Abstract
Background
The objective of this study was to explore the cycle-to-cycle reproducibility of serum progesterone level and progesterone/estradiol (P/E2) ratio in the final step of triggering oocyte maturation in patients undergoing repeated consecutive controlled ovarian hyperstimulation for in vitro fertilization (COH-IVF) treatment and to investigate the clinical parameters associated with serum progesterone concentration and P/E2 ratio.
Methods
We retrospectively studied 524 cycles in 203 infertile women who underwent two or more fresh COH-IVF cycles from July 1998 to May 2012 in a university hospital IVF unit. The patients were divided into groups according to the number (2, 3 or > = 4) of total successive IVF cycles with successful oocyte retrieval. The within-subject reproducibility of serum P and P/E2 was tested by calculating intra-class correlation coefficients (ICCs). Multiple linear regression analysis was used to assess the association between patient variables and pre-ovulatory serum P level and P/E2 ratio.
Results
The ICCs in women who underwent 2, 3 and > = 4 IVF cycles were −0.052, 0.163 and 0.212, respectively, for serum P concentration and 0.180, 0.168 and 0.148, respectively, for P/E2 ratio. All ICCs for both serum P and P/E2 ratio were indicative of poor reproducibility. The number of oocytes was significantly positively related to P concentration, and endometrial thickness was significantly negatively related to P concentration and P/E2 ratio.
Conclusion
The cycle-to-cycle reproducibility of pre-ovulatory serum P concentration and P/E2 ratio was poor in individual patients, and these fluctuations were more cycle- than patient-dependent. The number of oocytes was the most significant factor relating to P concentration. By using milder stimulation approach to produce fewer oocytes in the next cycle is a strategy to overcome the high serum P concentration, while clinicians should consider each patient’s general condition including the age, ovarian reserve, embryo grading and the capacity of frozen-thawed embryo transfer.
Similar content being viewed by others
Background
It is well known that gonadotropin-releasing hormone (GnRH) agonists and antagonists, known as GnRH analogues, can effectively eradicate the premature luteinizing hormone surge, and they are almost routinely used during controlled ovarian hyperstimulation (COH) in modern in vitro fertilization (IVF) treatment. However, unpredicted elevation of serum progesterone without an increase luteinizing hormone (LH) in the late follicular phase still occurs in patients co-treated with GnRH-a and COH, a phenomenon called premature progesterone rise (PPR) [1]. The reported incidence of PPR varies greatly from 3 % to 71 %, and it has been reported to be as high as 35 % in GnRH agonist cycles and 38 % in antagonist cycles [2–5]. PPR has previously been defined based on absolute progesterone concentration or as a progesterone/estradiol (P/E2) ratio on the day of human chorionic gonadotropin (hCG) administration [6–8]. The effects of elevated serum progesterone on oocyte maturation, endometrial development and receptivity, and prognostic outcomes after embryo transfer are controversial. An increasing number of retrospective studies suggest that progesterone elevation on the day of hCG administration may have a negative effect on pregnancy rate, and this hypothesis was confirmed by a meta-analysis based on the analysis of 60,000 IVF cycles [9–11]. However, PPR remains a controversial issue because several studies did not find this association [6, 12, 13]. In addition, whether the level of serum progesterone in consecutive cycles remains constant or fluctuates in an individual undergoing repeated COH-IVF treatment is unknown.
In this study, we aimed to explore the inter-cycle reproducibility of serum progesterone and P/E2 ratio in the final step of triggering oocyte maturation in patients undergoing repeated consecutive COH-IVF treatment. The association of both serum progesterone concentration and P/E2 ratio, and the patient’s clinical characteristics and ovarian stimulation responses were also assessed.
