Abstract
Background
In an effort to minimize positive margins and subsequent re-excision after breast conserving surgery (BCS), many providers and facilities have implemented either a Full Cavity Shave (FCS) approach or adding the MarginProbe Radiofrequency Spectroscopy System.
Objective
We sought to create a functioning Pro-Forma for use by facilities and payers to evaluate and compare the cost savings of implementing FCS or MarginProbe based on personalized variable inputs.
Methods
A decision tree demonstrating three possible surgical pathways, BCS, BCS + FCS, and BCS + MarginProbe was developed with clinical inputs for re-excision rate, mastectomy as 2nd surgery, rate of reconstruction, and rate of 3rd surgery derived by a literature review. A surgical pathway cost formula was created using the decision tree and financial inputs derived by utilizing the nation’s largest database of privately billed health insurance claims and Medicare claims data (fairhealth.org). Using the surgical pathway formula and financial inputs, a customizable Pro-Forma was created for immediate cost savings analysis of BCS + FCS and BCS + Marginprobe using variable inputs. Costs are from the perspective of third-party payers.
Results
Utilizing MarginProbe to reduce re-excisions for positive margins can be associated with better cost-savings than FCS due to the increased pathology processing costs by using an FCS approach. The reduction in re-excision provided by both FCS and MarginProbe offset their increased expense to various degrees with cost savings of each method improving as baseline re-excisions rates increase, until ultimately each may become cost-neutral or cost-prohibitive when compared to BCS alone. Our data suggest that in the privately insured population, MarginProbe provides a cost-savings over BCS alone when baseline re-excision rates are over 20% and that FCS becomes cost-saving when baseline re-excision rates are over 29%. For Medicare patients, MarginProbe provides a cost-savings when baseline re-excision rates exceed 34%, and FCS becomes cost-saving for re-excision rates over 52%. Our Pro-Forma allows an individual provider or institution to evaluate the cost savings of the FCS approach and/or utilization of the MarginProbe device such that the additional cost or cost-savings of utilizing one or both of these methods can be quickly calculated based on their facility’s volume and baseline re-excision rate.
Conclusions
Our data suggest that utilizing either an FCS approach or the MarginProbe radiofrequency spectroscopy system may be a cost-saving solution to reducing the rate of re-excisions depending on a facility or practice’s surgical volume and baseline re-excision rate. The degree to which each of these interventions provides an added cost or cost-savings to healthcare payers can be evaluated by utilizing the Pro-Forma outlined herein with customizable variable inputs.
Similar content being viewed by others
Introduction
The American Cancer Society estimates that in 2023, over 350,000 women will be diagnosed with either invasive breast cancer or DCIS [1]. The majority (60–70%) of these patients will undergo Breast Conserving Surgery (BCS) also known as lumpectomy or partial mastectomy, as a less invasive alternative to total mastectomy [2, 3]. The goal of BCS is complete removal of the cancerous tumor while maintaining the cosmetic appearance of the breast. A meta-analysis of more than 1,500,000 patients found that when combined with adjuvant radiation therapy, BCS provides better survival to mastectomy in patients with early stage breast cancer [4].
Pathologically involved margins after lumpectomy double the risk of breast cancer recurrence, [5, 6] and typically necessitate a repeat operation to remove additional tissue and residual disease. In 2014, the Society of Surgical Oncology (SSO) and the American Society of Clinical Oncology (ASCO) announced a consensus guideline defining positive margins for early-stage invasive breast cancer as “no tumor on ink” [5]. This guideline was followed in 2016 by a 2 mm margin standard for DCIS, presented in a consensus statement by the SSO, ASCO and the American Society for Radiation Oncology (ASTRO) [6]. Despite widespread adoption of the consensus guidelines, the need for re-excision following lumpectomy is common, averaging 20% nationwide, ranging from less than 10% to greater than 70% amongst surgeons and institutions [7]. A recent analysis of 291,000 Medicare claims reported an overall re-excision rate of 19%, with wide variability amongst surgeons from 0 to 91.7%; moreover, the rate of re-excisions was found to decrease from 22% before the aforementioned “no tumor on ink” guideline to 17.2% afterward.8
Although breast re-excision is standard procedure in the setting of positive surgical margins, the additional surgery poses several risks for the patient, including increased incidence of complications, greater psychological and emotional burden, a decline in cosmetic outcomes secondary to larger tissue volume removal, and delays initiating adjuvant therapy. In addition, after partial mastectomy with oncoplastic reconstruction, a mastectomy is required if margins are found to be positive on final surgical pathology. Re-operations also lead to increased healthcare spending, adding additional financial burden to the patient and the healthcare system as a whole.
