Abstract
Background
Prevalence of hepatitis C virus (HCV) infection among people who inject drugs (PWID) in Iran is high. Since 2005, the Iranian government has implemented a harm reduction program to control HCV. We aimed to describe the prevalence of HCV antibody (Ab) in Iranian PWID before and after the implementation of harm reduction with cumulative meta-analysis.
Methods
Following PRISMA guidelines, we conducted a systematic review and meta-analysis of studies published on the seroprevalence of HCV among PWID. We systematically reviewed the literature to identify eligible studies up to December 2018 in international and national databases. Pooled prevalence and 95% confidence intervals were calculated using Der Simonian and Laird method, taking into account conceptual heterogeneity. Subgroup analyses were performed by harm reduction implementation and studies’ characteristics to assess the sources of heterogeneity. We used Cochran–Armitage test for the linear trend of the prevalence of HCV Ab among PWID.
Results
We reviewed 5966 papers and reports and extracted data from 62 eligible records. The pooled HCV Ab prevalence among PWID in Iran was 46.5% (95% confidence interval [95% CI] 41.1–52.0%). Overall, the Cochran–Armitage test for trend indicated a significant decreasing trend of HCV Ab prevalence (P = 0.04). The cumulative meta-analysis showed a slight decline in the prevalence of HCV Ab between the years 2005 and 2018.
Conclusions
The HCV Ab prevalence among PWID in Iran is high, with a considerable geographical variation. The prevalence of HCV Ab among PWID in Iran slightly decreased after 2005 which could be, at least to some extent, related to the implementation of extensive harm reduction programs in the country.
Similar content being viewed by others
Introduction
Hepatitis C virus (HCV) infection is the main global health concern. The global prevalence of viraemic HCV infection is estimated to be 1% in 2015, corresponding to 71.1 million (62.5–79.4) viraemic infections [1]. Evidence shows the incidence of three to four million people each year, and millions of people with chronic infection are at risk of developing cirrhosis and liver cancer [2]. HCV is transmitted widely through injection of the drug; however, unsafe medical injections were the predominant route of transmission in developing countries [3]. No effective HCV vaccine is yet available. Therefore, public health interventions are the only means of preventing HCV, especially in high-risk populations. People who inject drugs (PWID) are particularly at risk for contracting HCV and other blood-borne diseases, including those caused by human immunodeficiency virus (HIV) and hepatitis B virus (HBV) [4,5,6]. Opioid substances are associated with the highest drug-related burden [7, 8]. Injecting drug use has also expanded in the world in the last decades, and it is estimated that 15.6 million people inject drugs worldwide [9]. According to a Harm Reduction International report in 2013 and other sources, it is estimated that there are 170,000 to 230,000 PWID in Iran [10,11,12,13]. Opium has traditionally been used in Iran, but rapid changes in drug use patterns have occurred in recent decades, leading to an increased number of PWID [14, 15]. Iran has one of the highest numbers of people who use drugs (PWUD); many of them have a history of drug injection [14,15,16]. In Iran, a history of drug use, especially drug injection, is the main risk for transmission of HCV [17, 18]. World Health Organization has set a goal for the elimination of HCV by 2030 which needs continuous harm reduction for containment of HCV epidemics accompanied by “test and treat” initiatives in the target populations such as PWID (HCV micro-elimination) in Iran [19, 20]. More specifically, the prevalence of HCV antibody (Ab) among PWID in Iran has been reported 40–75%, depending on the study location [21]. A systematic review of PWID between 2000 and 2016 showed that the prevalence of HCV Ab in PWID in Iran was 42% (95% CI 33–52%) [22].
In Iran, during the end of 1990s and early 2000s, drug injection was common and general knowledge of PWUD on blood-borne infections was low [23, 24]. In 2002, Iran implemented a harm reduction program including opioid substitution treatment (OST), needle and syringe programs (NSP), outreach, and prison-based programs, primarily in response to the HIV epidemics among PWID [25]. These programs included education, OST by methadone and buprenorphine, and ensuring access to sterile syringes and needles, as well as condoms [25]. The need for a harm reduction program originated in a survey of 900 street drug users which found that the HIV prevalence was 25% among PWID [26]. These programs have been scaled up at the national level of Iran and assigned as an official policy since 2005 [25, 27]. The Iranian Ministry of Health reported that in 2007, 654 centers provided methadone maintenance therapy (MMT) and buprenorphine maintenance therapy (BMT) to 20,000 and 2,000 opioid dependents, respectively. In prisons, 11,000 prisoners were receiving MMT [28]. According to the report of the Ministry of Health, in the year 2011, thousands of methadone clinics, mainly in the private sector, were providing OST and about 500,000 PWUD were receiving OST. Moreover, tens of thousands of prisoners were receiving MMT [29]. About the needle and syringe program, in 2007, a total of 120 drop-in-centers (DICs) and 150 outreach teams distributed 1,400,000 needles and syringes [28]. In mid-2011, hundreds of sites were providing needles and syringes, as well as condoms, and in 1 year, millions of syringes were distributed [30,31,32]. Although there is sufficient evidence on the effectiveness of NSP and OST in the reduction in self-reported injecting risky behavior [32,33,34], evidence regarding the effectiveness of these programs in the containment of HCV epidemics is inadequate in Iran [32, 33].
Previously, a systematic review had been conducted on the HCV prevalence among PWID in Iran, and the included studies were conducted from 2000 through 2016 [22]. The current systematic review was conducted to: (1) provide an updated estimate of the HCV Ab prevalence among PWID in Iran; (2) estimate the HCV Ab prevalence in study settings and geographical locations; (3) analyze the trend of HCV Ab prevalence over time; and 4) compare the HCV Ab prevalence before and after the implementation of harm reduction program in Iran.
Methods
An extensive and comprehensive search was done in the international (PubMed, ISI Web of Science, Scopus, Embase), regional (IMEMR), and national (Barakat Knowledge Network System) databases in December 2018. To access studies not yet published by that date, expert authors in this field were contacted. Moreover, the reference lists of the studies included in the final analysis as well as previous systematic reviews conducted in Iran were reviewed [22, 35]. In this review, PWID was defined as people who have injected illicit drugs at least once during the past 12 months. The methods used were following the PRISMA [36] and GATHER guideline [37] (Checklist presented in Appendix 1). The protocol was registered in PROSPERO (CRD42018104303).
Search strategy
A broad search was conducted using the MeSH terms and text words (and their combinations and truncated synonyms) of geographical location (i.e., country and province names) and HCV in electronic data sources including PubMed, EMBASE, Education Resource Information Center, MEDLINE, MEDLINE in process, PsycINFO, Scopus, and Web of Science, Iranmedex, Google Scholar, Iranian Data Bank of Hepatitis Research, Scientific Information Database (SID), Magiran, and the Iran Blood Transfusion Journal. In our search strategy, we did not apply any limitations in the time of publication and language. Iranian databases were searched using the related keywords and the Persian equivalents of HCV, considering all possible combinations. We reviewed the titles and abstracts to select potentially relevant papers. If there was doubt about the suitability of the paper based on the abstract, the full text was reviewed. We manually searched the references and relevant articles for inclusion. We also looked at the electronic abstract list of congresses conducted in Iran and also at the electronic database of students’ thesis through universities’ electronic libraries and Web sites. Furthermore, we searched and identified studies that were not captured by our database by reviewing the previously published meta-analyses and the reference lists in retrieved articles [22, 35, 38]. The search strategy is presented in Appendix 2.
