Abstract
Background
Remnant cholesterol (RC) reportedly contributes to the development of diabetes mellitus. However, evidence on the relationship between maternal RC and the risk of developing gestational diabetes mellitus (GDM) during pregnancy is limited. This study aimed to assess the relationship between maternal RC and GDM risk during early pregnancy, and explore the potential pathways involved in the relationship between RC levels and GDM risk.
Methods
From 2018 to 2021, a prospective birth cohort study was designed and carried out in China. The associations of maternal RC and other lipid parameters with GDM risk were estimated using logistic regression models and restricted cubic splines. Subgroup analyses were performed stratified by prepregnancy body mass index (pre-BMI), maternal age and gravidity. Mediation analyses were conducted to explore the mediating effect of some related factors on the relationship between RC levels and the risk of GDM.
Results
A total of 33,018 pregnant women were included. The median RC level was 0.47 ± 0.20 mmol/L. The prevalence of GDM was 15.19%. As RC quartiles increased, the incidence of GDM increased substantially, reaching 19.24% for the highest quartile of RC (P < 0.001). Maternal RC in the first trimester was positively correlated with GDM risk (OR: 2.254, 95% CI: 1.943–2.615). Compared to the lowest RC quartile, higher RC quartiles were correlated with an increased risk of GDM, and the ORs (95% CIs) for Q3 and Q4 were 1.208 (1.101–1.325) and 1.489 (1.364–1.626), respectively. Moreover, a linear dose–response relationship was found for this association (P for all < 0.001, P for nonlinearity > 0.05) and was consistent across subgroups with different pre-BMIs, maternal ages and gravidities (all P values for interactions > 0.05). Furthermore, the correlation between RC level and GDM risk was partially mediated by pre-BMI (9.20%) and blood glucose level (-11.1%).
Conclusions
Higher maternal RC levels in the early stage of pregnancy was positively associated with an increased risk of developing GDM. This association was partially mediated by pre- BMI and blood glucose levels.
Similar content being viewed by others
Background
Gestational diabetes mellitus (GDM) is a prevalent complication during pregnancy. Over recent years, the GDM incidence has increased steadily, and approximately 14% of all pregnancies were affected by GDM worldwide [1]. Epidemiological studies have shown that GDM increases unfavorable outcomes for both mothers and newborns. Pregnant women with GDM are at high risk of perinatal morbidity, including pregnancy-induced hypertension, cesarean section, shoulder dystocia and labor induction. Babies born to mothers who have GDM are prone to macrosomia, preterm delivery, low one-minute Apgar scores, large for gestational age and neonatal hypoglycemia [2]. In the long term, GDM sequelae are significantly related with maternal glucose metabolism disorders and cardiovascular disease [2, 3]. A comprehensive meta-analysis encompassing 20 studies and a total of 1,332,373 participants revealed that the risk of developing type 2 diabetes mellitus (T2DM) in women who experienced GDM was ten-fold greater compared to those who maintained a normal glucose levels throughout pregnancy [4]. Offspring born to mothers who had a GDM history face an increased likelihood of experiencing childhood adiposity and cardiovascular disease markers in their adult years [5, 6]. Therefore, identifying potential risk factors for GDM is essential as it could help with early prevention to decrease the risk of GDM development and adverse outcomes for both mothers and newborns.
