Abstract
Background
Obesity can be a significant challenge to health and quality of life (QoL). Bariatric surgery assists with weight loss and may help improve QoL. However, not all patients benefit from surgery. Personality traits may be related to QoL outcomes after bariatric surgery, but these associations are unclear.
Purpose
This research reviews the published literature on the associations between personality and QoL among post‐operative bariatric patients.
Method
Four databases (CINAHL Complete, Medline with Full Text, APA PsycINFO, and Scopus) were searched from inception until March 2022. Forward searching was conducted using Google Scholar, and backward reference citation searches were also performed.
Results
Five studies met inclusion criteria yielding data from N = 441 post-bariatric patients including both pre/post and cross-sectional designs. Higher agreeableness was related to lower overall health-related QoL (HRQol) and gastric HRQol and positively associated with psychological HRQol. Higher emotional stability was positively related to overall HRQol. Higher impulsivity was negatively associated with mental HRQol and was unrelated to physical HRQol. Effects for the remaining traits were either mainly mixed or null.
Conclusion
Personality traits may be associated with HRQol outcomes. However, it is difficult to reliably discern the role of personality traits for HRQol and QoL outcomes given the methodological issues and few published studies. More rigorous research is needed to address these issues and clarify possible associations.
Similar content being viewed by others
Introduction
Obesity has significant economic, social, and health implications to individuals and families worldwide [49]. Bariatric surgery is the only treatment intervention that has substantial, long‐term weight loss and medical benefits for those with severe obesity [33, 64]. The Bariatric Analysis and Reporting Outcome System (BAROS) outlines three main areas for assessment of ‘successful’ surgery: percentage of excess weight lost, changes in medical conditions, and quality of life (QoL) [16, 53]. QoL is widely accepted as the perception of one’s position in life, relative to culture and value systems, while considering goals, expectations, standards, and concerns [68].
As per The The WHOQOL Group [68], QoL is a complex concept is thought to reflect physical health, psychological state, level of independence, social relationships, personal beliefs, as well as the individual’s relationship with their lived environment. The WHOQOL Group [68] recommends capturing data on the following factors to comprehensively assess QoL: physical health, psychological state, level of independence, social relationships, relationship with the environment, and personal beliefs. A subcomponent of QoL is health-related quality of life (HRQol), which is how well a person functions in their life relative to their perceived wellbeing in physical, mental, and social domains of health [31]. Though distinct, these terms overlap and have been used interchangeably in the literature [36].
Surgical intervention may yield better improvements in QoL compared to other weight loss methods [22, 42], despite QoL often remaining lower than populations without obesity [1]. Of note, greater benefits have been reported for physical HRQol domains compared with mental HRQol [30, 35, 42] following bariatric surgery. Compared with non-surgical groups for example, improvements in mental QoL are not consistently observed from before to after bariatric surgery [66].
A systematic review of reviews [38] highlighted the relationship between weight loss and improved HRQol after bariatric surgery compared with controls. Outcomes varied greatly and some studies did not find any improvement. A range of possibilities for these inconsistencies has been hypothesised, including insufficient data due to dropout, lack of adequate follow-up, the emphasis of HRQol as a secondary outcome, and questionable quality of studies due to limited quality assessments [38]. It has also been hypothesised that additional factors may play a role in HRQol outcomes [38]. Indeed, Hindle and colleagues’ systematic review (2017) evaluated the role of early post-surgical psychosocial and weight-loss determinants of QoL (among other outcomes). This seminal work illustrates the complexity of QoL outcomes following surgery which results from multiple factors, including psychological determinants [32]. Individual differences, particularly personality traits, may be one aspect that contributes to the variability in QoL outcomes following bariatric surgery.
Five Factor Model (FFM) personality traits are defined as dimensions of relatively stable tendencies in thoughts, emotions, and behaviours across time [46]. Several models exist [3, 13, 24, 56] that purport the implications of individual personality differences. According to the FFM, individuals vary across five traits that contribute to behavioural tendencies over time [46]. Such tendencies may culminate in consequential health outcomes, including obesity across the lifespan [65], risk of future disease [67] and all cause-mortality [29, 52]. Growing evidence suggests that personality traits may also be critically important to consider within the context of QoL outcomes across a variety of populations [4, 19, 21, 26, 39, 57, 59, 73]. Yet to date, there is a lack of clarity on the relation between personality traits and QoL outcomes in bariatric populations.
Wimmelmann et al. [76] narrative review suggested that two personality traits (agreeableness and ‘neurotic predisposition’) were among the psychological variables associated with HRQol outcomes following bariatric surgery. However, studies identified in their review were limited and were not identified through systematic review procedures. There was also a lack of specificity on eligibility criteria, and unstandardised ‘composite’ traits were included as well as traits measured through established well-validated scales. Bordignon et al. [7] conducted a systematic review on personality traits and bariatric surgery outcomes, including QoL. Bordignon et al. [7] found that neuroticism had no association with QoL outcomes, in contrast to extensive findings among other health populations [4, 39, 59].
The association between personality traits and QoL outcomes following bariatric surgery remains unclear and warrants further investigation. We sought to examine studies of personality traits and QoL outcomes following bariatric surgery, regardless of quantitative study design. As such, this research systematically reviews and synthesises findings from the published literature to document the associations between personality traits and QoL outcomes among post‐operative bariatric patients.
Method
Protocol registration
This systematic review follows the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [54] and is registered within the PROSPERO database (registration number: CRD42021249681).
Eligibility criteria
The search template guiding this review was structured using the PEO template: Population (bariatric population), Exposure (personality traits), and Outcome (QoL).
