Abstract
Background
Following neoadjuvant chemotherapy, surgical resection is one of the most preferred treatment options for locally advanced gastric cancer patients. However, the optimal time interval between chemotherapy and surgery is unclear. This review aimed to identify the optimal time interval between neoadjuvant chemotherapy and surgery for advanced gastric cancer.
Methods
Beginning on November 12, 2022, we searched the PubMed, Cochrane Library, Web of Science databases, and Embase.com databases for relevant English-language research. Two authors independently screened the studies, assessed their quality, extracted the data, and analyzed the results. The primary goal was to investigate the relationship between the time interval to surgery (TTS) and long-term survival outcomes for patients. This study has been registered with PROSPERO (CRD42022365196).
Results
After an initial search of 4880 articles, the meta-analysis review ultimately included only five retrospective studies. Ultimately, this meta-analysis included 1171 patients, of which 411 patients had TTS of < 4 weeks, 507 patients had TTS of 4–6 weeks, and 253 patients had TTS of > 6 weeks. In survival analysis, patients with TTS of > 6 weeks had poorer overall survival outcomes than patients with TTS of 4–6 weeks (HR = 1.34, 95% CI: 1.03–1.75, P = 0.03). No significant differences were found in terms of disease-free survival the groups.
Conclusion
Based on the current clinical evidence, patients with locally advanced gastric cancer may benefit better with a TTS of 4–6 weeks; however, this option still needs additional study.
Similar content being viewed by others
Introduction
As the fourth greatest cause of cancer death worldwide and the fifth most common malignancy overall, stomach cancer affects approximately a million people annually and is a primary source of cancer diagnosis worldwide [1]. The prognosis of gastric cancer patients varies with different tumor stages. Advanced tumor stage was the main reason for the tumor burden for gastric cancer patients [2, 3]. In China, more than 70% of gastric cancer patients are in advanced stages once the diagnosis is confirmed [4, 5]. Therefore, there has been a considerable emphasis over the past several decades on discovering methods to increase the chance of survival for patients with locally advanced gastric cancer (LAGC). Since the MAGIC trial was published more than 10 years ago, neoadjuvant chemotherapy has been extensively discussed as part of the comprehensive treatment for LAGC [6]. Neoadjuvant chemotherapy (NCT) has been confirmed in subsequent studies to decrease tumor stage, eliminate micrometastasis, improve tolerance, increase the possibility of radical resection, boost the resection rate of patients with R0, and eventually increase patients’ overall survival times [7,8,9,10]. For locally advanced gastric cancer, neoadjuvant chemotherapy is recommended according to the gastric cancer guidelines of the National Comprehensive Cancer Network (NCCN) [11].
In the implementation of neoadjuvant chemotherapy, there are many clinical details that need attention during clinical practice, such as individual chemotherapy drug selection, selection of preoperative cycles, and interval time to surgery when finishing the preoperative chemotherapy. The interval time to surgery is a problem that needs to be comprehensively considered and evaluated by physicians and surgeons for gastric cancers. Patients whose symptoms have not yet resolved due to chemotherapy-related toxicities, deterioration of nutritional status, or serious comorbidities may have worse outcomes following surgery [12, 13]. However, concomitant surgical delay may worsen the prognosis, cause emotional suffering, and lower the quality of life [14, 15]. There is currently no consensus on the appropriate interval time to surgery (TTS) following the completion of NCT for LAGC, although primary tumor excision is often conducted within a few weeks following the last preoperative chemotherapy dose. Augustinas et al. [16] suggest that a greater rate of major pathologic response (mPR) was seen when there was less than 30 days between the conclusion of NCT and gastrectomy, while Liu et al. [17] described an interval time of more than 6 weeks as having relatively high odds of pathologic complete response (pCR).
Therefore, we conducted this research to analyze the optimal time interval from the end of chemotherapy to surgery for LAGC. The overall survival outcomes between different time intervals (< 4 weeks, 4–6 weeks, and > 6 weeks) were the primary endpoints in the present study.