In an effort to reduce the need for reoperation, Full Cavity Shave (FCS) has emerged as an accepted approach for mitigating positive margins at the time of initial surgery. Surgeons utilizing FCS systematically remove additional margins from all aspects of the lumpectomy cavity at the time of BCS. Some studies have shown that rates of positive margins are substantially lower when additional cavity shaves are removed during initial surgery, leading to a decrease in re-excisions by up to 50% or more [8,9,10,11,12,13].
Alternatively, surgeons may choose to utilize the MarginProbe Radiofrequency Spectroscopy System (Dilon Medical Technologies, Newport News) as an adjunctive tool for intraoperative margin assessment. MarginProbe utilizes radiofrequency spectroscopy to algorithmically analyze and detect cancerous tissue at the margins of excised lumpectomy specimens in real-time. By providing immediate feedback at the time of surgery, surgeons can take directed shavings, removing additional tissue from only the areas of concern. Like FCS, MarginProbe clinical trials report reduction in re-excision by 50% or more [14,15,16,17,18,19,20,21].
Although the clinical importance of minimizing the need for breast re-excision is clear, the cost savings in doing so is less understood. Few studies have directly compared the financial impact of re-excision after BCS or the cost savings of FCS, and to our knowledge none have performed a cost analysis of MarginProbe in comparison to BCS or BCS + FCS. We conducted a cost savings comparison of utilizing FCS or MarginProbe during BCS and examined the costs including the associated downstream resource utilization of each, presented as a customizable Pro-Forma for individual economic evaluation by third-party payers.
Methods
Cost perspective
For the purpose of this study, cost saving is reported from the perspective of third-party payers including commercial insurers and Medicare, as opposed to facility or patient perspective. The emotional and financial toll of reoperation on patients is known and acknowledged. Any additional cost to facility or payer due to reoperation or the prevention or reoperation may also impact the patient. Facilities must balance the clinical need to reduce re-excisions with the reality of adding additional procedural cost for a medical device without reimbursement, while conversely receiving payment for re-excision by third-party payers. Therefore, the least biased method to evaluate cost saving of methods to reduce re-excision will be from the perspective of the third-party payer [22, 23].
Clinical inputs
We searched the PubMed MEDLINE database for BCS outcomes related to average (invasive and DCIS) re-excision rates in the United States, published since 2014 [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24, 12, 13, 25,26,27,28,29,30,31,32,33,34,35,36]. We also searched reduction in re-excision as a result of utilizing FCS [12, 13, 36, 37] and reduction in re-excision as a result of utilizing MarginProbe [15,16,17,18,19,20,21, 38, 39] during the same timeframe. The ratio of reoperations as re-excision BCS vs. conversion to mastectomy was researched for both single and multiple reoperations after BCS [30, 40,41,42,43,44,45,46,47,48]. Further, we reviewed the literature for rate of mastectomy that is bilateral, as well as the average rate of implant reconstruction after mastectomy [49,50,51]. The American Society of Plastic Surgeons 2020 Plastic Surgery Statistics Report provided details on timing of reconstruction (immediate or delayed) [52]. All mastectomy data was limited to the United States to avoid bias as a result of different decision guidelines in other healthcare systems. Our own institutional data was analyzed to supplement these references.
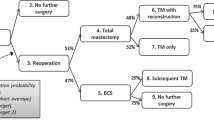
Using these clinical inputs, a decision tree was created illustrating the surgical care pathway for BCS alone, BCS + FCS or BCS + MarginProbe. (Fig. 1)
Financial inputs
Fairhealth.org was used to gather commercial cost data. Medicare data was collected from CMS.gov. To complement this comparison, we gathered data on the number of people who have healthcare insurance from the most recent U.S. Census Bureau report on healthcare coverage in the United States [53] which included a breakdown of types of insurance. The CPT codes used for the purposes of this study are found in Table 1.
Although CPT codes for BCS and BCS + FCS are identical, pathology CPT code 88,307 is paid on each specimen analyzed. Therefore, a FCS operation with multiple specimens incurs additional cost for payers than a BCS with fewer specimens for pathology analysis.
MarginProbe costs were provided directly by the device manufacturer. A one-time cost for the MarginProbe is priced at $50,000. The list price for the disposable probe is $995 per procedure. Actual pricing for console and disposable probes may be lower based on IDN contract pricing and negotiated procedure volume discounts. All cost savings analyses use device list price unless stated otherwise.