Several well-established risk factors for GDM include being an older mother, having a history of GDM, a family history of diabetes, being overweight or obesity before pregnancy and gaining too much weight during pregnancy [1, 7]. Recently, Hu et al. conducted a meta-analysis encompassing 292 studies and a total of 97,880 women (28,232 with GDM and 69,648 controls), confirming that maternal dyslipidemia is significantly associated with GDM. Further analysis revealed that among total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-c) and high-density lipoprotein cholesterol (HDL-c) levels, TG level was the most crucial element linked to GDM. During pregnancy, women who diagnosed GDM had 20% higher TG levels compared to those without GDM and elevated TG levels occur in the first trimester and throughout pregnancy [8]. A study utilizing Mendelian randomization techniques indicated that TG demonstrated notable bidirectional causal relationship with the levels of fasting insulin, whereas HDL-c and LDL-c had weaker or nonexistent impacts on glycemic characteristics [9]. Remnant cholesterol (RC) is defined as a lipoprotein cholesterol rich in TGs, which includes intermediate and very low-density lipoproteins in the fasted state and chylomicron remnants in the nonfasted state [10]. Emerging evidence has shown that RC contributes to the development of T2DM, cardiovascular risk and overall mortality in the general population [11,12,13,14], and RC is believed to change in the early stage of T2DM development, even before glucose abnormalities [15]. Although two studies have investigated the correlations between maternal RC levels and GDM risk in pregnant women [16, 17], more evidence is needed to confirm this association during pregnancy and explore the potential pathways involved in the relationships between maternal RC levels and GDM risk. This will help to prevent GDM and improve pregnancy outcomes.
The objectives of this research were (1) to explore the associations of maternal RC during the first trimester with GDM risk based on a large population in China; (2) to investigate these associations among subgroups with different maternal ages, prepregnancy body mass index (pre-BMIs) and gravidities; and (3) to explore the potential pathways between RC and GDM risk. This prospective birth cohort study was designed based on the China Birth Cohort Study (CBCS) to solve the above questions.
Methods
Research design and participants
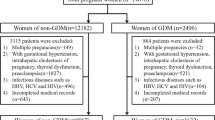
This cohort study was performed at Beijing Obstetrics and Gynecology Hospital, Capital Medical University, from February 2018 to December 2021. The participants were enrolled at 6–13+6 gestational weeks in the present study following the inclusion criteria of CBCS [18]. A total of 40,549 singleton pregnancies in pregnant women were included and followed up until the completion of pregnancy. To reduce the risk of data bias, pregnant women who were diagnosed with prediabetes mellitus (n = 977) or hypertension before pregnancy (n = 1,040) were excluded. Pregnant women who had missing laboratory data (n = 3,904) or incomplete baseline data (n = 1,610) were excluded. In the analysis, 33,018 pregnant women were ultimately included. According to previous publications, odds ratio between RC and GDM risk was 1.458 [16], with the prevalence of GDM was approximately 15% [19, 20]. The estimated sample size required 1199, which allowed us to explore the relationship between RC level and GDM. This estimation assumes an alpha of 0.05 (probability of type I error) and delta of 0.10 (admissible error). Therefore, the current participants achieved a level for strong statistical power. This study adhered to the Declaration of Helsinki on medical protocols and ethics. Written informed consent forms were signed by each participant. The research protocol was received approval from the Ethics Committee of the Beijing Obstetrics and Gynecology Hospital, Capital Medical University (2018-KY-003–02).
Data acquisition
The baseline characteristics of the participants were obtained using an electronic standardized questionnaire at enrollment. Demographic information consisted of birthdates, ethnicity, levels of education, employment status, height, prepregnancy weight, family annual income, alcohol consumption, smoking status, fertilization method, gravidity, maternal health records, and the date of last menstrual period. Pregnancy women were divided into three groups according to their pre-BMIs: those with a pre-BMI < 24 kg/m2 were normal weight, those with a pre-BMI between 24 and 28 kg/m2 were considered overweight and those with a pre-BMI ≥ 28 kg/m2 were classified as obesity [21]. The date of last menstrual period was verified through ultrasound at baseline.
Data on maternal fasting blood glucose (FBG), levels of TC, TG, HDL-c, and LDL-c in early pregancy were acquired from medical records of the hospital. These indicators were detected following a standard operating procedure with an automated chemistry/immunology analyzer. RC (mmol/L) was derived using the formula: TC (mmol/L)-HDC-c (mmol/L)-LDL-c (mmol/L).
