time constraints. No attempts were made to synthesize the evidence for input parameters quantitatively or to systematically quality assure the data using available checklists. Data for the model came from several sources focused on patients with AKI where possible and supplemented by studies on CKD, author assumptions, and personal communication. Utility values, survival data, and transition probabilities are from various international sources. Importantly, the age of patients in papers from which utility values were sourced ranged from 45-to 65, while the average Rwandan dialysis patient is 38, and thus, utilities were overestimated. Local costing data were valuable in contextualizing the study. However, they were more focused on HD due to limited provision of PD, and they excluded the cost of infrastructure, overhead, and staff time for both HD or PD [9]. Other local reports, co-author assumptions and personal communication were used to fill data gaps, including staff time and equipment costs. Overhead was estimated as a percentage of operating costs (overhead + staff). Uncertainty remains about the costs and resources needed for PD because the local secondary data used reflected sparse provision of PD in hospitals. If time had allowed, the study would have benefited from more detailed costing on PD.
While the aim was to complete the analysis within six weeks, ultimately the assessment took about three to four months to complete.
Generalizability
A few factors may limit this study’s generalizability. First, these results reflect an analysis of PD and HD delivered in a tertiary care setting due to current practice and data availability. If the intervention had been PD delivered at lower-level facilities or at home, as is often the case in other countries, the analysis may have found PD to be much more cost-effective[13]. Second, these results are based on a time and data-constrained analysis that pragmatically sourced local and international data. This increased the chance of uncertainty and bias. Our findings may have limited generalizability to other contexts and should not be interpreted without caution alongside other studies on dialysis in LMICs. Other studies often focus on ESRD patients who can either get HD in hospital or PD in lower-level facilities or at home, and often conclude that a PD-first policy is preferable[13,14,15,16]. If policymakers in Rwanda were considering coverage options for patients with ESRD or lower-level provision of PD, a separate cost-effectiveness analysis and budget impact analysis would need to be undertaken to understand the implications of the new policy choice.
Reflections on ‘adaptive’ HTA
This cost-effectiveness analysis undertook an aHTA approach by deviating from what may be regarded as the ‘gold standard’ of HTA. This was done to reflect the local policymaker context, the availability of data, and general practicality constraints. The iDSI reference case served as a crucial principles-based framework to explore the suitability of the present analysis. Strategic choices were made on how to deliver evidence given the constraints, in a way that was still fit for policy makers’ purposes. This was done in two ways.
First, policymakers sought to conduct a rapid HTA to have 'proof of concept' for using HTA in decision-making. To conduct the analysis quickly, a topic was selected for which there were locally available cost data and supplemented by a pragmatic approach to collecting additional data as described in the limitations above. The implication of these choices naturally have impacts on the generalizability and potential bias of the analysis.
Second, the choice to exclude a 'no comparator' arm was made to reflect the local context. Dialysis is a hotly debated topic everywhere due to its high cost, and for ESRD, its limited effectiveness. From a purely economic perspective, some have argued that dialysis is an inefficient use of resources better spent elsewhere [38]. However, dialysis is a good illustration that priority-setting choices are not limited to cost-effectiveness. Dialysis is provided in many countries, including LMICs, on the grounds of financial risk protection and it being a moral imperative for universal health coverage [39]. The reality is that many LMICs have a shifting burden of disease, with existing coverage for dialysis services in LMICs being described as inadequate [40]. There is a real need to provide evidence to inform open debates about the optimal solution to providing dialysis.
Thus, the 'adaptive' choices in methodology made by the co-authors for this paper reflect a conscious effort to address policymaker needs in a deliberate departure from ‘gold standard’ HTA approaches. The pilot successfully raised awareness about HTA among key stakeholders, provided evidence for price negotiations, and identified key data needs that should be considered part of a strategy to support HTA development in the country [41, 42].
Conclusion
Our de novo model suggests that HD may be cost-effective from the payer perspective compared with PD, and significant cost savings may be achieved by reducing the costs of HD commodities. While the relative robustness of this economic evaluation was constrained by adopting an aHTA approach, it was nonetheless a useful policy tool for Rwandan policymakers as it helped build the foundation for evidence-based priority setting in the future.
