Abstract
Introduction
Chronic kidney disease (CKD) is a progressive disease of growing prevalence, posing serious concerns for global public health. While the economic burden of CKD is substantial, data on the cost of CKD is limited, despite growing pressures on healthcare systems. In this review, we summarise the available evidence in 31 countries and regions and compile a library of costing methodology and estimates of CKD management and disease-associated complications across 31 countries/regions within the Inside CKD programme.
Methods
We collected country/region-specific CKD costs via a pragmatic rapid literature review of local literature and engagement with local experts. We extracted cost data and definitions from identified sources for CKD stages G3a–5, kidney failure with replacement therapy by modality, covering haemodialysis, peritoneal dialysis, and kidney transplants, and disease-associated complications in local currency, converted to United States dollars (USD) and inflated to 2022.
Results
Annual direct costs associated with CKD management rose by an average factor of 4 in each country/region upon progression from stage G3a to G5. Mean annual costs per patient increased considerably more from early stages versus dialysis (stage G3a, mean: $3060 versus haemodialysis, mean: $57,334; peritoneal dialysis, mean: $49,490); with estimates for annual costs of transplant also substantially higher (incident: $75,326; subsequent: $16,672). The mean annual per patient costs of complications were $18,294 for myocardial infarction, $8463 for heart failure, $10,168 for stroke and $5975 for acute kidney injury. Costing definitions varied widely in granularity and/or definition across all countries/regions.
Conclusion
Globally, CKD carries a significant economic burden, which increases substantially with increasing disease severity. We identified significant gaps in published costs and inconsistent costing definitions. Cost-effective interventions that target primary prevention and disease progression are essential to reduce CKD burden. Our results can be used to guide cost collection and facilitate better comparisons across countries/regions to inform healthcare policy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Chronic kidney disease (CKD) is a progressive disease of considerable burden to healthcare systems worldwide; later stages of CKD in particular carry a significant burden, and, with the growing prevalence of the condition, there is a need to project healthcare burdens to forecast future needs. |
Inside CKD is a research programme designed to project the burden of CKD and to assess the impact of policy interventions at a population level using a validated microsimulation model. Here, we report the derivation of a multinational cost data library of patient-level direct costs for CKD and associated complications specific to 31 countries and regions. |
The average annual direct costs per patient increased considerably with progression of CKD severity across all settings, particularly on reaching kidney failure, and subsequent enrolment on kidney replacement therapy. |
This study highlights the need to tackle CKD in the early stages of disease to avoid progression to more advanced stages, where the economic burden of disease increases considerably. |
This article documents the development of a comprehensive global library of cost data, and highlights significant divergence in costing methodology and/or poor data availability for published costs in several countries/regions despite the substantial economic burden of CKD. |
Introduction
Chronic kidney disease (CKD) is a serious progressive condition estimated to affect approximately 700–840 million people, with worldwide prevalence estimated at 8–14% [1,2,3]. CKD is the third fastest growing cause of death worldwide, with aging populations and the rise of common CKD risk factors such as type 2 diabetes mellitus and hypertension [1, 4]. Guidelines from Kidney Disease: Improving Global Outcomes (KDIGO) stratify CKD according to glomerular filtration rate (GFR, G1–G5) and urine albumin to creatinine ratio (UACR), with GFR stage G5 being the most severe stage, indicative of kidney failure [5, 6].
Patients in stages G1 and G2 are often asymptomatic [7], and studies have shown that up to 93% of patients with evidence of CKD stage G3 are unaware of their clinical status [8]. This delays access to interventions that could slow down or prevent disease progression. Approximately half of patients with CKD stage G3 are expected to progress to more advanced disease within 10 years [9]. There are substantial differences in disease burden between earlier and later stages of CKD, with patients experiencing significant reductions in health-related quality of life and life expectancy on progression to kidney failure [10, 11].
