Abstract
Background
Neoadjuvant chemotherapy (NAC) for locally advanced gastric and gastroesophageal junction adenocarcinoma (LAGC) has been recommended in several guidelines. However, there is no global consensus about the optimum of NAC regimens. We aimed to determine the optimal NAC regimen for LAGC.
Methods
A systematic review and Bayesian network meta-analysis was performed. The literature search was conducted from inception to June 2022. The odds ratio (OR) value and 95% confidence interval (95% CI) were used for assessment of R0 resection rate and pathological complete response rate (pCR) as primary outcomes. The hazard ratio (HR) value and 95% CI were interpreted for the assessment of overall survival (OS) and disease-free survival (DFS) as second outcomes. The risk ratio (RR) value and 95% CI were used for safety assessment.
Results
Twelve randomized controlled trials were identified with 3846 eligible participants. The network plots for R0 resectability, OS, and DFS constituted closed loops. The regimens of TPF (taxane and platinum plus fluoropyrimidine), ECF (epirubicin and cisplatin plus fluorouracil), and PF (platinum plus fluoropyrimidine) showed a meaningful improvement of R0 resectability, as well as OS and/or DFS, compared with surgery (including surgery-alone and surgery plus postoperative adjuvant chemotherapy). Importantly, among these regimens, TPF regimen showed significant superiority in R0 resection rate (versus ECF regimen), OS (versus ECF regimen), DFS (versus PF and ECF regimens), and pCR (versus PF regimen).
Conclusions
The taxane-based triplet regimen of TPF is likely the optimal neoadjuvant chemotherapy regimen for LAGC patients.
Similar content being viewed by others
Background
Despite many progresses made in early detection of gastric and gastroesophageal junction (GEJ) adenocarcinoma in the past decades, more than two-thirds of patients are diagnosed at advanced stages, and the overall survival remains low [1, 2]. In addition to radical surgery, multimodal approaches for gastric and GEJ cancer have been proposed to improve the prognosis. Preoperative chemotherapy for gastric and GEJ cancer was first reported in 1976 [3]. Until the MAGIC trial was reported in 2006, the perioperative chemotherapy with ECF regimen (epirubicin and cisplatin plus fluorouracil) for resectable adenocarcinoma of the stomach has been demonstrated to decrease tumor size and stage, and significantly improve progression-free and overall survival, as compared with surgery-alone [4]. In 2007, ECF regimen was officially recommended in the National Comprehensive Cancer Network (NCCN) guideline as category 1 evidence of neoadjuvant chemotherapy (NAC) for gastric cancer [5]. Since then, an increasing number of clinical trials concerning NAC for gastric and GEJ cancer have been conducted. NAC is better tolerated than postoperative adjuvant chemotherapy [6, 7]. Further, NAC improves the chance of radical resection [8], and eradicates potential micrometastases, and evaluates the chemosensitivity [4, 9]. Thus, NAC has gradually become the preferred approach for localized advanced gastric and GEJ cancer (LAGC). Currently, the guidelines for gastric and GEJ cancer of NCCN, European Society for Medical Oncology (ESMO), Japanese Gastric Cancer Association (JGCA) and Chinese Society of Clinical Oncology (CSCO) have described numerous recommended neoadjuvant treatments [7, 10,11,12].
However, there is no global consensus about the optimum of NAC regimens for LAGC. In clinical practice, physicians select a certain NAC regimen for specific patient mainly depending on the patient’s performance status in combination with physicians’ experience. Although accumulating meta-analyses have demonstrated significant survival or other benefits in favor of NAC or neoadjuvant chemoradiotherapy versus surgery in patients with gastric and GEJ adenocarcinoma [13, 14], there is still a lack of systematic evaluation of effectiveness and safety of each NAC regimen for determining the optimal regimen.
Unlike the conventional meta-analysis, network meta-analysis allows comparison of multiple NAC schemes in which there is no head-to-head comparison [15, 16]. Herein, a systematic review and Bayesian network meta-analysis was performed. Twelve randomized controlled trials (RCTs) concerning NAC for LAGC were identified from 17 published papers [4, 9, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31], which involved 11 regimens. To facilitate analysis, these regimens were categorized into four types based on pharmacology, named TP regimen [taxane (paclitaxel) plus platinum (cisplatin)], PF regimen [platinum (cisplatin or oxaliplatin) plus fluoropyrimidine (Fluorouracil or tegafur gimeracil oteracil potassium capsule (S-1) or capecitabine)], ECF regimen (epirubicin and cisplatin plus fluorouracil/capecitabine), and TPF regimen [taxane (docetaxel) and platinum (cisplatin or oxaliplatin) plus fluoropyrimidine (fluorouracil or S-1)]. The results revealed that the regimens of TPF, ECF, and PF showed a clinically meaningful improvement of R0 resectability, as well as overall survival (OS), and/or disease-free survival (DFS), compared with surgery. Importantly, among these regimens, TPF regimen showed significant superiority in R0 resection rate (versus ECF regimen), OS (versus ECF regimen), DFS (versus PF regimen and ECF regimen), and pathological complete response rate (versus PF regimen). TPF regimen showed a relatively higher incidence of the grade 3/4 adverse events than others, while the postoperative 30-day mortality in ECF regimen was increased compared those in TPF regimen and PF regimen. Collectively, this study provides a novel and definitive evidence that taxane-based triplet regimen, TPF, is an optimal NAC regimen for LAGC patients with good performance status.
