Abstract
Background
People who inject drugs (PWID) are at high risk for hepatitis C (HCV), hepatitis B (HBV) and HIV without accessible harm reduction programmes. Coverage of needle and syringe and opioid substitution therapy (OST) services in South Africa is below global recommendations and no hepatitis services exist for PWID. We assessed HCV, HBV and HIV prevalence and risk factors among PWID accessing harm reduction services in Cape Town, Durban and Pretoria to inform policy and programming.
Methods
We conducted a cross-sectional survey among PWID in these cities between August 2016 and October 2017. Participants were opportunistically sampled while accessing services. Study team members administered a questionnaire that assessed sociodemographic characteristics, drug use and sexual risk practices. We tested for HCV (antibody, viral load and genotype), HBV surface antigen (HBsAg) and HIV. Bivariate and multivariate analyses assessed associations with HCV serostatus.
Results
Nine hundred and forty-three PWID were included in the per protocol analysis. The majority (87%, 819/943) were male, the overall median age was 29 and most lived on the street (66%, 626/943). At last injection, 77% (722/943) reported using a new needle and syringe and 17% (163/943) shared equipment. HIV prevalence was 21% (196/926), HBsAg positivity 5% (47/936), HCV seroprevalence 55% (513/937), HCV viraemic prevalence (proportion tested with detectable HCV) 43% (404/937) and HCV viraemic rate (proportion HCV antibody positive with detectable HCV) 79% (404/513). HCV genotype 1a (73%, 270/368) was the most prevalent. In multivariate analysis, HCV infection was positively associated with residing in Pretoria (adjusted odds ratio (aOR) 1.27, 95% CI 1.21–1.34), living on the street (aOR 1.90, 95% CI 1.38–2.60), frequent injecting (aOR 1.58, 95% CI 1.15–2.16) and HIV infection (aOR 1.69, 95% CI 1.15–2.47), and negatively associated with black race (aOR 0.52, 95% CI 0.36–0.74) and sexual activity in the previous month (aOR 0.61, 95% CI 0.42–0.88).
Conclusions
HCV and HIV are major health threats affecting PWID in these cities. Access to OST and needle and syringe services needs to be increased and integrated with HCV services. Social and structural factors affecting PWID who live on the street need to be addressed.
Similar content being viewed by others
Background
Globally, viral hepatitis is responsible for the deaths of approximately 1.34 million people every year, similar to the annual number of deaths from HIV/AIDS (1.3 million), malaria (0.9 million) and tuberculosis (1.3 million) [1,2,3]. In sub-Saharan Africa, approximately 60 million people are chronically infected with the hepatitis B virus (HBV) and 10.2 million people are chronically infected with hepatitis C virus (HCV) [1]. The region remains an epicentre for HIV with 25.7 million people living with HIV [2]. Most HBV infections occur in childhood through horizontal transmission, while most HIV infections occur during adolescence and adulthood through sexual contact [4,5,6]. Most HCV infections occur parenterally, through exposure to blood or unsafe medical practice [1, 5, 6]. People who inject drugs (PWID) who cannot access harm reduction services, specifically needle and syringe programmes and opioid substitution therapy (OST), are at particularly high risk of HCV, HIV and if non-immune, for HBV infection [7, 8]. In 1995, universal HBV vaccination was introduced in South Africa’s Expanded Programme of Immunisation [9]. Many current PWID in South Africa were born before this vaccine was introduced and hence a pool of chronic HBV remains, with HCV and HIV providing the bulk of new blood borne infections among PWID [9].
Screening for these infections includes the use of antibody and/or antigen tests, either point-of-care or laboratory-based. HIV confirmatory diagnosis in the sub-Saharan African context (a generalised HIV epidemic) usually involves a second, highly specific, rapid test from a different manufacturer [10]. A positive HBV surface antigen (HBsAg) is the marker for current infection, with further HBV serological assessment used to guide treatment. For HCV, confirmation of active viraemia is usually based on demonstrating HCV ribonucleic acid (RNA) on polymerase chain reaction (PCR) testing. Furthermore, HCV genotyping has until recently been performed to assess which of the six most frequent HCV genotypes is present to inform treatment choice. However, genotyping is not necessarily routinely required if pan-genotypic direct acting antivirals (DAAs) are available [8, 11].
Chronic HCV infection is associated with significant morbidity and mortality due to associated risks for cirrhosis and hepatocellular carcinoma [1]. Hepatitis C is readily treatable, and in most cases curable, with DAAs but access to therapy in South Africa is currently limited as these medications have yet to be registered, and a national viral hepatitis programme has yet to be fully implemented.
Viral hepatitis and HIV among people who inject drugs
In sub-Saharan Africa, there were an estimated 1.4 million (95% uncertainty interval [UI] 0.6–3.8 million) PWID aged 15–64 years in 2017. Opioids (mostly heroin) are the most commonly injected drug in the region (78%), followed by stimulants, including cocaine and methamphetamine (51%) [7]. The frequency and potential risks of injecting vary by type and quality of the substance used, access to OST, individual patterns of use and the severity of the substance use disorder [12].
The estimated HBsAg prevalence among PWID in sub-Saharan Africa is 4% (95% UI 2–6%); HCV seroprevalence 22% (95% UI 18–27%) and HIV 18% (95% UI 11–25%) [7].