Availability of data and materials
The datasets used and/or analysed during the study are not publicly available due to the analysis being completed under the permission of RSSB, but are available from the corresponding author, in consultation with RSSB on reasonable request.
Abbreviations
- aHTA:
-
Adaptive health technology assessment
- AKI:
-
Acute kidney injury
- CBHI:
-
Community-based health insurance
- CKD:
-
Chronic kidney disease
- ESRD:
-
End-stage renal disease
- GDP:
-
Gross domestic product
- HD:
-
Hemodialysis
- HTA:
-
Health technology assessment
- ICER:
-
Incremental cost-effectiveness ratio
- iDSI:
-
International decision support initiative
- LMIC:
-
Low- and middle-income country
- PD:
-
Peritoneal dialysis
- PSA:
-
Probabilistic sensitivity analysis
- QALY:
-
Quality-adjusted life year
- RMH:
-
Rwanda Military Hospital
- RSSB:
-
Rwanda Social Security Board
- RWF:
-
Rwandan franc
- US$:
-
United States dollar
References
MoH. Fourth Health Sector Strategic Plan. https://www.minecofin.gov.rw/index.php?eID=dumpFile&t=f&f=15856&token=7aabf4f0ec53ed2685b9bd0a1f9df78a60651a35
Umuhoza SM, Musange SF, Nyandwi A, Gatome-Munyua A, Mumararungu A, Hitimana R, et al. Strengths and weaknesses of strategic health purchasing for universal health coverage in Rwanda. Heal Syst Reform. 2022;8:2. https://doi.org/10.1080/23288604.2022.2061891.
RSSB. CBHI Scheme. 2024. https://www.rssb.rw/scheme/cbhi-scheme
Current health expenditure per capita (current US$) - Rwanda | Data. [cited 2022 Jan 7]. https://data.worldbank.org/indicator/SH.XPD.CHEX.PC.CD?locations=RW
O’Rourke B, Oortwijn W, Schuller T. The new definition of health technology assessment: A milestone in international collaboration. Vol. 36, International Journal of Technology Assessment in Health Care. Cambridge University Press; 2020. p. 187–90. https://doi.org/10.1017/S0266462320000215
Nemzoff C, Ruiz F, Chalkidou K, Mehndiratta A, Guinness L, Cluzeau F, et al. Adaptive health technology assessment to facilitate priority setting in low-income and middle-income countries. BMJ Glob Heal. 2021;6(4): e004549.
Teerawattananon Y, Dabak SV, Khoe LC, Bayani DBS, Isaranuwatchai W. To include or not include: renal dialysis policy in the era of universal health coverage. BMJ. 2020;1:368. https://doi.org/10.1136/bmj.m82.
Teerawattananon Y. To include or not include: renal dialysis policy in the era of universal health coverage. 2020;1:2018–20.
RSSB. Utilization and Expenditure Review of Dialysis For RSSB Patients. 2018.
World Economic Outlook Database: October 2021 [Internet]. [cited 2022 Jan 6]. Available from: https://www.imf.org/en/Publications/WEO/weo-database/2021/October
Teerawattananon Y, Luz A, Pilasant S, Tangsathitkulchai S, Chootipongchaivat S, Tritasavit N, et al. How to meet the demand for good quality renal dialysis as part of universal health coverage in resource-limited settings? Heal Res Policy Syst. 2016;14(1):1–8. https://doi.org/10.1186/s12961-016-0090-7.
Pike E, Hamidi V, Ringerike T, Wisloff T, Klemp M. More use of peritoneal dialysis gives significant savings: a systematic review and health economic decision model. J Clin Med Res. 2017;9(2):104–16.
Teerawattananon Y, Mugford M, Tangcharoensathien V. ford M, Tangcharoensathien V. Economic evaluation of palliative management versus peritoneal dialysis and hemodialysis for end-stage renal disease: Evidence for. Value Heal. 2007;10(1):61–72. https://doi.org/10.1111/j.1524-4733.2006.00145.x.
Afiatin A, Khoe LC, Kristin E, Masytoh LS, Herlinawaty E, Werayingyong P, et al. Economic evaluation of policy options for dialysis in end-stage renal disease patients under the universa. PLoS ONE. 2017;12(5):1–10.