Methods
This study was in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension statement for network meta-analyses (PRISMA-NMA) [32]. The protocol was registered with PROSPERO (CRD42022303124). The study was performed basing on the information from published literatures, and the Institutional Review Board exemption was granted for the innocuousness of the review study.
Search strategy
The literature search was conducted using PubMed, Embase, Web of Science, Cochrane Library, and ClinicalTrials.gov published in English from inception to June 2022. The search terms and the detailed retrieval strategies are listed in Additional file 3: Table S1. To avoid omission, the important conference abstracts were included, and the ongoing RCTs were followed for the latest advances, and the relevant references of the included articles were further searched. For the literatures published at different stages of the same study, the data were merged. The bibliographies of included studies were also checked for additional trials.
Study selection
The inclusion criteria included (1) phase II/III randomized controlled trials (RCTs); (2) histologically primary locally advanced adenocarcinoma of the stomach or gastroesophageal junction (GEJ) with no evidence of distant metastases or other unresectable factors; (3) studies comparing two or more treatment regiments of surgery (including surgery-alone and surgery plus postoperative adjuvant chemotherapy) and/or NAC; (4) two or more cycles of NAC, and (5) studies containing at least one efficacy and/or safety outcome, including R0 resection rate, pathological complete response (pCR), OS, DFS, grade 3/4 adverse events, and postoperative 30-day mortality.
The RCTs of radiotherapy, chemoradiotherapy, targeted therapy or immunotherapy, were excluded. The trials involving methotrexate and mitomycin, which were seldom used in gastric cancer chemotherapy currently, were also excluded [33, 34].
Data collection and study quality assessment
Two investigators independently performed literature searching, reviewing, and information extracting to a pre-determined spreadsheet. Any disagreement was resolved through discussion with another independent reviewer.
If the original literature did not provide the hazard ratio (HR) and 95% confidence interval (95% CI), the Engauge Digitizer and statistical formula were used to extract and calculate the natural logarithm (ln) of HR (ie, ln [HR]) and the standard error (SE) of the ln multiplied by the HR (ie, SE (ln [HR])) [35].
For safety assessment, the numbers of grade 3/4 adverse events and the deaths within 30 days after surgery that occurred in different NAC regimens were collected. The probability of an adverse event in each regimen was expressed as a percentage.
The Cochrane risk-of-bias tool was used to assess the risk of bias in an individual study, which is based on random sequence generation, allocation concealment, blinding of participating personnel, blinding of outcome assessment, outcome data integrity, selective reporting, and other biases. The risk of bias was assessed as high, low, or unclear.
Quality of evidence
The quality of evidence is assessed using four-step approach according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) [36], which is mainly based on the study limitations, reporting bias, inconsistency of results, indirectness of evidence and imprecision. The GRADE rates the quality of evidence as high, moderate, low, and very low quality. High quality of evidence represents the strong confidence in the estimate of effect [37].
Statistical analysis
All direct and indirect evidence were pooled to compare the efficacy and safety of different NAC regimens. The odds ratio (OR) value and 95% CI were used for assessment of R0 resection rate and pCR as primary outcomes. The corresponding HR value and 95% CI were interpreted for assessment of OS and DFS as second outcomes. The risk ratio (RR) value and 95% CI were used for safety assessment.
Statistical models based on the Bayesian framework were constructed using “gemtc” package in R (version 4.1.2) (RStudio, Boston, MA). The network plots were generated using Stata (version 14.0) (StataCorp, Texas, USA). For each analysis, four Markov chains were set, and each chain produced 50,000 iterations with the 20,000 iterations discarded as burn-in period. Convergence of iterations was assessed with trace plots and the Gelman–Rubin–Brooks statistic [38]. The ranking probability of regimens was estimated by calculating the surface under the cumulative ranking curve (SUCRA) for each regimen [39]. The SUCRA value ranges from 0 to 100%, where the regimens with higher SUCRA values are represented to have better efficacy.