Methods
Subjects
This retrospective, single-center cohort study involved consecutive infertile couples who underwent two or more fresh IVF and/or intracytoplasmic sperm injection-embryo transfer (ICSI-ET) cycles from July 1998 to May 2012 in our IVF unit. Women older than 45 years of age and those with intervals of more than 5 years from the first to the last IVF cycle were excluded. The patients were divided into groups according to the number (2, 3 or ≥ 4) of total successive IVF cycles with successful oocyte retrieval. The patients’ characteristics included age, body mass index, basal follicle-stimulating hormone (FSH), luteinizing hormone, estradiol levels on cycle day 3, and causes of infertility. The study was approved by the Institutional Review Board of the Ethics Committee of Chang Gung Medical Foundation, Taiwan in March 2014 (CGMF IRB No.: 103-1156B).
Ovarian stimulation protocols
All women received a GnRH-a long protocol, a GnRH-a short protocol or a GnRH antagonist protocol depending on ovarian reserve, which was assessed by the patient’s age, baseline serum FSH concentration, previous ovarian response to gonadotropins, and the preference of each clinician. The initial dose of gonadotropin was individualized (varied from 75 to 450 IU) for each patient using either human menopausal gonadotropin (hMG) or FSH (purified or recombinant), with further dose adjustments based on each patient’s ovarian response as assessed by serum estradiol concentration and sonographic monitoring of follicular growth. In the GnRH antagonist protocol, 0.25 mg of cetrorelix acetate (Cetrotide®; Serono, Baxter Oncology GmbH, Halle, Germany) was administered daily starting on day 6 of ovarian stimulation or when the lead follicle reached ≥ 14 mm in diameter; administration continued until the day of hCG injection. When the lead follicle reached 16–18 mm in diameter, hMG and FSH were discontinued, and hCG (Ovidrel®; Serono, Modugno, Italy) was administered. Oocyte retrieval was scheduled 36–38 h later. Standard IVF or ICSI procedures, depending on semen parameters, were used to achieve oocyte fertilization, as previously described [14, 15].
On day 3, all embryos were graded on a scale of 0 to 4, which was based on a modification of Veeck's morphological grading system and our previous report [16, 17]. Embryo transfer was performed 3 to 5 days after oocyte retrieval, and no more than 4 embryos were transferred per cycle. During the luteal phase, each patient received 800 mg/day of micronized progesterone (Utrogestan; Piette International Laboratories, Brussels, Belgium) intravaginally or 90 mg of progesterone vaginal gel once daily (Crinone 8 %; Serono Pharmaceuticals Ltd., UK) starting on the day after oocyte retrieval. Clinical pregnancy was defined as one or more gestational sacs detected by transvaginal ultrasound.
Hormone measurements
Serum P and E2 were measured on the day of hCG administration of each IVF cycle using a commercially available immunoassay system (ADVIA Centaur ® XP, Siemens, USA). The lower limits of detection were 0.15 ng/mL for P and 11.8 pg/mL for E2. The intra- and inter-assay coefficients of variation were 5.2 % and 3.5 %, respectively, for P and 5.0 % and 4.1 %, respectively, for E2. The P/E2 ratio was calculated as P (ng/mL) x 1,000/E2 (pg/mL).
Statistical analysis
All statistical analyses were performed using SPSS (ver. 17.0; Statistical Package for Social Sciences, Inc., Chicago, IL, USA). Continuous data are reported as the mean ± standard deviation and compared in the three groups by one—way analysis of variance (ANOVA), whereas categorical variables were compared by the χ 2 or Fisher’s exact tests. Fisher’s least significant difference post hoc test was applied when ANOVA revealed statistical significance. To assess the central tendency and distribution of the measurements, we visualized pre-ovulatory serum P concentrations and P/E2 ratios per cycle within the same patient using box plots. The within—subject reproducibility of serum P and P/E2 was estimated by calculating intra-class correlation coefficients (ICCs) and their 95 % confidence intervals [18]. ICCs were defined as the ratio of between-subject variability to total variability, the latter including between—and within-subject variability. ICC values ≥ 0.75, between 0.60 and 0.74, between 0.40 and 0.59 and < 0.40 or a negative value were interpreted as excellent, good, fair, and poor, respectively [19, 20]. Multiple linear regression analysis was used to assess the association between patient variables and pre-ovulatory serum P level or P/E2 ratio. All P values were two-sided, and a P value of less than 0.05 was considered to be statistically significant.
