Abstract
Background
Stromal cells in tumor microenvironment could promote immune escape through a variety of mechanisms, but there are lacking research in the field of gastric cancer (GC).
Methods
We identified differential expressed immune-related genes (DEIRGs) between the high- and low-stromal cell abundance GC samples in The Cancer Genome Atlas and GSE84437 datasets. A risk score was constructed basing on univariate cox regression analysis, LASSO regression analysis, and multivariate cox regression analysis in the training cohort (n=772). The median value of the risk score was used to classify patients into groups with high and low risk. We conducted external validation of the prognostic signature in four independent cohorts (GSE26253, n=432; GSE62254, n=300; GSE15459, n=191; GSE26901, n=109) from the Gene Expression Omnibus (GEO) database. The immune cell infiltration was quantified by the CIBERSORT method.
Results
The risk score contained 6 genes (AKT3, APOD, FAM19A5, LTBP3, NOV, and NOX4) showed good performance in predicting 5-year overall survival (OS) rate and 5-year recurrence-free survival (RFS) rate of GC patients. The risk death and recurrence of GC patients growing with the increasing risk score. The patients were clustered into three subtypes according to the infiltration of 22 kinds of immune cells quantified by the CIBERSORT method. The proportion of cluster A with the worst prognosis in the high-risk group was significantly higher than that in the low-risk group; the risk score of cluster C subtype with the best prognosis was significantly lower than that of the other two subtypes.
Conclusion
This study established and validated a robust prognostic model for gastric cancer by integrated analysis 1804 samples of six centers, and its mechanism was explored in combination with immune cell infiltration characterization.
Similar content being viewed by others
Background
Tumor microenvironment (TME) is a mixture of fluid, immune cells, stromal cells, and blood vessels that wrap the tumor [1]. Stromal cells are the main component of TME, including angiogenic vascular cell (AVC), cancer-associated fibroblast (CAF), and cancer-associated adipocyte cell (CAA) [2], which is closely related to the occurrence, development, invasion, and metastasis of the tumor [3, 4]. Therefore, stromal cells have been paid growing attention as a potential therapeutic target to effectively inhibit the progression of cancer [5,6,7].
The morbidity and mortality of gastric cancer (GC) have always been in the forefront of malignant tumors [8, 9]. Most patients with GC are in advanced stage when they are diagnosed, which leads to poor prognosis of GC after surgery [10]. In recent years, with the emergence of new treatments such as targeted therapy and immunotherapy [11, 12], the overall prognosis of GC has been greatly improved, but it is still unsatisfactory, and the conventional TNM staging is difficult to accurately evaluate the prognosis of GC after surgery, so developing an effective prognostic evaluation scheme has always been a research hotspot in the field of GC.
The immune response of tumor is an important process in the occurrence and development of tumor [13]. Without immune monitoring, the malignant biological behavior of tumor will be further accelerated, thus promoting the proliferation, invasion, and metastasis of tumor [14]. The latest study found that the synergistic action of stromal cells and immune cells makes TME appear as an immunosuppressive microenvironment, which provides favorable conditions for the growth and immune escape of tumor cells [15,16,17]. Therefore, understanding the interaction between stromal cells and immunophenotype plays is expected to find new targets to curb tumor progression.
This study explored the relationship between stromal cells and immune-related genes, established and validated a robust prognostic signature for GC by intergrated analysis of 1804 samples of six centers.
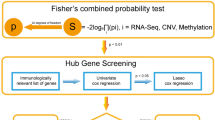
Materials and methods
Data acquisition
We obtained the gene expression profiles and corresponding clinical data from The Cancer Genome Atlas (TCGA, https://portal.gdc.cancer.gov/) and the Gene Expression Omnibus (GEO) database (GSE84437, https:// www.ncbi.nlm.nih.gov/geo/). There were 341 and 431 GC patients with completed prognostic information in the TCGA and the GSE84437 dataset respectively. The gene expression profiles and corresponding clinical data of the four independent cohorts (GSE26253, n=432; GSE62254, n=300; GSE15459, n=191; GSE26901, n=109) were downloaded from the GEO database. During the process of data acquisition, we complied with the access principles of TCGA and GEO database. The data analyzed in our work were acquired from public databases; the approval from the local ethics committee was not needed. The workflow of this study is shown in Fig. 1.
