Abstract
Background
Previous findings have revealed that disorders of lipid metabolism may be a risk factor for pulmonary function damage; however, the combined effect of dyslipidemia and central obesity on pulmonary function is unclear. The cardiometabolic index (CMI) is a composite of serum lipids (triglyceride (TG)/high-density lipoprotein cholesterol (HDL-C)) and visceral fat parameters (waist-to-height ratio (WHtR)). This research aimed to investigate the link between CMI and pulmonary function, employing large-scale demographic data sourced from the National Health and Nutrition Examination Survey (NHANES) database.
Methods
This cross-sectional study used data involving 4125 adults aged 20 and above collected by NHANES between 2007 and 2012. We defined CMI as the exposure variable and measured outcomes using forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and FEV1/FVC to evaluate pulmonary function. Weighted multiple linear regression models and subgroup analyses were employed to investigate separate relationships between CMI and pulmonary function. In addition, to investigate variations across different strata and evaluate the robustness of the findings, interaction tests and sensitivity analyses were conducted.
Results
Results from the weighted multiple linear regression analysis indicated a unit increase in log2-CMI was associated with a reduction of 82.63 mL in FEV1 and 112.92 mL in FVC. The negative association remained significant after transforming log2-CMI by quartile (Q). When the log2-CMI level reached Q4, β coefficients (β) were -128.49 (95% CI: -205.85, -51.13), -169.01 (95% CI: -266.72, -71.30), respectively. According to the interaction test findings, the negative association linking log2-CMI with FEV1 and FVC persists regardless of confounding factors including age, gender, BMI, physical activity (PA), and smoking status. A subsequent sensitivity analysis provided additional confirmation of the stability and reliability of the results. For females, the inflection points for the nonlinear relationships between log2-CMI and FEV1, as well as log2-CMI and FVC, were identified at 2.33 and 2.11, respectively. While in males, a consistent negative association was observed.
Conclusions
Our findings suggest that higher CMI is associated with lower FEV1 and FVC. CMI may serve as a complementary consideration to the assessment and management of pulmonary function in clinical practice.
Similar content being viewed by others
Introduction
The function of the lungs to ventilate and replace air provides important support for life activities. Spirometry is a widely utilized method for evaluating pulmonary function, with key indicators including forced expiratory volume in one second (FEV1), forced vital capacity (FVC), FEV1/FVC [1]. Pulmonary function assessment is crucial for diagnosing and managing respiratory diseases [2, 3], major health issues globally that contribute to more than 4 million deaths each year [4]. Additionally, pulmonary function has also been proven to be a reference for assessing the risk of cardiovascular system diseases [5,6,7,8,9].
Proposed by Wakabayashi & Daimon in 2015, the cardiometabolic index (CMI) multiplies the Waist-to-Height Ratio (WHtR) by the ratio of triglyceride (TG) to high-density lipoprotein cholesterol (HDL-C) to assess the combined effects of body fat distribution and serum lipid levels [10]. Previous studies have revealed associations between CMI and various health conditions, including diabetes, cardiovascular disease, kidney disease, and metabolic disorders, among others [11,12,13,14,15]. Meanwhile, several studies have further explored the potential threshold points of CMI in predicting the risk of certain diseases. Wakabayashi et al. [10] identified that there may be a risk of developing diabetes when the CMI exceeds 0.800 in females or 1.748 in males. CMI of roughly 0.35 might serve as a potential cutoff point for the risk of non-alcoholic fatty liver disease [16]. For hyperuricemia, the optimal threshold point of CMI was 0.485 [15].
Recently, growing attention has been focused on the connection between lipid metabolism and pulmonary function. Research indicates that spirometry, measured by tests including FEV1 and FVC along with their percentage predictions, is notably decreased in patients with metabolic syndrome (MetS) versus those without it [17]. Elevated C-reactive protein (CRP) concentrations due to increased visceral adiposity and inflammation triggered by low HDL-C levels may be potential mechanisms for impaired pulmonary function [18,19,20,21]. Leone et al. [22] found abdominal obesity to be a crucial factor in the relationship between MetS and reduced pulmonary function, and abdominal obesity is positively associated with obstructive and restrictive ventilation patterns regardless of body mass index (BMI). Adipose tissue may be an additional source of systemic inflammation, and serum CRP, a marker of systemic inflammation, may mediate the negative association of the abdominal obesity with restrictive and obstructive ventilation patterns [23, 24]. Additionally, the results of a case-control study showed that general (BMI ≥ 27 kg/m2) and central obesity (WHtR ≥ 0.5) were independent risk factors for poor asthma control in asthmatics, with adjusted ORs of 1.49 (95%CI: 1.09,2.03) and 1.62 (95%CI: 1.22,2.15), respectively [25]. In a prospective cohort study including 426,524 participants of UK Biobank, a negative association was found between HDL-C and the incidence of lung cancer [26].
