Abstract
Background
Suboptimal health status (SHS) is the intermediate health state between health and disease, refers to medically undiagnosed or functional somatic syndromes, and has been a major global public health challenge. However, both the etiology and mechanisms associated with SHS are still unclear. Breakfast eating behavior is a dietary pattern marker and previous studies have presented evidence of associations between failure to consume breakfast and increased diseases. Accordingly, in view of the significance of breakfast eating behaviors with respect to health status, the associations between breakfast eating habits and healthy lifestyle, SHS require further elucidation.
Methods
A cross-sectional survey was conducted within a clustered sample of 24,159 individuals aged 12–80 years in 2012–13 within the population of Southern China. Breakfast eating habits were categorically defined by consumption frequency (‘scarcely, sometimes or always’). Health-promoting lifestyle was assessed via the health-promoting lifestyle profile (HPLP-II). SHS was evaluated using the medical examination report and Sub-health Measurement Scale V1.0 (SHMS V1.0).
Results
Of the 24,159 participants, the prevalence rates for the ‘health’ , ‘SHS’ , and ‘disease’ were 18.8%, 46.0%, and 35.2%, respectively. Overall, 19.6% of participants reported ‘scarce’ breakfast eating habits, with frequent breakfast eaters scoring higher on both HPLP-II and SHMS V1.0. After demographic adjustment, regression analyses revealed a significant association between breakfast eating habits and healthy lifestyle (p <0.001). There were lower levels of breakfast consumption regularity amongst individuals with SHS than those with disease. Categorically ‘scarce’ breakfast eaters were approximately three times more likely to be assigned SHS (OR: 2.745, 95% CI: 2.468-3.053), while infrequent breakfast eaters (‘sometimes’) were just less than twice as likely to be assessed as being of SHS (OR: 1.731, 95% CI: 1.595-1.879).
Conclusions
Breakfast eating habits are significantly associated with a healthy lifestyle, and appear to be a useful predictor of a healthy lifestyle. Irregular breakfast eating habits are related to an increased risk of SHS; increased breakfast eating frequency may contribute to lowering the prevalence of SHS in Southern China.
Similar content being viewed by others
Background
It has been regularly and widely propounded that breakfast is the most important meal of the day; breakfast consumption has been shown to improve energy, control appetite and reduce the risk of overeating [1,2]. Breakfast eating behavior is considered a dietary pattern marker, in addition to an essential healthy lifestyle component [3,4]. Previous studies have presented evidence of associations between failure to consume breakfast and increased bodyweight [5,6], in addition to contraction of cardiovascular disease [7], metabolic conditions [8,9], dyslipidemia and insulin resistance [10], type 2 diabetes mellitus [11] and reproductive dysfunction [12]. Moreover, regular breakfast consumption has been correlated with energy balance [13], behavioral and cognitive functioning [14,15], personal wellbeing and mental health [3,16]. Furthermore, significant relationships between health status and lifestyle have been evidenced, as underscored with the importance of breakfast eating due to the concurrent positive effects on health status [17,18].
In parallel with social economic development and the increasing pace of life, a growing appreciation for the importance of health has developed. The overarching concept of health status has been categorized into three distinct types, namely health, disease and the intermediate state between health and disease, referred to as suboptimal health status (SHS). SHS refers to medically undiagnosed or functional somatic syndromes [19-22], characterized by a decline in vitality, physiological function and the capacity to adapt to varying conditions [23]. People in SHS frequently suffer from symptoms including chronic fatigue, headaches, dizziness, depression, anxiety, non-specific pain (e.g. back pain and chest pain), functional system disorders (e.g. digestive system, cardiovascular system, respiratory system, urinary system). Accordingly, SHS sufferers are typified by impaired quality of life, frequent hospital visits and incurred medical expenses [20,21]. A previous investigation by the current authors found that suboptimal health status was applicable to 65.1% of the surveyed population in Southern China [24], with SHS now a major global public health challenge [20,25,26]. Current prevention and intervention strategies recommend disease prevention and effective treatment of early-stage illness [27,28]. However, both the etiology and mechanisms associated with SHS require further elucidation.
Accordingly, in view of the significance of breakfast eating behaviors with respect to health status, the authors theorize that breakfast eating habits are likely related to SHS. To date, no human studies of breakfast eating behaviors with respect to SHS have been published, in concurrence with a paucity of data pertaining to the potential association between breakfast eating habits and health status within the Chinese population. Thus, a comprehensive cross-sectional study was conducted within Southern China which aimed to examine the existence of associations between breakfast eating habits, healthy lifestyles and the risk of SHS.