Estimation stromal cells abundance in tumor microenvironment of TCGA and GSE84437 dataset
ESTIMATE (Estimation of STromal and Immune cells in MAlignant Tumor tissues using Expression data) is a tool for predicting tumor purity based on single sample Gene Set Enrichment Analysis, and the presence of infiltrating stromal/immune cells in tumor tissues using gene expression data [18]. Stromal score generated from ESTIMATE algorithm captures the presence stroma in tumor tissue; generally, the higher the stromal score, the higher the stromal cell abundance in tumor tissue. We calculated the stromal score of the TCGA and GSE84437 dataset using the R package “estimate”. Patients in the two independent cohorts were divided into high- and low-stromal score groups according to the median value of stromal score respectively, the Kaplan-Meier survival analysis was used to compare the overall survival between the two groups, and the p value of log-rank test <0.05 was suggested to be statistical significance.
Identification of StromalScore Associated Immune-Related Genes (SAIRGs)
The immune-related gene list was obtained from the ImmPort database (https://immport.niaid.nih.gov). We extracted the immune-related genes from the TCGA and GSE84437 dataset, respectively, and identified the differentially expressed immune-related genes (DEIRGs) between the high- and low-stromal score group with Wilcoxon rank-sum test in “limma” R package in the TCGA and GSE84437 dataset. A false discovery rate (FDR) of < 0.001 was considered to be significant. The intersection DEIRGs of the two datasets were regarded as SAIRGs.
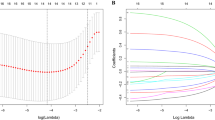
Development and validation of an immune-related gene prognostic signature
We used combat in R package “sva” to remove the batch effects between the TCGA and GSE84437 datasets and merged them into a training cohort contained 772 patients. The univariate Cox regression analysis was used for screening the prognostic related SAIRGs with p<0.05. The least absolute shrinkage and selection operator (LASSO) algorithm was applied to remove the overfitting between prognostic related genes with penalty parameter tuning performed via 10-fold cross-validation. We subsampled the dataset 1000 times and selected the genes over 900 repeated times while the LASSO penalized Cox analysis was implemented [19]. A subselection of genes was detected as a result of a penalty proportional to their size to shrink the regression coefficient [19]. Only genes with nonzero regression coefficients were retained for subsequent multivariate Cox regression analyses. A risk score was constructed using regression coefficients derived from multivariate Cox regression analysis of each gene multiple the expression level of each gene [20, 21]. The GC patients were classified into low-risk and high-risk groups considering the median risk score. The LASSO regression analysis was performed with “glmnet” R package. The Kaplan–Meier survival curve and the time depend ROC curve were generated with the R package “survminer” and “survivalROC” respectively to assess the performance of the risk score. The risk score’s performance was conducted external validation in four independent cohorts (GSE26253, n=432; GSE62254, n=300; GSE15459, n=191; GSE26901, n=109).
Immune cell infiltration (ICI) characterization
CIBERSORT is an analytical tool from the Alizadeh Lab developed by Newman et al. to provide an estimation of the abundances of member cell types in a mixed cell population, using gene expression data [22]. The 22 kinds of immune cell infiltration (ICI) proportions were quantified by the CIBERSORT method in this research; the samples with high prediction accuracy (p < 0.05) of prediction were considered for subsequent analysis [23].We conducted cluster analysis based on the R-package “consensusclusterplus” according to the results of ICI.
Results
The higher stromal score associated with poor prognosis of GC
The GC patients with higher stromal score who had unfavorable clinical outcome were observed in the two large sample and independent cohorts (Fig. 2A, C). Next, we identified the DEIRGs between the high- and low-stromal score group in the TCGA and GSE84437 respectively (Fig. 2B, D). A total of 167 intersection DEIRGs were retained the subsequent analysis (Fig. 2E).
