Abstract
Background
Sub-health which is the state between health and disease is a major global public health challenge. As a reversible stage, sub-health can work as a effective tool for the early detection or prevention of chronic disease. The EQ-5D-5L (5L) is a widely used, generic preference-based instrument while its validity in measuring sub-health is not clear. The aim of the study was thus to assess its measurement properties in individuals with sub-health in China.
Methods
The data used were from a nationwide cross-sectional survey conducted among primary health care workers who were selected on the basis of convenience and voluntariness. The questionnaire was composited of 5L, Sub-Health Measurement Scale V1.0 (SHMS V1.0), social-demographic characteristics and a question assessing the presence of disease. Missing values and ceiling effects of 5L were calculated. The convergent validity of 5L utility and VAS scores was tested by assessing their correlations with SHMS V1.0 using Spearman’s correlation coefficient. The known-groups validity of 5L utility and VAS scores was assessed by comparing their values between subgroups defined by SHMS V1.0 scores using the Kruskal–Wallis test. We also did an analysis in subgroups according to different regions of China.
Results
A total of 2063 respondents were included in the analysis. No missing data were observed for the 5L dimensions and only one missing value was for the VAS score. 5L showed strong overall ceiling effects (71.1%). The ceiling effects were slightly weaker on the “pain/discomfort” (82.3%) and “anxiety/depression” (79.5%) dimensions compared with the other three dimensions (nearly 100%). The 5L weakly correlated with SHMS V1.0: the correlation coefficients were mainly between 0.2 and 0.3 for the two scores. 5L was yet not sensitive in distinguishing subgroups of respondents with different levels of sub-health, especially the subgroups with adjacent health status (p > 0.05). The results of subgroup analysis were generally consistent with those of the full sample.
Conclusions
It appears that the measurement properties of EQ-5D-5L in individuals with sub-health are not satisfactory in China. We thus should be cautious to use it in the population.
Similar content being viewed by others
Background
In parallel with the change of living environment and the increasing pace of life, more and more people are in the state of sub-health [1], which refers to the state between health and disease that does not meet the criterion for health nor the clinical diagnostic criteria for diseases according to modern medicine [2]. Chinese scholar Wang Yuxue first formally introduced its concept in the 1980s [3]. It is derived from traditional Chinese medicine (TCM) characterized by a decline in vitality, physiological function and the capacity for adaptation over a certain period of time [2, 4]. In many countries, much attention has been paid on perceived poor health “medically unexplained symptoms (MUS)” [5]. They are two concepts that have some similarities but are not exactly identical. MUS contains a series of clinical defined conditions commonly with diagnostic criteria mainly focusing on physiological symptomatic outcomes like pain and fatigue [6, 7]. However, sub-health is not a strict clinical concept and should be considered as a dynamic process. It includes physical, mental and social adaptation performance of the subject, which highlights both psychological and social factors, so it carries a wider connotation than MUS [3, 8, 9].
Sub-health now is a major global public health challenge [6, 7, 10, 11]. Previous investigations conducted in China within different groups of people have shown that 60%-70% of surveyed individuals are sub-healthy [12, 13]. Sub-health is a low-quality health state and people in this state are typified by impaired health related quality of life (HRQoL) [6, 7, 10]. They may frequently suffer from physical, mental and social interactional problems, like fatigue, pain, sleep disorder, depression, agitation, fear, inability to assume appropriate social roles and so on. As a reversible stage, sub-health has a bidirectional transformation to health or disease so it can work as a effective tool for the early detection or prevention of chronic disease [4, 14,15,16,17]. Hence, it is necessary to accurately measure sub-health status, which can help to promote early interventions in the population and thus to avoid the generation of disease and further to reduce the burden of disease and healthcare expenditure.