Chang YT, Hwang JS, Hung SY, Tsai MS, Wu JL, Sung JM, et al. Cost-effectiveness of hemodialysis and peritoneal dialysis: A national cohort study with 14 years follow-up and matched for como. Sci Rep. 2016;6:1–12. https://doi.org/10.1038/srep30266.
Surendra NK, Manaf MRA, Hooi LS, Bavanandan S, Nor FSM, Khan SSF, et al. Cost utility analysis of end stage renal disease treatment in Ministry of Health dialysis centres, Malaysia: Hemodialysis versus continuous ambulatory peritoneal dialysis. PLoS ONE. 2019;14(10):1–16.
Remuzzi, Giuseppe, Horton R. Acute renal failure: an unacceptable death sentence globally. Lancet. 2013;382. http://www.theisn.org/isn-information/saving-young-lives-in-
Naicker S. End-stage renal disease in Sub-Saharan Africa. Kidney Int [Internet]. 2013 [cited 2020 Feb 25];3:161–3. http://www.kidney-international.org
Nsengiyumva V, Igiraneza G, Lameire N. Definition and epidemiology of acute kidney injury. Rwanda Med J. 2018;75(2):17–23.
Ashuntantang G, Osafo C, Olowu WA, Arogundade F, Niang A, Porter J, et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: a systematic review. Lancet Glob Heal. 2017;5(4):e408–17.
Igiraneza G, Ndayishimiye B, Nkeshimana M, Dusabejambo V, Ogbuagu O. Clinical Profile and Outcome of Patients with Acute Kidney Injury Requiring Hemodialysis: Two Years’ Experience at a Tertiary Hospital in Rwanda. Biomed Res Int. 2018;2018.
Igiraneza G, Dusabejambo V, Finklestein FO, Rastegar A. Challenges in the recognition and management of acute kidney injury by hospital. Kidney Int Reports. 2020. https://doi.org/10.1016/j.ekir.2020.04.003.
Liu L, Zhang L, Gj L, Fu P. Peritoneal dialysis for acute kidney injury ( Review ). Cochrane Database Syst Rev. 2017. https://doi.org/10.1002/14651858.CD011457.pub2/epdf/standard.
Nemzoff C, Anil Shah H, Heupink LF, Regan L, Ghosh S, Pincombe M, et al. Adaptive health technology assessment: a scoping review of methods. Value Heal. 2023.
Wilkinson T, Sculpher MJ, Claxton K, Revill P, Briggs A, Cairns JA, et al. The International Decision Support Initiative Reference Case for Economic Evaluation: An Aid to Thought. Value Health. 2016;19(8):921–8. http://linkinghub.elsevier.com/retrieve/pii/S1098301516304405
Consumer price index (2010 = 100) | Data. [cited 2020 May 14]. https://data.worldbank.org/indicator/fp.cpi.totl
The World Bank. World Development Indicators | Exchange rates and prices [Internet]. 2020 [cited 2020 May 13]. http://wdi.worldbank.org/table/4.16
Global Health Observatory Data Repository - Life Tables - Rwanda. WHO. 2016 [cited 2020 Mar 31]. https://apps.who.int/gho/data/view.main.61370?lang=en
Klarenbach S, Manns B, Pannu N, Clement FM, Wiebe N, Tonelli M. Economic evaluation of continuous renal replacement therapy in acute renal failure. Int J Technol Assess Health Care. 2009;25(3):331–8.
Garay OU, Palacios A, Pichon-Riviere A, Augustovski F, Martí SG, Hernández-Vásquez A, et al. The cost-effectiveness of continuous versus intermittent renal replacement therapies in acute kidney injury: perspective of the social services for the elderly in Argentina. Value Heal Reg Issues. 2018;2019(20):142–8.
Haacker M, Hallett TB, Atun R. On discount rates for economic evaluations in global health. [cited 2020 May 19]; https://academic.oup.com/heapol/article-abstract/35/1/107/5591528
Ochalek J, Lomas J, Claxton K. Estimating health opportunity costs in low-income and middle-income countries: a novel approach and evidence from cross-country data. BMJ Glob Heal. 2018;3(6): e000964.
Bertram MY, Lauer JA, De Joncheere K, Edejer T, Hutubessy R, Kieny MP, et al. Cost-effectiveness thresholds: pros and cons. Bull World Health Organ. 2016;94(12):925–30.