Results
A total of 524 fresh IVF cycles in 203 infertile women were included in the analysis, and the mean interval from the first to the last IVF cycle was 19.1 ± 15.5 months. Of these 203 women, 125 (61.5 %) underwent two fresh IVF cycles, 52 (25.6 %) underwent three cycles, and 26 (12.8 %) underwent four to seven IVF cycles. The patient baseline demographic, cycle characteristics and cycle outcomes of the three groups are summarized in Table 1.
The mean serum P concentration and P/E2 ratio on the day of hCG administration were 1.62 ng/mL and 1.11, respectively. As expected, the women who had more IVF treatment cycles tended to be older and had longer intervals between IVF treatments, particularly for patients who underwent ≥ 4 IVF cycles. In addition, the main IVF protocol also changed, from the GnRHa long protocol to the short and antagonist protocols. There were no differences among the three groups in body mass index, method of assisted reproductive technology (ART), duration of ovarian stimulation and normal fertilization rate. Interestingly, the pre-ovulatory serum P concentration was significantly lower among patients who underwent more IVF cycles, while the P/E2 ratio was similar among the three groups. Peak E2 concentrations, number of follicles ≥ 16 mm in diameter, and the number of oocytes retrieved were higher among women who underwent 2 or 3 IVF cycles than among those who underwent ≥ 4 cycles. In contrast, women who underwent ≥ 4 IVF cycles required a higher dose of gonadotropin but had fewer follicles than women who underwent 2 or 3 IVF cycles. In addition, fewer oocytes were collected, the endometrium was thinner, and the mean embryo score per embryo was lower in women who underwent ≥ 4 IVF cycles. These women also had lower rates of implantation, clinical pregnancy and live birth despite an equal number of embryos being transferred.
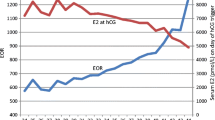
The distributions of serum P concentration and P/E2 ratio on the day of hCG administration across 2 ~ 4 consecutive IVF cycles are depicted in Fig. 1. The median serum P concentrations in the 125 women who underwent 2 IVF cycles each were 1.61 ng/mL in the first cycle and 1.64 ng/mL in the second cycle, and the median P/E2 ratios were 0.76 and 0.83, respectively. In the 52 patients who underwent 3 IVF cycles, the median serum P concentration ranged from 1.39 to 1.58 ng/mL, and the median P/E2 ratio ranged from 0.70 to 0.80, with both showing similar distribution patterns in each cycle. However, the box plots of the patients who underwent 4 IVF cycles showed markedly different distributions across individual cycles.
The ICC data are summarized in Table 2. The ICCs among women who underwent 2, 3, and ≥ 4 IVF cycles were −0.052, 0.163 and 0.212, respectively, for serum P concentration and 0.180, 0.168 and 0.148, respectively, for P/E2 ratio. All of these ICCs were indicative of poor reproducibility.
Multiple linear regression analysis showed that after adjusting for possible confounders, serum P concentration was positively correlated with E2 concentration (P = 0.009) and the number of oocytes retrieved (P < 0.001) and negatively correlated with endometrial thickness (P = 0.043) (Table 3). Additionally, after adjusting for possible confounders, the P/E2 ratio was positively correlated with duration of stimulation (P < 0.001) and negatively correlated with the number of oocytes retrieved (P = 0.002) and endometrial thickness (P = 0.012) (Table 4).
Discussion
To the best of our knowledge, this study is the first to assess the inter-cycle reproducibility of pre-ovulatory serum P measurements and P/E2 ratio in individual women who underwent multiple IVF/ICSI cycles. Our major finding is that the cycle-to-cycle reproducibility of both parameters was poor in individual patients. These inter-cycle variations during repeated IVF cycles suggest that neither serum P concentration nor P/E2 ratio in a subsequent IVF cycle can be predicted from the results in a previous cycle. Factors significantly associated with serum P concentration included E2 concentration on the day of hCG administration, the number of oocytes collected and the thickness of the endometrium; factors significantly associated with the P/E2 ratio included the duration of stimulation, the number of oocytes retrieved and the thickness of the endometrium.