Methods
Study design and population
The study was a cross-sectional descriptive survey, with a three-stage stratified sampling method employed. In stage one, six areas of South China (Guangzhou, Zhuhai, Huizhou, Jiangmen, Zhanjiang, and Shaoguan) were selected to be representative of economic characteristics, population demographic and geographic distribution. In the second stage of sampling, one region was randomly selected from each of the aforementioned areas. In the final stage, one unit (e.g. schools, companies, government agencies or factories) was selected from each region.
Overall, 28,144 individuals aged 12–80 years from 14 primary sampling units undertook the baseline survey in 2012–13, with 24,159 individuals (11,796 men and 12,363 women) included for the current analysis. Due to the invalid responses information (e.g. breakfast eating habits, baseline characteristics or the scale written in chaos), 3,985 respondents were excluded from further consideration, resulting in a valid response rate of 85.8%. Informed oral consent was obtained from every participant prior to data collection. Verbal consent was deemed sufficient as participants had previously volunteered for the study and could refuse to participate. All data were kept strictly confidential. The ethics committee also approved the consent procedure.
Survey instrument
The developed questionnaire was a combination of self-designed questionnaire items and a standardized questionnaire. The self-designed questionnaire components comprised the general demographic characteristics (including age, gender, BMI, married status, education level, occupation, smoking, and drinking) and breakfast eating frequency assessment, defined according to frequency of behavior using a three-point respond format, “scarcely, sometimes, always”, with the rating score ranging from 1 to 3. The standardized components were based upon the “Sub-Health Measurement Scale V1.0 (SHMS V1.0)” and the “Health-promoting lifestyle profile (HPLP-II)” to permit assessment of participants’ health status and health-promoting lifestyles. Uniform instructions were provided by trained investigators, with questionnaires self-completed by participants over a 30 minute period.
SHS assessment
Health status assessment was performed in accordance with a medical examination report and SHMS V1.0, according to clinical guidelines for SHS published by the China Association of Chinese Medicine [23,29]. SHMS V1.0 was developed by our research group, with Chinese research data indicating that the scale has a high level of reliability and validity, with a Cronbach α and split-half reliability coefficients of 0.917 and 0.831, respectively [30]. The scale consists of 39 items in total, 35 of which are divided among three symptom dimensions (physiological symptoms - 14 items, psychological symptoms - 12 items and social symptoms - 9 items). Participants were asked about uncomfortable symptoms that they had experienced during the previous month, with total scores then calculated. A low total score represents a high likelihood of SHS (i.e. poor health). Prior to surveying, participants had attended an annual unit health examination in hospital, comprising medical history, a physical examination, blood haematology and biochemical analyses, rest ECG and chest radiography. After exclusion of participants diagnosed with clinical disease in the health examination by clinical doctors, threshold values for SHS within the physiological, psychological and society dimensions of SHMS V1.0 were 68, 67 and 67, respectively. If participants were not in SHS with respect to any of these three dimensions (physiological, psychological and society), they were considered healthy [23,30].
Lifestyle health assessment
HPLP-II has been widely used as a measuring tool for assessing health promoting behaviors and is considered to offer both reliability and validity, domestically and internationally [31,32]. It comprises 52 items assessing six dimensions of lifestyle: self-realization, health responsibility, sports and exercise, nutrition, interpersonal relationship and stress management. It may be used to assess the frequency of the health promoting behaviors, based on a self-reported four-point Likert scale: “never, sometimes, usually, always”, with the rating score ranging from 1 to 4. The minimum and maximum HPLP-II scores are 52 and 208, respectively. The higher score represents a maximal level of health with respect to lifestyle. Health promoting lifestyle score is divided into four grades: poor (52–90), general (91–129), good (130–168) and excellent (169–208).
Statistical methods
Descriptive statistics have been presented as frequencies. Univariate analyses were used to compare varying breakfast eating frequencies with both lifestyle health and health status scores using one-way ANOVA and Bonferroni correction for ad-hoc multiple comparisons. Multinomial logistic regression was used to estimate the typical profile for irregular breakfast eaters based upon demographic variables. The reference group was defined as those participants with the lowest level of exposure i.e. habitual breakfast eaters, or excellent lifestyle behavior. Multinomial logistic regression was used to estimate associations when using lifestyle health and health status as the outcomes of interest. Adjustments were made for potential confounders within multivariable models based upon collated demographic data. Estimation of the odds associated with self-reported symptoms of SHMS V1.0 was undertaken by adding breakfast eating frequency and demographic adjustments to multinomial logistic regression. The percentage of participants with missing values associated with relevant covariates was small e.g. 1.0% for smoking, and 0.7% for alcohol consumption; accordingly, all participants with available data for all covariates were included for multivariable analysis. All data analyses were done using SPSS 13.0. All p-values were two sided, with values <0.05 considered statistically significant.