Price comparison formula
Using the clinical and financial inputs in combination with the Decision Tree, a cost formula was created for each surgical pathway (Fig. 2) for input into a Pro-Forma Model.
N = Number of Patients | BCS = Breast Conserving Surgery | Recon = Reconstruction |
|---|---|---|
R = Rate | FCS = Full Cavity Shave | IR = Immediate Reconstruction |
C = Cost | MP = MarginProbe | DR = Delayed Reconstruction |
Re = Reoperation | TM = Total Mastectomy | BI = Bilateral Mastectomy |
Cost savings analysis
We referenced the Cost Savings Economic Evaluation framework provided by the Office of the Associate Director for Policy and Strategy on the cdc.gov website [54] to perform three analyses for output on the Pro-Forma: (1) The cost savings of adding FCS to BCS, (2) the cost savings of adding MarginProbe to BCS, and (3) the cost savings of MarginProbe and FCS compared to each other. In this case, where both MarginProbe and FCS reduce re-excisions and therefore cost to the payer, the two methods demonstrate different cost savings due to cost of preventing each positive margin.
Re-excision rate reduction as a result of implementing either MarginProbe or FCS to BCS alone were set by default to 50%. The rate of reduction can be adjusted in the Pro-Forma. The MarginProbe console and disposable probe costs are set at list price by default but can be adjusted in the Pro-Forma.
Net costs/net savings were calculated by subtracting the formula-calculated pathway cost from the pathway cost of its comparator. i.e., the net cost of adding FCS to BCS is the pathway cost of FCS minus the pathway cost of BCS alone. Net costs/net savings are presented on both a per patient basis and total annual basis based on BCS volume inputs in the Pro-Forma. When the intervention improves re-excision rates but is more costly, the cost savings is also presented as a ratio, reported as “cost per re-excision prevented.”
Results
Overview
All surgical pathway costs are dependent on multiple factors, including the patient’s insurance coverage, the provider’s current rate of re-excision, and the final rate of re-excision after adding FCS or MarginProbe to BCS. BCS + FCS pathway costs begin higher than BCS alone due to pathology charges for each of the additional shave specimens from the six anatomical faces of the lumpectomy cavity. BCS + MP costs begin higher than BCS alone due to an average two additional shave margins and device cost. The reduction in re-excision provided by adding FCS or MarginProbe to BCS may offset the increased spending to various degrees based on baseline re-excision rate, until ultimately, each may become cost-neutral or provide a cost-savings.
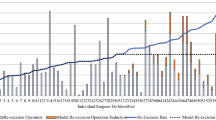
In the commercially insured population, MarginProbe provides added cost to standard of care BCS when re-excision rates are below 20%, where it then becomes cost-neutral. Using an FCS approach adds additional cost when re-excision rates are below 29%, where it then becomes cost-neutral. For uninsured patients, MarginProbe becomes cost-neutral for a baseline re-excision rate of 25%, and FCS is cost-neutral when re-excisions reach 51%. Finally, in the Medicare population, MarginProbe was found to add additional cost up to a baseline re-excision rate of 34% where it becomes cost-neutral, and FCS provided added cost until a re-excision rate of 52% was reached. Pathway cost comparisons along the range of baseline re-excision rates in Commercially Insured, Uninsured, and Medicare patients are illustrated in Fig. 3.
Using the pro-forma for customized analysis
Individualized analysis for consideration of surgical pathways across various patient populations, procedure volumes and current standard of care is made possible by utilizing the Pro-Forma. Examples A-B demonstrate its utility for evaluating the economic impact of adopting either method of margin management in additional to BCS, as well as comparing the effect of changing from one method to the other when it is already part of the facility standard of care.
Example A – low volume facility, currently using BCS (can update examples however the group wants)
In this example of a typical 400 bed facility, inputs include an annual procedure volume of 45 lumpectomies of which 42% are Medicare and 58% are commercially insured. The re-excision rate is 19.6% and the analysis considers MarginProbe at list price.
Implementing FCS would add an additional $1,458 per patient. It would cost $14,881 to prevent one re-excision. Alternatively, adding MarginProbe to BCS procedures would incur an initial capital expenditure of $50,000 and an additional $397 per patient preventing one re-excision for every $4,055 spent.