In South Africa, as in many settings globally, people who use drugs are criminalised and face high levels of stigma and discrimination [13]. Access to harm reduction services is limited and almost exclusively provided by non-profit organisations. The first needle and syringe service in South Africa was established in Cape Town in 2012, focusing on men who have sex with men (MSM) [14]. In 2015, this service transitioned to a different service provider and was accessible to a wider range of PWID. In the same year, needle and syringe services were established in Durban and Pretoria [15] and small OST demonstration projects have been operating in these cities since 2017 [16]. To date, harm reduction services have focused on HIV risk reduction, with very little focus on HCV [13]. There are no accurate empirical estimates of the number of PWID in the country. Existing estimates based on data modelled from a national household survey are between 67,000 and 75,000 [17, 18] and PWID populations in Cape Town, Durban and Pretoria are estimated at 1517, 1245 and 4514, respectively [19]. Programmatic evidence indicates that the number of people injecting drugs is increasing [20].
HIV prevalence among PWID participating in a South African five city study in 2013 was 14% [21]. Data around HBV and HCV epidemiology among PWID in South Africa has been limited to programmatic data and small, single site studies. A private, not-for-profit health facility in Pretoria that screened 271 PWID in 2013/14 identified an HCV seroprevalence of 24% [22]. More recently, 27% of MSM that use drugs who participated in a study in Cape Town (n = 41) were HCV antibody positive. Among them, 80% had injected heroin or methamphetamine in the previous 3 months [14].
When this study was being planned, the South African National Department of Health (NDOH) was in the process of developing national viral hepatitis policy. However, PWID-focused hepatitis services were not included, largely due to limited local data.
This study aimed to assess the prevalence of HCV, HBV and HIV and their co-infections among PWID and related risk factors for HCV infection in three South African cities. It was also intended to provide key baseline information to inform national hepatitis policy and programming.
Methods
We planned to recruit 960 PWID (320 in Cape Town, Durban and Pretoria, respectively). This sample size was based on available resources. People who inject drugs were defined as people having injected a substance for non-therapeutic purposes, irrespective of the type of drug injected or the mode of injection, in the previous 12 months. All participants had to be 18 years or older. Data collection took place between August 2016 and October 2017.
Study activities were integrated into existing HIV prevention and sexual health services provided by non-profit organisations targeting PWID in these cities. MSM were recruited in a targeted sub-study at different sites looking into HBV, HCV and HIV prevalence and risks in that population. These results are not included here.
An overview of study procedures is provided in Fig. 1. Participants who provided written informed consent were administered a confidential health screening questionnaire that was completed in English and clarified in the appropriate language as needed by the peers/nurses administering it. The questionnaire solicited demographic information (age, sex, race and housing), substance use (substances used in previous month and injecting in last month, including injecting frequency, needle and syringe reuse and sharing), use of OST and sexual risk behaviour.
Consenting participants had 20 ml whole blood drawn. HIV, HBV and HCV point-of-care (POC) testing was performed and samples from all HCV POC reactive individuals were sent to the National Institute for Communicable Diseases (NICD) in Johannesburg for confirmatory HCV enzyme-linked immunosorbent assay (ELISA), HCV PCR confirmatory viral load testing and genotyping. POC HIV testing was done in line with national protocols using a serial testing strategy [10]. POC HBsAg and HCV testing was performed using the Determine™ HBsAg (Alere Inc., MA, USA) and OraQuick® HCV rapid antibody test (Orasure Technologies Inc., PA, USA), respectively. All samples that were sent to the laboratory were subjected to anti-HCV testing (ARCHITECT Anti-HCV assay) on the ARCHITECT i1000SR system following the manufacturer’s instructions (Abbott Laboratories, Diagnostics Division, IL, USA). Samples that tested antibody positive were tested quantitatively using the COBAS® AmpliPrep/COBAS® TaqMan® HCV Quantitative Test v2.0 on the COBAS® Ampliprep Taqman® Analyser (Roche Molecular Systems, CA, USA). For HCV genotyping, 10 μl of biotinylated PCR amplicon was applied to nitrocellulose strips using the Versant HCV genotyping 2.0 assay (LiPA, Innogenetics, Ghent, Belgium). Genotyping results were interpreted using the reading card over the strip and the reading chart provided in the assay.
Participants received counselling around viral hepatitis and were provided with condoms, lubricant, information and education material and sterile injecting equipment. Participants diagnosed with HIV were referred to HIV care services. Those with a positive HBsAg screening test were referred to a pre-identified health facility for work-up and assessment for treatment. Participants with a negative HBsAg POC test were offered HBV vaccination. Those with a positive HCV screening test were given a follow-up date to return to obtain the results of additional laboratory testing. At the follow-up visit, the study nurse provided further counselling and linkage to care was arranged for additional work up and management of HCV infection. This was either at a designated gastrointestinal or liver clinic, where these existed, or at a pre-identified district hospital, where specialised clinics did not exist.