Study selection
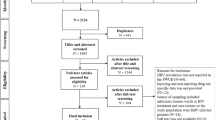
All records identified through our search were imported into an EndNote library where duplicate publications were identified and excluded (Fig. 1). Similar to our previous systematic reviews [39], the remaining unique reports underwent two stages of screening, performed by AR and HSH. The titles and abstracts were first screened, and those deemed relevant or potentially relevant underwent further screening, in which the full texts were retrieved and assessed for eligibility, based on our inclusion and exclusion criteria. Eligible reports were included in this study, while the remaining ineligible reports were excluded for reasons indicated in Fig. 1. The references of all full-text articles and literature reviews were also screened for further potentially relevant reports.
Eligibility criteria
The objective of screening was to identify the scientific documents with epidemiological evidence on the prevalence and/or incidence of HCV Ab among PWID. The following five eligibility criteria were used in the selection of relevant studies: document type, study design, disease area, geographical setting, and population.
Concerning the document type, all scientific documents reporting original data (i.e., gathered directly by conducting surveys and laboratory tests on specimens), in the form of a peer-reviewed manuscript, progress report, abstract, technical report, or substantive scientific commentary, were included. Documents not reporting epidemiological data (e.g., legal cases, legislation) and those not reporting original data (e.g., data simulation), as well as documents lacking scientific and methodological details needed for the assessment of the validity of findings (e.g., media reports), were excluded. Documents that were self-described as “systematic reviews” or “meta-analyses” (scientific documents such as peer-reviewed manuscripts or abstracts summarizing results from a group of epidemiological studies) were retained for hand searching of the references. All study designs reporting data on the prevalence and incidence of disease, including cross-sectional studies, cohort studies, population case–control studies, and even experimental studies (e.g., randomized controlled trials) in which a biological survey was conducted to test for HCV before the introduction of the intervention (baseline) were included. Case reports, case series, and qualitative studies were excluded. For the disease area, studies with biological evidence on infection with HCV were included. Self-reported data on the diseases were excluded. The geographical scope was limited to studies conducted within Iran; the studies conducted among Iranian populations residing outside of Iran were not included. For the study population, studies conducted in human subjects who self-identified as current or former drug users were included. Studies on populations who were in short-term mandatory drug treatment and rehabilitation detention centers were included. Studies in non-human subjects, blood donors, dialysis patients, pregnant women, families or sexual partners of HCV/HBV patients, and populations with other chronic diseases (e.g., studies reporting HCV among people with liver cancer) were excluded. No limits were set on study implementation or publication date.
Data extraction, quality assessment, and risk of bias
Two authors (AR and HSH) reviewed the retrieved studies independently, and the following information was extracted: name of the first author, year of publication, date of study, location of study, total sample size, the prevalence of HCV Ab, recruitment setting, and recruitment method. The third author (SMA) was determined as the arbiter to resolve any disagreements.
Two independent investigators (AR and HSH) assessed the quality of the studies using the Critical Appraisal Skills Programme (CASP) tools for observational studies [40] and a critical appraisal tool for prevalence studies [41]. We used the following criteria for critical appraisal: (1) sampling method; (2) recruitment setting; (3) presenting the type of test; (4) presenting the definition of PWID; and (5) refusal rate. The documents were evaluated in terms of the above-mentioned criteria. Discrepancies were resolved by discussion or through consultation with the third investigator (SMA).
Data analysis
The extracted data were entered into the Excel software. Then, Stata 16.0 was used for analysis. Pooled prevalence and 95% confidence intervals were calculated using Der Simonian and Laird method, taking into account conceptual heterogeneity, and I2, Tau2, and X2 were applied to assess heterogeneity among studies. The “metaprop” command was used to calculate the pooled prevalence of HCV Ab and the prevalence in different subgroups, by available geographical locations and study settings. The pooled prevalence of HCV Ab before 2005 (before scale-up of the harm reduction program at the national level) and during and after 2005 (after scale-up of the harm reduction program at the national level) was presented in a forest plot, and the heterogeneity of studies conducted in each period was estimated. The Q test was applied to assess heterogeneity between periods. Furthermore, the presence and the effect of publication bias were investigated using a combination of the visual inspection of funnel plots and Begg’s and Egger’s tests. Moreover, a trim-and-fill analysis was performed to assess the stability of overall prevalence when the results suggested obvious publication bias. The prevalence of HCV Ab for each province was also calculated and depicted on the map, using the GIS software.
To assess differences in the accumulation of evidence for HCV Ab prevalence in PWID in Iran, cumulative meta-analyses were conducted. The cumulative meta-analysis provides cumulative pooled estimates and 95% CIs. As studies are successively added, the overall prevalence and 95% CIs are recalculated providing evidence of the evolution of HCV Ab prevalence over time. To assess the sequential contributions of studies and evaluate changes in HCV Ab prevalence over time, studies were added alphabetically by years of implementation to a random-effects model using the “metacum” user-written command in Stata version 16.0. Besides, the sequential contributions of studies were evaluated before 2005 and during and after 2005 for HCV Ab prevalence over time by cumulative meta-analysis.
For investigating the trend of HCV Ab prevalence over time, the pooled prevalence every 3 years was estimated and presented in a line graph because the number of studies conducted in each year was few. The Cochran–Armitage test for linear trend was used by Winpepi software to test the variation in the prevalence of HCV Ab.
Results
Study screening and characteristics
A total of 7550 documents were found through searching databases, and 300 were retrieved through other review articles. After removing the duplicates, the titles and abstracts of 5966 documents were screened, of which 5683 documents were excluded because of not meeting the study criteria. If the inclusion criteria were not clear from the abstract, the full text was assessed. In this stage, 221 documents were excluded for different reasons. Finally, data were extracted and subjected to a meta-analysis from the remaining 62 documents (60 cross-sectional studies and 2 case–control studies) (Fig. 1) [15, 21, 42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101].
The prevalence of HCV Ab was assessed in 27,033 PWID in 62 studies. The smallest and largest sample size was 34 and 3,284 PWID, respectively. Twenty-three studies were conducted in DICs, and 16 were done in hospitals and healthcare centers. Table 1 presents the characteristics of the studies. There is a differential distribution of the studies across time by the study recruitment setting (Appendix 3).
Risk of bias in studies
The risk of bias and the quality of the study were assessed for the 62 included studies. Most of the studies did not have optimal condition. The highest risk of bias was related to the recruitment setting and sampling method that was seen in most of the studies (Appendix 4).
Pooled HCV Ab prevalence among PWID and subgroups
The pooled HCV Ab prevalence was 46.5% (95% confidence interval [95% CI] 41.1–52.0%), among PWID in Iran (Fig. 2). The pooled prevalence of HCV Ab according to the recruitment setting in a descending order was as follows: prisons [14 studies, N = 6,399, P = 59.4%, 95% CI 50.1–68.7%], behavioral disease counseling centers [two studies, N = 297, P = 58.3%, 95% CI 47.3–69.3%], community-based settings [five studies, N = 4,954, P = 46.5%, 95% CI 38.0–55.1%], hospitals and healthcare centers [16 studies, N = 2,198, P = 44.1%, 95% CI 27.7–60.5%], and DICs [23 studies, N = 12,841, P = 38.0%, 95% CI 30.6–45.4%] (Fig. 3).