Results
Sample characteristics
Baseline characteristics of all study participants are presented in Table 1. Of the 24,159 participants (11,796 men and 12,363 women), the mean age was 27.07 years. The prevalence rates for the ‘health’ , ‘SHS’ , and ‘disease’ groups of participants were 18.8% (4,533), 46.0% (11,121), and 35.2% (8,505), respectively. The major diseases that were reported affected the respiratory, digestive systems and endocrine or autoimmune systems, such as chronic rhinitis (10.6%), chronic pharyngolaryngitis (9.4%), chronic gastritis (4.7%), gynaecopathia (4.3%), chronic insomnia (3.8%), haemorrhoids (3.5%), breast disease (3.1%), fatty liver (2.3%), hypertension (2,0%), chronic bronchitis (1.8%), gastroduodenal ulcer (1.8%), rheumatic disease (1.8%), hyperlipemia (1.3%), chronic joint disease (1.2%), chronic otitis media (0.9%), thyroid disease (0.8%), cholecystitis (0.6%), chronic hepatitis (0.5%), heart disease (0.5%), diabetes (0.4%), prostatic diseases (0.4%), cancar (0.4%), asthma (0.3%), cerebrovascular disease (0.2%), arteriosclerosis (0.1%), tuberculosis (0.1%), chronic nephritis (0.1%).
Profile of irregular breakfast eaters
Baseline population demographics of the group characterized by irregular breakfast eating are presented in Table 2. Results indicate that demographic characteristics are significantly associated with irregular breakfast eating, particularly amongst those reporting the lowest level of breakfast eating frequency. Participants who reported poor breakfast eating habits were more likely to be young, male, unmarried, have a lower level of formal education and higher levels of smoking and drinking.
Breakfast eating frequency compared with health-promoting lifestyle and health status
Results of one-way ANOVA for breakfast eating frequency compared with both health-promoting lifestyle and health status are presented in Table 3. Those who reported the lowest level of breakfast eating frequency accounted for 19.6% of the total sample population. Analyses revealed significant differences with respect to six dimensions of health-promoting lifestyle and breakfast eating frequency, in addition to the total HPLP-II score (F (2, 24156) = 1738.884, P = 0.000). After Bonferroni correction for multiple comparisons, this difference was statistically significant (p <0.001). Conversely, habitual breakfast eaters scored significantly higher on health status scales and the total HPLP-II score (F (2, 24156) = 502.081, P = 0.000). Bonferroni ad-hoc tests revealed significant differences with respect to breakfast eating frequency (p <0.001).
Associations between breakfast eating frequency and health-promoting lifestyle
Associations found between breakfast eating frequency and health-promoting lifestyle are presented in Table 4. Multivariable regression analyses with adjusted demographic variables revealed a significant association between breakfast eating frequency and health-promoting lifestyle (p <0.001). Compared with habitual breakfast eaters, those with the lowest breakfast eating frequency were approximately 95 times more likely to exhibit a poor health-promoting lifestyle (OR 95.415, 95% CI 58.489-155.654), while those that infrequently ate breakfast were almost 12 times more likely to exhibit a poor health-promoting lifestyle (OR 11.855, 95% CI 8.839-15.900). Furthermore, skipping or infrequent breakfast eating had marked associations with respect to other components of a healthy lifestyle including poor nutrition (OR 193.085, 95% CI 90.922-410.041), poor interpersonal relationships (OR 34.195, 95% CI 25.824-45.280), poor stress management (OR 33.339, 95% CI 26.0259-42.710), poor self-realization (OR 11.504, 95% CI 9.371-14.122)), poor health responsibility (OR 9.828, 95% CI 6.072-15.909) and low levels of sports and exercise (OR 6.526, 95% CI 5.233-8.139).