Materials and methods
The Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 [18] criteria were followed throughout the course of this systematic review and meta-analysis. On October 18, 2022, we prospectively registered this study on PROSPERO with the identifier CRD42022365196 as part of our project.
Literature search
To find relevant studies, a systemic search was performed on the PubMed, Cochrane Library, Web of Science databases, and Embase.com, with some adjustments made to the subject words and free words to make it more specific to each database. The search strategies were developed by QL, and the PubMed search strategies were as follows: ((“Stomach Neoplasms”[Mesh]) OR (((((Gastric Neoplasms[Title/Abstract]) OR (Stomach Cancers[Title/Abstract])) OR (Gastric Cancer[Title/Abstract])) OR (gastric carcinoma[Title/Abstract])) OR (gastric tumor [Title/Abstract]))) AND (("Neoadjuvant Therapy"[Mesh]) OR ((((((neoadjuvant chemotherapy [Title/Abstract]) OR (new adjuvant chemotherapy[Title/Abstract])) OR (new auxiliary chemotherapy[Title/Abstract])) OR (preoperative adjuvant chemotherapy [Title/Abstract])) OR (neoadjuvant chemical therapy[Title/Abstract])) OR (new supplementary chemotherapy[Title/Abstract]))). By manually searching the references of the included publications, studies were found that had been missed during the initial literature search. The last date of the search was November 12, 2022.
Inclusion and exclusion
For consideration in this systematic review, studies were required to fulfil the following conditions: (1) patients have not developed distant metastasis, (2) patients are treated surgically after preoperative chemotherapy, and (3) TTS is documented. The exclusion criteria were as follows: (1) studies that were not reviewed by experts in the field, (2) the relevant information about the patient was not recorded, and (3) languages other than English.
Literature screening
After the initial search was completed and duplicates were automatically removed, the two authors (Q. L. and S. T. H.) independently reviewed all the articles. First, titles and abstracts were used to sort the papers into relevant groups for further screening. Next, the two authors downloaded the full articles of relevant studies and manually screened them for inclusion and exclusion according to the current study’s inclusion and exclusion criteria. If there were any disagreements, the team talked discussed, and the third reviewers (J. K. H. and W. H. Z.) verified the consensus. Every author was responsible for overseeing the project.
Data extraction
First, we set up a table to extract the basic information of the studies, and two authors used the same table to collect the data independently. The following data were collected: author, publication year, title, country, type of study, time-to-surgery interval, sample size, stage of patients, regimen of NCT, time of follow-up, perioperative complications, and postoperative survival outcomes. The 3-year OS and DFS data with time-outcome events were extracted from the survival curve. If the necessary information was missing from the primary source, we reached out to the study’s corresponding author to collect this material. Any discrepancies were settled by the third reviewers (J. K. H. and W. H. Z.).
Quality assessment
Two authors (Q. L., S. T. H.) independently analyzed the five included retrospective studies for methodological quality and resolved disagreements through consultation. Studies were assessed for their quality using the Newcastle–Ottawa Quality Assessment Scale (NOS) [19]. The NOS were classified into three groups based on their characteristics: selection, comparability, and exposure/outcome and then sorted into eight distinct categories. Each high-quality selection and exposure/outcome could receive up to one more star, and the comparability categorization could receive up to two more stars. Finally, according to the stars, the studies were ranked as high (six to nine stars) or low (zero to five stars) quality.
Statistical analysis
The I2 and Q statistics were used to assess the degree of heterogeneity between the included studies. Considering the heterogeneity in study characteristics such as patient inclusion and exclusion criteria, time-to-surgery interval heterogeneity, chemotherapy regimens, and medical conditions, I2 > 50% or P < 0.1 was considered substantial heterogeneity. When there was no substantial heterogeneity, the fixed-effects model was selected over the random-effects model. In addition, the random-effects model was utilized. Hazard ratios for survival outcomes were calculated as 95% confidence intervals (CIs). Both fixed and random models were used to examine the possible impact of model choice on the meta-analysis results. The ancillary tools used in this meta-analysis include RevMan 5.4.1 software (RevMan Cochrane Training), Engauge Digitizer software (http://digitizer.sourceforge.net), and R statistical software (Version 4.2.2). In addition, statistical significance is assumed at the P < 0.05 level.