The possible mechanism of PPR is likely due to an excess number of mature follicles, each of which produces a normal amount of P during the late follicular phase of COH [9, 12, 21]. We found that pre-ovulatory serum P concentrations were significantly higher among women who underwent 2 or 3 cycles than among those who underwent ≥ 4 IVF cycles. In addition, the peak E2 concentration was higher and more oocytes were collected in those who underwent 2 or 3 cycles than in those who underwent ≥ 4 IVF cycles. Multiple regression analysis showed that serum P concentration was positively correlated with both the number of oocytes retrieved and the peak E2 level, which is consistent with the results of previous studies and with the above hypothesis [9, 11]. Thus, it is an option to overcome PPR by using milder stimulation approach to produce fewer oocytes in the next cycle. However, clinicians should consider each patient’s general condition including the age, ovarian reserve, embryo grading and the capacity of frozen-thawed embryo transfer.
We also observed a negative correlation between serum P concentration and endometrial thickness, which may indicate advanced endometrial maturation. Advanced maturation of the endometrium, which has been reported during the peri—and post-ovulatory periods of the stimulation cycle [22–24], may be due to several factors, including supra-normal estradiol concentration, early and increased exposure of the endometrium to P and to hCG injections [25–28]. Other studies have implied that endometrial thickness and pattern may be useful indicators of endometrial receptivity, and they have shown that a premature secretory endometrial pattern is introduced by elevation of P. Advanced endometrial maturation may be unfavorable for implantation and have an adverse effect on pregnancy rates [29–32].
In this study, we retrospective analysis of a subgroup of patients who had undergone repeated IVF/ICSI cycles measured pre-ovulatory serum P concentration and P/E2 ratio over multiple IVF cycles in individual patients. Women who had undergone ≥ 4 IVF cycles showed relatively poor responder trend, which may be related to aging. Older women have poorer ovarian responses and yield fewer good quality embryos and fewer available embryos to be frozen than younger women. Increasing the number of attempted IVF cycles can result in a higher cumulative pregnancy rate. However, while IVF may largely overcome infertility in younger women, it does not reverse the age-dependent decline in fertility, especially in women aged ≥ 40 years [33]. Our findings suggest that a maximum of 4 treatment cycles may present a critical point in IVF because of the extremely low ovarian response and poor pregnancy outcomes occurring subsequently.
The relationship between PPR and pregnancy outcome remains the subject of much debate, and some studies have hypothesized that the possible detrimental effect of PPR is mainly through a negative impact on endometrial development at the end of the follicular phase rather than by negatively affecting embryo quality. This may result in embryo-endometrial asynchrony with poor endometrial receptivity [10, 34, 35], and this may reduce embryo implantation and pregnancy rates [24, 25]. Thus, freezing embryos and transferring them in a subsequent frozen-thawed cycle may avoid impairments in endometrial receptivity, which is why it is the method most frequently used to manage PPR.
The results of an oocyte donation program yielded similar observations as the present study. In that study, among 120 women who each donated oocytes on two occasions, the serum P level was ≥ 1.2 ng/mL in the first donation cycle but < 1.2 ng/mL (no further serum P elevation) in the second cycle. The study also reported that PPR did not have a negative impact on pregnancy rate [34]. Notably, these results provide additional evidence supporting inter-cycle variations in pre-ovulatory serum P concentration among women undergoing repeated oocyte donation IVF cycles.
No general consensus has been reached on the cut-off value for PPR. Studies designed to determine the most appropriate cut-off value have utilized receiver operating characteristic (ROC) analysis, trend analysis or arbitrary methods. In addition to pre-ovulatory serum P concentration, some studies have used P/E2 ratio to diagnose PPR, however, the optimal cut-off value for P/E2 ratio has been reported to range from 0.55 to 1.2 and P/E2 ratio has not been shown to definitively predict IVF outcomes [6–8, 36]. We have previously presented data suggesting that progesterone concentration is not the only factor determining the clinical pregnancy and live birth rates, and we have found that PPR has an obvious negative impact on pregnancy outcome only at extremely high progesterone concentration (P ≥ 1.94 ng/mL) [37].
