Abstract
Background
Apart from maximizing functional abilities and independence after stroke, improving overall health-related quality of life (HRQoL) should also become part of the stroke treatment and rehabilitation process goals. This study aimed to assess the HRQoL profiles and explore the dimension-specific associated factors of HRQoL among stroke survivors.
Methods
This was a cross-sectional study of stroke survivors attending post-stroke care clinics in three public hospitals in the states of Pahang and Terengganu, Malaysia. The HRQoL was assessed by EuroQol-5 dimension-5 levels. Data on socio-demographic, clinical profiles, malnutrition risk, and physical activity level were collected through an interviewer-administered survey. Descriptive analyses for HRQoL profiles and multiple logistic regression analyses for its associated factors were performed. Crude and adjusted odds ratios were reported.
Results
A total of 366 stroke survivors were recruited with a mean age of 59 ± 11 years. The most -commonly reported health problems were mobility (85%), followed by usual activities (82%), pain/discomfort (63%), anxiety/depression (51%) and self-care (41%). The mean of the EQ visual analogue scale and the median of the EQ5D summary index was reported at 60.3 ± 14.2 and 0.67 ± 0.37, respectively. Malnutrition risk (mobility, usual activities, and self-care), wheelchair users (self-care and usual activities), speech impairment (usual activities and pain/discomfort), number of stroke episodes (self-care and pain/discomfort), body mass index, physical activity level and types of strokes (usual activities), age and use of a proxy (anxiety/depression), working and smoking status (mobility), were factors associated with either single or multiple dimensions of HRQoL.
Conclusion
Routine malnutrition screening, tailored program for speech therapy, prevention of recurrent stroke, and physical activity promotion should be addressed and further reinforced in current rehabilitation interventions to improve the HRQoL among stroke survivors in Malaysia.
Similar content being viewed by others
Introduction
Stroke has a huge negative impact on its survivors, causing permanent functional impairments leading to dependency in daily activities, depressed mood, and social isolation [1]. Consequently, cumulative evidence has consistently demonstrated a lower health-related quality of life (HRQoL) among stroke survivors than those without stroke [2, 3]. Apart from maximizing functional abilities and independence after stroke, improving HRQoL has been gaining importance as part of the stroke treatment and rehabilitation process [4]. HRQoL provides information on a specific dimension of health status (e.g., physical, functional, cognitive, social, and psychological well-being) and evaluation of treatment effectiveness based on the patient’s own perceptive [5].
Findings on HRQoL profiles among stroke survivors have so far been inconsistent. Some studies reported the greatest problems in the psychological domain [6], while others reported in the physical domain [7, 8]. Estimates of HRQoL also varied between studies since socio-economic and cultural differences may have affected the degree of HRQoL. Ultimately, more research regarding HRQoL in different cultures would be meaningful in the generalization of findings.
Besides, it is also important to identify factors associated with HRQoL to make effective management strategies. Previous studies have reported a complex network of physical and psychological factors associated with HRQoL among stroke survivors. These factors included demographic factors (age, female gender, low education level, and poor socio-economic status) and clinical factors (stroke severity, stroke type, recurrent stroke, smoking, comorbidities, functional status/disability, and depression) [9,10,11]. Although limited, more studies have recently explored the role of physical activity and nutritional status on HRQoL [2, 12].
To our best knowledge, there is no study in Malaysia which had explored the role of comprehensive factors on socio-demographic, clinical, and lifestyle practices on HRQoL status among stroke survivors [13, 14]. Moreover, it is essential to identify which aspects of patients have been affected mainly by their stroke condition and modify the factors affecting HRQoL in specific dimensions to maximize their health improvement and treatment. This information is hard to discern if using the summary index of HRQoL alone. Therefore, this study aimed to examine the HRQoL profiles and their dimension-specific influencing factors among stroke survivors attending outpatient settings in Malaysia's public hospitals.
Materials and methods
Setting
A cross-sectional observational study was undertaken between May to August 2019 at post-stroke clinics in the government hospital of Peninsular Malaysia. Based on the statistics of discharge stroke cases in government hospitals in 2015–2016 [15], three hospitals with the highest annual report in the East Coast area of Peninsular Malaysia were selected as the study sites. These hospitals were Hospital Tengku Ampuan Afzan, Hospital Sultan Haji Ahmad Shah, and Hospital Sultanah Nur Zahirah. The study was conducted in the post-stroke care clinics across different departments, including Neurology and Rehabilitation.
Inclusion and exclusion criteria
The inclusion criteria were as follows: 18 years of age or older, diagnosed with ischaemic or haemorrhagic stroke, and able to communicate in Bahasa Malaysia. Stroke survivors suffering from a transient ischaemic attack, traumatic intracranial haemorrhage, subdural haemorrhage, severe organ failures and psychiatric illness were excluded. Stroke survivors with cognitive deficits or language deficits were included if there was a proxy of the respondent, who is his/her primary caregiver at home. It is recognised that proxy-respondents tend to over-report (more pessimistic) patient's health problems than patients themselves, which may lead to bias [16]. However, the use of proxy indirectly increased the response rates. It allowed us to examine the HRQoL among patients with cognitive and communication disabilities, which were often excluded in other surveys. All eligible patients attending the clinics were invited to participate in this study. The main research assistant interviewed all patients during the survey period.