Population
The population of interest was adult bariatric patients (≥ 18 years) who had undergone weight loss surgery (e.g., Roux-en-Y gastric bypass surgery, sleeve gastrectomy, gastric band, biliopancreatic diversion). Studies that reported data from ≥ 1 year post surgery were considered for inclusion. Studies which only reported data on participants prior to bariatric surgery (e.g., bariatric candidates) were excluded. Research on bariatric weight loss interventions or procedures, other than surgical interventions (e.g., pharmacological) were excluded, as well as surgical interventions where weight loss was not the primary function (e.g., aesthetic body contouring surgery). Surgical research on short term, removable bariatric devices (e.g., gastric balloon) was also excluded.
Exposure
All conceptualizations of personality traits [13, 17, 24, 27] were considered for inclusion in the current review, where studies reported the association between traits and QoL outcomes.
Outcome
Studies that reported QoL or HRQol, measured by multi-item or single item scales were included.
Studies
Peer reviewed publications including descriptive or analytical observational studies using either prospective (cohort studies) or retrospective (e.g., case control) data collection approaches were eligible for inclusion. Experimental studies were also eligible for inclusion (e.g., RCT). Articles that met exclusion criteria for the current review included other reviews, meta-analyses, letters to the editor, conference abstracts, or empirical commentaries. Qualitative studies were also excluded as well as research not published in English.
Information sources
The search was conducted from inception until March 2022, using the following electronic databases: CINAHL Complete, Medline with Full Text, APA PsycINFO through EBSCOhost; and Scopus. Forward (using Google Scholar) and backward reference citation searches were performed to identify additional relevant studies from the final articles. See Table 1 of supplementary material for Google Scholar search results. Search results were documented and saved within EndNote folders throughout the data collection period and email alerts were activated to capture new studies.
Search strategy
A search strategy was devised in line with Peer Review of Electronic Search Strategies (PRESS) [48], supported by an expert librarian and agreed upon by the review team. The search was executed in accordance with the PRISMA-S checklist [62] to complement the PRISMA Statement [54]. A combination of key words with MESH/subject headings/ thesaurus terms were utilised within each search engine. Search terms were developed across three concepts of ‘bariatric surgery’ ‘AND’ ‘trait’ ‘AND’ ‘quality of life’ and applied to each database. Surgical search terms were informed by prior works from Hindle et al. [32] and Sheets et al. [63]. See search strings in supplementary material, Table 2. To prevent missing unindexed articles, each search was performed in all text [TX]. Appropriate Boolean operators were applied in these instances. No cut-off date was applied to article publication and only peer-reviewed articles, published in English, within academic journals were included.
Selection process
Search results from each database were exported into EndNote. After duplicates were removed, 100% of the articles were independently blind screened (titles and abstracts) by two reviewers (SS and EK) using ‘Rayyan’ software, according to the eligibility criteria. Consensus was reached on these results and 100% of full-text articles were then independently blind-screened. Disagreement on one occasion was resolved by a third reviewer (PO). Cohen’s Kappa coefficient ranged from 0.67 to 0.92 during the screening stages, indicating high inter-rater reliability between reviewers [14].
Risk of bias
The internal validity of included studies was assessed using the US National Heart Lung and Blood Institute (NHLBI) quality appraisal tools, developed by the National Institutes of Health [51]. ‘Pre/post studies with no control group’ (PPSC) and ‘Observational cohort and cross-sectional studies’ (OCCSS) were deemed appropriate for the current research [44]. ‘Item 11’ within the PPSC was replaced with ‘item 14’ from the OCCSS, to account for confounding variables. The NHLBI tools included items to evaluate potential flaws promoting risk of bias (e.g., participant selection, attrition, confounders, study power, strength of causality etc.). These tools assist reviewers to focus on central concepts for critical appraisal of internal validity. Responses were “yes” (Y), “no” (N), “not applicable” (NA), “not reported” (NR) or “cannot determine” (CD). These tools were not designed to provide a list of factors comprising a numeric score [51]. Reviewers therefore considered the risk of bias presented by each respective flaw, relative to every study. This data was used to guide the overall quality rating as either “good,” “fair,” or “poor”. One author (SS) independently evaluated tool items for all studies and a second reviewer (EK) reviewed 60% of these.
Data extraction process and synthesis
Study characteristics tabulated to describe relevant study features are reported in Tables 1 and 2 (main effects were reported separately– see Table 3 in supplementary material). To avoid data extraction errors, spot checks were conducted by a second reviewer (EK) for 40% of articles. No errors were identified from these checks. Authors from three studies were contacted about missing data and reminder emails were sent for follow-up. Two authors responded with feedback. According to best practice guidelines for meta-analysis [20], it was not possible to employ quantitative analyses within this review. Small sample sizes, heterogeneity of measurement tools, variability of analyses, and differences in confounding variables indicated that narrative synthesis would best serve the data. Narrative ‘Synthesis Without Meta-analysis’ (SWiM) employing textual description of results was used. To provide transparency in narrative reporting, ‘SWiM’ guidelines were applied where possible in accordance with recommendations by Popay et al. [61] and Campbell et al. [9].
Results
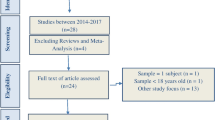
The database search yielded a total of 161 records after duplicates were removed. A further 155 records were removed from screening titles and abstracts. Full texts were retrieved for six articles which appeared to meet inclusion criteria. Two studies were excluded: one because the authors did not assess the relationship between personality and QoL [10]; the other study was not reported in English [2]. Forward and backward citation searches were conducted for the four articles that met inclusion criteria and resulted in one additional study [58]. A total of five articles met the inclusion criteria. Figure 1 illustrates the PRISMA flow diagram.