The prevalence of HCV Ab according to the provinces is presented in Fig. 4. The provinces with the highest and lowest HCV Ab prevalence were as follows: Gilan Province (N = 81, P = 88.9%, 95% CI 82.1–95.7%) and Chaharmahal Province (N = 133, P = 11.3%, 95% CI 5.9–16.7%), respectively. There were no data for 14 provinces (East Azerbaijan, West Azerbaijan, Ardabil, Kurdistan, Qazvin, Lorestan, Bushehr, Ilam, Qom, Semnan, North Khorasan, Yazd, Semnan, South Khorasan, and Sistan and Baluchestan) of Iran. In Tehran, the capital of Iran, and in Isfahan with the highest sample size, the pooled HCV Ab prevalence was 47.0% (95% CI 35.2–58.9%) and 40.6% (95% CI 31.9–49.3%), respectively.
The pooled prevalence of HCV Ab before 2005 and during and after 2005 was 49.5% (95% CI 40.6–58.4%) and 44.6% (95% CI 37.6–51.6%), respectively (test of group differences: Q = 0.7, P value = 0.39) (Appendix 5). Pooling the data before harm reduction program (before 2005), the HCV Ab prevalence in prison, hospitals and healthcare centers, and DICs was 61% (95% CI 49–72%), 43% (95% CI 25–61%) and 39% (95% CI 25–53%), respectively. Pooling the data after harm reduction program (during and after 2005), the HCV Ab prevalence in prison, hospitals and healthcare centers, and DICs was 58% (95% CI 43–73%), 46% (95% CI 17–75%) and 38% (95% CI 29–46%), respectively (Appendix 6).
Cumulative meta-analyses
A cumulative meta-analysis was conducted to reflect the dynamic trend of results and evaluate the influence of individual study on the overall results. Figure 5 shows a forest plot for the cumulative meta-analysis for the trend of HCV Ab prevalence in PWID. A high prevalence (53%) of HCV Ab was first observed in 2000 and remained unchanged or had paradoxical changes after 24 more studies published between 2000 to 2005, and thereafter, the prevalence of HCV Ab between 2005 to 2018 slowly declined (Fig. 5). The cumulative meta-analysis was also presented by the study setting in Appendix 7. The results showed that with an increasing number of studies in later years the prevalence of HCV Ab is somewhat reduced or unchanged in all settings. In the prison setting, the trend of HCV Ab prevalence was increasing by 2002, and then it was slightly declining. This declining trend was also observed for DIC and hospital and healthcare center settings. Besides, considering the potential sampling bias in the hospital setting, we performed the analysis for DIC and prison by the year of study implementation (Appendix 8). The results of this analysis also showed that before 2005, there was no clear trend for the prevalence of HCV Ab. But after 2005, there was a slight decrease until 2011; after that, the trend remained almost stable.
Trend analysis
Figure 6 presents the trend of HCV Ab prevalence in PWID in periods from 1995 to 2018. HCV Ab prevalence decreased from 58.3% (95% CI 49.7–66.8%) before 2003 to 44.5% (95% CI 32.7–56.4%) in 2003–2005 and then increased to the level of 55.1% (95% CI 43.7–66.5%) in 2006–2008 and then showed a decline to 32.1% (95% CI 23.0–41.1%) in studies between 2009 and 2011 and then showed a slight increase to the level of 47.9% (95% CI 41.9–53.9%) in studies during and after 2012. In 2009–2011, the decreasing trend of HCV Ab prevalence is statistically significant (b = − 0.23, 95% CI − 0.38, − 0.07, P value = 0.004). The Cochran–Armitage test for trend indicated a significant decreasing trend of HCV Ab in PWID in total (P value = 0.03).
The trend of HCV Ab prevalence among PWID was presented by the recruitment setting in Appendix 9. The trend of HCV Ab prevalence among PWID in the prison setting did not decrease significantly (Cochran–Armitage test for linear trend = 1.85, P value = 0.17). However, trend analysis results indicated a statistically significant decrease in HCV Ab prevalence among PWID in the hospitals and healthcare centers (Cochran–Armitage test for linear trend = 38.72, P value < 0.001) and DIC settings (Cochran–Armitage test for linear trend = 5.93, P value = 0.01) (Appendix 9).
Publication bias
When we plotted the prevalence estimates against their standard errors, there was no publication bias (Fig. 7). Furthermore, the results were confirmed with Begg and Mazumdar’s tau 0.22 (P value = 0.83) and Egger’s regression intercept 1.43 (P value = 0.15). Trim-and-fill method for calibration of publication bias was performed. However, the missing study was not identified by the trim-and-fill method.
Meta-regression analyses
The results of the univariate meta-regression analyses for investigation into the sources of heterogeneity showed that only the recruitment setting had a significant effect on HCV Ab prevalence: date of study (b = − 0.01, 95% CI − 0.02, 0.001, P value = 0.08), study type as cross-sectional versus case–control study (b = − 0.13, 95% CI − 0.45, 0.17, P value = 0.38), sampling method as random sampling versus convenience sampling (b = 0.001, 95% CI − 0.17, 0.17, P value = 0.98), recruitment setting as hospitals and healthcare centers versus prison (b = − 0.15, 95% CI − 0.29, − 0.01, P value = 0.03), DIC versus prison (b = − 0.21, 95% CI − 0.34, − 0.08, P value = 0.001), and community-based setting versus prison (b = − 0.12, 95% CI − 0.32, 0.06, P value = 0.20). Univariate meta-regression showed that the 8.81% of between-study variance is explained by date of study, 0.22% by study design, 0.0% by sampling method, and 21.88% by recruitment setting.
Discussion
PWID is the main population affected by HCV infection worldwide [102]. The present systematic review and meta-analysis was conducted on 62 observational studies, involving 27,033 PWID. This study examined the prevalence of HCV Ab before and after implementation of the harm reduction program in PWID in Iran. To our knowledge, this is the first systematic review and meta-analysis to examine the prevalence of HCV Ab among PWID before and after implementation of the harm reduction program. In the period since the last major systematic reviews [22, 38], there has been an increase in the amount of evidence documenting drug injection and the prevalence of HCV Ab in PWID in Iran. This updated estimation showed that approximately one in two PWID in Iran are tested positive for HCV Ab, with substantial regional- and provincial-level variations in the prevalence of this blood-borne infection. The results showed a high prevalence of HCV Ab among PWID in Iran, which is consistent with a worldwide estimate in this population [103] and other systematic reviews [22, 38], and still lower than the prevalence reported in certain other countries (e.g., Bulgaria, Estonia, and South Africa) [104, 105] but higher than in studies conducted in Kuwait (12.3%) [106], Kingdom of Saudi Arabia (42.7%) [107], and Brazil (35.6%) [108]. These differences in the prevalence can be attributed to differences in the health systems, screening methods, and the type of high-risk behaviors of individuals [109, 110]. In particular, in the developing countries, the harm reduction programs such as syringe distribution are not fully implemented [111]. Moreover, in the countries with high coverage of HCV care, cases are diagnosed and treated earlier and the transmission of HCV is prevented in the community, which can also be the reason for the inconsistent findings among different studies [112, 113].
The pooled prevalence of HCV Ab was 49% before 2005 and 45% during and after 2005. Evaluation of the trend showed a slightly decreasing trend in the prevalence of HCV Ab in PWID over time. Besides, with the evaluation of the cumulative meta-analysis of HCV Ab prevalence, it seems there was a slightly declined or stable prevalence of HCV Ab among PWID in Iran. The study of Nematollahi et al. [22] showed a decreasing trend in the prevalence of hepatitis C among high-risk groups (β = − 0.021) in 2000–2015. These studies confirmed the findings of the current systematic review, which showed a slight decline in the prevalence of HCV Ab among PWID since 2005.