Comparing the two interventions directly, implementing a MarginProbe program in lieu of FCS would be cost-neutral for the first year due to the initial capital cost of the MarginProbe console, and then would reduce healthcare spend by nearly $1,061 per patient and save nearly $48,000 per year while reducing re-excisions below 10%. (Fig. 4)
Example B – high volume facility, currently using FCS
This example represents a high-volume facility performing 400 BCS per year. FCS is standard of care for each procedure, and the re-excision rate is 5.1%. The payer-mix is 31% Medicare, 69% private insurance. MarginProbe variables are set to list price of $995 per disposable probe and a one-time cost of $50,000 for the system console.
Converting to MarginProbe from FCS would reduce per patient cost by $1,082 and provide an annual healthcare savings of over $430,000 beginning after six weeks, while maintaining the same 5.1% re-excision rate. (Fig. 5)
Discussion
Successful BCS is predicated on achieving pathologically clear margins. Reoperation due to margin involvement has been described as “the other breast-cancer epidemic” [55] and much focus has been placed on reducing re-excision rates across the United States.
Multiple best practices and methods have been accepted as part of a surgeon’s “toolbox” and meant be used simultaneously to minimize the need for re-excision surgery as recommended by the American Society of Breast Surgeons (ASBrS) [7]. Examples include localization of non-palpable lesions, specimen orientation of three or more margins, oncoplastic technique, and specimen radiograph with surgeon intraoperative review.
FCS has also been recommended as a part of the toolbox, as a method to reduce the burden of positive margins [7]. Cost-savings associated with FCS have been mixed [56,57,58]. Our Pro-Forma illustrates the dependency of baseline re-excision rate on the economic utility of FCS. Likewise, the cost of utilizing MarginProbe for intraoperative margin assessment may or may not be offset by reduction in re-excision, dependent on the facility’s beginning rate of re-excision.
Our Pro-Forma considers only the surgical phase of breast-cancer treatment, as the post-surgical treatment pathways would be the same for both FCS and MarginProbe patients. One shortcoming of the Pro-Forma is that it does not take into consideration radiation therapy costs, which does not impact a comparison of FCS and MarginProbe to each other but may alter the significance of the two methods in comparison to BCS alone, due to more conversion to mastectomy (and therefore less radiation) in a percentage of patients with positive margins undergoing standard BCS. It would not be difficult to adjust the Pro-Forma to consider radiation therapy costs based on a facility’s unique parameters.
There are no known head-to-head studies of FCS versus MarginProbe. Therefore, although the Pro-Forma allows for variable inputs for the rate of re-excision reduction of each, the assumption of each reducing reoperations by 50% is based on published literature of each method and is a current limitation of the Pro-Forma cost savings example reported.
Another way the Pro-Forma could be used is in only a subset of BCS patients at higher risk of positive margins and re-excision. For example, a facility utilizing intraoperative ultrasound for margin assessment during their 300 annual lumpectomies, with a re-excision rate of 4%, would see that although FCS and MarginProbe would lower re-excisions to 2%, it would be at an annual additional cost of nearly $850,000 for FCS or just over $500,000 for MarginProbe.
Conversely, the same facility could determine that their 12 re-excisions were nearly exclusively in DCIS patients and use the Pro-Forma to determine that utilizing FCS or MarginProbe only for their 36 annual DCIS patients per year, they would reduce their re-excisions by half, while saving $3,000 per year if using FCS, or saving almost $37,000 per year if using MarginProbe.
The personalization of the Pro-Forma enables exacting review and consideration to the cost and utility of the two surgical pathways. Any parameter can be attributed to a facility’s personalized input.
Conclusions
The clinical importance of minimizing positive margins and subsequent re-excision after BCS is well known. MarginProbe Radiofrequency Spectroscopy is solution than reduce the positive margins and re-excisions by 50% or more. The degree to which each of these interventions provides an added cost or savings to healthcare payers is dependent on facility breast-conserving procedural volume and baseline re-excision rate. Comparison of the two interventions as well as overall cost savings to healthcare payers can be evaluated by utilizing the Pro-Forma with customized variable inputs. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html
Data Availability
The data and material used for this manuscript are publicly available and presented in the reference section.
References
Cancer F, Fig. 2023. American Cancer Society. Accessed June 1, 2023, https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/2023-cancer-facts-figures.html.
Kummerow KL, Du L, Penson DF, Shyr Y, Hooks MA. Nationwide Trends in Mastectomy for early-stage breast Cancer. JAMA Surg. 2015;150(1):9. https://doi.org/10.1001/jamasurg.2014.2895.