However, limited research has thoroughly examined how dyslipidemia when coinciding with central obesity, impacts pulmonary function. Our study aimed to investigate CMI’s effects on pulmonary function using a wide U.S. demographic. It seeks to further reveal the relationship between lipids and lung health and to furnish essential references that could guide the prevention and management of respiratory conditions in clinical practice.
Methods
Study participants
The NHANES database is a survey conducted by the Centers for Disease Control and Prevention (CDC) every 2 years since 1960 to assess the overall health conditions of the population in the United States. The research protocol received official ethical approval [27], and written informed consent was obtained from all subjects or guardians [28]. Additional comprehensive information regarding the NHANES is available on the official website [29].
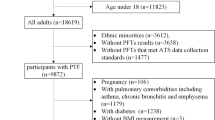
Our research utilized data from 2007 to 2012 of NHANES. 12,729 participants younger than 20, 1032 participants with a weight of 0, 9696 participants with missing data on CMI, 2019 participants with missing or low-quality spirometry data, and 841 participants with missing data on covariables were excluded. Finally, 4125 participants were involved (Fig. 1).
Study variables
CMI
The CMI, calculated using [TG (mmol/L)/HDL-C (mmol/L)] * [WHtR (cm)], served as the exposure variable [10]. We used CMI as a continuous variable and a categorical variable for association analysis to better understand the relationship between CMI and pulmonary function. To address the right-skewed distribution of the data on CMI, regression and subgroup analyses were performed by applying log2 transformations.
Pulmonary function assessment
Three indices obtained from spirometry—FEV1, FVC, and FEV1/FVC—were designed as outcome variables to evaluate pulmonary function. The NHANES spirometry program was based on standards set by the American Thoracic Society (ATS), and all health technicians underwent training in spirometry [30]. Spirometry results were analyzed by the National Institute for Occupational Safety and Health (NIOSH), which assigned five letter grades (A, B, C, D, and F) to the spirometry results recorded by each technician. To ensure data quality, our study used only data with FEV1 and FVC quality grades A and B, which were considered to meet or exceed the requirements of the ATS/ERS [31].
Covariables
Covariables were selected with reference to previously published literature [32,33,34]. Covariables included are as follows: age, gender, race, BMI, total cholesterol, education level, marital status, the ratio of family income to poverty (PIR), physical activity (PA), smoking status, alcohol intake, diabetes and hypertension. In addition, serum cotinine was also included, which is thought to reflect environmental tobacco smoke exposure status [35, 36], as well as FeNO, a non-invasive marker of airway inflammation [37, 38]. Supplementary Table S1 includes a thorough explanation of the variables and how they are categorized. A directed acyclic graph (DAG) was used to select confounders (Supplementary Figure S1) [39].
Statistical analysis
This investigation was carried out following CDC guidelines and took into account the complexity of the multistage cohort survey design [40]. R software was used for all analyses [41]. A statistically significant result was defined as P < 0.05. Continuous variables were expressed as mean and standard deviation (SD), whereas categorical variables were expressed as percentages. To manage the non-normal distribution observed in the CMI data, log2 transformations were utilized when performing association analysis. Generalized variance inflation factors and Spearman’s correlation analysis were used to check for collinearity among variables.
We built three weighted multiple linear regression models to investigate the relationship of CMI with pulmonary function. There was no covariables adjustment made to Model 1. Age, gender, and race adjustments were made to Model 2. Model 3 included adjustments for age, gender, race, BMI, total cholesterol, serum cotinine, FeNO, education level, marital status, PIR, PA, smoking status, and alcohol intake. Besides, subgroup analyses and interaction tests were performed for age, gender, BMI, PA, and smoking status. To explore possible nonlinear association, generalized additive model, smooth curve fitting, and threshold effect analysis are utilized. Additionally, sensitivity analysis was performed to confirm that the outcomes were reliable, where we excluded participants with asthma or chronic obstructive pulmonary disease (COPD) or asthma-COPD overlap (ACO).