Summary PRISMA flow chart ([54]
Study characteristics
Studies included within this review were published between 2009 – 2021 and provide data on a total of N = 441 post-bariatric patients. Most were female; due to some non-reported data from loss to follow-up, the exact number of female participants is unclear. Bariatric samples ranged from n = 51 to n = 127. Studies were conducted across multiple countries including Portugal [58], the Netherlands [69] China [41], and Israel [11]. Research by Caltabiano [8] was conducted online and participant demographics were not reported. Attrition was not applicable to Caltabiano [8] due to the cross-sectional design. Lee et al. [41] reported no dropouts within their sample, whereas Canetti et al. [11] assessed and reported no significant differences between initial measures from completers and non-completers. Neither Pereira et al. [58] or Van Hout et al. [69] described statistical investigation of loss to follow-up.
Of the five studies included in this review, participants underwent one of four surgical techniques. Two studies [8, 11] reported methods using the adjustable gastric band method. Two studies [11, 69]) reported participants who underwent laparoscopic vertical band gastroplasty. Three studies [8, 41, 58] also reported data from participants who underwent the gastric sleeve technique. Finally, participants within two articles [8, 58] received the gastric bypass method. Study characteristics are summarised in Table 1.
Study designs
One study [8] was cross-sectional, and reported Pearson correlation analyses and hierarchical regression analyses to assess the data. Four studies [41, 58, 69] had a prospective, pre/post research designs to assess participants at two time-points (pre-surgery and post-surgery). Van Hout et al. [69] also reported hierarchical multiple regression analyses. Canetti et al. [11] used a pre/post design and compared group outcomes between individuals who underwent bariatric surgery and controls (others in a weight-loss diet programme). To assess outcomes, they used correlation analyses and subsequently applied confirmatory structural equation modelling for appropriate variables. Pereira et al. [58] assessed participants before and after surgery, applying correlational analyses, hierarchical regression analyses and moderation analyses, to test for effects. Lee et al. [41] reported t-tests to summarise their results.
Personality inventories
Pereira et al. [58] used the Portuguese version [70] of the Barratt Impulsivity Scale (BIS) [55] to assess levels of trait impulsivity. Higher scores on this scale indicate greater impulsiveness. Caltabiano [8] used the International Personality Item Pool (IPIP) [27], which measures the five FFM traits: extraversion, agreeableness, conscientiousness, emotional stability (neuroticism), and intellect. Canetti et al. [11] measured neuroticism using the NEO- Personality Inventory Revised (NEO-PI-N). Canetti and colleagues (2009) also assessed a “neurotic predisposition” (NP). This concept, however was not assessed in the present review because it is not a validated personality trait construct. Lee et al. [41] assessed personality traits using the Chinese Personality Assessment Inventory (CPAI) [12], which measures factors from the ‘Big Seven’ model of Chinese indigenous personality [71]: agreeableness, competence, contentedness, extraversion, industriousness, open-mindedness, and other-orientation. Lee et al. [41] only reported findings for agreeableness, competence, extraversion, and open-mindedness. Finally, the Amsterdam Biographical Questionnaire (ABQ) [75] was used by Van Hout et al. [69] to assess neurotic lability-somatic symptoms. The ABQ is a personality inventory with four scales: neuroticism (psycho-neurotic complaints), neurosomatism (functional somatic complaints), extraversion, and social conformity or lie.
HRQol scales
One study [8] measured HRQol using the Obesity Related Well-Being questionnaire (ORWELL-97). The ORWELL-97 provides an overall HRQol score and two subscale scores: symptom occurrence (occurrence and severity of obesity-related symptoms e.g. “Does your weight interfere with your social activities?”) and relevance of symptoms (resultant subjective impairment in life e.g. “Is it important for you to spend your free time with friends?”) [45]. Higher scores indicate lower HRQol [45]. Another study [41] employed the Gastrointestinal Quality of Life Inventory (GQLI) to assess HRQol outcomes, yielding an overall HRQol score and four subscales: gastrointestinal symptoms, emotions (psychological), physical functions, and social functions. Higher scores on the GQLI indicate better HRQol [23]. The 36-Item Short Form Survey (SF-36) was used in two studies [58, 69] to assess HRQol. The SF-36 yields an overall score and two subscale scores: mental HRQol and physical HRQol. Higher scores indicate a more favourable health state [72].
Risk of bias results
Reviewers reached 100% agreement regarding quality assessment for each study. Results from the risk of bias assessment rated three articles [8, 58, 69] as “good”, indicating low risk of bias. One article [11] was rated as “fair”, indicating medium risk of bias. Canetti et al. [11] indicated their findings to be preliminary based upon an underpowered sample. Despite management of covariates within the analyses, additional uncontrolled variables (weight loss) were suspected to have impacted results. Another article [41] was rated as “poor”, indicating high risk of bias. Major concerns were the lack of covariates, limited eligibility criteria, and statistical under-reporting that challenged the integrity of the results, according to reviewers. Studies included in this review did not control for differences between surgical techniques. As such, in the synthesis below, it is important to evaluate the results from this study with caution given its poor-quality rating. Overall, the internal validity based upon risk of bias for the included studies ranges from poor to good. Further risk of bias results are reported in Additional file 4; Table 4 I – V, Additional file 5; Tables 5 and 6.
Synthesis of quantitative evidence
Neuroticism
The association between neuroticism and HRQol outcomes varied across studies. Canetti et al. [11] tested for an association between neuroticism, measured by the NEO-PI-N scale, and HRQol, measured by the SF-36. The correlation was not significant. Van Hout et al. [69] did not report a significant association between neurotic lability-symptoms measured by the ABQ and physical HRQol according to the SF-36. Caltabiano [8] used a cross-sectional design to investigate the association between neuroticism measured by the IPIP [28] and HRQol according to the ORWEL-97, among female participants after bariatric surgery. Pearson correlations indicated a significant association between emotional stability (inverse of neuroticism) and overall HRQol, symptom occurrence, and symptom relevance. Subsequent hierarchical regression analysis revealed a medium-sized, positive association for emotional stability with overall HRQol. A medium-sized negative association between emotional stability and symptom occurrence and symptom relevance was also reported.