Results
Study selection
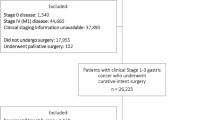
The number of potentially relevant studies identified through the literature search across four databases was 4880, and after automatic deduplication, 3268 articles were identified as the only literature. After reading the titles and abstracts of the 3268 articles, 3254 were ruled ineligible, leaving 14 articles to be reviewed in full text. Five studies were disqualified because of a literature review or insufficient data; a lack of data led to the exclusion of one protocol study, and three studies were abstracts from conferences. Manually searching the reference lists did not yield any additional studies. There were only five studies [16, 17, 20,21,22] that satisfied all of the inclusion criteria set by this meta-analysis, so only those results were used. The entire systematic literature review is shown in Fig. 1.
Study characteristics
Table 1 provides detailed information on the five studies included in this study. These five studies [16, 20,21,22,23], published between 2018 and 2021, included 1171 patients with LAGC who were treated with surgery after NCT from 2006 to October 2018. The NCT regimens included S-1 and oxaliplatin (SOX); epirubicin, oxaliplatin, and capecitabine (EOX); capecitabine and oxaliplatin (XELOX); epirubicin, cisplatin, and 5-FU (ECF); docetaxel, oxaliplatin, leucovorin, and 5-fluoracil (FLOT); fluoropyrimidine- and platinum-based doublet (FP); epirubicin, cisplatin, and capecitabine (ECX); and other chemotherapy regimens. The five studies differed in their TTS groupings. Three studies [17, 20, 22] examined three TTS, including > 6 weeks, 4–6 weeks, and < 4 weeks. In one study [16], TTS was divided into ≥ 43 days, 31–42 days, and ≤ 30 days. Patients whose TTS ≥ 43 days, 31–42 days, and ≤ 30 days were classified as belonging to the > 6 weeks, 4–6 weeks, and < 4 weeks, respectively, for the purposes of data analysis. In another study [21], TTS was divided into ≤ 21 days, 22–28 days, 29–35 days, 36–42 days, and 43–84 days. Likewise, TTS ≤ 21 days and 22–28 days combined were considered < 4 weeks, TTS 29–35 days and 36–42 days combined were considered 4–6 weeks, and TTS 43–84 days were considered > 6 weeks. Therefore, the number of patients included in the analysis was 411 with TTS < 4 weeks, 507 with TTS 4–6 weeks, and 253 with TTS > 6 weeks. Based on the NOS assessment [19], five studies were reviewed, with four receiving seven stars (showing high quality) and one receiving eight stars (also indicating high quality).
Overall survival
The overall survival outcomes were reported in all five studies [16, 17, 20,21,22]. According to the study’s findings, in terms of overall survival outcomes, no statistically significant differences were found among < 4 weeks and 4–6 weeks (HR 1.04, 95% CI: 0.69–1.57, and P = 0.85) and > 6 weeks (HR 0.83, 95% CI: 0.52–1.33, and P = 0.44). There was a significant decline in overall survival associated with > 6 weeks when compared to 4–6 weeks (HR 1.34, 95% CI: 1.03–1.75, and P = 0.03) and no significant heterogeneity (I2 = 0%, P = 0.48). Figure 2 demonstrates these results.
Disease-free survival
DFS was noted in four studies [16, 17, 20, 21], and 393 individuals with TTS < 4 weeks, 481 individuals with TTS 4–6 weeks, and 237 individuals with TTS > 6 weeks were ultimately incorporated into the analysis.