Data analysis was performed using STATA 11.2 (Statacorp LLC, Texas, USA). Data was initially analysed using descriptive statistics, stratified by city and biological sex. POC seroprevalence was calculated for HIV, HBV and HCV based on number of reactive POCs divided by the number of PWID participants that were tested as per protocol. HCV viraemic prevalence was calculated by dividing the number of participants with detectable viral load over the number of eligible PWID participants who had a HCV POC test. The HCV viraemic rate was calculated by dividing the number of participants with detectable viral load over the number of HCV POC positives. Bivariate analysis was done between HCV antibody status (reactive/ non-reactive) and selected demographic, drug using and sexual risk factors. Age and frequency of injecting were categorised into binary variables based on their median value. HCV antibody status was the outcome of interest in multivariate analysis. The model was adjusted for biological sex, age, race, city, living on the street, injecting practices (frequency, new needle at last injection, sharing needle at last injection), sexual practices (sexually active in last month, condom use at last penile-vaginal sex) and HIV status.
The study was approved by the Human Research Ethics Committee of the University of Cape Town (ref: 004/2016), the Research Ethics Committee of the University of the Witwatersrand (ref: M160510) and the Western Cape (ref: WC_2016RP19_818) and KwaZulu-Natal (ref: KZN_2016RP59_986) Provincial Department of Health Ethics Committees. Participants were not remunerated for their participation.
Results
Sociodemographics
Nine hundred and forty-three PWID were included in the per protocol analysis. The majority (87%, 819/943) were male, the median age was 29 and most were black (41%, 388/943) and living on the street (66%, 626/943). Demographic characteristics among PWID participants were similar across the three cities, apart from proportionately more people of mixed ancestry and fewer black participants in Cape Town than in the other sites, and a higher proportion of PWID living on the street in Durban (Table 1).
Substance use
The most frequently reported illegal substance used in the previous month was heroin (86%, 811/943). Methamphetamine or amphetamine-type stimulants (ATS) were the second most commonly used type of drug (28%, 262/943), with notably higher frequency of use in Cape Town compared to the other cities. Almost all (94%, 886/943) the participants had injected heroin in the previous month. Two-thirds (69%, 649/943) of all participants reported injecting any drug four or more times per day. At their last injection, most participants (77%, 722/943) reported using a new needle and syringe. A fifth (17%, 163/943) reported sharing needles at their last injection. Five percent (43/943) of participants had been on OST for at least 30 days at the time of the study (Table 2).
Sexual risk practices
Forty-three percent (410/943) of the participants reported sexual activity in the previous month; higher among females (62%, 77/124) than males (41%, 333/819). Females and males reported similar numbers of sexual partners in the last week (median of 1, IQR 1–2 for females and median of 1, IQR 0–1 for males). Seven participants (four males, three females) reported receptive anal intercourse in the previous month. About half (52%, 212/410) of the participants reported condom use at last penile-vaginal sex, and 6% (24/410) reported exchanging drugs or goods for sex (13 males and 11 females). Thirty-eight percent of males (127/333) and 49% of females (38/77) reported alcohol or other substance use during their last sexual encounter, which was notably lower in Durban compared to the other cities (Table 3).
Testing results
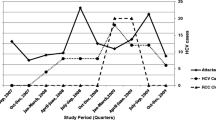
Details of the testing results are provided in Table 4. A fifth of the participants (20%, 188/926) had their first HIV test as part of this study. HIV prevalence was 21% (196/926); 26% (31/119) among females and 20% (165/807) among males. HIV prevalence ranged from 7% (20/290) in Cape Town to 38% (122/319) in Pretoria. HIV prevalence was similar between male and female participants in Cape Town and Pretoria, with notably higher HIV prevalence among females than males in Durban (39%, 12/31 versus 15%, 42/286). HBsAg positivity was 5% (47/936); 5% (43/814) among males and 3% (4/122) among females, and similar across cities. Overall, anti-HCV positivity was 55% (513/937). HCV RNA was detected in 404 of the 513 participants who were anti-HCv positive yielding a viraemic rate of 79%. There was however marked variation in the HCV viraemic prevalence across cities, ranging from 35% in Durban, 44% in Cape Town to 84% in Pretoria. Overall, 12% (113/926) were HCV-HIV co-infected, 2% (21/936) HCV-HBV co-infected, 2% (14/925) HIV-HBV co-infected and eight participants were HCV-HBV-HIV triple-infected.
HCV genotyping was possible on 96% (386/401) of the samples with detectable viral load. The most prevalent HCV genotypes were 1a (66%), 3a (14%), 3 (3%) and 1 (3%). Significantly, no genotype 5 was detected.
Bivariate and multivariate analysis
The results from the bivariate and multivariate analysis are shown in Table 5. In bivariate analysis, positive HCV seroprevalence was positively associated with residing in Pretoria (OR 1.26, 95% CI 1.21–1.32, p < 0.001), living on the street (OR 1.59, 95% CI 1.21–2.09, p = 0.001) and injecting four or more times per day (OR 1.67, 95% CI 1.25–2.19, p < 0.001). HCV infection was negatively associated with the use of new injecting equipment at last injection (OR 0.70, 95% CI 0.51–0.94, p = 0.020), sexual activity in the last month (OR 0.40, 95% CI 0.31–0.52, p < 0.001) and condom use at last penile-vaginal sex (OR 0.48, 95% CI 0.35–0.65, p < 0.001).
The frequency of injecting among men was significantly lower among those who were sexually active compared to men who had not been sexually active in the previous month (OR 0.58, 95% CI 0.43–0.79, p < 0.001). Furthermore, men who were sexually active were more likely to have used a new needle and syringe the last time they injected compared to men who were not sexually active (OR 1.47, 95% CI 1.05–2.06, p = 0.024). Drug using risk practices among women were similar to those among men when analysed in relation to their sexual activity in the last month.