Katipamula R, Degnim AC, Hoskin T, et al. Trends in Mastectomy Rates at the Mayo Clinic Rochester: Effect of Surgical Year and Preoperative magnetic resonance imaging. J Clin Oncol. 2009;27(25):4082–8. https://doi.org/10.1200/jco.2008.19.4225.
De la Cruz Ku G, Karamchandani M, Chambergo-Michilot D, et al. Does breast-conserving surgery with Radiotherapy have a better survival than mastectomy? A Meta-analysis of more than 1,500,000 patients. Ann Surg Oncol. 2022;10(10):6163–88. https://doi.org/10.1245/s10434-022-12133-8. /01 2022.
Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical oncology–american Society for Radiation Oncology Consensus Guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast Cancer. Int J Radiation Oncology*Biology*Physics. 2014;88(3):553–64. https://doi.org/10.1016/j.ijrobp.2013.11.012.
Morrow M, Van Zee KJ, Solin LJ, et al. Society of Surgical oncology–american Society for Radiation Oncology–American Society of Clinical Oncology Consensus Guideline on margins for breast-conserving surgery with whole-breast irradiation in Ductal Carcinoma in situ. Practical Radiation Oncology. 2016;6(5):287–95. https://doi.org/10.1016/j.prro.2016.06.011.
McEvoy MP, Landercasper J, Naik HR, Feldman S. Update of the american society of breast Surgeons Toolbox to address the lumpectomy reoperation epidemic. Gland Surg. 2018;7(6):536–53. https://doi.org/10.21037/gs.2018.11.03.
Keskek M, Kothari M, Ardehali B, Betambeau N, Nasiri N, Gui GP. Factors predisposing to cavity margin positivity following conservation surgery for breast cancer. Eur J Surg Oncol Dec. 2004;30(10):1058–64. https://doi.org/10.1016/j.ejso.2004.07.019.
Jacobson AF, Asad J, Boolbol SK, Osborne MP, Boachie-Adjei K, Feldman SM. Do additional shaved margins at the time of lumpectomy eliminate the need for re-excision? Am J Surg Oct. 2008;196(4):556–8. https://doi.org/10.1016/j.amjsurg.2008.06.007.
Rizzo M, Iyengar R, Gabram SG, et al. The effects of additional tumor cavity sampling at the time of breast-conserving surgery on final margin status, volume of resection, and pathologist workload. Ann Surg Oncol Jan. 2010;17(1):228–34. https://doi.org/10.1245/s10434-009-0643-x.
Zavagno G, Donà M, Orvieto E, et al. Separate cavity margins excision as a complement to conservative breast cancer surgery. Eur J Surg Oncol Jul. 2010;36(7):632–8. https://doi.org/10.1016/j.ejso.2010.05.018.
Chagpar AB, Killelea BK, Tsangaris TN, et al. A Randomized, Controlled Trial of Cavity Shave margins in breast Cancer. N Engl J Med. Aug 2015;6(6):503–10. https://doi.org/10.1056/NEJMoa1504473.
Dupont E, Tsangaris T, Garcia-Cantu C, et al. Resection of Cavity Shave margins in stage 0-III breast Cancer patients undergoing breast conserving surgery: a prospective Multicenter Randomized Controlled Trial. Ann Surg May. 2021;1(5):876–81. https://doi.org/10.1097/sla.0000000000003449.
Allweis TM, Kaufman Z, Lelcuk S, et al. A prospective, randomized, controlled, multicenter study of a real-time, intraoperative probe for positive margin detection in breast-conserving surgery. Am J Surg Oct. 2008;196(4):483–9. https://doi.org/10.1016/j.amjsurg.2008.06.024.
Schnabel F, Boolbol SK, Gittleman M, et al. A randomized prospective study of lumpectomy margin assessment with use of MarginProbe in patients with nonpalpable breast malignancies. Ann Surg Oncol May. 2014;21(5):1589–95. https://doi.org/10.1245/s10434-014-3602-0.
Thill M, Dittmer C, Baumann K, Friedrichs K, Blohmer JU. MarginProbe®--final results of the german post-market study in breast conserving surgery of ductal carcinoma in situ. Breast Feb. 2014;23(1):94–6. https://doi.org/10.1016/j.breast.2013.11.002.
Sebastian M, Akbari S, Anglin B, Lin EH, Police AM. The impact of use of an intraoperative margin assessment device on re-excision rates. Springerplus. 2015;4:198. https://doi.org/10.1186/s40064-015-0801-5.