Outcomes
During 24–28 weeks of gestation, all participants underwent a 75-g oral glucose tolerance test (OGTT) following the guidelines of the International Association of Diabetes and Pregnancy Study Groups (IADPSG) [19]. GDM was diagnosed based on the following criteria: if the blood glucose level exceeded 92 mg/dL (5.1 mmol/L) during fasting, if the glucose level was above 180 mg/dL (10.0 mmol/L) 1 h after glucose intake, or above 153 mg/dL (8.5 mmol/L) 2 h post glucose intake.
Statistical analyses
The mean ± standard deviation (SD) is utilized for displaying continuous variables exhibiting a normal distribution, while median along with the interquartile range (IQR) is used to express variables having a skewed distribution. The assessment of normally distributed continuous variables was conducted utilizing one-way analysis of variance (ANOVA), whereas the Kruskal–Wallis test served as the evaluative method for those exhibiting a skewed distribution. For categorical variables, frequencies (%) are expressed and comparisons were made using the χ2 test.
This study divided the participants into four groups based on RC quartiles. To explore the relationship between maternal RC and the likelihood of developing GDM, a logistic regression model was employed. Three models were used in the present analyses. The first model (Model 1) was not adjusted for any variables. The second model (Model 2) was corrected for the age of mothers, maternal ethnicity, status of employment, maternal education, levels of family annual income, prep-BMI, alcohol consumption status, smoking status, fertilization method and gravidity. The third model (Model 3), built upon Model 2, included adjustment for the FBG level in the first trimester of pregnancy. To analyze the nonlinear dose‒response association between RC and GDM risk, a restricted cubic spline was employed, using four knots at the 5th, 35th, 65th and 95th percentiles. Adjustment for all potential confounding factors was made to calculate the odds ratio (OR) and 95% confidence interval. Subgroup analyses were conducted according to maternal age (< 35 years, ≥ 35 years), pre-BMI (≤ 18.5 kg/m2, 18.5–24 kg/m2, > 24 kg/m2) and gravidity (first pregnancy and > 1 pregnancy) via a logistic regression model. Mediation analyses were performed to examine whether the associations were mediated by related factors. In the analyses, the predictor variable was maternal RC; the mediators were the prep-BMI and FBG level; and the outcome variable was GDM. Mediation analysis was also adjusted for the age of mothers, maternal ethnicity, status of employment, maternal education, pre-BMI, levels of family annual income, alcohol consumption status, smoking status, fertilization method, gravidity, and fasting blood glucose level in early pregnancy, unless the variable was used as a modifier.
Differences were considered statistically significant for two-tailed tests with P < 0.05. The study utilized SAS version 9.3 (SAS Institute, Inc., North Carolina) for all data analyses.
Results
Participant characteristics
The baseline characteristics of 33,018 pregnant women according to the RC quartiles are shown in Table 1. Significant differences were observed in maternal age, family annual income, employment status, education level, pre-BMI, alcohol consumption status, the method of fertilization and gravidity among the four quartile groups (all P < 0.001). The overall mean age of participants was 31.96 ± 3.83 years at delivery. As the RC quartiles increased, the participants tended to be older, the percentage of obese individuals increased significantly, more participants became pregnant using assisted reproductive technology, and more participants had multiple pregnancies (all P < 0.001). Moreover, the mean RC level of all participants was 0.47 ± 0.20 mmol/L. In the first trimester, all the laboratory measurements, including the FBG, TG, TC, HDL-c and LDL-c levels, were significantly different across the four RC quartile groups (all P < 0.001). Additionally, of all participants, 5,017 (15.19%) pregnant women developed GDM. The prevalence of GDM increased substantially with increasing RC quartile (P < 0.001), reaching 19.24% in the highest RC quartile (Table 1).