Sample size
Based on single mean formula [17], 95% confidence interval, standard deviation 17 for EQ-visual analogue scale (EQ-VAS) [18], margin error of 2, and attrition rate of 20%, a minimum sample size of 347 was required.
Independent variables and measurements
Data on sociodemographic, clinical, nutritional status and physical activity level were collected. Sociodemographic data included age, sex, marital situation, employment status, household income, and level of education. Clinical history and medical record were examined to collect information on types of strokes, number of stroke episodes, time since stroke, location of stroke, presence of aphasia, number of comorbidities, and wheelchair users in daily life.
Besides, patients were screened for malnutrition risk based on the Malnutrition Risk Screening Tool- Hospital (MRST-H) [19, 20]. Patients who scored two and above were classified as high malnutrition risk. The screening tool included questions on financial dependency, self-feeding ability, unintentional weight loss, and measurements of mid-upper arm circumference and calf circumference. Measurements of body weight and height were conducted to determine the patient's body mass index (BMI). The patient was categorized as obese if his or her BMI more or equal to 27.5 kg/m2 based on cut-off points for the Asian population [21]. Knee height, mid-upper arm circumference and previously validated predictive equations were used to estimate the weight and height of stroke survivors who were unable to stand unassisted [22, 23].
Participants' physical activity level after stroke was assessed by the short Malay version of the International Physical Activity Questionnaire (IPAQ) [24, 25]. IPAQ comprises seven items with four activities domains (vigorous, moderate, walking and sitting). The total metabolic equivalent of task (MET)-minutes per week were calculated. Participants were classified into low (< 600 MET-min/week), moderate (600–2999 MET-min/week), or high physical activity level (≥ 3000 MET-min/week) based on the standard scoring protocol [26].
Dependent variables and measurements
There is no single accepted definition of HRQoL so far. The complexity and diversity of health domains have been reflected by numerous tools available to measure HRQoL, such as the EuroQoL, Short-Form Health Survey, WHOQoL-Bref, and Stroke Specific Quality of Life Scale (SS-QoL). This study used EuroQoL-5 Dimensions- 5 Levels (EQ-5D-5L) considering its availability of validated Malay Version [27], validity in stroke population [28, 29], and limitations of other instruments as reported by previous local study [30]. Besides, the instrument is cognitively undemanding and needs only a few minutes to complete. It consists of two components: the EQ-5D descriptive system and EQ visual analogue scale (EQ-VAS). The ED-5Q-5L description system contains five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The participants were asked to rate their health today based on a five-point scale, indicating increasing severity of problems (1 = no problems, 2 = slight problems, 3 = moderate problems, 4 = severe problems and 5 = extreme problems). The participants were also asked to self-rate "their health today" based on a scale of 0–100 (from worst to best score) using the VAS. Additionally, an EQ-5D summary index was derived by applying a formula attaches values (weights) to each of the levels in each dimension, with reference to the Malaysian EQ-5D-5L value set published by Shafie et al. (2018) [31]. The EQ-5D summary index can be ranged from 0 (representing death) to 1 (representing full health), and with negative values (representing states worse than death). Results were presented by predefined age-groups (< 50; 50–59; 60–69 and ≥ 70) and by sex (male and female).
Statistical analysis
Both descriptive and inferential statistics were used with IBM SPSS version 25.0 for Windows. Frequencies and percentages were determined for categorical variables. Mean, and standard deviation was established for numerical variables. A univariate analysis was conducted to investigate dimension-specific HRQoL in stroke survivors. Each dimension in the EQ-5D was categorized into two groups of outcome variables according to previous studies [2, 32]: (1) having problems (slight, moderate, severe and extreme problems) and (2) no problem at all. Socio-demographic characteristics, clinical profiles, nutritional status and physical activity level (independent variables) were compared using the Chi-square test or Fisher's exact test between those having problems and not having problems. Multiple logistic regression was performed to examine predictors of each dimension by including variables with p-value < 0.25 at the univariable analysis. Besides, variables such as age (continuous), sex, and use of proxy respondents were also included in view of their possible confounding effects. Adjusted odds ratios and 95% confidence interval were reported. The fitness of model for each dimension was checked by classification table, Hosmer–Lemeshow's test, and ROC value. Correlations and multicollinearity between variables were checked. P-values of less than 0.05 was considered significant.