Blohmer JU, Tanko J, Kueper J, Groß J, Völker R, Machleidt A. MarginProbe© reduces the rate of re-excision following breast conserving surgery for breast cancer. Arch Gynecol Obstet Aug. 2016;294(2):361–7. https://doi.org/10.1007/s00404-016-4011-3.
Coble J, Reid V. Achieving clear margins. Directed shaving using MarginProbe, as compared to a full cavity shave approach. Am J Surg Apr. 2017;213(4):627–30. https://doi.org/10.1016/j.amjsurg.2016.12.019.
Kupstas A, Ibrar W, Hayward RD, Ockner D, Wesen C, Falk J. A novel modality for intraoperative margin assessment and its impact on re-excision rates in breast conserving surgery. Am J Surg. Mar 2018;215(3):400–3. https://doi.org/10.1016/j.amjsurg.2017.11.023.
Geha RC, Taback B, Cadena L, Borden B, Feldman S. A single institution’s randomized double-armed prospective study of lumpectomy margins with adjunctive use of the MarginProbe in nonpalpable breast cancers. Breast J Nov. 2020;26(11):2157–62. https://doi.org/10.1111/tbj.14004.
Blank MM, Papageorge M, Chen L, Driscoll D, Graham R, Chatterjee A. Hidden Bias in cost-analysis research: what is the prevalence of under-reporting cost perspective in the General Surgical Literature? J Am Coll Surg Dec. 2017;225(6):823–828e12. https://doi.org/10.1016/j.jamcollsurg.2017.08.013.
Blank MM, Chen L, Papageorge M, Driscoll D, Graham R, Chatterjee A. The underreporting of cost perspective in cost-analysis research: a systematic review of the plastic surgery literature. J Plast Reconstr Aesthet Surg. Mar 2018;71(3):366–76. https://doi.org/10.1016/j.bjps.2017.12.008.
Kaczmarski K, Wang P, Gilmore R, et al. Surgeon Re-Excision Rates after breast-conserving surgery: a measure of low-value care. J Am Coll Surg Apr. 2019;228(4):504–512e2. https://doi.org/10.1016/j.jamcollsurg.2018.12.043.
Chung A, Gangi A, Amersi F, Bose S, Zhang X, Giuliano A. Impact of Consensus Guidelines by the Society of Surgical Oncology and the American Society for Radiation Oncology on margins for breast-conserving surgery in stages 1 and 2 invasive breast Cancer. Ann Surg Oncol Dec. 2015;22(Suppl 3):422–7. https://doi.org/10.1245/s10434-015-4829-0.
Rosenberger LH, Mamtani A, Fuzesi S, et al. Early adoption of the SSO-ASTRO Consensus Guidelines on margins for breast-conserving surgery with whole-breast irradiation in stage I and II invasive breast Cancer: initial experience from Memorial Sloan Kettering Cancer Center. Ann Surg Oncol. 2016;23(10):3239–46. https://doi.org/10.1245/s10434-016-5397-7.
Merrill AL, Tang R, Plichta JK, et al. Should New No Ink on Tumor Lumpectomy Margin Guidelines be Applied to Ductal Carcinoma in situ (DCIS)? A Retrospective Review using shaved cavity margins. Ann Surg Oncol. 2016;23(11):3453–8. https://doi.org/10.1245/s10434-016-5251-y. /10/01 2016.
Patten CR, Walsh K, Sarantou T, et al. Changes in margin re-excision rates: experience incorporating the no ink on tumor guideline into practice. J Surg Oncol Dec. 2017;116(8):1040–5. https://doi.org/10.1002/jso.24770.
Schulman AM, Mirrielees JA, Leverson G, Landercasper J, Greenberg C, Wilke LG. Reexcision Surgery for Breast Cancer: An Analysis of the American Society of Breast Surgeons (ASBrS) MasterySM Database Following the SSO-ASTRO “No Ink on Tumor” Guidelines. Annals of Surgical Oncology. 2017;24(1):52–58. doi:10.1245/s10434-016-5516-5.
Metcalfe LN, Zysk AM, Yemul KS, et al. Beyond the margins—economic costs and complications Associated with repeated breast-conserving surgeries. JAMA Surg. 2017;152(11):1084. https://doi.org/10.1001/jamasurg.2017.2661.
Bhutiani N, Mercer MK, Bachman KC, et al. Evaluating the Effect of Margin Consensus Guideline publication on operative patterns and financial impact of breast Cancer operation. J Am Coll Surg. Jul 2018;227(1):6–11. https://doi.org/10.1016/j.jamcollsurg.2018.01.050.