To evaluate the consistency of direct and indirect evidence, the model fit was assessed by comparing the consistent model with the inconsistent model, and the node-splitting method was used to explore the local inconsistency [40]. Q test and I2 were used to assess the heterogeneity of studies. I2 values less than 25% were considered as low heterogeneity, 25–50% as medium heterogeneity, and above 50% as high heterogeneity. A comparative-adjusted funnel plots were used to identify the small sample effect between studies and to test publication bias.
Results
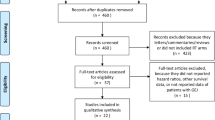
The literature retrieval process is shown in Fig. 1. Twelve RCTs were included in this study. A total of 3846 eligible participants were recruited, with sample size between 69 and 1022 patients. The characteristics of the included studies are shown in Table 1. As shown in Additional file 4: Table S2, the global I2 values and the results of local inconsistency test indicated that the fixed-effects models were suitable for analyzing R0 resection rate, OS, and DFS.
R0 resection rate
R0 resection rate after NAC was reported in all 12 studies. The network plot constituted a closed loop (Fig. 2A). As shown in Fig. 2B, C, the regimens of TPF (OR 2.57, 95% CI 1.73 to 3.86, P < 0.001), PF (OR 2.06, 95% CI 1.54 to 2.77, P < 0.001), and ECF (OR 1.65, 95% CI 1.15 to 2.38, P = 0.007) could improve the R0 resection rate compared with surgery, whereas TP did not enhance R0 resectability. The SUCRA values were 92.04% for TPF regimen, 70.24% for PF regimen, 45.95% for ECF regimen and 32.86% for TP regimen, and the SUCRA value for surgery was 8.91% (Fig. 2D). Importantly, TPF regimen showed significant improvement in curative resection rate versus ECF regimen (OR 1.56, 95% CI 1.09 to 2.23, P = 0.014), and there was no superiority among the remaining regimens.
Network meta-analysis of R0 resection rate. A Network of R0 resection rate. The size of the nodes and the thickness of the edges are weighted according to the number of studies evaluating each treatment and direct comparison, respectively. B Forest plots of comparisons for R0 resection rate (S, surgery). C Comparative effectiveness of neoadjuvant treatments in network meta-analysis. Hazard ratio (HR) (95% CI) for comparisons is in cells in common between column-defining and row-defining treatment. Bold cells are significant. HR < 1 favors column-defining treatment. D The SUCRA values of each regimen and surgery
Overall survival and disease-free survival
Eleven of 12 studies provided the results of OS and/or DFS. The network plots for OS or DFS constituted a closed loop (Fig. 3A, C). As shown in Fig. 3B, E, the triplet regimens including TPF (HR 0.69, 95% CI 0.57 to 0.84, P < 0.001) and ECF (HR 0.83, 95% CI 0.69 to 0.99, P = 0.043) could improve OS of the patients versus surgery, while the doublet regimens, PF and TP, did not have significant OS benefit. The SUCRA values were 91.35% for TPF regimen, 52.26% for ECF regimen, 50.84% for PF regimen and 46.13% for TP regimen. The SUCRA value for surgery was 9.42%. The pairwise comparison indicated that TPF regimen significantly improves OS versus ECF regimen (HR 0.84, 95% CI 0.71 to 0.99, P = 0.039), and there was no superiority among the remaining regimens.
Network meta-analysis of OS and DFS. A Network of OS. The size of the nodes and the thickness of the edges are weighted according to the number of studies evaluating each treatment and direct comparison, respectively. B Forest plots of comparisons for OS (S, surgery). C Network of DFS. The size of the nodes and the thickness of the edges are weighted according to the number of studies evaluating each treatment and direct comparison, respectively. D Forest plots of comparisons for DFS (S, surgery). E Comparative effectiveness of neoadjuvant treatments in network meta-analysis. Hazard ratio (HR) (95% CI) for comparisons is in cells in common between column-defining and row-defining treatment. Bold cells are significant. For OS, HR < 1 favors column-defining treatment. For DFS, HR < 1 favors row-defining treatment
As shown in Fig. 3D, E, the regimens of TPF (HR 0.59, 95% CI 0.49 to 0.71, P < 0.001), ECF (HR 0.73, 95% CI 0.61 to 0.87, P < 0.001), and PF (HR 0.80, 95% CI 0.69 to 0.92, P = 0.002) could improve DFS of the patients versus surgery, and the study of TP regime did not provide the result of DFS. The SUCRA values were 99.64% for TPF regimen, 59.96% for ECF regimen and 40.37% for PF regimen, and the SUCRA value for surgery was less than 1.0%. Importantly, TPF regimen had superiority in DFS over PF regimen (HR 0.74, 95% CI 0.60 to 0.93, P = 0.007) and ECF regimen (HR 0.81, 95% CI 0.69 to 0.96, P = 0.012), respectively. There was no significant difference in DFS between ECF regimen and PF regimen.