Results
Participant characteristics
Of the 4125 individuals, 2055 were females (50.45%) and 2070 were males (49.55%) with a mean age of 44.67 ± 0.44 years. Participants were classified by the quartiles (Q) of the CMI. The average values recorded for pulmonary function indices among participants included FEV1 (3260.49 ± 19.11 mL), FVC (4191.17 ± 20.02 mL), and the FEV1/FVC ratio (0.78 ± 0.00). Participants in different CMI quartile groups showed a significant difference in age, FEV1/FVC, serum cotinine, BMI, total cholesterol, gender, race, education level, PIR, PA, smoking status, and alcohol intake (all P < 0.05) (Table 1). Nemenyi test was used to conducted post-hoc analysis among different races (Supplementary Figure S2).
Association between CMI and pulmonary function
The generalized variance inflation factors for all variables are under 5 (Supplementary Table S2), and the |r| value from the Spearman’s correlation analysis is below 0.7 (Supplementary Figure S3), suggesting there is no significant collinearity. In the weighted multiple linear regression analysis, significant association were found between CMI and pulmonary function (Table 2). In the fully adjusted model 3, the log2-CMI and FEV1 showed a negative association (β= -82.63, 95%CI: -120.56, -44.70). This negative association persisted even after the log2-CMI was converted into quartiles, and the β value of Q4 compared to Q1 was -128.49 (95% CI: -205.85, -51.13), with the effect value gradually increasing as the level of log2-CMI increased (P for trend < 0.001). Concurrently, a consistent negative association was observed between log2-CMI and FVC, with a β value of -112.92 (95% CI: -160.73, -65.11) for continuous log2-CMI and -169.01 (95% CI: -266.72, -71.30, P for trend < 0.001) for categorical log2-CMI that rose to the Q4 level. However, no significant association was found between CMI and the FEV1/FVC (P = 0.667). We performed further multivariate regression analyses of the components of CMI with FEV1 and FVC to identify the major contributors and the result showed that WHtR had the greatest effect on FEV1 and FVC (Supplementary Table S3).
Moreover, generalized additive model, smooth curve fitting, and threshold effect analysis were utilized to explore more about how CMI affects pulmonary function. The results indicated a consistent negative association between the two (Fig. 2A and B). Gender-stratified results showed a possible U-shaped association between CMI and pulmonary function in female participants (Fig. 2D and E). Based on the threshold effect analysis, results suggested that at log2-CMI < 2.33, CMI was negatively correlated with FEV1 in females (β= -93.34, 95%CI: -139.59, -47.10), however, the positive association was not significant after the inflection point, we found the same trend in the association between CMI and FVC in females, with a log2-CMI inflection point value of 2.11 (Table 3). In males, a constant negative association between CMI and pulmonary function was maintained.
Smoothed curve fitting by generalized additive model between CMI and pulmonary function. Figures A-C: all participants (A) log2-CMI and FEV1, (B) log2-CMI and FVC, (C) log2-CMI and FEV1/FVC; Figures D-F: females (D) log2-CMI and FEV1, (E) log2-CMI and FVC, (F) log2-CMI and FEV1/FVC; Figures G-H: males (G) log2-CMI and FEV1, (H) log2-CMI and FVC, (I) log2-CMI and FEV1/FVC.
Subgroup analysis
To further explore the potential factors influencing the association between CMI and FEV1 as well as CMI and FVC, subgroup analyses and interaction tests by age, gender, BMI, PA, and smoking status were performed (Supplementary Table S4). The negative association was not dependent on age, gender, BMI, PA, smoking status (all P for interaction > 0.05).
Sensitivity analysis
When 766 participants with asthma or COPD or ACO were excluded from the sensitivity analyses, the negative association between CMI and FEV1 as well as CMI and FVC remained unaffected (Supplementary Table S5). In model 3, log2-CMI maintains a negative association with FEV1, FVC (β=-87.17, 95%CI: -127.57, -46.78; β=-103.6, 95%CI: -152.42, -54.79). The association between CMI and FEV1/FVC remained non-significant (P = 0.371).
