Abstract
Background
Falls impose significant health and economic burdens on community-dwelling older persons. Decision modelling can inform commissioning of alternative falls prevention strategies. Several methodological challenges arise when modelling public health interventions including community-based falls prevention. This study aims to conduct a systematic review (SR) to: systematically identify community-based falls prevention economic models; synthesise and critically appraise how the models handled key methodological challenges associated with public health modelling; and suggest areas for further methodological research.
Methods
The SR followed the 2021 PRISMA reporting guideline and covered the period 2003–2020 and 12 academic databases and grey literature. The extracted methodological features of included models were synthesised by their relevance to the following challenges: (1) capturing non-health outcomes and societal intervention costs; (2) considering heterogeneity and dynamic complexity; (3) considering theories of human behaviour and implementation; and (4) considering equity issues. The critical appraisal assessed the prevalence of each feature across models, then appraised the methods used to incorporate the feature. The methodological strengths and limitations stated by the modellers were used as indicators of desirable modelling practice and scope for improvement, respectively. The methods were also compared against those suggested in the broader empirical and methodological literature. Areas of further methodological research were suggested based on appraisal results.
Results
46 models were identified. Comprehensive incorporation of non-health outcomes and societal intervention costs was infrequent. The assessments of heterogeneity and dynamic complexity were limited; subgroup delineation was confined primarily to demographics and binary disease/physical status. Few models incorporated heterogeneity in intervention implementation level, efficacy and cost. Few dynamic variables other than age and falls history were incorporated to characterise the trajectories of falls risk and general health/frailty. Intervention sustainability was frequently based on assumptions; few models estimated the economic/health returns from improved implementation. Seven models incorporated ethnicity- and severity-based subgroups but did not estimate the equity-efficiency trade-offs. Sixteen methodological research suggestions were made.
Conclusion
Existing community-based falls prevention models contain methodological limitations spanning four challenge areas relevant for public health modelling. There is scope for further methodological research to inform the development of falls prevention and other public health models.
Similar content being viewed by others
Background
The process of ageing encompasses multidimensional changes in physical and psychosocial domains [1]. Associated with ageing are risks of geriatric syndromes (e.g., falls, incontinence, delirium, and frailty) as symptoms of age-related impairments to multiple organ and physiological systems [2,3,4]. Around a third of people aged 65 and over (65+) fall each year [5]. As a geriatric syndrome, falls impose significant morbidity and mortality burdens [6], including fear of falling [7,8,9], depression [10], functional dependence [11,12,13], and fatality [14,15,16]. Falls can impose high costs on the health and social care systems [17,18,19], and on patients and wider society through out-of-pocket (OOP) care expenditure [20, 21], informal caregiver burden [22,23,24], and productivity loss [25, 26].
The National Institute for Health and Care Excellence (NICE) falls prevention clinical guideline (CG161) for England and Wales recommends that community-dwelling people aged 65+ are routinely screened for falls risk. High-risk individuals should be referred to multifactorial intervention involving multidisciplinary falls risk assessment, followed by tailored treatments including exercise, home assessment and modification (HAM), vision correction and medication change [5]. This proactive (i.e., initiated by professional referral) pathway may be supplemented by a reactive pathway for persons admitted to a medical facility for a fall (recommended by CG161), and self-referral to community programmes [27, 28]. Trial-based evidence suggests multifactorial and single-component community-based interventions significantly reduce the number of falls and/or fallers [29,30,31].
Commissioning of these community-based interventions should be informed by economic evaluations that consider the costs and consequences of any falls prevention strategy against the next best alternative use of resources [32]. Decision modelling is a vehicle for economic evaluation that can combine multiple epidemiological, intervention, and economic parameters from diverse sources [33]. Decision models have several advantages relative to economic evaluations alongside single clinical studies, such as the ability to incorporate long-term trajectories of falls risk, synthesise evidence from a range of sources, and evaluate all relevant intervention scenarios [34].
There are methodological challenges which are likelier to arise when economic evaluation is applied to public health rather than clinical interventions [35,36,37,38]. The former typically target general populations rather than narrowly defined patient groups, thereby generating significant heterogeneity in intervention access and outcomes across individuals and population subgroups; persistent variation over time generates dynamic complexity. Inequalities in outcomes across subgroups also become a normative issue and often an explicit policy objective to reduce. Moreover, public health interventions frequently require behavioural changes at the individual lifestyle and communal levels, raising issues in implementation. The determinants of health targeted by public health interventions are much broader than the biological mechanisms modified by clinical treatments, and include, for example, the physical/social environment. Public health interventions hence often require the involvement of non-healthcare stakeholders, and their evaluations should involve the tracking of wider non-health outcomes and non-healthcare costs. These challenges are particularly pertinent to decision modelling: first because models are well-positioned to incorporate key methodological solutions—e.g., expanding the evaluation horizon to account for dynamic complexity and appraising the efficiency-equity impacts of multiple intervention strategies; and second due to a concomitant risk that failing to address the challenges would produce less-than-credible model structures and results [39, 40].
Community-based falls prevention could be conceived as a representative public health intervention for several reasons. First, the multidimensional and syndromic nature of falls generates significant heterogeneity in falls risk among the general older population and the associated need for risk screening and multiple intervention pathways as noted. Second, falls are closely associated with frailty [41, 42], which in turn is closely associated with socioeconomic deprivation [43, 44]. Hence, the falls prevention strategy should consider social inequities of health across population subgroups. Third, falls prevention access is highly dependent upon older persons’ motives and professional behaviour [45,46,47] and therefore face significant implementation issues [48]. These features of falls prevention suggest that the aforementioned challenges to public health economic evaluation apply equally to falls prevention economic evaluations, particularly falls prevention economic models.
A systematic review approach can be used to critically appraise how existing falls prevention economic models have handled the methodological challenges, and thereby assist in the conceptualisation of future models [39]. A previous systematic overview of systematic reviews found that such critical appraisal was not performed comprehensively by the seven existing systematic reviews of community-based falls prevention economic evaluations [49]. For example, the extracted modelling features were limited to model type and brief summaries of data sources. Broader challenges for public health economic modelling were rarely considered, with only one review appraising how previous models incorporated wider costs and outcomes (e.g., productivity loss) [50], while another appraised how they considered issues of equity [51]. The reviews also covered heterogeneous sets of models such that their results do not constitute a comprehensive appraisal.
These findings motivated the current de novo systematic review, the methods and first part of results of which were recently published in a separate article [52]. The latter identified 46 models of community-based falls prevention, applied a methodological and reporting quality checklist designed by falls prevention experts [53], narratively synthesised methodological features relevant to falls epidemiology, falls prevention intervention and evaluation methods, and generated methodological and commissioning recommendations for falls prevention modellers and commissioners. The current article continues the narrative synthesis and appraisal, focusing on how the 46 models handled the challenges specific to public health economic modelling, and generates suggestions for further methodological research.
Challenges to public health economic modelling
A previous systematic methodological review identified the following four key challenge categories to public health modelling [40]: (1) capturing non-health outcomes and societal intervention costs of falls prevention; (2) considering heterogeneity and dynamic complexity in health determinants and intervention need; (3) considering theories of human behaviour and implementation; and (4) considering issues of equity. These provide the analytical public health modelling challenges (PHMC) framework for appraising the falls prevention economic models identified by the systematic review and are described in more detail in this section. A caveat is that the challenges do not exhaust the range of methodological issues present within public health economic modelling but rather highlight the key ones discussed in the literature as identified by the systematic methodological review [40].
Capturing non-health outcomes and societal intervention costs
Public health issues and interventions frequently affect non-health outcomes and expend resources outside the public healthcare system [36, 40, 53,54,55]. Prominent non-health effects of falls include: reduction in social wellbeing [56,57,58], often poorly captured in health status/utility measures [59]; OOP care expenditures (around 12% of annual care costs of fallers) [20]; loss in paid and unpaid productivity [26, 55] and the related loss in older persons’ wellbeing [60]; and informal caregiver cost (around 22% of annual care costs of fallers) [23] and health-related stress, particularly when the caregivers themselves are old/frail [61,62,63]. Meanwhile, falls prevention interventions incur societal costs, including: social stigma in participation (although this can also bring social benefits [64]), particularly in contexts where geriatric health promotion is uncommon [47]; private co-payments and costs (e.g., for transport); and time opportunity costs for participants and accompanying caregivers [65, 66]. Falls prevention may also bring benefits that chiefly accrue to the community rather than to individuals [67,68,69]; for example, community-wide participation can strengthen the community’s ability to organise other health promotion initiatives. The communal benefits should be weighed against the resources invested for social mobilisation, particularly those not reimbursed by the public sector (e.g., volunteer labour). Whilst the evaluation perspective will be dependent upon the decision-making context, it is likely useful to policymakers for models to capture as many of these outcomes and costs as possible.