Results
Respondent’s characteristics
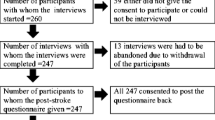
A total of 448 respondents were screened from three hospitals during the survey; however, 30 respondents were excluded based on exclusion criteria, and 20 refused to participate. Hence 398 respondents were recruited. Additionally, 32 of them had an unknown type of stroke (ischaemic or haemorrhagic); thus, only 366 were included in the statistical analysis. There were no missing data in this survey since face-to-face interview was employed and the researcher checked the completeness of the questionnaire before ending each survey. The respondents' socio-demographic background, clinical profiles, nutritional status and physical activity level data are shown in Table 1. Our stroke survivors were predominantly aged more than 60 years old, male, married, completed secondary education level, not working, and earning a household income of less than Malaysian Ringgit (MYR) 3000/ United States Dollar 719. The majority of them had underlying hypertension and dyslipidaemia, while half of them had diabetes mellitus. Most of the patients were first-time stroke survivors, while 20% were recurrent stroke survivors. Almost three quarters (72%) of the survey was completed by the stroke survivors, while the rest (28%) was completed by a proxy of the respondent.
Descriptive analyses of EQ-5D profiles, EQ-VAS and EQ5D index
Table 2 shows the distribution of the problem status of each dimension in the EQ-5D questionnaire. Almost all stroke survivors (98%) reported having problems in either one or multiple dimensions of HRQoL. Our stroke survivors commonly reported having problems (slight to extreme problems) in the dimension of mobility (85%), followed by usual activities (82%), pain/discomfort (63%), anxiety/depression (51%) and self-care (41%). On the other hand, Table 3 displays the mean values of the VAS and median values of EQ5D index stratified by age group and sex. The mean of EQ-VAS and median of EQ5D index was reported at 60.3 ± 14.2 and 0.67 ± 0.37, respectively. There were no significant differences between males and females in both means of EQ-VAS (p = 0.739) and median of EQ5D-index (p = 0.286). The mean of VAS (64–70) and median of EQ5D-index (0.68–0.70) were highest in the < 50 age group for both female and male patients, and they seemed to reduce gradually with increasing age.
Associations between socio-demographic, clinical profiles, nutritional status, and physical activity level with specific dimension of HRQoL at univariate analysis
Table 4 shows the associations between socio-demographic, clinical profiles, nutrition status, and physical activity level with a specific dimension of HRQoL at univariate analysis. Factors found to be significantly associated with the physical dimensions of HRQoL (mobility, usual activities, and self-care) were working status, household income, number of stroke episodes, obesity, smoking status, aphasia, wheelchair user, malnutrition risk, physical activity level and use of a proxy respondent. Conversely, younger age, malnutrition risk, use of a proxy respondent and wheelchair user were significantly associated with the psychological dimensions of HRQoL (pain/discomfort and anxiety/depression). Sex, marital status, education levels, number of comorbidities, types of strokes, and time since stroke were not significantly associated with any dimension of HRQoL at univariate analysis.
Dimension-specific associated factors of EQ-5D-5L
Table 5 shows the dimension-specific associated factors of EQ-5D-5L using multivariable logistic regression after adjusted for confounding variables. This study revealed that high malnutrition risk patients were two to three times more likely to report having problems in all physical dimensions of HRQoL namely mobility, self-care and usual activities. Similarly, wheelchair-bound stroke survivors were 14 to 34 times higher risk of having problems in self-care and usual activities dimensions than their counterparts. Besides, stroke survivors with recurrent stroke were twice more likely to report problems in self-care and pain/discomfort. Stroke survivors with aphasia were at higher odds of reporting problems in the usual activities yet lower odds of reporting problems in pain/discomfort. Haemorrhagic stroke and low physical activity levels were significantly associated with higher odds of having problems in usual activities. Unemployment and use of a proxy respondent were found to be associated with higher odds of having problems in mobility and anxiety/depression dimension, respectively. Conversely, older age, obesity, and active smoking was associated with lower odds of having problems in anxiety/depression, usual activities, and mobility dimension, respectively.
Discussion
This study showed that stroke survivors reported having problems in different dimensions of HRQoL, with the highest frequency reported in the mobility dimension and the lowest in the self-care dimension. High malnutrition risk, wheelchair users, presence of aphasia, recurrent stroke, low physical activity level, haemorrhagic stroke, and unemployment were associated with higher odds of having problems in the physical dimensions of HRQoL (mobility, usual activities, and self-care). Conversely, obesity and active smoking were associated with lower odds of having problems in the physical dimensions of HRQoL. The presence of aphasia, recurrent stroke, younger age, and proxy use was significantly associated with the psychological dimensions of the HRQoL (pain/discomfort and anxiety/depression).
The overall HRQoL as reported using VAS and summary of EQ5D-index was 60 and 0.67, respectively. Although there is no specific classification of VAS according to the EQ-5D manual, the reported value of 60 indicating average or moderate health status. This finding was consistent with previous studies in Korea (61) [33], yet lower than that reported in Sweden and Malaysia (70–71) [18, 34], and higher than that reported in Spain (50) [35]. Additionally, the summary of EQ5D-index (0.67) obtained in this study was in line with findings in France (0.63) [36] and US (0.69) [37], but lower than those in Norway (0.74) [9] and Singapore (0.83) [38].