The final study revealed that the HR values for DFS were 0.96 (< 4 weeks vs. 4–6 weeks, 95% CI: 0.77–1.20 and P = 0.73), 0.88 (< 4 weeks vs. > 6 weeks, 95% CI: 0.51–1.51, and P = 0.64), and 1.13 (> 6 weeks vs. 4–6 weeks, 95% CI: 0.73–1.75, and P = 0.58), respectively. There were no statistically significant differences between the comparison groups. These outcomes are displayed in Fig. 3.
Pathological response
Pathological complete response (pCR) data from four of the five studies were published [17, 20,21,22], and all of the studies included evaluations of curative effects according to RECIST1.1 [24]. According to the results of the final analysis, the odds ratio (OR) values for pCR were 1.24 (< 4 weeks vs. 4–6 weeks, 95% CI: 0.72–2.14, and P = 0.44), 0.61 (< 4 weeks vs. > 6 weeks, 95% CI: 0.32–1.15, and P = 0.13), and 1.70 (> 6 weeks vs. 4–6 weeks, 95% CI: 0.93–3.31, and P = 0.09), respectively. The comparative groups did not differ significantly from one another. These outcomes are shown in Fig. 4.
Data on the pathologic response were reported in three of the five studies [16, 20, 22]. One of the studies [16] evaluated the curative effect according to Becker et al. [25], which was excluded from the pooled analysis. The other two articles [20, 22] used RECIST1.1 [24], and the analysis results suggested that the OR values for mPR were 1.21 (< 4 weeks vs. 4–6 weeks, 95% CI: 0.68–2.17, and P = 0.51), 0.99 (< 4 weeks vs. > 6 weeks, 95% CI: 0.50–1.94, and P = 0.97), and 1.22 (> 6 weeks vs. 4–6 weeks, 95% CI: 0.66–2.27, and P = 0.52), respectively. The comparative groups did not differ significantly from one another. These outcomes are displayed in Fig. 5.
Postoperative complications
A total of 36.74% of patients (187/509) experienced postoperative complications according to two papers on postoperative complications [16, 20]. The findings of the final analysis show that OR for postoperative complications was 0.84 (< 4 weeks vs. 4–6 weeks, 95% CI: 0.54–1.30, and P = 0.42), 0.90 (< 4 weeks vs. > 6 weeks, 95% CI: 0.54–1.49, and P = 0.67), and 0.93 (> 6 weeks vs. 4–6 weeks, 95% CI: 0.59–1.45, and P = 0.74), respectively. The comparative groups did not differ significantly from one another. These results are shown in Fig. 6.
Discussions
This meta-analysis was performed to evaluate whether there is a correlation between the TTS and survival outcomes for patients with LAGC. Although surgery following neoadjuvant chemotherapy at intervals of 4–6 weeks has been adopted in some clinical studies [6, 24, 26], there is no definitive evidence for this interval or for shortening or prolonging it. This research included 1171 individuals with LAGC, and it was concluded that those with TTS 4–6 weeks had improved overall survival; however, there was no appreciable improvement in disease-free survival.
The optimal time to have surgery following neoadjuvant chemotherapy or radiation varies depending on the specialty. Regarding rectal cancer, evidence from several randomized controlled trials has suggested that patients with rectal cancer have higher pCR, better prognosis, and better recurrence-free survival with longer intervals between operations after chemoradiotherapy [27,28,29]. The results of a meta-analysis of 26 trials showed that the PCR and downstaging rates for patients with rectal cancer were higher, and that there was longer DFS survival without increased surgical morbidity given a delay of at least 8 weeks between the end of NCT and surgery [30]. It is possible that this is because rectal cancer patients’ responses to chemoradiotherapy are time dependent, with complete tumor regression taking several months [31]. These findings suggest that prolonging the surgical interval beyond 8 weeks may facilitate surgical resection rather than impede it. Similarly, in breast cancer research, Rachel A. Sanford et al. [32] sought to delve into the link between TTS and survival outcomes. Their research of 110 breast cancer patients treated with NCT suggested that an interval between NCT and surgery of 4–6 weeks had a favorable effect on OS compared with TTS < 4 weeks or > 6 weeks.
