Abstract
Background
Monostotic fibrous dysplasia (MFD) involving the spine is rare, and the treatment options are controversial. Surgery is needed when patients suffer from persistent pain, spinal cord compression/injury, and vertebral collapse/instability. Treatment methods include biopsy/observation, corpectomy with instrumented fusion, posterior fusion, vertebroplasty (VP), curettage and bone graft, and complete removal of the vertebra with a combined anterior and posterior fusion procedure.
Case presentation
The patient was a 56-year-old woman with a 2-year history of neck pain. No obvious abnormalities were detected on neurological or physical examination, and laboratory findings were all within normal limits. An imaging examination suggested a C7 vertebral bone tumor. The patient refused to continue conservative observation treatment and requested surgery. Open VP of the C7 vertebral body was carried out, and her postoperative neck pain was completely relieved. The postoperative pathological results supported the diagnosis of fibrous dysplasia, and the patient was ultimately diagnosed with MFD. At the 12-month follow-up visit, the patient reported no clinical symptoms, and no signs of tumor recurrence were detected.
Conclusion
VP can relieve pain while stabilizing the spine. Thus, the surgical treatment of MFD vertebral lesions by VP is a valuable option.
Similar content being viewed by others
Background
Fibrous dysplasia (FD) was first reported by Lichtenstein in 1938 [1]. FD is a benign bone tumor in which normal bone tissue and bone marrow are replaced by proliferative fibrous tissue [2], representing approximately 5–7% of benign bone tumors [3]. FD can be classified as monostotic fibrous dysplasia (MFD) or polyostotic fibrous dysplasia (PFD). PFD may be accompanied by endocrine disorders such as McCune-Albright syndrome (MAS) [4]. MFD accounts for 70% of the reported cases of FD. However, MFD involving the cervical vertebrae is quite rare, and the treatment methods are controversial. Surgery is needed when patients suffer from persistent pain, spinal cord compression/injury, and vertebral collapse/instability. Here, we report a case of MFD at C7 that was successfully treated with vertebroplasty (VP). We also searched PubMed and the Web of Science with the keywords “fibrous dysplasia” and “spine” to evaluate the literature regarding the surgical treatment of cervical MFD and have provided a summary of the treatment of spinal FD with VP.
Case presentation
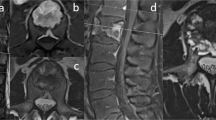
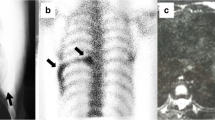
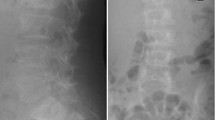
A 56-year-old female patient was admitted to our hospital with a 2-year history of neck pain. No obvious abnormalities were detected on neurological or physical examination, and laboratory findings were all within normal limits. Computed tomography (CT) (Fig. 1a, b) demonstrated low density in the seventh cervical vertebra, with high-density hardening visible around the edges. Magnetic resonance imaging (MRI) of the cervical spine (Fig. 1c, d) indicated an expansile lytic lesion with isointensity on T1-weighted imaging and hyperintensity on T2-weighted imaging. These findings were explained to the patient as the possible causes of neck pain, and options for continued conservative observation or surgical treatment were provided. The patient refused to continue conservative observation treatment and requested surgery. The preoperative treatment team communicated sufficiently about the case, considered the existing clinical data of benign bone tumors, and recommended two surgical treatment options: (1) open biopsy with direct excision and internal fixation, which would involve extensive trauma and a long recovery time, or (2) open biopsy with bone cement injection, with later treatment options to be determined according to the pathological results after surgery and reoperation to remove the lesion, if necessary. The patient chose the scheme 2. C7 VP was performed after inducing general anesthesia. Imaging examinations were performed at 3 days, 6 months, and 1 year after surgery (Fig. 2a, b; 3a; 4a, b). The postoperative pathological results supported the diagnosis of FD (Fig. 5a, b), and the patient was ultimately diagnosed with MFD. At the 12-month follow-up visit, the patient reported no clinical symptoms, and no signs of tumor recurrence were detected.