In multivariate analysis, positive HCV serostatus was positively associated with residing in Pretoria (aOR 1.27, 95% CI 1.21–1.34, p < 0.001), living on the street (aOR 1.90, 95% CI 1.38–2.60, p < 0.001), frequent injecting (aOR 1.58, 95% CI 1.15–2.16, p = 0.005) and being HIV infected (aOR 1.69, 95% CI 1.15–2.47, p = 0.008), and negatively associated with black race (aOR 0.52, 95% CI 0.36–0.74, p < 0.001) and being sexually active in the previous month (aOR 0.61, 95% CI 0.42–0.88, p = 0.008).
Discussion
This is the largest published quantitative study of HBV, HCV and HIV among PWID in South Africa to date. The study demonstrates a significantly higher prevalence of HCV infection among PWID (43%) than previously known [23]. Notably, HCV prevalence among PWID in Pretoria was substantially higher than in other cities. This study did not explore the reasons for this geographical variation. However, expert consultation in other settings has suggested that injecting practices as a drug using culture have been in existence for longer in Pretoria than other cities, potentially suggesting a reason for this finding [24].
A large proportion of the participants lived on the street, accounted for by the recruitment of participants through existing harm reduction services that target people from lower socio-economic circumstances. People who live on the street often have limited financial resources to purchase injecting equipment, contributing to the increased likelihood of reuse, sharing and use of contaminated injecting equipment [25]. People living on South African streets who use drugs have little or no access to private spaces to do so, and frequently experience human rights violations, including assault, confiscation of possessions (including injecting equipment) and being moved [26,27,28]. Consequently, conditions for safe injecting are limited. The multivariate analysis found an increased likelihood of HCV infection among people living on the street, reinforcing the importance of addressing social and structural factors to enhance HIV and HCV health outcomes.
The study found that HCV risk is positively associated with increased injection frequency. This is supported by the per injection risk without 100% access to sterile injecting equipment [29]. The high level of reported use of new needles is surprising, and may reflect a social desirability bias, considering that the majority of people inject four or more times a day and access to sterile injecting equipment is limited. Existing harm reduction services in these cities distribute between 10 and 14 sterile needles and syringes at each encounter with a PWID client, with these projects aiming to visit locations where PWID are provided with services once or twice a week.Footnote 1 An assessment of needle and syringe service coverage in Pretoria and Cape Town was completed in 2017 and results are forthcoming [24]. The reported levels of needle and syringe sharing highlight the need for increased saturation of needle and syringe services.
Overall, few PWID (5% of the sample) had access to OST in these cities, which is to be expected as OST remains in the pilot stages [16]. It is also unclear if the reported OST access was sustained or over limited periods and if the dosage was aligned to global recommendations [8].
High coverage of OST and needle and syringe services can reduce the risk of HCV infection by 74% [30]. Modelling data from Kenya (PWID population of 50,000 with HCV prevalence of 11%) shows that providing 75% needle and syringe coverage and 50% OST would reduce the risk of HCV incidence among PWID by 69% by 2030, and elimination targets would be reached through the addition of treating chronic HCV infections among 1000 PWID over 5 years [31].
This research confirmed the findings of a previous study that documented elevated HIV prevalence among PWID compared to the general population [21]. In multivariate analysis, HIV infection is significantly associated with HCV serostatus, highlighting the shared transmission routes of these viruses and the need to integrate viral hepatitis and HIV services for PWID. The study also documents HBsAg prevalence similar to the general population [4]. While a relatively small proportion of people were found to be co-infected with HBV/HCV/HIV, the added morbidity and mortality requires that co-infection remains an important area for consideration. The relative exclusive prevalence of HCV genotypes 1a and 3a is similar to that in other countries where HCV infection is predominantly spread through sharing contaminated injecting equipment among PWID [32, 33]. However, of note in South Africa, genotype 5a (a predominant genotype in patients with liver disease [34]) was not found among PWID and suggests that 5a circulates in the general population and not in PWID.
Participants in this study were recruited from among those who currently access or who were reachable to organisations implementing harm reduction services, specifically mobile needle and syringe distribution and collection services in these cities. Unsurprisingly, the participants were overwhelmingly male given that globally, a higher proportion of PWID are male compared to female, with the proportion of female PWID ranging from 3% in South Asia to 33% in Australasia, and 12% in sub-Saharan Africa [7]. Programmatic data from the services that operate in these cities reflects that between 10 and 13% of service users are women [35]. While this is possibly due to higher numbers of men who inject drugs than women in South Africa, it also likely reflects barriers preventing women who inject drugs from accessing harm reduction services—including stigma, discrimination and services that do not address their specific needs [36]. Previous studies among South African and African PWID also included a smaller proportion of women who inject drugs [21, 37]; however, globally, a higher proportion of women who inject drugs are reached [38]. Nevertheless, there is global [39] and sub-Saharan [40] recognition of the need for gender-appropriate and specific HIV and HCV services for women who inject drugs due to their specific needs.