Association of maternal RC levels with GDM risk
The relationships between maternal RC levels and GDM risk in early pregnancy determined by logistic regression models are shown in Table 2. A significant relationship between maternal RC levels and GDM risk was found (OR: 2.254, 95% CI: 1.943–2.615). In addition, an increased risk of GDM was observed with increasing RC quartiles compared with the lowest RC quartile. Following adjustments for confounding variables, the ORs and 95% CIs for Q2, Q3 and Q4 were 1.086 (0.991–1.190), 1.208 (1.101–1.325) and 1.489 (1.364–1.626), respectively (Table 2). Further analysis with multivariable-adjusted restricted cubic splines revealed a linear relationship between RC levels and GDM risk (P for all < 0.001, P for nonlinearity = 0.425; Fig. 1). Subgroup analyses confirmed that the correlation between RC levels and GDM risk remained consistent across subgroups with different maternal ages, pre-BMIs and gravidities (Table 3).
Associations between maternal lipid parameters in the first trimester and the risk of GDM, plotted with restricted cubic splines. Odds ratios and 95% CI were estimated using logistic regression model adjusted for maternal age, ethnicity, education, employment, family annually income, smoking, alcohol consumption, pre-pregnancy BMI, fertilization way, first pregnancy and fasting blood glucose in first trimester. GDM, gestational diabetes mellitus; RC, remnant cholesterol
Mediation analysis of the association between maternal RC and GDM risk
To explore the potential pathways between maternal RC levels and GDM risk, mediation analyses were performed using the factors related to pre-BMI and fasting blood glucose levels in the first trimester as potential mediators. The results revealed that pre-BMI partially mediated the relationship between maternal RC and GDM risk. The direct effect was 0.0097 (95% CI: 0.0072, 0.0100), and the mediation proportion was 9.20% (Fig. 2A). In contrast, a negative mediating effect of FBG levels was found on the relationship between RC and GDM risk. The direct effect was -0.0099 (95% CI: -0.0134, -0.0100), and the mediation proportion was -11.10% (Fig. 2B).
Mediation analyses of association between maternal RC and GDM. A contribution of pre-pregnancy BMI; B contribution of FBG. ***P < 0.001. Adjusted for maternal age, ethnicity, education, employment, family annually income, smoking, alcohol consumption, pre-pregnancy BMI, fertilization way, first pregnancy, fasting blood glucose in the first trimester of pregnancy, unless the one used as a modifier. RC, remnant cholesterol; GDM, gestational diabetes mellitus; pre-pregnancy BMI, pre-pregnancy body mass index; FBG and fasting blood glucose
Discussion
In this prospective birth cohort study of 33,018 pregnant women, we observed a linear upward trend in the risk of GDM with increasing maternal RC in the first trimester of pregnancy. This association was consistent across subgroups with different maternal ages, pre-BMIs and gravidities. Further analyses revealed that both pre-BMI and FBG levels partially contributed to these pathways.
Elevated lipid levels during pregnancy are correlated with the likelihood of developing GDM. Pregnant women with GDM displayed elevated levels of TC, TGs, and LDL-c, along with decreased levels of HDL-c than pregnant women without GDM [8]. Moreover, remnant cholesterol contains more cholesterol, which is believed to be more detrimental to pancreatic β-cells and more closely associated with insulin resistance [22, 23]. Previous research has indicated that RC levels were linked to prediabetes, T2DM development and glucose metabolism in the general population[11, 13, 14, 24,25,26] and this association is more significant in females [14, 25]. The findings of the present study also demonstrated that elevated maternal RC levels in the early stage of pregnancy increased the likelihood of GDM development. This result aligns with the findings of two recent studies investigating pregnant women. A prospective cohort study including 2528 participants was designed by Wang et al. and they demonstrated that increased RC levels during gestational weeks 16–17 were independent of traditional risk factors for GDM [17]. Another secondary analysis with 590 singleton participants based on a prospective cohort study showed similar results: higher levels of RC were significantly associated with GDM risk. They further found that pregnant women whose RC level is more than 24.30 mg/dL were at a high risk of developing GDM [16]. These results suggest that more attention should be given to RC levels during early pregnancy in clinical practice to identify GDM risk beyond traditional lipid parameters. In addition, a linear dose‒response relationship was also found between maternal RC and the risk of GDM in this study, which is in line with previous research showing a continuous correlation between RC levels and GDM risk in pregnant women [17]. Previous studies reported different results in the general population and illustrated a nonlinear relationship between elevated RC levels and T2DM or prediabetes risk [11, 13, 26].