In general, more than half of our stroke survivors reported having problems in almost all dimensions of HRQoL, indicating poor health status from the patient's perspective. The sequence of the most reported health problem by stroke survivors in this study (mobility, usual activities, pain/discomfort, anxiety/depression, and self-care) was not so different from findings from a previous study in Australia (usual activities 58%, mobility 57%, pain/discomfort 49%, anxiety/depression 47%, and self-care 33%) [7]. Of the five domains, mobility and usual activities domains were the most reported problems. The high prevalence is probably because most of the respondents were recruited from the rehabilitation centre, where many suffered from specific limb weaknesses that require rehabilitation services. Almost 30 percent of the stroke survivors were wheelchair users, while others complained of gait, balance and fatigue issues while walking. Walking impairment often have a negative impact on activities of daily living and social participation [39]. The usual activity domain includes working, housework, family or leisure activities, which requires an ability to move around. Besides, a previous local study showed that almost one-fifth of the stroke survivors discharged from rehabilitation clinics of the hospital demonstrated unfavourable scores for mobility and activities of daily living (ADL) [14].
In this study, high malnutrition risk was significantly associated with higher odds of having problems in all physical dimensions of HRQoL. This is in line with a prospective study in Germany, which found a significant negative association between malnutrition risk and EQ-5D index at one year after stroke survivors ward discharge [12]. Studies on the relationship between malnutrition risk and HRQoL among stroke population were relatively limited [12, 40], although evidence exists to indicate higher malnutrition risk and lower HRQoL among the elderly population [41, 42]. However, it remains unclear whether malnutrition was the cause or the consequence or if the association was through mediators [43]. Malnutrition contributed to the development of sarcopenia with loss of lean body mass and muscle function [44]. Consequently, it decreases the physical functioning of stroke survivors, especially in mobility, self-care and usual activities. Second, negative emotions and depression might affect food intake [45], which might interact with the nutritional status [43]. Given the high prevalence of malnutrition risk and its significance with HRQoL, it is important to monitor the stroke survivor's nutritional status routinely even after discharge from the ward. Prompt and optimal nutritional strategies should be taken to prevent further deterioration of nutritional status among these high malnutrition risk groups.
On the other hand, stroke survivors with aphasia or language deficits were at higher risk of having problems in the self-care dimension, yet at lower risk of having pain/discomfort problem. This is similar to the finding by other studies that reported a significant negative impact of aphasia on HRQoL among stroke survivors [3, 46]. Stroke survivors with aphasia faced significant difficulties in participating in complex social activities such as work, family and leisure activities that involve other people [46]. Moreover, the presence of speech and language difficulties may hinder effective communication about self-care needs, food preferences and expression of pain and discomfort [47]. As a result, stroke survivors with aphasia may not obtain the appropriate care and treatment they need from the caregiver or healthcare members.
Interestingly, this study found that obese stroke survivors were less likely to report problems in the usual activities dimension. The relationship between BMI and HRQoL have been inconclusive, with some studies reporting no significant associations [12, 33]. Conversely, recent observational studies have suggested that overweight or obese patients had better survival rates, functional outcomes, and less stroke recurrence than those normal or underweight [48, 49]. However, these studies were subjected to several methodological limitations due to their observational study design, selection bias, survival bias, BMI limitation in indicating obesity, and inaccurate body weight measurement [49]. The relationship between obesity and better functional status should be interpreted in caution as it may be subjected to collider bias or driven by malnutrition among some individuals in the non-obese group. Moreover, body composition changes were more prominent in stroke survivors than in healthy individuals [50]. Significantly lower bone mineral content and lean mass was found in the stroke survivors (but was unlikely to be captured by BMI alone) as compared with their counterparts of similar age, regardless of the presence of limb paralysis [50]. This warrants future prospective studies to explore the impact of changes in BMI, body composition and malnutrition risk on stroke survivors’ functional outcomes.
Low physical activity level was significantly associated with all three physical dimensions of HRQoL, which are aligned with results from a previous study in Korea [2]. However, its effect remained significant only in the usual activities dimension after adjusting for other variables. The causal relationship between physical activity and HRQoL is not known. Poor HRQoL probably leads to low physical activity and the relationship may be confounded by stroke severity. Conversely, increased physical activity was associated with better post-stroke HRQoL [51, 52]. The benefits of physical activity on physical and mental health have been shown, such as improved motor ability and fitness levels, improved emotional wellbeing and reduced depression level [53]. Therefore, more efforts are needed to increase further patient's participation in physical activity and exercise along with the conventional rehabilitation treatment.