Sub-health is rich in connotation and should be comprehensively assessed from various aspects. Currently the assessment and measurement of sub-health is based on individual symptoms and social background, physiological and biochemical test results, relevant TCM theories, specific questionnaires and scales, or a combination of those methods [18]. However, there is no standardized criterion. Instrument-based measurement can reflect the subjective and multidimensional manifestations of sub-health in a relatively objective manner, which is a widely used sub-health measurement method. Its advantages include being quantitative and easy-to-use. The instruments used in current sub-health researches include Sub-Health Measurement Scale V1.0 (SHMS V1.0) [19], Suboptimal Health Status Questionnaire-25 (SHSQ-25) [20, 21], Sub-Health Self-Rating Scale (SHSRS) [22], Self-Rated Health Measurement Scale Version1.0 (SRHMS V1.0) [23, 24], etc. Among them, the SHMS V1.0 developed by Xu et al. is a reliable and valid tool widely used for measuring sub-health (Cronbach's alpha coefficient of 0.917 and KMO statistic of 0.927) [1, 12, 13, 19, 25,26,27,28,29]. Although those scales can reflect the health status of individuals, the variety of them hinders the result comparisons between studies using different scales due to not exactly consistent development ideas behind those scales. Moreover, the instruments cannot provide health utilities, thus cannot be used in economic evaluations. The EQ-5D-5L (5L) is a widely used, generic preference-based instrument with good reliability and validity in many specific groups of people [30,31,32]. If it is a valid sub-health measurement instrument, health utilities in sub-health and result comparisons among different studies could be available, which lay a foundation for further researches. However, to the best of our knowledge, there is a lack of study on the performance of 5L in sub-healthy population at present.
Hence, the study aimed to assess whether the 5L can effectively reflect the impact of sub-health on HRQoL using the SHMS V1.0 as an external standard. Given the fact that primary health care workers in China are at high risk of being sub-health due to their long-term heavy workloads [33], the study was conducted based on data from primary health care workers in China.
Methods
Sampling and data collection
The study used data from a cross-sectional survey conducted in primary health care institutions across multiple cities in mainland China from July to August 2021. The definition of primary health care institutions in this survey refers to the relevant provisions of Law of the people’s Republic of China on the Promotion of Basic Medical and Health Care. They mainly include township (street) health centers, community health service centers (stations), village health offices, infirmaries and clinics. Respondents meeting the following criteria were included in the analysis: (1) Full-time health care workers of the institutions; (2) ≧1 year of working experience; (3) Not clinically diagnosed with any disease.
The study sample was selected on the basis of convenience and voluntariness. First, thirty one provinces, autonomous regions and municipalities in mainland China were divided into four region groups (ten in the Eastern Region, six in the Central Region, twelve in the Western Region, and three in the Northeast Region) according to their economic levels and future development strategies. Then investigators from all provinces, autonomous regions and municipalities included in each region were recruited respectively. After receiving uniform training, investigators visited at least two local primary care institutions by convenience to conduct face-to-face questionnaire survey. At the study site, according to the principle of voluntariness, investigators invited health care workers to participate in the survey, providing them with the purposes, contents, and requirements of the survey. Then, investigators confirmed with consenting individuals the time and undisturbed places for the survey. After being reminded of the bullet points and prompts in questions, the respondents answered questionnaires independently on removable electronic devices (mobile phone, tablet, etc.) provided by the investigators, and the data were uploaded to the electronic database system in real time. We assigned data auditors to examine the collected data in time. If many missing items or logical errors were found, the questionnaire will be discarded and fed back to the corresponding investigator so as to timely conduct the investigation again. The questionnaire relevant to this study was composited of social-demographic characteristics (including age, gender, height, weight, education level, years of experience, professional title, annual income, type of household, marital status, region and location of healthcare institution), 5L, SHMS V1.0 and a question assessing the presence of disease. The order of the SHMS V1.0 and 5Lwas randomly assigned to avoid order effect. The two scales’ items were respectively set as 5L and SHMS V1.0 question groups. Then we set up two “element packages” containing the 5L and SHMS V1.0 question sets in reverse order. In each questionnaire, only one “element package” was randomly displayed to realize the randomization of the response order of the two scales.
The protocol of this study was approved by the Ethics Committee of China Pharmaceutical University (No. CPU2019015). Informed consent was obtained from all individual participants included in the study.