RC is considered a new predictor of hyperglycemia that is better than traditional lipid parameters both in the general population and in pregnant women [14, 16, 27]. Huh et al. performed a cohort study involving 8,485,539 adults and reported that the relationship between RC and incident T2DM risk was more significant in younger and obese participants [13]. Previous studies also reported that individuals at low risk of T2DM who had a high level of RC were more likely to develop T2DM [13, 15]. These results suggest that although the relationship between maternal RC and GDM risk was not affected in the different subgroups in the present study, extra care should be given to pregnant women who have a low risk of GDM and high levels of RC.
The potential mediating effects of homeostasis model assessment of insulin resistance (HOMA-IR), high-sensitivity C-reactive protein (Hs-CRP) and white blood cell (WBC) counts levels on the correlation between RC levels and diabetes mellitus (DM) risk were investigated in the general population, and the results suggested that there was a partial mediation of the correlation between RC and the risk of diabetes mellitus by insulin resistance and inflammation [25]. However, at present, no mediation analysis on the relationship between maternal RC and GDM risk in pregnant women has been performed. The present study revealed that participants with increased levels of RC, particularly those in the Q4 group, had significantly greater pre-BMIs than did those with lower RC levels and showed that pre-BMI partially contributed to the correlation between maternal RC and GDM risk. Additionally, a negative mediating effect of FBG levels on this association was shown. In line with the present study, Choi et al. reported a negative relationship between remnant lipoprotein levels and fasting glucose levels in 135 healthy children and adolescents, although the difference was not significant [28].
The molecular mechanism underlying the correlation between RC levels and GDM risk is not fully understood. Insulin resistance and β-cell malfunction are the main factors that may explain this association. A previous study showed that elevated RC could promote increased inflammatory levels [29] and subsequently contribute to insulin resistance [22, 30]. In addition, higher RC levels may decrease the activity of glucokinase and affect the function of β-cells, leading to a reduction in glucose-stimulated insulin secretion and GDM development [31].
Strengths and limitations of the study
This birth cohort study involved a large sample to comprehensively evaluate the relationship between the levels of maternal RC in the early stage of pregnancy and GDM risk. The contributions of related factors in the pathways between RC and GDM risk were investigated. Several limitations of the current research warrant discussion. First, this study was carried out at a single-center study. Even though it included a substantial sample size, the findings of this study were not nationally representative. Second, the levels of maternal lipids were only collected in early pregnancy and were not available for the second trimester. Therefore, information on lipid changes was not obtained. Third, the level of RC was not measured in this study. Maternal RC was calculated following the guidelines set by European Atherosclerosis Society in 2019 [32]. It has been reported that calculated RC levels could be an alternative to measured RC levels for estimating the risk of many diseases, as they are highly correlated [33, 34]. Finally, the structured questionnaire used at enrollment was a self-report questionnaire. However, doctors, nurses and trained researchers provided guidance to participants.
Conclusion
Elevated maternal RC in the early stage of pregnancy increased the likelihood of GDM development, and this association was partially mediated by pre-BMI and blood glucose levels. These findings indicated that monitoring the levels of RC during early pregnancy may help to prevent GDM in a timely manner.
Availability of data and materials
Anonymized data are available upon reasonable request.
Data Availability
No datasets were generated or analysed during the current study.