Impulsivity, extraversion, and openness
Pereira et al. [58] investigated the association between impulsivity as measured by the BIS [55] and post-surgical mental and physical HRQol, using the SF-36. Impulsivity was significantly associated with mental QoL [58]. No relationship between impulsiveness and physical HRQol was identified [58]. Results were mixed for extraversion. Lee et al. [41] found that extraversion was positively associated with overall HRQol and with social HRQol, whereas Caltabiano [8] found no significant associations between extraversion and HRQol. There was no association between openness and HRQol outcomes. Caltabiano [8] found that openness (measured as intellect imagination) was not significantly associated with HRQol (total, symptom relevance, or symptom occurrence). Open-mindedness, a concept within the Chinese ‘Big Seven’ model of personality which is somewhat similar to FFM openness [71] was also unrelated to all HRQol outcomes [41].
Agreeableness and conscientiousness
Caltabiano [8] found a medium-sized negative association between agreeableness and overall HRQol, with a medium positive association with symptom relevance and symptom occurrence. Lee et al. [41] identified similar associations with agreeableness as part of the Chinese ‘Big Seven’ personality model. Agreeableness was negatively associated with gastrointestinal symptoms (suggesting more gastrointestinal complaints) but was positively associated with psychological HRQol, suggesting higher psychological HRQol. Agreeableness was unrelated to physical HRQol and overall HRQol [41]. Conscientiousness was unrelated to HRQol [8]. Competence, a factor somewhat similar to conscientiousness within the Chinese ‘Big Seven’ Model of personality (differs from FFM competence) [37], was unrelated to HRQol outcomes [41]. Other traits within the Chinese Big Seven (industriousness, other-orientation, and contentedness) were not reported by Lee et al. [41].
Discussion
This review applied a rigorous systematic approach to appraise and synthesise evidence for an association between personality traits and QoL outcomes among post-surgical bariatric patients. This was the first systematic review to report evidence from all quantitative designs on studies that measured personality from a trait perspective. Overall, neuroticism appears to be associated with worse HRQol, whereas extraversion was found to be associated with higher HRQol, although null associations were also found for these two traits. The association was most mixed for agreeableness, with both positive and negative associations depending on the HRQol domain. Openness and conscientiousness were unrelated to HRQol. Few published studies, however examined the associations between personality and HRQol outcomes in this population.
Findings surrounding possible associations with neuroticism were mixed. The negative association between neuroticism and QoL outcomes is well established among other populations such as general health [57, 59], chronic disease [4], and breast cancer [39]. Two studies identified in this review found no significant association for neuroticism [11, 69]. Both studies had small sample sizes that may have limited power to detect significant associations. Conversely, Caltabiano [8], with a substantially larger sample size did identify significant associations. Therefore, these findings may have been due to sampling issues, rather than a unique nuance within the bariatric population. It is well established that those high in neuroticism (low emotional stability) are more predisposed to stress, self-consciousness, and impulsivity than those lower in neuroticism (high emotional stability) [17]. As such, individuals lower in emotional stability may perceive their post-surgical aliments as highly threatening and ruminate over these in the potential absence of robust coping mechanisms.
Impulsivity is typically viewed as a subcomponent of neuroticism within the FFM [17, 18, 34] and is the reactive predisposition to act without planning or considering the consequences [50]. Impulsivity may be associated with worse psychological HRQol outcomes [58]. Links between mental health challenges and neuroticism are well established [43], therefore findings from Pereira et al. [58] are consistent with research expectations. Though personality traits are heterogeneous among bariatric patients [25], evidence suggests that impulsivity is associated with weight status [6], and thus is likely to present in greater proportions among bariatric populations, highlighting potential challenges for surgical patients.
Agreeableness may have unique implications for HRQol due to socially adaptive features of this trait, but studies are sparse, and results are inconsistent. This prosocial trait is defined as being trustful and forgiving, straightforward, modest, compliant, tenderminded, and altruistic [18, 47]. Therefore, improvements to psychological HRQol among bariatric patients who score higher in agreeableness [41] are unsurprising and remain consistent with other psychological research [40]. Remarkably, higher agreeableness was also related to worse outcomes in physical HRQol domains. Similarly, to neuroticism, these findings need to be replicated to determine whether this discrepancy is due to chance or whether there is a substance difference across HRQol domains. No associations were reported for conscientiousness and openness.
Several challenges limit the literature on personality traits and QoL outcomes. First, most studies are observational and use linear models such as cross-sectional and pre/post designs. Although useful, more samples are needed that measure QoL at multiple points over time to reliably detect change. Second, there is a lack of control variables in many of the included studies that presents significant challenges to reliably interpreting the data. More careful consideration of covariates can help to better identify trait effects. Third, there were recruitment issues, and some studies were predominantly female. Despite the higher global incidence of females using bariatric surgery [74], the under representation of males may impact the generalisability of results to the wider bariatric population. Future research should increase equity of access for males in bariatric research. Fourth, the heterogeneity of traits assessed within this literature needs to be addressed in future research. Two studies only examined a single personality trait. Future research needs to examine the potential relevance of each of the broad personality traits from the Five Factor Model of Personality and their underlying facets to provide a more comprehensive assessment.