Considering heterogeneity and dynamic complexity
The ageing process that encompasses multidimensional changes in physical and psychosocial domains gives rise to high levels of heterogeneity in health status, functioning and healthcare needs [1]. This is particularly relevant to falls and other geriatric syndromes with multifactorial risk profiles spanning the physical, psychological and environmental domains [2, 5, 70]. Heterogeneity introduces variations in falls risk and consequences (e.g., injury severity) and intervention cost, implementation (e.g., care pathways, demand) and efficacy [71]; accounting for these subgroup variations offers opportunities to target subgroups that best meet the decisional criteria (e.g., cost-effectiveness, equity) and/or tailor interventions according to heterogeneous needs [72]. Dynamic complexity arises from intertemporal interaction between causal mechanisms and further increases the heterogeneity between individuals and subgroups. Falls prevention operates in a dynamically complex system characterised by features such as feedback loops (e.g., physical decline increases falls risk and falls accelerate physical decline) (p. 42) [73]. Models should capture the heterogeneity and dynamic complexity of the within-model causal mechanisms—e.g., falls risk, comorbidity level, intervention need and demand—and assess their impact on outcomes.
Considering theories of human behaviour and implementation
Geriatric health behaviours are strongly shaped by individual psychology (e.g., motivation to prevent functional decline) and social interaction [69, 73,74,75]. These behaviours determine the prevalence and trajectory of risk factors and the implementation quality of interventions in terms of initial access, adherence and long-term participation [76, 77]. Directly parameterising the psychological and sociological factors would generate model outcomes that are highly sensitive to changes in these factor values [73]. Meanwhile, even just conducting sensitivity/scenario analyses to explore how the model outcomes vary according to different implementation levels would generate useful, heuristic information for decision-makers, specifically regarding investment decisions on auxiliary strategies to improve implementation (e.g., community marketing) [78, 79].
Considering issues of equity
As highlighted by an international expert panel, healthcare decision-makers face several priority setting criteria beyond cost-effectiveness [54]. These criteria include prioritising the care needs of those in socially deprived subgroups and those with more severe disease and past health loss among similar-age peers. These two vulnerable subgroups overlap in practice given the strong influence of social factors (e.g., income, housing) on health both over the earlier life course and contemporaneously in old age [1, 80]. Prioritising these subgroups likely worsens the overall cost-effectiveness of the intervention given factors such as the ‘double jeopardy’ problem whereby vulnerable groups derive lower efficacy (e.g., due to comorbidity-related contraindications) and/or poorer implementation quality [81, 82]. Models should quantify such equity-efficiency trade-offs and their impact on decisions [37, 82].
Methods
The systematic review methods were previously described in the aforementioned article [52]. “Systematic review methods” section summarises the associated search methods and inclusion criteria. “Critical appraisal methods” section then describes the methods for critically appraising the included models under the PHMC framework.
Systematic review methods
The systematic review protocol is registered on the Prospective Register of Systematic Reviews (CRD42021232147). The review followed the 2021 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline [83]: see checklist in separate article [52]. The search covered the period 2003–2020, 12 academic databases and grey literature. A previous systematic review of falls prevention economic evaluations, conducted to inform the NICE falls prevention clinical guideline, covered the period up to 2003 [84]. The current review hence updates the latter, albeit focusing on modelling studies. The search strategy was an intersection between terms for falls, older people, and economic evaluation; the separate article reports all database search strategies [52]. Two researchers independently reviewed the titles and abstracts of identified articles at the first stage and the full texts of approved articles at the second stage.
A study was included if it: (i) targets a population of community-dwelling older persons (aged 60+) and/or individuals aged 50–59 at high falls risk; (ii) evaluates intervention(s) designed to reduce the number of falls or fall-related injuries; (iii) is evaluated against any comparator(s); (iv) reports outcomes of economic evaluation [32]; (v) uses a decision model [32]; and (vi) has English full text. Methodological features of models relevant to the PHMC framework were extracted by JK using a proforma and then discussed in the team regarding their relevance and importance.
Critical appraisal methods
The methodological features of included models were synthesised by their relevance to the four PHMC challenge categories. Critical appraisal first assessed the prevalence of the given feature across models, then appraised the methods used to incorporate the feature. For example, the proportion of models that accounted for productivity loss associated with falls was assessed. Then, amongst models that accounted for the loss, the range of methods used for doing so were described and compared. The methodological strengths and limitations stated by the models’ authors were used as indicators of desirable modelling practice and scope for improvement, respectively. Where relevant, the methods were also compared against those suggested in the literature informing the PHMC framework in “Challenges to public health economic modelling” section. Based on the appraisal results as well as the literature in “Challenges to public health economic modelling” section, suggestions were made regarding further methodological research in each PHMC challenge category.
Results
Search results and overview
In total, 15,730 titles and abstracts and 92 full texts were screened from which 46 decision models were identified. See the separate article for the PRISMA flow diagram and the list of studies excluded at the full-text screening stage [52].
Table 1 provides an overview of the 46 identified models. Most models (n = 25; 52.2%) targeted a general population of community-dwelling adults aged 60+ or 65+. The four types of economic analysis were: cost-effectiveness analysis (CEA); cost–benefit analysis (CBA); return-on-investment analysis (ROI); and cost-utility analysis (CUA), commonly in the form of cost per quality-adjusted life year (QALY). See Additional file 1: Table S1 for definitions of these analysis types. The two costing perspectives were public sector and societal. Some models adopted multiple analysis types and perspectives, resulting in 69 distinct analyses. CUA was most used (n = 32; 46.4%), followed by ROI and CEA (each n = 17; 24.6%), then CBA (n = 3; 4.3%). Around a third of analyses (n = 22) adopted the societal perspective.
Exercise was the most evaluated intervention type (n = 17 models), followed by multifactorial intervention (n = 13). There were four model type categories: binary decision (n = 14 models)—comparing the state of the world with and without the intervention and without transition probabilities or time cycles; static (n = 9)—all except one [85] were decision trees without time cycles; cohort-level Markov (n = 19); and patient- or individual-level Markov (n = 4). Time horizons varied between 1 year and lifetime; cycle lengths (for models with cycles) varied between 1 month and 1 year.
Critical appraisal results
The critical appraisal results are presented by the four categories of public health modelling challenges.
Capturing non-health outcomes and societal intervention costs
Eighteen models operationalised analyses from the societal perspective (see Table 1). Of these, 15 described the non-health outcomes and/or societal intervention costs incorporated in the analyses, as tabulated in Table 2. The three models not included in Table 2 conducted evaluations from the US healthcare perspective (broader than Medicare/Medicaid), which would have included private healthcare costs, but did not specify the cost type or proportion by sector [86,87,88].
Only Honkanen et al. [119] incorporated the social wellbeing loss of fracture-induced residence change from community to nursing home, expressed within a health state utility (HSU) decrement. Here, HSU values are based on a preference-based quality-adjustment scale anchored at 0 (a state equivalent to dead) and 1 (full health) which can be combined with length of life to estimate QALYs; the HSU decrements represent a move away from a more preferred health state. Other models similarly assigned utility decrements for long-term care admission, but it was unclear whether these were specifically associated with residence change or with severity of admission-related fall [89,90,91,92]. The use of HSU values to express social wellbeing is noteworthy given their narrow health dimensions. The exclusion of non-health benefits of interventions were frequently mentioned as a limitation, particularly for exercises generating social participation [93,94,95] and wellbeing gain (e.g., self-confidence) [96, 97]. On the intervention cost side, Honkanen et al. [119] expressed the social cost of hip protector use (discomfort, embarrassment) again within a HSU decrement; the impact was significant, producing an overall QALY loss from intervention for younger subgroups.
Five models incorporated OOP care expenditure: transport costs for fallers [98]; home care [99, 100]; non-specific care [101]; and cost of private insurance [102]. Of these, none incorporated private co-payments as an intervention cost. Seven incorporated intervention co-payments borne by individuals or organisations (but not OOP care expenditure): exercise enrolment [93, 103, 104]; transport cost for participants [105]; venue hire [94, 106]; and local stakeholder involvement [107].
Only Johansson et al. [107] incorporated productivity as an outcome. Specifically, the productivity value (net consumption) was assigned to older persons by age group; hip fractures would then reduce net productivity by shortening life expectancy. On the intervention cost side, Johansson et al. [107] included the time opportunity costs of unpaid volunteering and older persons’ participation. Three further models incorporated time opportunity costs of volunteers and/or participants but not productivity outcomes [95, 97, 106]. Two models mentioned time commitments by volunteers but did not apply monetary values [94, 103].
Three models incorporated informal caregiver burden as productivity loss [99, 100, 107]; none incorporated the health impact on caregivers. Likewise, none incorporated the informal caregivers’ time opportunity cost in accompanying intervention participants.
Two models—both evaluating a combined programme of environmental modifications and multifactorial intervention—discussed the intervention impact on community empowerment but did not quantify it [103, 107]. Both also perceived community involvement—community healthcare staff raising falls risk awareness [103] and local stakeholders designing and delivering interventions [107]—solely as intervention costs rather than as empowerment.