Discussion
Our analysis demonstrates that individuals with higher CMI levels tend to exhibit a restrictive pattern rather than an obstructive pattern, consistent with previous findings of studies exploring the association between MetS and pulmonary function [20, 42,43,44]. We found that for each unit increase in log2-CMI (i.e., doubling of CMI), FEV1 and FVC decreased by 82.63 mL (95% CI: -120.56, -44.70) and 112.92 mL (95% CI: -160.73, -65.11), respectively. In females, the inflection points for the nonlinear associations between CMI and FEV1 as well as CMI and FVC were 3.95 and 3.30, respectively, while in males a more constant negative relationship was consistently maintained.
Earlier studies have separately examined the relationship between various lipid indices and pulmonary function. Lee et al. [45] found that compared to the normal group, low HDL-C levels decreased FVC and FEV1 by 0.74-2.19% p and 0.86-2.68% p, respectively, and the association between FEV1/FVC and all the cholesterol markers was not significant. Another study revealed that WHtR was shown to correlate with pulmonary health, and a WHtR greater than or equal to 0.55 was significantly associated with lung aging (β = 6.393, P < 0.001). In this study, lung age was calculated based on a formula that included height and FVC. Also, among patients with MetS, the percentage of restrictive pattern (23.4%) was significantly higher than that of obstructive pattern (10.3%) and mixed pattern (7.3%) (p < 0.001) [46]. Moreover, there’s also a study that revealed a link between adiposity changes and pulmonary function deterioration. The results of a prospective cohort study including 5011 subjects (median follow-up 8 years) found negative association between the fat mass index and both FVC and FEV1 across genders, with the waist-to-hip ratio also showing a similar relationship with these spirometric parameters in males [47]. Our study builds on these studies to further investigate the combined effects of central obesity and abnormalities of lipid metabolism on pulmonary function to explore the potential synergistic effects of the two on pulmonary function, and identifies gender differences in the nonlinear relationship between CMI and pulmonary function in subsequent analyses, providing new insights into the effects of CMI on pulmonary function across genders.
The exact mechanisms regarding the association between CMI and pulmonary function have not been fully elucidated. Previous studies have illustrated the potential mechanisms of lipid metabolism for lung volume. It has been suggested that disorders of lipid metabolism can increase mechanical restriction and inflammatory responses in the lungs by altering the composition and function of surface-active substances, leading to a decrease in FVC and FEV1 [48]. Adipose deposits in the chest wall and abdomen have also been shown to potentially limit total lung capacity and lead to reduced expiratory reserve capacity by decreasing lung compliance and altering respiratory patterns [49, 50]. Since it mainly affects the mechanical expansion of the lungs, it manifests itself as a reduction in lung capacity rather than airflow obstruction [51]. Besides, it has been suggested that lung biology is fundamentally dependent on lipid transport [52]. Lungs of high-density lipoprotein-deficient apolipoprotein knockout mice were found to have varying degrees of abnormalities, including airway hyperresponsiveness, reduced alveolar development, increased oxidative stress, and collagen deposition [53, 54].
At present, the mechanisms regarding the gender difference in the association between CMI and pulmonary function have not been elucidated, and we hypothesize that they may be related to the following factors. Gender differences in lipid profiles have been commonly explored in the past, and males are thought to have riskier lipid levels than females [55, 56]. Findings have shown that males possess higher TG and lower HDL-C than females [57,58,59]. Also, several studies have revealed gender differences in lipoprotein particle size, which is considered an important consideration in assessing cardiovascular disease risk. Elevated levels of small, dense LDL are strongly associated with the risk of coronary artery disease [60,61,62], whereas large HDL appears to be protective [63, 64]. Findings have shown that males have higher concentrations of small LDL than females and much lower concentrations of large HDL [57, 65, 66]. In addition, gender differences in lipids during the life course should not be ignored [67]. In early to middle adulthood, males have higher LDL-C levels and lower HDL-C levels than females [68].