A diverse cross-section of South African racial groups was recruited across sites, indicating that substance use and injecting practices are issues affecting people across race or ethnicity. The relative order of the size of racial groups in the study sites reflected the demographic characteristics of the relevant cities [41]. However, the relative over-representation of white PWID remains (27% of the sample, versus 8% of the general population) [41]. It is not clear from this study if there are relatively more white PWID or if this is due to selection bias. Most of the study sites where centrally located in areas where PWID congregate. Non-white PWID living in poorer, peripheral areas of the city may have not been reached by existing harm reduction services and therefore not recruited in the study. There is no published evidence supporting different levels of stigma around injecting drug use among different racial groups in these cities, but this may also have been a factor. It is also unclear why lower HCV risk was found among black PWID. Data was not collected on length of participant injecting history, so no analysis can be made on associations between injecting history and race groups as a proxy for other factors.
The findings from this study around substance use reflect substance use treatment data that shows the prevalence of poly drug use in South Africa and different usage patterns across the country [35]. Study and treatment data point to heroin being the most commonly injected drug, and methamphetamine/ATS injecting being highest in Cape Town.
Proportionately more women than men reported sexual activity in the previous month and condom use was similarly sub-optimal. More women than men reported transactional sex for drugs, which has previously been identified among women who inject in South Africa [21].
Interestingly, men who reported recent sexual activity showed lower risk drug use practices than their counterparts who did not report being sexually active. This may be because higher frequency of opioid use is associated with reduced libido, and can induce impotence among men [42]. It may therefore be that men engaging in regular sexual activity are those using less opioids, and are therefore able to exercise greater care with each instance of injection. It may also be that sexual activity is indicative of the existence of intimate partnerships that impact on risky injecting behaviours. While intimate couples who inject drugs together often engage in needle sharing and higher risk injecting practices within the couple [43], there is also increasing evidence that drug use tends to lessen when people have close social relationships and that couples set negotiated standards and limits to such use [44]. This can include agreements about where, when, how, and with whom drugs are injected [45]. Furthermore, concerns for placing primary sexual partners at risk of infectious diseases may contribute to safer injecting [13]. These limits on injecting behaviour in intimate relationships may be some of the reasons that recent sexual activity was found to be generally protective against HCV infection.
Limitations
The opportunistic nature of the sampling method prevents extrapolation to larger PWID populations in these cities and beyond. However, the findings confirm previous local studies and global experience. Information bias may have influenced the reliability of measures assessing substance use and sexual activity (including under reporting of anal sex and exchange of sex for drugs and/or goods). The low frequency of reported alcohol or substance use at the time of sex in Durban is suspected to be an underestimation, as other sexual risk practices were similar to the other cities. This difference could be attributable to several factors. One factor may have been due to differential solicitation of this question by study team members in Durban compared to the other cities. Another potential explanation is potential differences in social norms around discussing sexual practices among PWID in the various cities; however, there is no published evidence supporting this. The researchers were experienced in working with PWID so PWID were likely to feel safe in participation; however, the reporting of favourable (less risky) practices may have been encouraged by the fact that participants were engaging with the same people who provided harm reduction services. This may have resulted in underestimation of HCV risks and over-estimation of access to and use of needle and syringe services.
Conclusions
HCV, and to a lesser extent HIV, are major health threats affecting PWID in South Africa. On-going high risk practices are influenced by limited access to OST and needle and syringe services, as well as the social and structural factors affecting PWID who live on the street in the context of criminalisation of people who use drugs. Furthermore, in the absence of HCV treatment, an increase in HCV infections is inevitable without a rapid, targeted response that is appropriate and acceptable to PWID. Programmatic responses should also focus on prioritising treatment within Pretoria where HCV and HIV prevalence is highest, with intensified prevention messaging in that city. However, hepatitis awareness and prevention activities need to be up-scaled in other cities where HCV prevalence has not yet reached such high proportions.
Intensified efforts are needed to reach and provide services to women who inject drugs and to ensure that these services are inclusive of their sexual and reproductive health needs. Tailored outreach and viral hepatitis testing and treatment services, facilitated by gender appropriate teams should be considered as services scale up.
Broader social issues related to living conditions and social isolation need to be considered in holistic responses to HCV and HIV infection among PWID in these cities. Interventions that address structural issues that may be contributing to the elevated HCV risk among PWID living on the street are needed, which are not limited to exploration of safe injecting facilities, and enhanced support from law enforcement for needle and syringe services.
This study was limited to a description of HCV, HBV and HIV among PWID in these cities that have (potential) access to harm reduction services. Additional research is needed on the epidemiology of these infections among PWID in other South African contexts (urban and rural), as well as within the correctional services system. Greater insights are also needed into factors associated with on-going parenteral risk in the presence of harm reduction services. Models that explore innovative ways to provide integrated HCV-HBV-HIV and other holistic services to PWID in the South African context are needed to inform the granular detail and implementation experience that will be necessary for an effective HCV response. Future research is needed to understand health care providers’ knowledge around viral hepatitis and HIV among PWID.
Eliminating viral hepatitis as a public health threat in South Africa by 2030 will only be an attainable reality once hepatitis prevention, testing and treatment services are provided to all PWID as needed. Services will need to include access to sterile injecting equipment, OST and HIV and HCV testing and treatment. Like many other counties, South Africa has the guidelines and a national action plan to address this issue, but political support, appropriate resource allocation and dedicated and passionate people that include the PWID community will be required to support implementation and reach this ambitious goal.
Notes
Personal communication with Andrea Schneider, Step Up Project national coordinator (4 December 2018).