Where outcomes are generated and costs incurred outside the public healthcare system, their valuation methods should change accordingly [32]. Yet only Beard et al. [103] used the value of a statistical life to estimate the consumption value of disability-adjusted life year (DALY) burden of falls under CBA. There may also be intersectoral differences in productive efficiencies (i.e., outcome generated per resource invested), leading to intersectoral variations in cost-effectiveness thresholds [108]. Typically, public healthcare systems generate less health per input (i.e., have lower productive efficiency) than what people are willing to pay for and obtain in the private sector (p. 97–98) [32]. Hence, the cost-effectiveness threshold for comparing the incremental benefits and costs under the public sector is lower than that for comparing societal benefits and costs [108]. Incorporating this threshold differential may have changed the final decision in several models [94, 99, 100].
Overall, comprehensive incorporation of non-health outcomes and societal intervention costs is uncommon among models operationalising analyses from the societal perspective. A pressing issue is the balanced incorporation of non-health outcomes and societal intervention costs to prevent models over-estimating (if intervention costs are excluded) or under-estimating (if outcomes excluded) the cost-effectiveness of interventions.
Considering heterogeneity and dynamic complexity
Heterogeneity
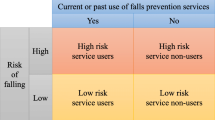
Overall, 27 (58.7%) models conducted at least one analysis related to heterogeneity. Table 3 categorises these analyses into subgroup analysis (SA), targeting analysis (TA), and analysis of heterogeneous intervention needs (IN) and specifies the relevant subgroup delineating variables.
Age and sex were the most common delineators, used in 24 models. The use of social delineators was infrequent: four models from the same research group used ethnicity [94, 109,110,111], while one used health authority region [112]. Smith et al. [85] compared different cut-off levels (i.e., targeting scenarios) based on multivariate falls risk estimated from routine care data. Osteoporosis and carotid sinus hypersensitivity were the only chronic disease delineators [95, 104, 113]; psychotropic medication use delineated intervention need in two models [104, 114]. Physical capacity delineators included mobility, functional status and vitamin D level. Five models incorporated heterogeneous intervention subgroups [104, 113,114,115,116]; of these, two incorporated non-mutually exclusive interventions [113, 115].
Pega et al. [111] was unique in characterising heterogeneity in efficacy for the same intervention across recipient subgroups: in one scenario analysis, the falls rate ratio of HAM compared to usual care was set to be 0.62 for those at high falls risk and 0.94 for low risk. Studies generally favoured the use of pooled efficacy estimates from meta-analyses: 23 of 35 models using external efficacy sourced meta-analysis estimates; however, pooled estimates can mask heterogeneity in efficacy. With some exceptions [92, 105, 111, 116], there was little effort to discern whether a single or pooled estimate would better reflect the heterogeneity in efficacy. Likewise, heterogeneity in intervention cost was poorly modelled: only Honkanen et al. [119] allowed the cost of a hip protector to vary by recipients’ functional status and residence.
An issue in several models concerned how evaluation outcomes were compared across heterogeneously sized target subgroups. Specifically, there was a need to compare both incremental cost-per-unit ratios (e.g., ICER) and aggregate outcomes; an example of the latter is incremental net monetary benefit (INMB) computed by multiplying the total incremental health (e.g., QALY) gain by the cost-effectiveness threshold to obtain its monetary equivalent and subtracting the total incremental cost. An intervention tailored to a specific subgroup may generate a very favourable cost-per-unit ratio but a low aggregate benefit due to the small subgroup size (p. 118–122) [117]. Accordingly, Day et al. [104] compared both the ICER and total falls prevented across six heterogeneously sized subgroups with different intervention needs; here, Otago exercise had the least favourable ICER (although still cost-effective) but the most favourable aggregate impact in terms of the number of hospitalised falls prevented. By contrast, Moriarty et al. [120] estimated the most favourable ICER for modification of inappropriate non-steroidal anti-inflammatory drug (NSAID) relative to benzodiazepine and proton pump inhibitor (PPI) modifications (all three dominated no modification as comparator); however, the prevalence of inappropriate NSAID use was 4.1% compared to 23.6% for PPI. Hence, if aggregate benefits are considered, PPI modification likely becomes the policy priority, not NSAID as concluded by the study. Likewise, PHE [116] estimated that HAM had the most favourable ROI and ICER (with no intervention as comparator) relative to three exercise interventions; but HAM targeted a subgroup 17 times smaller than the latter, thus generating the smallest INMB.
Dynamic complexity
Table 4 shows the time-variant falls risk factors and determinants of background health (expressed in HSU values) and comorbidity care costs incorporated in 17 models (13 cohort- and four individual-level Markov models) with time horizons longer than 5 years.
The time-variant risk factors were grouped into three categories: ‘age’, ‘falls incidence’, and ‘other’ (e.g., fear of falling). For the four individual-level Markov models, fracture risks were updated for individuals by age progression in each cycle. For the 13 cohort-level models, accounting for the age-based risk progression would have required tunnel states for each model state, but this was not mentioned or graphed. Tunnel states exist within each pre-specified Markov model state and have differing transition probabilities to other states to reflect the changes in risk that would occur over the time spent in the given model state [118]; the proportion of the Markov cohort who do not transition to another model state would instead transition to the tunnel states. Lack of tunnel states would bias the results against those who are younger at baseline: the falls risk kept low despite ageing would reduce the absolute number of falls prevented by the intervention and hence its cost-effectiveness. Fifteen incorporated fall/fracture incidence within modelled time as a risk factor, establishing a feedback loop. Only five models incorporated progression of other risk factors. Eldridge et al. [115] modelled individuals transitioning in and out of the state of fear of falling which increased the risks of hip fracture, long-term care (LTC) admission and mortality. Honkanen et al. [119] modelled transitions to functional dependence which increased the risks of hip fracture, LTC admission and mortality. Therefore, Eldridge et al. [115] and Honkanen et al. [119] captured the natural trajectory of geriatric health (using binary indicators) that interacted with fracture incidence and risk.
Only two models incorporated dynamic changes to intervention need: Honkanen et al. [119] allowed the type of hip protector to change according to functional status; Nshimyumukiza et al. [113] shifted individuals to a reactive fracture prevention pathway when a fracture occurred. It was unclear in Nshimyumukiza et al. [113] whether fracture risk screening was repeated each cycle to change the proactive intervention components. Eldridge et al. [115] did not model the progressions of factors included in the falls risk assessment tool (FRAT; e.g., mobility, chronic diseases, medication use) that determined the proactive components nor incorporate repeated risk screening after the baseline year. Deverall [94] was unique in allowing the cost of group exercise to vary dynamically from NZ$480 per person in the 1st year to NZ$62 in subsequent years for those who persist.
All models in Table 4 except OMAS [114] performed CUA. Of these, Honkanen et al. [119] was most thorough in characterising the trajectory of HSU values which progressed by age, functional status, residence and hip fracture incidence. The four individual-level models did not incorporate such geriatric health/frailty progression, but allowed severe fractures to have permanent impacts on utilities. Nine allowed utility progression by age alone, which precluded capturing the heterogeneous health progression within the same age group. Honkanen et al. [119] was again most thorough in characterising the trajectory of comorbidity care costs.
Additional file 1: Table S2 describes the entry and exit patterns for the above non-binary models. Nshimyumukiza et al. [113] was unique in incorporating incoming cohorts each year for the first 10 years. Other models mentioned the non-incorporation of incoming cohorts as a limitation that underestimated the total intervention costs and benefits [93, 104, 111]. Wilson et al. [110] and Pega et al. [111] incorporated annual probabilities of households moving in/out of modified housing which altered the need for HAM. Concerning model exit via mortality, four used fall-related and other-cause mortality rates [94, 109,110,111], while the rest used fall-related and all-cause rates, which double-counts the former. Seven faced a similar issue in double-counting fall-related LTC admission [89,90,91, 114, 115, 119, 120].
Overall, the assessment of heterogeneity was limited, confined primarily to comparisons delineated by demographic factors and binary disease or physical capacity status (e.g., mobile vs. non-mobile); the latter neglects the nature of geriatric health best characterised as a position on a continuous spectrum [1]. Likewise, the dynamic progressions in falls risk profile, intervention need, health utilities and care costs were poorly captured.
Considering theories of human behaviour and implementation
No model directly parameterised psychological and social causal mechanisms based on individual and social behavioural theories. Nevertheless, 31 (67.4%) models reported at least one implementation level, as shown in Table 5. See also Additional file 1: Table S3 for references concerning the terms used to describe the implementation levels which are distinguished by demand and supply dimensions: e.g., uptake and adoption describe demand and supply for initial access, respectively.