CKD is also associated with a substantial economic burden worldwide, particularly upon reaching kidney failure, due to the need for resource intensive kidney replacement therapy (KRT)—comprised of either dialysis or kidney transplantation—imposing both significantly high healthcare costs and major societal burden [12, 13]. Furthermore, patients with advanced CKD experience a higher risk of cardiovascular diseases, including stroke, myocardial infarction, and heart failure, leading to further healthcare resource utilisation and economic burden [14, 15].
Despite the well-recognised significance of preventing kidney function decline, approximately half of the countries included in the Global Kidney Health Atlas do not have management guidelines or strategies for improving the care of patients with CKD [16]. With the growing prevalence of CKD and the unmet need for improved CKD management, effective strategies are needed to guide decision-makers in the healthcare sector. As part of evidence-based policy decisions, economic evaluations are invaluable tools for enabling national healthcare systems to assess present and future demands for resource use and healthcare service delivery.
The Inside CKD research programme aims to project the epidemiological, clinical, and economic burdens of CKD at a population level, and to assess the impact of policy interventions on this burden using patient-level microsimulation-based modelling. In this article, we describe the generation of a global CKD cost library via a series of pragmatic literature reviews for management of CKD and associated complications in 31 countries or regions.
Methods
Study Design
Detailed methods for the broader Inside CKD programme have been published previously [17]. In this article, we describe the derivation of a library of patient-level cost data to characterise the global burden of disease and to parameterise the Inside CKD model with health economic inputs for modelling analyses across 31 countries or regions (Fig. 1).
To identify the most accurate available estimates of costs associated with CKD, we worked with local research organisations to conduct pragmatic literature searches of cost data published in 31 countries and regions available in English or local languages. Given the anticipated paucity of available data across most settings, no restrictions were placed upon the date of publications and/or the date of cost estimate. If multiple sources existed, the most appropriate source was selected according to recency, robustness of methodology, and closest alignment to the required parameters/population for the microsimulation model. All cost data were validated by local clinical experts in conjunction with the Inside CKD scientific steering committee (Table S1) [17].
Where pragmatic literature searches could not identify the necessary cost estimates/sources, we consulted local experts for each country or region to address data availability issues. If no country-/region-specific sources were available, a suitable proxy country/region was selected to provide the necessary parameters for health economic inputs.
The selection of appropriate proxies was defined according to a multi-dimensional algorithm that accounted for relatability of economy and epidemiology. Briefly, three key indicators were assessed using the World Bank Data repository (Table 1) [18,19,20]. A list of proxy countries/regions for each setting was created based on having similar values to the index country for all three selected indicators, and proxies were selected based on relative similarity versus other settings. If data were not available for a proxy selected through this method, then a country that is close to the target country of interest was selected. This was supplemented by advice from external experts in relation to verifying proxy data and suggesting alternatives to the proxies selected using this method if necessary.
Inclusion Criteria
The model required country-/region-specific inputs for annual direct costs only. Estimates associated with GFR-defined CKD stages (G3a–G5) that would typically include costs pertaining to routine disease management costs were considered. Costs for stages G1 and G2 were not included as they were assumed to be negligible. Annual cost inputs for health states defined by dialysis (haemodialysis, peritoneal dialysis) or kidney transplantation (year of incidence and of the succeeding year onwards) were also identified, which would include direct costs associated with the cost of delivering KRT. No indirect costs were included in the model owing to a paucity of data. Costs associated with complications resulting from CKD progression—cardiovascular complications (myocardial infarction, stroke, and heart failure) and acute kidney injury—were extracted and presented separately [17].
Data Extraction
Direct medical care-related cost inputs were extracted from the identified data sources in the published currency. Cost estimates were inflated to 2022 prices according to the gross domestic product deflator data from the International Monetary Fund [21]. If necessary, inflated values were normalised to the native currency for each country/region by accounting for purchasing power parity (PPP), also according to data from the International Monetary Fund [22]. The inflated values were also converted to United States dollars (USD) to facilitate comparisons across countries and regions, accounting for PPP in conversion to USD to best capture expenditure as a function of health spending per capita; conversion rates to USD are detailed in the supplementary materials (Table S2). PPP considers the conversion rate that would need to be applied to the currency of one country in order to buy the same amount of goods and services in another country, and therefore implied PPP rates may differ substantially from market exchange rates.