Globally, studies have shown that implementing NSP and maintenance treatment with methadone reduces high-risk behaviors [30,31,32]. According to the actions associated with harm reduction in Iran after 2005, this study indicated that the prevalence of HCV Ab among PWID in Iran did not increase. Although the difference in the prevalence before 2005 and after 2005 was not significant, there seemed to be lower prevalence estimates in later years. This study examined the prevalence of HCV Ab which is defined as the number of affected persons with HCV Ab in the population at a specific time [114]. Moreover, when there is a gradual decreasing or stable prevalence of HCV Ab, it is partly attributable to a decrease in the incidence of HCV infection. Thus, the stable or slightly declining prevalence of HCV Ab after 2005 which indicates that new cases of the disease are less reported after 2005 can be partly caused by implementation of the harm reduction program. However, it should be noted that the decrease or stability in the prevalence of HCV Ab may also be influenced by other factors such as the high mortality of PWID with HCV infection, exclusion from being PWID by stopping drug injection and study design differences. Furthermore, another issue that may justify the stable or decreasing prevalence of HCV Ab is that over the past two decades in Iran, drug use patterns changed from traditional drug use, mainly heroin and opium to the recreational use of amphetamine-type stimulants, especially crystal methamphetamine [115, 116]. Several Iranian studies showed that the prevalence of blood-borne infections (including HCV) among people with methamphetamine use is less than those with traditional drug use [39, 117,118,119]. This is because drug injection or syringe sharing is more in traditional drug users than methamphetamine users [17, 119]. More, the prevalence of HCV Ab is different by the recruitment setting and there is a differential distribution of studies across time by the recruitment setting (e.g., more studies in DICs in recent years) causing a declining trend in the pooled results for HCV Ab prevalence. Therefore, it is needed to be confirmed by a cohort study thoroughly the impact of the harm reduction program on the incidence of HCV infection among PWID. To the best of our knowledge, no study in Iran measured the incidence of HCV infection among PWID. Van Den Berg et al. [34] confirmed in the Amsterdam Addiction Cohort study that the incidence of HCV infection among PWID who received both OST and high coverage NSP was approximately one-third lower than that of those who received either OST or NSP alone. In addition, Sharifi et al. [120] indicated that HIV infection incidence among PWID in 2014 was 5.39 (95% CI 4.71, 6.16) per 1,000 person-years (PY), significantly lower than 17.07 in 2009 (95% CI 15.34, 19.34). Moreover, HIV infection incidence decreased among inmates from 1.34 (95% CI 1.08, 1.67) in 2009 to 0.49 (95% CI 0.39, 0.61) per 1,000 PY in 2013. This study suggested that after an increase in the 2000s, the HIV infection incidence decreased and stabilized among PWID and prisoners in Iran. This could be explained by expanding the preventive interventions, e.g., an increasing number of harm reduction centers for PWID and scaling up free harm reduction services such as increased coverage of the NSP among PWID. The above-mentioned studies suggested that a harm reduction intervention is needed to reach PWID early on to be effective in reducing the risk of HCV transmission. This is especially applicable to Iran if the overall coverage of the NSP and OST programs has reached sufficient among PWID. Other studies have confirmed the effectiveness of the harm reduction program as well [121,122,123,124]. In addition, the study by Rahimi et al. [125] reported that the prevalence of HIV was 14.3% before 2007 and 9.7% after 2007. These studies are approving the findings of the current systematic review, which showed sufficient evidence on the effectiveness of harm reduction program in the containment of HCV epidemics among PWID in Iran.
Some limitations of our study were differences in the studies carried out in different provinces and insufficient data from several provinces. The prevalence of HCV Ab in PWID had a wide range in different provinces (11–89%). The regional differences, at least somewhat, might be as a result of variations in time of the study and recruitment settings. It might also be due to differences in socio-demographic characteristics, access conditions for study participants, and high-risk behaviors of PWID in provinces of Iran. In addition, the number of studies conducted in each province is different. In a study [126] conducted in China, the prevalence of HCV Ab was different in various geographical regions. It has been stated that this finding may be due to the differences in the pattern of high-risk behaviors, poverty, and ethnicity in different provinces. These findings indicated that the burden of HCV is still high in some areas, and the scale-up of interventions to prevent and treat HCV among PWID remains a crucial priority to address the HCV epidemics. In the included primary studies, no data were also available about PWID living in the rural areas. Most studies were either conducted in the urban areas or did not report any information about the place of residence (urban versus rural). The reason may be the tendency of PWID to cluster in the cities and urban areas in Iran. Besides, the settings where services for PWID are provided, like DICs, are the main settings for recruitment in the surveys and are mainly located in the cities. However, it causes limitations in the extrapolation of the results to all PWID in the country. Finally, the quality of tests used to determine HCV varied in the included studies and the proportions of the participants receiving the OST and NSP may influence the results of this review; however, we were unable to conduct additional subgroup analysis by the quality of tests and coverage of OST and NSP in this meta-analysis because of the lack of data.
Despite the above-mentioned limitations, the results of this meta-analysis are valuable due to its large sample size, offering evidence to support the hypothesis that after the extensive implementation of harm reduction programs in Iran, the HCV epidemic among PWID has been controlled. We also performed a cumulative meta-analysis by the study date to investigate a trend of the HCV Ab prevalence, and the result indicated that our conclusion was robust when more new studies were added.
Conclusions
There is a large burden of HCV infection among PWID in Iran. The prevalence of HCV Ab in PWID decreased after 2005, and although not significant, there seemed to be lower prevalence estimates in later years. There are great variations in the prevalence of HCV Ab between different provinces. However, there is no sufficient information available from many provinces. Overall, the results of our study supported the effectiveness of harm reduction program in reducing HCV transmission.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Blach S, Zeuzem S, Manns M, Altraif I, Duberg A-S, Muljono DH, et al. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol. 2017;2(3):161–76.
Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45(4):529–38.
Mohd Hanafiah K, Groeger J, Flaxman AD, Wiersma ST. Global epidemiology of hepatitis C virus infection: new estimates of age-specific antibody to HCV seroprevalence. Hepatology. 2013;57(4):1333–42.
Friedland G. Infectious disease co-morbidities adversely affecting substance users with HIV: hepatitis C and tuberculosis. J Acquir Immune Defic Syndr. 2010;55(01):S37.
Nelson PK, Mathers BM, Cowie B, Hagan H, Des Jarlais D, Horyniak D, et al. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews. Lancet. 2011;378(9791):571–83.
Walsh N, Maher L. HIV and viral hepatitis C coinfection in people who inject drugs: implications of new direct acting antivirals for hepatitis C virus treatment. Curr Opin HIV AIDS. 2012;7(4):339–44.
Merz F. United Nations Office on drugs and crime: world drug report 2017. SIRIUS-Zeitschrift für Strategische Analysen. 2018;2(1):85–6.
Degenhardt L, Whiteford HA, Ferrari AJ, Baxter AJ, Charlson FJ, Hall WD, et al. Global burden of disease attributable to illicit drug use and dependence: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1564–74.
Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Global Health. 2017;5(12):e1192–207.