A notable feature was the frequent reliance on modeller assumptions to parameterise the implementation levels, which was widely acknowledged as a limitation by authors [96, 97, 104, 106, 113, 121]. Of the 18 models that reported access levels, five relied on assumptions [87, 91, 92, 112, 116]. Only Turner et al. [124] distinguished between adoption and uptake: in the main intervention scenario, professionals’ adoption of sedative de-prescribing is imperfect, and only in an alternative scenario does it become 100%; meanwhile, older persons’ uptake remains at 53% in both scenarios. Nine models reported compliance levels, four relying on assumptions [87, 106, 120, 122]. Honkanen et al. [119] uniquely applied per-protocol rather than intention-to-treat (ITT) efficacy from RCT; the adherence rate then determined the intervention effectiveness. In other models that used ITT evidence and applied compliance rates, there was a risk of confounding. For example, OMAS [114] specified the adherence rates for their interventions and seemingly applied the ITT efficacies to both adherers and non-adherers, which would underestimate the efficacy for adherers and overestimate for non-adherers. Of the 19 models that reported sustainability durations, 13 used assumptions [89, 90, 92, 95, 101, 106, 107, 110, 111, 113, 114, 116, 122]. Under long model horizons, rudimentary assumptions on intervention sustainability would produce misleading results. For example, Church et al. [90] did not allow for sustained access to ongoing interventions such as exercise, while one-off procedures such as expedited cataract surgery were assumed to generate permanent efficacy, thus significantly advantaging the latter.
Table 5 also lists the outcomes used for one-way sensitivity or scenario analyses that involved changes in implementation levels. Twelve of 31 (38.7%) models did not assess varying implementation levels, and several acknowledged this as a limitation [92, 101, 112]. Cost-per-unit ratios were the most common outcomes used (by 15 models). A key disadvantage of ratios is that their association with implementation levels depends strongly on the cost summary method, specifically whether fixed/sunk intervention costs are incorporated. If fixed costs are translated to per-participant rates, higher implementation level would raise the net intervention cost and health benefit at the constant rates such that the cost-per-unit ratio remains constant. Accordingly, models without fixed costs found that varying implementation had minimal impacts on cost-per-unit ratio [91, 93,94,95, 102, 104, 110, 111, 119]. By contrast, Comans et al. [105] incorporated fixed costs and estimated the uptake rates needed for multifactorial interventions to generate ROI ratios above one. Hence, ratios ought to be interpreted alongside aggregate outcomes to enable holistic evaluations. For example, Zarca et al. [122] found that adherence rate of 30% was sufficient to generate a favourable ICER and ruled out further information campaigns to improve adherence; but this potentially neglects the aggregate benefits foregone by low adherence.
Twelve models evaluated the effect of varying implementation on aggregate outcomes: total number of falls prevented [93, 104, 115]; incremental costs and QALYs in CUA [94, 95, 110, 111, 120, 123, 124]; and aggregate net economic saving in ROI [87, 102]. Of the latter, Howland et al. [87] estimated that increasing the uptake of multiple-component interventions from a base case rate of 50% to 75% would generate savings of $2.79 million for a population of 44,000. This represents the maximum amount the decision-maker could spend on auxiliary implementation strategies to achieve the bespoke uptake increase. Yet, models seldom discussed how the variations in implementation levels were generated, often assessing the variations under deterministic sensitivity analysis (i.e., to assess parameter uncertainty) rather than under scenario analysis as distinct intervention strategies (e.g., [94, 110, 111]).
An issue related to implementation is the presence of capacity or budget constraint which defines the feasible levels of implementation [72]; no model incorporated such constraints. PHE [116], for example, assumed that in a typical English local health authority area, around 5000 older persons would receive group exercise at any time. With a maximum of 10 participants per group, this would require 500 venues per week, which is likely beyond the venue capacity of most local health authorities. For decision-makers overseeing a specific geographical region, the sizes of the newly incoming cohorts (e.g., newly turned age 60 or 65) would affect the capacity use over time; yet, as mentioned, only Nshimyumukiza et al. [113] incorporated incoming cohorts (and only for the first 10 years).
Overall, the most pressing methodological issue regarding behaviour and implementation concerns parameterising the long-term intervention sustainability using appropriate evidence rather than modeller assumptions. Moreover, there is greater scope for conducting value of implementation (VoIM) analyses and incorporating capacity constraints to improve model credibility [72, 78].
Considering issues of equity
Only seven (15.2%) models, shown in Table 6, incorporated vulnerable subgroups based on social deprivation and/or health severity. Two potential causes of reduced capacity to benefit for these subgroups (relative to non-vulnerable peers) could be discerned from the models: (i) the double jeopardy (DJ) problem—i.e., vulnerable individuals derive lower efficacy and/or poorer implementation quality; and (ii) life expectancy differential (LED) problem—i.e., vulnerable individuals derive less QALY gain from an intervention improving HSU values due to shorter remaining life expectancy.
Only the four models from the same BODE3 research group incorporated social subgroups delineated by ethnicity (Maori vs. non-Maori) [94, 109,110,111]. All four reported lower QALY gains and higher ICERs for the Maori group. Except Boyd et al. [109], they also investigated the cause of reduced capacity to benefit: under a hypothetical scenario of equal life expectancy, the Maori group experienced higher per-capita QALY gain than the non-Maori group. Hence, the LED problem was identified as the main cause of reduced capacity. But homogenous parameters across ethnic subgroups for intervention cost, efficacy and implementation precluded analysis of the DJ problem. The latter was only narratively discussed, with reference to non-ethnic social delineators. For example, Wilson et al. [110] mentioned that HAM uptake is likely lower for low-income populations who are likelier to rent; Pega et al. [111] mentioned that public campaign to promote do-it-yourself HAM would disproportionately benefit homeowners.
Three models incorporated severity subgroups delineated by variables other than age, sex and individual falls risk factors (e.g., falls history). Eldridge et al. [115] incorporated a severity subgroup of individuals with fear of falling as indicator of generalised frailty. Fear did not influence the intervention type, efficacy, cost or uptake; hence, the DJ problem was precluded. Instead, the higher mortality risk faced by those with fear means that the LED problem was present. Another key feature is the model’s incorporation of health utility levels for health states: those with and without fear had utilities of 0.67 and 1, respectively, prior to fracture, and the same utility 0.31 after fracture; the respective utility decrements are hence 0.36 and 0.69. This improves the cost-effectiveness of fracture prevention for those without fear. Nevertheless, the model did not report any subgroup results.
Honkanen et al. [119] incorporated a severity subgroup of functionally dependent individuals who generated less favourable cost-effectiveness result than the whole population. Specifically, hip protector use no longer dominated no intervention for functionally dependent women aged 80 and 85 unlike the whole population. This could partly be attributed to the DJ problem because the dependent subgroup incurred a higher intervention cost to achieve the same efficacy as the independent. Interestingly, fracture cost was lower for the dependent, meaning that fracture prevention is less cost-effective for them. The LED likely also contributed via the higher mortality risk faced by the dependent.
Smith et al. [85] operationalised a multivariate falls risk prediction tool that included several indicators of frailty. The 1-year horizon precluded any LED problem. The model applied homogenous intervention efficacy, cost and implementation level for all frailty/risk level, removing any DJ problem. This generated potentially misleading outcomes: for example, the model estimated that only the 1.8% highest risk individuals should be referred to the intervention to achieve positive financial returns; but these individuals likely have significantly reduced capacity to benefit due to their comorbidities. The model hence likely overestimated the cost-effectiveness of targeting the most vulnerable.
No model conducted analyses that quantified the equity-efficiency trade-off. Except Boyd et al. [109], the BODE3 models only explored the hypothetical scenario of equal life expectancy across subgroups and did not evaluate intervention strategies prioritising intervention access/outcomes for the Maori subgroup. They nevertheless discussed several such equity-oriented intervention strategies: Wilson et al. [110] and Pega et al. [111] suggested analysis of HAM targeting low-income renters; Boyd et al. [109] discussed how public sector provision of cataract surgery should counteract worsening health inequity under private sector provision. They did not discuss any methodological aspects of equity analysis such as estimating the relative importance of equity and efficiency gains. For severity-based equity issues, only Honkanen et al. [119] reported the subgroup results but did not evaluate any strategy prioritising the severity subgroup. Overall, equity considerations are limited within existing models.
Suggestions for further methodological research
The results of the critical appraisal of the models by the systematic review were translated to 16 suggestions for further methodological research, sub-categorised by the four key challenges. These are shown in Table 7 alongside the textual justification for each suggestion.
Discussion
This systematic review and critical appraisal explored how 46 existing economic models of community-based falls prevention addressed four key methodological challenges associated with public health economic modelling and made methodological research suggestions that may inform future model development. The appraisal results supplement those concerning falls epidemiology, falls prevention intervention, and evaluation methods in the first part of the review results [52].
Although the four challenges were appraised separately, the significant interactions between them should be noted. Incorporation of non-health outcomes would increase the heterogeneity and dynamic complexity in analysis [1]. Wider intervention benefits and costs are closely associated with implementation quality: for example, social benefits act as uptake facilitators [5], and co-payments as barriers [46]. Likewise, long-term behavioural and implementation patterns are dynamically complex due to feedback loops (e.g., initially successful adherence reinforces persistence). Intervention need is also dynamically complex, dependent on history of previous intervention receipts; however, there is little guidance as to how intervention prescription should vary by history [5, 27, 125].