Identification of StromalScore Associated Immune-Related Genes (SAIRGs). A The Kaplan–Meier survival analysis regarding stromal score and OS in the TCGA cohort. B The heatmap of differential expressed immune-related genes (DEIRGs) between the high- and low-stromal score in the TCGA cohort. C The Kaplan–Meier survival analysis regarding stromal score and OS in the GSE84437 cohort. D The heatmap of differentially expressed immune-related genes (DEIRGs) between the high- and low-stromal score in the GSE84437 cohort. E The Venn plot of intersection genes
Identification of prognostic related DEIRGs
The TCGA and GSE84437 datasets were intergrated into one large sample training cohort (n=772) for the establishment of the prognostic model. By univariate Cox regression analysis, we screened 79 prognostic related genes from the 167 intersection DEIRGs (Fig. 3).
Construction of a six-immune gene prognostic signature in the training cohort
A total of six genes were retained to construct the risk score by LASSO regression analysis and multivariate Cox regression analysis. The risk score = AKT3* 0.05467+ APOD* 0.002885+ FAM19A5* 0.05842+ LTBP3* 0.02132+ NOV* 0.0529+ NOX4* 0.1367. According to the median value, 386 patients with risk score greater than 0.9438 were assigned into the high risk group, and the remaining 386 patients with risk score less than 0.9438 were assigned into the low risk group. The patients in the high risk group showed significantly reduced overall survival (OS) compared to the low risk group (Fig. 4A). The area under the curve (AUC) values for the risk score predicting OS at 1, 3, and 5 years were 0.619, 0.631, and 0.645 respectively (Fig. 4B). As suggested by the univariate and multivariate Cox regression analysis, the risk score could be served as an independent prognostic risk factor (Fig. 4C, D).
Prognostic assessment of the risk score in the training cohort. A The Kaplan–Meier survival analysis regarding risk score and OS in the training cohort. B The time-dependent ROC analysis of the risk score for predicting the OS of patients in the training cohort. C The forest plot of the univariate Cox analysis. D The forest plot of the multivariate Cox analysis
The prognostic signature was applicable for patients with different clinical features
The six genes of the signature were all upregulated in the high risk group (Fig. 5A). The risk death of GC patients growing with the increasing risk score (Fig. 5B). The poor prognosis of high risk group in each clinical subgroup demonstrated the prognostic signature was suitable for patients with different clinical characteristics (Fig. 5C).
Internal validation of the prognostic signature in the TCGA and GSE84437 cohort
The patients in the high risk group exhibited significantly lower OS than the low risk patients in both TCGA and GSE84437 cohort (Fig. 6A, C). The AUC values of the risk score predicting 5-year survival rate of GC patients in TCGA and GSE84437 cohort were 0.661 and 0.666, respectively (Fig. 6B, D).
Internal validation of the risk score in the TCGA and GSE84437 cohort. A, B The Kaplan–Meier survival analysis and the time-dependent ROC analysis of the signature for predicting the OS of patients in the TCGA cohort. C, D The Kaplan–Meier survival analysis and the time-dependent ROC analysis of the signature for predicting the OS of patients in the GSE84437 cohort
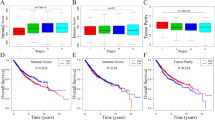
Exploration the relationship between the prognostic signature and the immune cell infiltration characterization
According to the infiltration of 22 kinds of immune cells, the patients were clustered into three subtypes (Fig. 7A, B). There were significant differences in the prognosis of different subtypes; cluster A had the worst prognosis, while cluster C had the best prognosis (Fig. 7C). The proportion of cluster A in high-risk group was significantly higher than that in low-risk group (Fig. 7D). The risk score of cluster A and cluster B was significantly higher than that of cluster C (Fig. 7E).