We extracted information on the measurement and valuation of cost estimates, including the source type (categorised as published literature, healthcare databases, other electronic articles, expert opinion or proxy) and any provided definition of cost estimates within the source material. For the USA, cost estimates were also extracted dependent on payer type (Medicare and commercial).
Analysis
Mean and median values were compared across countries/regions and disease stages; the definitions, recency and type of cost sources were descriptively analysed. Median and interquartile ranges (IQR) are also graphically presented in boxplots.
Compliance with Ethics Guidelines
This study was conducted in accordance with ethical principles of the Declaration of Helsinki and Good Clinical Practice guidelines. This article is a review and does not contain any new studies with human participants or animals performed by any of the authors. Any data used for the purpose of the present study were anonymised.
Results
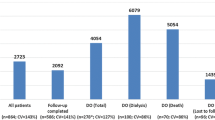
Of the 31 countries or regions included in the study, only 9 countries/regions had available sources for all cost parameters, and a further 7 countries/regions used proxy sources for five or more parameters. Annual disease management costs stratified by GFR-defined CKD stages (G3a–G5) were typically the most poorly reported, with 12 countries/regions lacking sufficient data to parameterise all four health states. Six countries/regions lacked available local sources for at least one of the annual costs defined by KRT modality for patients with kidney failure, specifically haemodialysis (n = 2), peritoneal dialysis (n = 2), transplant (n = 3) and transplant maintenance (n = 6). Data availability for CKD-related complications were variable. Annual estimates for the management of myocardial infarction were unavailable for 11 countries/regions, and costs for the management of heart failure were unavailable in 9. Seven countries/regions did not have estimates for acute kidney injury, and five countries/regions did not have available cost data for stroke.
Mean and median (IQR) values for cost estimates across all settings are provided in Table 2. Boxplots for health states and complications across all countries/regions are presented in Fig. 2.
Median standardised per patient CKD costs, per annum for (a) CKD health state, (b) complication. Upper and lower bars indicate minimum and maximum values; the line between light and dark blue boxes indicates the median value; the borders of the dark and light blue boxes indicate the interquartile range. Costs are calculated using country specific PPP conversion rates, listed in Table S2. PPP purchasing power parity, CKD chronic kidney disease, GFR glomerular filtration rate
Medical Costs for Patients with CKD by KDIGO GFR Stage
Per patient disease management costs by GFR stage and country or region, standardised to 2022 US dollars and accounting for PPP, are presented in Fig. 3, with mean annual costs across all countries and regions of $3060, $3544, $5332 and $8736 for stages G3a, G3b, G4 and G5, respectively (Table 2). Median annual costs per patient by CKD stage were $2214 for stage G3a (lowest $38 Poland; highest $13,124 USA, commercial), $2674 for stage 3b (lowest $152 Poland; highest $15,514 USA, commercial), $5797 for stage 4 (lowest $305 Poland; highest $18,270 USA, commercial) and $8227 for stage 5 not on KRT (lowest $343 Poland; highest $20,603 Canada). The costs of CKD increased on average by a factor of 4 from stage G3a to G5 across countries/regions (min: 1.27, USA Medicare; max: 11.0, Philippines). Costs by CKD stage are presented in local currency (2022 values) in Table S3.
Country-/region-specific annual per patient CKD management costs by KDIGO GFR stage. Costs are calculated using country-specific PPP conversion rates, listed in Table S2. PPP purchasing power parity, CKD chronic kidney disease, KDIGO Kidney Disease Improving Global Outcomes, GFR glomerular filtration rate
Costing data for the four stages were estimated from a single source for 27 countries/regions. For four countries/regions (Philippines, Singapore, Spain and Thailand), costing data was drawn from two sources for different stages. Notably, annual CKD stage costs for both commercial and Medicare patients in the USA were defined from one source.
