Abstract
Background
Ovarian tissue transplantation can restore fertility in young cancer survivors, however the detrimental loss of follicles following transplantation of cryopreserved ovarian tissue is hampering the efficiency of the procedure. This study investigates whether needle puncturing prior to transplantation can enhance revascularization and improve follicle survival in xenotransplanted human ovarian cortex.
Methods
Cryopreserved human ovarian cortex pieces (N = 36) from 20 women aged 24–36 years were included. During the thawing process, each piece of tissue was cut in halves; one half serving as the untreated control and the other half was punctured approximately 150–200 times with a 29-gauge needle. The cortex pieces were transplanted subcutaneously to immunodeficient mice for 3, 6 and 10 days (N = 8 patients) and for 4 weeks (N = 12 patients). After 3, 6 and 10 days, revascularization of the ovarian xenografts were assessed using immunohistochemical detection of CD31 and gene expression of angiogenic factors (Vegfα, Angptl4, Ang1, and Ang2), and apoptotic factors (BCL2 and BAX) were performed by qPCR. Follicle density and morphology were evaluated in ovarian xenografts after 4 weeks.
Results
A significant increase in the CD31 positive area in human ovarian xenografts was evident from day 3 to 10, but no significant differences were observed between the needle and control group. The gene expression of Vegfα was consistently higher in the needle group compared to control at all three time points, but not statistically significant. The expression of Ang1 and Ang2 increased significantly from day 3 to day 10 in the control group (p < 0.001, p = 0.0023), however, in the needle group this increase was not observed from day 6 to 10 (Ang2 p = 0.027). The BAX/BCL2 ratio was similar in the needle and control groups. After 4-weeks xenografting, follicle density (follicles/mm3, mean ± SEM) was higher in the needle group (5.18 ± 2.24) compared to control (2.36 ± 0.67) (p = 0.208), and a significant lower percentage of necrotic follicles was found in the needle group (19%) compared to control (36%) (p = 0.045).
Conclusions
Needle puncturing of human ovarian cortex prior to transplantation had no effect on revascularization of ovarian grafts after 3, 6 and 10 days xenotransplantation. However, needle puncturing did affect angiogenic genes and improved follicle morphology.
Similar content being viewed by others
Background
Cryopreservation and autotransplantation of human ovarian cortex tissue has gained ground worldwide as the only fertility preserving option for prepubertal girls and patients in need of immediate cancer treatment [1,2,3,4]. Since the first live birth in 2004 [5], the number of live births has now exceeded 200 and live births rates in women transplanted with ovarian tissue range from 20–30% [6,7,8,9,10,11]. Following ovarian tissue transplantation (OTT) an endocrine recovery of 72–95% has been reported [6]. However, the patients present with consistently low AMH after OTT reflecting the low number of surviving follicles in the ovarian grafts [1, 3, 12,13,14,15,16]. During cryopreservation and thawing less than 20% of the primordial follicles are lost, however, following transplantation 60–80% or more of the follicles are lost during grafting [17,18,19,20,21]. This massive follicle loss observed after OTT is hampering the efficiency of the procedure [22,23,24], and increasing the follicle survival after OTT could improve reproductive outcomes in transplanted women.
The massive follicle loss in the ovarian grafts is due to ischemia and hypoxia and the injury following reperfusion early in the post-transplantation period [22,23,24]. Multiple approaches have aimed to reduce the damage caused by hypoxia and ischemia/ reperfusion injury in ovarian tissue with varying results [21, 25,26,27]. Studies have attempted to accelerate and increase the revascularization of the ovarian graft by the use of vascular endothelial factor (VEGF), basic fibroblast growth factor (bFGF), Er:YAG laser and adipose stem cells to shorten the period of ischemia and to avoid reperfusion failure [21, 28,29,30,31,32]. Revascularization of the ovarian tissue is crucial for its survival and several studies have shown a correlation between improved angiogenesis and higher follicle survival [33, 34], which has made the revascularization process a target of possible optimization of follicle survival after OTT. In cardiovascular surgery, controlled tissue damage has been utilized to induce angiogenesis for decades [35]. Moreover, laser channels has been shown to induce angiogenesis in ischemic animal models [36,37,38,39,40,41]. In a porcine model tissue damage done by needle punctures was able to induce angiogenesis at the same level as laser treatment [42]. The aim of this study was to study if controlled tissue damage, through mechanical injury using needle puncturing, could induce angiogenesis in xenotransplanted human ovarian tissue and subsequently improve follicle survival and morphology.
Materials and Methods
Human ovarian tissue
Donated ovarian cortex tissue from 20 women aged 24–36 years (mean ± SD; 30.6 ± 3.7) was included in this study. The ovarian cortex tissue was cryopreserved for fertility preservation using slow-freezing as previously described [20], at the Laboratory of Reproductive Biology, Copenhagen University Hospital, Denmark between 2001–2011. Indications for fertility preservation for these women were breast cancer (N = 10), Hodgkin's lymphoma (N = 2), brain cancer (N = 1), sarcoma (N = 1), benign disease (N= 1), and other cancers (N = 5).
Animals
Ten female immunodeficient Naval Medical Research Institute (NMRI)-NUDE mice aged 6–7 weeks were purchased from Taconic, Denmark. Mice were housed in groups, fed pellets and water ad libitum, and kept under controlled 12-h light/12-h dark cycles at 20–22 °C. One week after arrival the mice were anesthetized using Zoletil (Virbac, France), xylazin (Scanvet, Denmark), and butorphanol (Zoetis, New Jersey) before they were ovariectomized to increase endogenous FSH levels. Post-operative analgesia in the form of buprenorphine (Temgesic, Indivior UK Limited, UK) and carprofen (Norodyl, ScanVet, Denmark) was used. Two weeks after ovariectomy either six (4-week study) or eight pieces (3, 6, 10 days study) of human ovarian cortex were transplanted subcutaneously to the back of each mouse. After surgery the mice were single housed for at least 1 week. Euthanasia was performed by cervical dislocation, upon graft retrieval.