The relationship between the risk score and the immune cell infiltration characterization. A, B The heatmap and boxplot of immune cell infiltration for the three subtypes. C The Kaplan–Meier survival analysis the three subtypes. D The barplot of proportions of the three subtypes in high- and low-risk groups. E The vioplot of the risk score difference among the three subtypes
External validation of the prognostic signature in four independent cohorts
The high risk group had significantly lower overall survival (OS) and recurrence-free survival (RFS) in the four independent cohorts (Fig. 8A, D, G, J). The AUC values of the risk score predicting 5-year survival rate of GC patients in the GSE62254, GSE15459, and GSE26901 cohorts were 0.646, 0.700, and 0.723, respectively (Fig. 8B, E, H). The AUC values of the risk score predicting 5-year RFS of GC patients in the GSE26253 cohort was 0.640 (Fig. 7K). The high-risk group had a higher risk of death and recurrence (Fig. 8C, F, I, L).
External validation of the prognostic model. A, B The Kaplan–Meier survival analysis and the time-dependent ROC analysis of the signature for predicting the OS of patients in the GSE62254 cohort. C The distribution of risk score, and the survival status of patients in in the GSE84437 cohort. D, E The Kaplan–Meier survival analysis and the time-dependent ROC analysis of the signature for predicting the OS of patients in the GSE15459 cohort. F The distribution of risk score, and the survival status of patients in in the GSE15459 cohort. G, H The Kaplan–Meier survival analysis and the time-dependent ROC analysis of the signature for predicting the OS of patients in the GSE26901 cohort. I The distribution of risk score, and the survival status of patients in in the GSE26901 cohort. J, K The Kaplan–Meier survival analysis and the time-dependent ROC analysis of the signature for predicting the RFS of patients in the GSE26253 cohort. L The distribution of risk score, and the recurrent status of patients in in the GSE26253 cohort
Discussion
Tumor heterogeneity is one of the characteristics of malignant, and it is also a major challenge for human beings to overcome tumors [24]. Clinically, some blood indexes, such as lymphocyte/monocyte ratio, neutrophil/lymphocyte ratio, and platelet/lymphocyte ratio, are of great significance for monitoring the progress and prognosis of many diseases, including virus infection, autoimmune diseases, and so on, because of their advantages of dynamic and real-time detection [25]. Although simple blood indicators can provide reference for monitoring cancer treatment and guiding prognosis to a certain extent, they play a very limited role in evaluating tumor heterogeneity. The proposal of tumor microenvironment (TME) provides new insights for human beings to better understand the heterogeneity of tumors [26]. Stromal cells are one of the most abundant and critical components of TME, which could affect many aspects of tumor progression by remodeling extracellular matrix, such as proliferation, invasion, angiogenesis, and metastasis [27]. According to the latest viewpoint, stromal cells can also secrete a variety of cytokines and chemokines or indirectly interact with immune cells in tumor microenvironment to regulate the transformation, infiltration, and function of immune cells, making TME in an immunosuppressive state [28]. To further clarify the mechanism of stromal cells in tumor immune regulation is expected to find a new strategy for the treatment of cancer.
Gastric cancer (GC), as a common digestive system tumor, is the fifth largest malignant tumor in the world and the third leading cause of cancer death [29]. Surgical resection, radiotherapy, and chemotherapy are still the main treatment methods, but the effect is not ideal [12]. In recent years, experts in the field of GC research have pointed out that parameters reflecting individual immune status, such as preoperative systemic immune-inflammation index (SII) [30], Follistatin-like 1 (FSTL1) [31], immune T cell subsets (including CD3+, CD4+, CD8+, CD4+/CD8+ ratio, NK Cells) [32], the preoperative and the postoperative neutrophil-to-lymphocyte ratios (NLR) [33,34,35,36], and platelet-lymphocyte ratio (PLR) [37], may be useful prognostic indicators of GC. Previously studies have shown that immune-related genes can effectively predict the prognosis of patients with colonic adenocarcinoma [38], but the relationship between immune-related genes and the prognosis of GC has not been fully clarified. Considering the occult pathogenesis of GC, its recurrence and metastasis are closely related to tumor microenvironment; further understanding of the role of stromal cells in the immune regulation of GC is expected to improve the current treatment strategy for GC.