The sources for identified CKD stage cost data were most commonly published literature or proxy sources, with 13 countries/regions parameterised using local published estimates and 12 countries/regions used estimates from proxy sources. Other sources for this data included electronic healthcare database analyses in six countries, and expert opinion for one country (Turkey). Excluding proxy sources and those derived from expert elicitation, most estimates were published within the past decade, with only two sources reporting estimates for cost years prior to 2012, both for Spain.
If reported, most extracted cost definitions included costs related to outpatient care and medication. Cost definitions could also include diagnostics/screening, complication management and procedural costs. Some estimates also incorporated inpatient care costs and could include emergency visits, while others specifically excluded hospitalisation costs. The granularity of cost definitions varied widely.
Medical Costs for Patients with Kidney Failure on KRT
Standardised annual per patient KRT costs per country/region, standardised to 2022 US dollars and accounting for PPP, are shown in Fig. 4. Mean annual costs were $57,334 for haemodialysis, $49,490 for peritoneal dialysis, $75,326 for the first year following a kidney transplant and $16,672 for transplant maintenance costs after the first year. The median costs by KRT modality across all included countries and regions were $49,926 for haemodialysis (lowest $5183 India; highest $136,597 Netherlands), $42,990 for peritoneal dialysis (lowest $5183 India; highest $125,449 Netherlands), $64,638 for year 1 following a kidney transplant (lowest $11,707 Taiwan; highest $158,486 Israel and Germany) and $14,095 for subsequent years of kidney transplant maintenance (lowest $3361 Romania; highest $49,603 USA). Local costs (2022 values) by KRT modality are presented in Table S4.
The annual treatment costs of haemodialysis (mean: $57,334; median: $49,926) and peritoneal dialysis (mean: $49,490 median: $42,990) were considerably greater than for patients without kidney failure, with costs many times higher than typical costs for patients with stage 3a CKD (mean: $3060; median: $2214). The treatment cost of the incident year of a kidney transplant was particularly high (mean: $75,326; median: $64,638), before dropping substantially in subsequent years (mean: $16,672; median: $14,095). Nevertheless, the maintenance costs post-transplant remained higher compared with patients with kidney failure who had not yet initiated KRT (mean: $8736; median: $8227).
Two countries/regions had no region-specific data available for any of the KRT costs investigated in this study (Israel and Saudi Arabia), while a further three countries/regions had missing data for at least one of the KRT-related costs.
In contrast to annual CKD stage-specific costs, separate sources are commonly used for KRT modalities for each country or region. Excluding proxy estimates, most of the estimates were derived from published literature (n = 67), while others were typically sourced from governmental or healthcare sources or inpatient claims databases (n = 27), with a relatively small number of estimates derived from other electronic articles (n = 9) or expert opinion (n = 8).
Excluding values derived from expert opinion and proxy settings, most costs were derived from source estimates from the year 2012 or later (n = 78), with 25 estimates derived from source costs from earlier than 2012.
The relative detail of definitions from which KRT cost estimates were derived were variable. Costs associated with patients on dialysis typically consisted of costs relating specifically to dialysis procedures, and could often include medications and outpatient costs. Transportation costs were sometimes included, as were inpatient costs, procedures and tests. Costs associated with the first year of transplant, in addition to the procedural cost of transplant, could also include hospitalisations, outpatient care and medication. A higher proportion of estimates had no definition for maintenance of kidney transplants in subsequent years, but otherwise consisted most commonly of outpatient and medication costs.