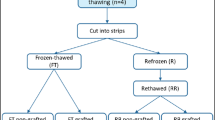
Thawing and needle puncturing
Thirty-six pieces of cryopreserved ovarian tissue was thawed according to standard clinical procedure [43]. Each cortex piece (approximately 5 × 5x2 mm) was cut into two halves, after the initial thawing, where one half functioned as the untreated control and the other half as the piece receiving needle puncturing. The mechanical injury treatment in the form of needle puncturing was performed during the second half of the thawing procedure, without prolonging the thawing process. The treatment was performed by impaling the cortex piece with a 29-gauge needle 150–200 times, to ensure that the whole tissue piece was covered with small puncture wounds, see Fig. 1. A29-gauge needle (0.337 mm) was chosen to inflict small puncture wounds and to avoid removal of tissue during the puncturing. After treatment both treated and untreated tissue pieces were processed through the rest of the thawing process.
Needle puncturing of human ovarian cortex tissue prior to transplantation. Periodic acid-Shiff (PAS) stained section from cryopreserved and thawed human ovarian cortex tissue. (a) Human ovarian cortex tissue with no needle punctures, serving as the untreated control. (b) Needle punctured human ovarian cortex, showing holes throughout the tissue. Scale bar = 200 μm
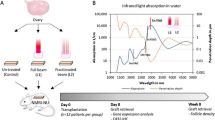
Experimental design and xenotransplantation
The experimental design is presented in Fig. 2. After thawing and preparation of the cortex pieces, the pieces were directly transplanted to ovariectomized NMRI-NUDE mice. Two separate xenograft studies were performed in parallel to evaluate the effect of mechanical injury by needle puncturing during short-term (3, 6 and 10 days) and long-term (4 weeks) xenografting compared to an untreated control. Grafts were retrieved after 3, 6 and 10 days to evaluate the critical revascularization window of the ovarian cortex xenograft (N = 8; 2 cortex pieces from 8 patients, 8 xenografts per mouse). The 4-week setup was performed for follicle density evaluation because at this time point, atretic follicles has been reabsorbed and only surviving follicles permeate the ovarian xenografts (N = 12; 1 cortex piece from 12 patients, 6 xenografts per mouse). Grafts retrieved after short-term xenotransplantation on day 3, 6 and 10, were evaluated for gene expression by quantitative reverse transcription PCR (qRT-PCR) and revascularization by immunohistochemistry (IHC). Follicle counts and morphological assessment was evaluated in the 4-week xenografts.
Experimental setup. Cryopreserved ovarian cortex tissue from 20 patients was thawed and cut into two halves with one half receiving needle puncturing and the other half serving as the untreated control. The cortex pieces were xenografted to immunodeficient mice. Grafts was retrieved after 3, 6 and 10 days (N = 8) for immunohistochemistry and gene expression analysis, and after 4 weeks for histological analysis of follicle density and morphology. (a) CD31 staining after 10 days of xenografting from control group. Scale bar = 250 µm. (b) PAS-stained section from 4-week xenografted ovarian tissue showing representative follicles. Scale bar = 100 µm
Graft retrieval and histological processing
Grafts were dissected from the mice and cleaned for surrounding murine tissue. Grafts retrieved after 3, 6 and 10 days were cut into half; one half for qRT-PCR was snapfrozen and stored at -80ºC, and the other half was fixated in 4% paraformaldehyde (PFA) for IHC analysis. The grafts retrieved after 4 weeks were fixed in Bouin’s solution for histological evaluation. The fixation was done overnight, then dehydrated and embedded in paraffin for sectioning. For IHC the samples were sectioned at 5 μm thickness, and for follicle evaluation the samples were sectioned at 10 μm thickness for Periodic-Acid-Schiff (PAS) staining.
Quantitative RT-PCR
The human ovarian cortex tissue was homogenized, and RNA-isolation, reverse transcription and qRT-PCR was performed as previously described [26]. In brief, samples were soaked in -80 °C Invitrogen™ RNAlater™-ICE Frozen Tissue Transition Solution (Cat. No. AM7030, ThermoFisher Scientific) overnight and transferred to RLT lysis buffer (Cat. No. 79216, Qiagen) with β-mercaptoethanol. Samples was homogenized using a Qiagen TissueLyser II (Cat. No. 85300) and RNA-isolation was performed with a RNeasy mini kit (Cat. No. 74106, Qiagen) (Silica spin columns: Cat. No 1920–250, EpochLifeScience). Isolated RNA was used to do first-strand cDNA synthesis using the High Capacity cDNA Reverse Transcription Kit (Cat. No. 4368814, Applied Biosystems, ThermoFisher Scientific, Carlsbad, CA, USA) following manufacturer’s instructions. For qRT-PCR analysis TaqMan technology (Applied Biosystems) using TaqMan® fast advanced master mix (Cat. No. 4444964, ThermoFisher Scientific). Predesigned TaqMan® gene expression assays were performed using following genes: Murine Vascular Endothelial Growth Factor Alpha (Vegfα),Angiopoietin 1 (Angpt1), Angiopoietin 2 (Angpt2), Angiopoietin-like 4 (Angptl4) and human B-Cell Lymphoma 2 (BCL2) and BCL-2 associated X protein (BAX), (probe-id: Vegfα, Mm00437306_m1; Angpt1, Mm00456503_m1; Angpt2, Mm00545822_m1; Angptl4, Mm00480431_m1; BCL2, Hs00608023_m1; BAX, Hs00180269_m1). Glyceraldehyde 3-phosphatdehydrogenase (Gapdh/GAPDH) was used as endogenous control for both murine and human gene expression assays [44] (probe-id: GAPDH, Hs02786624_g1; Gapdh, Mm99999915_m1). The cDNA samples were amplified in duplicates using the LightCycler®480 quantitative PCR instrument (Roche, version 1.5.0.39) as previously described [21, 26].