There were considerable inter-cycle variations in serum P concentration and P/E2 ratio on the day of hCG administration in the current study; the changes were bidirectional and went either down or up. Further questions, such as whether women who always have constant “normal” pre-ovulatory serum P levels in repeated IVF cycles have better pregnancy outcomes, remain unresolved. Our study did not assess the recurrence of PPR. The design of the study had several potential biases, such as three different stimulation protocols used and different types of gonadotropin preparations for ovarian stimulation, which may mask the possible effect on serum P concentration and the cycle outcome. Another limitation is the small number of patients undergoing repeated IVF cycles. Further studies are required to answer the unsolved questions mentioned above, investigate the effects of recurrent PPR, and re-examine the reproducibility and potential clinical meaning of these parameters.
Conclusions
Cycle-to-cycle reproducibility of pre-ovulatory serum P concentrations and P/E2 ratio was poor in individual patients, and the fluctuations were more cycle- than patient-dependent. The number of oocytes was the most significant factor relating to the P concentration. By using milder stimulation approach to produce fewer oocytes in the next cycle is a strategy to overcome PPR, while clinicians should consider each patient’s general condition including the age, ovarian reserve, embryo grading and the capacity of frozen-thawed embryo transfer.
Abbreviations
- ART:
-
Assisted reproductive technology
- COH:
-
Controlled ovarian hyperstimulation
- ET:
-
Embryo transfer
- FSH:
-
Follicle-stimulating hormone
- GnRHa:
-
Gonadotropin-releasing hormone agonist
- hCG:
-
human chorionic gonadotropin
- hMG:
-
human menopausal gonadotrophins
- ICCs:
-
Intra-class correlation coefficients
- IVF:
-
In vitro fertilization
- ICSI:
-
Intracytoplasmic sperm injection
- LH:
-
luteinizing hormone
- P:
-
Progesterone
- P/E2 :
-
Progesterone/estradiol
- PPR:
-
Premature progesterone rise
References
Al-Azemi M, Kyrou D, Kolibianakis EM, Humaidan P, Van Vaerenbergh I, Devroey P, et al. Elevated progesterone during ovarian stimulation for IVF. Reprod Biomed Online. 2012;24:381–8.
Edelstein MC, Seltman HJ, Cox BJ, Robinson SM, Shaw RA, Muasher SJ. Progesterone levels on the day of human chorionic gonadotropin administration in cycles with gonadotropin-releasing hormone agonist suppression are not predictive of pregnancy outcome. Fertil Steril. 1990;54:853–7.
Silverberg KM, Burns WN, Olive DL, Riehl RM, Schenken RS. Serum progesterone levels predict success of in vitro fertilization/embryo transfer in patients stimulated with leuprolide acetate and human menopausal gonadotropins. J Clin Endocrinol Metab. 1991;73:797–803.
Ubaldi F, Camus M, Smitz J, Bennink HC, Van Steirteghem A, Devroey P. Premature luteinization in in vitro fertilization cycles using gonadotropin-releasing hormone agonist (GnRH-a) and recombinant follicle-stimulating hormone (FSH) and GnRH-a and urinary FSH. Fertil Steril. 1996;66:275–80.
Bosch E, Valencia I, Escudero E, Crespo J, Simon C, Remohi J, et al. Premature luteinization during gonadotropin-releasing hormone antagonist cycles and its relationship with in vitro fertilization outcome. Fertil Steril. 2003;80:1444–9.
Lai TH, Lee FK, Lin TK, Horng SG, Chen SC, Chen YH, et al. An increased serum progesterone-to-estradiol ratio on the day of human chorionic gonadotropin administration does not have a negative impact on clinical pregnancy rate in women with normal ovarian reserve treated with a long gonadotropin releasing hormone agonist protocol. Fertil Steril. 2009;92:508–14.