Pathological complete response
Postoperative pathological remission was analyzed in 11 of 12 studies. The patient number with pCR in each study was collected, and the pCR rate of each regimen was calculated. As shown in Fig. 4A, the pCR rate was 11.21% for TPF regimen, 7.21% for ECF regimen, 5.01% for PF regimen, and 5.13% for TP regimen. Importantly, the TPF regimen showed significant improvement in pCR compared with PF regimen (OR 2.40, 95% CI 1.55 to 3.69, P < 0.001), and there was no superiority among the remaining regimens (Fig. 4B).
Safety assessment
Nine of 12 studies reported the NAC-related complications. The grade 3/4 adverse events and postoperative 30-day mortality were reviewed systematically. The regimens of TPF, ECF, and PF showed certain incidences of adverse events and postoperative 30-day mortality (Additional file 1: Figure S1A). The study of TP regimen did not provide the results of adverse events.
As for hematological events, TPF and ECF regimens had higher incidence of neutropenia and leucopenia than PF regimen. The TPF regimen had more leucopenia than ECF regimen. The ECF regimen had higher incidence of serious thrombocytopenia. As for gastroenterological events, the highest incidence of nausea and vomiting occurred in ECF regimen. It was also higher in TPF regimen than that in PF regimen. The severest diarrhea occurred in TPF regimen, and the incidence of diarrhea was higher in ECF regimen than that in PF regimen. The incidence of fatigue was similar to that of nausea and vomiting among these regimens. In addition, these NAC regimens did not significantly increase the deaths within 30 days after surgery. However, the postoperative 30-day mortality in ECF regimen was increased compared with TPF regimen (RR 3.38, 95% CI 1.39 to 8.21, P = 0.007) or PF regimen (RR 2.59, 95% CI 1.33 to 5.05, P = 0.005) (Additional file 1: Figure S1B).
Quality assessment and publication bias
According to the Cochrane risk-of-bias tool, the bias assessment for eligible RCTs is shown in Additional file 2: Figure S2A with no severe risk of bias. The GRADE results of R0 resection rate, OS, and DFS are shown in Additional file 5: Table S3. The result of the comparison-adjusted funnel plots for R0 resection rate (Additional file 2: Figure S2B) did not show evidence of obvious asymmetry, suggesting the absence of publication bias.
Discussion
To our knowledge, this is the first network meta-analysis of RCTs to explore the effectiveness and safety of the NAC regimens for LAGC. The results indicate that the regimens of TPF, PF, and ECF enhance R0 resection rate and improve pCR, which results in survival benefits for the LAGC patients. Importantly, the taxane-based triplet regimen of TPF has been demonstrated to have significant advantages of R0 resectability, OS, DFS, and pCR among these regimens although it shows relatively higher prevalence of grade 3/4 adverse events, which makes TPF the optimal regimen for LAGC patients with good performance status.
The primary objective of NAC for LAGC is to increase R0 resection rate and pCR [8]. In this analysis, the regimens of TPF, PF, and ECF could significantly improve R0 resectability. Importantly, the effects of NAC regimens on R0 resection rate are consistent with those on survivals. Even if some studies suggested that the increased R0 resection rate usually cannot translate into a survival benefit [9], our study promotes us to attribute the survival advantages of NAC to the improved curative resectability. Basi et al. further suggested that R0 resection status can effectively predict mid-term survival in LAGC patients [41]. Intriguingly, TPF regimen had the superiority of R0 resectability over ECF regimen, and no difference was observed among TPF, PF, and TP regimen. Two grading systems, Becker or Mandard, are accepted to assess the tumor regression following NAC for LAGC [23]. Although they have different rating criterion, pCR remains consistent between them. In this analysis, the proportion of patients who achieved pCR ranged from 5.01% to 11.21%. Importantly, TPF regimen showed meaningful improvement in pCR compared with PF regimen, which is consistent with the increased R0 resectability and survival benefits. Major pathologic response has been demonstrated to be associated with the improvement of survival in LAGC patients [7, 42]. The study by Kurokawa et al. has indicated that pathological response exhibits higher response assessment validity and yields the best surrogate endpoint for OS [43].