Immunohistochemical analysis
To analyse the revascularization of the xenografts, the endothelial cell marker CD31 was used to visualize murine blood vessels. Four sections from each graft were stained. A murine liver section was included as a positive control, and non-grafted human ovarian tissue was used as a negative control. The IHC analysis was performed as described previously [21, 26]. In brief, sections were de-paraffinized, rehydrated and antigen retrieval was performed using 10 mM sodium citrate (pH 6), following blocking using horse blocking serum (Vector Laboratories, Burlingame, CA, USA) and blocking of endogenous activity with 3% H2O2. Next, monoclonal anti-rabbit CD31 (Pecam-1) primary antibody (catno.: 77699, Cell Signaling Technology, Herlev, Denmark. Dilution: 1:100) diluted in 1% bovine serum albumin (1:100) was added to the slides and incubated overnight at 4 °C in a humid chamber. The following day the sections were incubated with the secondary antibody (ImmPRESS™ HRP Horse Anti-Rabbit IgG Polymer Detection Kit, Peroxidase, Cat. No. MP-7401, Vector Laboratories, Burlingame, CA, USA), washed and staining was visualized with 3.3′-diaminobenzidine tetrahydrochloride (DAB + Substrate Chromogen System, Dako, Glostrup, Denmark) and briefly dipped in diluted (1:3 water) Mayers Hematoxylin. IgG-negative controls were performed by excluding the primary and only using antibody dilution buffer. Digital pathology using Whole Slide Imaging (WSI) technology and the Visiopharm Author™ module was used to quantify the CD31-positive endothelial area and the number of vessels per mm2. The scanning of the slides was performed using the NanoZoomer S360 digital slide scanner with magnification × 40 and one focal point. Scanned WSI files were analysed in the Visiopharm Integrator System (VIS) using the APP via the Visiopharm Author™ module. The APP used has been described earlier [21, 45]. The APP automatically recognized the tissue as the ROI, and afterwards murine host tissue was manually excluded before running the APP. Vessels were subdivided into three categories according to size: micro vessels (< 300 µm2), small vessels (300–1000 µm2) and large vessels (> 1000–3000 µm2). Heatmaps were generated for each section to visualize and highlight the CD31 positive areas in the ovarian tissue xenografts (Fig. 3).
Follicle density and morphology
Follicle density was evaluated in the xenografts after 4 weeks. Only morphological ‘normal’ follicles with clear nucleus were counted, and follicles were defined and counted as previously described [26]. Primordial follicles were characterized by an oocyte surrounded by a single layer of flat granulosa cells. Primary follicles as oocytes surrounded by a layer of cuboidal granulosa cells, and secondary with two or more layers of cuboidal granulosa cells [46]. Morphologically, follicles were subcategorized as healthy follicles or atretic follicles [47, 48]. For area measurement Olympus BH-2 microscope with Visiopharm Integrator System software (Visiopharm, Hoersholm, Denmark, version 4.6.1779) was used. Density was calculated by the total number of follicles and the volume of the graft based on the area measurements. Follicle morphology was subcategorized (healthy or atretic), percentages from total number of the subcategories was used to visualize the data (Fig. 6).
Statistical analyses
Statistical analysis was performed using R version 4.2.1. (R Foundation for Statistical Computing, Vienna, Austria) (linear mixed model, multiple comparison Tukey post hoc). Gene expression, CD31 positive area (%), and follicle morphology data was log transformed, before analyzing data. All analyses comparing control and treatment with respect to gene expressions, CD31 positive areas, vessel densities, follicle densities and morphology were analysed with a linear mixed-effects model with patient as a random effect as each woman contributes with more than one sample in the study. Differences between individual groups were analysed using a Tukey post hoc test. P-values < 0.05 were considered significant, p > 0.10 as tendencies.
Results
Revascularization
The murine CD31 area in the human ovarian cortex tissue was determined after 3, 6 and 10 days of xenografting with or without needle puncturing prior to transplantation. The CD31 positive area was calculated as the percentage of the total section area, and the CD31 density was calculated as the number of vessels per mm2. Furthermore, heatmaps was generated to make a visual representation of where the CD31 positive areas was located in the tissue (Fig. 3). There was a significant increase in the CD31 area from day 3 until day 10 with a dramatic increase in the CD31 area between day 6 and day 10 (Fig. 4a). In the 3-day xenografts there was an average of 0.02 ± 0.01% CD31 positive area in the needle group and 0.05 ± 0.02% in the control group. In the 6-day xenografts there was an average of 0.31 ± 0.11% CD31 positive area in the needle group and 0.34 ± 0.08% in the control group. For the 10-day xenografts there was an average of 2.8 ± 0.56% CD31 positive area in the needle group and 3 ± 0.56% in the control group. No significant differences were found in CD31 positive area between the control and needle group.
Revascularization of human ovarian xenografts after 3, 6 and 10 days. (a) Graph showing mean CD31 positive area of total section area (%) from each timepoint and group (mean ± SEM). (b) Graph showing vessel density from each timepoint and group, lines indicate significant difference between timepoints but no treatment effect
The vessel density (vessels/mm2) on day 3 was 10.26 ± 6.08 vessels/mm2 for the control group and 5.62 ± 3.47 vessels/mm2 for the needle group (Fig. 4b). On day 6 the vessel density was 32.13 ± 19.74 vessels/mm2 for the control group and 48.27 ± 42.7 vessels/mm2 for the needle group. The vessel density was 552.9 ± 337.5 vessels/mm2 for the control group and 326.4 ± 116.39 vessels/mm2 for the needle group on day 10, however, there was no significant difference between needle and control group at any timepoint (p = 0.223, p = 0.377 and p = 0.626). There was a significant increase in vessel density between the different timepoints in both groups (p < 0.05).
The APP subdivided the CD31 positive areas into categories according to size: micro vessels (< 300 µm2), small vessels (300–1000 µm2) and large vessels (> 1000–3000 µm2). The distribution of between the subgroups was not different at any timepoint and the main proportion of vessels was micro vessels (97–88%). Table 1 includes the data from CD31 and the distribution of the subgroups.
Expression of angiogenic and apoptotic genes
Gene expression of angiogenic and apoptotic markers was evaluated in human ovarian tissue after 3, 6 and 10 days xenografting. The expression of murine Ang1 and Ang2 had similar patterns of expression over the different time points for both the needle and control group (Fig. 5a+ b). In the control group both genes increased from day 3, to day 6 and to day 10, however, in the needle group the expression of Ang1 and Ang2 did not increase from day 6 to day 10 but remained at the level of day 6 (p < 0.001, p = 0.027). The gene expression of murine Vegfα showed a tendency toward a higher expression in the needle group compared to the control group at all three timepoints (Fig. 5c), and for day 6 this difference was almost significant (p = 0.051). The expression of murine Angptl4 was similar on day 3 and 6 (Fig. 5d), but there was a decrease from day 6 to day 10 in both control and needle groups and the decrease was significant for the needle group (p = 0.043). The ratio of human BAX/BCL2 was similar at all three time points and there was no difference between the needle and control groups (Fig. 5e).