In two independent cohorts with a sample size of more than 300 (TCGA, GSE84437), we observed poor prognosis in patients with high stromal cell abundance, which further confirmed the negative effect of stromal cells on the prognosis of GC. By comparing the expression of immune genome in patients with high stromal score and low stromal score, we obtained a total of 167 common differential genes in two independent cohorts. TCGA and GSE84437 were intergrated into a large sample cohort (n=772) to analyze the prognostic value of the intersection genes. After univariate cox regression analysis, LASSO regression analysis, and multivariate cox regression analysis, a six-gene risk score was established.
Through internal validation (TCGA, n=341; GSE84437, n=431) and external validation (GSE26253, n=432; GSE62254, n=300; GSE15459, n=191; GSE26901, n=109), we found that risk score had good predictive ability for predicting 5-year overall survival (OS) rate and 5-year recurrence-free survival (RFS) rate of GC patients. The risk of death and recurrence increased with the increase of risk score, indicating that risk score played an important role in the progression of GC. Given the heterogeneity of GC, the robustness of risk score may be an effective auxiliary tool to evaluate the prognosis of GC.
In recent years, judging the prognosis of tumors by immunophenotype has become a research hotspot [39,40,41], but similar studies in GC are still very rare. We attempted to reveal the underlying mechanism of the risk score by performed the cluster analysis of immune cell infiltration (ICI). The patients were divided into three subtypes according to the difference of ICI. There were significant differences in the prognosis of different subtypes. Cluster A, the worst prognosis group, accounted for more than half of the high-risk group; the risk score of cluster C subtype with the best prognosis was significantly lower than that of the other two subtypes. Therefore, the difference of immune infiltration may be an important reason leading the difference of prognosis between different risk groups.
Stromal cells in tumor microenvironment have a variety of tumor-promoting functions and promote immune escape through a variety of mechanisms, but there are no clinical inhibitors for tumor stromal cells. In intrahepatic cholangiocarcinoma, m2 polarized tumor-associated macrophages promote epithelial-mesenchymal transformation by activating AKT3/PRAS40 signaling pathway [42]. In colorectal cancer, propofol inhibits cell proliferation and metastasis by regulating miR-124-3p.1/AKT3 [43]. In ovarian cancer, the overexpression of AKT3 could promote the proliferation and migration of cancer cells [44]. However, the specific role of AKT3 in the progression of gastric cancer is unknown. Apolipoprotein D (APOD) is a protein regulated by androgen and estrogen. The increased expression of APOD could predict poor prognosis in patients with breast cancer independent of the expression of ER α and AR [45]. In patients with mantle cell lymphoma, patients with high expression of FAM19A5 are more likely to relapse or die [46]. LTBP3 is a new cancer target protein, which has a unique function in the regulation of vascularization of tumor cells dependent on angiogenesis [47]. Nephroblastoma overexpressed protein (NOV), an early member of the CCN family, has recently been thought to be involved in a series of inflammatory processes such as wound healing, alveolar epithelial cell inflammation, cancer metastasis, and macrophage foam cell formation [48]. NOX4 played an important role in maintaining the phenotype of immunosuppressive cancer-associated fibroblasts (CAF) in tumors; immunotherapy could be enhanced by suppressing NOX4 to overcome CD8T cell rejection mediated by CAFs [49]. The above six molecules may be expected to become potential targets for targeted therapy of stromal cells.
This study provided new insights into the prognosis assessment of patients with gastric cancer by analyzing the gene expression profiles and prognostic data of 1804 patients from six centers. This is the largest scale retrospective study we have ever known about the development of a prognostic model for gastric cancer, but it does not mean that multicenter prospective studies are no longer necessary. The effect of stromal cells on tumor is not only limited to immune regulation, but also includes metabolic reprogramming and many other aspects, which need to be further explored. In addition, there are few reports on the specific role of the above six genes in the development of gastric cancer, which need to be further clarified.