Preoperative imaging of the patient with cervical fibrous dysplasia. a, b CT images demonstrated low density of the seventh cervical vertebra, with high-density hardening visible around the edges. c, d MRI scans of the cervical spine indicated an expansile lytic lesion with isointensity on T1-weighted imaging and hyperintensity on T2-weighted imaging
Discussion
FD is a non-hereditary disease; one possible mechanism is the multi-synthetase-activating mutation of the GNAS1 gene on chromosome 20q13.2-13.3 in somatic cells during embryonic development [5, 6]. Because the number of mutant cells often decreases with age, FD has age-related self-limiting characteristics [7] and a high incidence rate among teenagers in the general population. Lesions most often present in the long bones of the legs, arms, ribs, and pelvis, as well as in craniofacial bones. The spine is involved in 1.4–5.5% of FD lesions [8, 9]. FD progresses slowly, and malignancies rarely occur [10]. The natural courses of MFD, PFD, and MAS are quite different [2]. MFD generally stops developing once skeletal development ceases, and the lesion itself can be repaired. PFD and MAS can continue to develop after the bones mature, and the lesions can continue to progress, resulting in new pathological fractures or deformities [9, 11]. FD without local symptoms does not require surgical treatment [2], but the possibility of pathological fracture and deformity should be carefully assessed. Surgery is needed when patients suffer from persistent pain, spinal cord compression/injury, and vertebral collapse/instability.
Our literature review revealed 17 cases of surgically treated MFD involving cervical vertebrae, and the characteristics of these cases (including the one case presented in this study) are summarized in Table 1 [12,13,14,15,16,17,18,19,20,21,22,23,24]. None of these patients had pathological fractures or neurological deficits prior to surgery, and good results were achieved after surgical treatment. For lesions located on the posterior side of the vertebral body, laminectomy and fusion with or without internal fixation were performed [13, 14, 16, 18, 19, 21,22,23]. Three treatments were performed for vertebral body invasion: (1) Curettage of the lesion in the vertebral body followed by bone grafting was used in some cases [12, 15], although lesion recurrence and bone graft resorption were reported after this treatment in a long-term literature review [25, 26]. (2) Corpectomy with instrumented fusion was also used as a treatment and is a relatively thorough method for removing the lesion [16, 17, 23, 24]. If there is no spinal cord compression from the vertebral body, if the tumor is benign, and if the progression is slow, overly aggressive treatment should be avoided [21], especially because these tumors are rarely malignant. (3) VP [20] was used for the treatment of osteoporotic vertebral collapse, vertebral angiomas, and malignant tumors and has achieved good clinical results [27, 28]. VP has the advantages of less trauma, a shorter hospitalization duration, and faster recovery.
Our literature review revealed only 7 patients (including the 1 patient reported in this study) who underwent VP for the treatment of spinal fibrous dysplasia, as shown in Table 2 [20, 23, 29,30,31]; 2 patients had MFD, and 5 had PFD. Pathological fractures occurred in 5 patients, involving 13 vertebrae. The outcomes of these patients have been uniformly good, and no complications related to cement implantation have been reported. During the follow-up period, the patients experienced pain relief and showed no deformity or limited progression of spinal deformity.
The injection of bone cement increases the strength of the vertebral body and effectively improves the stability of the spinal system [32]. The chemical activity of the cement during the solidification process generates heat, destroying the nerve endings around the fracture, resulting in an analgesic effect [33]. Poly methyl methacrylate (PMMA) bone cement itself has a certain cytotoxic effect, which may lead to decreased cell metabolic activity, cell death or injury, the growth of new tumor cells, and decreased cell proliferation in vertebral bodies that have been solidified using cement [34, 35].
