Abstract
Background
Prolonged postoperative ileus (PPOI) is a common complication after colorectal surgery that increases patient discomfort, hospital stay, and financial burden. However, predictive tools to assess the risk of PPOI in patients undergoing laparoscopic low anterior resection have not been developed. Thus, the purpose of this study was to develop a nomogram to predict PPOI after laparoscopic low anterior resection for rectal cancer.
Methods
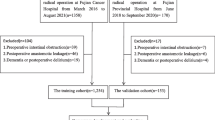
A total of 548 consecutive patients who underwent laparoscopic low anterior resection for midlow rectal cancer at a single tertiary medical center were retrospectively enrolled between January 2019 and January 2023. Univariate and multivariate logistic regression analysis was performed to analyze potential predictors of PPOI. The nomogram was constructed using the filtered variables and internally verified by bootstrap resampling. Model performance was evaluated by receiver operating characteristic curve and calibration curve, and the clinical usefulness was evaluated by the decision curve.
Results
Among 548 consecutive patients, 72 patients (13.1%) presented with PPOI. Multivariate logistic analysis showed that advantage age, hypoalbuminemia, high surgical difficulty, and postoperative use of opioid analgesic were independent prognostic factors for PPOI. These variables were used to construct the nomogram model to predict PPOI. Internal validation, conducted through bootstrap resampling, confirmed the great discrimination of the nomogram with an area under the curve of 0.738 (95%CI 0.736–0.741).
Conclusions
We created a novel nomogram for predicting PPOI after laparoscopic low anterior resection. This nomogram can assist surgeons in identifying patients at a heightened risk of PPOI.
Similar content being viewed by others
Introduction
The recovery of bowel function is an important indicator following colorectal surgery, and typically, it returns to normal within 2–4 days [1, 2]. However, when the recovery of bowel function takes longer than expected, it is called prolonged postoperative ileus (PPOI). PPOI often leads to discomfort, heightened psychological distress, prolonged hospitalization, and increased hospitalization costs [3, 4].
The pathogenesis of PPOI is multifactorial and intricate [1]. Presently, risk factors such as advanced age, the use of opioid analgesics, open surgery, gastrointestinal stretch, and inflammation are considered to be key mechanisms of PPOI [5, 6]. Of note, few studies have specifically assessed the risk factors of PPOI following rectal surgery [7]. Frequent neoadjuvant irradiation, manipulation in a narrow pelvis, and creation of a diverting ileostomy may lead to a specific risk of PPOI after rectal surgery [7, 8]. The construction of PPOI prediction models can help to assess the risk of PPOI. Consequently, these models make a significant contribution to the development of strategies to reduce or prevent the occurrence of PPOI. However, to our knowledge, few studies have used nomogram prediction models to assess the risk of PPOI after colorectal surgery, especially in patients undergoing rectal surgery [5, 9, 10].
Hence, this study aimed to analyze the predictive factors for PPOI after laparoscopic anterior resection for rectal cancer and to develop a nomogram for predictive purposes.
Patients and methods
Study population
The data of consecutive patients with midlow rectal cancer who underwent elective low anterior resection, between January 2019 and January 2023, were retrospectively retrieved from our prospectively collected database. To avoid confounding bias, we excluded patients with open surgery, combined multiple organ resection, and secondary surgery for postoperative recurrence.
Operation and perioperative management
All operations were performed by an experienced surgical team, following the total mesorectal excision operation protocol. The surgical techniques were performed as described in previous reports [11, 12].
Patients were treated by the same perioperative enhanced recovery care program. Preoperative evaluation included clinical examination, serological assessment, colonoscopy, thoracoabdominal and pelvic computed tomography (CT), and pelvic magnetic resonance imaging. All patients underwent preoperative mechanical bowel preparation, and prophylactic antibiotics were administered.
Postoperative care included a clear liquid diet on postoperative day 1 and diet advancement as tolerated. In addition, the urinary catheter was removed on postoperative day 1 if there was no difficulty in urination. The utilization of postoperative use of opioid analgesics was evaluated based on the patient's postoperative visual analog scale.