Expression of angiogenic and apoptotic genes in human ovarian xenografts after 3, 6 and 10 days. (a-d) Relative expression of the murine angiogenic genes: Angiopoetin 1 (Ang1); Angiopoetin 2 (Ang2); vascular endothelial growth factor alpha (Vegfα); Angiopoetin-like-4 (Angptl4). (e) Ratio of human anti- and- pro- apoptotic factors B-cell lymphoma2 (BCL2) and Bcl-2-associated X protein (BAX). Data presented as (mean ± SEM), and significant differences between timepoints are indicated by lines and symbols represent significant treatment effect
Follicle density and morphology
The xenografted ovarian tissue retrieved after 4 weeks was used to evaluate the morphology and the total number of follicles in each graft (Fig. 6). A total of 1150 follicles were counted. Based on the follicle number and the volume of the graft, the follicle densities were estimated (Fig. 6a). The mean follicle density in the xenografted needle treated tissue was 5.18 follicles/mm3 ± 2.24 with a range of 0.3 to 26.0 follicles/mm3, compared to a density of 2.36 follicles/mm3 ± 0.67 with a range of 0.3 to 5.7 follicles/mm3 in the xenografted controls. Moreover, 7 out of 12 patients had a higher follicle density in the needle group compared to the control. These results showed a 1.7-fold higher follicle density for the treatment group compared to the grafted controls, however this difference was not significant (p = 0.208) (Fig. 6b). There was no significant difference between follicle stages in the two groups, with 93–97% of all follicles counted being primordial follicles. After morphological assessment, 292 out of the total 1150 follicles were categorized as atretic. For the needle group 19% of the follicles was atretic and for the grafted control it was 36% (Fig. 6e), and this difference was significant (p = 0.045).
Follicle density and morphology in human ovarian xenografts after 4 weeks. (a) Follicle density for control and needle group after 4-week xenografting. Each dot represents a patient, and values are shown as number follicles per mm3 (mean ± SEM). (b) Follicle density given in fold change within paired samples from the same patient. (c, d) PAS-staining showing representative examples of follicles (scale bar = 100 µm) in the control (c) and needle group (d). (e) Follicle morphology shown in percentage of total number of follicles. Symbol represent significant treatment effect
Discussion
This is the first study investigating if mechanical injury by needle puncturing could increase revascularization and hereby follicle survival in xenotransplanted human ovarian tissue. Current results showed no statistically significant differences in murine vessel density in human ovarian xenografts after needle puncturing compared to untreated control grafts. However, gene expression data did show differences in the expression patterns of angiogenic factors indicating an effect of the needle puncturing on the regulation of these genes. Furthermore, a higher follicle survival was observed in the needle group compared to control, although not statistically significant, and there was a significant difference in morphology, where the needle group had more morphological healthy follicles compared to control. Taken together our findings indicate that needle puncturing does not directly increase revascularization of ovarian xenografts, but it appears to affect the expression of angiogenic genes and has a positive effect on the follicle morphology.
Without vascular re-anastomosis, the tissue grafted is solely dependent on the development and invasion of new blood vessels. Xenografting studies has previously shown that the host is primarily responsible for revascularization of the xenografted human ovarian cortex [49]. And research in rodents has shown that the first signs of revascularization is observed two to three days after transplantation and stabilization is achieved after a little more than a week [49,50,51]. As expected, we observed very little murine vessel formation on day 3, confirming that this time point shows the initial vessel formation, this also correlates with another study which could not measure the partial pressure of O2 before day 3 in xenografted human ovarian tissue [52]. After 6 days we observed an increase in vessel formation compared to day 3 xenografts, however, the observed increase was not significantly higher. Between day 6 and 10 we observed a significant increase in vessel density in the human ovarian xenografts, reaching a vascularized area of approximately 3% of the grafts, which is comparable with our previous study [21]. These results show that the main vascularization of the grafted ovarian tissue occurs between day 6 and 10, confirming that areas of the graft are subjected to prolonged ischemia and hypoxia lasting up to at least 6 days. These results together with our previous findings [21] indicate that the burst in vessel formation occurs after 6 to 10 days, showing that the burst in vascularization happens during a short window of two to three days, giving us insight at which time point the ischemia/ reperfusion injury is the most intense. Furthermore, current results did not show any difference in vessel density between the needle group and control group, and we therefore conclude that needle puncturing did not increase revascularization of xenografted human ovarian tissue. In our previous study we used Er:YAG laser to induce controlled tissue damage in human ovarian cortex prior to xenotransplantation, and we found a significant decrease in revascularization and follicle survival compared to control after grafting which indicated that this form of tissue damage was detrimental to the graft [21]. Our current results using needle puncturing showed no signs of detrimental effects on revascularization, follicle survival or the ratio of BAX/BCL2, demonstrating that this is not a harmful procedure.
The gene expression data of Vegf, did show a tendency toward a treatment effect on day 6, and there was a higher expression level in the needle group compared to control at the other time points. Moreover, there was a consistent and similar expression on all time points, showing that Vegfα is expressed in the human ovarian tissue early and consistently after transplantation. The expression of Ang1 and Ang2 had similar patterns, which was surprising due to their opposite nature. ANG1 and ANG2 act through the same tyrosine kinase receptor, Tie-2. They both have pro-angiogenic effects in the presence of VEGF, however they exert opposite effects upon receptor binding. ANG1 stabilizes the blood vessels formed through the actions of VEGF [53], whereas ANG2 destabilizes and in the presence of VEGF is important for endothelial cell proliferation and migration [54]. If VEGF is not present ANG2 has antagonizing effects and leads to vessel destabilization followed by regression and endothelial cell death [55,56,57]. Moreover, ANG1 and ANG2 is an intricate and complex balance important for angiogenesis and has been shown to be important for follicular angiogenesis, ovulation, and corpus luteum formation [58]. The observed increase of Ang1 and Ang2 could be explained by the increase in angiogenic processes, however, Ang2 is also increased and important during inflammation and hypoxia [59,60,61], which could explain the increase of Ang2 expression from day 3, 6 and also day 10 for the control group. However, the same increase was not observed for the needle group, which is consistent with our previous results using the Er:YAG laser [21]. ANGPTL4 has been proposed to have the same context dependent pro- and anti-angiogenic effect as ANG2 [62,63,64], and also having the same co-dependent relationship with VEGF to be proangiogenic [65]. Furthermore, ANGPTL4 is important for wound healing and expression is stimulated by hypoxia [64, 66]. Angptl4 was similarly expressed on day 3 and 6, but there was observed a decrease for both groups from day 6 to day 10, which could indicate the first pro-angiogenic period, where wound healing and revascularization is occurring stimulated by the hypoxic period, where on day 10 there may be a stabilization which leads to the decrease in Angptl4 expression. Taken together, the results indicate that the needle puncturing did affect the expression of angiogenic genes, and it illustrates the complexity of the revascularization process.