The interactions between the first three challenges and the last (i.e., equity considerations), warrant further attention. First, capturing non-health outcomes and societal intervention costs likely exacerbates the inequitable outcome differences between social- and severity-based subgroups. For example, incorporating wider consumption benefits of HAM advantages richer homeowners [110]. Incorporating productivity loss likely disadvantages the socially deprived and frail subgroups who are less likely to be in paid/unpaid employment prior to a fall. Yet excluding the wider outcomes simply masks the equity consequences (e.g., that publicly funded HAM may constitute a regressive wealth transfer towards homeowners); their inclusion is necessary to design policies that address the holistic needs of vulnerable older persons [126]. The main implication is that evaluations from the societal perspective should rigorously plan equity analyses, engaging with stakeholders both inside and outside the healthcare system to understand intersectoral equity-related priorities.
Second, there is a close overlap between considerations of heterogeneous intervention need and severity-based equity issues [85, 115, 119]. One factor influencing both intervention need and health severity is cognitive impairment, which is a key falls risk factor [5] and a frailty indicator [28]. Yet there is relatively little trial-based efficacy evidence for cognitively impaired persons, with many RCTs purposefully excluding them [29]; they also require tailored intervention attributes such as caregiver accompaniment [66]. These features likely mean that the cognitively impaired experience a substantially different intervention pathway, though there is little guidance in current guidelines [5, 27, 125], as well as a significant DJ problem. Any model targeting the general community-dwelling older population should actively incorporate the dual consideration of intervention need and severity-based inequity since it implicitly targets a sizeable cognitively impaired subgroup; e.g., 22% of UK men aged 65–84 have mild cognitive impairment [127]. Generalised frailty similarly warrants the dual consideration: tailored interventions exist that can generate positive health benefits for the frailest [128]; yet their outcomes are likely markedly worse than those of the less frail subgroups, as shown in one trial-based economic evaluation of multifactorial intervention [81]. Therefore, decision-makers aiming to implement an inclusive intervention programme benefitting the frailest should articulate their severity-based priorities beyond cost-effectiveness [54].
Third, social status and culture are known to influence geriatric health behaviour [129], and health severity can both motivate and deter intervention participation [74, 130]; there is hence another intersection between equity and behavioural and implementation considerations. Complex interventions such as proactive multifactorial intervention may face greater implementation challenges (e.g., routine risk screening, coordinating multidisciplinary team) but better reach vulnerable groups who are less likely to self-refer to voluntary programmes [131]. The consideration of aggregate outcomes in VoIM magnifies the priority setting challenges: vulnerable subgroups forming a minority would likely generate lower aggregate benefits from implementation improvements than the less vulnerable majority (even if the former’s cost-per-unit ratio is more favourable). Indeed, previous applications of the equity-oriented distributional cost-effectiveness analysis (DCEA) framework have compared alternative implementation strategies with differing impacts on efficiency and equity [82, 111, 132]. Conduct of VoIM therefore warrants equity analyses, consulting with stakeholders on the likely subgroup-specific impacts of local implementation strategies.
Consideration of the above modelling challenges holds relevance to other public health areas. Inclusion of non-health outcomes and societal intervention costs has been identified as a key methodological challenge for all geriatric public health interventions [50, 55]. Modelling for other geriatric syndromes that are symptoms of multiple age-related impairments would benefit from consideration of heterogeneity and dynamic complexity [2, 133]. Periodic risk screening to track the dynamic progression in risk and associated intervention changes is relevant to all adult age groups [134]. Diverse integrated care schemes face implementation problems that would benefit from VoIM analyses [135]. Social determinants of health inequities are present over the life course [136, 137], while consideration of disease severity is recommended for all NICE decision-making in the UK [138]. In all, any public health conceptual modelling would benefit from a systematic appraisal of existing models as conducted here for community-based falls prevention [39].
An important avenue of further research concerns the availability of data required to implement the methodological aspects highlighted by the appraisal. Forthcoming work by the current authors seeks to develop a falls prevention economic model that implements the aspects using publicly available data [139], specifically the English Longitudinal Survey of Ageing (ELSA) [140] and falls prevention RCTs. Other longitudinal surveys and electronic health records similarly contain sufficient data to explore the associations between falls, multivariate frailty, and further indicators of geriatric health [42, 141, 142]. Falls prevention RCTs can provide several key data parameters including older persons’ capability and accompanying caregivers’ health [66] and the probability of meeting physical activity targets [143]. Overall, data availability appears not to be an insurmountable obstacle, while any data issues confronted could motivate and inform further primary data collections.
A key strength of this critical appraisal is the range of the methodological challenges covered: one previous systematic review covered only the challenge of capturing non-health outcomes [50], while another covered only equity issues [51]. The range was moreover informed by a previous systematic methodological review [40], supplemented by geriatric health literature (e.g., [1, 2]). A key limitation was the appraisal’s reliance on published content; contacting modellers would have rectified methodological ambiguities in several areas. A further limitation was that the search strategy had not been validated by an expert systematic reviewer or information specialist. Nevertheless, the review achieved the most comprehensive coverage of community-based falls prevention models to date, including 26 models unidentified by previous systematic reviews in this area [49].
An important caveat is that the methodological appraisals in this article do not exhaust the range of issues relevant to falls prevention modelling but rather focus on those highlighted by the systematic methodological review as being critical for public health economic model’s credibility [40]. Further appraisal results reported in the separate article should be referred [52]. Moreover, the methodological research suggestions in Table 7 do not constitute an exhaustive and authoritative list but rather contributes to ongoing methodological discussions. Finally, the broad range of methodological features appraised meant that in-depth discussions around any specific feature were precluded; for these, the literature cited in “Challenges to public health economic modelling” section—e.g., the overview on capturing the health and wellbeing impacts on informal caregivers [61]—should be referred as starting points.
Conclusion
Existing models for economic evaluation of community-based falls preventions contain methodological limitations spanning four challenge areas relevant for public health economic modelling. The appraisal in this work can inform the conceptual modelling of future falls prevention economic models to increase their credibility, as well as highlighting aspects for further methodological research within public health economic modelling. Stakeholders for modelling should explore how the four challenges and their interactions are specifically relevant to their decision-making context.
Availability of data and materials
The extracted data from the systematic review are available from the corresponding author upon reasonable request.
Abbreviations
- CBA:
-
Cost–benefit analysis
- CEA:
-
Cost-effectiveness analysis
- CG:
-
Clinical guideline
- CUA:
-
Cost-utility analysis
- DALY:
-
Disability-adjusted life year
- DCEA:
-
Distributional cost-effectiveness analysis
- DJ:
-
Double jeopardy
- HAM:
-
Home assessment and modification
- ICER:
-
Incremental cost-effectiveness ratio
- INMB:
-
Incremental net monetary benefit
- ITT:
-
Intention-to-treat
- LED:
-
Life expectancy differential
- LTC:
-
Long-term care
- NICE:
-
National Institute for Health and Care Excellence
- NSAID:
-
Non-steroidal anti-inflammatory drug
- OOP:
-
Out-of-pocket
- PPI:
-
Proton pump inhibitor
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses#
- QALY:
-
Quality-adjusted life year
- ROI:
-
Return on investment
- VoIM:
-
Value of implementation
References
World Health Organization. World report on ageing and health. Geneva: World Health Organization; 2015.
Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780–91.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):M255–63.
Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence: unifying the approach to geriatric syndromes. JAMA. 1995;273(17):1348–53.
National Institute for Health and Care Excellence. Falls in older people: assessing risk and prevention. National Institute for Health and Care Excellence. Clinical guideline 161 (nice.org.uk/guidance/cg161). 2013.
James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT, et al. The global burden of falls: global, regional and national estimates of morbidity and mortality from the global burden of disease study 2017. Inj Prevent. 2020;26(Suppl 2):i3–11.
Gottschalk S, Konig H-H, Schwenk M, Jansen C-P, Nerz C, Becker C, et al. Mediating factors on the association between fear of falling and health-related quality of life in community-dwelling German older people: a cross-sectional study. BMC Geriatr. 2020;20(1):401.
Iglesias CP, Manca A, Torgerson DJ. The health-related quality of life and cost implications of falls in elderly women. Osteoporos Int. 2009;20(6):869–78.
Zijlstra G, Van Haastregt J, Van Eijk JTM, van Rossum E, Stalenhoef PA, Kempen GI. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing. 2007;36(3):304–9.
Kim JH. Experiences of falling and depression: results from the Korean longitudinal study of ageing. J Affect Disord. 2021;281:174–82.
Sekaran NK, Choi H, Hayward RA, Langa KM. Fall-associated difficulty with activities of daily living in functionally independent individuals aged 65 to 69 in the United States: a cohort study. J Am Geriatr Soc. 2013;61(1):96–100.
Hajek A, König HH. The onset of falls reduces perceived autonomy among middle aged and older adults. Results from a longitudinal nationally representative sample. Arch Gerontol Geriatr. 2020;90: 104115.
Schulz C, Büchele G, Rehm M, Rothenbacher D, Roigk P, Rapp K, et al. Patient characteristics as indicator for care dependence after hip fracture: a retrospective cohort study using health insurance claims data from Germany. J Am Med Dir Assoc. 2019;20(4):451-5.e3.