Landercasper J, Borgert AJ, Fayanju OM, et al. Factors Associated with Reoperation in breast-conserving surgery for Cancer: a prospective study of american society of breast surgeon members. Ann Surg Oncol Oct. 2019;26(10):3321–36. https://doi.org/10.1245/s10434-019-07547-w.
Mamtani A, Zabor EC, Rosenberger LH, Stempel M, Gemignani ML, Morrow M. Was Reexcision less frequent for patients with lobular breast Cancer after publication of the SSO-ASTRO Margin Guidelines? Ann Surg Oncol Nov. 2019;26(12):3856–62. https://doi.org/10.1245/s10434-019-07751-8.
Havel L, Naik H, Ramirez L, Morrow M, Landercasper J. Impact of the SSO-ASTRO Margin Guideline on Rates of Re-excision after lumpectomy for breast Cancer: a Meta-analysis. Ann Surg Oncol May. 2019;26(5):1238–44. https://doi.org/10.1245/s10434-019-07247-5.
Mamtani A, Romanoff A, Baser R, Vincent A, Morrow M, Gemignani ML. Adoption of SSO-ASTRO Margin Guidelines for Ductal Carcinoma in situ: what is the impact on Use of additional surgery? Ann Surg Oncol Jan. 2021;28(1):295–302. https://doi.org/10.1245/s10434-020-08610-7.
Howard-McNatt M, Dupont E, Tsangaris T, et al. Impact of Cavity Shave margins on Margin Status in patients with pure Ductal Carcinoma in situ. J Am Coll Surg Apr. 2021;232(4):373–8. https://doi.org/10.1016/j.jamcollsurg.2020.11.019.
Wang K, Ren Y, He J. Cavity shaving plus lumpectomy versus lumpectomy alone for patients with breast Cancer undergoing breast-conserving surgery: a systematic review and Meta-analysis. PLoS ONE. 2017;12(1):e0168705. https://doi.org/10.1371/journal.pone.0168705.
Hermann N, Haas I, Mlinger P, Koifman Z. Margin assessment before intraoperative radiotherapy during breast conserving surgery—does the addition of MarginProbe decrease the need for addition of fractionated whole breast radiation? Breast J 05/01. 2020;2610.1111/tbj.13865.
Cen C, Chun J, Kaplowitz E, et al. Margin Assessment and Re-excision Rates for Patients who have neoadjuvant chemotherapy and breast-conserving surgery. Ann Surg Oncol. 2021;28(9):5142–8. https://doi.org/10.1245/s10434-020-09524-0.
McCahill LE, Single RM, Aiello Bowles EJ, et al. Variability in Reexcision following breast conservation surgery. JAMA. 2012;307(5):467. https://doi.org/10.1001/jama.2012.43.
Waljee JF, Hu ES, Newman LA, Alderman AK. Predictors of re-excision among women undergoing breast-conserving surgery for cancer. Ann Surg Oncol May. 2008;15(5):1297–303. https://doi.org/10.1245/s10434-007-9777-x.
Morrow M, Jagsi R, Alderman AK, et al. Surgeon recommendations and receipt of mastectomy for treatment of breast cancer. Jama Oct. 2009;14(14):1551–6. https://doi.org/10.1001/jama.2009.1450.
Cellini C, Hollenbeck ST, Christos P, et al. Factors associated with residual breast cancer after re-excision for close or positive margins. Ann Surg Oncol Oct. 2004;11(10):915–20. https://doi.org/10.1245/aso.2004.12.037.
Wilke LG, Czechura T, Wang C, et al. Repeat surgery after breast conservation for the treatment of stage 0 to II breast carcinoma: a report from the National Cancer Data Base, 2004–2010. JAMA Surg Dec. 2014;149(12):1296–305. https://doi.org/10.1001/jamasurg.2014.926.
Sanchez C, Brem RF, McSwain AP, Rapelyea JA, Torrente J, Teal CB. Factors associated with re-excision in patients with early-stage breast cancer treated with breast conservation therapy. Am Surg Mar. 2010;76(3):331–4.
Piper ML, Wong J, Fahrner-Scott K, et al. Success rates of re-excision after positive margins for invasive lobular carcinoma of the breast. NPJ Breast Cancer. 2019;5:29. https://doi.org/10.1038/s41523-019-0125-7.