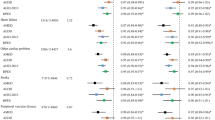
Association between breakfast eating habits and health status
Odds ratios pertaining to breakfast eating frequency and health status are presented in Table 5. Positive frequency-responses were noted with respect to the likelihood of both SHS and disease in concurrence with breakfast eating frequency. There were lower levels of breakfast consumption regularity amongst individuals with SHS than those with disease. Those respondents reporting a scarce level of frequency were almost three times more likely to contract SHS (odds ratio 2.745, 95% confidence interval 2.468 to 3.053), while those citing infrequent breakfast consumption were approximately 1.7 times more likely to contract SHS (OR 1.731, 95% CI 1.879-21.595), relative to habitual breakfast eaters (p <0.001). Similarly, the group characterized by the lowest frequency was approximately 88% more likely to contract disease than habitual breakfast eaters (OR 1.878, 95% CI 1.673-2.108). There were significant effects on the likelihood of SHS with respect to three symptomatic dimensions (physiological, psychological and social); for example, compared with habitual breakfast eaters, individuals with the lowest breakfast eating frequency were approximately 63% more likely to exhibit physiological SHS (OR 1.625, 95% CI 1.468-1.800), while odds ratios of 1.588 (95% CI 1.412-1.786) and 1.83 (95% CI 1.612-2.078) were associated with physiological SHS and social SHS, respectively, within the same group. Results remained consistent throughout analyses, with all evidence indicating that breakfast consumption frequency (dependent variable) has significant associations with self-reported symptoms when the three aforementioned dimensions are employed as model outcomes (Additional file 1: Tables S1, S2 and S3 in the Data Supplement).
Discussion
To date, the current study represents the first comprehensive investigation of the associations between healthy lifestyle, SHS and breakfast eating habits within the Chinese population. Findings indicate that irregular breakfast eating is associated with myriad unhealthy lifestyle behaviors. A significant association was found between the frequency of breakfast consumption and the prevalence of both SHS and disease; a frequency-response effect was noted, with increased breakfast consumption being correlated with decreased prevalence of both conditions. Habits pertaining to breakfast consumption were significantly associated with all three health status dimensions (physiological, psychological and social).
Breakfast eating habits and demographic characteristics
The lowest level of breakfast consumption was observed amongst <25 years of age, with breakfast skipping increasing in prevalence with the transition to adulthood. Overall, results indicate that adolescents are more likely to skip breakfast, with similar findings having been previously reported [17,33]. Females, married individuals and those with higher levels of education exhibited more frequent breakfast eating habits; similar findings have been reported within a nationally representative UK sample [3]. Moreover, analyses revealed that categorically unhealthy behaviors such as smoking or drinking were frequently accompanied by a decreasing frequency of breakfast consumption. Further studies and resulting strategies are required to communicate the importance of breakfast eating in order to effectively meet the health requirements of specific population demographics.
Breakfast eating habits and health-promoted lifestyle
Findings indicate a significant relationship between breakfast consumption and participant lifestyle. Those who frequently consumed breakfast tended to be associated with healthier overall lifestyle patterns, including elevated attention towards personal nutrition, enhanced interpersonal relationships and stress management capabilities and frequent physical activity. For example, habitual breakfast eaters exhibited a higher proclivity towards physical activities than infrequent breakfast eaters [3], while those that often skipped breakfast were associated with a higher daily intake of fat, cholesterol and energy than habitual breakfast eaters [34]. Assessment of breakfast eating habits may represent a powerful tool for the prediction of a healthy lifestyle.
Breakfast eating habits and SHS
The World Health Organization (WHO) has defined health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” since 1948 [35]. This concept is put forward from the high pace of life of the body and mental reaction and people's emphasis on quality of life. But this definition is still a controversy for in the research of intension about health, there are problems as obscurities in definition [36]. The controversy, however, drove the need for a definition and a deeper understanding of the intermediate state between health and disease, that’s what is called SHS, which have been put forward to account for it by Wang [27,28,37]. Results in this study indicate a high prevalence of SHS among the sample population (46%), which is similar to previous reports [24,38]. High though the prevalence of SHS is, the mechanism underlying SHS has yet to be ascertained and there has been a lack of objective clinical diagnostics for SHS. SHS questionnaires have been developed and widely used as diagnostic instruments of SHS in China, such as Suboptimal Health Status Questionnaire-25 (SHSQ-25) [39,40] and Multidimensional Sub-health Questionnaire of Adolescents (MSQA) [41]. SHSQ-25 is mainly aimed at physiological and psychological SHS and MSQA mainly suitable for adolescents. SHMS V1.0, however, is a multidimensional, self-report symptom inventory including physiological, psychological and social dimensions [30], which corresponds to the greater understanding of WHO’s definition about health. Since the mechanism underlying SHS has yet to be ascertained, the objective measurements for SHS are in the condition of exploration. Li, G., et al. [42] have investigated the biomarkers of SHS being attributable to the oxidative stress perspective, and found that SHS was associated with the plasma levels of thiobarbituric acid-reactive substances (TBARS).