Drevet S, Bornu BC, Boudissa M, Bioteau C, Mazière S, Merloz P, et al. One-year mortality after a hip fracture: prospective study of a cohort of patients aged over 75 years old. Geriatrie et psychologie neuropsychiatrie du vieillissement. 2019;17(4):369–76.
Lee Y-K, Lee Y-J, Ha Y-C, Koo K-H. Five-year relative survival of patients with osteoporotic hip fracture. J Clin Endocrinol Metab. 2014;99(1):97–100.
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–90.
Tian Y, Thompson J, Buck D, Sonola L. Exploring the system-wide costs of falls in older people in Torbay. London: The King’s Fund; 2013.
Davis J, Robertson M, Ashe M, Liu-Ambrose T, Khan K, Marra C. International comparison of cost of falls in older adults living in the community: a systematic review. Osteoporos Int. 2010;21(8):1295–306.
Scuffham P, Chaplin S, Legood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol Community Health. 2003;57(9):740–4.
Sach TH, Logan PA, Coupland CA, Gladman JR, Sahota O, Stoner-Hobbs V, et al. Community falls prevention for people who call an emergency ambulance after a fall: an economic evaluation alongside a randomised controlled trial. Age Ageing. 2012;41(5):635–41.
Hoffman GJ, Hays RD, Shapiro MF, Wallace SP, Ettner SL. The costs of fall-related injuries among older adults: annual per-faller, service component, and patient out-of-pocket costs. Health Serv Res. 2017;52(5):1794–816.
Roe B, Howell F, Riniotis K, Beech R, Crome P, Ong BN. Older people and falls: health status, quality of life, lifestyle, care networks, prevention and views on service use following a recent fall. J Clin Nurs. 2009;18(16):2261–72.
Jenkyn KB, Hoch JS, Speechley M. How much are we willing to pay to prevent a fall? Cost-effectiveness of a multifactorial falls prevention program for community-dwelling older adults. Can J Aging/La Revue canadienne du vieillissement. 2012;31(2):121–37.
Lin PC, Lu CM. Hip fracture: family caregivers’ burden and related factors for older people in Taiwan. J Clin Nurs. 2005;14(6):719–26.
United Nations. Political declaration and Madrid international plan of action on ageing. Second World Asembly of Aging. 2002.
Cook J. The socio‐economic contribution of older people in the UK. Working with older people. 2011.
Public Health England. Falls and fracture consensus statement: Supporting commissioning for prevention. London: Public Health England; 2017.
Foster C, Reilly J, Jago R, Murphy M, Skelton D, Cooper A, et al. UK chief medical officers’ physical activity guidelines. Department of Health and Social Care. 2019.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012. https://doi.org/10.1002/14651858.CD007146.pub3.
Sherrington C, Fairhall NJ, Wallbank GK, Tiedemann A, Michaleff ZA, Howard K, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019. https://doi.org/10.1002/14651858.CD012424.pub2.
Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, et al. Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2018. https://doi.org/10.1002/14651858.CD012221.pub2.
Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015.
Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. Oxford: Oxford University Press; 2006.
Brennan A, Akehurst R. Modelling in health economic evaluation. Pharmacoeconomics. 2000;17(5):445–59.
Kelly MP, McDaid D, Ludbrook A, Powell J. Economic appraisal of public health interventions. London: Health Development Agency; 2005.
Weatherly H, Drummond M, Claxton K, Cookson R, Ferguson B, Godfrey C, et al. Methods for assessing the cost-effectiveness of public health interventions: key challenges and recommendations. Health Policy. 2009;93(2–3):85–92.
Cookson R, Drummond M, Weatherly H. Explicit incorporation of equity considerations into economic evaluation of public health interventions. Health Econ Policy Law. 2009;4(2):231–45.
Lorgelly PK, Lawson KD, Fenwick EA, Briggs AH. Outcome measurement in economic evaluations of public health interventions: a role for the capability approach? Int J Environ Res Public Health. 2010;7(5):2274–89.
Squires H, Chilcott J, Akehurst R, Burr J, Kelly MP. A framework for developing the structure of public health economic models. Value Health. 2016;19(5):588–601.
Squires H, Chilcott J, Akehurst R, Burr J, Kelly MP. A systematic literature review of the key challenges for developing the structure of public health economic models. Int J Public Health. 2016;61(3):289–98.
Fang X, Shi J, Song X, Mitnitski A, Tang Z, Wang C, et al. Frailty in relation to the risk of falls, fractures, and mortality in older Chinese adults: results from the Beijing longitudinal study of aging. J Nutr Health Aging. 2012;16(10):903–7.
Li G, Thabane L, Ioannidis G, Kennedy C, Papaioannou A, Adachi JD. Comparison between frailty index of deficit accumulation and phenotypic model to predict risk of falls: data from the global longitudinal study of osteoporosis in women (GLOW) Hamilton cohort. PLoS ONE. 2015;10(3): e0120144.
Clark S, Shaw C, Padayachee A, Howard S, Hay K, Frakking TT. Frailty and hospital outcomes within a low socioeconomic population. QJM. 2019;112(12):907–13.
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394(10206):1365–75.
Kwon J, Lee Y, Young T, Squires H, Harris J. Qualitative research to inform economic modelling: a case study in older people’s views on implementing the NICE falls prevention guideline. BMC Health Serv Res. 2021;21(1):1–19.
Child S, Goodwin V, Garside R, Jones-Hughes T, Boddy K, Stein K. Factors influencing the implementation of fall-prevention programmes: a systematic review and synthesis of qualitative studies. Implement Sci. 2012;7(1):91.
Bunn F, Dickinson A, Barnett-Page E, Mcinnes E, Horton K. A systematic review of older people’s perceptions of facilitators and barriers to participation in falls-prevention interventions. Ageing Soc. 2008;28(4):449–72.
McIntyre A, Mackenzie L, Harvey M. Engagement of general practitioners in falls prevention and referral to occupational therapists. Br J Occup Ther. 2019;82(2):71–9.
Kwon J, Lee Y, Squires H, Franklin M, Young T. Economic evaluation of community-based falls prevention interventions for older populations: a systematic methodological overview of systematic reviews. BMC Health Serv Res. 2022;22:1–19.
Huter K, Dubas-Jakóbczyk K, Kocot E, Kissimova-Skarbek K, Rothgang H. Economic evaluation of health promotion interventions for older people: do applied economic studies meet the methodological challenges? Cost Eff Resour Alloc. 2018;16(1):14.
Public Health England. A structured literature review to identify cost-effective interventions to prevent falls in older people living in the community. London: Public Health England; 2018.
Kwon J, Squires H, Franklin M, Lee Y, Young T. Economic models of community-based falls prevention: a systematic review with subsequent commissioning and methodological recommendations. BMC Health Serv Res. 2022;22:1–36.
Davis J, Robertson MC, Comans T, Scuffham P. Guidelines for conducting and reporting economic evaluation of fall prevention strategies. Osteoporos Int. 2011;22(9):2449–59.
Norheim OF, Baltussen R, Johri M, Chisholm D, Nord E, Brock D, et al. Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost Eff Resour Alloc. 2014;12(1):18.
Huter K, Kocot E, Kissimova-Skarbek K, Dubas-Jakóbczyk K, Rothgang H. Economic evaluation of health promotion for older people-methodological problems and challenges. BMC Health Serv Res. 2016;16(5):328.
Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist. 2002;42(1):17–23.
Scheffer AC, Schuurmans MJ, Van Dijk N, Van Der Hooft T, De Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37(1):19–24.
Sixsmith A, Sixsmith J. Ageing in place in the United Kingdom. Ageing Int. 2008;32(3):219–35.
Coast J, Flynn TN, Natarajan L, Sproston K, Lewis J, Louviere JJ, et al. Valuing the ICECAP capability index for older people. Soc Sci Med. 2008;67(5):874–82.
Baker LA, Cahalin LP, Gerst K, Burr JA. Productive activities and subjective well-being among older adults: the influence of number of activities and time commitment. Soc Indic Res. 2005;73(3):431–58.
Koopmanschap MA, van Exel NJA, van den Berg B, Brouwer WB. An overview of methods and applications to value informal care in economic evaluations of healthcare. Pharmacoeconomics. 2008;26(4):269–80.
Mello JDA, Macq J, Van Durme T, Cès S, Spruytte N, Van Audenhove C, et al. The determinants of informal caregivers’ burden in the care of frail older persons: a dynamic and role-related perspective. Aging Mental Health. 2017;21(8):838–43.
Kuzuya M, Masuda Y, Hirakawa Y, Iwata M, Enoki H, Hasegawa J, et al. Falls of the elderly are associated with burden of caregivers in the community. Int J Geriatr Psychiatry. 2006;21(8):740–5.
Hwang J, Wang L, Siever J, Medico TD, Jones CA. Loneliness and social isolation among older adults in a community exercise program: a qualitative study. Aging Ment Health. 2019;23(6):736–42.
Krol M, Brouwer W. How to estimate productivity costs in economic evaluations. Pharmacoeconomics. 2014;32(4):335–44.
Nyman SR, Ingram W, Sanders J, Thomas PW, Thomas S, Vassallo M, et al. Randomised controlled trial of the effect of Tai Chi on postural balance of people with dementia. Clin Interv Aging. 2019;14:2017.