Abbreviations
- RC:
-
Remnant cholesterol
- GDM:
-
Gestational diabetes mellitus
- T2DM:
-
Type 2 diabetes mellitus
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- LDL-c:
-
Low density lipoprotein-cholesterol
- HDL-c:
-
High density lipoprotein cholesterol
- CBCS:
-
The China Birth Cohort Study
- BMI:
-
Body mass index
- FBG:
-
Fasting blood glucose
- OGTT:
-
Oral glucose tolerance test
- IADPSG:
-
International Association of Diabetes and Pregnancy Study Groups
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- ANOVA:
-
One-way analysis of variance
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- WBCs:
-
White blood cells
- Hs-CRP:
-
High-sensitivity C-reactive protein
References
Juan J, Yang H. Prevalence, prevention, and lifestyle intervention of gestational diabetes mellitus in China. Int J Environ Res Public Health. 2020;17(24):9517.
Ye W, Luo C, Huang J, et al. Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis. BMJ. 2022;377:e067946.
Farrar D, Simmonds M, Bryant M, et al. Hyperglycaemia and risk of adverse perinatal outcomes: systematic review and meta-analysis. BMJ. 2016;354:i4694.
Vounzoulaki E, Khunti K, Abner SC, et al. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361.
Lowe WL Jr, Scholtens DM, Lowe LP, et al. Association of gestational diabetes with maternal disorders of glucose metabolism and childhood adiposity. JAMA. 2018;320(10):1005–16.
American DA. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14–31.
Zhang C, Rawal S, Chong YS. Risk factors for gestational diabetes: is prevention possible? Diabetologia. 2016;59(7):1385–90.
Hu J, Gillies CL, Lin S, et al. Association of maternal lipid profile and gestational diabetes mellitus: a systematic review and meta-analysis of 292 studies and 97,880 women. EClinicalMedicine. 2021;34:100830.
Zhu Z, Wang K, Hao X, et al. Causal graph among serum lipids and glycemic traits: a mendelian randomization study. Diabetes. 2022;71(8):1818–26.
Varbo A, Benn M, Nordestgaard BG. Remnant cholesterol as a cause of ischemic heart disease: evidence, definition, measurement, atherogenicity, high risk patients, and present and future treatment. Pharmacol Ther. 2014;141(3):358–67.
Yuan L, Liu J, Huang Z, et al. Elevated remnant cholesterol increase 6-year type 2 diabetes mellitus onset risk. Clin Chim Acta. 2023;541:117253.
Varbo A, Freiberg JJ, Nordestgaard BG. Extreme nonfasting remnant cholesterol vs extreme LDL cholesterol as contributors to cardiovascular disease and all-cause mortality in 90000 individuals from the general population. Clin Chem. 2015;61(3):533–43.
Huh JH, Roh E, Lee SJ, et al. Remnant Cholesterol Is an Independent Predictor of Type 2 Diabetes: A Nationwide Population-Based Cohort Study. Diabetes Care. 2023;46(2):305–12.
Xie G, Zhong Y, Yang S, et al. Remnant Cholesterol is an Independent Predictor of New-Onset Diabetes: A Single-Center Cohort Study. Diabetes Metab Syndr Obes. 2021;14:4735–45.
Carvalho LSF, Bensenor IM, Nogueira ACC, et al. Increased particle size of triacylglycerol-enriched remnant lipoproteins, but not their plasma concentration or lipid content, augments risk prediction of incident type 2 diabetes. Diabetologia. 2021;64(2):385–96.
Gao Y, Hu Y, Xiang L. Remnant cholesterol, but not other cholesterol parameters, is associated with gestational diabetes mellitus in pregnant women: a prospective cohort study. J Transl Med. 2023;21(1):531.
Wang W, Li N, Wang X, et al. Remnant cholesterol is associated with gestational diabetes mellitus: a cohort study. J Clin Endocrinol Metab. 2023;108(11):2924–30.
Yue W, Zhang E, Liu R, et al. The China birth cohort study (CBCS). Eur J Epidemiol. 2022;37(3):295–304.
Zhang E, Su S, Gao S, et al. Elevated serum uric acid to creatinine ratio is associated with adverse pregnancy outcomes: a prospective birth cohort study. Int J Med Sci. 2024;21(9):1612–21.