Strengths and limitations
Two major strengths of the present study are the comprehensive search of the literature across multiple databases and the rigorous methodology employed. Conversely, the main limitation of this systematic review is the few studies included, due to the paucity of published research. This limits the inferences and recommendations possible for research and practice. Owing to the infancy of such investigation, this review includes research impacted by bias which further impedes comparisons. Despite this inclusion, research with a poor-quality rating helped to clarify what future research in the area needs to address. Additionally, of the three relevant studies that reported dropouts [11, 58, 69], comparisons between included participants and those lost to follow-up were described in only one study [11]. Attrition is common and problematic in bariatric populations [15, 60]. Therefore, methods to comprehensively report patient data following surgery are necessary to promote meaningful understanding in the area. Furthermore, despite including validated HRQol scales, heterogeneity among these in the current review constrained interpretation and encouraged greater emphasis on health rather than QoL. For example, Lee et al. [41] employed the GIQLI. However, many of the GIQLI items measure gastrointestinal symptoms and physical HRQol rather than broader components of HRQol. This impacts comparability of results and requires caution when interpreting QoL outcomes across the bariatric population.
Additionally, Grading of Recommendations Assessment, Development and Evaluation (GRADE) analysis [5] was not conducted for studies within the current review as per SWiM guidelines [9], due to the low levels of evidence associated with the included observational study designs. Furthermore, papers were limited to those published in English which favours researchers’ bias towards their native language and constrains the breadth of evidence available. Finally, due to the unique yet overlapping dimensions which HRQol and QoL present, it is preferable to report these separately. However, this was not possible in the current review as research investigating personality traits and multifaceted QoL outcomes for post-surgical bariatric patients has not yet been conducted. This highlights a significant gap in the research. Instead, all included studies explored the associations between personality traits and HRQol, which can be understood as only one component of overall QoL. Research focused on HRQol alone, limits the universality required to inform overall adjustment to life after bariatric surgery. To address this, future research would benefit from exploring associations between personality traits and the multifactorial components of QoL.
Conclusion
Overall, findings from the current review offer emerging evidence that personality traits may impact HRQol outcomes following bariatric surgery. However, considering both the methodological issues and paucity of research in the area, it is difficult to reliably discern the role and mechanisms which personality traits play in HRQol and QoL outcomes. This finding is compounded by the lack of study replication over time. Research in the area remains concerned with health and HRQol outcomes rather than broader, multifaceted markers to adjustment in life after bariatric surgery. To this end, it is surprising that research investigating the role of personality traits and QoL outcomes following bariatric surgery does not exist. Therefore, more research is needed to address the issues identified in the current review, and to clarify the association between personality traits and QoL outcomes among people who undergo bariatric surgery.
Availability of data and materials
All review data are available within the manuscript and supplementary materials.
Abbreviations
- BMI:
-
Body mass index
- PRISMA:
-
Preferred Reporting Items for Systematic reviews and Meta-Analyses
- NHLBI:
-
(US) National Heart Lung and Blood Institute
- HRQol:
-
Health-Related Quality of Life
- SWiM:
-
Synthesis without meta-analysis
- QoL:
-
Quality of life
References
Andersen JR, Aasprang A, Karlsen TI, Natvig GK, Våge V, Kolotkin RL. Health-related quality of life after bariatric surgery: a systematic review of prospective long-term studies. Surg Obes Relat Dis. 2015;11(2):466–73 (https://www.soard.org/article/S1550-7289(14)00433-X/fulltext).
Ardelt-Gattinger E, Lechner H. Psychological aspects of bariatric surgery [Review]. Zentralbl Chir. 2002;127(12):1057–63. https://doi.org/10.1055/s-2002-36465.
Ashton MC, Perugini M, De Vries RE, Boies K, Lee K, Szarota P, Di Blas L, De Raad B. A Six-Factor Structure of Personality-Descriptive Adjectives: Solutions from Psycholexical Studies in Seven Languages [Article]. J Pers Soc Psychol. 2004;86(2):356–66. https://doi.org/10.1037/0022-3514.86.2.356.
Axelsson M, Lötvall J, Cliffordson C, Lundgren J, Brink E. Self-efficacy and adherence as mediating factors between personality traits and health-related quality of life. Qual Life Res. 2013;22(3):567–75 (https://link.springer.com/content/pdf/10.1007/s11136-012-0181-z.pdf).
Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, Vist GE, Falck-Ytter Y, Meerpohl J, Norris S. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6 (https://www.jclinepi.com/article/S0895-4356(10)00332-X/pdf).
Bénard M, Camilleri GM, Etilé F, Mejean C, Bellisle F, Reach G, Hercberg S, Péneau S. Association between impulsivity and weight status in a general population. Nutrients. 2017;9(3):217. https://doi.org/10.3390/nu9030217.
Bordignon S, Aparício MJG, Bertoletti J, Trentini CM. Personality characteristics and bariatric surgery outcomes: A systematic review [Review]. Trends Psychiatr Psychother. 2017;39(2):124–34. https://doi.org/10.1590/2237-6089-2016-0016.
Caltabiano ML. Personality, weight loss and obesity-related well-being post-bariatric surgery. Eating Weight Disord. 2021. https://doi.org/10.1007/s40519-020-01086-0.
Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, Hartmann-Boyce J, Ryan R, Shepperd S, Thomas J. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368. https://doi.org/10.1136/bmj.l6890.
Canetti L, Bachar E, Bonne O. Deterioration of mental health in bariatric surgery after 10 years despite successful weight loss. Eur J Clin Nutr. 2016;70(1):17–22 (https://www.nature.com/articles/ejcn2015112.pdf).
Canetti L, Berry EM, Elizur Y. Psychosocial predictors of weight loss and psychological adjustment following bariatric surgery and a weight-loss program: the mediating role of emotional eating. Int J Eat Disord. 2009;42(2):109–17. https://doi.org/10.1002/eat.20592.
Cheung FM, Cheung FM, Leung K, Fan RM, Song W-Z, Zhang J-X, Zhang J-P. Development of the Chinese Personality Assessment Inventory. J Cross Cult Psychol. 1996;27(2):181–99. https://doi.org/10.1177/0022022196272003.