Conclusion
This study established and validated a robust prognostic model for gastric cancer by intergrated analysis of 1804 samples of 6 centers, and its mechanism was explored in combination with immune cell infiltration characterization.
Availability of data and materials
The datasets analyzed for this study were obtained from The Cancer Genome Atlas (TCGA, https://portal.gdc.cancer.gov/) and Gene Expression Omnibus (GEO, https://www.ncbi.nlm.nih.gov/geo/).
Abbreviations
- GC:
-
Gastric cancer
- TCGA:
-
The Cancer Genome Atlas
- GEO:
-
Gene Expression Ominibus
- TME:
-
Tumor microenvironment
- ESTIMATE:
-
Estimation of STromal and Immune cells in MAlignant Tumor tissues using Expression data
- DEIRGs:
-
Differential expressed immune-related genes
- SAIRGs:
-
StromalScore Associated Immune-Related Genes
- LASSO:
-
Least absolute shrinkage and selection operator
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under curve
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- ICI:
-
Immune cell infiltration
References
Li F, Kitajima S, Kohno S, Yoshida A, Tange S, Sasaki S, et al. Retinoblastoma inactivation induces a protumoral microenvironment via enhanced CCL2 secretion. 2019;79(15):3903–15.
Egeblad M, Nakasone ES, Werb ZJD. Tumors as organs: complex tissues that interface with the entire organism. 2010;18(6):884–901.
Quail DF. Joyce JAJNm: Microenvironmental regulation of tumor progression and metastasis. 2013;19(11):1423–37.
Spaw M, Anant S. Thomas SMJMc: Stromal contributions to the carcinogenic process. 2017;56(4):1199–213.
Dykes SS, Hughes VS, Wiggins JM, Fasanya HO, Tanaka M, Siemann DJO. Stromal cells in breast cancer as a potential therapeutic target. 2018;9(34):23761.
Shi Y, Du L, Lin L. Wang YJNrDd: Tumour-associated mesenchymal stem/stromal cells: emerging therapeutic targets. 2017;16(1):35–52.
Onoyama M, Kitadai Y, Tanaka Y, Yuge R, Shinagawa K, Tanaka S, et al. Combining molecular targeted drugs to inhibit both cancer cells and activated stromal cells in gastric cancer. 2013;15(12):1391–9.
Thrift AP, El-Serag HBJCG. Hepatology: burden of gastric cancer. 2020;18(3):534–42.
Rawla P, Barsouk AJPg: Epidemiology of gastric cancer: global trends, risk factors and prevention. 2019, 14(1):26.
Patel TH, Cecchini MJCTOO. Targeted therapies in advanced gastric cancer. 2020;21(9):1–14.
Coutzac C, Pernot S, Chaput N, Zaanan AJCROH. Immunotherapy in advanced gastric cancer, is it the future? 2019;133:25–32.
Johnston FM, Beckman MJC. Updates on management of gastric cancer. 2019;21(8):67.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Mortezaee KJLS: Immune escape: a critical hallmark in solid tumors. 2020:118110.
Sun Q, Zhang B, Hu Q, Qin Y, Xu W, Liu W, et al. The impact of cancer-associated fibroblasts on major hallmarks of pancreatic cancer. 2018;8(18):5072.
Poggi A, Giuliani MJV. Mesenchymal stromal cells can regulate the immune response in the tumor microenvironment. 2016;4(4):41.
Poggi A, Varesano S, Zocchi MRJFii. How to hit mesenchymal stromal cells and make the tumor microenvironment immunostimulant rather than immunosuppressive. 2018, 9:262.
Yoshihara K, Shahmoradgoli M, Martínez E, Vegesna R, Kim H, Torres-Garcia W, Trevi O V, Shen H, Laird PW, Levine DAJNC. Inferring tumour purity and stromal and immune cell admixture from expression data. 2013, 4.