Data obtained during the current study exhibit a marked association between SHS prevalence, disease and breakfast consumption frequency, with a positive frequency response evident between the likelihood of both SHS and disease contraction with breakfast eating habits i.e. decreased consumption frequency concurrent with increased likelihood of an adverse health response. Overall, SHS was more evident than disease within the sample population. Moreover, the positive association found between breakfast consumption habits and the instance of disease confirms results of previous studies [34], thus calling for further investigation of the association between breakfast consumption behaviors and the instance of SHS. Furthermore, results revealed a significant association between breakfast eating habits and assessed health status with respect to three symptomatic dimensions (physiological, psychological and social), based upon 35 existing symptom definitions from SHMS V1.0. Previous studies have reported that breakfast consumption is related to psychological variables, including eating style (cognitive restraint, uninhibited eating and emotional eating) [3]; this may be explanatory with respect to the aforementioned associations with both psychological and social health.
Tanaka et al. [43] have found that skipping breakfast was associated with an elevated prevalence of fatigue, while Smith et al. [44] provide evidence that consumption of high fibre cereals could represent a simple method for fatigue reduction. Smith et al. [45] have also shown that habitual breakfast consumption is was associated with a lower prevalence with respect to the common cold. Lawton et al. [46] previously reported that consumption of high fibre breakfast cereals may improve self-assessed digestive functionality and general wellbeing.
Meal timing may be causative with respect to the metabolic effects leading to SHS or disease; previous studies have shown that skipping breakfast may reduce insulin sensitivity in response to pre-loading, thus disturbing lipid profiles [10,47]. Further, omission of breakfast has been associated with impacts on overall diet composition via disruption of daily energy intake and up-regulation of appetite later in the day, leading to deleterious metabolic and endocrine-related variation in response to food consumed later in the morning [1,47,48]. Accordingly, less frequent eaters exhibit an inherently higher likelihood of contracting chronic diseases including diabetes, obesity and cardiovascular disease [34,49] in addition to SHS, thus further emphasizing the need for regular breakfast consumption.
Healthy lifestyles, SHS and breakfast eating habits
A potential reason for lower levels of breakfast consumption regularity amongst individuals with SHS than those with disease may be an inherently higher appreciation of the importance of lifestyle among the latter group. This hypothesis is supported by previous findings which have shown that breakfast consumption is correlated with individual consciousness [3].
An improved understanding of the role of breakfast consumption behaviors may have broad applications in public health and health promotion; the study demonstrates that breakfast eating behaviors may be an accurate behavioral marker for healthy lifestyle promotion, particularly in terms of SHS or disease. Previous studies have shown that underlying health-related risk factors include increased psychological pressure, poor dietary habits, sleep deprivation, social competition, sedentary activities, smoking and alcohol abuse [25,50-52], thus supporting findings from the current study. Our results suggest that habitual breakfast consumption leads to improved health and wellbeing via individual consciousness of healthy lifestyle decisions. Further studies should further examine breakfast food types and quality, and address these potential mechanisms of SHS and disease at the individual or population level via larger and longer trials.
Study strengths and limitations
The current study represents the first comprehensive investigation of associations between breakfast eating habits and SHS within the Chinese population. Potential confounders have been accounted for via consideration of baseline sample characteristics. Furthermore, this study is the first to demonstrate that breakfast eating behaviors are significantly associated with physiological, psychological and social health.
As with any respondent-completed questionnaire survey, responses may comprise a level of inherent inaccuracy or bias. The survey sample was comprised of a disproportionate number of students, thus representing a potential lack of population representivity. Moreover, although adjustments were made for several factors potentially associated with health and lifestyle, data pertaining to all variables related with breakfast eating were not collated (e.g. breakfast food type and quality), and were thus not included for analyses; future research should address these research limitations.
Conclusions
The presented cross-sectional survey is the first to assess breakfast eating habits in relation to healthy lifestyles and suboptimal health status within the Chinese population; highlighted associations are significant. Breakfast eating behaviors were found to be associated with suboptimal health status within three distinct categories, namely physiological, psychological and social health. Study findings provide evidence which supports regular breakfast consumption; appropriate dietary habits may contribute to reducing the prevalence of SHS and associated disease at both the individual and population levels in China, thus leading to healthier lifestyles and the associated social and economic benefits.
Additional file
References
Giovannini M, Agostoni C, Shamir R: Symposium overview: Do we all eat breakfast and is it important?. Crit Rev Food Sci Nutr. 2010, 50: 97-99. 10.1080/10408390903467373.
Jackson LW: The most important meal of the day: why children skip breakfast and what can be done about it. Pediatr Ann. 2013, 42: 184-187. 10.3928/00904481-20130823-10.