Cloninger CR, Svrakic DM, Przybeck TR. A psychobiological model of temperament and character. Arch Gen Psychiatr. 1993;50(12):975–90 (https://jamanetwork.com/journals/jamapsychiatry/article-abstract/496431).
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Measur. 1960;20(1):37–46. https://doi.org/10.1177/001316446002000104.
Colombo O, Ferretti VV, Ferraris C, Trentani C, Vinai P, Villani S, Tagliabue A. Is drop-out from obesity treatment a predictable and preventable event? Nutr J. 2014;13:13–13. https://doi.org/10.1186/1475-2891-13-13.
Costa JM, Soares JB. Bariatric Analysis and Reporting Outcome System (BAROS): toward the uniform assessment of bariatric surgery outcomes. GE Port J Gastroenterol. 2015;22(3):85. https://doi.org/10.1016/j.jpge.2015.04.004.
Costa PT, McCrae RR. Revised NEO personality inventory (NEO-PI-R) and NEO five-factor (NEO-FFI) inventory professional manual. Odessa FL: Psychological Assessment Resources; 1992. https://doi.org/10.4135/9781849200479.n9.
Costa PT, McCrae RR. Domains and facets: Hierarchical personality assessment using the Revised NEO Personality Inventory. J Personality Assess. 1995;64(1):21–50. https://doi.org/10.1207/s15327752jpa6401_2.
de Mol M, Visser S, Aerts J, Lodder P, van Walree N, Belderbos H, den Oudsten B. The association of depressive symptoms, personality traits, and sociodemographic factors with health-related quality of life and quality of life in patients with advanced-stage lung cancer: an observational multi-center cohort study. BMC Cancer. 2020;20(1):1–14. https://doi.org/10.1186/s12885-020-06823-3.
Deeks JJ, Higgins JP, Altman DG, Group CSM. Analysing data and undertaking meta‐analyses. Cochrane handbook for systematic reviews of interventions. 2019. 241–284. https://doi.org/10.1002/9781119536604.ch10.
Demirci K, Demirci S, Taşkıran E, Kutluhan S. The effects of temperament and character traits on perceived social support and quality of life in patients with epilepsy. Epilepsy Behav. 2017;74:22–6. https://doi.org/10.1016/j.yebeh.2017.05.039.
Driscoll S, Gregory DM, Fardy JM, Twells LK. Long-term health-related quality of life in bariatric surgery patients: a systematic review and meta-analysis. Obesity. 2016;24(1):60–70 (https://onlinelibrary.wiley.com/doi/pdfdirect/10.1002/oby.21322?download=true).
Eypasch E, Williams JI, Wood-Dauphinee S, Ure B, Schmulling C, Neugebauer E, Troidl H. Gastrointestinal Quality of Life Index: development, validation and application of a new instrument. J British Surg. 1995;82(2):216–22 (https://academic.oup.com/bjs/article-abstract/82/2/216/6166220?redirectedFrom=fulltext).
Eysenck H, Eysenck SBG. Manual of the Eysenck Inventory. London: London University Press; 1964. https://doi.org/10.1007/978-0-387-79948-3_2025.
Generali I, De Panfilis C. Personality traits and weight loss surgery outcome. Curr Obes Rep. 2018;7(3):227–34 (https://link.springer.com/content/pdf/10.1007/s13679-018-0315-x.pdf).
Ghiggia A, Pierotti V, Tesio V, Bovero A. Personality matters: relationship between personality characteristics, spirituality, demoralization, and perceived quality of life in a sample of end-of-life cancer patients. Supportive Care in Cancer. 2021;29(12):7775–83 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8550274/pdf/520_2021_Article_6363.pdf).
Goldberg LR. The development of markers for the Big-Five factor structure. Psychol Assess. 1992;4(1):26. https://doi.org/10.1037/1040-3590.4.1.26.
Goldberg LR, Johnson JA, Eber HW, Hogan R, Ashton MC, Cloninger CR, Gough HG. The international personality item pool and the future of public-domain personality measures. J Res Pers. 2006;40(1):84-96. https://doi.org/10.1016/j.jrp.2005.08.007.
Graham EK, Rutsohn JP, Turiano NA, Bendayan R, Batterham PJ, Gerstorf D, Katz MJ, Reynolds CA, Sharp ES, Yoneda TB, Bastarache ED, Elleman LG, Zelinski EM, Johansson B, Kuh D, Barnes LL, Bennett DA, Deeg DJH, Lipton RB, Pedersen NL, Piccinin AM, Spiro A, Muniz-Terrera G, Willis SL, Warner Schaie K, Roan C, Herd P, Hofer SM, Mroczek DK. Personality predicts mortality risk: An integrative data analysis of 15 international longitudinal studies. J Res Pers. 2017;70:174–86. https://doi.org/10.1016/j.jrp.2017.07.005.
Hachem A, Brennan L. Quality of life outcomes of bariatric surgery: a systematic review. Obes Surg. 2016;26(2):395–409. https://doi.org/10.1007/s11695-015-1940-z.
Hays RD, Reeve BB Measurement and modeling of health-related quality of life. In J. In Killewo, Heggenhougen, K, Quah SR (Eds.). (2010) (Ed.), Epidemiology and Demography in Public Health (pp. 195–205). San Diego: Academic Press; 2008.
Hindle A, Piedad Garcia X, Brennan L. Early post-operative psychosocial and weight predictors of later outcome in bariatric surgery: a systematic literature review. Obes Rev. 2017;18(3):317–34. https://doi.org/10.1111/obr.12496.
Jakobsen GS, Småstuen MC, Sandbu R, Nordstrand N, Hofsø D, Lindberg M, Hertel JK, Hjelmesæth J. Association of bariatric surgery vs medical obesity treatment with long-term medical complications and obesity-related comorbidities. JAMA. 2018;319(3):291–301 (https://jamanetwork.com/journals/jama/articlepdf/2669729/jama_jakobsen_2018_oi_170160.pdf).