Kelly MP, Powell JE, Bartle N. Health needs assessment. Oxford Textbook of Global Public Health. 2015.
Walker D, Aedo C. Methodological issues in assessing the cost-effectiveness of interventions to improve the health of older people. In: Ageing well, vol. 127. London: ROUTLEDGE in Association with GSE Research; 2007. p. 127–37.
Shiell A, Hawe P. Health promotion community development and the tyranny of individualism. Health Econ. 1996;5(3):241–7.
Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–68.
Sculpher M. Subgroups and heterogeneity in cost-effectiveness analysis. Pharmacoeconomics. 2008;26(9):799–806.
Earnshaw SR, Richter A, Sorensen SW, Hoerger TJ, Hicks KA, Engelgau M, et al. Optimal allocation of resources across four interventions for type 2 diabetes. Med Decis Mak. 2002;22(1_suppl):80–91.
Squires H. A methodological framework for developing the structure of Public Health economic models. Sheffield: University of Sheffield; 2014.
Schüz B, Wurm S, Warner LM, Wolff JK, Schwarzer R. Health motives and health behaviour self-regulation in older adults. J Behav Med. 2014;37(3):491–500.
Cleland C, Reis RS, Ferreira Hino AA, Hunter R, Fermino RC, Koller de Paiva H, et al. Built environment correlates of physical activity and sedentary behaviour in older adults: a comparative review between high and low-middle income countries. Health Place. 2019;57:277–304.
Yardley L, Bishop FL, Beyer N, Hauer K, Kempen GI, Piot-Ziegler C, et al. Older people’s views of falls-prevention interventions in six European countries. Gerontologist. 2006;46(5):650–60.
Tuvemo Johnson S, Martin C, Anens E, Johansson A-C, Hellström K. Older adults’ opinions on fall prevention in relation to physical activity level. J Appl Gerontol. 2018;37(1):58–78.
Fenwick E, Claxton K, Sculpher M. The value of implementation and the value of information: combined and uneven development. Med Decis Mak. 2008;28(1):21–32.
Hoomans T, Severens JL. Economic evaluation of implementation strategies in health care. Implement Sci. 2014;9(1):1–6.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43.
Matchar DB, Eom K, Duncan PW, Lee M, Sim R, Sivapragasam NR, et al. A cost-effectiveness analysis of a randomized control trial of a tailored, multifactorial program to prevent falls among the community-dwelling elderly. Arch Phys Med Rehabil. 2019;100(1):1–8.
Asaria M, Griffin S, Cookson R. Distributional cost-effectiveness analysis: a tutorial. Med Decis Mak. 2016;36(1):8–19.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097.
Royal College of Nursing. Clinical practice guideline for the assessment and prevention of falls in older people. Clinical practice guidelines. London: Royal College of Nursing; 2005.
Smith MI, de Lusignan S, Mullett D, Correa A, Tickner J, Jones S. Predicting falls and when to intervene in older people: a multilevel logistical regression model and cost analysis. PLoS ONE. 2016;11(7): e0159365.
Frick KD, Kung JY, Parrish JM, Narrett MJ. Evaluating the cost-effectiveness of fall prevention programs that reduce fall-related hip fractures in older adults. J Am Geriatr Soc. 2010;58(1):136–41.
Howland J, Shankar KN, Peterson EW, Taylor AA. Savings in acute care costs if all older adults treated for fall-related injuries completed matter of balance. Inj Epidemiol. 2015;2(1):25.
Ling C, Henderson S, Henderson R, Henderson M, Pedro T, Pang L. Cost benefit considerations of preventing elderly falls through environmental modifications to homes in Hana, Maui, Hawaii. Med J. 2008;67(3):65.
Church J, Goodall S, Norman R, Haas M. An economic evaluation of community and residential aged care falls prevention strategies in NSW. N S W Public Health Bull. 2011;22(3–4):60–8.
Church J, Goodall S, Norman R, Haas M. The cost-effectiveness of falls prevention interventions for older community-dwelling Australians. Aust N Z J Public Health. 2012;36(3):241–8.
Farag I, Howard K, Ferreira ML, Sherrington C. Economic modelling of a public health programme for fall prevention. Age Ageing. 2015;44(3):409–14.
Franklin M, Hunter RM. A modelling-based economic evaluation of primary-care-based fall-risk screening followed by fall-prevention intervention: a cohort-based Markov model stratified by older age groups. Age Ageing. 2019;49(1):57–66.
Day L, Finch CF, Harrison JE, Hoareau E, Segal L, Ullah S. Modelling the population-level impact of tai-chi on falls and fall-related injury among community-dwelling older people. Inj Prevent. 2010;16(5):321–6.
Deverall E, Kvizhinadze G, Pega F, Blakely T, Wilson N. Exercise programmes to prevent falls among older adults: modelling health gain, cost-utility and equity impacts. Inj Prevent. 2018;25(4):258–63.
Mori T, Crandall C, Ganz DA. Cost-effectiveness of combined oral bisphosphonate therapy and falls prevention exercise for fracture prevention in the USA. Osteoporos Int. 2017;28(2):585–95.
Chartered Society of Physiotherapy. The falls prevention economic model: physiotherapy commissioning support tool. In: (WSYBCSU) WaSYaBCSU, editor. 2016.
Carande-Kulis V, Stevens JA, Florence CS, Beattie BL, Arias I. A cost–benefit analysis of three older adult fall prevention interventions. J Saf Res. 2015;52:65–70.
Hektoen LF, Aas E, Luras H. Cost-effectiveness in fall prevention for older women. Scand J Public Health. 2009;37(6):584–9.
Sach TH, Foss AJ, Gregson RM, Zaman A, Osborn F, Masud T, et al. Falls and health status in elderly women following first eye cataract surgery: an economic evaluation conducted alongside a randomised controlled trial. Br J Ophthalmol. 2007;91(12):1675–9.
Sach T, Foss A, Gregson R, Zaman A, Osborn F, Masud T, et al. Second-eye cataract surgery in elderly women: a cost-utility analysis conducted alongside a randomized controlled trial. Eye. 2010;24(2):276.
Hiligsmann M, Ben Sedrine W, Bruyère O, Evers SM, Rabenda V, Reginster J-Y. Cost-effectiveness of vitamin D and calcium supplementation in the treatment of elderly women and men with osteoporosis. Eur J Public Health. 2014;25(1):20–5.
Wu S, Keeler EB, Rubenstein LZ, Maglione MA, Shekelle PG. A cost-effectiveness analysis of a proposed national falls prevention program. Clin Geriatr Med. 2010;26(4):751–66.
Beard J, Rowell D, Scott D, van Beurden E, Barnett L, Hughes K, et al. Economic analysis of a community-based falls prevention program. Public Health. 2006;120(8):742–51.
Day L, Hoareau E, Finch C, Harrison JE, Segal L, Bolton TG, et al. Modelling the impact, cost and benefits of falls prevention measures to support policy-makers and program planners. 2009.
Comans T, Brauer S, Haines T. A break-even analysis of a community rehabilitation falls prevention service. Aust N Z J Public Health. 2009;33(3):240–5.
Miller TR, Dickerson JB, Smith ML, Ory MG. Assessing costs and potential returns of evidence-based programs for seniors. Eval Health Prof. 2011;34(2):201–25.
Johansson P, Sadigh S, Tillgren P, Rehnberg C. Non-pharmaceutical prevention of hip fractures—a cost-effectiveness analysis of a community-based elderly safety promotion program in Sweden. Cost Eff Resour Alloc. 2008;6:11.
Tong T. Broadening the perspective of economic evaluation in health care—a case study in dementia care in the UK. Sheffield: University of Sheffield; 2017.
Boyd M, Kvizhinadze G, Kho A, Wilson G, Wilson N. Cataract surgery for falls prevention and improving vision: modelling the health gain, health system costs and cost-effectiveness in a high-income country. Inj Prev. 2020;26(4):302–9.
Wilson N, Kvizhinadze G, Pega F, Nair N, Blakely T. Home modification to reduce falls at a health district level: modeling health gain, health inequalities and health costs. PLoS ONE. 2017;12(9): e0184538.
Pega F, Kvizhinadze G, Blakely T, Atkinson J, Wilson N. Home safety assessment and modification to reduce injurious falls in community-dwelling older adults: cost-utility and equity analysis. Inj Prevent. 2016;22(6):420–6.
Ippoliti R, Allievi I, Falavigna G, Giuliano P, Montani F, Obbia P, et al. The sustainability of a community nurses programme aimed at supporting active ageing in mountain areas. Int J Health Plann Manag. 2018;33(4):e1100–11.
Nshimyumukiza L, Durand A, Gagnon M, Douville X, Morin S, Lindsay C, et al. An economic evaluation: simulation of the cost-effectiveness and cost-utility of universal prevention strategies against osteoporosis-related fractures. J Bone Miner Res. 2013;28(2):383–94.
Secretariat OMA. The falls/fractures economic model in Ontario residents aged 65 years and over (FEMOR). Ont Health Technol Assess Ser. 2008;8(6):1.