Reeves S, Halsey LG, McMeel Y, Huber JW: Breakfast habits, beliefs and measures of health and wellbeing in a nationally representative UK sample. Appetite. 2013, 60: 51-57. 10.1016/j.appet.2012.09.024.
Ruxton CH, Kirk TR: Breakfast: a review of associations with measures of dietary intake, physiology and biochemistry. Br J Nutr. 1997, 78: 199-213. 10.1079/BJN19970140.
Schembre SM, Wen CK, Davis JN, Shen E, Nguyen-Rodriguez ST, Belcher BR, Hsu YW, Weigensberg MJ, Goran MI, Spruijt-Metz D: Eating breakfast more frequently is cross-sectionally associated with greater physical activity and lower levels of adiposity in overweight Latina and African American girls. Am J Clin Nutr. 2013, 98: 275-281. 10.3945/ajcn.112.045849.
Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y, Saito K, Shimano H, Yamada N, Sone H: Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med. 2011, 53: 260-267. 10.1016/j.ypmed.2011.08.030.
di Giuseppe R, Di Castelnuovo A, Melegari C, De Lucia F, Santimone I, Sciarretta A, Barisciano P, Persichillo M, De Curtis A, Zito F, Krogh V, Donati MB, de Gaetano G, Iacoviello L: Typical breakfast food consumption and risk factors for cardiovascular disease in a large sample of Italian adults. Nutr Metab Cardiovasc Dis. 2012, 22: 347-354. 10.1016/j.numecd.2010.07.006.
Wennberg M, Gustafsson PE, Wennberg P, Hammarstrom A: Poor breakfast habits in adolescence predict the metabolic syndrome in adulthood. Public Health Nutr. 2014, 28: 1-8. 10.1017/S1368980013003509.
Odegaard AO, Jacobs DJ, Steffen LM, Van Horn L, Ludwig DS, Pereira MA: Breakfast frequency and development of metabolic risk. Diabetes Care. 2013, 36: 3100-3106. 10.2337/dc13-0316.
Farshchi HR, Taylor MA, Macdonald IA: Deleterious effects of omitting breakfast on insulin sensitivity and fasting lipid profiles in healthy lean women. Am J Clin Nutr. 2005, 81: 388-396.
Mekary RA, Giovannucci E, Cahill L, Willett WC, van Dam RM, Hu FB: Eating patterns and type 2 diabetes risk in older women: breakfast consumption and eating frequency. Am J Clin Nutr. 2013, 98: 436-443. 10.3945/ajcn.112.057521.
Fujiwara T, Nakata R: Skipping breakfast is associated with reproductive dysfunction in post-adolescent female college students. Appetite. 2010, 55: 714-717. 10.1016/j.appet.2010.08.005.
Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D: The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr. 2014, 100: 539-547. 10.3945/ajcn.114.083402.
Rampersaud GC, Pereira MA, Girard BL, Adams J, Metzl JD: Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc. 2005, 105: 743-760. 10.1016/j.jada.2005.02.007.
Simeon D, Grantham-McGregor S: Cognitive function, undernutrition, and missed breakfast. Lancet. 1987, 2: 737-738. 10.1016/S0140-6736(87)91092-0.
O'Sullivan TA, Robinson M, Kendall GE, Miller M, Jacoby P, Silburn SR, Oddy WH: A good-quality breakfast is associated with better mental health in adolescence. Public Health Nutr. 2009, 12: 249-258. 10.1017/S1368980008003935.
Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB: Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011, 364: 2392-2404. 10.1056/NEJMoa1014296.
Kastorini CM, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB: The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol. 2011, 57: 1299-1313. 10.1016/j.jacc.2010.09.073.
Schmid G, Dinkel A, Henningsen P, Dieterich M, Hopfner A, Pieh C, Lahmann C: Assessment of psychological aspects of somatoform disorders: a study on the German version of the Health Attitude Survey (HAS). Compr Psychiatry. 2014, 55: 155-164. 10.1016/j.comppsych.2013.08.013.
Schaefert R, Hausteiner-Wiehle C, Hauser W, Ronel J, Herrmann M, Henningsen P: Non-specific, functional, and somatoform bodily complaints. Dtsch Arztebl Int. 2012, 109: 803-813.
Henningsen P, Zipfel S, Herzog W: Management of functional somatic syndromes. Lancet. 2007, 369: 946-955. 10.1016/S0140-6736(07)60159-7.
Sharpe M, Mayou R, Bass C: Concepts, theories and terminology. Treatment of Functional Somatic Symptoms. Edited by: Mayou R, Bass C, Sharpe M. 1995, Oxford University Press, Oxford, 3-16.