For gastric cancers, many researchers have attempted to find the best TTS to improve the prognosis of patients. Wang et al. [21] categorized 426 patients with LAGC into five groups to determine whether different time intervals to surgery would improve patient outcomes. They found that patients who underwent surgery within 22–35 days had a better OS (P = 0.001) and DFS (P = 0.017) without increasing postoperative complications or decreasing pCR rates [21]. Liu et al. classified 176 patients into TTS < 4 weeks, 4–6 weeks, and > 6 weeks, indicating that patients with TTS > 6 weeks had a better pCR compared to those with TTS of 4–6 weeks, but OS and DFS were not significantly different [17]. However, Wu et al.’s findings suggest that TTS has no effect on histopathological response or survival results [20]. In our study, we found that patients with TTS of 4–6 weeks have a survival benefit, and those with TTS > 6 weeks or < 4 weeks have no advantage in survival. However, limited by the included research, the number of cases, and the low level of evidence, the optimal TTS selection may be restricted at 4–6 weeks. Integrated current evidence and NCCN guidelines recommend that TTS of 4–6 weeks might be a better option for LAGC patients.
In addition, improving the R0 resection rate and pCR rate is another treatment objective of NCT [33]. The tumor pathological response rate is one of the important evaluation indices of drug treatment. Tumor pathology responses have been demonstrated to be related to increased survival in LAGC, and the major pathological responses have a beneficial effect on OS and pCR [34, 35]. However, in this study, not all studies included reporting of the tumor pathological response rate. Based on the limited number of studies, the TTS and pathological response were not correlated.
Because surgical trauma and gastric cancer lymph node clearing range and neoadjuvant chemotherapy inevitably cause a reaction, tissue edema fibrosis can raise the possibility of complications during and after surgery [36]. The choice of appropriate TTS must also be considered from the perspective of balancing systemic and local reactions and long-term survival after chemotherapy. However, fewer studies have been conducted on the correlation between TTS and intraoperative and postoperative complications; therefore, additional prospective studies are needed to test and confirm these assumptions.
On the other hand, NCT brings a greater survival benefit than chemotherapy after surgery for resectable gastric cancer [37]. A recent meta-analysis reported that TPF (taxane and platinum plus fluoropyrimidine) triple neoadjuvant chemotherapy was more beneficial for pCR, OS, and DFS in patients with gastric cancer than other regimens [38]. NCT may be associated with increased morbidity and mortality [23]. NCT may cause adverse events such as leukopenia, neutropenia, nausea and vomiting, and fatigue in patients, with a higher incidence of triple therapy [38]. Prolonged TTS in some patients may be related to these complications.
Limitations
The main limitation of the study is that only five retrospective clinical studies were included. The primary aim of this study was to analyze the effects of the time interval to surgery on the outcome of neoadjuvant therapy for gastric cancer patients. The limited number of investigations and the majority of studies are from one country affected the power of the study and could be a of cause research bias. In addition, we did not analyze the effects of different drug regimens of TTS on the efficacy of neoadjuvant therapy. In the present study, we did not limit the neoadjuvant drug regimens that were included in the study. However, all of the studies included in the analysis were not restricted to single chemotherapy regimens but adopted multi-chemotherapy regimens. Therefore, the effects of different drug regimens of TTS on treatment outcome were not analyzed. Last, there are many factors that affect the short-term and long-term efficacy of neoadjuvant therapy. For example, immune status, primary tumor stage, and tumor molecular characteristics are all important influencing factors. Due to the limited number of retrospective clinical studies, the influences of these factors on TTS and treatment outcome were not analyzed in this study.
Although with this, our study suggests that a time interval to surgery of 4–6 weeks after neoadjuvant chemotherapy may be the most appropriate choice for patients with advanced gastric cancer treated with neoadjuvant chemotherapy based on current clinical evidence. Of course, to make better treatment decisions and choose the appropriate TTS for different patients, more high-quality research is worth looking forward to in the future. Perhaps prospective, large sample, and multicenter research will be helpful for solving this problem.