Furthermore, stroke survivors who ambulate using wheelchair were more likely to have problems in the physical dimensions of HRQoL such as self-care and usual activities. Similarly, those who suffered from recurrent stroke were more likely to have pain/discomfort and self-care problems. Recurrent stroke is common among stroke survivors (20%), and it is often more severe and disabling than the first episode [54]. We observed that 40% of the recurrent stroke survivors were ambulating using a wheelchair, and 16% of them required tube feeding and were thus more likely to have self-care problems. Additionally, pain and discomfort observed among recurrent stroke cases was probably associated with shoulder pain, central post-stroke pain, pain from spasticity or muscle stiffness, and discomfort from tube feeding [55]. Therefore, apart from optimizing the stroke rehabilitation process, future stroke prevention strategies must be implemented to enhance HRQoL among stroke survivors.
On the other hand, smoking was associated with lower odds of having problems in the mobility dimension. In other words, persistent smoking was more commonly observed in those without mobility issues or who have better functional status as observed by other studies [56, 57]. Financial constraints, mobility impairment and lack of social gathering might have restricted patients’ access to cigarettes supply since many were dependent on others for income sources or were having walking impairment during the survey. Persistent smoking in stroke survivors was undesirable since smoking has been associated with increased risk of future cardiovascular and death events as well as poorer functional outcomes [58, 59]. Thus, more intensive strategies should be implemented to assist in smoking cessation among persistent smokers.
Other significant factors associated with HRQoL were non-modifiable factors such as age (anxiety/depression), unemployment (mobility), haemorrhagic stroke (usual activities), and use of proxy (anxiety/depression), with each affecting different dimension of HRQoL respectively. We found that anxiety/depression was more commonly found in younger stroke survivors. The mean age of stroke onset in this study was 57, which was 15 years younger than those in developed countries (72 years old) [60]. Moreover, 18% of the stroke survivors were young stroke with stroke onset at less than 50 years old. Stroke is a disastrous disease, and it can bring a sudden change in life events and a decline in health status both physically and psychologically. It is also associated with heavier financial burden through loss of patient’s job, cost of nursing care and medical bills [61], especially for those still in the working age. Consequently, it may induce stress and anxiety among these young stroke survivors.
This study also showed that stroke survivors who were not working during the survey were more likely to have mobility issues. Among these stroke survivors who were not working, 23% of them were unemployed (< 60 years), 42% were retirees, and 27% were housewives. Ability to walk with good balance and walking speed greatly affected stroke survivor’s ability to return to work, particularly among the young stroke survivors [62, 63]. Additionally, we also observed that some stroke survivors had early retirement due to significant physical impairments.
The use of a proxy was associated with higher odds of having problem in the anxiety/depression dimension as compared to that of self-reporter. A considerable proportion of stroke survivors cannot self-report because of cognitive, communication, and disability problems. Dorman et al. (1997) have shown moderate agreement between responses from patients and those from their proxies for the physical domains, but less good for the more subjective domains [64]. In fact, some studies demonstrated that proxy bias is most significant in the psychological dimension of HRQoL. Thus, proxy responses may not be suitable for the anxiety dimension [65, 66]. Therefore, results in the measurement of psychological dimension of HRQoL need to be interpreted with caution when there is a considerable amount of proxy respondents in a survey.
Notably, this study did not find any association between sex and HRQoL. The influence of sex on the HRQoL of stroke survivors have remained inconsistent, with some studies reported lower EQ-5D scores among females [11, 67], while others showed no associations [38, 68].
Limitations
This study has several limitations. First, this finding's generalisability is limited because they were based on an observational cross-sectional study design. Second, variables on the severity of stroke (as indicated by the National Institutes of Health Stroke Scale) and degree of disability (as indicated by the Modified Rankin Scale) were not examined in this study. Variables on NIHSS and MRS were either largely missing or required a manual search in the patient’s record, which requires more time and human resources. Despite these limitations, this is probably among the first few multi-centred studies investigating the association between widely varied variables (socio-demographics, clinical profiles, nutritional status, and physical activity) with each dimension of HRQoL among stroke survivors using the EQ-5D-5L instrument. Therefore, we believe that it may shed some light on the causes of poor HRQoL after stroke.
Conclusion
In summary, high malnutrition risk, aphasia, low physical activity, wheelchair user, obesity, younger age, unemployment, recurrent stroke, haemorrhagic stroke, smoking, and use of a proxy respondent were significantly associated with different dimensions HRQoL among stroke survivors. Routine malnutrition screening, tailored program for speech therapy, prevention of recurrent stroke, and physical activity promotion should be addressed and further reinforced in current rehabilitation interventions to improve the HRQoL among stroke survivors in Malaysia.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, but restrictions apply to the availability of these data and are not publicly available.
Abbreviations
- BMI:
-
Body mass index
- EQ-5D-5L:
-
EuroQoL-5 Dimensions- 5 Levels
- EQ-VAS:
-
EQ-visual analogue scale
- HRQoL:
-
Health-related quality of life
- IPAQ:
-
International Physical Activity Questionnaire
- MET:
-
Metabolic equivalent of task
- MRST-H:
-
Malnutrition Risk Screening Tool-Hospital
- MYR:
-
Malaysian Ringgit
- ROC:
-
Receiver operating characteristic
References
De Wit L, Theuns P, Dejaeger E, et al. Long-term impact of stroke on patients’ health-related quality of life. Disabil Rehabil. 2017;39:1435–40.