Ou YC, Lan KC, Chang SY, Kung FT, Huang FJ. Increased progesterone/estradiol ratio on the day of HCG administration adversely affects success of in vitro fertilization-embryo transfer in patients stimulated with gonadotropin-releasing hormone agonist and recombinant follicle-stimulating hormone. Taiwan J Obstet Gynecol. 2008;47:168–74.
Younis JS, Matilsky M, Radin O, Ben-Ami M. Increased progesterone/estradiol ratio in the late follicular phase could be related to low ovarian reserve in in vitro fertilization-embryo transfer cycles with a long gonadotropin-releasing hormone agonist. Fertil Steril. 2001;76:294–9.
Bosch E, Labarta E, Crespo J, Simon C, Remohi J, Jenkins J, et al. Circulating progesterone levels and ongoing pregnancy rates in controlled ovarian stimulation cycles for in vitro fertilization: analysis of over 4000 cycles. Hum Reprod. 2010;25:2092–100.
Xu B, Li Z, Zhang H, Jin L, Li Y, Ai J, et al. Serum progesterone level effects on the outcome of in vitro fertilization in patients with different ovarian response: an analysis of more than 10,000 cycles. Fertil Steril. 2012;97:1321–7 e1-4.
Venetis CA, Kolibianakis EM, Bosdou JK, Tarlatzis BC. Progesterone elevation and probability of pregnancy after IVF: a systematic review and meta-analysis of over 60 000 cycles. Hum Reprod Update. 2013;19:433–57.
Venetis CA, Kolibianakis EM, Papanikolaou E, Bontis J, Devroey P, Tarlatzis BC. Is progesterone elevation on the day of human chorionic gonadotrophin administration associated with the probability of pregnancy in in vitro fertilization? A systematic review and meta-analysis. Hum Reprod Update. 2007;13:343–55.
Griesinger G, Mannaerts B, Andersen CY, Witjes H, Kolibianakis EM, Gordon K. Progesterone elevation does not compromise pregnancy rates in high responders: a pooled analysis of in vitro fertilization patients treated with recombinant follicle-stimulating hormone/gonadotropin-releasing hormone antagonist in six trials. Fertil Steril. 2013;100:1622.
Kung FT, Chang SY, Yang CY, Lin YC, Lan KC, Huang LY, et al. Transfer of nonselected transferable day 3 embryos in low embryo producers. Fertil Steril. 2003;80:1364–70.
Kung FT, Lin YC, Tseng YJ, Huang FJ, Tsai MY, Chang SY. Transfer of frozen-thawed blastocysts that underwent quarter laser-assisted hatching at the day 3 cleaving stage before freezing. Fertil Steril. 2003;79:893–9.
Veeck LL. Atlas of the human oocyte and early conceptus. 1st ed. Baltimore: Williams & Wilkins; 1986.
Lan KC, Huang FJ, Lin YC, Kung FT, Hsieh CH, Huang HW, et al. The predictive value of using a combined Z-score and day 3 embryo morphology score in the assessment of embryo survival on day 5. Hum Reprod. 2003;18:1299–306.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8.
Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284–90.
Hallgren KA. Computing inter-rater reliability for observational data: an overview and tutorial. Tutor Quant Methods Psychol. 2012;8:23–34.
Fanchin R, Righini C, Olivennes F, Ferreira AL, de Ziegler D, Frydman R. Consequences of premature progesterone elevation on the outcome of in vitro fertilization: insights into a controversy. Fertil Steril. 1997;68:799–805.
Lass A, Peat D, Avery S, Brinsden P. Histological evaluation of endometrium on the day of oocyte retrieval after gonadotrophin-releasing hormone agonist-follicle stimulating hormone ovulation induction for in-vitro fertilization. Hum Reprod. 1998;13:3203–5.
Ubaldi F, Bourgain C, Tournaye H, Smitz J, Van Steirteghem A, Devroey P. Endometrial evaluation by aspiration biopsy on the day of oocyte retrieval in the embryo transfer cycles in patients with serum progesterone rise during the follicular phase. Fertil Steril. 1997;67:521–6.