Conclusions
The current meta-analysis revealed that surgery within 6 weeks after NCT in patients with LAGC is associated with increased overall survival. Certainly, further clinical trials are warranted to ascertain the survival benefit of TTS of 4–6 weeks for patients with gastric cancer.
Availability of data and materials
On reasonable request, the corresponding author will provide the data that support the conclusions of this study.
Abbreviations
- LAGC:
-
Local advanced gastric cancer
- NCT:
-
Neoadjuvant chemotherapy
- TTS:
-
Interval time to surgery
- mPR:
-
Major pathologic response
- pCR:
-
Pathologic complete response
- DFS:
-
Disease-free survival
- OS:
-
Overall survival
- NOS:
-
Newcastle-Ottawa Quality Assessment Scale
References
Sung H, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Sexton RE, et al. Gastric cancer: a comprehensive review of current and future treatment strategies. Cancer Metastasis Rev. 2020;39(4):1179–203.
Cunningham SC, et al. Survival after gastric adenocarcinoma resection: eighteen-year experience at a single institution. J Gastrointest Surg. 2005;9(5):718–25.
Chen W, et al. Annual report on status of cancer in China, 2011. Chin J Cancer Res. 2015;27(1):2–12.
Zheng R, et al. Cancer incidence and mortality in China, 2016. JNCC. 2022;2(1):1–9.
Cunningham D, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20.
Coccolini F, et al. Neoadjuvant chemotherapy in advanced gastric and esophago-gastric cancer. Meta-analysis of randomized trials. Int J Surg. 2018;51:120–7.
van Hagen P, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med. 2012;366(22):2074–84.
Ajani JA, et al. Paclitaxel-based chemoradiotherapy in localized gastric carcinoma: degree of pathologic response and not clinical parameters dictated patient outcome. J Clin Oncol. 2005;23(6):1237–44.
Lowy AM, et al. A pilot study of preoperative chemoradiotherapy for resectable gastric cancer. Ann Surg Oncol. 2001;8(6):519–24.
Ajani JA, et al. Gastric cancer, version 2.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2022;20(2):167–92.
Charalampakis N, et al. Co-morbidities rather than age impact outcomes in patients receiving preoperative therapy for gastroesophageal adenocarcinoma. Ann Surg Oncol. 2017;24(8):2291–301.
Robb WB, et al. High-grade toxicity to neoadjuvant treatment for upper gastrointestinal carcinomas: what is the impact on perioperative and oncologic outcomes? Ann Surg Oncol. 2015;22(11):3632–9.
Robinson KM, et al. Diagnostic delay, quality of life and patient satisfaction among women diagnosed with endometrial or ovarian cancer: a nationwide Danish study. Qual Life Res. 2012;21(9):1519–25.
Gray RE, et al. Presurgery experiences of prostate cancer patients and their spouses. Cancer Pract. 1999;7(3):130–5.
Bausys A, et al. Impact of the interval between neoadjuvant chemotherapy and gastrectomy on short- and long-term outcomes for patients with advanced gastric cancer. Ann Surg Oncol. 2021;28(8):4444–55.
Liu Y, et al. Timing of surgery after neoadjuvant chemotherapy for gastric cancer: impact on outcomes. World J Gastroenterol. 2018;24(2):257–65.
Hutton B, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Wu C, et al. Impact of the time from the completion of neoadjuvant chemotherapy to surgery on the outcomes of patients with gastric cancer. Transl Cancer Res. 2019;8(5):1853–62.
Wang Y, et al. Optimal timing to surgery after neoadjuvant chemotherapy for locally advanced gastric cancer. Front Oncol. 2020;10:613988.
Ocaña Jiménez J, et al. Impact of interval timing to surgery on tumor response after neoadjuvant treatment for gastric cancer. Rev Esp Enferm Dig. 2020;112(8):598–604.
Lin JX, et al. Effectiveness and safety of apatinib plus chemotherapy as neoadjuvant treatment for locally advanced gastric cancer: a nonrandomized controlled trial. JAMA Netw Open. 2021;4(7):e2116240.