Instruments
SHMS V1.0
SHMS V1.0 has been widely used in college students, residents in different regions, and has showed good reliability and validity in measuring sub-health [25,26,27]. Its Cronbach's alpha coefficient was 0.939 for our sample. SHMS V1.0 is composited of three subscales, ten dimensions and 39 items in total, each in a Likert 5-point format, with four general items of sub-health (GS). The three subscales are physical sub-health scale (PS), mental sub-health scale (MS) and social sub-health scale (SS). PS contains four dimensions of physical symptom, organic function, physical mobility function, and vitality. MS includes three dimensions of positive emotion, psychosocial symptom and cognitive function. SS contains three dimensions of social adaptability, social resource and social support. For SHMS V1.0, the conversion score (sc) is adopted to do analysis. It is defined as:
where sr is the raw score calculated by summing the corresponding item scores except ones of four overall assessment items. sr(min) is the theoretical minimum score of sr and sr(max) is the theoretical maximum score of sr. Higher conversion scores mean better health status.
EQ-5D-5L
5L is a generic preference-based instrument for measuring health and consists of two parts: a descriptive system and a visual analog scale (VAS). The system comprises five dimensions of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, with each consisting of only one item. Each item has five levels of response describing no, slight, moderate, severe, and extreme problems (“1” being the no problems and “5” being the extreme problems). The 5L can describe a total of 3125 potential health states of the respondent on the day of survey, with “11,111” being the full health and “55,555” the worst health state. EQ-VAS is a vertical line with a scale ranging from 0 to 100, with 100 on the top representing the “best imaginable health state” and 0 at the bottom representing the “worst imaginable health state”. In the study, the responses to the five dimensions of 5L were converted into utility scores using the Chinese 5L value set [34].
Data analysis
Descriptive statistics including mean, standard deviation (SD) and percentage were used to present characteristics of the study sample. The mean values (SD) of 5L utility and EQ-VAS scores were respectively calculated and the missing data of 5L were examined. The distributions of responses to different dimensions and the proportion of respondents reporting the full health of 5L were also reported.
We assessed the convergent validity of 5L by analyzing its relationship with SHMS V1.0, using Spearman’s correlation coefficient. We hypothesized that the respective correlation of 5L utility and EQ-VAS scores with SHMS V1.0 total and subscale scores would be moderate or strong, as well as the similar dimensions from the two instruments including Pain/discomfort and Organic function; Mobility and Physical mobility function; Pain/discomfort and Physical mobility function; Usual activities and Vitality; Anxiety/depression and Psychosocial symptom. The values of correlation coefficients less than 0.3 were considered to be weak, values between 0.3 and 0.49 were regarded as moderate, and values of 0.5 and above as strong [35].
The known-groups validity of 5L was assessed by identifying whether subgroups known to be different in health status could be distinguished by 5L’s utility and VAS scores [36]. Five known-groups (i.e., health, mild sub-health, moderate sub-health, severe sub-health and illness) were defined according to SHMS V1.0 total, PS, MS or SS score respectively. The demarcation score boundaries were determined according to the demarcation norms of the SHMS V1.0 in Chinese civil servants (Additional file 1) [37]. Since both the distributions of utility and VAS scores were skewed, the non-parametric Kruskal–Wallis H rank test with pairwise comparisons was performed to assess their known-groups validity. We hypothesized that the higher the SHMS V1.0 total, PS, MS or SS scores, the higher the 5L utility and EQ-VAS scores.
Since the responses to preference-based HRQoL scales may vary among different regions [38], we also analyzed the convergent validity and known-groups validity in subgroups determined by different regions of China (i.e., the Eastern, Central, Western and Northeast Regions).
Microsoft® Excel 2016 and IBM SPSS 26 were used for data analysis. All effects were considered statistically significant at p < 0.05.
Results
Descriptive statistics
A total of 2167 questionnaires from 913 primary health care institutions nationwide were returned and 2063 respondents (34.7% in the Eastern Region, 25.8% in the Central Region, 31.8% in the Western Region, and 7.7% in the Northeast Region) were included in the final analysis, with the response rate being 95.2%.