Variable and outcome definition
We adopted the definition of PPOI as proposed by Vather et al. [13]. PPOI was diagnosed when patients met at least two of the following five criteria on or after postoperative day 4: (a) nausea or vomiting, (b) inability to tolerate a solid oral diet over the last 24 h, (c) abdominal distension, (d) absence of flatus over the last 24 h, and (e) ileus noted on computed tomography (CT) scans.
The distance between the intertuberous and interspinous was measured by CT. In addition, Slice-O-matic software (version 4.3, Tomovision, Montreal, QC, Canada) was employed for body composition analysis [14]. Visceral adipose tissue area (VAT) and skeletal muscle area (SMA) were measured at the third lumbar vertebra (L3) level on the CT image, and mesorectal fat area (MFA) was measured at the level of the tip of the ischial spine. In this study, the upper quartile distributions for males and females were used as the cutoff points for VAT and MFA, respectively. Additionally, the lower quartile distributions were used as the cutoff points for SMA. Sarcopenia was defined as low-SMA and visceral obesity was defined as high VAT.
When a patient met three or more of the following five criteria, the case was classified as high surgery difficulty: narrow pelvis (intertuberous distance < 100 mm and interspinous distance < 120 mm), large MFA (> 24.14 cm2), low-grade tumor (tumor height ≤ 5 cm), large tumor (diameter > 5 cm), and T4 stage. Postoperative complications were classified according to the Clavien-Dindo classification [15].
Construction and validation of the nomogram
Univariate logistic regression analysis was performed to initially assess associations of various indexes with PPOI. All indexes with a p value < 0.1 were included in the multivariate analysis. The variance inflation factor was calculated to ensure no collinearity among the covariates.
A nomogram based on the multivariable logistic regression was constructed. The model was validated internally using 500 bootstrap resampling to reduce overfit bias. The discrimination performance of the nomogram was assessed using receiver operating characteristic (ROC) curve analysis. Calibration curve analysis was used to assess the accuracy of the model. Additionally, decision curve analysis (DCA) was used to evaluate the clinical usefulness of the model.
Statistical analysis
The data were analyzed by SPSS (version 25.0, IBM Corp, Armonk, New York, USA) and R software (version 4.2.1, http://www.r-project.org/). Normally distributed continuous data were analyzed by Student’s t test and expressed as mean (± standard deviation [SD]); non-normally distributed data were analyzed by Wilcoxon rank-sum test and expressed as median (interquartile range [IQR]). Categorical data were compared using chi-squared test or Fisher’s exact test and expressed as n (%). All of the statistical analyses were two-sided, and the statistical significance was set at p value < 0.05.
Results
Patient characteristics and outcomes
A total of 548 patients were included in this study, of whom 72 developed PPOI (13.1%). When comparing baseline characteristics between the two groups (Table 1), it was observed that patients in the PPOI group were older than those in the non-PPOI group (66.5 years [61–71.15] vs. 64.5 years [58–70], p = 0.043). In addition, more patients in the PPOI group had a history of abdominal surgery (p = 0.049) and hypoproteinemia (p = 0.011). Intergroup differences in gender, smoking history, drinking history, comorbidities, and ASA classification did not differ significantly.
Furthermore, the operation time was longer in the PPOI group (170 min [140–201.5] vs. 155 min [126.3–182.0], p = 0.026). There were no statistically significant differences in terms of pathological outcomes, including tumor diameter, harvested lymph nodes, tumor differentiation, and tumor stage (Table 2).
The postoperative characteristics of the two groups are shown in Table 3. Regarding the utilization of postoperative opioid analgesics, 44.3% of patients in the PPOI group required opioid analgesics, in contrast to 24.4% in the non-PPOI group. According to the Clavien-Dindo classification, there were no significant differences between the two groups in terms of minor complications (grades I–II). However, it is noteworthy that major complications (grades III–IV) were more commonly observed in the PPOI group. In the PPOI group, the postoperative hospital stay was significantly longer (p < 0.001), and inpatient costs were higher (p < 0.001).