Current results showed significantly fewer atretic follicles and a tendency toward a higher follicle density in the needle group compared to the control group. Moreover, no signs of follicle activation were observed in the needle punctured tissue as the vast majority of follicles were primordial follicles (97%) which was similar to the control group (93%). These results is comparable to our previous study where the Er:YAG laser treatment resulted in a lower follicle survival, however, the proportion of follicles in the different stages did not differ and did not suggest follicle activation in the laser treated group compared to control [21]. The effect on the follicle survival cannot be explained by a higher revascularization of the tissue, however we did observe an effect on the angiogenic genes, showing that the needle puncturing did affect the gene expression in the xenografted tissue. Therefore, it is plausible that other signaling pathways associated with wound healing can be affected by the needle puncturing and contribute to the beneficial effects on follicle survival. Furthermore, controlled tissue damage in the form of needle puncturing can to some degree be compared with tissue fragmentation, because both methods inflict mechanical injury to the tissue. De Roo and colleagues' found that fragmentation of human ovarian tissue before culture resulted in activation of primordial follicles through the hippo and PI3K/Akt pathway [67]. Furthermore, ovarian fragmentation has been studied as a way to activate follicle growth as treatment for premature ovarian insufficiency [68]. However, a study by Lunding and colleagues did not find the same effect of fragmentation when human ovarian tissue was transplanted to immunodeficient mice for 6 weeks as no significant differences in follicle stages were reported [69]. These studies demonstrate that there are contradicting results regarding follicle activation following ovarian tissue fragmentation or disruption. Taken together, there is evidence that the way the mechanical injury is performed influences the outcome, and that is also varies between tissue types [21, 42, 70]. In this study, the mechanisms behind the positive effects on follicle survival and morphology induced by the needle puncturing cannot be explained by increased revascularization which warrants further investigations to uncover potential mechanisms and to investigate the possibilities with mechanical injury.
Conclusion
Needle puncturing of thawed human ovarian tissue prior to transplantation was not able to increase revascularization in the human ovarian xenografts. However, needle puncturing did affect the expression of angiogenic genes and resulted in slightly higher follicle survival and significantly better follicle morphology in the ovarian xenografts compared to control. Current results call for further investigations of needle puncturing in the context of OTT.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Yding Andersen C, Mamsen LS, Kristensen SG. FERTILITY PRESERVATION: freezing of ovarian tissue and clinical opportunities. Reproduction. 2019;158:F27-34. https://doi.org/10.1530/REP-18-0635.
Jensen AK, Macklon KT, Fedder J, Ernst E, Humaidan P, Andersen CY. 86 successful births and 9 ongoing pregnancies worldwide in women transplanted with frozen-thawed ovarian tissue: focus on birth and perinatal outcome in 40 of these children. J Assist Reprod Genet. 2017;34:325–36. https://doi.org/10.1007/S10815-016-0843-9.
Donnez J, Dolmans MM. Ovarian cortex transplantation: 60 reported live births brings the success and worldwide expansion of the technique towards routine clinical practice. J Assist Reprod Genet. 2015;32:1167–70. https://doi.org/10.1007/S10815-015-0544-9.
Mamsen LS, Kelsey TW, Ernst E, Macklon KT, Lund AM, Andersen CY. Cryopreservation of ovarian tissue may be considered in young girls with galactosemia. J Assist Reprod Genet. 2018;35:1209–17. https://doi.org/10.1007/S10815-018-1209-2.
Donnez PJ, Dolmans MM, Demylle D, Jadoul P, Pirard C, Squifflet J, et al. Livebirth after orthotopic transplantation of cryopreserved ovarian tissue. Lancet. 2004;364:1405–10. https://doi.org/10.1016/S0140-6736(04)17222-X.
Donnez J, Dolmans MM. Fertility preservation in women. N Engl J Med. 2017;377:1657–65. https://doi.org/10.1056/NEJMra1614676.
Donnez J, Dolmans MM, Diaz C, Pellicer A. Ovarian cortex transplantation: time to move on from experimental studies to open clinical application. Fertil Steril. 2015;104:1097–8. https://doi.org/10.1016/J.FERTNSTERT.2015.08.005.
Dolmans MM, Falcone T, Patrizio P. Importance of patient selection to analyze in vitro fertilization outcome with transplanted cryopreserved ovarian tissue. Fertil Steril. 2020;114:279–80. https://doi.org/10.1016/J.FERTNSTERT.2020.04.050.
Shapira M, Dolmans MM, Silber S, Meirow D. Evaluation of ovarian tissue transplantation: results from three clinical centers. Fertil Steril. 2020;114:388–97. https://doi.org/10.1016/J.FERTNSTERT.2020.03.037.
Jensen AK, Kristensen SG, Macklon KT, Jeppesen J V, Fedder J, Ernst E, et al. Outcomes of transplantations of cryopreserved ovarian tissue to 41 women in Denmark n.d. https://doi.org/10.1093/humrep/dev230.
Khattak H, Malhas R, Craciunas L, Afifi Y, Amorim CA, Fishel S, et al. Fresh and cryopreserved ovarian tissue transplantation for preserving reproductive and endocrine function: a systematic review and individual patient data meta-analysis. Hum Reprod Update. 2022;28:400–16. https://doi.org/10.1093/HUMUPD/DMAC003.
Gellert SE, Pors SE, Kristensen SG, Bay-Bjørn AM, Ernst E, Yding AC. Transplantation of frozen-thawed ovarian tissue: an update on worldwide activity published in peer-reviewed papers and on the Danish cohort. J Assist Reprod Genet. 2018;35:561–70. https://doi.org/10.1007/S10815-018-1144-2.
Janse F, Donnez J, Anckaert E, De Jong FH, Fauser BCJM, Dolmans MM. Limited value of ovarian function markers following orthotopic transplantation of ovarian tissue after gonadotoxic treatment. J Clin Endocrinol Metab. 2011;96:1136–44. https://doi.org/10.1210/JC.2010-2188.
Greve T, Schmidt KT, Kristensen SG, Ernst E, Andersen CY. Evaluation of the ovarian reserve in women transplanted with frozen and thawed ovarian cortical tissue. Fertil Steril. 2012;97:1394–8. https://doi.org/10.1016/J.FERTNSTERT.2012.02.036.