Kwon S, Park J-H, Kim W-S, et al. Health-related quality of life and related factors in stroke survivors: data from Korea National Health and Nutrition Examination Survey (KNHANES) 2008 to 2014. PLoS ONE. 2018;13:e0195713–e0195713.
Min KB, Min JY. Health-related quality of life is associated with stroke deficits in older adults. Age Ageing. 2015;44:700–4.
Sonrası İ, Kalitesi Y, Birtane M et al. Quality of life after stroke. Trak Univ Tip Fak Derg; 27.
Carod-Artal FJ. Determining quality of life in stroke survivors. Expert Rev Pharmacoecon Outcomes Res. 2012;12:199–211.
Lopez Espuela F, Portilla Cuenca JC, Leno Diaz C, et al. Sex differences in long-term quality of life after stroke: influence of mood and functional status. Neurologia. 2020;35:470–8. https://doi.org/10.1016/j.nrl.2017.10.002.
Thayabaranathan T, Andrew NE, Kilkenny MF, et al. Factors influencing self-reported anxiety or depression following stroke or TIA using linked registry and hospital data. Qual Life Res. 2018;27:3145–55.
Visser MM, Heijenbrok-Kal MH, Spijker AV, et al. Coping, problem solving, depression, and health-related quality of life in patients receiving outpatient stroke rehabilitation. Arch Phys Med Rehabil. 2015;96:1492–8.
Naess H, Lunde L, Brogger J. The effects of fatigue, pain, and depression on quality of life in ischemic stroke patients: the Bergen Stroke Study. Vasc Heal Risk Manag. 2012;8:407–13.
Ramos-Lima MJM, Brasileiro I de C, Lima TL de, et al. Quality of life after stroke: impact of clinical and sociodemographic factors. Clinics (Sao Paulo) 2018; 73: e418–e418.
Phan HT, Blizzard CL, Reeves MJ, et al. Sex differences in long-term quality of life among survivors after stroke in the INSTRUCT. Stroke. 2019;50:2299–306.
Katona M, Schmidt R, Schupp W, et al. Predictors of health-related quality of life in stroke patients after neurological inpatient rehabilitation: a prospective study. Heal Qual Life Outcomes. 2015;13:58.
Wan-Fei K, Syed Hassan ST, Munn Sann L, et al. Depression, anxiety and quality of life in stroke survivors and their family caregivers: a pilot study using an actor/partner interdependence model. Electron Phys. 2017;9:4924–33. https://doi.org/10.19082/4924.
Nor Azlin M, Saperi S, Syed Mohamed A, et al. Functional limitation and health-related quality of life, and associated factors among long term stroke survivors in a Malaysian community. Med J Malaysia. 2016;71:313–21.
Health Informatics Centre Ministry of Health Malaysia. Statistics of discharge stroke cases in government hospitals in 2015–2016. 2018.
Pickard AS, Johnson JA, Feeny DH, et al. Agreement between patient and proxy assessments of health-related quality of life after stroke using the EQ-5D and Health Utilities Index. Stroke. 2004;35:607–12. https://doi.org/10.1161/01.STR.0000110984.91157.BD.
Naing NN. Determination of sample size. Malays J Med Sci. 2003;10:84–6.
Nor Azlin M, Saperi S, Syed Mohamed A, et al. Function and quality of life following stroke rehabilitation: have our stroke patients gained optimum recovery? BMC Public Health. 2012;12:A7.
Sakinah H, Suzana S, Noor Aini MY, et al. Development of a local malnutrition risk screening tool-hospital (MRST-H) for hospitalised elderly patients. Malays J Nutr. 2012;18:137–47.
Tan SL, Sakinah H, Hasmah A, et al. Re-evaluation of Malnutrition Risk Screening Tool-Hospital (MRST-H) for geriatric patients: a multicentre study in peninsular Malaysia. Sains Malaysiana. 2016;45:1311–7.
International Diabetes Institute, World Health Organization, International Association for the Study of Obesity and the International Obesity Task Force. In: The Asia-Pacific perspective: redefining obesity and its treatment. Geneva: Sydney: Health Communications Australia, 0-9577082-1-1 (2000). Accessed 15 Nov 2019.
Shahar S, Pooy NS. Predictive equations for estimation of stature in Malaysian elderly people. Asia Pac J Clin Nutr. 2003;12:80–4.
Database TI co. PA. The Ross Knee Height Caliper. 2019, https://priorart.ip.com/IPCOM/000006911 (2002).
Chu AH, Moy FM. Reliability and validity of the Malay International Physical Activity Questionnaire (IPAQ-M) among a Malay population in Malaysia. Asia Pac J Public Heal. 2015;27:NP2381–9.