Chi Y-L, Blecher M, Chalkidou K, Culyer A, Claxton K, Edoka I, et al. What next after GDP-based cost-effectiveness thresholds? Gates Open Res. 2020;4:176. https://gatesopenresearch.org/articles/4-176/v1
Bilcke J, Beutels P. Generating, Presenting, and Interpreting Cost-Effectiveness Results in the Context of Uncertainty: A Tutorial for Deeper Knowledge and Better Practice. Med Decis Mak. 2022;42(4):421–35. https://journals-sagepub-com.ez.lshtm.ac.uk/doi/full/https://doi.org/10.1177/0272989X211045070
Drummond M, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Fourth. (Firm) P, editor. 2015.
Singh A, Hussain S, Kher V, Palmer AJ, Jose M, Antony B. A systematic review of cost-effectiveness analyses of continuous versus intermittent renal replacement therapy in acute kidney injury. Expert Rev Pharmacoecon Outcomes Res. 2022;22(1):27–35. https://www.tandfonline.com/doi/abs/https://doi.org/10.1080/14737167.2021.1916471
Crosby L, Baker P, Hangoma P, Barasa E, Hamidi V, Chalkidou K. Dialysis in Africa: the need for evidence-informed decision making. Vol. 8, The Lancet Global Health. Elsevier Ltd; 2020 [cited 2020 Jun 25]. p. e476–7. http://www.thelancet.com/article/S2214109X20300589/fulltext
Luyckx VA, Moosa MR. Priority Setting as an Ethical Imperative in Managing Global Dialysis Access and Improving Kidney Care. Semin Nephrol. 2021;41(3):230–41. http://www.seminarsinnephrology.org/article/S0270929521000747/fulltext
Teerawattananon Y, Tungsanga K, Hakiba S, Dabak S. Dispelling the myths of providing dialysis in low- and middle-income countries. Nat Rev Nephrol 2020 171. 2020;17(1):11–2. https://www.nature.com/articles/s41581-020-00346-7
Hollingworth S, Downey L, Ruiz F, Odame E, Dsane-Selby L, Gyansa-Lutterrodt M, et al. What do we need to know? Data sources to support evidence-based decisions using health technology assessment in Ghana. Heal Res Policy Syst. 2020.
Downey L, Rao N, Guinness L, Asaria M, Prinja S, Sinha A, et al. Identification of publicly available data sources to inform the conduct of Health Technology Assessment in India [version 2; referees: 2 approved, 1 approved with reservations]. F1000 Res. 2018;7:1–18.
Acknowledgements
The authors are grateful to all the stakeholders involved in this study, including RSSB, the MoH, and the School of Public Health, for their engagement at each step in the HTA process. In particular, the authors would like to thank nephrologists Dr. Joseph Ntarindwa, Dr. Kabahizi Jules, and Dr. Rugamba Gilbert; Dr. Regis Hitimana from the University of Rwanda School of Public Health; the entire team at the Clinton Health Access Initiative including Diana Kizza, Maelle Barbancon, and Natasha Salant; and Pete Baker from the Center for Global Development. Additionally, the team would like to thank Dr. Nick Pritchard, the director of nephrology at Addenbrooke’s Hospital in Cambridge, UK, for providing expert opinion into the care pathway and available research on dialysis used to inform the model.
Funding
This analysis was supported by the international Decision Support Initiative with funding from the UK Department for International Development and the Swedish International Development Agency.
Author information
Authors and Affiliations
Contributions
CN, NA, SH, AR, KC, and FR conceptualized and designed the work. CN, NA, TO, GI, IK, SC, AR, and MR acquired data and/or conducted analysis. CN, NA, KC, and FR interpreted the data. CN wrote the first draft of the paper, and all authors provided inputs and feedback for revision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the London School of Hygiene and Tropical Medicine’s ethics committee, reference number 28265, and the Rwanda National Ethics Committee, IRB00001497. RSSB approved this study, and no incentives were given to any individuals who participated in this analysis. ‘Personal communication’ data inputs were sourced solely from co-authors on this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1.
See Fig. 3.
Appendix 2: Data collection
To drive the search strategy, the team developed an initial high level data summary with needs and potential sources for the HTA—as presented in Table 6 below—and shared it with key policy makers.
-
1.