Medical Costs for Cardiovascular Complications and Acute Kidney Injury in Patients with CKD
Annual per patient costs for cardiovascular complications and acute kidney injury, standardised to 2022 US dollars and accounting for PPP, are shown in Fig. 5. The mean annual costs were $18,294 for myocardial infarction, $8463 for heart failure, $10,168 for stroke, and $5975 for acute kidney injury. The median annual costs per patient for cardiovascular complications related to CKD across all included countries and regions were $13,928 (lowest $1005 Taiwan; highest $90,051 Colombia and Mexico) for myocardial infarction, $8633 (lowest $158 Hungary; highest $24,930 USA) for heart failure, $8579 (lowest $694 Brazil; highest $26,766 France) for stroke, and $4568 (lowest $219 Japan; highest $37,587 Belgium) for acute kidney injury. Medical cost estimates for cardiovascular complications and acute kidney injury costs in local currency units (2022 values) are presented in Table S5.
Most of the identified sources were published literature (myocardial infarction: 16; heart failure: 18; stroke: 22; acute kidney injury: 9), except for acute kidney injury for which most estimates were derived from healthcare databases (n = 15). Those without available local data were sourced from published estimates from proxy sources (myocardial infarction: 11; heart failure: 9; stroke: 5; acute kidney injury: 6). No country/region lacked data for all estimates, but six lacked available estimates for three out of four complications.
Excluding proxy sources and estimates derived from expert elicitation, most estimates were published in or after 2012, but 12 sources were older (myocardial infarction: 5; heart failure: 1; stroke: 5; acute kidney injury: 1).
Most extracted cost definitions for cardiovascular complications included components that related to inpatient care resulting from the events. However, the granularity of these definitions varied substantially and could also commonly include medication and outpatient costs, while testing and transportation costs were less frequent. Definitions for acute kidney injury were typically either assigned hospitalisation costs specifically relating to acute kidney injury (typically from diagnosis-related group sources) or costs per minor hospitalisation event if a precise estimation was unavailable.
Discussion
In this article, we have documented the development of an international cost data library of annual medical costs for patients with CKD, in addition to the costs for major complications associated with CKD in 31 countries and regions as part of the Inside CKD global burden of disease programme. Through pragmatic literature searching and engagement with local experts, this study has compiled country-/region-specific health state costs, dependent on CKD stage and KRT modality, and clinical event-related costs. This library enables the parameterisation of economic evaluations to determine the burden of CKD and to evaluate new disease management strategies and their influence on national healthcare expenditure.
CKD progression dramatically increased disease management costs across the identified sources in most countries/regions. The cost for stage G3a CKD across all countries and regions considered in the Inside CKD research programme increased on average by 4 times on progressing to stage G5. Furthermore, as many patients will initiate KRT upon reaching stage G5, most commonly via dialysis, these costs will increase even further. The highest average cost across all CKD stages and KRT modalities was observed for the procedural year of kidney transplantation, which is estimated at a mean cost of $75,326 annually per patient across all investigated geographies. Notably, the annual per patient costs post-transplant ($16,672) remain considerably higher than the costs associated with stage G5. Thus, upon reaching kidney failure requiring KRT, annual per patient costs increase permanently and substantially, even after transplant. Proactive strategies to slow progression therefore have the potential to substantially reduce the considerable rising economic burden of advancing stages of CKD.
The reported annual per patient costs of CKD are substantial when compared to other high-burden diseases. Notably, the direct per patient medical costs associated with type 2 diabetes mellitus in the US have been reported to average, as a median value, between $1700 and $2100 [23]. For chronic obstructive pulmonary disorder, the direct per patient medical costs in the US have been reported to average, as a mean, $3943 [24]. The mean cost in the USA of patients in CKD stage 3a in this study was $3060, and $11,908 or $13,124 for Medicare and commercial settings, respectively. Importantly, CKD costs can still be substantial at a relatively early stage of CKD, and rise further upon kidney failure. Accordingly, while patients on dialysis only comprise approximately 0.15% of the global population, they are typically the subject of 2–4% of national health care budget expenditure [13].