Ersöz Hüseyinsinoğlu B, Kuran Aslan G, Tarakci D, et al. Physical activity level of ambulatory stroke patients: is it related to neuropsychological factors? Noro Psikiyatr Ars. 2017;54:155–61.
IPAQ Research Committee. Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ)—short and long forms. IPAQ Research Committee, http://www.ipaq.ki.se/scoring.htm (2005). Accessed 20 Nov 2019.
Shafie AA, Vasan Thakumar A, Lim CJ, et al. Psychometric performance assessment of Malay and Malaysian English version of EQ-5D-5L in the Malaysian population. Qual Life Res. 2019;28:153–62.
Hunger M, Sabariego C, Stollenwerk B, et al. Validity, reliability and responsiveness of the EQ-5D in German stroke patients undergoing rehabilitation. Qual Life Res. 2012;21:1205–16.
Pinto EB, Maso I, Vilela RNR, et al. Validation of the EuroQol quality of life questionnaire on stroke victims. Arq Neuropsiquiatr. 2011;69:320–3.
Samsiah M, Das S, Chee SY, et al. The ideal measurement of the quality of life in post stroke patients: an urban study. Clin Ter. 2011;162:209–15.
Shafie AA, Vasan Thakumar A, Lim CJ, et al. EQ-5D-5L valuation for the Malaysian population. Pharmacoeconomics. 2019;37:715–25. https://doi.org/10.1007/s40273-018-0758-7.
Kim Y, Kim MC, Park H-SS, et al. Association of the anxiety/depression with nutrition intake in stroke patients. Clin Nutr Res. 2018;7:11–20.
Jeon NE, Kwon KM, Kim YH, et al. The factors associated with health-related quality of life in stroke survivors age 40 and older. Ann Rehabil Med. 2017;41:743–52.
Algurén B, Fridlund B, Cieza A, et al. Factors associated with health-related quality of life after stroke: a 1-year prospective cohort study. Neurorehabil Neural Repair. 2011;26:266–74.
Ramírez-Moreno J, Muñoz-Vega P, Alberca S, et al. Health-related quality of life and fatigue after transient Ischemic attack and minor stroke. J Stroke Cerebrovasc Dis. 2018;28:276–84. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.09.046.
Broussy S, Saillour-Glenisson F, García-Lorenzo B, et al. Sequelae and quality of life in patients living at home 1 year after a stroke managed in stroke units. Front Neurol. 2019. https://doi.org/10.3389/fneur.2019.00907.
Xie J, Wu EQ, Zheng ZJ, et al. Impact of stroke on health-related quality of life in the noninstitutionalized population in the United States. Stroke. 2006;37:2567–72.
Yeoh YS, Koh GC, Tan CS, et al. Can acute clinical outcomes predict health-related quality of life after stroke: a one-year prospective study of stroke survivors. Health Qual Life Outcomes. 2018;16:221.
Singam A, Ytterberg C, Tham K, et al. Participation in complex and social everyday activities six years after stroke: predictors for return to pre-stroke level. PLoS ONE. 2015;10:e0144344.
Lin SC, Lin KH, Lee YC, et al. Test-retest reliability of the Mini Nutritional Assessment and its relationship with quality of life in patients with stroke. PLoS ONE. 2019;14:e0218749.
Hernandez-Galiot A, Goni I. Quality of life and risk of malnutrition in a home-dwelling population over 75 years old. Nutrition. 2017;35:81–6.
Kvamme J-M, Olsen JA, Florholmen J, et al. Risk of malnutrition and health-related quality of life in community-living elderly men and women: the Tromsø study. Qual Life Res. 2011;20:575–82.
Ghimire S, Baral BK, Pokhrel BR, et al. Depression, malnutrition, and health-related quality of life among Nepali older patients. BMC Geriatr. 2018;18:191.
Sieber CC. Malnutrition and sarcopenia. Aging Clin Exp Res. 2019;31:793–8.
Paquet C, St-Arnaud-McKenzie D, Kergoat MJ, et al. Direct and indirect effects of everyday emotions on food intake of elderly patients in institutions. J Gerontol Ser A Biol Sci Med Sci. 2003;58:M153–8. https://doi.org/10.1093/gerona/58.2.m153.
Spaccavento S, Craca A, Del Prete M, et al. Quality of life measurement and outcome in aphasia. Neuropsychiatr Dis Treat. 2014;10:27–37.
Bouziana S, Tziomalos K. Malnutrition in patients with acute stroke. J Nutr Metab. 2011;2011:167898.
Burke DT, Al-Adawi S, Bell RB, et al. Effect of body mass index on stroke rehabilitation. Arch Phys Med Rehabil. 2014;95:1055–9.
Oesch L, Tatlisumak T, Arnold M, et al. Obesity paradox in stroke—myth or reality? A systematic review. PLoS ONE. 2017;12:e0171334.