DueholmHjorth IM, Kristensen SG, Dueholm M, Humaidan P. Reproductive outcomes after in vitro fertilization treatment in a cohort of Danish women transplanted with cryopreserved ovarian tissue. Fertil Steril. 2020;114:379–87. https://doi.org/10.1016/J.FERTNSTERT.2020.03.035.
Lotz L, Dittrich R, Hoffmann I, Beckmann MW. Ovarian tissue transplantation: experience from Germany and worldwide efficacy. Clin Med Insights Reprod Heal. 2019;13:117955811986735. https://doi.org/10.1177/1179558119867357.
Dolmans MM, Martinez-Madrid B, Gadisseux E, Guiot Y, Yuan WY, Torre A, et al. Short-term transplantation of isolated human ovarian follicles and cortical tissue into nude mice. Reproduction. 2007;134:253–62. https://doi.org/10.1530/REP-07-0131.
Dath C, Van Eyck AS, Dolmans MM, Romeu L, DelleVigne L, Donnez J, et al. Xenotransplantation of human ovarian tissue to nude mice: comparison between four grafting sites. Hum Reprod. 2010;25:1734–43. https://doi.org/10.1093/HUMREP/DEQ131.
Gavish Z, Spector I, Peer G, Schlatt S, Wistuba J, Roness H, et al. Follicle activation is a significant and immediate cause of follicle loss after ovarian tissue transplantation. J Assist Reprod Genet. 2018;35:61–9. https://doi.org/10.1007/S10815-017-1079-Z.
Kristensen SG, Liu Q, Mamsen LS, Greve T, Pors SE, Bjørn AB, et al. A simple method to quantify follicle survival in cryopreserved human ovarian tissue. Hum Reprod. 2018;33:2276–84. https://doi.org/10.1093/HUMREP/DEY318.
Mamsen LS, Olesen HØ, Pors SE, Hu X, Bjerring P, Christiansen K, et al. Effects of Er:YAG laser treatment on re-vascularization and follicle survival in frozen/thawed human ovarian cortex transplanted to immunodeficient mice. J Assist Reprod Genet. 2021;38:2745–56. https://doi.org/10.1007/S10815-021-02292-0.
Gosden RG, Baird DT, Wade JC, Webb R. Restoration of fertility to oophorectomized sheep by ovarian autografts stored at -196 degrees C. Hum Reprod. 1994;9:597–603. https://doi.org/10.1093/OXFORDJOURNALS.HUMREP.A138556.
Baird DT, Campbell B, De Souza C, Telfer E. Long-term ovarian function in sheep after ovariectomy and autotransplantation of cryopreserved cortical strips. Eur J Obstet Gynecol Reprod Biol. 2004;113:55–9. https://doi.org/10.1016/j.ejogrb.2003.11.023.
Demeestere I, Simon P, Emiliani S, Delbaere A, Englert Y. Orthotopic and heterotopic ovarian tissue transplantation. Hum Reprod Update. 2009;15:649–65. https://doi.org/10.1093/HUMUPD/DMP021.
Mahmoodi M, Mehranjani MS, Mohammad S, Shariatzadeh A, Eimani H, Shahverdi A. N-acetylcysteine improves function and follicular survival in mice ovarian grafts through inhibition of oxidative stress. Reprod Biomed Online. 2015;30:101–10. https://doi.org/10.1016/j.rbmo.2014.09.013.
Olesen HØ, Pors SE, Jensen LB, Grønning AP, Lemser CE, Nguyen Heimbürger MTH, et al. N-acetylcysteine protects ovarian follicles from ischemia-reperfusion injury in xenotransplanted human ovarian tissue. Hum Reprod. 2021;36:429–43. https://doi.org/10.1093/humrep/deaa291.
Tuncer S, Atilgan R, Pala Ş, Kuloğlu T, Artaş G, Aydın S. N-Acetylcysteine and benfotiamine protect autotransplanted ovarian tissue from ischemia-reperfusion injury: an experimental Study. Exp Clin Transplant. 2018. https://doi.org/10.6002/ECT.2017.0320.
Yang H, Lee HH, Lee HC, Ko DS, Kim SS. Assessment of vascular endothelial growth factor expression and apoptosis in the ovarian graft: can exogenous gonadotropin promote angiogenesis after ovarian transplantation? Fertil Steril. 2008;90:1550–8. https://doi.org/10.1016/J.FERTNSTERT.2007.08.086.
Manavella DD, Cacciottola L, Desmet CM, Jordan BF, Donnez J, Amorim CA, et al. Adipose tissue-derived stem cells in a fibrin implant enhance neovascularization in a peritoneal grafting site: a potential way to improve ovarian tissue transplantation. Hum Reprod. 2018;33:270–9. https://doi.org/10.1093/humrep/dex374.
Gao J, Huang Y, Li M, Zhao H, Zhao Y, Li R, et al. Effect of local basic fibroblast growth factor and vascular endothelial growth factor on subcutaneously allotransplanted ovarian tissue in ovariectomized mice. PLoS One. 2015;10:e0134035. https://doi.org/10.1371/JOURNAL.PONE.0134035.
Kang BJ, Wang Y, Zhang L, Xiao Z, Li SW. bFGF and VEGF improve the quality of vitrified-thawed human ovarian tissues after xenotransplantation to SCID mice. J Assist Reprod Genet. 2016;33:281–9. https://doi.org/10.1007/S10815-015-0628-6.
Dolmans MM, Cacciottola L, Amorim CA, Manavella D. Translational research aiming to improve survival of ovarian tissue transplants using adipose tissue-derived stem cells. Acta Obstet Gynecol Scand. 2019;98:665–71. https://doi.org/10.1111/aogs.13610.
Cacciottola L, Nguyen TYT, Chiti MC, Camboni A, Amorim CA, Donnez J, et al. Long-term advantages of ovarian reserve maintenance and follicle development using adipose tissue-derived stem cells in ovarian tissue transplantation. J Clin Med. 2020;9:1–18. https://doi.org/10.3390/JCM9092980.
Cacciottola L, Courtoy GE, Nguyen TYT, Hossay C, Donnez J, Dolmans MM. Adipose tissue–derived stem cells protect the primordial follicle pool from both direct follicle death and abnormal activation after ovarian tissue transplantation. J Assist Reprod Genet. 2021;38:151–61. https://doi.org/10.1007/s10815-020-02005-z.