Table 1 displays characteristics of the study respondents. Six hundred and thirty-four (30.7%) were male and 1429 (69.3%) were female. Their mean age (SD) was 37.6 (9.6) years.
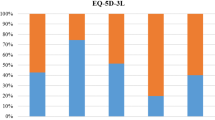
There were no missing responses to the 5L dimensions and only one missing value for the VAS score. The mean values (SD) of 5L utility and VAS scores were 0.974 (0.057) and 86.4 (14.9), respectively. A total of 1466 (71.1%) respondents reported full health (“11,111”). The distributions of the responses to 5L are shown in Table 2. Nearly all respondents reported no problems on the mobility, self-care and usual activities dimensions. Around 80% reported no problems on the dimensions "pain/discomfort" and "anxiety/depression", and nearly 20% reported slight problems (Level 2). Almost no respondents reported serious or extreme problems on all of the dimensions (Level 4 and Level 5).
Convergent validity
The 5L utility score weakly correlated with SHMS V1.0 scores. Comparing the correlations of 5L utility score with SHMS V1.0 total and the three subscales scores, the 5L utility score most strongly correlated with the SHMS V1.0 total score and weakliest related to the SS score. The correlations between the EQ-VAS and SHMS V1.0 scores were similar but they were generally better than those between the 5L utility score and SHMS V1.0 scores (Table 3). The correlation coefficients for the five pairs of potentially relevant dimensions between SHMS V1.0 and 5L were all lower than 0.3 (weak correlation). Correlation coefficient of the SHMS V1.0 vitality dimension and the 5L usual activities dimension was only -0.056 (Table 4).
The results of the subgroup analysis were generally consistent: correlation coefficients were generally lower than 0.3 (Additional file 2). The correlations of 5L utility score and EQ-VAS with SHMS V1.0 were best respectively in the Central Region and Northeast Region. The 5L weakliest correlated with SHMS V1.0 SS score for all subgroups. The correlations between EQ-VAS and SHMS V1.0 in all regions were slightly better compared with those between the 5L utility score and SHMS V1.0.
Known-groups validity
The mean values (SD) of 5L utility score and EQ-VAS score for each group are shown in Table 5. The utility and VAS scores of 5L were both significantly different in at least two of the five groups divided by overall, physical, mental or social health status (p < 0.001, Table 5). The Kruskal–Wallis H value of the 5L utility score in the physical health was 113.1 which was higher than those in the mental health (87.5) and social health (43.0). The EQ-VAS also had the lowest Kruskal–Wallis H value in social health (101.2) compared with those in physical and mental health (130.2 and 155.9). The 5L utility score did not significantly distinguish the “illness” and “severe sub-health” groups nor the “health” and “mild sub-health” groups in overall, physical, mental and social health (p > 0.05, Additional file 3). EQ-VAS was also insensitive in distinguishing between adjacent health status groups. Subgroup analysis had generally consistent results (Additional file 2).
Discussion
This is the first study to assess the measurement performance of 5L in measuring the effect of sub-health on HRQoL, filling a gap in the field of the applicability of 5L in sub-healthy population and laying a foundation for further research in sub-health measurement. Based on the results of a representative sample of primary health care workers in China, the measurement properties of 5L in sub-health may not be satisfactory. Many studies have reported that the 5L shows good measurement properties in many types of cancer [30], hemophilia [31], osteoarthritis [32], etc. The health status of people with clinically diagnosed disease usually declines significantly, while the majority (86%) of the respondents in sub-health of this study were mild to moderate, the difference between whose health status and full health was not obvious. The possible reason could be that the 5L, although a new version of EQ-5D, is still insensitive to the health difference between slightly declined health status and full health.