Valero MG, Mallory MA, Losk K, et al. Surgeon variability and factors Predicting for Reoperation following breast-conserving surgery. Ann Surg Oncol. 2018;25(9):2573–8. https://doi.org/10.1245/s10434-018-6526-2.
Singer L, Brown E, Lanni T. Jr. Margins in breast conserving surgery: the financial cost & potential savings associated with the new margin guidelines. Breast Aug. 2016;28:1–4. https://doi.org/10.1016/j.breast.2016.04.007.
Baskin AS, Wang T, Bredbeck BC, Sinco BR, Berlin NL, Dossett LA. Trends in Contralateral Prophylactic Mastectomy utilization for small unilateral breast Cancer. J Surg Res. 2021;262:71–84. https://doi.org/10.1016/j.jss.2020.12.057.
Ilonzo N, Tsang A, Tsantes S, Estabrook A, Thu Ma AM. Breast reconstruction after mastectomy: a ten-year analysis of trends and immediate postoperative outcomes. Breast Apr. 2017;32:7–12. https://doi.org/10.1016/j.breast.2016.11.023.
Jonczyk MM, Jean J, Graham R, Chatterjee A. Surgical trends in breast cancer: a rise in novel operative treatment options over a 12 year analysis. Breast Cancer Res Treat Jan. 2019;173(2):267–74. https://doi.org/10.1007/s10549-018-5018-1.
2020 Plastic Surgery Statistics Report. American Society of Plastic Surgeons. Accessed September 18., 2021, https://www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf.
Keisler-Starkey K, Bunch L. Health Insurance Coverage in the United States: 2020. September 2021:P60-274. Current Population Reports. https://www.census.gov/content/dam/Census/library/publications/2021/demo/p60-274.pdf.
Center for Disease Control and Prevention. Cost-Effectiveness Analysis. Accessed October 2., 2021, https://www.cdc.gov/policy/polaris/economics/cost-effectiveness/index.html.
Cody HS 3rd, Van Zee KJ. Reexcision–the other breast Cancer Epidemic. N Engl J Med. Aug 2015;6(6):568–9. https://doi.org/10.1056/NEJMe1507190.
Chagpar AB, Horowitz NR, Killelea BK, et al. Economic impact of routine cavity margins Versus Standard partial mastectomy in breast Cancer patients. Ann Surg. 2017;265(1):39–44. https://doi.org/10.1097/sla.0000000000001799.
Corsi F, Sorrentino L, Bonzini M, et al. Cavity shaving reduces involved margins and reinterventions without increasing costs in breast-conserving surgery: a propensity score-matched study. Ann Surg Oncol Jun. 2017;24(6):1516–24. https://doi.org/10.1245/s10434-017-5774-x.
Cartagena LC, McGuire K, Zot P, Pillappa R, Idowu M, Robila V. Breast-conserving surgeries with and without Cavity shave margins have different re-excision Rates and Associated overall cost: institutional and patient-driven decisions for its utilization. Clin Breast Cancer. 2021;10(5):e594–e601. https://doi.org/10.1016/j.clbc.2021.03.003.
Funding
No direct funding was received. We have received assistance with analysis and interpretation of data as well as drafting of manuscript from Lisa Cadena, MBA. She is a current consultant to Dilon Technologies and she was a previous salaried employee. She was not involved in development of the surgical pathway cost formula or acquisition of data/results.
Author information
Authors and Affiliations
Contributions
Study conception and design: Gilmore, Dembinski, Habibi. Acquisition of data/results: Gilmore, Chen, Dembinski, Reissis, Milek. Analysis and interpretation of data: Gilmore, Dembinski, Cadena, Habibi. Drafting of manuscript: Gilmore, Cadena, Habibi. Critical revision: Gilmore, Habibi.
Corresponding author
Ethics declarations
Ethical approval approval and consent to participate
(Not Applicable) The analysis was made on publicly available data and peer reviewed publications.
Competing interests
We have received assistance with analysis and interpretation of data as well as drafting of manuscript from Lisa Cadena, MBA. She is a current consultant to Dilon Technologies and she was a previous salaried employee. She was not involved in development of the surgical pathway cost formula or acquisition of data/results. Mehran Habibi is consultant for Dilon Technologies.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gilmore, R., Chen, J., Dembinski, R. et al. Cost minimization in breast conserving surgery: a comparative study of radiofrequency spectroscopy and full cavity shave margins. Cost Eff Resour Alloc 21, 66 (2023). https://doi.org/10.1186/s12962-023-00477-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-023-00477-1