Bi J, Huang Y, Xiao Y, Cheng J, Li F, Wang T, Chen J, Wu L, Liu Y, Luo R, Zhao X: Association of lifestyle factors and suboptimal health status: a cross-sectional study of Chinese students. BMJ Open. 2014, 4: e5156-10.1136/bmjopen-2014-005156.
Sun X, Wei M, Zhu C, Wang X, Zhao X, Luo R: The epidemiological investigation of sub-health in Guangdong. Shandong Med J. 2008, 48: 59-60.
Ma N, Liu M: Research progress on the epidemiology of sub-health state. China Prev Med. 2012, 7: 556-559.
Hilderink PH, Collard R, Rosmalen JG, Oude VR: Prevalence of somatoform disorders and medically unexplained symptoms in old age populations in comparison with younger age groups: a systematic review. Ageing Res Rev. 2013, 12: 151-156. 10.1016/j.arr.2012.04.004.
Wang W, Yan Y: Suboptimal health: a new health dimension for translational medicine. Clin Transl Med. 2012, 1: 28-10.1186/2001-1326-1-28.
Wang W, Russell A, Yan Y: Traditional Chinese medicine and new concepts of predictive, preventive and personalized medicine in diagnosis and treatment of suboptimal health. EPMA J. 2014, 5: 4-10.1186/1878-5085-5-4.
Medicine CAOC: The TCM Clinical Guidelines of Suboptimal Health Status. 2006, China Press TCM, Beijing
Xun J, Feng L, Luo R, Qiu J, Zhang J, Zhao X, Lu Y, Wu Q: Assessment of the reliability and validity of the Sub-health Measurement Scale Version1.0. J South Med Univ. 2011, 31: 33-38.
Pinar R, Celik R, Bahcecik N: Reliability and construct validity of the health-promoting lifestyle profile II in an adult Turkish population. Nurs Res. 2009, 58: 184-193. 10.1097/NNR.0b013e31819a8248.
Wang Y, Wu L, Xia W, Sun C, Wei C, Shang T: Reliability and validity of Chinese version of the health-promoting lifestyle profile. Chin J Sch Health. 2007, 28: 889-891.
Morgan KJ, Zabik ME, Stampley GL: The role of breakfast in diet adequacy of the U.S. adult population. J Am Coll Nutr. 1986, 5: 551-563. 10.1080/07315724.1986.10720156.
Timlin MT, Pereira MA: Breakfast frequency and quality in the etiology of adult obesity and chronic diseases. Nutr Rev. 2007, 65: 268-281. 10.1111/j.1753-4887.2007.tb00304.x.
WHO: Constitution of the World Health Organization. 2006, www.who.int/governance/eb/who_constitution_en.pdf.
Jadad AROL: How should health be defined?. BMJ. 2008, 337: 1363-1364. 10.1136/bmj.a2900.
Wang LM, Zhao X, Wu XL, Li Y, Yi DH, Cui HT, Chen JX: Diagnosis analysis of 4 TCM patterns in suboptimal health status: a structural equation modelling approach. Evid Based Complement Alternat Med. 2012, 2012: 970985-
Xie Y, Liu B, Pu H, He L, Yi D, Li W, Hu J, Gao R, He L, Gao Y, Peng X: Analysis on risk factors of sub-health among different crowds in Beijing. Chin J Public Health. 2006, 22: 1106-1107.
Yan YX, Dong J, Liu YQ, Yang XH, Li M, Shia G, Wang W: Association of suboptimal health status and cardiovascular risk factors in urban Chinese workers. J Urban Health. 2012, 89: 329-338. 10.1007/s11524-011-9636-8.
Yan YX, Liu YQ, Li M, Hu PF, Guo AM, Yang XH, Qiu JJ, Yang SS, Shen J, Zhang LP, Wang W: Development and evaluation of a questionnaire for measuring suboptimal health status in urban Chinese. J Epidemiol. 2009, 19: 333-341. 10.2188/jea.JE20080086.
Cao H, Sun Y, Wan Y, Hao J, Tao F: Problematic Internet use in Chinese adolescents and its relation to psychosomatic symptoms and life satisfaction. BMC Public Health. 2011, 11: 802-10.1186/1471-2458-11-802.
Li G, Xie F, Yan S, Hu X, Jin B, Wang J, Wu J, Yin D, Xie Q: Subhealth: definition, criteria for diagnosis and potential prevalence in the central region of China. BMC Public Health. 2013, 13: 446-10.1186/1471-2458-13-446.