Fleming R, Jenkins J. The source and implications of progesterone rise during the follicular phase of assisted reproduction cycles. Reprod Biomed Online. 2010;21:446–9.
Bourgain C, Devroey P. The endometrium in stimulated cycles for IVF. Hum Reprod Update. 2003;9:515–22.
Fanchin R, de Ziegler D, Castracane VD, Taieb J, Olivennes F, Frydman R. Physiopathology of premature progesterone elevation. Fertil Steril. 1995;64:796–801.
Basir GS OWS, Ng EH, Ho PC. Morphometric analysis of peri-implantation endometrium in patients having excessively high oestradiol concentrations after ovarian stimulation. Hum Reprod. 2001;16:435–40.
Han SW, Lei ZM, Rao CV. Treatment of human endometrial stromal cells with chorionic gonadotropin promotes their morphological and functional differentiation into decidua. Mol Cell Endocrinol. 1999;147:7–16.
Zhao J, Zhang Q, Li Y. The effect of endometrial thickness and pattern measured by ultrasonography on pregnancy outcomes during IVF-ET cycles. Reprod Biol Endocrinol. 2012;10:100.
Gonen Y, Casper RF, Jacobson W, Blankier J. Endometrial thickness and growth during ovarian stimulation: a possible predictor of implantation in in vitro fertilization. Fertil Steril. 1989;52:446–50.
Chen SL, Wu FR, Luo C, Chen X, Shi XY, Zheng HY, et al. Combined analysis of endometrial thickness and pattern in predicting outcome of in vitro fertilization and embryo transfer: a retrospective cohort study. Reprod Biol Endocrinol. 2010;8:30.
Detti L, Yelian FD, Kruger ML, Diamond MP, Rode A, Mitwally MF, et al. Endometrial thickness is related to miscarriage rate, but not to the estradiol concentration, in cycles down-regulated with gonadotropin-releasing hormone antagonist. Fertil Steril. 2008;89:998–1001.
Malizia BA, Hacker MR, Penzias AS. Cumulative live-birth rates after in vitro fertilization. N Engl J Med. 2009;360:236–43.
Melo MA, Meseguer M, Garrido N, Bosch E, Pellicer A, Remohi J. The significance of premature luteinization in an oocyte-donation programme. Hum Reprod. 2006;21:1503–7.
Hofmann GE, Bentzien F, Bergh PA, Garrisi GJ, Williams MC, Guzman I, et al. Premature luteinization in controlled ovarian hyperstimulation has no adverse effect on oocyte and embryo quality. Fertil Steril. 1993;60:675–9.
Elgindy EA. Progesterone level and progesterone/estradiol ratio on the day of hCG administration: detrimental cutoff levels and new treatment strategy. Fertil Steril. 2011;95:1639–44.
Tsai YR, Huang FJ, Lin PY, Kung FT, Lin YJ, Lin YC, et al. Progesterone elevation on the day of human chorionic gonadotropin administration is not the only factor determining outcomes of in vitro fertilization. Fertil Steril. 2015;103:106–11.
Acknowledgements
The authors thank Yun-Fang Chiang, RN, Department of Obstetrics and Gynecology at Chang Gung Memorial Hospital, for assistance in patient registration and data collection. We thank Professor Hsueh-Wen Chang (from the Department of Biological Sciences in National Sun Yat-Sen University, Taiwan) and Associate Professor Chia-Hao Chang (from the Department of Nursing, Chang Gung University of Science and Technology, Chiayi Campus, Chiayi, Taiwan) for assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
YJL and FTK participated in the design of the study and drafted the manuscript. KCL, FJH, PYL and HJC helped in the study coordination and the data collection. FTK supervised and conceived of the study. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Lin, YJ., Lan, KC., Huang, FJ. et al. Reproducibility and clinical significance of pre-ovulatory serum progesterone level and progesterone/estradiol ratio on the day of human chorionic gonadotropin administration in infertile women undergoing repeated in vitro fertilization cycles. Reprod Biol Endocrinol 13, 41 (2015). https://doi.org/10.1186/s12958-015-0037-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12958-015-0037-9