Abbreviations
- AIDS:
-
Acquired immunodeficiency syndrome
- aOR:
-
Adjusted odds ration
- ATS:
-
Amphetamine-type stimulants
- CI:
-
Confidence interval
- CPT:
-
Cape Town
- DAA:
-
Direct acting antiviral
- DBN:
-
Durban
- ELISA:
-
Enzyme-linked immunosorbent assay
- HBsAg:
-
HBV surface antigen
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- HIV:
-
Human immunodeficiency virus
- MSM:
-
Men who have sex with men
- NDOH:
-
South African National Department of Health
- NICD:
-
National Institute for Communicable Diseases
- OST:
-
Opioid substitution therapy
- PCR:
-
Polymerase chain reaction
- POC:
-
Point-of-care
- PTA:
-
Pretoria
- PWID:
-
People who inject drugs
- RNA:
-
Ribonucleic acid
- UI:
-
Uncertainty interval
- WHO:
-
World Health Organisation
References
World Health Organization. Global hepatitis report, 2017. Geneva: WHO; 2017. Available from: https://apps.who.int/iris/bitstream/handle/10665/255016/9789241565455-eng.pdf;jsessionid=47CAD7FA53D5A32ED4FC61E568F7E958?sequence=1.
UNAIDS. Fact sheet—world AIDS day 2018. Geneva: UNAIDS; 2018.
Dalal S, Beunza JJ, Volmink J, Adebamowo C, Bajunirwe F, Njelekela M, et al. Non-communicable diseases in sub-Saharan Africa: what we know now. Int J Epidemiol. 2011;40:885–901. Available from: https://doi.org/10.1093/ije/dyr050. [cited 2011 Aug 30].
Spearman CW, Afihene M, Ally R, Apica B, Awuku Y, Cunha L, et al. Hepatitis B in sub-Saharan Africa: strategies to achieve the 2030 elimination targets. Lancet Gastroenterol Hepatol. 2017;2:2121 Available from: https://doi.org/10.1016/S2468-1253(17)30295-9.
Barth RE, Huijgen Q, Taljaard J, Hoepelman AIM. Hepatitis B/C and HIV in sub-Saharan Africa: an association between highly prevalent infectious diseases. A systematic review and meta-analysis. Int J Infect Dis. 2010;14:e1024–31 Available from: https://doi.org/10.1016/j.ijid.2010.06.013.
Matthews PC, Maria A, Goulder PJR, Klenerman P. Epidemiology and impact of HIV coinfection with hepatitis B and Hepatitis C viruses in sub-Saharan Africa. J Clin Virol. 2014;61:20–33 Available from: https://doi.org/10.1016/j.jcv.2014.05.018.
Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health; 2017;5:e1192–e1207. Available from: https://doi.org/10.1016/S2214-109X(17)30375-3. The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY-NC-ND 4.0 license
World Health Organization (WHO). Guidelines for the care and treatment of persons diagnosed with chronic hepatitis c virus infection. Geneva: WHO; 2018.
Burnett RJ, Kramvis A, Dochez C, Meheus A. An update after 16 years of hepatitis B vaccination in South Africa. Vaccine. 2012;30:C45–51. Available from: https://doi.org/10.1016/j.vaccine.2012.02.021.
World Health Organization. Consolidated guidelines on HIV testing services. Geneva: WHO; 2015.
World Health Organization. Guidelines on hepatitis B and C testing. Geneva: WHO; 2017. Available from: https://apps.who.int/iris/bitstream/handle/10665/254621/9789241549981-eng.pdf?sequence=1.
Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, et al. HIV and risk environment for injecting drug users: the past, present, and future. Lancet. 2010;376:268–84. Available from: https://doi.org/10.1016/S0140-6736(10)60743-X. [cited 2012 Mar 9].
Scheibe A, Shelly S, Versfeld A, Howell S, Marks M. Safe treatment and treatment of safety: call for a harm-reduction approach to drug-use disorders in South Africa. South African Heal Rev. 2017;20:197–204.
Semugoma NP, Rebe K, Sonderup MW, Kamkeumah M, De Swardt G, Struthers H, et al. Hepatitis C: a South African literature review and results from a burden of disease study among a cohort of drug-using men who have sex with men in Cape Town, South Africa. S Afr Med J. 2017;107:1116–20.
Scheibe A, Shelly S, Lambert A, Schneider A, Basson R, Medeiros N, et al. Using a programmatic mapping approach to plan for HIV prevention and harm reduction interventions for people who inject drugs in three South African cities. Harm Reduct J. Harm Reduct J. 2017;14:35. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5463380/pdf/12954_2017_Article_164.pdf.
Scheibe A, Marks M, Shelly S, Gerardy T, Domingo A, Hugo J. Developing an advocacy agenda for increasing access to opioid substitution therapy as part of comprehensive services for people who use drugs in South Africa, vol. 108; 2018. p. 800–2.
Petersen Z, Myers B, van Hout M-C, Plüddemann A, Parry C. Availability of HIV prevention and treatment services for people who inject drugs: findings from 21 countries. Harm Reduct J. 2013;10:13. Available from: https://harmreductionjournal.biomedcentral.com/articles/10.1186/1477-7517-10-13. [cited 2013 Aug 26].