Tanaka M, Mizuno K, Fukuda S, Shigihara Y, Watanabe Y: Relationships between dietary habits and the prevalence of fatigue in medical students. Nutrition. 2008, 24: 985-989. 10.1016/j.nut.2008.05.003.
Smith A, Bazzoni C, Beale J, Elliott-Smith J, Tiley M: High fibre breakfast cereals reduce fatigue. Appetite. 2001, 37: 249-250. 10.1006/appe.2001.0428.
Smith AP: Breakfast, stress and catching colds. J Fam Health Care. 2003, 13: 2-
Lawton CL, Walton J, Hoyland A, Howarth E, Allan P, Chesters D, Dye L: Short term (14 days) consumption of insoluble wheat bran fibre-containing breakfast cereals improves subjective digestive feelings, general wellbeing and bowel function in a dose dependent manner. Nutrients. 2013, 5: 1436-1455. 10.3390/nu5041436.
Astbury NM, Taylor MA, Macdonald IA: Breakfast consumption affects appetite, energy intake, and the metabolic and endocrine responses to foods consumed later in the day in male habitual breakfast eaters. J Nutr. 2011, 141: 1381-1389. 10.3945/jn.110.128645.
Farshchi HR, Taylor MA, Macdonald IA: Beneficial metabolic effects of regular meal frequency on dietary thermogenesis, insulin sensitivity, and fasting lipid profiles in healthy obese women. Am J Clin Nutr. 2005, 81: 16-24.
Liese AD, Roach AK, Sparks KC, Marquart L, D'Agostino RJ, Mayer-Davis EJ: Whole-grain intake and insulin sensitivity: the insulin resistance atherosclerosis study. Am J Clin Nutr. 2003, 78: 965-971.
Zunhammer M, Eberle H, Eichhammer P, Busch V: Somatic symptoms evoked by exam stress in university students: the role of alexithymia, neuroticism, anxiety and depression. PLoS One. 2013, 8: e84911-10.1371/journal.pone.0084911.
van der Windt DA, Dunn KM, Spies-Dorgelo MN, Mallen CD, Blankenstein AH, Stalman WA: Impact of physical symptoms on perceived health in the community. J Psychosom Res. 2008, 64: 265-274. 10.1016/j.jpsychores.2007.10.003.
Steptoe A, Wardle J, Pollard TM, Canaan L, Davies GJ: Stress, social support and health-related behavior: a study of smoking, alcohol consumption and physical exercise. J Psychosom Res. 1996, 41: 171-180. 10.1016/0022-3999(96)00095-5.
Acknowledgments
We thank our study participants. We also thank administrators of selected units for their contribution to the data collection and case ascertainment. This work was supported by the NSFC-Guangdong joint fund (No. U1132001), National Science Foundation of China (No. 81173146, 8120262281373707 and 81403447), Natural Science Foundation of Guangdong Province, China (No. S2012010009177), Guangdong Provincial Department of Science and Technology and Guangdong Provincial Academy of Traditional Chinese Medicine joint fund (No. 2011B032200004, 2012A032500004 and 2013A032500008), Guangdong Provincial Department of Science and Technology fund (No. 2011B031700018), China Postdoctoral Science Foundation (No. 2014 M552187), and Science & Technical Plan of Guangzhou, Guangdong, China (No. 2011 J4300108). As for the human participant protection, the study was approved by the Ethics Committee of Nanfang Hospital in Guangzhou, China (2012) LunShenZi (No. 035).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
Study concept and design: RL, XZ; acquisition of data: JC, YL, JC, TW, YT, XS, FL, YX, PJ, LW, LX and SW; analysis and interpretation of data: JC, JC and YL; drafting of the manuscript: JC, JC and YL; critical revision of the manuscript for important intellectual content: XZ; study supervision: RL and XZ. All authors were involved in the formulation of the research questions. All authors read and approved the final manuscript.
Electronic supplementary material
12967_2014_348_MOESM1_ESM.docx
Additional file 1: Associations between the self-report symptoms of SHMS V1.0 and breakfast eating. Table S1. Odds of the self-report physiological symptoms of SHMS V1.0 for the risk profile groups of breakfast eating. Table S2. Odds of the self-report physiological symptoms of SHMS V1.0 for the risk profile groups of breakfast eating. Table S3. Odds of the self-report social symptoms of SHMS V1.0 for the risk profile groups of breakfast eating. (DOCX 46 KB)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Chen, J., Cheng, J., Liu, Y. et al. Associations between breakfast eating habits and health-promoting lifestyle, suboptimal health status in Southern China: a population based, cross sectional study. J Transl Med 12, 348 (2014). https://doi.org/10.1186/s12967-014-0348-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12967-014-0348-1