Factors associated with PPOI
Univariate analysis showed that age ≥ 65 years, previous abdominal surgery, hypoproteinemia, anemia, hypokalemia, high surgical difficulty, operative time ≥ 180 min, estimated blood loss ≥ 100 ml, conversion, postoperative use of opioid analgesic, and perioperative transfusion were potential predictors of PPOI. Subsequent multivariate logistic regression analysis showed that age ≥ 65 years (OR = 1.816, 95%CI 1.040–3.172, p = 0.036), hypoproteinemia (OR = 2.565, 95%CI 1.183–5.563, P = 0.017), high surgical difficulty (OR = 2.934, 95%CI 1.406–6.121, p = 0.004), and postoperative use of opioid analgesic (OR = 2.624, 95%CI 1.513–4.553, p = 0.001) were independent predictors of PPOI (Table 4).
Construction of a nomogram for PPOI
Based on the results of multivariable logistic regression analysis, a nomogram was generated to predict the incidence of PPOI (Fig. 1). A higher total score indicated a higher likelihood of PPOI, which was calculated by summing the scores for each variable.
The bias-corrected calibration plot with 500-sample bootstrapping for the prediction model demonstrated satisfactory consistency (Fig. 2). Similarly, the discriminative ability of the model was evaluated using the bias-corrected AUC, which was estimated using bootstrap resampling with 500 iterations. The calculated AUC was found to be 0.738 (95%CI 0.736–0.741) (Fig. 3). Furthermore, the decision curve demonstrates that utilizing the nomogram to predict the probability of PPOI provides more benefit than either the treat-all-patients scheme or the treat-none scheme, indicating that the nomogram has clinical value (Fig. 4).
Discussion
Currently, the concept of enhanced recovery after surgery is widely accepted by surgeons. PPOI as a common complication that hinders postoperative recovery has received widespread attention. In the present study, 13.1% of the patients were diagnosed with PPOI, which is comparable to the 15% occurrence of PPOI following laparoscopic rectal surgery reported by Elisabeth et al. [7]. Liang et al. reported an incidence of PPOI of 19.75% in gastrectomy for gastric cancer [5], while Lind et al. showed an incidence of 10.2% by analyzing 1254 patients with colorectal cancer [10].
In this study, we evaluated the relationship between clinical characteristics and the occurrence of PPOI in patients who underwent laparoscopic anterior resection for rectal cancer. Age ≥ 65 years, hypoproteinemia, high surgical difficulty, and postoperative use of opioid analgesic have been proven to be significantly correlated with PPOI. The selected predictors were then used to construct a nomogram that could help identify patients at risk of PPOI. In addition, it has been confirmed that this nomogram has a good diagnostic performance and has been validated internally. Understanding the clinical factors that predispose to PPOI is the first step in developing tools that can help predict its occurrence. This, in turn, may help to identify individuals at risk and allow early intervention to mitigate or terminate episodes.
In this study, a significant correlation was observed between hypoproteinemia and PPOI, this finding is similar to a study by Liang et al. [9]. Hypoalbuminemia is common in patients with gastrointestinal cancers, primarily attributed to dietary deficiencies, impaired liver function, increased loss of ascites, and gastrointestinal bleeding. Hypoproteinaemia may lead to intestinal edema, which affects the recovery of intestinal function [16]. Furthermore, hypoalbuminemia has also been reported to be an indicator of deterioration in performance status or tumor progression [17]. Several studies have also demonstrated that preoperative albumin levels can be predictive of surgical risk and postoperative complications [18,19,20].
Of note, the multivariable analysis also indicated that advanced age was an independent risk factor for PPOI, which is consistent with several previous studies [5, 7]. This observation could be attributed to the fact that older adults tend to have a higher prevalence of medical comorbidities, clinical frailty, and relatively poorer nutritional and functional statuses compared to younger adults [21]. Our study emphasizes the necessity of perioperative dietary interventions for older patients and those with hypoalbuminemia.
Vather et al. demonstrated that high surgical difficulty, as self-assessed by the surgeon, is a risk factor for developing PPOI after colorectal surgery [16]. In this study, we assessed the difficulty of surgery based on factors that have been previously reported to influence surgical difficulty [22,23,24]. It is worth noting that this method is more objective than a surgeon’s self-assessment. In this study, we also found high surgical difficulty is an independent risk factor for PPOI. Operation in patients with high surgical difficulty, exposure, resection, and anastomosis will be more challenging. Specifically, performing the procedure in a narrow pelvis may increase the risk of rectal wall or vascular trauma [25].