There are several challenges in the application of VP for MFD: (1) It is difficult to accurately diagnose the disease preoperatively because there is a lack of characteristic imaging manifestations, and the FD diagnosis depends on pathology results; in addition, CT-guided percutaneous biopsy for the evaluation of spinal lesions has a reported diagnostic accuracy of approximately 90% [36]. However, the positive FD diagnosis rate is low [23, 37]. Because it is impossible to make a clear diagnosis before surgery, other methods may be applied; thus, it is recommended that open biopsy be carried out when vertebral FD is suspected [23, 36]. (2) Expansive osteolysis and pathological fractures in FD may lead to the leakage of bone cement upon injection. The edge of vertebral sclerosis in FD can reduce cement leakage. VP has been suggested to reduce the cement leakage caused by vertebral fracture during kyphoplasty (KP) stretching [23]. (3) The efficacy of VP treatment is uncertain due to the lack of large-scale case studies and long-term follow-up results. With the increase in the application of VP for the treatment of vertebral tumors, the efficacy of VP in terms of pain relief and spinal stabilization and the underlying mechanisms will be further demonstrated.
Conclusion
VP has been widely used for the treatment of bone tumors, but its uses for the treatment of spinal FD is relatively rare. To the best of our knowledge, this report represents the second case in which VP is used for the treatment of spinal MFD. MFD is a benign tumor with slow progression. As VP can relieve pain while stabilizing the spine, the surgical treatment of MFD vertebral lesions by VP is a valuable option.
Availability of data and materials
The data are available from the corresponding author on reasonable request.
References
Lichtenstein L. Polystotic fibrous dysplasia. Arch Surg. 1938;36:877–98.
Dicaprio MR. Fibrous dysplasia. Pathophysiology, evaluation, and treatment. J Bone Joint Surg Am. 2005;87(8):1848–64.
Campanacci M. Bone and soft tissue tumors: clinical features, imaging, pathology and treatment. 2nd ed. New York: Springer; 1999. p. 247–64.
Fletcher CDM, Bridge JA, Hogendoorn P, Mertens F. World Health Organization classification of tumours of soft tissue and bone: fibrous dysplasia. 4th ed. Lyon: IARC Press; 2013. p. 352–3.
Weinstein LS, Shenker A, Gejman PV, et al. Activating mutations of the stimulating G protein in the McCune-Albright syndrome. N Engl J Med. 1991;325(24):1688–95.
Cohen MM Jr. Fibrous dysplasia is a neoplasm. Am J Med Genet. 2001;98(4):290–3.
Kuznetsov SA, Cherman N, Riminucci M, et al. Age-dependent demise of GNAS-mutated skeletal stem cells and “normalization” of fibrous dysplasia of bone. J Bone Miner Res. 2008;23(11):1731–40.
Saglik Y, Atalar H, Yildiz Y, et al. Management of fibrous dysplasia. A report on 36 cases. Acta Orthop Belg. 2007;73(1):96–101.
Ippolito E, Bray EW, Corsi A, et al. Natural history and treatment of fibrous dysplasia of bone: a multicenter clinicopathologic study promoted by the European Pediatric Orthopaedic Society. J Pediatr Orthop B. 2003;12(3):155–77.
Yalniz E, Er T, Ozyilmaz F. Fibrous dysplasia of the spine with sarcomatous transformation: a case report and review of the literature. Eur Spine J. 1995;4(6):372–4.
Al L, Magur E, Lee JS, et al. Fibrous dysplasia in the spine: prevalence of lesions and associations with scoliosis. J Bone Joint Surg Am. 2004;86(3):531–7.
Rosendahl-Jensen S. Fibrous dysplasia of the vertebral column. Acta Chir Scand. 1956;111(6):490–4.
Stirrat AN, Fyfe IS, Fisher CJ. Fibrous dysplasia of the axis: a case report. Spine. 1989;14(2):243–5.
Hu SS, Healey JH, Huvos AG. Fibrous dysplasia of the second cervical vertebra. A case report. J Bone Joint Surg Am. 1990;72(5):781–3.
Ohki I. Monostotic fibrous dysplasia in the spine. J West Pacif Orthop Assoc. 1990;27:107–10.
Villas C, Martínez-Peric R. Monostotic fibrous dysplasia of a cervical vertebra. Eur Spine J. 1992;1(2):137–9.
Marshman LA, David KM, O’Donovan DG, Chawda SJ. Fibrous dysplasia of the cervical spine presenting as a pathological fracture. Br J Neurosurg. 2004;18(5):527–33.