Strengths and limitations
The present study has the following strengths. First, our study examined cross-sectional data from a sizable, generally representative U.S. population, and all of our analyses took into account sampling weights to make our results generalizable and representative on a national scale; second, we employed weighted multiple linear regression analysis in conjunction with subgroup and sensitivity analyses to confirm the consistency and reliability of the results. However, we should also recognize some limitations. First, the cross-sectional design of the NHANES data limited our ability to determine a cause-and-effect relationship between CMI and pulmonary function. Second, despite our thorough attempts to account for several potential covariables, we were unable to completely exclude the effects of other unmeasured or residual confounders. Finally, sample selection bias based on study design and data quality control needs may affect the representativeness and generalizability of the study results.
Conclusions
Our findings demonstrate a negative association between levels of CMI and pulmonary function, providing a new perspective on the assessment and management of pulmonary function. More high-quality, extensive prospective research is required in the future to confirm our results and to explore the underlying mechanisms of the negative association.
Data availability
The dataset utilized for this study has been deposited into a publicly available repository, which can be found on the website: https://wwwn.cdc.gov/nchs/nhanes.
Abbreviations
- β:
-
β coefficients
- ACO:
-
Asthma-chronic obstructive pulmonary disease overlap
- ATS:
-
American Thoracic Society
- BMI:
-
Body mass index
- CDC:
-
Centers for Disease Control and Prevention
- CMI:
-
Cardiometabolic index
- COPD:
-
Chronic obstructive pulmonary disease
- CRP:
-
C-reactive protein
- DAG:
-
Directed acyclic graph
- FEV1:
-
Forced expiratory volume in one second
- FVC:
-
Forced vital capacity
- HDL-C:
-
High-density lipoprotein cholesterol
- MetS:
-
Metabolic syndrome
- NHANES:
-
National Health and Nutrition Examination Survey
- NIOSH:
-
National Institute for Occupational Safety and Health
- PA:
-
Physical activity
- PIR:
-
The ratio of family income to poverty
- Q:
-
Quartile
- SD:
-
Standard deviation
- TG:
-
Triglyceride
- WHtR:
-
Waist-to-height ratio
References
Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of Spirometry 2019 Update. An official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200(8):e70–88.
Liou TG, Kanner RE, Spirometry. Clin Rev Allergy Immunol. 2009;37(3):137–52.
Ponce MC, Sankari A, Sharma S. In: StatPearls, editor. Pulmonary function tests. Treasure Island (FL): StatPearls Publishing; 2023.
Prevalence and attributable health burden of chronic respiratory diseases. 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet Respiratory Med. 2020;8(6):585–96.
Granell R, Haider S, Deliu M, Ullah A, Mahmoud O, Fontanella S, et al. Lung function trajectories from school age to adulthood and their relationship with markers of cardiovascular disease risk. Thorax. 2024;79(8):770–7.
Higbee DH, Granell R, Sanderson E, Davey Smith G, Dodd JW. Lung function and cardiovascular disease: a two-sample Mendelian randomisation study. Eur Respir J. 2021;58(3).
Corlateanu A, Covantev S, Mathioudakis AG, Botnaru V, Cazzola M, Siafakas N. Chronic obstructive Pulmonary Disease and Stroke. Copd. 2018;15(4):405–13.
Guerra S, Sherrill DL, Venker C, Ceccato CM, Halonen M, Martinez FD. Morbidity and mortality associated with the restrictive spirometric pattern: a longitudinal study. Thorax. 2010;65(6):499–504.
Cestelli L, Gulsvik A, Johannessen A, Stavem K, Nielsen R. Reduced lung function and cause-specific mortality: a population-based study of Norwegian men followed for 26 years. Respir Med. 2023;219:107421.
Wakabayashi I, Daimon T. The cardiometabolic index as a new marker determined by adiposity and blood lipids for discrimination of diabetes mellitus. Clin Chim Acta. 2015;438:274–8.
Song J, Li Y, Zhu J, Liang J, Xue S, Zhu Z. Non-linear associations of cardiometabolic index with insulin resistance, impaired fasting glucose, and type 2 diabetes among US adults: a cross-sectional study. Front Endocrinol. 2024;15:1341828.
Wakabayashi I, Sotoda Y, Hirooka S, Orita H. Association between cardiometabolic index and atherosclerotic progression in patients with peripheral arterial disease. Clin Chim Acta. 2015;446:231–6.
Wang H, Chen Y, Sun G, Jia P, Qian H, Sun Y. Validity of cardiometabolic index, lipid accumulation product, and body adiposity index in predicting the risk of hypertension in Chinese population. Postgrad Med. 2018;130(3):325–33.