As the scope of this review extended to countries and regions across the income spectrum, our study provides a concise overview of the availability of disease management costs to inform the development of global CKD policy. The cost library can support the Partnership for Health System Sustainability objective to “improve global health by providing qualitative and quantitative evidence to inform policy, and promote action at national and international levels to strengthen health system sustainability and resilience” [25].
While previous studies have been typically limited to specific cost types and countries/regions [26,27,28], our review considered a more comprehensive set of costs related to CKD management and disease-associated complications across 31 countries and regions. This global scope provides a broad overview of CKD costs, highlighting the vast differences across settings. To achieve this task, experts from each country/region and local research organisations were consulted to supplement our searches of publicly available sources to confirm that the best available data could be incorporated.
This review is also subject to limitations. First, data availability was a significant issue in the generation of the CKD cost library, as evidenced by the necessity of proxy countries/regions and expert opinion, despite the high prevalence and associated cost of illness of CKD globally. Different sources of data may use differing sample sizes or study types, with varying inherent confounders within each study. Because of the differences in available data, assessing how representative estimated costs are of the true costs to each country is problematic. When estimates were available, cost definitions detailing the components included could not be identified for several countries and regions. Even when detailed specification of cost estimates were available, the components that contributed to CKD-specific medical costs were variable, but could include clinic visits in primary and/or secondary care, treatment costs, inpatient care associated with CKD co-morbidities, healthcare staff costs, patient transportation and rehabilitation. Further, differences in data collection methods (e.g., administrative vs. patient reported), or the financing and policy of healthcare systems or GDP per capita in each country/region, may also differ between countries. This may contribute to the significant differences in CKD costs and definitions noted across countries and regions: for example, total costs across CKD stage 5 ranged from $343 in Poland to $20,603 in Canada. As such, it is important to note that accurately comparing CKD costs between countries and regions is difficult due to numerous differences in costing methodologies, and to the granularity of reporting and payer systems. Given this inherent limitation of the available evidence, we considered that costing methodology provided additional context, where reported, of the derived estimates regarding the limitations of translation of local unit costs in CKD.
Publicly available costs were used to compile the cost library; however, this may not reflect actual costs paid by healthcare systems. The scope of this study excluded indirect costs, which are known to be significant in CKD [29, 30], in part due to the poorer availability of data in published literature versus direct costs. Relatively few countries have accurate national registries of ESKD and KRT, and limited data are available for earlier stages of CKD. In addition, the incidence and prevalence of ESKD per million population varies widely between countries [31], as does the provision of treatments. This may be linked in part to cultural issues: for example, in Japan, maintenance haemodialysis is the preferred treatment, with deceased donor kidney transplantation not usually considered [32]. Societal differences may also have an effect with some healthcare systems, placing greater emphasis on optimising the provision of kidney transplantation, leading to higher rates of transplantation [33]. The economic performance of a country may also contribute to differences in treatment, with higher income countries better able to afford expensive modes of care associated with ESKD.
Conclusion
The economic burden associated with CKD is significant and increases dramatically with disease progression. Implementing cost-effective management strategies targeting early detection and disease progression that consider local context and resources is essential to reduce the global burden of CKD. The compilation of the international CKD cost library provides a comprehensive overview of CKD costing studies on a global scale to help inform CKD healthcare policy decision-making.
References
Hill NR, Fatoba ST, Oke JL, et al. Global prevalence of chronic kidney disease—a systematic review and meta-analysis. PLoS ONE. 2016;11(7): e0158765.
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl. 2022;12(1):7–11.
Lv JC, Zhang LX. Prevalence and disease burden of chronic kidney disease. Adv Exp Med Biol. 2019;1165:3–15.
Cockwell P, Fisher L-A. The global burden of chronic kidney disease. Lancet. 2020;395(10225):662–4.
Levey AS, de Jong PE, Coresh J, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011;80(1):17–28.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2009;113:S1–130.
Hirst JA, Hill N, O’Callaghan CA, et al. Prevalence of chronic kidney disease in the community using data from OxRen: a UK population-based cohort study. Br J Gen Pract. 2020;70(693):e285–93.