The goal of any treatment strategy for cancer is to improve survival. Several meta-analyses have demonstrated the clinically significant survival benefits of NAC for LAGC patients compared with the upfront surgery or surgery plus postoperative adjuvant chemotherapy [14, 44, 45], and NAC even brings more survival benefits than postoperative chemotherapy for resectable gastric and GEJ cancer [46]. In this network meta-analysis, the triplet chemoagents, TPF and ECF, showed significant benefits of OS and DFS versus surgery. However, PF regimen exhibited only DFS benefit without OS benefit, and TP regimen had no survival benefit. This is an extraordinary finding. Although the study of Ychou et al. demonstrated perioperative chemotherapy using fluorouracil/cisplatin significantly increase DFS and OS in LAGC patients [17], several other trials did not show OS benefits of PF regimen [9, 22, 29]. Zhang et al. has reported that perioperative S-1/oxaliplatin (SOX) shows a clinically meaningful improvement of 3-year DFS compared with adjuvant capecitabine/oxaliplatin (CapOx) in patients with D2 gastrectomy [31]. SOX regimen has been recommended as NAC for potentially curable gastric cancer in CSCO guidelines [12]. The results of OS in Zhang’s study are worthy to be awaited to approve this recommendation. Importantly, TPF regimen showed significant advantages in OS and DFS over ECF regimen, and had DFS superiority over PF regimen, suggesting the optimality of TPF as NAC regimen for LAGC.
According to ethical principles, NAC is usually followed by postoperative adjuvant chemotherapy in LAGC patients, namely perioperative chemotherapy. Among these enrolled studies, patients in the intervention groups of two early studies received NAC without postoperative adjuvant chemotherapy [9, 18], and patients in the control groups of three early studies only underwent radical surgery without any chemotherapy [4, 9, 17]. Our analysis aimed to elucidate the NAC-related survival benefits for LAGC patients, but the subsequent postoperative adjuvant chemotherapy may influence the survivals. A latest meta-analysis demonstrated that perioperative triplet-based chemotherapy improves both OS and DFS compared to surgery alone or other preoperative strategies for gastric and GEJ cancer [47]. Currently, we cannot draw conclusion on the survival benefits of different combinations of NAC with postoperative adjuvant chemotherapy from these enrolled studies. Thus, further associated clinical trials are needed.
NAC seems to be associated with increased morbidity and mortality [48]. The safety assessment indicated that the triplet regimens had higher incidence of grade 3/4 adverse events, especially neutropenia, leucopenia, nausea and vomiting and fatigue, than the doublet therapy. Importantly, there were more leucopenia and diarrhea in TPF regimen than those in ECF regimen, and more nausea and vomiting and fatigue in ECF regimen than those in TPF regimen. Furthermore, the deaths within 30 days after surgery in ECF regimen were much more than those in TPF regimen and PF regimen. These results indicate that TPF regimen at least has the similar safety as ECF regimen.
Our study has some limitations. Although TPF regimen was shown to be the optimal option, we cannot perform further network meta-analysis for the optimal specific regimen in the category of TPF such as FLOT due to the lack of relevant studies. In addition, the optimal number of cycles is also an important issue for optimal regimen. However, we cannot draw clear conclusion of treatment duration of TPF regimen. The duration of these eligible RCTs ranged from 2 to 4 cycles, and the stratified analysis showed that the 3 or 4 cycles of NAC had more survival benefits than 2 cycles (Additional file 6: Table S4). Several clinical trials have been conducted for the optimal duration of certain regimens for LAGC [20, 21, 25, 26, 48]. An ongoing randomized controlled trial, RESONANCE-II [49], which evaluates the efficacy and safety of three versus six cycles of NAC SOX for LAGC patients, deserves to be expected.
Conclusions
The individualized selection of chemoagents is difficult. This study identified the triplet regimen of TPF to be the optimal NAC regimen for LAGC. Certainly, further clinical trials are warranted to ascertain the efficacy of taxane-based triplet regimen and optimal cycles of treatment.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- NAC:
-
Neoadjuvant chemotherapy
- OR:
-
Odds ratio
- RR:
-
Risk ratio
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- pCR:
-
Pathological complete response
- OS:
-
Overall survival
- DFS:
-
Disease-free survival
- TPF:
-
Taxane and platinum plus fluoropyrimidine
- ECF:
-
Epirubicin and cisplatin plus fluorouracil
- PF:
-
Platinum plus fluoropyrimidine
- TP:
-
Taxane plus platinum
- GEJ:
-
Gastroesophageal junction
- AC:
-
Adjuvant chemotherapy
- LAGC:
-
Localized advanced gastric and GEJ cancer
- ESMO:
-
European Society for Medical Oncology
- JGCA:
-
Japanese Gastric Cancer Association
- CSCO:
-
Chinese Society of Clinical Oncology
- RCTs:
-
Randomized controlled trials
- AEs:
-
Adverse events
- PRISMA-NMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension statement for network meta-analyses
- SE:
-
Standard error
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
- SUCRA:
-
Surface under the cumulative ranking curve
- SOX:
-
S-1/oxaliplatin
- CapOx:
-
Capecitabine/oxaliplatin
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Arnold M, Morgan E, Bardot A, Rutherford MJ, Ferlay J, Little A, et al. International variation in oesophageal and gastric cancer survival 2012–2014: differences by histological subtype and stage at diagnosis (an ICBP SURVMARK-2 population-based study). Gut. 2022. https://doi.org/10.1136/gutjnl-2021-325266.