The HTA developers reviewed an already completed iDSI review on dialysis requested by RSSB in early 2019 which summarized the available evidence on the costs and cost-effectiveness of dialysis for AKI patients with a focus on SSA and specifically, Rwanda.
-
2.
Four local nephrologists and one international nephrologist expert on dialysis were identified. Consultation with these experts helped to unearth additional published and unpublished studies on clinical effectiveness and financing/costing studies in the field of dialysis of which experts had knowledge. These consultations also informed the structure of the model by clarifying the care pathway for patients with AKI.
-
3.
Where there were data missing, the team drew on the iDSI network to source reliable dialysis models and studies. This included models and studies from Thailand’s Health Intervention and Technology Assessment Program (HITAP), a core partner of iDSI, which has led important dialysis studies in Southeast Asia and are known to represent a reliable source of information to support this model development.
-
4.
A simple literature search strategy supplemented the above information. It was designed and used to search two electronic databases: EMBASE (Ovid) and PubMed (Ovid). This simple search strategy combined terms for the interventions or comparators of interest with terms for the target condition (dialysis for AKI) as well as terms for CKD as it was not the target condition, but the authors expected it to be better studied than AKI. It was also focused on available studies in Sub-Saharan and/or East Africa, to establish whether there are more locally relevant studies than those sourced through the above methods.
Full details of the terms used in the literature search are presented below in Table 7.
-
Past 10 years only
-
No limits applied for study design or language
Appendix 3: Cost summary and breakdown
This appendix provides a detailed overview of costs included in each cost component and how they were calculated. All costs are expressed per patient and have been adjusted to 2022 RWF and current US dollars using the consumer price index (CPI) method (where adjusted costs = base year costs x (2022 CPI/base year CPI)), and the 2022 exchange rate US$ 1: RWF 1031
The Table 8 below provides an overview of costs which have been included in base case modelling, as well as the scenario
Direct medical costs
Direct medical costs for PD included the cost of a PD catheter, catheter insertion, anesthesia, drugs, consumables, labs, dialysate, and palliative care. These figures were provided by RSSB as a supplement to the RSSB 2018 dialysis costing study; lab costs for PD and HD were assumed to be equivalent. Direct medical costs for HD included drugs, HD catheter, HD kit, laboratory tests, other acts/procedures (catheter insertion, IV injection, medical fee, and wound dressing), other consumables not specific to the dialysis kit, and other laboratory tests (those not done by all facilities). These figures were sourced directly from the RSSB 2018 dialysis costing study. Both interventions were presented in that study as a session cost for a ‘new’ case and a session cost for ‘old’ cases. For each, we summed the cost of the initial ‘new’ session plus a ‘per session’ cost for the remaining 17 sessions modelled (and in scenario analysis, the remaining four sessions). The per patient direct medical unit cost for HD was calculated using a straight line average of the total direct medical costs for provision across the four facilities where HD is delivered to CBHI patients (King Faisal Hospital (KFH), Rwanda Military Hospital (RMH), The University Teaching Hospital of Kigali (CHUK), and The University Teaching Hospital of Butare (CHUB)), while the cost for PD was sourced from the only hospital which provides PD services, KFH
Direct non-medical costs
Both PD and HD incurred additional direct costs from salaries and overheads. Annual salary costs were calculated using a combination of staffing needs estimated by local experts and co-authors and salaries drawn from the 2019 Rwanda Health Labor Force Survey (which reported salaries in 2016 RWF). Staffing needs for PD and HD are summarized in Table 9 below. At CHUK, we assumed that 100% of each staff is allocated to HD services and used 2017–2018 patient volumes to calculate a unit cost per patient for staff. Then, due to uncertainty about staffing of PD services, we use the proportionate total cost of PD:HD services (74%) multiplied by the unit cost for HD services to estimate the unit cost for PD services (Table 9). Overheads were assumed to be 30% of total annual operating costs (staff + overheads)
Appendix 4.
See Fig. 4
Appendix 5.
See Table 10.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nemzoff, C., Ahmed, N., Olufiranye, T. et al. Rapid cost-effectiveness analysis: hemodialysis versus peritoneal dialysis for patients with acute kidney injury in Rwanda. Cost Eff Resour Alloc 22, 35 (2024). https://doi.org/10.1186/s12962-024-00545-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-024-00545-0