There were no missing responses to the all 5L dimensions and the instrument had good completion rate, which was consistent with the results of several studies before [32, 39, 40], suggesting its good feasibility in the population. On the other hand, around 70% of respondents reported “no problems” on all the 5L dimensions. This result is higher than that of the general population (50.8%) [41]. The possible reason is that the general population includes people with disease, while the primary health care workers in the study are engaged in their daily work without disease. The proportions of subjects reporting “no problems” on the “pain/discomfort” and “anxiety/depression” dimensions were 82.3% and 79.5%, respectively. Compared with the other three dimensions accounting for nearly 100%, the ceiling effects were slightly weaker on those two specific dimensions. Previous studies in specific patient and general populations have also reported that “anxiety/depression” and “pain/discomfort” were two dimensions presenting relatively more frequent problems [42,43,44]. It also reflected that the mental problems were important factors affecting the health of primary health care workers in China, which was similar to the existing report [33].
The convergent validity of 5L utility score in measuring sub-health was poor. Its correlations with the SHMS V1.0 overall and three subscales scores were low, especially with the SHMS V1.0 SS score. As a sub-health specific scale, SHMS V1.0 covers a wide range of dimensions in the physical, mental and social health; whereas the 5L contains only five dimensions and lacks dimension related to social health. In terms of similar dimensions between the two instruments, the SHMS V1.0 items are profounder and richer, and the measured content is more comprehensive and detailed. Thus it can detect different health status of the population effectively. For example, the SHMS V1.0 “organic function” dimension includes measurements of vision and hearing in addition to measurements of gastrointestinal and head pain or discomfort. In contrast to the 5L “anxiety/depression” dimension consisting of a single item, the SHMS V1.0 “psychosocial symptom” dimension contains 5 items specifically measuring feelings like nervousness, fear, loneliness and so on. Those feelings often accompany or easily exacerbate to anxiety or depression, so the SHMS V1.0 can capture less severe changes in psychological symptoms. We were surprised that a very low correlation between the "mobility" dimension of the 5L and a similar dimension of the SHMS V1.0, "physical mobility function" (r = − 0.099) was identified. The same was true for 5L "usual activity" dimension and SHMS V1.0 "vitality" dimension (r = − 0.056). In addition, the multiple items within a certain dimension facilitate multiple reflections around that dimension by subjects, and thus better reflect the true situation. The correlations between the EQ-VAS and the SHMS V1.0 overall and three subscale scores were not strong but better compared with those between 5L utility score and SHMS V1.0 scores. It indicates to some extent that the EQ-VAS is able to reflect health dimensions that the 5L descriptive system do not include, which corresponds to the prior finding [45].
Based on the Kruskal–Wallis H values and the results of pairwise comparisons of 5L across the overall, physical, mental and social health, the 5L had the poorest known-groups validity in social health and was not sufficiently effective in distinguishing groups of respondents with different levels of sub-health, especially for the respondents with adjacent health status. The known-groups validity of EQ-VAS score was slightly better compared with the 5L utility score. The possible explanation is that the respondents may provide a global assessment of their health on the EQ-VAS, which is not limited to the five dimensions of 5L.
Previous studies have shown that the 5L could hardly reflect the effects of fatigue, interpersonal relationships, sleep, vision, hearing and drug-induced adverse reactions (such as loss of libido and hair loss) on HRQoL [46,47,48,49,50]. Those factors are important for determining whether an individual is in full health or with varying degrees of sub-health. In addition, 5L takes the same day as the recall period which may not be conducive to the measurement of sub-health characterizing as a long-term chronic state.
There are some limitations to the study. Although SHMS V1.0 is a widely used sub-health measurement instrument, choosing it as an external criterion may still be not enough thus influencing the accuracy of sub-health measurement and the assessment of measurement properties of 5L. The value set used to calculate 5L utility score was derived from a previous study based on a sample of urban residents from five cities in China [35], but 37% of the sample in this study was agricultural households, which might have caused potential bias. In addition, because the study was based on a cross-sectional survey, we cannot evaluate the responsiveness of 5L in the sub-healthy population.
Conclusions
To conclude, it appears that the EQ-5D-5L lacks measurement properties in measuring HRQoL in sub-healthy population in China. Hence, we should be cautious to use it in some sub-healthy groups whose health is close to full health.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due these data will still be used as auxiliary data in our other studies and we do not wish to publish them publicly but they are available from the corresponding author on reasonable request.