John O, Donahue E, Kentle R. The big five inventory-Versions 4a and 54. Berkeley, CA: University of California. Berkeley, Institute of Personality and Social Research; 1991.
Jumbe S, Bartlett C, Jumbe SL, Meyrick J. The effectiveness of bariatric surgery on long term psychosocial quality of life–A systematic review. Obes Res Clin Pract. 2016;10(3):225–42. https://doi.org/10.1016/j.orcp.2015.11.009.
Karimi M, Brazier J. Health, Health-Related Quality of Life, and Quality of Life: What is the Difference? Pharmacoeconomics. 2016;34(7):645–9. https://doi.org/10.1007/s40273-016-0389-9.
Kim U, Yang G, Hwang KK. Indigenous and cultural psychology: Understanding people in context. Springer. 2006. https://link.springer.com/content/pdf/10.1007%2F0-387-28662-4.pdf.
Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clinical obesity. 2017;7(5):273–89. https://doi.org/10.1111/cob.12203.
Lai H-L, Chen C-I, Lu C-Y, Yao Y-C, Huang C-Y. Relationships among personality, coping, and concurrent health-related quality of life in women with breast cancer. Breast Cancer. 2019;26(5):544–51. https://doi.org/10.1007/s12282-019-00954-7.
Lamers SM, Westerhof GJ, Kovács V, Bohlmeijer ET. Differential relationships in the association of the Big Five personality traits with positive mental health and psychopathology. J Res Pers. 2012;46(5):517–24. https://doi.org/10.1016/j.jrp.2012.05.012.
Lee YC, Lee CK, Liew PL, Lin YC, Lee WJ. Evaluation of quality of life and impact of personality in Chinese obese patients following laparoscopic sleeve gastrectomy [Article]. Hepatogastroenterology. 2011;58(109):1248–51. https://doi.org/10.5754/hge10619.
Lindekilde N, Gladstone B, Lübeck M, Nielsen J, Clausen L, Vach W, Jones A. The impact of bariatric surgery on quality of life: a systematic review and meta-analysis. Obes Rev. 2015;16(8):639–51 (https://onlinelibrary.wiley.com/doi/10.1111/obr.12294).
Lyon K, Elliott R, Ware K, Juhasz G, Brown L. Associations between Facets and Aspects of Big Five Personality and Affective Disorders: A Systematic Review and Best Evidence Synthesis. J Affect Disord. 2021;288:175–88. https://doi.org/10.1016/j.jad.2021.03.061.
Ma L-L, Wang Y-Y, Yang Z-H, Huang D, Weng H, Zeng X-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil Med Res. 2020;7(1):7–7. https://doi.org/10.1186/s40779-020-00238-8.
Mannucci E, Ricca V, Barciulli E, Di Bernardo M, Travaglini R, Cabras PL, Rotella CM. Quality of life and overweight: the obesity related well-being (Orwell 97) questionnaire. Addict Behav. 1999;24(3):345–57. https://doi.org/10.1016/S0306-4603(98)00055-0.
McCrae R, Costa P. Personality in adulthood. New York: Guilford Press; 1990.
McCrae RR, Sutin AR. A Five-Factor Theory Perspective on Causal Analysis. Eur J Pers. 2018;32(3):151–66. https://doi.org/10.1002/per.2134.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–6 (https://www.jclinepi.com/article/S0895-4356(16)00058-5/pdf).
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, Kushner RF, Lindquist R, Pessah-Pollack R, Seger J. Surg Obes Relat Dis. 2020;16(2):175–247 (https://www.soard.org/article/S1550-7289(19)31079-2/fulltext).
Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatr. 2001;158(11):1783–93. https://doi.org/10.1176/appi.ajp.158.11.1783.
National Institutes of Health. (2014, 2021). Study Quality Assessment Tools. National Heart, Blood, and Lung Institute. Retrieved 01 June from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
O’Súilleabháin PS, Turiano NA, Gerstorf D, Luchetti M, Gallagher S, Sesker AA, Terracciano A, Sutin AR. Personality pathways to mortality: Interleukin-6 links conscientiousness to mortality risk. Brain, Behav Immun. 2021;93:238–44 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7979517/pdf/nihms-1673875.pdf).
Oria HE, Moorehead MK. Updated bariatric analysis and reporting outcome system (BAROS). Surg Obes Relat Dis. 2009;5(1):60–6. https://doi.org/10.1016/j.soard.2008.10.004.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Online). 2021;372. https://doi.org/10.1136/bmj.n71.
Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51(6):768–74. https://doi.org/10.1002/1097-4679(199511)51:6. (<768::AID-JCLP2270510607>3.0.CO;2-1).
Paulhus DL, Williams KM. The Dark Triad of personality: Narcissism, Machiavellianism, and psychopathy. J Res Pers. 2002;36(6):556–63. https://doi.org/10.1016/S0092-6566(02)00505-6.
Pereira-Morales AJ, Adan A, Lopez-Leon S, Forero DA. Personality traits and health-related quality of life: the mediator role of coping strategies and psychological distress. Ann Gen Psychiatr. 2018;17(1):1–9. https://doi.org/10.1186/s12991-018-0196-0.
Pereira MG, Faria S, Lopes H. Quality of Life One Year After Bariatric Surgery: the Moderator Role of Spirituality [Article]. Obes Surg. 2019;29(4):1207–15. https://doi.org/10.1007/s11695-018-03669-4.
Pocnet C, Dupuis M, Congard A, Jopp D. Personality and its links to quality of life: Mediating effects of emotion regulation and self-efficacy beliefs. Motiv Emot. 2017;41(2):196–208. https://doi.org/10.1007/s11031-017-9603-0.