Huo J, Wu L, Zang YJFiO. Construction and validation of a universal applicable prognostic signature for gastric cancer based on seven immune-related gene correlated with tumor associated macrophages. 2021, 11.
Huo J, Wu L, Zang Y. A robust nine-gene prognostic signature associated with tumour doubling time for hepatocellular carcinoma. Life Sci. 2020;260:118396–6.
Huo J, Cai J, Guan G, Liu H, Wu L. A ferroptosis and pyroptosis molecular subtype-related signature applicable for prognosis and immune microenvironment estimation in hepatocellular carcinoma. 2021;9(3118).
Newman AM, Liu CL, Green MR, Gentles AJ, Feng W, Xu Y, Hoang CD, Diehn M, Alizadeh AAJNM. Robust enumeration of cell subsets from tissue expression profiles. 2015, 12(5):453-457.
Huo J, Wu L, Zang YJJotm. Eleven immune-gene pairs signature associated with TP53 predicting the overall survival of gastric cancer: a retrospective analysis of large sample and multicenter from public database. 2021, 19(1):1-18.
Polyak KJNM. Tumor heterogeneity confounds and illuminates: a case for Darwinian tumor evolution. 2014;20(4):344.
Nakamoto S, Ikeda M, Kubo S, Yamamoto M, Notsu AJSR. Systemic immunity markers associated with lymphocytes predict the survival benefit from paclitaxel plus bevacizumab in HER2 negative advanced breast cancer.
Hanahan D, Coussens LJCC. Accessories to the crime: functions of cells recruited to the tumor microenvironment. 2012;21(3):309–22.
Tlsty TD. Stromal cells can contribute oncogenic signals. In: Seminars in cancer biology: 2001: Elsevier; 2001. p. 97–104.
Barros MR, De Melo CML, Rego MLCMG, De Lima RDCP, De Freitas AC, Venuti AJJoE. Research CC: Activities of stromal and immune cells in HPV-related cancers. 2018, 37(1):137.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal AJCacjfc. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. 2018, 68(6):394-424.
Inoue H, Kosuga T, Kubota T, Konishi H, Shiozaki A, Okamoto K, et al. Significance of a preoperative systemic immune-inflammation index as a predictor of postoperative survival outcomes in gastric cancer. World J Surg Oncol. 2021;19(1):173.
Li L, Huang S, Yao Y, Chen J, Li J, Xiang X, et al. Follistatin-like 1 (FSTL1) is a prognostic biomarker and correlated with immune cell infiltration in gastric cancer. World J Surg Oncol. 2020;18(1):324.
Xin F, Mzee SAS, Botwe G, He H, Zhiyu S, Gong C, et al. Short-term evaluation of immune levels and nutritional values of EN versus PN in gastric cancer: a systematic review and a meta-analysis. World J Surg Oncol. 2019;17(1):114.
Kim EY, Song KY. The preoperative and the postoperative neutrophil-to-lymphocyte ratios both predict prognosis in gastric cancer patients. World J Surg Oncol. 2020;18(1):293.
Chen J, Hong D, Zhai Y, Shen P. Meta-analysis of associations between neutrophil-to-lymphocyte ratio and prognosis of gastric cancer. World J Surg Oncol. 2015;13(1):122.
Jin H, Zhang G, Liu X, Liu X, Chen C, Yu H, et al. Blood neutrophil-lymphocyte ratio predicts survival for stages III-IV gastric cancer treated with neoadjuvant chemotherapy. World J Surg Oncol. 2013;11(1):112.
Nakamura N, Kinami S, Fujii Y, Miura S, Fujita J, Kaida D, et al. The neutrophil/lymphocyte ratio as a predictor of peritoneal metastasis during staging laparoscopy for advanced gastric cancer: a retrospective cohort analysis. World J Surg Oncol. 2019;17(1):108.
Zhang X, Zhao W, Yu Y, Qi X, Song L, Zhang C, et al. Clinicopathological and prognostic significance of platelet-lymphocyte ratio (PLR) in gastric cancer: an updated meta-analysis. World J Surg Oncol. 2020;18(1):191.