Abbreviations
- TCM:
-
Traditional Chinese medicine
- MUS:
-
Medically unexplained symptoms
- HRQoL:
-
Health related quality of life
- SHMS V1.0:
-
Sub-health measurement scale V1.0
- GS:
-
General items of sub-health
- PS:
-
Physical sub-health scale
- MS:
-
Mental sub-health scale
- SS:
-
Social sub-health scale
- VAS:
-
Visual analog scale
References
Ma C, Xu W, Zhou L, Ma S, Wang Y. Association between lifestyle factors and suboptimal health status among Chinese college freshmen: a cross-sectional study. BMC Public Health. 2018;18:105.
Rong Z. Interpretation of the clinical guidelines of Chinese medicine in sub-health. Mod Distance Educ Chin Med. 2009;7:79–80.
Yuxue W. Sub-health issues in a nutshell. PLA Health. 2005;6–9.
Wang W, Russell A, Yan Y. Traditional Chinese medicine and new concepts of predictive, preventive and personalized medicine in diagnosis and treatment of suboptimal health. Epma J. 2014;5:4.
Brown RJ. Introduction to the special issue on medically unexplained symptoms: background and future directions. Clin Psychol Rev. 2007;27:769–80.
Henningsen P, Zipfel S, Herzog W. Management of functional somatic syndromes. Lancet. 2007;369:946–55.
Schaefert R, Hausteiner-Wiehle C, Häuser W, Ronel J, Herrmann M, Henningsen P. Non-specific, functional, and somatoform bodily complaints. Dtsch Arztebl Int. 2012;109:803–13.
Chen F, Xiaolin X, Tianfang W. Concept category and taxonomy of sub-health. J Liaoning Univ TCM. 2010;12:43–5.
Jinhua Z, Jun X, Jimeng H, Liyi F, Ren L. Quantitative study of sub-health measurement. Guangdong Med J. 2009;30:1746–8.
Hilderink PH, Collard R, Rosmalen JG, Oude Voshaar RC. Prevalence of somatoform disorders and medically unexplained symptoms in old age populations in comparison with younger age groups: a systematic review. Ageing Res Rev. 2013;12:151–6.
Ma N, Liu M. Research progress on the epidemiology of sub-health state. China Prev Med. 2012;13:556–9.
Xue Y, Xu J, Liu G, Huang C, Feng Y, Xu M, Jiang L, Wang X, Xie J, Chen X. Evaluation of sub-health status of Chinese urban residents using the Sub-health Measurement Scale Version 1.0. Chin Gen Pract. 2021;24:834–41.
Pan Y, Yan J, Lu W, Shan M. Sub-health status survey and influential factor analysis in Chinese during coronavirus disease 2019 pandemic. J Korean Acad Nurs. 2021;51:5–14.
Wenqi Z, Yumin H. On the Concepts of “Treating Latent Disease Before Onset” and Sub-health. SHJTCM. 2008;57–59.
Kupaev V, Borisov O, Marutina E, Yan YX, Wang W. Integration of suboptimal health status and endothelial dysfunction as a new aspect for risk evaluation of cardiovascular disease. Epma J. 2016;7:19.
Adua E, Roberts P, Wang W. Incorporation of suboptimal health status as a potential risk assessment for type II diabetes mellitus: a case-control study in a Ghanaian population. Epma J. 2017;8:345–55.
Wang Y, Liu X, Qiu J, Wang H, Liu D, Zhao Z, Song M, Song Q, Wang X, Zhou Y, Wang W. Association between ideal cardiovascular health metrics and suboptimal health status in Chinese population. Sci Rep. 2017;7:14975.
Hui Z, Yuan L, Feifei X, Zhiyu W, Chun L. Status of evaluation and diagnosis of sub-health state and countermeasures. SHJTCM. 2016;50:8–10.
Xu J, Feng LY, Luo R, Qiu JC, Zhang JH, Zhao XS, Lu Y, Wei Q. Assessment of the reliability and validity of the Sub-health Measurement Scale Version1.0. South Med Univ. 2011;31:33–8.