Opioids are commonly used for pain management after surgery, which is highly effective in treating both acute and chronic pain. However, opioid therapy also affects bowel function by causing opioid-induced bowel dysfunction [26]. Opioids can cause inhibition of water and electrolyte excretion and enhanced non-propulsive contractions through activation of μ-receptors located in the enteric nervous system [27]. The relationship between opioids and PPOI has been well characterized in previous studies [28, 29]. Our study also confirms that patients using opioids have a higher risk of PPOI. The peripherally acting μ-receptor antagonists such as methylnaltrexone and alvimopan are designed to block the side effects of opioids in the gastrointestinal tract while preserving the pain-relieving effects of opioids [25]. These drugs are expected to be utilized in the prevention of PPOI.
Prolonged postoperative ileus (PPOI) is a common complication after colorectal surgery, leading to an increased risk of complications, extended hospitalization, and significant financial burdens for healthcare facilities [30, 31]. Individualized treatment has been gradually emphasized in current clinical practice. In patients at higher risk of PPOI, strategies such as minimizing surgical trauma, optimizing fluid management, reducing opioid use, encouraging early physical activity and promoting gum chewing have been reported as effective measures to prevent PPOI [32]. Additionally, in these patients, special care should be taken in postoperative monitoring to prevent aspiration pneumonia and PPOI-related death [33].
This study has several limitations. First, this study is retrospective in nature, and the sample size was relatively small. Second, this model lacks external validation, and to address this limitation, we have employed bootstrap resampling for internal validation. Despite the abovementioned limitations, this study boasts several notable advantages. To the best of our knowledge, this is the first nomogram specifically designed to predict PPOI after laparoscopic low anterior resection for rectal cancer. Furthermore, we conducted measurements of patients’ pelvic and body composition, facilitating a more comprehensive assessment of surgical difficulty and the nutritional status of the patients.
Conclusion
We created a novel nomogram for predicting PPOI after laparoscopic low anterior resection. This nomogram can assist surgeons in identifying patients at a heightened risk of PPOI.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author on reasonable request.
Abbreviations
- PPOI:
-
Prolonged postoperative ileus
- CT:
-
Computed tomography
- VAT:
-
Visceral adipose tissue area
- SMA:
-
Skeletal muscle area
- MFA:
-
Mesorectal fat area
- DCA:
-
Decision curve analysis
- ROC:
-
Receiver operating characteristic
- ASA:
-
American Society of Anesthesiologists Classification
- NOSES:
-
Natural orifice specimen extraction surgery
- CDC:
-
Clavien-Dindo Classification
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
References
Bragg D, El-Sharkawy AM, Psaltis E, Maxwell-Armstrong CA, Lobo DN. Postoperative ileus: recent developments in pathophysiology and management. Clin Nutr. 2015;34(3):367–76.
Pavoor R, Milsom J. Postoperative ileus after laparoscopic colectomy: elusive and expensive. Ann Surg. 2011;254(6):1075.
Mao H, Milne TGE, O’Grady G, Vather R, Edlin R, Bissett I. Prolonged postoperative ileus significantly increases the cost of inpatient stay for patients undergoing elective colorectal surgery: results of a multivariate analysis of prospective data at a single institution. Dis Colon Rectum. 2015;62(5):631–7.
Peters EG, Pattamatta M, Smeets BJJ, Brinkman DJ, Evers S, de Jonge WJ, Hiligsmann M, Luyer MDP. The clinical and economical impact of postoperative ileus in patients undergoing colorectal surgery. Neurogastroenterol Motil. 2020;32(8): e13862.
Liang WQ, Zhang KC, Cui JX, Xi HQ, Cai AZ, Li JY, Liu YH, Liu J, Zhang W, Wang PP, Wei B, Chen L. Nomogram to predict prolonged postoperative ileus after gastrectomy in gastric cancer. World J Gastroenterol. 2019;25(38):5838–49.
Sugawara K, Kawaguchi Y, Nomura Y, Suka Y, Kawasaki K, Uemura Y, Koike D, Nagai M, Furuya T, Tanaka N. Perioperative factors predicting prolonged postoperative ileus after major abdominal surgery. J Gastrointest Surg. 2018;22(3):508–15.