Abdul Sultan A, Wittbrodt E, Malvolti E, et al. POS-300 Patient-reported early stage chronic kidney disease. Kidney Int Rep. 2021;6(4):S129.
Baek SD, Baek CH, Kim JS, et al. Does stage III chronic kidney disease always progress to end-stage renal disease? A ten-year follow-up study. Scand J Urol Nephrol. 2012;46(3):232–8.
Pagels AA, Söderkvist BK, Medin C, et al. Health-related quality of life in different stages of chronic kidney disease and at initiation of dialysis treatment. Health Qual Life Outcomes. 2012;10:71.
United States Renal Data System. Annual Data Report: Epidemiology of kidney disease in the United States. 2022 Available at: https://adr.usrds.org/2022 [Accessed 01/07/2022].
Elshahat S, Cockwell P, Maxwell AP, et al. The impact of chronic kidney disease on developed countries from a health economics perspective: A systematic scoping review. PLoS ONE. 2020;15(3): e0230512.
Vanholder R, Annemans L, Brown E, et al. Reducing the costs of chronic kidney disease while delivering quality health care: a call to action. Nat Rev Nephrol. 2017;13(7):393–409.
Darlington O, Dickerson C, Evans M, et al. Costs and healthcare resource use associated with risk of cardiovascular morbidity in patients with chronic kidney disease: Evidence from a systematic literature review. Adv Ther. 2021;38(2):994–1010.
Sarnak MJ, Levey AS, Schoolwerth AC, et al. Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Hypertension. 2003;42(5):1050–65.
Bello AK, Okpechi IG, Levin A, et al. ISN–Global Kidney Health Atlas: A report by the International Society of Nephrology: An Assessment of Global Kidney Health Care Status focussing on Capacity, Availability, Accessibility. Affordability and Outcomes of Kidney Disease: International Society of Nephrology; 2023.
Tangri N, Chadban S, Cabrera C, et al. Projecting the epidemiological and economic impact of chronic kidney disease using patient-level microsimulation modelling: Rationale and methods of Inside CKD. Adv Ther. 2023;40(1):265–81.
The World Bank. Domestic private health expenditure (% of current health expenditure). 2021. Available at: https://data.worldbank.org/indicator/SH.XPD.PVTD.CH.ZS [Accessed 01/06/2021].
The World Bank. Current health expenditure per capita, PPP (current international $). 2021. Available at: https://data.worldbank.org/indicator/SH.XPD.CHEX.PP.CD [Accessed 01/06/2021].
The World Bank. UHC service coverage index. 2021. Available at: https://data.worldbank.org/indicator/SH.UHC.SRVS.CV.XD [Accessed 01/06/2022].
International Monetary Fund. World Economic Outlook Database. 2022. Available at: https://www.imf.org/en/Publications/WEO/weo-database/2022/October [Accessed 01/11/2022].
International Monetary Fund. World Economic Outlook Report. 2022. Available at: https://www.imf.org/en/Publications/WEO/Issues/2022/10/11/world-economic-outlook-october-2022 [Accessed 27/02/2023].
Brandle M, Zhou H, Smith BRK, et al. The direct medical cost of type 2 diabetes. Diabetes Care. 2003;26(8):2300–4.
Dalal AA, Christensen L, Liu F, et al. Direct costs of chronic obstructive pulmonary disease among managed care patients. Int J Chron Obstruct Pulmon Dis. 2010;5:341–9.
World Economic Forum. Partnership for Health System Sustainability and Resilience. 2022. Available at: https://www.weforum.org/phssr [Accessed 24/03/2022].
Honeycutt AA, Segel JE, Zhuo X, et al. Medical costs of CKD in the medicare population. J Am Soc Nephrol. 2013;24(9):1478–83.
Gandjour A, Armsen W, Wehmeyer W, et al. Costs of patients with chronic kidney disease in Germany. PLoS ONE. 2020;15(4): e0231375.