Fujimoto S, Akao T, Itol B, Koshizuka I, Koyano K. A study of survival in patients with stomach cancer treated by a combination of preoperative intra-arterial infusion therapy and surgery. Cancer. 1976;37:1648–53.
Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Eng J Med. 2006;355(1):11–20.
NCCN Clinical Practice Guidelines in Oncology. 2007 Gastric Cancer. V.1(10).
Sah BK, Xu W, Zhang B, Zhang H, Yuan F, Li J, et al. Feasibility and safety of perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel for locally advanced gastric cancer patients in China. Front Oncol. 2021;10:567529.
Smyth EC, Verheij M, Allum W, Cunningham D, Cervantes A, Arnold D. ESMO guidelines committee. gastric cancer ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016. https://doi.org/10.1093/annonc/mdw350.
Ajani JA, Mansfield PF, Lynch PM, Pisters PW, Feig B, Dumas P, et al. Enhanced staging and all chemotherapy preoperatively in patients with potentially resectable gastric carcinoma. J Clin Oncol. 1999;17:2403–11.
Schuhmacher C, Gretschel S, Lordick F, Reichardt P, Hohenberger W, Eisenberger CF, et al. Neoadjuvant chemotherapy compared with surgery alone for locally advanced cancer of the stomach and cardia: European organisation for research and treatment of cancer randomized trial 40954. J Clin Oncol. 2010;28:5210–8.
Ajani JA, D’Amico TA, Almhanna K, Bentrem DJ, Chao J, Das P, et al. Gastric cancer, version 3.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2016;14:1286–312.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer. 2021. https://doi.org/10.1007/s10120-020-01042-y.
Wang FH, Zhang XT, Li YF, Tang L, Qu XJ, Ying JE, et al. The Chinese society of clinical oncology (CSCO): clinical guidelines for the diagnosis and treatment of gastric cancer, 2021. Cancer Commun (Lond). 2021;41:747–95.
Petrelli F, Ghidini M, Barni S, Sgroi G, Passalacqua R, Tomasello G. Neoadjuvant chemoradiotherapy or chemotherapy for gastroesophageal junction adenocarcinoma: a systematic review and meta-analysis. Gastric Cancer. 2019;22:245–54.
Jiang L, Yang KH, Guan QL, Chen Y, Zhao P, Tian JH. Survival benefit of neoadjuvant chemotherapy for resectable cancer of the gastric and gastroesophageal junction: a meta-analysis. J Clin Gastroenterol. 2015;49:387–94.
Rücker G. Network meta-analysis, electrical networks and graph theory. Res Synth Methods. 2012;3:312–24.
Fujii T, Le Du F, Xiao L, Kogawa T, Barcenas CH, Alvarez RH, et al. Effectiveness of an adjuvant chemotherapy regimen for early-stage breast cancer: a systematic review and network meta-analysis. JAMA Oncol. 2015;1:1311–8.
Ychou M, Boige V, Pignon JP, Conroy T, Bouché O, Lebreton G, et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 2011;29:1715–21.
Biffi R, Fazio N, Luca F, Chiappa A, Andreoni B, Zampino MG, et al. Surgical outcome after docetaxel-based neoadjuvant chemotherapy in locally-advanced gastric cancer. World J Gastroenterol. 2010;16:868–74.
Fazio N, Biffi R, Maibach R, Hayoz S, Thierstein S, Brauchli P, Bernhard J, Stupp R, Andreoni B, Renne G, Crosta C. Preoperative versus postoperative docetaxel–cisplatin–fluorouracil (TCF) chemotherapy in locally advanced resectable gastric carcinoma: 10-year follow-up of the SAKK 43/99 phase III trial. Ann Oncol. 2016;27(4):668–73.
Yoshikawa T, Tanabe K, Nishikawa K, Ito Y, Matsui T, Kimura Y, et al. Induction of a pathological complete response by four courses of neoadjuvant chemotherapy for gastric cancer: early results of the randomized phase II COMPASS trial. Ann Surg Oncol. 2014;21:213–9.
Yoshikawa T, Morita S, Tanabe K, Nishikawa K, Ito Y, Matsui T, et al. Survival results of a randomised two-by-two factorial phase II trial comparing neoadjuvant chemotherapy with two and four courses of S-1 plus cisplatin (SC) and paclitaxel plus cisplatin (PC) followed by D2 gastrectomy for resectable advanced gastric cancer. Eur J Cancer. 2016;62:103–11.