UNAIDS. Do no harm. Health, human rights and people who use drugs. Report. Geneva: UNAIDS; 2016. Available from: http://www.unaids.org/sites/default/files/media_asset/donoharm_en.pdf.
South African National AIDS Council: Key Populations Cascades Stakeholder Group. 2018. Report of the South African Key Populations Cascades Stakeholder Group Workshop. Summary and Recommendations from February 2018 workshop. Pretoria: SANAC; 2018.
South African Medical Research Council. South African community epidemiology network on drug use. SACENDU reports 1998 - 2016. Available from: http://www.mrc.ac.za/intramural-research-units/ATOD-sacendu. Accessed 1 Sept 2018.
Scheibe A, Makapela D, Brown B, Santos M, Hariga F, Virk H. HIV prevalence and risk among people who inject drugs in five South African cities. Int J Drug Policy. 2016;30:107 Available from: https://doi.org/10.1016/j.drugpo.2016.01.004.
Sediba Hope Medical Centre. Viral hepatitis sceening. Pretoria: Sediba Hope Medical Centre; 2013.
Sonderup MW, Afihene M, Ally R, Apica B, Awuku Y, Cunha L, et al. Hepatitis C in sub-Saharan Africa: the current status and recommendations for achieving elimination by 2030. Lancet Gastroenterol Hepatol. 2017;2:910–9 Available from: https://doi.org/10.1016/S2468-1253(17)30249-2.
South African National AIDS Council (SANAC). Key Populations Cascade Stakeholder Group. Reports of the South African key populations stakeholder group workshop: February 2018. Pretoria: SANAC; 2018.
Linton SL, Celentano DD, Kirk GD, Mehta SH. The longitudinal association between homelessness, injection drug use, and injection-related risk behavior among persons with a history of injection drug use in Baltimore, MD. Drug Alcohol Depend. 2013;132:457–65. Available from: https://doi.org/10.1016/j.drugalcdep.2013.03.009.
Shelly S, Broughton I, Mcbide A, van Hofmeyer Z, Medeiros N, van Staden C, et al. Every single person looks at us bad. Cape Town: South African Network of People Who Use Drugs; 2017. p. 1–43.
TB HIV Care Association. Step Up Project. Human rights violations report 2017. Cape Town: TB HIV Care Association; 2017. Available from: http://www.stepupprojectsouthafrica.org/
Scheibe A, Lambert A, Schneider A, Shelly S, Basson R, Medeiros N, et al. Using programmatic mapping to identify locations where people who inject drugs congregate and to estimate their population sizes in three South African cities. In: 21st International AIDS Conference. Poster Presentation THPEES90. Durban: IAS; 2016.
Abdul-Quader AS, Feelemyer J, Modi S, Stein ES, Briceno A, Semaan S, Horvath T, Kennedy GE, Des Jarlais DC. Effectiveness of Structural-Level Needle/Syringe Programs to Reduce HCV and HIV Infection Among People Who Inject Drugs: A Systematic Review. AIDS Behav. 2013;17(9):2878-92. http://chipts.ucla.edu/wp-content/uploads/2015/07/Effectiveness-of-Structural-Level-Needle-Syringe-Programs-to-Reduce-HCV-and-HIV-Infection-Among-People-Who-Inject-Drugs-A-Systematic-Review.pdf.
Platt L, Minozzi S, Reed J, Vickerman P, Hagan H, French C, et al. Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database Syst Rev. 2017;2017:CD012021. Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012021.pub2/full.
Vickerman P, Stone J, Walker J. Kenya the impact of prevention and treatment interentions for PWID in East Africa. Presentation. Brisol: University of Brisol; 2018.
Wiessing L, Ferri M, Grady B, Kantzanou M, Sperle I, Cullen KJ, et al. Hepatitis C virus infection epidemiology among people who inject drugs in Europe: a systematic review of data for scaling up treatment and prevention. Khudyakov YE, editor. PLoS One. 2014;9:e103345. Available from: https://doi.org/10.1371/journal.pone.0103345.
Robaeys G, Bielen R, Azar DG, Razavi H, Nevens F. Global genotype distribution of hepatitis C viral infection among people who inject drugs. J Hepatol. European Association for the Study of the. Liver. 2016;65:1094–103 Available from: https://doi.org/10.1016/j.jhep.2016.07.042.
Prabdial-Sing N, Chirwa T, Thaver J, Smuts H, Vermeulen M, Suchard M, et al. Hepatitis C genotype distribution in patient and blood donor samples in South Africa for the period 2008-2012. J Viral Hepat. 2016;23:881–8. Available from: https://doi.org/10.1111/jvh.12571.
South African Community Epidemiology Network on Drug Use. Monitoring alcohol, tobaccoe and other drug use trends in South Africa. Phase 43. Cape Town: South African Medical Research Council; 2018. p. 1–68.
Versfeld A, Scheibe A, Shelly S, Wildschut J, Versfeld A, Scheibe A, et al. Empathic response and no need for perfection: reflections on harm reduction engagement in South Africa. Crit Public Health. 2018;1596:1–11 Available from: https://doi.org/10.1080/09581596.2018.1443204.
MEWA, Reach Out Trust, The Omari Project, Carriere M, Essink L. Women who use drugs in Kenya: the needs of female drug users. Amsterdam: Mainline; 2016.