Noroozi M, Ahounbar E, Eddin Karimi S, Ahmadi S, Najafi M, Bazrafshan A, et al. HIV risk perception and risky behavior among people who inject drugs in Kermanshah, Western Iran. Int J Behav Med. 2017;24(4):613–8.
Sharifi H, Mirzazadeh A, Noroozi A, Marshall BD, Farhoudian A, Higgs P, et al. Patterns of HIV risks and related factors among people who inject drugs in Kermanshah, Iran: a latent class analysis. J Psychoact Drugs. 2017;49(1):69–73.
Mumtaz GR, Weiss HA, Thomas SL, Riome S, Setayesh H, Riedner G, et al. HIV among people who inject drugs in the Middle East and North Africa: systematic review and data synthesis. PLoS Med. 2014;11(6):e1001663.
Rahimi-Movaghar A, Amin-Esmaeili M, Aaraj E, Hermez J. Assessment of situation and response to drug use and its harms in the Middle East and North Africa, 2012. Middle East and North Africa Harm Rediction Association (MENAHRA). 2013.
Amin-Esmaeili M, Rahimi-Movaghar A, Gholamrezaei M, Razaghi EM. Profile of people who inject drugs in Tehran, Iran. Acta Med Iran. 2016;54:793–805.
Amin-Esmaeili M, Rahimi-Movaghar A, Razaghi EM, Baghestani AR, Jafari S. Factors correlated with hepatitis C and B virus infections among injecting drug users in Tehran, IR Iran. Hepat Mon. 2012;12(1):23.
Rahimi-Movaghar A, Amin-Esmaeili M, Aaraj E, Hermez J. Assessment of situation and response to drug use and its harms in the Middle East and North Africa, 2012. Beirut: Middle East North Africa Harm Rediction Association; 2013.
Moradi G, Hajarizadeh B, Rahmani K, Mohamadi-Bolbanabad A, Darvishi S, Zareie B, et al. Drug use and risk behaviour profile, and the prevalence of HIV, hepatitis C and hepatitis B among people with methamphetamine use in Iran. Int J Drug Policy. 2019;73:129–34.
Hariri S, Sharafi H, Sheikh M, Merat S, Hashemi F, Azimian F, et al. Continuum of hepatitis C care cascade in prison and following release in the direct-acting antivirals era. Harm Reduct J. 2020;17(1):1–9.
Hesamizadeh K, Sharafi H, Rezaee-Zavareh MS, Behnava B, Alavian SM. Next steps toward eradication of hepatitis C in the era of direct acting antivirals. Hepat Mon. 2016;16(4):e37089.
Sharafi H, Poustchi H, Azimian F, Tamadoni B, Ramezani R, Gouya MM, et al. Performance of a rapid diagnostic test for screening of hepatitis C in a real-life prison setting. J Clin Virol. 2019;113:20–3.
Zamani S, Radfar R, Nematollahi P, Fadaie R, Meshkati M, Mortazavi S, et al. Prevalence of HIV/HCV/HBV infections and drug-related risk behaviours amongst IDUs recruited through peer-driven sampling in Iran. Int J Drug Policy. 2010;21(6):493–500.
Nematollahi S, Ayubi E, Almasi-Hashiani A, Mansori K, Moradi Y, Veisani Y, et al. Prevalence of hepatitis C virus infection among high-risk groups in Iran: a systematic review and meta-analysis. Public Health. 2018;161:90–8.
Narenjiha H, Rafiei H, Baghestani A, Nouri R, Shirinbayan P, Farhadi M. Rapid situation assessment of drug abuse in Iran (year 2004) Research report. Tehran: Dariush Institute; 2007.
Razzaghi E, Rahimi A, Hosseini M, Chatterjee A. Rapid Situation Assessment (RSA) of drug abuse in Iran. Prevention Department, State Welfare Organization, Ministry of Health, IR of Iran United Nations International Drug Control Program. 1999.
Razzaghi E, Nassirimanesh B, Afshar P, Ohiri K, Claeson M, Power R. HIV/AIDS harm reduction in Iran. Lancet. 2006;368(9534):434–5.
Nissaramanesh B, Trace M, Roberts M. The rise of harm reduction in the Islamic Republic of Iran. Beckley Foundation Drug Policy Programme, Briefing Paper. 2005;8.
Zafarghandi MBS, Jadidi M, Khalili N. Iran’s activities on prevention, treatment and harm reduction of drug abuse. Int J High Risk Behav Addict. 2015;4(4):e22863.
HEALTH IMO. National report on drug treatment and harm reduction services. Tehran: Iran Ministry of Health, Office for Mental and social Health and Substance Abuse; 2008 (in Persian).
Doroudi F. Islamic Republic of Iran AIDS Progress Report, On monitoring of the United Nations general assembly special session on HIV and AIDS 2013.
Aspinall EJ, Nambiar D, Goldberg DJ, Hickman M, Weir A, Van Velzen E, et al. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: a systematic review and meta-analysis. Int J Epidemiol. 2013;43(1):235–48.
Karki P, Shrestha R, Huedo-Medina TB, Copenhaver M. The impact of methadone maintenance treatment on HIV risk behaviors among high-risk injection drug users: a systematic review. Evid Based Med Public Health. 2016;2:e1229.
Palmateer N, Kimber J, Hickman M, Hutchinson S, Rhodes T, Goldberg D. Evidence for the effectiveness of sterile injecting equipment provision in preventing hepatitis C and human immunodeficiency virus transmission among injecting drug users: a review of reviews. Addiction. 2010;105(5):844–59.
Kimber J, Palmateer N, Hutchinson SJ, Hickman M, Goldberg DJ, Rhodes T. Harm reduction among injecting drug users-evidence of effectiveness. 2010.
Van Den Berg C, Smit C, Van Brussel G, Coutinho R, Prins M. Full participation in harm reduction programmes is associated with decreased risk for human immunodeficiency virus and hepatitis C virus: evidence from the Amsterdam Cohort Studies among drug users. Addiction. 2007;102(9):1454–62.
Amiri FB, Mostafavi E, Mirzazadeh A. HIV, HBV and HCV coinfection prevalence in Iran-a systematic review and meta-analysis. PLoS ONE. 2016;11(3):e0151946.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. 2010.
Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. PLoS Med. 2016;13(6):e1002056.
Malekinejad M, Navadeh S, Lotfizadeh A, Rahimi-Movaghar A, Amin-Esmaeili M, Noroozi A. High hepatitis C virus prevalence among drug users in Iran: systematic review and meta-analysis of epidemiological evidence (2001–2012). Int J Infect Dis. 2015;40:116–30.
Rajabi A, Dehghani M, Shojaei A, Farjam M, Motevalian SA. Association between tobacco smoking and opioid use: a meta-analysis. Addict Behav. 2018;92:225–35.
Checklists C. Critical Appraisal Skills Programme (CASP). 2018.
Munn Z, Moola S, Riitano D, Lisy K. The development of a critical appraisal tool for use in systematic reviews addressing questions of prevalence. Int J Health Policy Manag. 2014;3(3):123.
Noroozi A. Bio-behavioral survey among injecting drug users and their sexual partners in Karaj. Isfahan and Gorgan, final report, United Nation Office of Drug and Crime 2011. https://www.unodc.org/documents/islamicrepublicofiran//Couple_BSS_Final_Report.pdf. 2011.
Mirahmadizadeh A, Kadivar M, Hemmati A, Javadi A. In international conference on AIDS. 2004. p. 16.