Guo Q, Wang Y, Liu Y, Wang Y, Deng L, Liao L, et al. Association between the cardiometabolic index and chronic kidney disease: a cross-sectional study. Int Urol Nephrol. 2024;56(5):1733–41.
Liu XZ, Li HH, Huang S, Zhao DB. Association between hyperuricemia and nontraditional adiposity indices. Clin Rheumatol. 2019;38(4):1055–62.
Zou J, Xiong H, Zhang H, Hu C, Lu S, Zou Y. Association between the cardiometabolic index and non-alcoholic fatty liver disease: insights from a general population. BMC Gastroenterol. 2022;22(1):20.
Chen WL, Wang CC, Wu LW, Kao TW, Chan JY, Chen YJ, et al. Relationship between lung function and metabolic syndrome. PLoS ONE. 2014;9(10):e108989.
Faber DR, van der Graaf Y, Westerink J, Visseren FL. Increased visceral adipose tissue mass is associated with increased C-reactive protein in patients with manifest vascular diseases. Atherosclerosis. 2010;212(1):274–80.
Shaaban R, Kony S, Driss F, Leynaert B, Soussan D, Pin I, et al. Change in C-reactive protein levels and FEV1 decline: a longitudinal population-based study. Respir Med. 2006;100(12):2112–20.
Rogliani P, Curradi G, Mura M, Lauro D, Federici M, Galli A, et al. Metabolic syndrome and risk of pulmonary involvement. Respir Med. 2010;104(1):47–51.
von Eckardstein A, Hersberger M, Rohrer L. Current understanding of the metabolism and biological actions of HDL. Curr Opin Clin Nutr Metab Care. 2005;8(2):147–52.
Leone N, Courbon D, Thomas F, Bean K, Jégo B, Leynaert B, et al. Lung function impairment and metabolic syndrome: the critical role of abdominal obesity. Am J Respir Crit Care Med. 2009;179(6):509–16.
Franssen FM, O’Donnell DE, Goossens GH, Blaak EE, Schols AM. Obesity and the lung: 5. Obesity and COPD. Thorax. 2008;63(12):1110–7.
Mannino DM, Ford ES, Redd SC. Obstructive and restrictive lung disease and markers of inflammation: data from the Third National Health and Nutrition Examination. Am J Med. 2003;114(9):758–62.
Huang HL, Huang YJ, Chu YC, Chen CW, Yang HC, Hwang JS, et al. Exploring factors underlying poorly-controlled asthma in adults by integrating phenotypes and Genotypes Associated with obesity and asthma: a case-control study. J Asthma Allergy. 2023;16:135–47.
Wang J, Wang Q, Shi Z, Yan X, Lei Z, Zhu W. Serum lipid levels, genetic risk, and lung cancer incidence: A large prospective cohort study. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2024.
National Health and Nutrition Examination Survey. NCHS Ethics Review Board (ERB) Approval*. National Center for Health Statistics. https://www.cdc.gov/nchs/nhanes/irba98.htm. Accessed 10 May 2024.
National Health and Nutrition Examination Survey. NCHS Ethics Review Board (ERB) Approval*. Centers for Disease Control and Prevention (CDC). https://search.cdc.gov/search/?query=Centers for Disease Control and Prevention CDC.&siteLimit=NCHS&dpage=1. Accessed 10 May 2024.
National Health and Nutrition Examination Survey. NHANES Questionnaires, Datasets, and Related Documentation. National Center forHealth Statistics. https://wwwn.cdc.gov/Nchs/Nhanes/. Accessed 10 May 2024.
National Health and Nutrition Examination Survey (NHANES). Respiratory Health Spirometry Procedures Manual. https://wwwn.cdc.gov/nchs/data/nhanes/2011-2012/manuals/spirometry_procedures_manual.pdf. Accessed 10 May 2024.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–38.
Tan MY, Wang JT, Wang GP, Zhu SX, Zhai XL. The Association between Dietary Magnesium Intake and pulmonary function: recent fndings from NHANES 2007–2012. Biological trace element research. 2024.
Weng L, Xu Z, Chen Y, Chen C. Associations between the muscle quality index and adult lung functions from NHANES 2011–2012. Front Public Health. 2023;11:1146456.