Yan YX, Liu YQ, Li M, Hu PF, Guo AM, Yang XH, Qiu JJ, Yang SS, Shen J, Zhang LP, Wang W. Development and evaluation of a questionnaire for measuring suboptimal health status in urban Chinese. J Epidemiol. 2009;19:333–41.
Guo Z, Meng R, Zheng Y, Li X, Zhou Z, Yu L, Tang Q, Zhao Y, Garcia M, Yan Y, et al. Translation and cross-cultural validation of a precision health tool, the Suboptimal Health Status Questionnaire-25, in Korean. J Glob Health. 2022;12:04077.
Bi JL, Chen J, Sun XM, Nie XL, Liu YY, Luo R, Zhao XS. The development and evaluation of a sub-health self-rating scale for university students in China. BMC Public Health. 2019;19:330.
Jun X, Yaning X, Bo L, Minyan H. The study of validity on self-rated health measuremnet scale-the revised version 1.0. Chin J Clin Rehab. 2002;2082–2085.
Jun X, Jian T, Yipeng W, Minyan H. Evaluation of the self-rated health measuremnet scale-the revised Version 1.0. Chin J Ment Health. 2003;301–305.
Miao J, Liu J, Wang Y, Zhang Y, Yuan H. Reliability and validity of SHMS v1.0 for suboptimal health status assessment of Tianjin residents and factors affecting sub-health: A cross-sectional study. Medicine (Baltimore). 2021;100:e25401.
Bi J, Huang Y, Xiao Y, Cheng J, Li F, Wang T, Chen J, Wu L, Liu Y, Luo R, Zhao X. Association of lifestyle factors and suboptimal health status: a cross-sectional study of Chinese students. BMJ Open. 2014;4: e005156.
Wu S, Xuan Z, Li F, Xiao W, Fu X, Jiang P, Chen J, Xiang L, Liu Y, Nie X, et al. Work-Recreation balance, health-promoting lifestyles and suboptimal health status in Southern China: a cross-sectional study. Int J Environ Res Public Health. 2016;13.
Chen J, Cheng J, Liu Y, Tang Y, Sun X, Wang T, Xiao Y, Li F, Xiang L, Jiang P, et al. Associations between breakfast eating habits and health-promoting lifestyle, suboptimal health status in Southern China: a population based, cross sectional study. J Transl Med. 2014;12:348.
Chen J, Xiang H, Jiang P, Yu L, Jing Y, Li F, Wu S, Fu X, Liu Y, Kwan H, et al. The Role of healthy lifestyle in the implementation of regressing suboptimal health status among college students in China: A nested case-control study. Int J Environ Res Public Health. 2017;14.
Zeng X, Sui M, Liu B, Yang H, Liu R, Tan RL, Xu J, Zheng E, Yang J, Liu C, et al. Measurement properties of the EQ-5D-5L and EQ-5D-3L in six commonly diagnosed cancers. Patient. 2021;14:209–22.
Xu RH, Dong D, Luo N, Wong EL, Wu Y, Yu S, Yang R, Liu J, Yuan H, Zhang S. Evaluating the psychometric properties of the EQ-5D-5L and SF-6D among patients with haemophilia. Eur J Health Econ. 2021;22:547–57.
Bilbao A, García-Pérez L, Arenaza JC, García I, Ariza-Cardiel G, Trujillo-Martín E, Forjaz MJ, Martín-Fernández J. Psychometric properties of the EQ-5D-5L in patients with hip or knee osteoarthritis: reliability, validity and responsiveness. Qual Life Res. 2018;27:2897–908.
Xiyue Z. Research progress on psychological problems and interventions for health care workers under the COVID-19 epidemic. J Jilin Med Univ. 2022;43:145–7.
Luo N, Liu G, Li M, Guan H, Jin X, Rand-Hendriksen K. Estimating an EQ-5D-5L Value Set for China. Value Health. 2017;20:662–9.
Cohen J. Statistical power analysis for the behavioral-sciences: cohen. J Perceptual and Motor Skills. 1988;67:1007–1007.
Bolarinwa OA. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J. 2015;22:195–201.