M. M. Prevalence of HIV, hepatitis B and C among drug abusers admitted to ICU of Baharloo hospital in 2010 [Ph.D. thesis of Forensic Medicine]: Tehran University of Medical Sciences; 2012.
Zamani S, Ichikawa S, Nassirimanesh B, Vazirian M, Ichikawa K, Gouya MM, et al. Prevalence and correlates of hepatitis C virus infection among injecting drug users in Tehran. Int J Drug Policy. 2007;18(5):359–63.
Zali MR, Aghazadeh R, Nowroozi A, Amir-Rasouly H. Anti-HCV antibody among Iranian IV drug users: is it a serious problem? Arch Iran Med. 2001;4(3):115–9.
Zadeh SM, Kassaian N, Ataei B, Nokhodian Z, Adibi P. Hepatitis C screening in intravenous drug users under treatment with methadone: an action research study. J Isfahan Med School. 2011;28.
Tayeri K, Kasaeian N, Fadaei NR, Ataei B. The prevalence of hepatitis B, hepatitis C and associated risk factors in intravenous drug addicts (IVDA) with HIV in Isfahan. J Isfahan Med School IUMS. 2008;26(90):273–8.
Tavanaee SA, Khaleghi NM. Epidemiologic evaluation and some species in injection drug users that admitted in infectious department of Imam Reza Hospital (2007–2009). J Med Counc IRI. 2012;30(2):155–61.
Sofian M, Aghakhani A, Banifazl M, Azadmanesh K, Farazi A-A, McFarland W, et al. Viral hepatitis and HIV infection among injection drug users in a central Iranian City. J Addict Med. 2012;6(4):292–6.
Sharif M, Sherif A, Sayyah M. Frequency of HBV, HCV and HIV infections among hospitalized injecting drug users in Kashan. Indian J Sex Transm Dis AIDS. 2009;30(1):28.
Sharhani A, Mehrabi Y, Noroozi A, Nasirian M, Higgs P, Hajebi A, et al. Hepatitis C virus seroprevalence and associated risk factors among male drug injectors in Kermanshah, Iran. . Hepat Mon. 2017;17(10):e58739.
Sayad B, Shams ASF, Keyvani H, Rezaei M, Asadi T, Vaziri S, et al. Seroepidemiology of hepatitis C in Kermanshah (West of Iran, 2006). Hepat Mon. 2008;8(2):141–6.
Sarkari B, Eilami O, Khosravani A, Sharifi A, Tabatabaee M, Fararouei M. High prevalence of hepatitis C infection among high risk groups in Kohgiloyeh and Boyerahmad Province, Southwest Iran. Arch Iran Med. 2012;15(5):268.
Salehi A, Naghshvarian M, Marzban M, Lankarani KB. Prevalence of HIV, HCV, and high-risk behaviors for substance users in drop in centers in southern Iran. J Addict Med. 2015;9(3):181–7.
Saleh M, Kazemifar AM, Saleh AE, Hosseinpour NAA, Samimi R. Prevalence of HIV, hepatitis B and C seropositivity in expired IV drug abusers in Hamedan. Sci J Forensic Med. 2011;16(4):253–7.
RostamiJalilian M, Ghaemi O, Kassaeian N. Relationship of hepatitis B and C with deep vein thrombosis in IV drug abusers. J Mil Med. 2006;8(1):78–81.
Rezaei F, Noroozi A, Armoon B, Farhoudian A, Massah O, Sharifi H, et al. Social determinants and hepatitis C among people who inject drugs in Kermanshah, Iran: Socioeconomic status, homelessness, and sufficient syringe coverage. J Subst Use. 2017;22(5):474–8.
Ramezani A, Amirmoezi R, Volk JE, Aghakhani A, Zarinfar N, McFarland W, et al. HCV, HBV, and HIV seroprevalence, coinfections, and related behaviors among male injection drug users in Arak, Iran. AIDS Care. 2014;26(9):1122–6.
Rahimi-Movaghar A, Razaghi EM, Sahimi-Izadian E, Amin-Esmaeili M. HIV, hepatitis C virus, and hepatitis B virus co-infections among injecting drug users in Tehran. Iran Int J Infect Dis. 2010;14(1):e28–33.
Rahbar AR, Rooholamini S, Khoshnood K. Prevalence of HIV infection and other blood-borne infections in incarcerated and non-incarcerated injection drug users (IDUs) in Mashhad, Iran. Int J Drug Policy. 2004;15(2):151–5.
Nokhodian Z, Meshkati M, Adibi P, Ataei B, Kassaian N, Yaran M, et al. Hepatitis C among intravenous drug users in Isfahan, Iran: a study of seroprevalence and risk factors. Int J Prev Med. 2012;3(Suppl1):S131.
Nobari RF, Meshkati M, Ataei B, Heidari K, Kassaian N, Nokhodian Z, et al. Positive hepatitis C virus antibody in cases with history of intravenous drug abuse via community announcement: a useful experience. J Isfahan Med School. 2011;28:1564–70.
Naderi N. Epidemiology of hepatitis C in hospitalized addicts in Loghman Hakim Hospital, 2000–2001. Tehran: Shahid Beheshti University of Medical Sciences; 2003.
Moradi G, Gouya MM, Azimizan Zavareh F, Mohamadi Bolbanabad A, Darvishi S, Aghasadeghi MR, et al. Prevalence and risk factors for HBV and HCV in prisoners in Iran: a national bio-behavioural surveillance survey in 2015. Tropical Med Int Health. 2018;23(6):641–9.
Momen-Heravi M, Afzali H, Moosavipanah H, editors. Prevalence of anti HIV, ANTIHCV and HBSAG positive among injection drug users in Kashan-Iran. New York: Springer; 2012.
Mohtasham-Amiri ZRM, Jaafari-Shakib RAJ-S. The prevalence of hepatitis C infection in drug prisoners, Lakan Prison in Rasht. Payesh. 2006;6:5–10 ((in Persian)).
Mir-Nasseri S, Poustchi H, Nasseri-Moghadam S, Nouraie S, Tahaghoghi S, Afshar P, et al. HCV in intravenous drug users. Govaresh. 2005;10(2):80–6.
Mir-Nasseri MM, MohammadKhani A, Tavakkoli H, Ansari E, Poustchi H. Incarceration is a major risk factor for blood-borne infection among intravenous drug users: incarceration and blood borne infection among intravenous drug users. Hepat Mon. 2011;11(1):19.
Mirahmadizadeh AR, Majdzadeh R, Mohammad K, Forouzanfar M. Prevalence of HIV and hepatitis C virus infections and related behavioral determinants among injecting drug users of drop-in centers in Iran. Iran Red Crescent Med J IRCMJ. 2009;11(3):325–9.
Meshkati M, Taeri K, Etedali E, Farid F, editors. Prevalence of Hepatitis B, C and HIV/AIDS in injecting drug users referred to the Behavioral Diseases Counseling Center in 2004. The first National Congress of infection in drug addicts in Iran; 2007.
Meidani M, Farzaneh S, Ajami Baferani A, Hassan Zade A. Seroprevalence of HTLV1, 2 virus among injection drug addicts in Isfahan, 2007–2008. SSU J. 2009;17(4):286–90.