Chen S, Cao GD, Wei W, Yida L, Xiaobo H, Lei Y, et al. Prediction and identification of immune genes related to the prognosis of patients with colon adenocarcinoma and its mechanisms. World J Surg Oncol. 2020;18(1):146.
Wartenberg M, Cibin S, Zlobec I, Vassella E, Eppenberger-Castori S, Terracciano L, Eichmann MD, Worni M, Gloor B, Perren AJCcr. Integrated genomic and immunophenotypic classification of pancreatic cancer reveals three distinct subtypes with prognostic/predictive significance. 2018, 24(18):4444-4454.
Abadie J, Nguyen F, Loussouarn D, Peña L, Gama A, Rieder N, Belousov A, Bemelmans I, Jaillardon L, Ibisch CJBcr et al. Canine invasive mammary carcinomas as models of human breast cancer. Part 2: immunophenotypes and prognostic significance. 2018, 167(2):459-468.
Wang Y, Feng W, Liu PJC. Genotype-immunophenotype analysis reveals the immunogenomic subtype and prognosis of multiple myeloma. 2020.
Sun D, Luo T, Dong P, Zhang N, Chen J, Zhang S, Dong L, Janssen HL, Zhang SJJoCB. M2-polarized tumor-associated macrophages promote epithelial-mesenchymal transition via activation of the AKT3/PRAS40 signaling pathway in intrahepatic cholangiocarcinoma. 2020, 121(4):2828-2838.
Li Y, Dong W, Yang H, Xiao GJBL. Propofol suppresses proliferation and metastasis of colorectal cancer cells by regulating miR-124-3p. 1/AKT3. 2020, 42(3):493-504.
Zhao J, Yang T, Ji J, Zhao F, Li C, Han XJCGT. RHPN1-AS1 promotes cell proliferation and migration via miR-665/Akt3 in ovarian cancer. 2020:1-9.
Jankovic-Karasoulos T, Bianco-Miotto T, Butler MS, Butler LM, McNeil CM, O’Toole SA, et al. Elevated levels of tumour apolipoprotein D independently predict poor outcome in breast cancer patients. 2020;76(7):976–87.
Wang Y-F, Huang S-Y, Zhang Z-H, Dong F, Wang Y, Jing H-M, Ke X-YJZsyxyxzz. Clinical efficacy of allo-HSCT on FLT3-ITD positive AML patients. 2020, 28(4):1183-1188.
Deryugina EI, Zajac E, Zilberberg L, Muramatsu T, Joshi G, Dabovic B, et al. LTBP3 promotes early metastatic events during cancer cell dissemination. 2018;37(14):1815.
Wei Y, Peng L, Li Y, Zhang N, Shang K, Duan L, Zhong J, Chen JJJoIR. Higher serum CCN3 is associated with disease activity and inflammatory markers in rheumatoid arthritis. 2020, 2020.
Ford K, Hanley CJ, Mellone M, Szyndralewiez C, Heitz F, Wiesel P, et al. NOX4 inhibition potentiates immunotherapy by overcoming cancer-associated fibroblast-mediated CD8 T-cell exclusion from tumors. 2020;80(9):1846–60.
Acknowledgements
None
Funding
None
Author information
Authors and Affiliations
Contributions
Junyu Huo and Liqun Wu designed this study, Ge Guan collected the data, and Junyu Huo analyzed the data in this study, interpreted the findings, and drafted the manuscript. Liqun Wu and Jinzhen Cai carried out the data management and revised the manuscript. All authors reviewed the final version of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huo, J., Guan, G., Cai, J. et al. Integrated analysis of 1804 samples of six centers to construct and validate a robust immune-related prognostic signature associated with stromal cell abundance in tumor microenvironment for gastric cancer. World J Surg Onc 20, 4 (2022). https://doi.org/10.1186/s12957-021-02485-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-021-02485-y