Hain E, Maggiori L, Mongin C, Prost AlDJ, Panis Y. Risk factors for prolonged postoperative ileus after laparoscopic sphincter-saving total mesorectal excision for rectal cancer: an analysis of 428 consecutive patients. Surg Endosc. 2018;32(1):337–44.
Reichert M, Weber C, Pons-Kühnemann J, Hecker M, Padberg W, Hecker A. Protective loop ileostomy increases the risk for prolonged postoperative paralytic ileus after open oncologic rectal resection. Int J Colorectal Dis. 2018;33(11):1551–7.
Liang WQ, Zhang KC, Li H, Cui JX, Xi HQ, Li JY, Cai AZ, Liu YH, Zhang W, Zhang L, Wei B, Chen L. Preoperative albumin levels predict prolonged postoperative ileus in gastrointestinal surgery. World J Gastroenterol. 2020;26(11):1185–96.
Lin Z, Li Y, Wu J, Zheng H, Yang C. Nomogram for prediction of prolonged postoperative ileus after colorectal resection. BMC cancer. 2022;22(1):1273.
Feroci F, Vannucchi A, Bianchi PP, Cantafio S, Garzi A, Formisano G, Scatizzi M. Total mesorectal excision for mid and low rectal cancer: laparoscopic vs robotic surgery. World J Gastroenterol. 2016;22(13):3602–10.
Pan J, Wang B, Feng Z, Sun Z, Xia C, Zhang Q, Ren S. Robotic versus laparoscopic total mesorectal excision for mid-low rectal cancer with difficult anatomical conditions. Asian J Surg. 2022;45(12):2725–32.
Vather R, Trivedi S, Bissett I. Defining postoperative ileus: results of a systematic review and global survey. J Gastrointest Surg. 2013;17(5):962–72.
Chin EC, Leung CK, Yu DJ, Yu AP, Bernal JK, Lai CW, Chan DKC, Ngai HH, Yung PSH, Lee CH, Fong DY, Keating SE, Coombes JS, Siu PM. Effects of one-year once-weekly high-intensity interval training on body adiposity and liver fat in adults with central obesity: Study protocol for a randomized controlled trial. J Exerc Sci Fit. 2022;20(2):161–71.
Hu WH, Eisenstein S, Parry L, Ramamoorthy S. Preoperative malnutrition with mild hypoalbuminemia associated with postoperative mortality and morbidity of colorectal cancer: a propensity score matching study. Nutr J. 2019;18(1):33.
Kim Y, Kim YM, Kim JH, Youn YH, Kim JW, Park H. Peri-operative inflammatory marker as a predictive factor for prolonged post-operative ileus after gastrectomy for gastric cancer. J Neurogastroenterol Motil. 2021;27(4):588–95.
Vather R, Josephson R, Jaung R, Robertson J, Bissett I. Development of a risk stratification system for the occurrence of prolonged postoperative ileus after colorectal surgery: a prospective risk factor analysis. Surgery. 2015;157(4):764–73.
McMillan DC. An inflammation-based prognostic score and its role in the nutrition-based management of patients with cancer. Proc Nutr Soc. 2008;67(3):257–62.
Bendersky V, Sun Z, Adam MA, Rushing C, Kim J, Youngwirth L, Turner M, Migaly J, Mantyh CR. Determining the optimal quantitative threshold for preoperative albumin level before elective colorectal surgery. J Gastrointest Surg. 2017;21(4):692–9.
Hart A, Sun Y, Titcomb TJ, Liu B, Smith JK, Correia MLG, Snetselaar LG, Zhu Z, Bao W. Association between preoperative serum albumin levels with risk of death and postoperative complications after bariatric surgery: a retrospective cohort study. Surg Obes Relat Dis. 2022;18(7):928–34.
Kudsk KA, Tolley EA, DeWitt RC, Janu PG, Blackwell AP, Yeary S, King BK. Preoperative albumin and surgical site identify surgical risk for major postoperative complications. JPEN J Parenter Enteral Nutr. 2003;27(1):1–9.