Larney S, Peacock A, Leung J, Colledge S, Hickman M, Vickerman P, et al. Global, regional, and country-level coverage of interventions to prevent and manage HIV and hepatitis C among people who inject drugs: a systematic review. Lancet Glob Health. 2017;5:1–13. Available from: https://doi.org/10.1016/S2214-109X(17)30373-X. The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC BY-NC-ND 4.0 license.
Harris M, Rhodes T. Hepatitis C treatment access and uptake for people who inject drugs: a review mapping the role of social factors. Harm Reduct J. 2013;10:7. Available from: https://doi.org/10.1186/1477-7517-10-7.
Zamudio-Haas S, Mahenge B, Saleem H, Mbwambo J, Lambdin BH. Generating trust: programmatic strategies to reach women who inject drugs with harm reduction services in Dar es Salaam, Tanzania. Int J Drug Policy. 2016;30:43–51. Available from: https://doi.org/10.1016/j.drugpo.2016.01.012.
Statistics South Africa. Mid-year population estimates 2018. Pretoria: Statistics South Africa; 2018. Available from: https://www.statssa.gov.za/publications/P0302/P03022018.pdf.
Briand Madrid L, Morel S, Ndiaye K, Mezaache S, Rojas Castro D, Mora M, et al. Factors associated with perceived loss of libido in people who inject opioids: results from a community-based survey in France. Drug Alcohol Depend. 2018;190:121–7 Available from: https://doi.org/10.1016/j.drugalcdep.2018.05.030.
Morris MD, Evans J, Montgomery M, Yu M, Briceno A, Page K, et al. Intimate injection partnerships are at elevated risk of high-risk injecting: a multi-level longitudinal study of HCV-serodiscordant injection partnerships in San Francisco, CA. PLoS One. 2014;9:e109282.
Rance J, Rhodes T, Fraser S, Bryant J, Treloar C. Practices of partnership: negotiated safety among couples who inject drugs. Heal An Interdiscip J Soc Study Heal Illn Med. 2018;22:3–19. Available from: https://doi.org/10.1177/1363459316660859.
Morris MD, Bates A, Andrew E, Hahn J, Page K, Maher L. More than just someone to inject drugs with: injecting within primary injection partnerships. Drug Alcohol Depend. 2015;156:275–81. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4633359/pdf/nihms730583.pdf.
Acknowledgements
The authors would like to thank the study participants. Additional thanks go to Andrea Schneider, Kalvanya Padayachee, Dawie Nel, Nelson Medeiros, Angela MacBride, Yolaan Andrews and the teams that implemented the study. Implementation at TB HIV Care sites was possible through addition of this service to existing HIV prevention and testing services supported by the United States President’s Emergency Plan for AIDS Relief and the United States Centers for Disease Control and Prevention and the Global Fund. The authors further thank all the laboratory staff at the Centre for Vaccines and Immunology, Jayendrie Thaver, Lucinda Gaelejwe, Susan Malfeld, Lillian Makhathini and for the transport logistics and cost management, Angella Musisi.
Funding
Funding for the study was received from the Bristol-Myers Squibb Foundation. The funder was not involved in the design of the study, or the collection, analysis or interpretation of data.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
AS led protocol development, is involved in oversight of implementation, data analysis, development of drafts and incorporation of co-author inputs and finalisation of manuscript. KY is involved in oversight of implementation, input into drafts and review and approval of final manuscript. LM is involved in oversight of implementation, participation in data quality control and analysis, as well as input into drafts and review and approval of final manuscript. RLB is involved in oversight of implementation, input into data interpretation, input into drafts and review and approval of final manuscript. AV is involved in oversight of implementation, input into drafts and review and approval of final manuscript. CWS is involved in oversight of implementation, input into drafts and review and approval of final manuscript. MWS is involved in oversight of implementation, input into drafts and review and approval of final manuscript. NP-S is involved in oversight of the laboratory implementation, data quality control and analysis, input into drafts and review and approval of final manuscript. JM is involved in laboratory data quality control and analysis, input into drafts and review and approval of final manuscript. AP is involved in protocol development for diagnostics, diagnostic data review, draft review and final review. KR provided technical input into study design, data interpretation and review and approval of final manuscript. HH contributed to the design of the work, interpretation of data, input into drafts and review and approval of final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Human Research Ethics Committee of the University of Cape Town (ref: 004/2016), the Research Ethics Committee of the University of the Witwatersrand (ref: M160510) and the Western Cape (ref: WC_2016RP19_818) and KwaZulu-Natal (ref: KZN_2016RP59_986) Provincial Department of Health Ethics Committees. All participants provided written informed consent.
Consent for publication
Not applicable
Competing interests
AS: is a faculty member of the Bristol-Myers Squibb Foundation and has received an honorarium from Gilead Pharmaceuticals to present hepatitis prevalence data at a South African conference for HIV clinicians.
KY: No competing interests
LM: No competing interests
RB: No competing interests
AV: No competing interests
CWS: No competing interests
MS: No competing interests
KR: No completing interests
NPS: No competing interests
JM: No competing interests
AP: No competing interests
HH: No competing interests
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Scheibe, A., Young, K., Moses, L. et al. Understanding hepatitis B, hepatitis C and HIV among people who inject drugs in South Africa: findings from a three-city cross-sectional survey. Harm Reduct J 16, 28 (2019). https://doi.org/10.1186/s12954-019-0298-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12954-019-0298-2