Gao S, Su S, Zhang E, et al. Association between gestational cardiovascular health in the first trimester and pregnancy outcomes in the China birth cohort. Public Health. 2024;232:100–7.
Zhou B, Coorperative Meta-Analysis Group Of China Obesity Task F. [Predictive values of body mass index and waist circumference to risk factors of related diseases in Chinese adult population]. Zhonghua Liu Xing Bing Xue Za Zhi. 2002;23(1):5–10.
Ohnishi H, Saitoh S, Takagi S, et al. Relationship between insulin-resistance and remnant-like particle cholesterol. Atherosclerosis. 2002;164(1):167–70.
Sokooti S, Flores-Guerrero JL, Heerspink HJL, et al. Triglyceride-rich lipoprotein and LDL particle subfractions and their association with incident type 2 diabetes: the PREVEND study. Cardiovasc Diabetol. 2021;20(1):156.
Peng J, Zhao F, Yang X, et al. Association between dyslipidemia and risk of type 2 diabetes mellitus in middle-aged and older Chinese adults: a secondary analysis of a nationwide cohort. BMJ Open. 2021;11(5):e042821.
Hu X, Liu Q, Guo X, et al. The role of remnant cholesterol beyond low-density lipoprotein cholesterol in diabetes mellitus. Cardiovasc Diabetol. 2022;21(1):117.
Li M, Zhang W, Zhang M, et al. Nonlinear relationship between untraditional lipid parameters and the risk of prediabetes: a large retrospective study based on Chinese adults. Cardiovasc Diabetol. 2024;23(1):12.
Hadi Alijanvand M, Aminorroaya A, Kazemi I, et al. Prevalence and predictors of prediabetes and its coexistence with high blood pressure in first-degree relatives of patients with type 2 diabetes: A 9-year cohort study. J Res Med Sci. 2020;25:31.
Choi YJ, Jo YE, Kim YK, et al. High plasma concentration of remnant lipoprotein cholesterol in obese children and adolescents. Diabetes Care. 2006;29(10):2305–10.
Varbo A, Benn M, Tybjaerg-Hansen A, et al. Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation. 2013;128(12):1298–309.
Funada J, Sekiya M, Otani T, et al. The close relationship between postprandial remnant metabolism and insulin resistance. Atherosclerosis. 2004;172(1):151–4.
Hao M, Head WS, Gunawardana SC, et al. Direct effect of cholesterol on insulin secretion: a novel mechanism for pancreatic beta-cell dysfunction. Diabetes. 2007;56(9):2328–38.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88.
Jepsen AM, Langsted A, Varbo A, et al. Increased remnant cholesterol explains part of residual risk of all-cause mortality in 5414 patients with ischemic heart disease. Clin Chem. 2016;62(4):593–604.
Varbo A, Nordestgaard BG. Remnant lipoproteins. Curr Opin Lipidol. 2017;28(4):300–7.
Acknowledgements
We sincerely thank all participants and researchers in eligible studies.
Funding
This work was supported by grants from The National Key Research and Development Program of China (2016YFC1000101), Beijing Hospitals Authority Youth Programme (No. QML20231407), R&D Program of Beijing Municipal Education Commission (KM202310025006) and Leading Talents in the Construction Project of High Level Public Health Technical Talents in Beijing (2022–1-003).
Author information
Authors and Affiliations
Contributions
CY, RL, WY, EZ and SS designed the study and interpreted the results. SS and EZ wrote the original draft and performed the formal analysis. SG, YZ, JH, SX, JY and QZ collected data. All authors reviewed and approved the final version of manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the Beijing Obstetrics and Gynecology Hospital, Capital Medical University (2018-KY-003–02). The written informed consent was signed by all the participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Su, S., Zhang, E., Gao, S. et al. Associations of remnant cholesterol in early pregnancy with gestational diabetes mellitus risk: a prospective birth cohort study. Lipids Health Dis 23, 243 (2024). https://doi.org/10.1186/s12944-024-02230-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12944-024-02230-w