Xue K, Ying X, Bu Z, Wu A, Li Z, Tang L, et al. Oxaliplatin plus S-1 or capecitabine as neoadjuvant or adjuvant chemotherapy for locally advanced gastric cancer with D2 lymphadenectomy: 5-year follow-up results of a phase II-III randomized trial. Chin J Cancer Res. 2018;30:516–25.
Al-Batran SE, Hofheinz RD, Pauligk C, Kopp HG, Haag GM, Luley KB, et al. Histopathological regression after neoadjuvant docetaxel, oxaliplatin, fluorouracil, and leucovorin versus epirubicin, cisplatin, and fluorouracil or capecitabine in patients with resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4-AIO): results from the phase 2 part of a multicentre, open-label, randomised phase 2/3 trial. Lancet Oncol. 2016;17:1697–708.
Al-Batran SE, Homann N, Pauligk C, Goetze TO, Meiler J, Kasper S, Kopp HG, Mayer F, Haag GM, Luley K, Lindig U. FLOT4-AIO Investigators. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomised, phase 2/3 trial. The Lancet. 2019;393(10184):1948–57.
Aoyama T, Nishikawa K, Fujitani K, Tanabe K, Ito S, Matsui T, et al. Early results of a randomized two-by-two factorial phase II trial comparing neoadjuvant chemotherapy with two and four courses of cisplatin/S-1 and docetaxel/cisplatin/S-1 as neoadjuvant chemotherapy for locally advanced gastric cancer. Ann Oncol. 2017;28:1876–81.
Hayashi T, Yoshikawa T, Sakamaki K, Nishikawa K, Fujitani K, Tanabe K, et al. Primary results of a randomized two-by-two factorial phase II trial comparing neoadjuvant chemotherapy with two and four courses of cisplatin/S-1 and docetaxel/cisplatin/S-1 as neoadjuvant chemotherapy for advanced gastric cancer. Ann Gastroenterol Surg. 2020;4:540–8.
Sah BK, Zhang B, Zhang H, Li J, Yuan F, Ma T, et al. Neoadjuvant FLOT versus SOX phase II randomized clinical trial for patients with locally advanced gastric cancer. Nat Commun. 2020;11:6093.
Terashima M, Iwasaki Y, Mizusawa J, Katayama H, Nakamura K, Katai H, et al. Stomach cancer study group, japan clinical oncology group. randomized phase III trial of gastrectomy with or without neoadjuvant S-1 plus cisplatin for type 4 or large type 3 gastric cancer, the short-term safety and surgical results Japan clinical oncology group study (JCOG0501). Gastric Cancer. 2019;22:1044–52.
Iwasaki Y, Terashima M, Mizusawa J, Katayama H, Nakamura K, Katai H, et al. Gastrectomy with or without neoadjuvant S-1 plus cisplatin for type 4 or large type 3 gastric cancer (JCOG0501): an open-label, phase 3, randomized controlled trial. Gastric Cancer. 2021;24:492–502.
Kang YK, Yook JH, Park YK, Lee JS, Kim YW, Kim JY, et al. PRODIGY: a phase III study of neoadjuvant docetaxel, oxaliplatin, and S-1 plus surgery and adjuvant S-1 versus surgery and adjuvant S-1 for resectable advanced gastric cancer. J Clin Oncol. 2021;39:2903–13.
Zhang X, Liang H, Li Z, Xue Y, Wang Y, Zhou Z, et al. RESOLVE study group. Perioperative or postoperative adjuvant oxaliplatin with S-1 versus adjuvant oxaliplatin with capecitabine in patients with locally advanced gastric or gastro-oesophageal junction adenocarcinoma undergoing D2 gastrectomy (RESOLVE): an open-label, superiority and non-inferiority, phase 3 randomised controlled trial. Lancet Oncol. 2021;22:1081–92.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–84.
Hartgrink HH, van de Velde CJ, Putter H, Songun I, Tesselaar ME, Kranenbarg EK, et al. Cooperating Investigators of The Dutch Gastric Cancer Group. Neo-adjuvant chemotherapy for operable gastric cancer: long term results of the Dutch randomised FAMTX trial. Eur J Surg Oncol. 2004;30:643–9.
Ross P, Nicolson M, Cunningham D, Valle J, Seymour M, Harper P, et al. Prospective randomized trial comparing mitomycin, cisplatin, and protracted venous-infusion fluorouracil (PVI 5-FU) with epirubicin, cisplatin, and PVI 5-FU in advanced esophagogastric cancer. J Clin Oncol. 2002;20:1996–2004.
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16.
Puhan MA, Schünemann HJ, Murad MH, Li T, Brignardello-Petersen R, Singh JA, et al. GRADE Working Group. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE Working Group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Brooks SP, Gelman A. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat. 1998;7:434–55.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64:163–71.
Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29:932–44.