Tamura K, Matsuda K, Fujita Y, Iwahashi M, Mori K, Yamade N, Hotta T, Noguchi K, Sakata Y, Takifuji K, Iwamoto H, Mizumoto Y, Yamaue H. Optimal assessment of frailty predicts postoperative complications in older patients with colorectal cancer surgery. World J Surg. 2021;45(4):1202–9.
Escal L, Nougaret S, Guiu B, Bertrand MM, de Forges H, Tetreau R, Thézenas S, Rouanet P. MRI-based score to predict surgical difficulty in patients with rectal cancer. Br J Surg. 2018;105(1):140–6.
Yamamoto T, Kawada K, Kiyasu Y, Itatani Y, Mizuno R, Hida K, Sakai Y. Prediction of surgical difficulty in minimally invasive surgery for rectal cancer by use of MRI pelvimetry. BJS open. 2020;4(4):666–77.
De Giorgio R, Zucco FM, Chiarioni G, Mercadante S, Corazziari ES, Caraceni A, Odetti P, Giusti R, Marinangeli F, Pinto C. Management of opioid-induced constipation and bowel dysfunction: expert opinion of an italian multidisciplinary panel. Adv Ther. 2021;38(7):3589–621.
Becker G, Blum HE. Novel opioid antagonists for opioid-induced bowel dysfunction and postoperative ileus. Lancet. 2009;373(9670):1198–206.
Chamie K, Golla V, Lenis AT, Lec PM, Rahman S, Viscusi ER. Peripherally acting μ-opioid receptor antagonists in the management of postoperative ileus: a clinical review. J Gastrointest Surg. 2021;25(1):293–302.
Alhashemi M, Fiore JF Jr, Safa N, Al Mahroos M, Mata J, Pecorelli N, Baldini G, Dendukuri N, Stein BL, Liberman AS, Charlebois P, Carli F, Feldman LS. Incidence and predictors of prolonged postoperative ileus after colorectal surgery in the context of an enhanced recovery pathway. Surg Endosc. 2019;33(7):2313–22.
Ju H, Shen K, Li J, Feng Y. An increased total postoperative opiate dose is an independent risk factor for prolonged postoperative ileus after laparoscopic colorectal surgery: a case-control study. Korean J Anesthesiol. 2023. https://doi.org/10.4097/kja.22792.
Quiroga-Centeno AC, Jerez-Torra KA, Martin-Mojica PA, Castañeda-Alfonso SA, Castillo-Sánchez ME, Calvo-Corredor OF, Gómez-Ochoa SA. Risk factors for prolonged postoperative ileus in colorectal surgery: a systematic review and meta-analysis. World J Surg. 2020;44(5):1612–26.
Seo SHB, Carson DA, Bhat S, Varghese C, Wells CI, Bissett IP, O’Grady G. Prolonged postoperative ileus following right- versus left-sided colectomy: a systematic review and meta-analysis. Colorectal Dis. 2021;23(12):3113–22.
Yin YN, Xie H, Ren JH, Jiang NJ, Dai L. The impact of gum-chewing on postoperative ileus following gynecological cancer surgery: a systematic review and meta-analysis of randomized controlled trials. Front Oncol. 2022;12:1059924.
Yorkshire Surgical Research Collaborative. Multicentre observational study of gastrointestinal recovery after elective colorectal surgery. Colorectal Dis. 2018;20(6):536–44.
Acknowledgements
None.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Fangliang Guo and Zhiwei Sun conceived the study design. Zongheng Wang acquired the data for the study. Jianfeng Gao and Jiahao Pan analyzed and interpreted the data. Fangliang Guo drafted the manuscript. Shuangyi Ren and Qianshi Zhang revised the manuscript for important intellectual content. All authors revised and approved the manuscript for publication.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All the patients personally signed the consent. This study was conducted in accordance with the ethical principles outlined in the 1964 Declaration of Helsinki. Ethical approval for this study was obtained from the Institutional Review Board Ethics Committee at The Second Affiliated Hospital of Dalian Medical University.
Consent for publication
Not applicable.
Competing interests
The authors declared that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guo, F., Sun, Z., Wang, Z. et al. Nomogram for predicting prolonged postoperative ileus after laparoscopic low anterior resection for rectal cancer. World J Surg Onc 21, 380 (2023). https://doi.org/10.1186/s12957-023-03265-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-03265-6