Mao H, Lin T, Huang S, Xie Z, Jin S, Shen X, et al. The impact of brominated flame retardants (BFRs) on pulmonary function in US adults: a cross-sectional study based on NHANES (2007–2012). Sci Rep. 2024;14(1):6486.
Boffetta P, Clark S, Shen M, Gislefoss R, Peto R, Andersen A. Serum cotinine level as predictor of lung cancer risk. Cancer Epidemiol Biomarkers Prevention: Publication Am Association Cancer Res Cosponsored Am Soc Prev Oncol. 2006;15(6):1184–8.
Eisner MD. Environmental tobacco smoke exposure and pulmonary function among adults in NHANES III: impact on the general population and adults with current asthma. Environ Health Perspect. 2002;110(8):765–70.
ATS Workshop Proceedings: Exhaled nitric oxide and nitric oxide oxidative metabolism in exhaled breath condensate: Executive summary. American journal of respiratory and critical care medicine. 2006;173(7):811-3.
Dweik RA, Boggs PB, Erzurum SC, Irvin CG, Leigh MW, Lundberg JO, et al. An official ATS clinical practice guideline: interpretation of exhaled nitric oxide levels (FENO) for clinical applications. Am J Respir Crit Care Med. 2011;184(5):602–15.
Tennant PWG, Murray EJ, Arnold KF, Berrie L, Fox MP, Gadd SC, et al. Use of directed acyclic graphs (DAGs) to identify confounders in applied health research: review and recommendations. Int J Epidemiol. 2021;50(2):620–32.
Johnson CL, Paulose-Ram R, Ogden CL, Carroll MD, Kruszon-Moran D, Dohrmann SM et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital and health statistics Series 2, Data evaluation and methods research. 2013;(161):1–24.
The R Project for Statistical Computing. https://www.r-project.org/. Accessed 10 May 2024.
Ford ES, Cunningham TJ, Mercado CI. Lung function and metabolic syndrome: findings of National Health and Nutrition Examination Survey 2007–2010. J Diabetes. 2014;6(6):603–13.
Godfrey MS, Jankowich MD. The vital capacity is vital: epidemiology and clinical significance of the restrictive spirometry pattern. Chest. 2016;149(1):238–51.
Fimognari FL, Pasqualetti P, Moro L, Franco A, Piccirillo G, Pastorelli R et al. The association between metabolic syndrome and restrictive ventilatory dysfunction in older persons. The journals of gerontology Series A, Biological sciences and medical sciences. 2007;62(7):760–5.
Lee C, Cha Y, Bae SH, Kim YS. Association between serum high-density lipoprotein cholesterol and lung function in adults: three cross-sectional studies from US and Korea National Health and Nutrition Examination Survey. BMJ open Respiratory Res. 2023;10(1).
Molina-Luque R, Romero-Saldaña M, Álvarez-Fernández C, Rodríguez-Guerrero E, Hernández-Reyes A, Molina-Recio G. Waist to height ratio and metabolic syndrome as lung dysfunction predictors. Sci Rep. 2020;10(1):7212.
Park Y, Kim J, Kim YS, Leem AY, Jo J, Chung K, et al. Longitudinal association between adiposity changes and lung function deterioration. Respir Res. 2023;24(1):44.
Agudelo CW, Samaha G, Garcia-Arcos I. Alveolar lipids in pulmonary disease. A review. Lipids Health Dis. 2020;19(1):122.
Baffi CW, Winnica DE, Holguin F. Asthma and obesity: mechanisms and clinical implications. Asthma Res Pract. 2015;1:1.
Dixon AE, Peters U. The effect of obesity on lung function. Expert Rev Respir Med. 2018;12(9):755–67.
Sin DD, Jones RL, Man SF. Obesity is a risk factor for dyspnea but not for airflow obstruction. Arch Intern Med. 2002;162(13):1477–81.
Fessler MB. A New Frontier in Immunometabolism. Cholesterol in Lung Health and Disease. Annals Am Thorac Soc. 2017;14(Supplement5):S399–405.
Massaro D, Massaro GD. Apoetm1Unc mice have impaired alveologenesis, low lung function, and rapid loss of lung function. Am J Physiol Lung Cell Mol Physiol. 2008;294(5):L991–7.