Basi A, Sohrabkhani S, Zamani F, Baghai-Wadji M, Rabiei N, Razavi SM, et al. Comparing efficacy of preoperative neo-adjuvant chemotherapy and surgery versus surgery alone in patients with resectable gastroesophageal cancer. Int J Hematol Oncol Stem Cell Res. 2013;7:24–8.
Tomasello G, Petrelli F, Ghidini M, Pezzica E, Passalacqua R, Steccanella F, et al. Tumor regression grade and survival after neoadjuvant treatment in gastro-esophageal cancer: a meta-analysis of 17 published studies. Eur J Surg Oncol. 2017;43:1607–16.
Kurokawa Y, Shibata T, Sasako M, Sano T, Tsuburaya A, Iwasaki Y, et al. Validity of response assessment criteria in neoadjuvant chemotherapy for gastric cancer (JCOG0507-A). Gastric Cancer. 2014;17:514–21.
Ge L, Wang HJ, Yin D, Lei C, Zhu JF, Cai XH, et al. Effectiveness of 5-flurouracil-based neoadjuvant chemotherapy in locally-advanced gastric/gastroesophageal cancer: a meta-analysis. World J Gastroenterol. 2012;18:7384–93.
Miao ZF, Liu XY, Wang ZN, Zhao TT, Xu YY, Song YX, et al. Effect of neoadjuvant chemotherapy in patients with gastric cancer: a PRISMA-compliant systematic review and meta-analysis. BMC Cancer. 2018;18:118.
Hu Y, Hu D, Li W, Yu X. Neoadjuvant chemotherapy brings more survival benefits than postoperative chemotherapy for resectable gastric cancer: a meta-analysis of randomized controlled trials. J BUON. 2019;24:201–14.
Grizzi G, Petrelli F, Di Bartolomeo M, Viti M, Moraes MT, Luciani A, et al. (2022) Preferred neoadjuvant therapy for gastric and gastroesophageal junction adenocarcinoma: a systematic review and network meta-analysis. Gastric Cancer. 2022;25:982–7.
Lin JX, Xu YC, Lin W, Xue FQ, Ye JX, Zang WD, et al. Effectiveness and safety of apatinib plus chemotherapy as neoadjuvant treatment for locally advanced gastric cancer: a nonrandomized controlled trial. JAMA Netw Open. 2021;4:e2116240.
Wang X, Li S, Sun Y, Li K, Shen X, Xue Y, et al. The protocol of a prospective, multicenter, randomized, controlled phase III study evaluating different cycles of oxaliplatin combined with S-1 (SOX) as neoadjuvant chemotherapy for patients with locally advanced gastric cancer: RESONANCE-II trial. BMC Cancer. 2021;21:20.
Acknowledgements
The authors are grateful to Prof. Ping Liu (Department of Oncology, the First Affiliated Hospital, Nanjing Medical University) for his constructive opinions, to Prof. Chao Wang (School of Public Health, Nanjing Medical University) and Prof. Chuanlin Ding (University of Louisville School of Medicine) for their critical review of this paper.
Funding
This study was financially supported by the National Natural Science Foundation of China (81871959), the Key R and D Program of Jiangsu Province (Social Development, BE2018758), and the Key Medical Talents Program of Jiangsu Province (ZDRCA2016014).
Author information
Authors and Affiliations
Contributions
LS, TW and CL conceptualized this study and determined the methodology. TW and CL performed data curation and statistical analysis, and wrote the original draft. XL provided assistance in data curation and statistical analysis. JZ and SW participated in reviewing and editing this manuscript. LS performed formal analysis, and reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Figure S1. Systematic review of NAC-related grade 3/4 adverse events and postoperative 30-day mortality. (A) The frequency of grade 3/4 adverse events and postoperative 30-day mortality in each regimen. (B) Forest plots of comparisons for grade 3/4 adverse events and postoperative 30-day mortality (S, surgery).
Additional file 2:
Figure S2. Quality assessment and publication bias. (A) Risk of bias graph for all studies included. (B) The comparison-adjusted funnel plots for R0 resection rate.
Additional file 3: Table S1.
The MeSH terms and the related entry terms.
Additional file 4: Table S2.
Heterogeneity analysis and node-splitting analysis of inconsistency.
Additional file 5: Table S3.
Estimates of effects and quality ratings for comparison of regimens of neoadjuvant chemotherapy for locally advanced gastric cancer.
Additional file 6: Table S4.
The stratified analysis of OS, DFS and R0 resectability according to treatment duration.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, T., Li, C., Li, X. et al. The optimal neoadjuvant chemotherapy regimen for locally advanced gastric and gastroesophageal junction adenocarcinoma: a systematic review and Bayesian network meta-analysis. Eur J Med Res 27, 239 (2022). https://doi.org/10.1186/s40001-022-00878-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40001-022-00878-7