Darbà J, Marsà A. Chronic kidney disease in Spain: analysis of patient characteristics, incidence and direct medical costs (2011–2017). J Med Econ. 2020;23(12):1623–9.
Michalopoulos SN, Gauthier-Loiselle M, Aigbogun MS, et al. Patient and care partner burden in CKD patients with and without anemia: a US-based survey. Kidney Med. 2022;4(4): 100439.
Kirkeskov L, Carlsen RK, Lund T, et al. Employment of patients with kidney failure treated with dialysis or kidney transplantation—a systematic review and meta-analysis. BMC Nephrol. 2021;22(1):348.
United States Renal Data System. Annual Data Report: International Comparisons. 2022. Available at: https://usrds-adr.niddk.nih.gov/2022/end-stage-renal-disease/11-international-comparisons. Accessed 16/06/2023.
Aikawa A. Current status and future aspects of kidney transplantation in Japan. Renal Replacement Ther. 2018;4(1):50.
Mudiayi D, Shojai S, Okpechi I, et al. Global estimates of capacity for kidney transplantation in world countries and regions. Transplantation. 2022;106(6):1113–22.
Acknowledgements
Funding
Inside CKD is funded by AstraZeneca. Inside CKD is a project based on microsimulation data and so no drugs were supplied or funded. All statistical analyses were funded by AstraZeneca and conducted by HealthLumen. The corresponding author had full access to all data and had final responsibility for the decision to submit for publication. AstraZeneca also funded the journal’s Rapid Service and Open Access fees.
Medical Writing, Editorial, and Other Assistance
The authors would like to thank all participants in the Inside CKD study programme and members of the Scientific Steering Committee (see Table S1 in the supplementary material). The authors thank Peter Gabb and Carla De Villiers of Health Economics and Outcomes Research Ltd. for providing medical writing support/editorial support, which was funded by AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Author Contributions
Lise Retat and Juan Jose Garcia Sanchez conceptualised and designed the study. Lise Retat and Joshua Card-Gowers were responsible for data analysis. Vivekanand Jha, Saeed M.G. Al-Ghamdi, Guisen Li, Mai-Szu Wu, Panagiotis Stafylas, Lise Retat, Joshua Card-Gowers, Salvatore Barone, Claudia Cabrera, Juan Jose Garcia Sanchez contributed to interpretation of the results, preparation and review of the manuscript, as well as approval of the final manuscript for publication.
Disclosures
Lise Retat and Joshua Card Gowers are employees of HealthLumen Limited. HealthLumen Limited received funding from AstraZeneca for the conduction of this study. Vivekanand Jha has received fees from AstraZeneca, NephroPlus and Zydus Cadilla, and grants from Baxters Health care, Biocon and GlaxoSmithKline; all funds are paid to his organisation. Saeed M.G. Al-Ghamdi has received speaker honoraria from Astellas, Vifor Pharma and AstraZeneca. Guisen Li has no conflicts of interest to declare. Mai-Szu Wu has received speaker honoraria from AstraZeneca. Panagiotis Stafylas is the Scientific Director of HealThink. HealThink received funding from AstraZeneca for research & other projects. Juan Jose Garcia Sanchez, Salvatore Barone, and Claudia Cabrera are employees of AstraZeneca.
Compliance with Ethics Guidelines
This study was conducted in accordance with ethical principles of the Declaration of Helsinki and Good Clinical Practice guidelines. This article is a review and does not contain any new studies with human participants or animals performed by any of the authors. Any data used to the purpose of the present study were anonymised.
Data Availability
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at: https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jha, V., Al-Ghamdi, S.M.G., Li, G. et al. Global Economic Burden Associated with Chronic Kidney Disease: A Pragmatic Review of Medical Costs for the Inside CKD Research Programme. Adv Ther 40, 4405–4420 (2023). https://doi.org/10.1007/s12325-023-02608-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-023-02608-9