Malekinejad M, Mohraz M, Razai N, Khairandish P, McFarland W, Akbari R, et al., editors. Enhancing HIV surveillance capacity in Iran: lessons learned from implementation of respondent-driven sampling among injecting drug users. Unite For Sight. Fifth Annual International Health Conference, Building Global Health For Today and Tomorrow Yale University, New Haven, CT; 2008.
Khorvash F, Fasihi Dastjerdi M, Emami Naeini A. In 1st National Congress of Infection in Addicts. 2005:23–9.
Khodadadizadeh A, EsmaeiliNadimi A, Hosseini S, Shabanishahrbabaki Z. The prevalence of HIV, HBV and HCV in narcotic addicted persons referred to the outpatient clinic of Rafsanjan University of Medical Sciences in 2003. J Rafsanjan Univ Med Sci. 2006;5(1):23–30.
Kheirandish P, SeyedAlinaghi S, Jahani M, Shirzad H, Ahmadian MS, Majidi A, et al. Prevalence and correlates of hepatitis C infection among male injection drug users in detention, Tehran, Iran. J Urban Health. 2009;86(6):902.
Khani M, Vakili MM. Prevalence and risk factors of HIV, hepatitis B virus and hepatitis C virus infections in drug addicts among Zanjan prisoners. Arch Iran Med. 2003;6(1):1–4.
Keramat F, Eini P, Majzoobi M. Seroprevalence of HIV, HBV and HCV in persons referred to hamadan behavioral counseling center, west of Iran. Iran Red Crescent Med J. 2011;13(1):42.
Kassaian N, Adibi P, Kafashaian A, Yaran M, Nokhodian Z, Shoaei P, et al. Hepatitis C virus and associated risk factors among prison inmates with history of drug injection in Isfahan, Iran. Int J Prev Med. 2012;3(Suppl1):S156.
Kaffashian A, Nokhodian Z, Kassaian N, Babak A, Yaran M, Shoaei P, et al. The experience of hepatitis C screening among prison inmates with drug injection history. J Isfahan Med School. 2011;28:1565–71.
Ismail H, Rouhollah Y, Noorah S, Masoud S, Ali K, Fatemeh M. Investigation of intravenous drug users and determining the rate of HIV and hepatitis virus in Loghman Hakim hospital. Iran J Surg. 2005;13:89–94.
Imani R, Karimi A, Rouzbahani R, Rouzbahani A. Seroprevalence of HBV, HCV and HIV infection among intravenous drug users in Shahr-e-Kord, Islamic Republic of Iran. East Mediterr Health J. 2008;14(5):1136–41.
Hosseini M, Seyed ANS, Kheyr AP, Esmaeili JGR, Shirzad H, Karami N, et al. Prevalence and correlates of co-infection with human immunodeficiency virus and hepatitis C virus in male injection drug users in Iran. Arch Iran Med. 2010;13:318–23.
Honarvar B, Odoomi N, Moghadami M, Kazerooni PA, Hassanabadi A, Dolatabadi PZ, et al. Blood-borne hepatitis in opiate users in iran: a poor outlook and urgent need to change nationwide screening policy. PLoS ONE. 2013;8(12):e82230.
Hajinasrollah AYR, Salehi N, Saheh M, Khoshkar A, Malekpour F, Ghaseminejad A, et al. Prevalence of HIV, hepatitis B, and hepatitis C in drug abuser in Loghman Medical Center. IJS. 2006;13:89–94 ((in Persian)).
Ghasemian R, Najafi N, Amirkhanloo K. The study of infections due to injection drug abuse in the injecting drug users hospitalized at Imam Khomeini Hospital in Sari and Razi Hospital in Ghaemshahr in 2007–2009. J Mazandaran Univ Med Sci. 2011;21(83):9–15.
Eskandarieh S, Nikfarjam A, Tarjoman T, Nasehi A, Jafari F, Saberi-Zafarghandi M-B. Descriptive aspects of injection drug users in Iran’s national harm reduction program by methadone maintenance treatment. Iran J Public Health. 2013;42(6):588.
Davoodian P, Dadvand H, Mahoori K, Amoozandeh A, Salavati A. Prevalence of selected sexually and blood-borne infections in Injecting drug abuser inmates of Bandar Abbas and Roodan correction facilities, Iran, 2002. Braz J Infect Dis. 2009;13(5):356–8.
Azizi A, Amirian F, Amirian M. The prevalence of hepatitis C infection in self reported drug abusers and related factors. Hayat. 2011;17:55–61.
Ataei B, Meshkati M, Karimi A, Yaran M, Kassaian N, Nokhodian Z, et al. Hepatitis C screening in intravenuos drug users in golpayegan, isfahan through community announcement: pilot study. J Isfahan Med School. 2011;28:1537–45.
Ataei B, Babak A, Yaran M, Kassaian N, Nokhodian Z, Meshkati M, et al. Hepatitis C in intravenous drug users: seroprevalence and risk factors. J Isfahan Med School. 2011;28:1537–45.
Ataei B, Adibi P, Yaran M, Kassaian N, Nokhodian Z, Meshkati M, et al. Seroepidemiology of hepatitis C in cases with history of intravenous drug use in Isfahan province, Iran: P1138. Clin Microbiol Infect. 2010;16:326–31.
Asl RT, Eshrati B, Dell CA, Taylor K, Afshar P, Kamali M, et al. Outcome assessment of a triangular clinic as a harm reduction intervention in Rajaee-Shahr Prison, Iran. Harm Reduct J. 2013;10(1):41.
Aminzadeh Z, Sarhangi-poor K. Sero epidemiology of HIV, HBV, HCV and Syphilis among hospitalized IDUs in Loghman-Hakim hospital. Iran J Med Microbiol. 2007;1:53–6.
Amini S, Andalibi MS, Lamian S, Joulaei M, Mahmoudi FM. Prevalence of hepatitis G virus (HGV) in high-risk groups and blood donors in Tehran, Iran. Iran J Public Health. 2005.
Alizadeh AHM, Alavian SM, Jafari K, Yazdi N. Prevalence of hepatitis C virus infection and its related risk factors in drug abuser prisoners in Hamedan-Iran. World J Gastroenterol WJG. 2005;11(26):4085.
Alipour A, Haghdoost AA, Sajadi L, Zolala F. HIV prevalence and related risk behaviours among female partners of male injecting drugs users in Iran: results of a bio-behavioural survey, 2010. Sex Transm Infect. 2013;89(Suppl 3):iii41–4.
Alavi SM, Etemadi A. HIV/HBV, HIV/HCV and HIV/HTLV-1 co infection among injecting drug user patients hospitalized at the infectious disease ward of a training hospital in Iran. Pak J Med Sci. 2007;23(4):510.
Alavi SM, Alavi L. Seroprevalence study of HCV among hospitalized intravenous drug users in Ahvaz, Iran (2001–2006). J Infect Public Health. 2009;2(1):47–51.
Alam-Mehrjerdi Z, Moradi A, Xu F, Zarghami M, Salehi-Fadardi J, Dolan K. Willingness to receive treatment for hepatitis C among injecting drug users on methadone program: implications for education and treatment. Addict Health. 2016;8(2):90.
Alam Mehrjerdi Z, Abarashi Z, Noroozi A, Arshad L, Zarghami M. Correlates of shared methamphetamine injection among methamphetamine-injecting treatment seekers: the first report from Iran. Int J STD AIDS. 2014a;25(6):420–7.
Alter MJ, editor HCV routes of transmission: what goes around comes around. Seminars in liver disease; 2011: © Thieme Medical Publishers.