Wang W, Xu H, Shi Y, Nandedkar S, Zhang H, Gao H, et al. Genetic deletion of apolipoprotein A-I increases airway hyperresponsiveness, inflammation, and collagen deposition in the lung. J Lipid Res. 2010;51(9):2560–70.
Rochlani Y, Pothineni NV, Mehta JL. Metabolic syndrome: does it Differ between women and men? Cardiovasc Drugs Ther. 2015;29(4):329–38.
Johnson JL, Slentz CA, Duscha BD, Samsa GP, McCartney JS, Houmard JA, et al. Gender and racial differences in lipoprotein subclass distributions: the STRRIDE study. Atherosclerosis. 2004;176(2):371–7.
McNamara JR, Campos H, Ordovas JM, Peterson J, Wilson PW, Schaefer EJ. Effect of gender, age, and lipid status on low density lipoprotein subfraction distribution. Results from the Framingham offspring study. Arterioscler (Dallas Tex). 1987;7(5):483–90.
Brown SA, Hutchinson R, Morrisett J, Boerwinkle E, Davis CE, Gotto AM Jr. et al. Plasma lipid, lipoprotein cholesterol, and apoprotein distributions in selected US communities. The atherosclerosis risk in communities (ARIC) Study. Arteriosclerosis and thrombosis: a journal of vascular biology. 1993;13(8):1139–58.
Després JP, Couillard C, Gagnon J, Bergeron J, Leon AS, Rao DC, et al. Race, visceral adipose tissue, plasma lipids, and lipoprotein lipase activity in men and women: the Health, Risk factors, Exercise Training, and Genetics (HERITAGE) family study. Arterioscler Thromb Vasc Biol. 2000;20(8):1932–8.
Austin MA, Breslow JL, Hennekens CH, Buring JE, Willett WC, Krauss RM. Low-density lipoprotein subclass patterns and risk of myocardial infarction. JAMA. 1988;260(13):1917–21.
Lamarche B, Tchernof A, Moorjani S, Cantin B, Dagenais GR, Lupien PJ, et al. Small, dense low-density lipoprotein particles as a predictor of the risk of ischemic heart disease in men. Prospective results from the Québec Cardiovascular Study. Circulation. 1997;95(1):69–75.
Gardner CD, Fortmann SP, Krauss RM. Association of small low-density lipoprotein particles with the incidence of coronary artery disease in men and women. JAMA. 1996;276(11):875–81.
Ballantyne FC, Clark RS, Simpson HS, Ballantyne D. High density and low density lipoprotein subfractions in survivors of myocardial infarction and in control subjects. Metab Clin Exp. 1982;31(5):433–7.
Johansson J, Carlson LA, Landou C, Hamsten A. High density lipoproteins and coronary atherosclerosis. A strong inverse relation with the largest particles is confined to normotriglyceridemic patients. Arterioscler Thrombosis: J Vascular Biology. 1991;11(1):174–82.
Haffner SM, Mykkänen L, Valdez RA, Paidi M, Stern MP, Howard BV. LDL size and subclass pattern in a biethnic population. Arterioscler Thrombosis: J Vascular Biology. 1993;13(11):1623–30.
Lemieux I, Pascot A, Lamarche B, Prud’homme D, Nadeau A, Bergeron J, et al. Is the gender difference in LDL size explained by the metabolic complications of visceral obesity? Eur J Clin Invest. 2002;32(12):909–17.
Holven KB, van Roeters J. Sex differences in lipids: a life course approach. Atherosclerosis. 2023;384:117270.
Wang X, Magkos F, Mittendorfer B. Sex differences in lipid and lipoprotein metabolism: it’s not just about sex hormones. J Clin Endocrinol Metab. 2011;96(4):885–93.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
C.Y. Mo and J.L. Pu did the study conception, design, statistical analysis, results interpretation, and first draft. J.L. Pu participated in data collection and results discussion. Finally, Y.F. Zheng and Y.L. Li functioned as the final reviewers and corresponding authors. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The Research Ethics Review Board of the National Center for Health Statistics approved the study protocol. All subjects or guardians of the subjects provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mo, CY., Pu, JL., Zheng, YF. et al. The relationship between cardiometabolic index and pulmonary function among U.S. adults: insights from the National Health and Nutrition Examination Survey (2007–2012). Lipids Health Dis 23, 246 (2024). https://doi.org/10.1186/s12944-024-02235-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02235-5