Allen KB, Mahoney A, Aggarwal S, Davis JR, Thompson E, Pak AF, et al. Transmyocardial revascularization (TMR): current status and future directions. Indian J Thorac Cardiovasc Surg. 2018;34:330–9. https://doi.org/10.1007/S12055-018-0702-7.
Hughes GC, Lowe JE, Kypson AP, St Louis JD, Pippen AM, Peters KG, et al. Neovascularization after transmyocardial laser revascularization in a model of chronic ischemia. Ann Thorac Surg. 1998;66:2029–36. https://doi.org/10.1016/S0003-4975(98)01095-9.
Malekan R, Reynolds C, Narula N, Kelley ST, Suzuki Y, Bridges CR. Angiogenesis in transmyocardial laser revascularization. A nonspecific response to injury. Circulation. 1998;98:II62-5 discussion II66.
Kohmoto T, DeRosa CM, Yamamoto N, Fisher PE, Failey P, Smith CR, et al. Evidence of vascular growth associated with laser treatment of normal canine myocardium. Ann Thorac Surg. 1998;65:1360–7. https://doi.org/10.1016/S0003-4975(98)00236-7.
Pelletier MP, Giaid A, Sivaraman S, Dorfman J, Li CM, Philip A, et al. Angiogenesis and growth factor expression in a model of transmyocardial revascularization. Ann Thorac Surg. 1998;66:12–8. https://doi.org/10.1016/S0003-4975(98)00388-9.
Yamamoto N, Kohmoto T, Gu A, DeRosa C, Smith CR, Burkhoff D. Angiogenesis is enhanced in ischemic canine myocardium by transmyocardial laser revascularization. J Am Coll Cardiol. 1998;31:1426–33. https://doi.org/10.1016/S0735-1097(98)00086-2.
Horvath KA, Chiu E, Maun DC, Lomasney JW, Greene R, Pearce WH, et al. Up-regulation of vascular endothelial growth factor mRNA and angiogenesis after transmyocardial laser revascularization. Ann Thorac Surg. 1999;68:825–9. https://doi.org/10.1016/S0003-4975(99)00842-5.
Mueller XM, Tevaearai HT, Von Segesser LK, Chaubert P, Genton CY. Does laser injury induce a different neovascularisation pattern from mechanical or ischaemic injuries? Heart. 2001;85:697–701. https://doi.org/10.1136/HEART.85.6.697.
Rosendahl M, Schmidt KT, Ernst E, Rasmussen PE, Loft A, Byskov AG, et al. Cryopreservation of ovarian tissue for a decade in Denmark: a view of the technique. Reprod Biomed Online. 2011;22:162–71. https://doi.org/10.1016/J.RBMO.2010.10.015.
Cadenas J, Pors SE, Nikiforov D, Zheng M, Subiran C, Bøtkjær JA, et al. Validating reference gene expression stability in human ovarian follicles, oocytes, cumulus cells, ovarian medulla, and ovarian cortex tissue. Int J Mol Sci. 2022;23:886. https://doi.org/10.3390/IJMS23020886.
Kristensen SG, Olesen H, Zeuthen MC, Pors SE, Andersen CY, Mamsen LS. Revascularization of human ovarian grafts is equally efficient from both sides of the cortex tissue. Reprod Biomed Online. 2022;44:991–4. https://doi.org/10.1016/J.RBMO.2022.02.009.
McLaughlin M, Innell HL, Anderson RA, Telfer EE. Inhibition of phosphatase and tensin homologue (PTEN) in human ovary in vitro results in increased activation of primordial follicles but compromises development of growing follicles. Mol Hum Reprod. 2014;20:736–44. https://doi.org/10.1093/MOLEHR/GAU037.
Gougeon A. Dynamics of follicular growth in the human: a model from preliminary results. Hum Reprod. 1986;1:81–7. https://doi.org/10.1093/oxfordjournals.humrep.a136365.
Xiao Z, Zhang Y, Fan W. Cryopreservation of human ovarian tissue using the silver closed vitrification system. J Assist Reprod Genet. 2017;34:1435–44. https://doi.org/10.1007/s10815-017-1004-5.
Cacciottola L, Manavella DD, Amorim CA, Donnez J, Dolmans MM. In vivo characterization of metabolic activity and oxidative stress in grafted human ovarian tissue using microdialysis. Fertil Steril. 2018;110:534-544.e3. https://doi.org/10.1016/j.fertnstert.2018.04.009.
Dissen GA, Lara HE, Fahrenbach WH, Costa ME, Ojeda SR. Immature rat ovaries become revascularized rapidly after autotransplantation and show a gonadotropin-dependent increase in angiogenic factor gene expression. Endocrinology. 1994;134:1146–54. https://doi.org/10.1210/ENDO.134.3.8119153.
Nugent D, Newton H, Gallivan L, Gosden RG. Protective effect of vitamin E on ischaemia-reperfusion injury in ovarian grafts. J Reprod Fertil. 1998;114:341–6. https://doi.org/10.1530/JRF.0.1140341.
Van Eyck AS, Jordan BF, Gallez B, Heilier JF, Van Langendonckt A, Donnez J. Electron paramagnetic resonance as a tool to evaluate human ovarian tissue reoxygenation after xenografting. Fertil Steril. 2009;92:374–81. https://doi.org/10.1016/J.FERTNSTERT.2008.05.012.
Thurston G, Rudge JS, Ioffe E, Zhou H, Ross L, Croll SD, et al. Angiopoietin-1 protects the adult vasculature against plasma leakage. Nat Med. 2000;6:460–3. https://doi.org/10.1038/74725.
Maisonpierre PC, Suri C, Jones PF, Bartunkova S, Wiegand SJ, Radziejewski C, et al. Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science. 1997;277:55–60. https://doi.org/10.1126/SCIENCE.277.5322.55.
Carmeliet P. Angiogenesis in health and disease. Nat Med. 2003;9:653–60. https://doi.org/10.1038/NM0603-653.
Yancopoulos GD, Davis S, Gale NW, Rudge JS, Wiegand SJ, Holash J. Vascular-specific growth factors and blood vessel formation. Nature. 2000;407:242–8. https://doi.org/10.1038/35025215.
Lobov IB, Brooks PC, Lang RA. Angiopoietin-2 displays VEGF-dependent modulation of capillary structure and endothelial cell survival in vivo. Proc Natl Acad Sci U S A. 2002;99:11205–10. https://doi.org/10.1073/PNAS.172161899.