Eldridge S, Spencer A, Cryer C, Parsons S, Underwood M, Feder G. Why modelling a complex intervention is an important precursor to trial design: lessons from studying an intervention to reduce falls-related injuries in older people. J Health Serv Res Policy. 2005;10(3):133–42.
Public Health England. A return on investment tool for the assessment of falls prevention programmes for older people living in the community. England: Public Health England; 2018.
National Institute for Health and Care Excellence. Supporting investment in public health: review of methods for assessing cost effectiveness, cost impact and return on investment. London: NICE; 2011.
Carta A, Conversano C. On the use of Markov models in pharmacoeconomics: pros and cons and implications for policy makers. Front Public Health. 2020;8: 569500.
Honkanen LA, Mushlin AI, Lachs M, Schackman BR. Can hip protector use cost-effectively prevent fractures in community-dwelling geriatric populations? J Am Geriatr Soc. 2006;54(11):1658–65.
Moriarty F, Cahir C, Bennett K, Fahey T. Economic impact of potentially inappropriate prescribing and related adverse events in older people: a cost-utility analysis using Markov models. BMJ Open. 2019;9(1): e021832.
Tannenbaum C, Diaby V, Singh D, Perreault S, Luc M, Vasiliadis H-M. Sedative-hypnotic medicines and falls in community-dwelling older adults: a cost-effectiveness (decision-tree) analysis from a US Medicare perspective. Drugs Aging. 2015;32(4):305–14.
Zarca K, Durand-Zaleski I, Roux C, Souberbielle J, Schott A, Thomas T, et al. Cost-effectiveness analysis of hip fracture prevention with vitamin D supplementation: a Markov micro-simulation model applied to the French population over 65 years old without previous hip fracture. Osteoporos Int. 2014;25(6):1797–806.
Hirst A, Knight C, Hirst M, Dunlop W, Akehurst R. Tramadol and the risk of fracture in an elderly female population: a cost utility assessment with comparison to transdermal buprenorphine. Eur J Health Econ. 2016;17(2):217–27.
Turner JP, Sanyal C, Martin P, Tannenbaum C. Economic evaluation of sedative deprescribing in older adults by community pharmacists. J Gerontol Ser A Biol Sci Med Sci. 2020;76(6):1061–7.
Panel on Prevention of Falls in Older Persons, American Geriatrics Society, British Geriatrics Society. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–57.
Bowling A, Dieppe P. What is successful ageing and who should define it? BMJ. 2005;331(7531):1548–51.
Fish M, Bayer A, Gallacher J, Bell T, Pickering J, Pedro S, et al. Prevalence and pattern of cognitive impairment in a community cohort of men in South Wales: methodology and findings from the Caerphilly prospective study. Neuroepidemiology. 2008;30(1):25–33.
de Vries N, Van Ravensberg C, Hobbelen J, Rikkert MO, Staal J, Nijhuis-Van Der Sanden M. Effects of physical exercise therapy on mobility, physical functioning, physical activity and quality of life in community-dwelling older adults with impaired mobility, physical disability and/or multi-morbidity: a meta-analysis. Ageing Res Rev. 2012;11(1):136–49.
McMunn A, Breeze E, Goodman A, Nazroo J, Oldfield Z. Social determinants of health in older age. In: Marmot M, Wilkinson R, editors. Social determinants of health. 2nd ed. Oxford: Oxford Scholarship Online; 2009.
Dickinson A, Horton K, Machen I, Bunn F, Cove J, Jain D, et al. The role of health professionals in promoting the uptake of fall prevention interventions: a qualitative study of older people’s views. Age Ageing. 2011;40(6):724–30.
Day LM. Fall prevention programs for community-dwelling older people should primarily target a multifactorial intervention rather than exercise as a single intervention. J Am Geriatr Soc. 2013;61(2):284–5.
Collins B, Kypridemos C, Cookson R, Parvulescu P, McHale P, Guzman-Castillo M, et al. Universal or targeted cardiovascular screening? Modelling study using a sector-specific distributional cost effectiveness analysis. Prev Med. 2020;130: 105879.
Afzali HHA, Karnon J, Theou O, Beilby J, Cesari M, Visvanathan R. Structuring a conceptual model for cost-effectiveness analysis of frailty interventions. PLoS ONE. 2019;14(9): e0222049.
Breeze P, Thomas C, Squires H, Brennan A, Greaves C, Diggle PJ, et al. The impact of Type 2 diabetes prevention programmes based on risk-identification and lifestyle intervention intensity strategies: a cost-effectiveness analysis. Diabet Med. 2017;34(5):632–40.
Kumpunen S, Edwards N, Georghiou T, Hughes G. Why do evaluations of integrated care not produce the results we expect? Int J Care Coord. 2020;23(1):9–13.
Shiell A. Still waiting for the great leap forward. Health Econ Policy Law. 2009;4(2):255–60.
Marmot M. The health gap: the challenge of an unequal world. New York: Bloomsbury Paperbacks; 2015.
National Institute for Health and Care Excellence. Report on NICE Citizens Council meeting: Quality Adjusted Life Years (QALYs) and the severity of illness. National Institute for Health and Care Excellence; 2008.
Kwon J, Squires H, Young T. Economic modelling of NICE recommended community-based falls prevention: efficiency, equity and capacity implications. In: Publication F, editor. 2022.
English longitudinal study of ageing. ELSA dataset waves 0 to 9; 2019.
Clegg A, Bates C, Young J, Ryan R, Nichols L, Ann Teale E, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45(3):353–60.
Kojima G, Kendrick D, Skelton DA, Morris RW, Gawler S, Iliffe S. Frailty predicts short-term incidence of future falls among British community-dwelling older people: a prospective cohort study nested within a randomised controlled trial. BMC Geriatr. 2015;15(1):155.
Iliffe S, Kendrick D, Morris R, Masud T, Gage H, Skelton D, et al. Multicentre cluster randomised trial comparing a community group exercise programme and home-based exercise with usual care for people aged 65 years and over in primary care. Health Technol Assess (Winchester, England). 2014;18(49):vii–105.
Agartioglu Kundakci G, Yilmaz M, Sozmen MK. Determination of the costs of falls in the older people according to the decision tree model. Arch Gerontol Geriatr. 2020;87: 104007.
Albert SM, Raviotta J, Lin CJ, Edelstein O, Smith KJ. Cost-effectiveness of a statewide falls prevention program in Pennsylvania: healthy steps for older adults. Am J Manag Care. 2016;22(10):638–44.
Alhambra-Borrás T, Durá-Ferrandis E, Ferrando-García M. Effectiveness and estimation of cost-effectiveness of a group-based multicomponent physical exercise programme on risk of falling and frailty in community-dwelling older adults. Int J Environ Res Public Health. 2019;16(12):2086.
Lee RH, Weber T, Colon-Emeric C. Comparison of cost-effectiveness of vitamin D screening with that of universal supplementation in preventing falls in community-dwelling older adults. J Am Geriatr Soc. 2013;61(5):707–14.
McLean K, Day L, Dalton A. Economic evaluation of a group-based exercise program for falls prevention among the older community-dwelling population. BMC Geriatr. 2015;15:33.
Poole CD, Smith JC, Davies JS. The short-term impact of vitamin D-based hip fracture prevention in older adults in the United Kingdom. J Endocrinol Invest. 2014;37(9):811–7.
Poole CD, Smith J, Davies JS. Cost-effectiveness and budget impact of empirical vitamin D therapy on unintentional falls in older adults in the UK. BMJ Open. 2015;5(9): e007910.
van der Velde N, Meerding WJ, Looman CW, Pols HA, van der Cammen TJ. Cost effectiveness of withdrawal of fall-risk-increasing drugs in geriatric outpatients. Drugs Aging. 2008;25(6):521–9.
Li G, Ioannidis G, Pickard L, Kennedy C, Papaioannou A, Thabane L, et al. Frailty index of deficit accumulation and falls: data from the global longitudinal study of osteoporosis in women (GLOW) Hamilton cohort. BMC Musculoskelet Disord. 2014;15:185.
Brennan A, Chick SE, Davies R. A taxonomy of model structures for economic evaluation of health technologies. Health Econ. 2006;15(12):1295–310.
Acknowledgements
Not applicable.
Funding
Mr. Joseph Kwon was supported by the Wellcome Trust [108903/B/15/Z].
Author information
Authors and Affiliations
Contributions
All authors were involved in study conceptualisation. JK wrote the first manuscript draft. HS, MF and TY were involved in the writing of subsequent drafts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No approval or consent was needed.
Consent for publication
No consent was needed.
Competing interests
There are no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Definitions of analysis types in economic evaluation. Table S2. Dynamic entry and exit patterns for non-binary models with horizons longer than 5 years. Table S3. Implementation levels by demand and supply dimensions.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kwon, J., Squires, H., Franklin, M. et al. Systematic review and critical methodological appraisal of community-based falls prevention economic models. Cost Eff Resour Alloc 20, 33 (2022). https://doi.org/10.1186/s12962-022-00367-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12962-022-00367-y