Arantes M, Vaz AR, Honavar M. Fibrous dysplasia of the first cervical vertebra. Spine. 2008;33(24):933–5.
Sambasivan M, Sanalkumar P, Mahesh S, Nair KR, Basheer A. Monostotic fibrous dysplasia of the C4 cervical spine. Neurol India. 2008;56(4):497–8.
Kotil K, Ozyuvaci E. Fibrous dysplasia in axis treated with vertebroplasty. J Craniovertehr Junction Spine. 2010;1(2):118–21.
Meredith DS, Healey JH. Twenty-year follow-up of monostotic fibrous dysplasia of the second cervical vertebra: a case report and review of the literature. J Bone Joint Surg Am. 2011;93(13):e74.
Bangash MH, Bokhary RY, Alomar SA, Baeesa SS. Fibrous dysplasia of the atlas. Neurosciences (Riyadh). 2011;16(1):76–7.
Wu FL, Jiang L, Liu C, et al. Fibrous dysplasia of the mobile spine. Spine. 2013;38(23):2016–22.
Yang Y, Ma L, et al. Monostotic fibrous dysplasia involved in cervical vertebrae. Int J Clin Exp Pathol. 2017;10(3):3577–81.
Li L, Hou X, Li Q, Zhang L. En bloc resection and bone graft: does it alter the natural history of monostotic expansile fibrous dysplasia in children? World J Surg Oncol. 2014;12(1):349–55.
Leet AI, Boyce AM, Ibrahim KA, et al. Bone-grafting in polyostotic fibrous dysplasia. J Bone Joint Surg. 2016;98(3):211–9.
Polly DW, Chou D, Sembrano JN, et al. An analysis of decision making and treatment in thoracolumbar metastases. Spine. 2009;34(22):118–27.
Zarghooni K, Siewe J, Kaulhausen T, et al. Complications of vertebroplasty and kyphoplasty in the treatment of vertebral fractures: results of a questionnaire study. Acta Orthop Belg. 2012;78(4):512–8.
Deen HG, Fox TP. Balloon kyphoplasty for vertebral compression fractures secondary to polyostotic fibrous dysplasia. Neurosurg Spine. 2005;3(3):234–7.
Dang D, Baig MN, Christoforidis G, et al. C2/C3 pathologic fractures from polyostotic fibrous dysplasia of the cervical spine treated with percutaneous vertebroplasty. Eur Spine J. 2007;16(suppl 3):250–4.
Chen G, Yang H, Gan M, et al. Polyostotic fibrous dysplasia of the thoracic spine: case report and review of the literature. Spine. 2011;36(22):E1485–8.
Bostrom MPG, Lane JM. Future directions: augmentation of osteoporotic vertebral bodies. Spine. 1997;22(suppl 24):38–42.
Evans AJ, Jensen ME, Kip KE, et al. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethyl-methacrylate vertebroplasty retrospective report of 245 cases. Radiology. 2003;226(2):366–72.
San Millan Ruiz D, Burkhardt K, Jean B, Muster M, Martin JB, Bouvier J, et al. Pathology findings with acrylic implants. Bone. 1999;25(suppl 2):85–90.
Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology. 1996;199(1):241–7.
Lis E, Bilsky MH, Pisinski L, et al. Percutaneous CT-guided biopsy of osseous lesion of the spine in patients with known or suspected malignancy. Am J Neuroradiol. 2004;25(9):1583–8.
Nuñez JH, González-Tartière P, Erimeiku F, et al. Surgical treatment of cervical spine fibrous dysplasia: case report and literature review. Int J Spine Surg. 2018;12(6):659–64.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
XX was a major contributor in writing the manuscript, drafted the manuscript, took part in the literature search, and treated the patient. JHF and CY participated in the diagnosis and treatment decisions. TJ took part in the literature search. XXL provided writing and radiology assistance. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained for the publication of this case report and the accompanying images from the relative of the patient. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xin, X., Feng, J., Yue, C. et al. Monostotic fibrous dysplasia at C7 treated with vertebroplasty: a case report and review of the literature. World J Surg Onc 17, 186 (2019). https://doi.org/10.1186/s12957-019-1717-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12957-019-1717-2