Chang KV, Wu WT, Huang KC, et al. Segmental body composition transitions in stroke patients: trunks are different from extremities and strokes are as important as hemiparesis. Clin Nutr. 2020;39:1968–73. https://doi.org/10.1016/j.clnu.2019.08.024.
Nayak P, Kumaran SD, Babu AS, et al. Levels of physical activity and quality of life among community-dwelling adults with stroke in a developing country. Eur J Physiother. 2019;23:165–70.
Pinheiro M. Chronic hemiparetic subjects with higher physical activity levels report better quality of life. Rev Neurociências. 2014;22:221–6.
Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005;18:189–93.
Modrego PJ, Pina MA, Mar Fraj M, et al. Type, causes, and prognosis of stroke recurrence in the province of Teruel, Spain. A 5-year analysis. Neurol Sci. 2000. https://doi.org/10.1007/s100720070050.
Delpont B, Blanc C, Osseby GV, et al. Pain after stroke: a review. Revue Neurologique. 2018. https://doi.org/10.1016/j.neurol.2017.11.011.
McCarthy MJ, Huguet N, Newsom JT, et al. Predictors of smoking patterns after first stroke. Soc Work Health Care. 2013. https://doi.org/10.1080/00981389.2012.745460.
Sienkiewicz-Jarosz H, Zatorski P, Baranowska A, et al. Predictors of smoking abstinence after first-ever ischemic stroke: a 3-month follow-up. Stroke. 2009. https://doi.org/10.1161/STROKEAHA.108.542191.
Kim J, Gall SL, Dewey HM, et al. Baseline smoking status and the long-term risk of death or nonfatal vascular event in people with stroke a 10-year survival analysis. Stroke. 2012. https://doi.org/10.1161/STROKEAHA.112.668905.
Matsuo R, Ago T, Kiyuna F, et al. Smoking status and functional outcomes after acute ischemic stroke. Stroke. 2020. https://doi.org/10.1161/STROKEAHA.119.027230.
Abdul Aziz Z, Lee YYL, Ngah BA, et al. Acute Stroke Registry Malaysia, 2010–2014: results from the National Neurology Registry. J Stroke Cerebrovasc Dis. 2015;24:2701–9.
Kwok T, Lo RS, Wong E, et al. Quality of life of stroke survivors: a 1-year follow-up study. Arch Phys Med Rehabil. 2006;87:1177–82 (quiz 1287).
Jarvis HL, Brown SJ, Price M, et al. Return to employment after stroke in young adults: how important is the speed and energy cost of walking? Stroke. 2019;50:3198–204. https://doi.org/10.1161/STROKEAHA.119.025614.
Ntsiea MV, van Aswegen H, Lord S. Stroke survivors’ and employers’ perceived barriers and enablers of return to work after stroke. Physiotherapy. 2015;101:e1108. https://doi.org/10.1016/j.physio.2015.03.2006.
Dorman PJ, Waddell F, Slattery J, et al. Is the EuroQol a valid measure of health-related quality of life after stroke? Stroke. 1997;28:1876–82.
Pickard AS, Lin HW, Knight SL, et al. Proxy assessment of health-related quality of life in African American and white respondents with prostate cancer perspective matters. Med Care. 2009;47:176–83. https://doi.org/10.1097/MLR.0b013e31818475f4.
Sneeuw KCA, Aaronson NK, Sprangers MAG, et al. Comparison of patient and proxy EORTC QLQ-C30 ratings in assessing the quality of life of cancer patients. J Clin Epidemiol. 1998;51:617–31. https://doi.org/10.1016/S0895-4356(98)00040-7.
Bushnell CD, Reeves MJ, Zhao X, et al. Sex differences in quality of life after ischemic stroke. Neurology. 2014;82:922–31.
Sallinen H, Sairanen T, Strbian D. Quality of life and depression 3 months after intracerebral hemorrhage. Brain Behav. 2019;9:e01270.
Acknowledgements
The authors would like to thank the Director-General of Health Malaysia for the permission to publish this article. The authors are thankful to all participating hospitals, healthcare members, site investigators, stroke survivors and their caregivers for facilitating data collection.
Funding
This study received no grant from any funding agency.
Author information
Authors and Affiliations
Contributions
All authors involved in the conception and design of the study. HJW acquired the data. HJW, SH, and PLL analysed and interpreted the data. HJW drafted the article. SH, PLL and KAI substantively revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Medical Research and Ethics Committee [NMRR-18-3237-42977(IIR)] and Universiti Sultan Zainal Abidin Human Research Ethics Committee [UniSZA/UHREC/2019/102] had approved the study. The patient or his/her proxy provided written informed consent before enrolled on the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wong, H.J., Lua, P.L., Harith, S. et al. Health-related quality of life profiles and their dimension-specific associated factors among Malaysian stroke survivors: a cross sectional study. Health Qual Life Outcomes 19, 210 (2021). https://doi.org/10.1186/s12955-021-01847-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-021-01847-0