Jun X, Yan L, Liyi F, Jincai Q, Liai Z, Rongjie Q, Xinxin F, Juan X, Qian W. Preliminary study of sub-health measurement scale Version1.0 norms for Chinese civil servants. J South Med Univ. 2011;31:1654–62.
Liu GG, Guan H, Jin X, Zhang H, Vortherms SA, Wu H. Rural population’s preferences matter: a value set for the EQ-5D-3L health states for China’s rural population. Health Qual Life Outcomes. 2022;20:14.
Janssen MF, Pickard AS, Golicki D, Gudex C, Niewada M, Scalone L, Swinburn P, Busschbach J. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res. 2013;22:1717–27.
Scalone L, Ciampichini R, Fagiuoli S, Gardini I, Fusco F, Gaeta L, Del Prete A, Cesana G, Mantovani LG. Comparing the performance of the standard EQ-5D 3L with the new version EQ-5D 5L in patients with chronic hepatic diseases. Qual Life Res. 2013;22:1707–16.
Xie S, Wu J, Xie F. Population Norms for SF-6Dv2 and EQ-5D-5L in China. Appl Health Econ Health Policy. 2022;20:573–85.
Yfantopoulos J, Chantzaras A, Kontodimas S. Assessment of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in psoriasis. Arch Dermatol Res. 2017;309:357–70.
Kim TH, Jo MW, Lee SI, Kim SH, Chung SM. Psychometric properties of the EQ-5D-5L in the general population of South Korea. Qual Life Res. 2013;22:2245–53.
Yfantopoulos JN, Chantzaras AE. Validation and comparison of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in Greece. Eur J Health Econ. 2017;18:519–31.
Feng Y, Parkin D, Devlin NJ. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual Life Res. 2014;23:977–89.
Efthymiadou O, Mossman J, Kanavos P. Health related quality of life aspects not captured by EQ-5D-5L: Results from an international survey of patients. Health Policy. 2019;123:159–65.
Finch AP, Brazier JE, Mukuria C, Bjorner JB. An exploratory study on using principal-component analysis and confirmatory factor analysis to identify bolt-on dimensions: the EQ-5D case study. Value Health. 2017;20:1362–75.
Wang P, Chong SL, Tan RL, Luo N. A hearing bolt-on item increased the measurement properties of the EQ-5D-5L in a community-based hearing loss screening program. Eur J Health Econ 2022.
Spronk I, Polinder S, Bonsel GJ, Janssen MF, Haagsma JA. The relation between EQ-5D and fatigue in a Dutch general population sample: an explorative study. Health Qual Life Outcomes. 2021;19:135.
Geraerds A, Polinder S, Spronk I, Olde Loohuis AGM, de Groot A, Bronner MB, Haagsma JA. Sensitivity of the EQ-5D-5L for fatigue and cognitive problems and their added value in Q-fever patients. Qual Life Res. 2022;31:2083–92.
Acknowledgements
We thank primary health care workers who volunteered to participate in our research and the members involved in data collection and analysis.
Funding
No funding.
Author information
Authors and Affiliations
Author notes
Yueyue Liu and Chuchuan Wan contributed equally to this work and share first authorship.
Contributions
YL was a major contributor in writing the main manuscript. CW analyzed and interpreted the data regarding the research. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of China Pharmaceutical University (No.CPU2019015). All methods were performed in accordance with the relevant guidelines and regulations. Based on the principle of informed consent, all data were collected anonymously after obtaining the permission and informed consent signed by respondents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Demarcation norms of the SHMS V1.0 total and subscales scores in Chinese civil servants.
Additional file 2.
Convergent and known-groups validity of 5L utility score and EQ-VAS score in subgroups divided by different regions of China.
Additional file 3.
Pairwise comparisons of 5L utility score and EQ-VAS score in known groups divided by health status.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., Wan, C. & Xi, X. Measurement properties of the EQ-5D-5L in sub-health: evidence based on primary health care workers in China. Health Qual Life Outcomes 21, 22 (2023). https://doi.org/10.1186/s12955-023-02105-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-023-02105-1