Xu F, Stouffer RL. Local delivery of angiopoietin-2 into the preovulatory follicle terminates the menstrual cycle in rhesus monkeys. Biol Reprod. 2005;72:1352–8. https://doi.org/10.1095/BIOLREPROD.104.037143.
Fiedler U, Reiss Y, Scharpfenecker M, Grunow V, Koidl S, Thurston G, et al. Angiopoietin-2 sensitizes endothelial cells to TNF-alpha and has a crucial role in the induction of inflammation. Nat Med. 2006;12:235–9. https://doi.org/10.1038/NM1351.
Schuldt EA, Lieb W, Dörr M, Lerch MM, Völzke H, Nauck M, et al. Circulating angiopoietin-2 and its soluble receptor Tie-2 concentrations are related to inflammatory markers in the general population. Cytokine. 2018;105:1–7. https://doi.org/10.1016/J.CYTO.2018.02.003.
Geranmayeh MH, Rahbarghazi R, Farhoudi M. Targeting pericytes for neurovascular regeneration. Cell Commun Signal. 2019;17:26. https://doi.org/10.1186/S12964-019-0340-8.
Ito Y, Oike Y, Yasunaga K, Hamada K, Miyata K, Matsumoto S-I, et al. Inhibition of angiogenesis and vascular leakiness by angiopoietin-related protein 4. Cancer Res. 2003;63:6651–7.
Galaup A, Cazes A, Le Jan S, Philippe J, Connault E, Le Coz E, et al. Angiopoietin-like 4 prevents metastasis through inhibition of vascular permeability and tumor cell motility and invasiveness. Proc Natl Acad Sci U S A. 2006;103:18721–6. https://doi.org/10.1073/PNAS.0609025103.
Tan MJ, Teo Z, Sng MK, Zhu P, Tan NS. Emerging roles of angiopoietin-like 4 in human cancer. Mol Cancer Res. 2012;10:677–88. https://doi.org/10.1158/1541-7786.MCR-11-0519.
Le Jan S, Amy C, Cazes A, Monnot C, Lamandé N, Favier J, et al. Angiopoietin-like 4 is a proangiogenic factor produced during ischemia and in conventional renal cell carcinoma. Am J Pathol. 2003;162:1521–8. https://doi.org/10.1016/S0002-9440(10)64285-X.
Ng KTP, Xu A, Cheng Q, Guo DY, Lim ZXH, Sun CKW, et al. Clinical relevance and therapeutic potential of angiopoietin-like protein 4 in hepatocellular carcinoma. Mol Cancer. 2014;13:196. https://doi.org/10.1186/1476-4598-13-196.
De Roo C, Lierman S, Tilleman K, De Sutter P. In-vitro fragmentation of ovarian tissue activates primordial follicles through the Hippo pathway. Hum Reprod Open. 2020;2020:hoaa048. https://doi.org/10.1093/hropen/hoaa048.
Kawamura K, Cheng Y, Suzuki N, Deguchi M, Sato Y, Takae S, et al. Hippo signaling disruption and Akt stimulation of ovarian follicles for infertility treatment. Proc Natl Acad Sci U S A. 2013;110:17474–9. https://doi.org/10.1073/PNAS.1312830110.
Lunding SA, Andersen AN, Hardardottir L, Olesen H, Kristensen SG, Andersen CY, et al. Hippo signaling, actin polymerization, and follicle activation in fragmented human ovarian cortex. Mol Reprod Dev. 2020;87:711–9. https://doi.org/10.1002/MRD.23353.
Atluri P, Panlilio CM, Liao GP, Suarez EE, McCormick RC, Hiesinger W, et al. Transmyocardial revascularization to enhance myocardial vasculogenesis and hemodynamic function. J Thorac Cardiovasc Surg. 2008;135:289–91. https://doi.org/10.1016/J.JTCVS.2007.09.043. 291.e1; discussion 291.
Acknowledgements
For the histological processing, especially sectioning of samples, we wish to thank Marianne Sguazzino. Marjo Westerdahl is acknowledged for excellent technical assistance. We thank Oliver Carlsson form Visiopharm for assisting with optimization of the APP for quantification of CD31, and Clara Borelli-Møller and Julie Lee Aastrand from the Department of Technology at the University College Copenhagen for their work with histological staining and analysis, IHC staining and APP analysis. Finally, we are utmost grateful to all the women who donated their cryopreserved ovarian tissue for research and to all involved with the clinical activities in the ovarian tissue cryopreservation program in Denmark.
Funding
We are thankful for the funding from The University Hospital of Copenhagen, Rigshospitalet, The Danish Childhood Cancer Foundation, Doctor Sofus Carl Emil Friis and wife Olga Doris Friis scholarship, Carpenter Jørgen Holm and wife Elisa F. Hansen scholarship, and the Hørslev Foundation.
Author information
Authors and Affiliations
Contributions
Authors' contributions H.Ø.O and S.G.K. designed the study. H.Ø.O. conducted the animal studies, performed qPCR analysis, microscopy and digital image analysis, conducted the data analysis and wrote the manuscript. S.G.K. conducted the animal studies, interpreted data and revised the first and final draft of the manuscript. S.E.P. conducted the animal studies, statistical analysis, provided critical comments, contributed to interpretation and revised the first draft. C.S.A. conducted the animal studies, performed qPCR analysis, microscopy, contributed to the data analysis, contributed to interpretation and revised the first draft. M.C.Z. contributed to development of Visiopharm APP, data generation, supervising students, interpretation of data and revised the first draft. L.S.M. and A.T.P contributed to interpretation of data, provided critical comments and revised the first draft. All authors reviewed the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Cryopreservation and collection of patient data were approved by the Ministry of Health (J. no. 30–1372) and by the Danish authorities to comply with the European Union tissue directive. The use of donated human ovarian tissue for research was approved by the Scientific Ethics Committee of the Capital Region (J. no. H-2–2011-044). The use of animals was approved by the Danish Animal Experiments Inspectorate (case file 2015–15-0201–00505) under Danish legislation. Animals were treated in accordance with guidelines at the Department of Experimental Medicine, University of Copenhagen, Denmark, which is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Olesen, H.Ø., Pors, S.E., Adrados, C.S. et al. Effects of needle puncturing on re-vascularization and follicle survival in xenotransplanted human ovarian tissue. Reprod Biol Endocrinol 21, 28 (2023). https://doi.org/10.1186/s12958-023-01081-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-023-01081-x