Rashti R, Sharafi H, Alavian SM, Moradi Y, Mohamadi Bolbanabad A, Moradi G. Systematic review and meta-analysis of global prevalence of HBsAg and HIV and HCV antibodies among people who inject drugs and female sex workers. Pathogens. 2020;9(6):432.
Aceijas C, Rhodes T. Global estimates of prevalence of HCV infection among injecting drug users. Int J Drug Policy. 2007;18(5):352–8.
Scheibe A, Young K, Moses L, Basson RL, Versfeld A, Spearman CW, et al. Understanding hepatitis B, hepatitis C and HIV among people who inject drugs in South Africa: findings from a three-city cross-sectional survey. Harm Reduct J. 2019;16(1):28.
Altawalah H, Essa S, Ezzikouri S, Al-Nakib W. Hepatitis B virus, hepatitis C virus and human immunodeficiency virus infections among people who inject drugs in Kuwait: a cross-sectional study. Sci Rep. 2019;9(1):1–5.
Alibrahim OA, Misau YA, Alkali Mohammed MBF, Izzeldin S. Prevalence of hepatitis C viral infection among injecting drug users in a Saudi Arabian hospital: a point cross sectional survey. J Public Health Africa. 2018;9(1):726.
Silva MBS, Andrade TM, Silva LK, Rodart IF, Lopes GB, Carmo T, et al. Prevalence and genotypes of hepatitis C virus among injecting drug users from Salvador-BA, Brazil. Mem Inst Oswaldo Cruz. 2010;105(3):299–303.
Millman AJ, Nelson NP, Vellozzi C. Hepatitis C: Review of the epidemiology, clinical care, and continued challenges in the direct-acting antiviral era. Curr Epidemiol Rep. 2017;4(2):174–85.
Granados-García V, Flores YN, Díaz-Trejo LI, Méndez-Sánchez L, Liu S, Salinas-Escudero G, et al. Estimating the prevalence of hepatitis C among intravenous drug users in upper middle income countries: A systematic review and meta-analysis. PLoS ONE. 2019;14(2):e0212558.
Grassi A, Ballardini G. Hepatitis C in injection drug users: it is time to treat. World J Gastroenterol. 2017;23(20):3569.
Matthews G, Kronborg IJ, Dore GJ. Treatment for hepatitis C virus infection among current injection drug users in Australia. Clin Infect Dis. 2005;40(Supplement_5):S325–9.
Health UDo, Services H. Action plan for the prevention, care, & treatment of viral hepatitis. 2014. 2017.
Rothman KJ, Greenland S, Lash TL. Modern epidemiology: Wolters Kluwer Health/Lippincott Williams & Wilkins Philadelphia; 2008.
Mehrpour O. Methamphetamin abuse a new concern in Iran. DARU J Pharm Sci. 2012;20(1):73.
Shariatirad S, Maarefvand M, Ekhtiari H. Emergence of a methamphetamine crisis in Iran. Drug Alcohol Rev. 2013;32(2):223.
Amin-Esmaeili M, Rahimi-Movaghar A, Sharifi V, Hajebi A, Radgoodarzi R, Mojtabai R, et al. Epidemiology of illicit drug use disorders in Iran: prevalence, correlates, comorbidity and service utilization results from the Iranian Mental Health Survey. Addiction. 2016;111(10):1836–47.
Alam Mehrjerdi Z, Abarashi Z, Noroozi A, Arshad L, Zarghami M. Correlates of shared methamphetamine injection among methamphetamine-injecting treatment seekers: the first report from Iran. Int J STD. 2014b;25(6):420–7.
Bagheri N, Mirzaee M, Jahani Y, Karamouzian M, Sharifi H. Correlates of methamphetamine use among young Iranians: findings of a population-based survey in 2013. Am J Addict. 2017;26(7):731–7.
Sharifi H, Mirzazadeh A, Shokoohi M, Karamouzian M, Khajehkazemi R, Navadeh S, et al. Estimation of HIV incidence and its trend in three key populations in Iran. PLoS ONE. 2018;13(11):e0207681.
Alavian SM, Mirahmadizadeh A, Javanbakht M, Keshtkaran A, Heidari A, Mashayekhi A, et al. Effectiveness of methadone maintenance treatment in prevention of hepatitis C virus transmission among injecting drug users. Hepat Mon. 2013;13(8):e12411.
Platt L, Minozzi S, Reed J, Vickerman P, Hagan H, French C, et al. Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database Syst Rev. 2017;9(9):CD012021.
Platt L, Ward Z, Guiness L, Hickman M, Hope V. Assessing the impact and cost-effectiveness of needle/syringe provision and opiate substitution therapy on hepatitis C transmission among people who inject drugs in the United Kingdom: analysis of pooled datasets and economic modelling. Public Health Res. 2017;5(5):1–118.
Javanbakht M, Mirahmadizadeh A, Mashayekhi A. The long-term effectiveness of methadone maintenance treatment in prevention of hepatitis C virus among illicit drug users: a modeling study. Iran Red Crescent Med J. 2014;16(2):e13484.
Rahimi J, Gholami J, Amin‐Esmaeili M, Fotouhi A, Rafiemanesh H, Shadloo B, et al. HIV prevalence among People Who Inject Drugs (PWID) and related factors in Iran: a systematic review, meta‐analysis and trend analysis. Addiction. 2019.
Bao Y, Larney S, Peacock A, Colledge S, Grebely J, Hickman M, et al. Prevalence of HIV, HCV and HBV infection and sociodemographic characteristics of people who inject drugs in China: a systematic review and meta-analysis. Int J Drug Policy. 2019;70:87–93.
M. M. Prevalence of HIV, hepatitis B and C among drug abusers admitted to ICU of Baharloo hospital in 2010 [Ph.D. Thesis of Forensic Medicine]: Tehran: University of Medical Sciences; 2012.
Acknowledgements
Not applicable.
Funding
This systematic review was supported by Baqiyatallah Research Center for Gastroenterology and Liver Diseases, Baqiyatallah University of Medical Sciences (Grant Numbers 97-02-002272).
Author information
Authors and Affiliations
Contributions
SMA, HS, and AR designed the study protocol. AR and HS independently performed the literature searches and extraction of data. AR performed the statistical analysis. All authors contributed to the interpretation of data. AR and HS drafted the manuscript. All authors confirmed that they meet the ICMJE criteria for authorship. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1

Appendix 2

Appendix 3
See Fig. 8.
Appendix 4
See Fig. 9.
Appendix 5
See Fig. 10.
Appendix 6
See Fig. 11.
Appendix 7
See Fig. 12.
Appendix 8
See Fig. 13.
Appendix 9
See Fig. 14.
Trend of HCV Ab prevalence among PWID in Iran by recruitment setting. a Trend of HCV Ab prevalence among PWID in the prison setting, the Cochran–Armitage test, P value = 0.17. b Trend of HCV Ab prevalence among PWID in the hospital/healthcare center setting, the Cochran–Armitage test, P value < 0.001. c Trend of HCV Ab prevalence among PWID in the DIC setting, the Cochran–Armitage test, P value = 0.01
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rajabi, A., Sharafi, H. & Alavian, S.M. Harm reduction program and hepatitis C prevalence in people who inject drugs (PWID) in Iran: an updated systematic review and cumulative meta-analysis. Harm Reduct J 18, 12 (2021). https://doi.org/10.1186/s12954-020-00441-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12954-020-00441-9