Watanabe H, et al. New response evaluation criteria in solid tumours-revised RECIST guideline (version 11). Gan To Kagaku Ryoho. 2009;36(13):2495–501.
Becker K, et al. Histomorphology and grading of regression in gastric carcinoma treated with neoadjuvant chemotherapy. Cancer. 2003;98(7):1521–30.
Schuhmacher C, et al. Neoadjuvant chemotherapy compared with surgery alone for locally advanced cancer of the stomach and cardia: European Organisation for Research and Treatment of Cancer randomized trial 40954. J Clin Oncol. 2010;28(35):5210–8.
Garrer WY, et al. Appropriate timing of surgery after neoadjuvant chemoradiation therapy for locally advanced rectal cancer. Asian Pac J Cancer Prev. 2016;17(9):4381–9.
Francois Y, et al. Influence of the interval between preoperative radiation therapy and surgery on downstaging and on the rate of sphincter-sparing surgery for rectal cancer: the Lyon R90–01 randomized trial. J Clin Oncol. 1999;17(8):2396.
Akgun E, et al. Randomized clinical trial of short or long interval between neoadjuvant chemoradiotherapy and surgery for rectal cancer. Br J Surg. 2018;105(11):1417–25.
Ryan EJ, et al. Meta-analysis of the effect of extending the interval after long-course chemoradiotherapy before surgery in locally advanced rectal cancer. Br J Surg. 2019;106(10):1298–310.
Overgaard M, Overgaard J, Sell A. Dose-response relationship for radiation therapy of recurrent, residual, and primarily inoperable colorectal cancer. Radiother Oncol. 1984;1(3):217–25.
Sanford RA, et al. Impact of time from completion of neoadjuvant chemotherapy to surgery on survival outcomes in breast cancer patients. Ann Surg Oncol. 2016;23(5):1515–21.
Ajani JA, et al. Enhanced staging and all chemotherapy preoperatively in patients with potentially resectable gastric carcinoma. J Clin Oncol. 1999;17(8):2403–11.
Tomasello G, et al. Tumor regression grade and survival after neoadjuvant treatment in gastro-esophageal cancer: a meta-analysis of 17 published studies. Eur J Surg Oncol. 2017;43(9):1607–16.
Smyth EC, et al. Gastric cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl 5):v38–49.
Yang H, et al. Application of gross tissue response system in gastric cancer after neoadjuvant chemotherapy: a primary report of a prospective cohort study. Front Oncol. 2021;11:585006.
Hu Y, et al. Neoadjuvant chemotherapy brings more survival benefits than postoperative chemotherapy for resectable gastric cancer: a meta-analysis of randomized controlled trials. J buon. 2019;24(1):201–14.
Wang T, et al. The optimal neoadjuvant chemotherapy regimen for locally advanced gastric and gastroesophageal junction adenocarcinoma: a systematic review and Bayesian network meta-analysis. Eur J Med Res. 2022;27(1):239.
Funding
(1) Medical Science and Technique Project of Health Commission of Sichuan Province (No. 21PJ043), (2) Natural Science Foundation of Sichuan Province (No. 23NSFSC1611), and (3) Post-Doctor Research Project, West China Hospital, Sichuan University (No. 2020HXBH162).
Author information
Authors and Affiliations
Contributions
Qi Ling and Shi-Ting Huang conceived and designed the study. All authors were responsible for data collection, analysis, interpretation, and generation of figures, and Qi Ling and Shi-Ting Huang were involved in writing of the paper. Wei-Han Zhang took part in paper checking and modification. Jian-Kun Hu gave final approval of the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ling, Q., Huang, ST., Yu, TH. et al. Optimal timing of surgery for gastric cancer after neoadjuvant chemotherapy: a systematic review and meta-analysis. World J Surg Onc 21, 377 (2023). https://doi.org/10.1186/s12957-023-03251-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-023-03251-y