Ponzo V, Scumaci E, Goitre I, Beccuti G, Benso A, Belcastro S, Crespi C, De Michieli F, Pellegrini M, Scuntero P, Marzola E, Abbate-Daga G, Ghigo E, Broglio F, Bo S. Predictors of attrition from a weight loss program. A study of adult patients with obesity in a community setting. Eat Weight Disord. 2021;26(6):1729–36. https://doi.org/10.1007/s40519-020-00990-9.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews. Product ESRC Methods Programme Version. 2006;1(1):92 (https://www.lancaster.ac.uk/media/lancaster-university/content-assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf).
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, Koffel JB. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst Rev. 2021;10(1):1–19. https://doi.org/10.1186/s13643-020-01542-z.
Sheets CS, Peat CM, Berg KC, White EK, Bocchieri-Ricciardi L, Chen EY, Mitchell JE. Post-operative Psychosocial Predictors of Outcome in Bariatric Surgery. Obes Surg. 2014;25(2):330–45. https://doi.org/10.1007/s11695-014-1490-9.
Spirou D, Raman J, Smith E. Psychological outcomes following surgical and endoscopic bariatric procedures: A systematic review. Obesity Reviews. 2020;21(6):e12998 (https://onlinelibrary.wiley.com/doi/10.1111/obr.12998).
Sutin AR, Ferrucci L, Zonderman AB, Terracciano A. Personality and obesity across the adult life span. J Pers Soc Psychol. 2011;101(3):579 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3462003/pdf/nihms-314971.pdf).
Szmulewicz A, Wanis KN, Gripper A, Angriman F, Hawel J, Elnahas A, Alkhamesi NA, Schlachta CM. Mental health quality of life after bariatric surgery: A systematic review and meta-analysis of randomized clinical trials. Clin Obes. 2019;9(1):e12290 (https://onlinelibrary.wiley.com/doi/10.1111/cob.12290).
Terracciano A, Aschwanden D, Passamonti L, Toschi N, Stephan Y, Luchetti M, Lee JH, Sesker A, O’Súilleabháin PS, Sutin AR. Is neuroticism differentially associated with risk of Alzheimer’s disease, vascular dementia, and frontotemporal dementia? J Psychiatr Res. 2021;138:34–40. https://doi.org/10.1016/j.jpsychires.2021.03.039.
The WHOQOL Group. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;41(10):1403–9. https://doi.org/10.1016/0277-9536(95)00112-K.
Van Hout GCM, Hagendoren CAJM, Verschure SKM, Van Heck GL. Psychosocial predictors of success after vertical banded gastroplasty [Article]. Obes Surg. 2009;19(6):701–7. https://doi.org/10.1007/s11695-008-9446-6.
von Diemen L, Szobot CM, Kessler F, Pechansky F. Adaptation and construct validation of the Barraft Impulsiveness Scale (BIS 11) to Brazilian Portuguese for use in adolescents. Rev Bras Psiquiatr. 2007;29(2):153–6. https://doi.org/10.1590/S1516-44462006005000020.
Wang D, Fang L, Zuo Y. A psycho-lexical study on Chinese personality from natural language. Acta Psychologica Sinica. 1995;27(04):400 (http://journal.psych.ac.cn/acps/EN/Y1995/V27/I04/400).
Ware J, John E, Sherbourne C, Donald. The MOS 36-item short-form health survey (SF-36): I Conceptual framework and item selection. Med Care. 1992;473–483. https://www.jstor.org/stable/3765916.
Weber K, Canuto A, Giannakopoulos P, Mouchian A, Meiler-Mititelu C, Meiler A, Herrmann FR, Delaloye C, Ghisletta P, Lecerf T. Personality, psychosocial and health-related predictors of quality of life in old age. Aging Mental Health. 2015;19(2):151–8. https://doi.org/10.1080/13607863.2014.920295.
Welbourn R, Hollyman M, Kinsman R, Dixon J, Liem R, Ottosson J, Ramos A, Våge V, Al-Sabah S, Brown W. Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth IFSO global registry report 2018. Obes Surg. 2019;29(3):782–95. https://doi.org/10.1007/s11695-018-3593-1.
Wilde GJS. Neurotische Labiliteit Gemeten Volgens de Vragenlijstmethode. De Amsterdamse Biografische Vragenlijst [Neurotic Liability Measured with the Questionnaire Method. The Amsterdam Biographical Questionnaire]. 1970.
Wimmelmann CL, Dela F, Mortensen EL. Psychological predictors of mental health and health-related quality of life after bariatric surgery: A review of the recent research [Review]. Obes Res Clin Pract. 2014;8(4):e314–24. https://doi.org/10.1016/j.orcp.2013.11.002.
Acknowledgements
None declared.
Funding
None declared.
Author information
Authors and Affiliations
Contributions
SS and PO conceptualized this study. SS performed the literature search. Both SS and EK conducted the study selection, data extraction, and quality assessment. PO provided the final determination to achieve consensus when disagreement between authors was unresolved, relative to article screening. SS, PO, AS, and DF drafted the manuscript. All authors participated in the interpretation of data and critically revised the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 1.
Supplementary material A. Results from ‘forward’, and ‘backward’ citation search.
Additional file 2: Table 2.
Search strings.
Additional file 3: Table 3.
Summary of results and main effects.
Additional file 4: Table 4.
I – V. Risk of bias results data.
Additional file 5: Table 5.
Quality assessment for observational cohort and cross-sectional studies. Table 6. Quality assessment for pre/post studies with no control.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Summerville, S., Kirwan, E., Sutin, A.R. et al. Personality trait associations with quality-of-life outcomes following bariatric surgery: a systematic review. Health Qual Life Outcomes 21, 32 (2023). https://doi.org/10.1186/s12955-023-02114-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-023-02114-0